Abstract
Aim: Information on the epidemiology of multiresistant bacteria (MRB) with zoonotic potential is growing but still remains quite incomplete. This narrative mini-review provides a general overview of the epidemiology of the most important zoonotic MRB in cattle, swine and poultry in Europe.
Methods: A literature search was conducted mainly on the PubMed website including articles published until April 2012.
Results: Livestock-associated methicillin-resistant Staphylococcus aureus (LA-MRSA) especially poses a zoonotic risk to people working in close contact with livestock. These people may become carriers themselves and the hazard of transmission into health-care facilities needs surveillance. Extended-spectrum beta-lactamases (ESBL) producing bacteria are widely spread in both humans and livestock, sharing similar genotypes, especially of the CTX-M-group, which makes a zoonotic transfer very likely. Identical strains of vancomycin-resistant enterococci (VRE) were found both in humans and animals, after ingestion of animal strains transient colonization of the human gut may be possible. Only a few data are available on the transmission of methicillin-resistant coagulase-negative staphylococci (MR-CoNS) between humans and animals. Direct contact to colonized animals may be a risk factor as well as the exchange of resistance genes between human and animal staphylococci. Clostridium difficile (C. difficile) ribotype 078 emerges in livestock and humans and a zoonotic transmission seems probable as genotypes and diseases resemble each other.
Conclusion: All discussed MRB and C. difficile are important nosocomial agents which also occur in livestock and were found in foods of animal origin. Further analysis is needed to reveal the exact transmission routes and to perform a reliable risk assessment.
Keywords: livestock, zoonoses, MRSA, Clostridium difficile, E. coli, ESBL, vancomycin, VRE, multiresistant
Zusammenfassung
Zielsetzung: Die Intention des vorliegenden narrativen Mini-Reviews ist es, dem Leser einen Überblick über die Prävalenz und Epidemiologie multiresistenter Bakterien in Europa bei Rindern, Schweinen und Geflügel zu geben und deren zoonotisches Potential zu beleuchten.
Methode: Es wurde eine PubMed-Literaturrecherche unter Einschluss bis April 2012 publizierter Artikel durchgeführt.
Ergebnisse: Der livestock-associated Methicillin-resistente Staphylococcus aureus (LA-MRSA) ist nicht nur bei Nutztieren, sondern auch häufig bei engen Kontaktpersonen nachweisbar. Dem Eintrag durch kolonisierte und infizierte Personen ins Gesundheitswesen muss deshalb Beachtung geschenkt werden. Bakterien, die die Fähigkeit besitzen, β-Laktamasen mit einem erweitertem Wirkspektrum (ESBL) zu bilden, sind ebenfalls bei Mensch und Nutztier zu finden. Insbesondere die ESBL vom Typ CTX-M stehen im Verdacht, zwischen Mensch und Tier übertragen zu werden. Einige Studien legen nahe, dass eine Transmission von Vancomycin-resistenten Enterokokken (VRE), z.B. nach oraler Aufnahme kontaminierter tierischen Lebensmitteln, auf den Menschen möglich ist. Bezüglich des zoonotischen Potentials von multiresistenten Koagulase-negativen Staphylokokken (MR-CoNS) existieren hingegen nur wenige Publikationen. Es gibt jedoch erste Hinweise, dass eine zoonotische Übertragung möglich sein könnte und auch der Austausch von Resistenzgenen zwischen humanen und tierischen Bakterien scheint prinzipiell möglich. Die Nachweisrate von Clostridium difficile (C. difficile), v.a. des Ribotyps 078, hat bei Mensch und Tier gleichermaßen zugenommen. Nicht nur die Genotypen, auch die verursachten Infektionen weisen unabhängig von der betroffenen Spezies Gemeinsamkeiten auf.
Schlussfolgerung: Alle betrachteten multiresistenten Erreger sowie C. difficile spielen eine erhebliche Rolle bei nosokomialen Infektionen in der Humanmedizin und sind ebenfalls bei Nutztieren und Lebensmitteln tierischen Ursprungs zu finden. Weitere Studien sind nötig, um die exakten Transmissionsrouten zu identifizieren und eine valide Risikobeurteilung durchzuführen.
Introduction
Increasing resistance against antimicrobial substances in bacteria is a major problem in human as well as veterinary medicine [1], [2]. Multiresistant bacteria (MRB) with reduced susceptibility against different antibiotic classes are of exceptional clinical importance, as therapeutic options are very limited or no longer exist. While the role of MRB in human medicine is well acknowledged, the veterinary aspects of this problem have been largely neglected for a long time. The pathogenic potential of MRB, their zoonotic potential, i.e., the multiple ways of transmission to humans by direct and indirect contact and vice versa, as well as the economic implications altogether account for the huge public health impact of MRB in livestock.
There are several possible transmission pathways. First, there are agents with a wide host range, which can be directly transmitted from animal to human. Second, the antibiotic resistance genes can be transmitted from animal bacteria to commensals or infectious agents of humans through the food chain or direct contact. The third pathway is the direct transfer of obligate pathogen bacteria through food; to some extent also by contact to animals which mainly induces gastrointestinal infections (e.g., serotypes of the genus Salmonella) [3], [4]. Indirect transmission through vectors like the air, vermin, manure, contaminated water, etc. is also probable [5], [6], [7], [8]. A transmission from human to animal seems possible as well [9]. Transmission may lead to asymptomatic colonization as well as infection.
In contrast to other publications that focus on one specific MRB, this mini-review is meant to give an overview on the most important MRB and their role in livestock in Europe.
The most common MRB in human and veterinary medicine is the methicillin-resistant Staphylococcus aureus (MRSA) which first gained public attention for causing severe nosocomial human infections. Some years ago, animal strains like ST398 were detected in livestock, posing a new risk to human health [10]. Besides MRSA, other MRB colonizing the human digestive tract as well as the intestine of livestock have come into focus. Extended spectrum beta-lactamases (ESBL)-producing bacteria induce nosocomial infections in humans, with a rising incidence [11], [12]. Livestock has frequently been found to carry ESBL-producing bacteria of the blaCTX-M gene family, these genes are occasionally similar to the ones in human specimens [13], [14], [15]. Other potential pathogens in the animalistic digestive tract are vancomycin-resistant enterococci strains (VRE). This pathogen caused uproar in the 90s, when the glycopeptide antibiotic and growth promoter avoparcin was suspected to cause cross-resistance with antibiotics prescribed in human medicine [2], [16], [17]. Methicillin-resistant coagulase-negative staphylococci (MR-CoNS) are only gaining delayed public attention. CoNS are a heterogeneous group; in human medicine they are the most common cause of central line-associated bloodstream infections (CLABSI) [18], in contrast, in veterinary medicine some species of CoNS are known as a cause for mastitis in dairy cattle [19]. The zoonotic potential of these organisms is largely unknown, only few are regularly found in humans and in animals. The Gram-positive anaerobic Clostridium difficile is not a MRB by definition, it is included in this review because of rare therapeutic options due to intrinsic resistances. It is able to cause severe nosocomial diarrhea in human medicine [20], [21] and it has recently been recognized as a potential pathogen for young animals and as a zoonotic agent in veterinary medicine [22].
Methods
Search strategy
The literature was reviewed in MEDLINE on the internet homepage of the National Library of Medicine and by Google scholar. The search was done from June 1, 2011 to April 1, 2012. The following search terms were applied: “MRSA; multiresistant; Staphylococcus aureus; ESBL; extended spectrum beta lactamases; Clostridium difficile; VRE; vancomycin-resistant enterococci; MR-CoNS; multiresistant coagulase-negative staphylococci; resistance” linked with “and” to “animal; poultry; swine; pig or cattle”. In addition, the citations in each study found during the main search were reviewed for potential relevance. Finally, standard textbooks on infection control, bacteriology and microbiology were examined for information.
Selecting studies
All publications found with the mentioned keywords were checked for relevance. Publications about wildlife, pets and laboratory animals were excluded. The selection was limited to publications written in English and German. Mainly, publications describing the situation in Europe were used as well as a few relevant publications from America and Asia. At least one of the investigators decided on the relevance of each report. Reports were not blinded to the investigators so that they knew the names of the authors of all studies.
Results
Methicillin-resistant Staphylococcus aureus (MRSA)
Staphylococcus aureus (SA) is an important facultative pathogen and nosocomial agent in human medicine. The methicillin- or multiresistant Staphylococcus aureus (MRSA) is resistant to all β-lactam antibiotics. Resistance to other antibiotics like e.g., quinolones or macrolides is very common [23]. Due to several resistances, therapeutic options are very limited. MRSA can cause inter alia, skin and soft tissue infections, pneumonia or sepsis [24]. Besides hospital-acquired MRSA (HA-MRSA), community-associated MRSA (CA-MRSA) exists in non-hospitalized people. The third group is the livestock-associated MRSA (LA-MRSA), frequently belonging to the multi-locus sequence type ST398. Apart from the prominent ST398, many other sequence types of MRSA strains have been described in livestock. Some strains are exclusive to animals (e.g., ST151, ST771, ST130, ST837), others were detected in various hosts (e.g., ST22, ST254) [25], [26], [27], [28].
The methicillin resistance of MRSA is provoked by the mecA gene which is one common mobile genetic element located on the staphylococcal cassette chromosome mec (SCCmec). MecA encodes the penicillin-binding protein 2a (PBP2a), which has a low affinity to β-lactam antibiotics [1]. In 2011, a new variant emerged, that was not detectable by conventional MRSA tests. It was named mecALGA251 or mecC, belonging to different MRSA-types like CC130, CC705 or ST425. MecC-positive MRSA may cause bovine mastitis as well as wound infection in humans [29], [30]. It is a new diagnostic and therapeutic challenge to veterinary and human medicine and the global spread needs further investigation.
The Dutch were the first who found the connection between livestock and human reservoirs of MRSA. Voss et al. detected MRSA in a child of a pig farmer; despite several attempts of decolonization, the child and its family remained MRSA-positive. Constant re-colonization from a non-human reservoir was suspected and the farmer’s pigs were tested and found MRSA-positive [10]. This case triggered extensive research on the epidemiology of MRSA in pigs. Finally, the strain was identified as multilocus sequence type (MLST) 398 or frankly MRSA ST398. This strain was thereafter repeatedly found in pigs, farmers and contacts. Pigs show a particular high colonization with MRSA ST398. Accordingly, swine form an important reservoir for the transmission to humans [10] (Table 1 (Tab. 1)). In the Netherlands, 39% of tested pigs and 81% of pig herds were found to be MRSA-positive at the slaughterhouse [31]. One group found pig holdings with a prevalence of 13% concerning the individual animal and 18% with regard to the positive herds in the German Federal States of North Rhine-Westphalia and Lower Saxony. 23% of the persons with close animal contact were colonized with ST398 [32]. While these results may seem quite low in comparison to the study of the Netherlands, another study at the Dutch-German border showed 70% of colonized herds with ST398 [33].
Table 1. Prevalence of MRSA in different livestock species and in people with close animal contact (incomplete list).
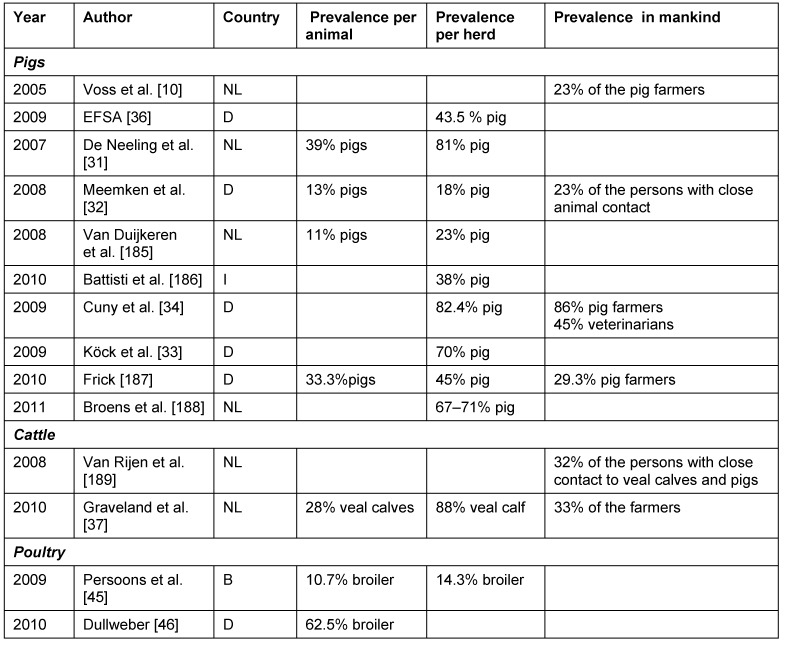
Cuny et al. screened pig farms in different German regions and found an even higher prevalence in pig herds of 82.5%. Furthermore, 86% of the pig farmers working with MRSA-positive pigs were also MRSA-positive, as well as 4.3% of the family members and 45% of the tested veterinarians. Humans without close contact to pigs did not show an increased colonization [34]. Interestingly, pigs raised in an alternative system were not found to be MRSA-positive [35].
In 2008, the European Food Safety Authority (EFSA) determined the prevalence of MRSA in holdings with breeding pigs in Europe. While in some countries MRSA was not detectable (e.g., Finland, Denmark), others showed a relatively high prevalence. Spain reached the highest level with 46%, followed by Germany (43.5%) and Belgium (40%). The average among the European Union revealed a prevalence of 14% in stocks with breeding pigs and of 26.9% in production holdings [36].
SA and MRSA are also important facultative pathogens for ruminants, where they appear either as a pathogen provoking clinical mastitis of the dairy cow or as opportunistic colonizer of veal calves [37]. For decades, SA has been known to cause mastitis and huge economic damage in dairy cattle [38], [39], [40]. The prevalence of clinical infections of the bovine udder with MRSA seems to be rather low at the moment [41], [42]; the colonization of veal calves might be more frequent. In the Netherlands, Graveland et al. detected a prevalence of 28% in the individual calf and a herd prevalence of 88% in 2010. Veal calf farmers were colonized at 33% and their family members at 8%; in comparison less than 0.1% of the Dutch general public without animal contact was identified as MRSA carrier. Furthermore, this study showed that the intensity of the animal contact and number of positive animals in the herd have a huge influence on the likelihood of human colonization [43].
As in pigs and ruminants, livestock-associated MRSA has been found in poultry. A comparison of Belgian SA-isolates from poultry from the 1970s and isolates from 2006 showed a significantly higher occurrence of antimicrobial resistance in the younger samples and all MRSA isolates were associated with ST398 [44]. Inter alia, the increase of resistance rates may be due to the use of antimicrobials. In another Belgian study, MRSA was found in broilers but not in laying hens which is presumably a result of the different antibiotic use [45]. Dullweber investigated the prevalence of MRSA in dust samples and tracheal swabs taken from broilers in northwest Germany and found 31.8% and 62.5% of swaps MRSA-positive, respectively [46].
The detection of MRSA in poultry meat is possible, as well [47], [48]. MRSA is also found in meat of other animal species like pig or cattle. At the slaughterhouse cross-contamination between the carcasses of MRSA-positive and -negative animals may be possible and retail meat can show a high prevalence of MRSA: In the Netherlands, 10.6% of beef, 15.2% of veal and 10.7% of pork from retail trade were MRSA-positive, but it was also found in lamb, mutton, game and poultry products [49]. Another Dutch study found only 2.5% of pork samples MRSA-positive [50] and in Spain the prevalence in foods totals 1.6% [51]. The varying prevalence may be explained by different sampling strategies and methods. MRSA can also occur in cheese and raw milk [52]. Therefore, the question arises whether MRSA is transmittable to humans through foods of animal origin if specific hygiene rules are neglected. In 2009, the EFSA assessed the risk to human health posed by MRSA through food. At that time no evidence for an increased risk of human colonization or infection through contaminated foods was found [53].
In general ST398 harbors less virulence factors than most HA-MRSA, nevertheless it may induce severe infections in humans [54], [55], [56], [57]. The number of infections due to ST398 is still low, in German hospitals infections with MRSA related to CC5, CC22 or CC45 are dominating [23]. The linages differ significantly by geographical region, country or continent.
In Germany and other countries, pig farmers are defined as risk patients for MRSA and admission screening is recommended [58], [59]. Livestock veterinarians are at risk as well, especially those who work at pig farms [60]. Livestock itself usually is an asymptomatic carrier of LA-MRSA, but exudative epidermitis in pigs, mastitis in cow and several infections in other animal species and pets are described [61], [62], [63], [64].
Extended spectrum beta-lactamases (ESBL)
Extended spectrum beta-lactamases (ESBL)-producing bacteria occur commonly in Enterobacteriaceae and non-fermenting bacteria. These plasmid-encoded enzymes provide a wide resistance against most β-lactam antibiotics. ESBL-producing bacteria mainly cause lower urinary tract infections (UTI) in humans; wound infections or bloodstream infections are also possible [65], [66]. Primary a nosocomial pathogen, it is nowadays also found in the community causing UTIs [12]. The treatment of severe infections is complicated by co-resistance to other antibiotic classes (e.g., quinolones, aminoglycosides) [67].
Besides humans, ESBL-producing organisms are found in pets, wild animals, zoo animals and livestock [68], [69], [70], [71], [72]. E. coli, Salmonella spp. and Klebsiella spp. are the most important ESBL producers in animals. E. coli and Klebsiella pneumonia also are the most frequent human ESBL isolates [73].
The TEM-52, SHV-12, CTX-M-1, CTX-M-14 and CTX-M-15 are ESBL enzymes frequently found in food producing animals and foods [74], [75]. Recently, the CTX-M group became the prevalent group in human medicine as well [76], especially in E. coli and Klebsiella spp. In humans, SHV-12, CTX-M-1, CTX-M-9, CTX-M-14 and CTX-M-15 are predominant enzymes in the European Union, while CTX-M-15 can be found worldwide [73], [76], [77].
In Denmark, a research group found a CTX-M-1 producing E. coli in pigs, pig farmers, manure and the air, which all shared the same IncN-plasmid blaCTX-M-1 [14], i.e. the environment also could play a role as an accessory risk factor [78], [79].
E. coli and Klebsiella spp. are important causes of mastitis in dairy cattle, but normally livestock only is an asymptomatic carrier of ESBL producers [80]. Madec et al. analyzed fecal samples of diseased (6.2% ESBL) and healthy (5.8% ESBL) cattle and isolated especially ESBL-producing E. coli. The majority of these contained genes of the CTX-M-1 group [81] which is in general a commonly found ESBL in livestock [74]. Comparing a conventional dairy cattle farm to an organic dairy farm in the Czech Republic, much more ESBL-producing bacteria (39% against <1%) were found in the conventional farm, which may demonstrate the effect of a much greater usage of cephalosporins [82].
Besides wild birds – which are not under the selective pressure of antibiotics – chicken and turkeys are frequent ESBL carriers [83], [84]. First, during the Spanish antimicrobial resistance surveillance program between 2000 and 2001, ESBL-producing bacteria were found in healthy chicken [85]. Since then, a lot of studies have been able to demonstrate the existence of ESBL-producing bacteria in poultry [86], [87], [88], [89], [90]. A study compared ESBL-producing E. coli of animal and human sources, the most isolates clearly differ from each other. Otherwise, the clonal lineage B2-E. coli O25:H4-ST131 producing CTX-M-9 and the D-E. coli O25a-ST648 group producing CTX-M-32 was found in poultry, which were very similar to those found in humans [91].
Recently, a Swiss study group found a very high prevalence of 63.4% ESBL-producing bacteria in healthy chicken fecal samples at the abattoir, the prevalence in pig, cattle and sheep samples varied between 8.6–15.3% [75]. A Dutch research group analogously found about 80% of poultry meat positive for ESBL-producers, those are highly similar to human rectal swabs obtained from hospitalized patients [15]. Several reports provide evidence of food-borne clinical outbreaks caused by multidrug-resistant Salmonella spp. [3], [4], [92]. However, there are also indications of transmission of ESBL-producing E. coli from foods of animal origin to humans or vice versa [15], [93]; a Dutch report showed that 19% of tested patients harbored ESBL genes which were indistinguishable from those in poultry isolates [13]. The comparison of pulsed-field gel electrophoresis (PFGE) patterns between poultry, poultry farmers and slaughterers demonstrates that direct animal contact may also be an important route for transmission [94]. An exchange of resistance genes between animal and human bacterial strains even seems possible [14].
Vancomycin-resistant enterococci (VRE)
Enterococci are commensals of the human and animal intestinal microflora. Besides their intrinsic resistance to cephalosporins, enterococci can acquire resistance e.g. to glycopeptides such as vancomycin through transmissible genetic elements. Enterococcus faecialis is the most frequent isolated strain in human patients, followed by Enterococcus faecium. These enterococci also occur in animals. Several different genotypes have been detected until now, vanA and vanB play an important role in human medicine. Even livestock is a frequent vanA carrier [17], [95], [96], [97]. The vanA gene is usually located in the transposon Tn1546 [98]. While animals are mainly asymptomatic carriers, VRE may lead to severe nosocomial infections in humans, such as UTIs or wound infections [99], [100], [101].
Reports about increasing detection of VRE in livestock caused serious concern in Europe in the 1990s [102], [103], [104]. The application of the glycopeptide-antibiotic avoparcin, used for growth promotion in livestock fattening, was controversially discussed.
There was strong suspicion of causing cross-resistance with vancomycin/teicoplanine; therefore a severe risk for human medicine was supposed. This has led to a ban of avoparcin in 1986 in Sweden, followed by Denmark and Germany and finally the entire EU since 1997 (Commission Directive 97/6 EC). However, some critics also doubted a correlation between avoparcin and increasing antibiotic resistance [103], [105], [106].
In 1995, VRE vanA-type was isolated from thawing liquids of frozen poultry and from raw minced meat of pigs in Germany [107]. In 1997, up to 15% and 16%, respectively, of samples from pork and broilers were found VRE positive in Denmark [108].
With the ban of avoparcin the occurrence of VRE in the intestine of healthy communities decreased from 12% (1994) to 3% (1997) [2] and also the prevalence occasionally decreased in meat [2], [103], [109].
Otherwise, in 2002, Heuer et al. tested the occurrence of VRE in Danish broiler farms, still finding a high prevalence of positive broiler flocks. VRE has even been detected in the environmental samples after cleaning and disinfection due to known persistence [110]. A transmission to following broiler herds seems probable. The co-selection by macrolides is presumed to be another cause of the persistence of VRE in the absence of avoparcin. The gene for macrolide resistance is located on the same plasmid as the vanA gene [111].
A high prevalence (77.1%) in poultry fecal samples was found in Austria in 2005, while the prevalence in samples from cattle and swine was much lower (21.6–23.3%) [112]. Recently, Ramos et al. still found 25.3% VRE-positive fecal samples in pigs in Portugal, but in contrast none were detected in bovine samples [113]. Even if the prevalence of VRE seems to decrease in several animals, VRE may persist in some areas and species.
Processed food may likewise act as vector of VRE besides living animal. Determing the zoonotic potential, van den Boogard et al. found 50% of the sampled turkeys and 39% of the farmers VRE-positive as well as at least 20% of the turkey slaughterers and 14% of samples of area residents without direct contact to those animals [102]. This demonstrates that close contact may be a risk factor for transmission between animals and humans.
Human VRE isolates can harbor the same Tn1546 variant found in livestock and foods, indicating a horizontal gene transfer in the intestine [114], [115]. However, transient colonization of the human intestine was demonstrated after ingestion of VRE of animal origin [116], [117]. Furthermore, the in vivo transfer of an avian vanA gene from E. faecium to a human vancomycin-susceptible E. faecium strain in volunteers was shown in 2006 [118]. This indicates that foods of animal origin may be a vector of resistance genes. VRE, isolated from pigs and humans of several European countries and the United States, were compared by PFGE in a study from Freitas et al. E. faecium clonal complex 5 (CC5) and CC17 were found in both animals and humans, showing similar or even identical PFGE patterns. CC5 E. faecium can also be detected in patients with UTIs [5]. Several different sequence types can be found both in hospitalized patients and livestock (e.g. ST16) [119], [120].
Methicillin-resistant coagulase-negative staphylococci (MR-CoNS)
Methicillin-resistant coagulase-negative staphylococci (MR-CoNS) represent a heterogeneous group with huge species diversity. The methicillin resistance is mediated through the SCCmec, similar to the resistance mechanism in MRSA. Inter alia, CoNS are commensal organisms of human and animal skin and mucous membranes. S. epidermidis, S. haemolyticus and S. hominis are the most important species in human samples [121], [122]. CoNS and especially MR-CoNS are known as relevant nosocomial pathogen in humans. The impact of MR-CoNS has been increasing for a period of 20 years; nowadays approximately one third of central line-associated bloodstream infections are caused by CoNS in Germany and almost two third of these samples are methicillin-resistant [18].
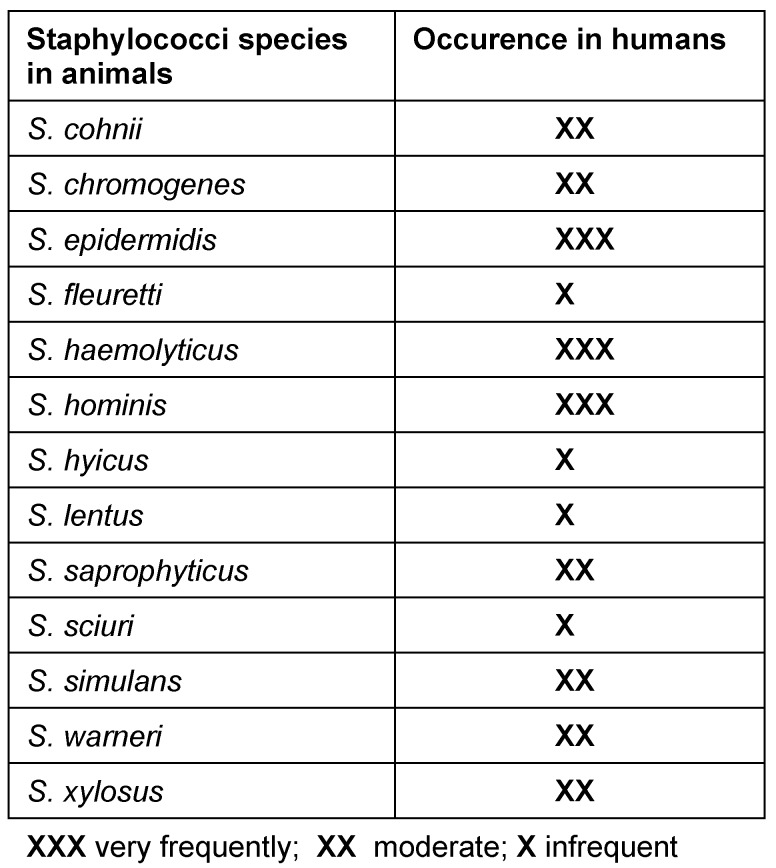
MR-CoNS have also been classified as emerging animal pathogens [123] as they are an important causative agent of mastitis in dairy cows and small ruminants. Different species of staphylococci are detectable, depending on the location; the skin colonization may be different than the colonization of the udder. The CoNS causing subclinical, or less often, clinical mastitis are i.a., S. xylosus, S. simulans, S. warneri or S. chromogenes but may also be S. epidermidis, S. haemolyticus and S. hominis [19], [124], [125] (Table 2 (Tab. 2)).
Table 2. Coagulase-negative Staphylococci in animals and their occurrence in humans [121], [122], [132], [190].
Subclinical mastitis due to MR-CoNS in cattle results in high economic losses caused by a decreased milk yield and an increased milk cell count. In this case, cows frequently get a dry cow therapy at the end of lactation, i.e., an antibiotic is directly injected into every udder quarter. This may lead to increasing resistance with penicillin-resistant CoNS being found in approximately 30% of the treated dairy cows [126], [127], [128].
Resistance in CoNS have also been found in pig [129], poultry, small ruminants [130], [131], [132] and veal calves [133]. Besides mastitis in dairy cattle (including small ruminants), livestock are typically asymptomatic carriers.
MR-CoNS are divided into a lot of species and subspecies, some of them only occur in certain animals or humans. But a lot of species have a broad host range. A direct transfer from animal to humans with close contact seems to be possible [131], this could be a threat especially to immunocompromised people. Another hazard is the horizontal transfer from resistance genes. Livestock are a huge reservoir for MR-CoNS and a transfer from resistance genes to other CoNS species or S. aureus is very likely [134], [135], [136], [137]. The same SCCmec types were already found in CoNS and S. aureus [138]. The relevance of a transfer to humans via foods is still little-known, but it is found in meat and bulk tank milk [131]. Whether foods of animal origin are dangerous to human health has to be verified in future investigations.
Clostridium difficile (C. difficile)
C. difficile is a spore forming and toxin producing anaerobic Gram-positive bacterium; frequently found in humans, animals and foods [139], [140], [141], [142], [143], [144]. It is a common cause of healthcare-associated diarrhea; a direct connection between the use of antibiotics and pseudomembranous diarrhea due to C. difficile is well acknowledged in human medicine [145]. The capability of forming spores makes Clostridia very resistant to environmental influences. C. difficile can produce different toxins: the two major toxins are toxin A and toxin B; some strains can produce a binary toxin. Toxin A is an enterotoxin and toxin B provides cytotoxic effects, whereas the effects of the binary toxin have not yet been completely clarified [146], [147]. Some strains, such as ribotype 027 can produce all three kind of toxins and harbor a mutation in the tcdC gene, a toxin regulatory gene. In human medicine, the hypervirulent ribotype 027 is presumably related to increased mortality and is of worldwide concern [148], [149]; the occurrence of this strain is also described in domestic animals and foods [150]. Besides this ribotype, other strains like 001, 014/020, 053, 017 or 078 are described in human isolates in Europe, with huge geographical differences [151], [152], [153], [154].
In livestock, ribotype 078 is commonly found [155], [156], [157], [158], but, e.g., ribotype 017 has also been described in farm animals [144]. Both ribotypes can cause severe intestinal human diseases [149], [159].
The pathogenic potential of C. difficile for pigs is currently not completely clarified, but it seems to play an important role in neonatal diarrhea. Alvarez-Perez isolated C. difficile in 25.9% of the Spanish newborn piglets; more than 94% carried genes to produce toxin A and B. C. difficile was detectable in diarrheic but also in clinically completely inconspicuous animals [22]. Using an enrichment technique, Hopman et al. were able to detect 100% of the tested piglets positive on C. difficile. Sows, the environment and the air were also tested positive and the possibility of an airborne transmission was discussed [157]. There seems to be an association between maturing of swine and other animal species and the decrease of C. difficile prevalence [141], [160], [161].
The pathogenicity of C. difficile for cattle, especially for calves, is still controversial. Occasionally, a higher prevalence in healthy calves than in diarrheic ones has been described, but the Clostridia in diseased calves were more often toxin producers [144]. Costa et al. found a prevalence of 61% in veal calves and they detected a tetracycline resistance in 76–93% of the C. difficile isolates [162].
To our knowledge only few data exist on C. difficile in poultry and there is no explicit evidence for an animal pathogenic potential in chicken or turkey. A study in Slovenian chicks found a prevalence of 100% in two week old animals and 40.9% in 18 week old ones. Furthermore, a lot of different ribotypes were detectable [141].
The zoonotic aspect of C. difficile is not completely clarified. As mentioned above, the same ribotypes may occur both in humans and animals, with ribotype 078 having emerged at the same time in humans and livestock. Furthermore, the identical C. difficile strains were already found in diseased pigs and humans [163].
In North America, C. difficile can be often isolated from meat [142], [164], [165]. For example in Canada, 20% of retail minced meat samples harbored C. difficile, including the human pathogenic ribotypes 077 and 014, one variant was highly similar to the ribotype 027 [143]. C. difficile contamination has also been confirmed in processed poultry meat in several countries all over the world [142], [164], [166]. The prevalence is low in meat in Europe. In Sweden, 2.4% of the meat samples were positive for C. difficile, all occurring in minced beef [167]. De Boer et al. found also a low prevalence in the Netherlands, 1.6% of the meat was sampled positive [166]. In Austria, 3% of meat samples harbored C. difficile [168]. Mortification of C. difficile through the preparation process is not reliable due to its capacity of spore forming [169]. Nevertheless, cases of transmission via foods have not been proven yet, therefore its role as a probable food-borne pathogen remains unclear.
Discussion
Bacterial multiresistance to antibiotics in livestock causes increasing concern in veterinary as well as human medicine. Still, the prevalence, transmission and zoonotic potential of multiresistant bacterial pathogens in livestock are largely unknown. While the livestock-associated MRSA has become somewhat prominent, the role of other pathogens, especially Gram-negative organisms, has not been widely acknowledged yet. With this mini-review, which is not considered exhaustive, we therefore tried to give an overview on the existing evidence and epidemiology of MRB in animals in Europe.
Healthcare and veterinary professionals should be aware of the increasing occurrence of ST398 in livestock; the same applies to the occurrence of new variants. Direct contact to animals has repeatedly been found to be associated with MRSA-colonization and infection in humans [34], [170]. Airborne transmission to other animal species and to insects, which can in turn become vectors, seems possible, too [8], [171], [172]. According to the Federal Institute for Risk Assessment (BfR) in Germany and the scientific opinion published by the EFSA, the risk of MRSA-transmission associated with foods or food handling is very low, but strict adherence to general hygiene guidelines in households is recommended to minimize the residual risk [53], [173]. It seems advisable that not only pig farm workers, but all subjects professionally exposed to close animal contact are classified as risk patients before admission to hospital. The EFSA confirmed that not only pigs, but also veal calves and broilers represent primary reservoirs for ST398 [53].
ESBL-producing Gram-negative rods may become an increasing problem in veterinary medicine in the next years. β-lactam antibiotics are the most applied group of antibiotics in veterinary medicine and a large therapy failure would lead to enormous economic and animal welfare problems [174]. Moreover, β-lactam antibiotics are also of utmost importance in human medicine. For Germany, only very limited data exist on the epidemiology of ESBL-producers in livestock, but the available data indicate a relevant ESBL prevalence in animals [175]. Meat has also been found to be frequently contaminated with ESBL [13], [176], even if it is of organic origin [177]. Reasons for the high prevalence in organic chicken meat could be multifarious, e.g., cross-contamination at the abattoir [178] or colonization of the parent animals. The high prevalence, especially found in poultry and poultry meat, the probable transmission to farmers [14] and the similar ESBL genes found in hospitalized patients [13], [15] show the importance of livestock as reservoir. Nonetheless, it is difficult to prove a direct transfer from non-pathogenic ESBL-producers via food or animal contact. Most reports compare gene patterns, but the origin of the resistance genes remains unclear.
The history of vancomycin resistance shows, that a restrictive policy can help to control antimicrobial resistance on a national and European scale. Seventeen years after the ban of the growth promoter avoparcin in the European Community, resistance rates in enterococci have at least not increased in livestock. Unfortunately, as a result the interest of veterinary medicine in VRE has noticeably decreased, even though studies show that VRE persists in livestock and the environment and is still a serious threat. The prevalence of VRE in human medicine is very heterogeneous in Europe. The predominant amount of European countries has shown an increase of VRE since 2000 (e.g., Germany, Czech Republic, France, Hungary, Norway, Spain, Ireland) [179]. Presumably, the increased prescription of vancomycin in human medicine for treatment of MRSA and severe C. difficile infections plays a major role in the spread of VRE [180]. The potential transmission of the vancomycin resistance to S. aureus is likewise a serious concern, additionally reducing the treatment options [181]. A transient colonization of the human gut with enterococci from animal sources is possible, and even the transfer of resistance genes has already been shown [117], [118]. Therefore, there is reasonable concern on the zoonotic hazards posed by VRE of livestock and foods of animal origin, but the precise extent of the hazard remains unclear.
The impact of animal MR-CoNS on human medicine is currently unclear. Livestock and companion animals are often carriers of MR-CoNS and therefore form an important reservoir. A transmission of resistance genes to staphylococci with pathogenic potential to humans, as well as the transmission through direct contact and foods of animal origin (e.g., raw milk) is conceivable [131], [134].
C. difficile infection (CDI) has primarily been a nosocomial problem. Recently, CDI has occured increasingly in the community [182], [183]. Livestock and foods of animal origin are discussed to be the main reservoir, but direct evidence is sparse. Another reason or at least a cofactor for the increase of C. difficile in the community may be the selective pressure induced by antibiotic use in hospitals and outpatient treatment. The prevalence of toxin-producing C. difficile in newborn humans is at a high level, i.e., up to 70%. Furthermore, almost all newborn piglets are colonized, but usually, animal and human newborns are not affected by colonization. During the maturation, the recovery rate decreases in livestock as well as in humans. The maturation of the immune system is presumed to be a factor for the development of clinical symptoms in older age groups [141], [184].
Conclusion
MRB are emerging pathogens with increasing importance for veterinary as well as human medicine. The underlying promoters for the spread of resistance, selection- and colonization-pressure caused by extensive use of antimicrobial chemotherapy, are basically similar for all MRB mentioned. While concerns with antimicrobial resistance and antibiotic use are currently rising in medicine as well as in the public, further studies are needed to analyze the epidemiology in and transmission chains to animals and humans. To implement evidence-based intervention measures, the risk associated with livestock husbandry, food chain work and companion animals has to be quantified. Interdisciplinary research between human and veterinary medicine is therefore highly diserable.
Notes
Competing interests
The authors declare that no competing interests exist.
Author’s contributions
CD did the research and drafted the manuscript. NOH, FW and AK contributed by advising, revising, reading and approving the final script.
Acknowledgments
The review is supported by the German Ministry for Education and Research (BMBF), HICARE-Gesundheitsregion Ostseeküste, Grant DM301KQ1001.
References
- 1.Chambers HF, Deleo FR. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat Rev Microbiol. 2009 Sep;7(9):629–641. doi: 10.1038/nrmicro2200. Available from: http://dx.doi.org/10.1038/nrmicro2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klare I, Badstübner D, Konstabel C, Böhme G, Claus H, Witte W. Decreased incidence of VanA-type vancomycin-resistant enterococci isolated from poultry meat and from fecal samples of humans in the community after discontinuation of avoparcin usage in animal husbandry. Microb Drug Resist. 1999;5(1):45–52. doi: 10.1089/mdr.1999.5.45. [DOI] [PubMed] [Google Scholar]
- 3.Mølbak K, Baggesen DL, Aarestrup FM, Ebbesen JM, Engberg J, Frydendahl K, Gerner-Smidt P, Petersen AM, Wegener HC. An outbreak of multidrug-resistant, quinolone-resistant Salmonella enterica serotype typhimurium DT104. N Engl J Med. 1999 Nov;341(19):1420–1425. doi: 10.1056/NEJM199911043411902. Available from: http://dx.doi.org/10.1056/NEJM199911043411902. [DOI] [PubMed] [Google Scholar]
- 4.Dechet AM, Scallan E, Gensheimer K, Hoekstra R, Gunderman-King J, Lockett J, Wrigley D, Chege W, Sobel J Multistate Working Group. Outbreak of multidrug-resistant Salmonella enterica serotype Typhimurium Definitive Type 104 infection linked to commercial ground beef, northeastern United States, 2003-2004. Clin Infect Dis. 2006 Mar;42(6):747–752. doi: 10.1086/500320. Available from: http://dx.doi.org/10.1086/500320. [DOI] [PubMed] [Google Scholar]
- 5.Freitas AR, Coque TM, Novais C, Hammerum AM, Lester CH, Zervos MJ, Donabedian S, Jensen LB, Francia MV, Baquero F, Peixe L. Human and swine hosts share vancomycin-resistant Enterococcus faecium CC17 and CC5 and Enterococcus faecalis CC2 clonal clusters harboring Tn1546 on indistinguishable plasmids. J Clin Microbiol. 2011 Mar;49(3):925–931. doi: 10.1128/JCM.01750-10. Available from: http://dx.doi.org/10.1128/JCM.01750-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kühn I, Iversen A, Finn M, Greko C, Burman LG, Blanch AR, Vilanova X, Manero A, Taylor H, Caplin J, Domínguez L, Herrero IA, Moreno MA, Möllby R. Occurrence and relatedness of vancomycin-resistant enterococci in animals, humans, and the environment in different European regions. Appl Environ Microbiol. 2005 Sep;71(9):5383–5390. doi: 10.1128/AEM.71.9.5383-5390.2005. Available from: http://dx.doi.org/10.1128/AEM.71.9.5383-5390.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gibbs SG, Green CF, Tarwater PM, Scarpino PV. Airborne antibiotic resistant and nonresistant bacteria and fungi recovered from two swine herd confined animal feeding operations. J Occup Environ Hyg. 2004 Nov;1(11):699–706. doi: 10.1080/15459620490515824. Available from: http://dx.doi.org/10.1080/15459620490515824. [DOI] [PubMed] [Google Scholar]
- 8.van de Giessen AW, van Santen-Verheuvel MG, Hengeveld PD, Bosch T, Broens EM, Reusken CB. Occurrence of methicillin-resistant Staphylococcus aureus in rats living on pig farms. Prev Vet Med. 2009 Oct;91(2-4):270–273. doi: 10.1016/j.prevetmed.2009.05.016. Available from: http://dx.doi.org/10.1016/j.prevetmed.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 9.Morgan M. Methicillin-resistant Staphylococcus aureus and animals: zoonosis or humanosis? J Antimicrob Chemother. 2008 Dec;62(6):1181–1187. doi: 10.1093/jac/dkn405. Available from: http://dx.doi.org/10.1093/jac/dkn405. [DOI] [PubMed] [Google Scholar]
- 10.Voss A, Loeffen F, Bakker J, Klaassen C, Wulf M. Methicillin-resistant Staphylococcus aureus in pig farming. Emerging Infect Dis. 2005 Dec;11(12):1965–1966. doi: 10.3201/eid1112.050428. Available from: http://dx.doi.org/10.3201/eid1112.050428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meyer E, Schwab F, Schroeren-Boersch B, Gastmeier P. Dramatic increase of third-generation cephalosporin-resistant E. coli in German intensive care units: secular trends in antibiotic drug use and bacterial resistance, 2001 to 2008. Crit Care. 2010;14(3):R113. doi: 10.1186/cc9062. Available from: http://dx.doi.org/10.1186/cc9062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pitout JD, Laupland KB. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis. 2008 Mar;8(3):159–166. doi: 10.1016/S1473-3099(08)70041-0. Available from: http://dx.doi.org/10.1016/S1473-3099(08)70041-0. [DOI] [PubMed] [Google Scholar]
- 13.Leverstein-van Hall MA, Dierikx CM, Cohen Stuart J, Voets GM, van den Munckhof MP, van Essen-Zandbergen A, Platteel T, Fluit AC, van de Sande-Bruinsma N, Scharinga J, Bonten MJ, Mevius DJ National ESBL surveillance group. Dutch patients, retail chicken meat and poultry share the same ESBL genes, plasmids and strains. Clin Microbiol Infect. 2011 Jun;17(6):873–880. doi: 10.1111/j.1469-0691.2011.03497.x. Available from: http://dx.doi.org/10.1111/j.1469-0691.2011.03497.x. [DOI] [PubMed] [Google Scholar]
- 14.Moodley A, Guardabassi L. Transmission of IncN plasmids carrying blaCTX-M-1 between commensal Escherichia coli in pigs and farm workers. Antimicrob Agents Chemother. 2009 Apr;53(4):1709–1711. doi: 10.1128/AAC.01014-08. Available from: http://dx.doi.org/10.1128/AAC.01014-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Overdevest I, Willemsen I, Rijnsburger M, Eustace A, Xu L, Hawkey P, Heck M, Savelkoul P, Vandenbroucke-Grauls C, van der Zwaluw K, Huijsdens X, Kluytmans J. Extended-spectrum ß-lactamase genes of Escherichia coli in chicken meat and humans, The Netherlands. Emerging Infect Dis. 2011 Jul;17(7):1216–1222. doi: 10.3201/eid1707.110209. Available from: http://dx.doi.org/10.3201/eid1707.110209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bates J. Epidemiology of vancomycin-resistant enterococci in the community and the relevance of farm animals to human infection. J Hosp Infect. 1997 Oct;37(2):89–101. doi: 10.1016/S0195-6701(97)90179-1. Available from: http://dx.doi.org/10.1016/S0195-6701(97)90179-1. [DOI] [PubMed] [Google Scholar]
- 17.Simonsen GS, Haaheim H, Dahl KH, Kruse H, Løvseth A, Olsvik O, Sundsfjord A. Transmission of VanA-type vancomycin-resistant enterococci and vanA resistance elements between chicken and humans at avoparcin-exposed farms. Microb Drug Resist. 1998;4(4):313–318. doi: 10.1089/mdr.1998.4.313. Available from: http://dx.doi.org/10.1089/mdr.1998.4.313. [DOI] [PubMed] [Google Scholar]
- 18.Hufnagel M, Burger A, Bartelt S, Henneke P, Berner R. Secular trends in pediatric bloodstream infections over a 20-year period at a tertiary care hospital in Germany. Eur J Pediatr. 2008 Oct;167(10):1149–1159. doi: 10.1007/s00431-007-0651-4. Available from: http://dx.doi.org/10.1007/s00431-007-0651-4. [DOI] [PubMed] [Google Scholar]
- 19.Gillespie BE, Headrick SI, Boonyayatra S, Oliver SP. Prevalence and persistence of coagulase-negative Staphylococcus species in three dairy research herds. Vet Microbiol. 2009 Feb;134(1-2):65–72. doi: 10.1016/j.vetmic.2008.09.007. Available from: http://dx.doi.org/10.1016/j.vetmic.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Aldeyab MA, Devine MJ, Flanagan P, Mannion M, Craig A, Scott MG, Harbarth S, Vernaz N, Davies E, Brazier JS, Smyth B, McElnay JC, Gilmore BF, Conlon G, Magee FA, Elhajji FW, Small S, Edwards C, Funston C, Kearney MP. Multihospital outbreak of Clostridium difficile ribotype 027 infection: epidemiology and analysis of control measures. Infect Control Hosp Epidemiol. 2011 Mar;32(3):210–219. doi: 10.1086/658333. Available from: http://dx.doi.org/10.1086/658333. [DOI] [PubMed] [Google Scholar]
- 21.Bartlett JG. Clostridium difficile infection: historic review. Anaerobe. 2009 Dec;15(6):227–229. doi: 10.1016/j.anaerobe.2009.09.004. Available from: http://dx.doi.org/10.1016/j.anaerobe.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 22.Alvarez-Perez S, Blanco JL, Bouza E, Alba P, Gibert X, Maldonado J, Garcia ME. Prevalence of Clostridium difficile in diarrhoeic and non-diarrhoeic piglets. Vet Microbiol. 2009 Jun;137(3-4):302–305. doi: 10.1016/j.vetmic.2009.01.015. Available from: http://dx.doi.org/10.1016/j.vetmic.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 23.Robert Koch-Institut. Auftreten und Verbreitung von MRSA in Deutschland 2010. Epidemiol Bull. 2011;(26):233–244. Available from: http://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2011/26/Art_01.html. [Google Scholar]
- 24.Enright MC. The evolution of a resistant pathogen--the case of MRSA. Curr Opin Pharmacol. 2003 Oct;3(5):474–479. doi: 10.1016/S1471-4892(03)00109-7. Available from: http://dx.doi.org/10.1016/S1471-4892(03)00109-7. [DOI] [PubMed] [Google Scholar]
- 25.Sung JM, Lloyd DH, Lindsay JA. Staphylococcus aureus host specificity: comparative genomics of human versus animal isolates by multi-strain microarray. Microbiology (Reading, Engl) 2008 Jul;154(Pt 7):1949–1959. doi: 10.1099/mic.0.2007/015289-0. Available from: http://dx.doi.org/10.1099/mic.0.2007/015289-0. [DOI] [PubMed] [Google Scholar]
- 26.Loeffler A, Boag AK, Sung J, Lindsay JA, Guardabassi L, Dalsgaard A, Smith H, Stevens KB, Lloyd DH. Prevalence of methicillin-resistant Staphylococcus aureus among staff and pets in a small animal referral hospital in the UK. J Antimicrob Chemother. 2005 Oct;56(4):692–697. doi: 10.1093/jac/dki312. Available from: http://dx.doi.org/10.1093/jac/dki312. [DOI] [PubMed] [Google Scholar]
- 27.Walther B, Wieler LH, Friedrich AW, Hanssen AM, Kohn B, Brunnberg L, Lübke-Becker A. Methicillin-resistant Staphylococcus aureus (MRSA) isolated from small and exotic animals at a university hospital during routine microbiological examinations. Vet Microbiol. 2008 Feb;127(1-2):171–178. doi: 10.1016/j.vetmic.2007.07.018. Available from: http://dx.doi.org/10.1016/j.vetmic.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 28.Walther B, Monecke S, Ruscher C, Friedrich AW, Ehricht R, Slickers P, Soba A, Wleklinski CG, Wieler LH, Lübke-Becker A. Comparative molecular analysis substantiates zoonotic potential of equine methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2009 Mar;47(3):704–710. doi: 10.1128/JCM.01626-08. Available from: http://dx.doi.org/10.1128/JCM.01626-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.García-Álvarez L, Holden MT, Lindsay H, Webb CR, Brown DF, Curran MD, Walpole E, Brooks K, Pickard DJ, Teale C, Parkhill J, Bentley SD, Edwards GF, Girvan EK, Kearns AM, Pichon B, Hill RL, Larsen AR, Skov RL, Peacock SJ, Maskell DJ, Holmes MA. Meticillin-resistant Staphylococcus aureus with a novel mecA homologue in human and bovine populations in the UK and Denmark: a descriptive study. Lancet Infect Dis. 2011 Aug;11(8):595–603. doi: 10.1016/S1473-3099(11)70126-8. Available from: http://dx.doi.org/10.1016/S1473-3099(11)70126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cuny C, Layer F, Strommenger B, Witte W. Rare occurrence of methicillin-resistant Staphylococcus aureus CC130 with a novel mecA homologue in humans in Germany. PLoS One. 2011;6(9):e24360. doi: 10.1371/journal.pone.0024360. Available from: http://dx.doi.org/10.1371/journal.pone.0024360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Neeling AJ, van den Broek MJ, Spalburg EC, van Santen-Verheuvel MG, Dam-Deisz WD, Boshuizen HC, van de Giessen AW, van Duijkeren E, Huijsdens XW. High prevalence of methicillin resistant Staphylococcus aureus in pigs. Vet Microbiol. 2007 Jun;122(3-4):366–372. doi: 10.1016/j.vetmic.2007.01.027. Available from: http://dx.doi.org/10.1016/j.vetmic.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 32.Meemken D, Cuny C, Witte W, Eichler U, Staudt R, Blaha T. Zum Vorkommen von MRSA bei Schweinen und bei Menschen mit beruflicher Exposition zum Schwein--Erste Ergebnisse einer Studie in Nordwestdeutschland. [Occurrence of MRSA in pigs and in humans involved in pig production--preliminary results of a study in the northwest of Germany]. DTW Dtsch Tierarztl Wochenschr. 2008 Apr;115(4):132–139. (Ger). [PubMed] [Google Scholar]
- 33.Köck R, Harlizius J, Bressan N, Laerberg R, Wieler LH, Witte W, Deurenberg RH, Voss A, Becker K, Friedrich AW. Prevalence and molecular characteristics of methicillin-resistant Staphylococcus aureus (MRSA) among pigs on German farms and import of livestock-related MRSA into hospitals. Eur J Clin Microbiol Infect Dis. 2009 Nov;28(11):1375–1382. doi: 10.1007/s10096-009-0795-4. Available from: http://dx.doi.org/10.1007/s10096-009-0795-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cuny C, Nathaus R, Layer F, Strommenger B, Altmann D, Witte W. Nasal colonization of humans with methicillin-resistant Staphylococcus aureus (MRSA) CC398 with and without exposure to pigs. PLoS One. 2009 Aug 27;4(8):e6800. doi: 10.1371/journal.pone.0006800. Available from: http://dx.doi.org/10.1371/journal.pone.0006800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cuny C, Friedrich AW, Witte W. Absence of livestock-associated methicillin-resistant staphylococcus aureus clonal complex CC398 as a nasal colonizer of pigs raised in an alternative system. Appl Environ Microbiol. 2012 Feb;78(4):1296–1297. doi: 10.1128/AEM.07260-11. Available from: http://dx.doi.org/10.1128/AEM.07260-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.European Food Safety Authority. Analysis of the baseline survey on the prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in holdings with breeding pigs, in the EU, 2008 - Part A: MRSA prevalence estimates. EFSA J. 2009;7(11):1376. doi: 10.2903/j.efsa.2009.1376. Available from: http://dx.doi.org/10.2903/j.efsa.2009.1376. [DOI] [Google Scholar]
- 37.Graveland H, Wagenaar JA, Heesterbeek H, Mevius D, van Duijkeren E, Heederik D. Methicillin resistant Staphylococcus aureus ST398 in veal calf farming: human MRSA carriage related with animal antimicrobial usage and farm hygiene. PLoS One. 2010 Jun 8;5(6):e10990. doi: 10.1371/journal.pone.0010990. Available from: http://dx.doi.org/10.1371/journal.pone.0010990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heringstad BK, Gunnar Ruane, John. Selection for mastitis resistance in dairy cattle: a review with focus on the situation in the Nordic countries. Livestock Production Science. 2000;64(2-3):95–106. doi: 10.1016/S0301-6226(99)00128-1. Available from: http://dx.doi.org/10.1016/S0301-6226(99)00128-1. [DOI] [Google Scholar]
- 39.Stephan R, Annemuller C, Hassan AA, Lammler C. Characterization of enterotoxigenic Staphylococcus aureus strains isolated from bovine mastitis in north-east Switzerland. Vet Microbiol. 2001;78(4):373–382. doi: 10.1016/S0378-1135(00)00341-2. Available from: http://dx.doi.org/10.1016/S0378-1135(00)00341-2. [DOI] [PubMed] [Google Scholar]
- 40.Smith TH, Fox LK, Middleton JR. Outbreak of mastitis caused by one strain of Staphylococcus aureus in a closed dairy herd. J Am Vet Med Assoc. 1998 Feb;212(4):553–556. [PubMed] [Google Scholar]
- 41.Spohr M, Rau J, Friedrich A, Klittich G, Fetsch A, Guerra B, Hammerl JA, Tenhagen BA. Methicillin-resistant Staphylococcus aureus (MRSA) in three dairy herds in southwest Germany. Zoonoses Public Health. 2011 Jun;58(4):252–261. doi: 10.1111/j.1863-2378.2010.01344.x. Available from: http://dx.doi.org/10.1111/j.1863-2378.2010.01344.x. [DOI] [PubMed] [Google Scholar]
- 42.Haran KP, Godden SM, Boxrud D, Jawahir S, Bender JB, Sreevatsan S. Prevalence and characterization of Staphylococcus aureus, including methicillin-resistant Staphylococcus aureus, isolated from bulk tank milk from Minnesota dairy farms. J Clin Microbiol. 2012 Mar;50(3):688–695. doi: 10.1128/JCM.05214-11. Available from: http://dx.doi.org/10.1128/JCM.05214-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Graveland H, Wagenaar JA, Bergs K, Heesterbeek H, Heederik D. Persistence of livestock associated MRSA CC398 in humans is dependent on intensity of animal contact. PLoS One. 2011 Feb 9;6(2):e16830. doi: 10.1371/journal.pone.0016830. Available from: http://dx.doi.org/10.1371/journal.pone.0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nemati M, Hermans K, Lipinska U, Denis O, Deplano A, Struelens M, Devriese LA, Pasmans F, Haesebrouck F. Antimicrobial resistance of old and recent Staphylococcus aureus isolates from poultry: first detection of livestock-associated methicillin-resistant strain ST398. Antimicrob Agents Chemother. 2008 Oct;52(10):3817–3819. doi: 10.1128/AAC.00613-08. Available from: http://dx.doi.org/10.1128/AAC.00613-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Persoons D, Van Hoorebeke S, Hermans K, Butaye P, de Kruif A, Haesebrouck F, Dewulf J. Methicillin-resistant Staphylococcus aureus in poultry. Emerging Infect Dis. 2009 Mar;15(3):452–453. doi: 10.3201/eid1503.080696. Available from: http://dx.doi.org/10.3201/eid1503.080696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dullweber A. Untersuchung von Methicillin-resistenten Staphylococcus aureus (MRSA) in Geflügelmastbeständen [PhD-Thesis] Hannover: Tierärztliche Hochschule; 2010. Available from: http://elib.tiho-hannover.de/dissertations/dullwebera_ws10.html. [Google Scholar]
- 47.Waters AE, Contente-Cuomo T, Buchhagen J, Liu CM, Watson L, Pearce K, Foster JT, Bowers J, Driebe EM, Engelthaler DM, Keim PS, Price LB. Multidrug-Resistant Staphylococcus aureus in US Meat and Poultry. Clin Infect Dis. 2011 May;52(10):1227–1230. doi: 10.1093/cid/cir181. Available from: http://dx.doi.org/10.1093/cid/cir181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fessler AT, Kadlec K, Hassel M, Hauschild T, Eidam C, Ehricht R, Monecke S, Schwarz S. Characterization of methicillin-resistant Staphylococcus aureus isolates from food and food products of poultry origin in Germany. Appl Environ Microbiol. 2011 Oct;77(20):7151–7157. doi: 10.1128/AEM.00561-11. Available from: http://dx.doi.org/10.1128/AEM.00561-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.de Boer E, Zwartkruis-Nahuis JT, Wit B, Huijsdens XW, de Neeling AJ, Bosch T, van Oosterom RA, Vila A, Heuvelink AE. Prevalence of methicillin-resistant Staphylococcus aureus in meat. Int J Food Microbiol. 2009 Aug;134(1-2):52–56. doi: 10.1016/j.ijfoodmicro.2008.12.007. Available from: http://dx.doi.org/10.1016/j.ijfoodmicro.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 50.van Loo IH, Diederen BM, Savelkoul PH, Woudenberg JH, Roosendaal R, van Belkum A, Lemmens-den Toom N, Verhulst C, van Keulen PH, Kluytmans JA. Methicillin-resistant Staphylococcus aureus in meat products, the Netherlands. Emerging Infect Dis. 2007 Nov;13(11):1753–1755. doi: 10.3201/eid1311.070358. Available from: http://dx.doi.org/10.3201/eid1311.070358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lozano C, López M, Gómez-Sanz E, Ruiz-Larrea F, Torres C, Zarazaga M. Detection of methicillin-resistant Staphylococcus aureus ST398 in food samples of animal origin in Spain. J Antimicrob Chemother. 2009 Dec;64(6):1325–1326. doi: 10.1093/jac/dkp378. Available from: http://dx.doi.org/10.1093/jac/dkp378. [DOI] [PubMed] [Google Scholar]
- 52.Normanno G, Corrente M, La Salandra G, Dambrosio A, Quaglia NC, Parisi A, Greco G, Bellacicco AL, Virgilio S, Celano GV. Methicillin-resistant Staphylococcus aureus (MRSA) in foods of animal origin product in Italy. Int J Food Microbiol. 2007 Jun;117(2):219–222. doi: 10.1016/j.ijfoodmicro.2007.04.006. Available from: http://dx.doi.org/10.1016/j.ijfoodmicro.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 53.European Food Safety Authority, ed. Technical specifications on the harmonised monitoring and reporting of antimicrobial resistance in methicillin-resistant Staphylococcus aureus in food-producing animals and food. EFSA J. 2012;10(10):2897. doi: 10.2903/j.efsa.2012.2897. Available from: http://dx.doi.org/10.2903/j.efsa.2012.2897. [DOI] [Google Scholar]
- 54.Declercq P, Petré D, Gordts B, Voss A. Complicated community-acquired soft tissue infection by MRSA from porcine origin. Infection. 2008 Dec;36(6):590–592. doi: 10.1007/s15010-007-7029-4. Available from: http://dx.doi.org/10.1007/s15010-007-7029-4. [DOI] [PubMed] [Google Scholar]
- 55.Schijffelen MJ, Boel CH, van Strijp JA, Fluit AC. Whole genome analysis of a livestock-associated methicillin-resistant Staphylococcus aureus ST398 isolate from a case of human endocarditis. BMC Genomics. 2010;11:376. doi: 10.1186/1471-2164-11-376. Available from: http://dx.doi.org/10.1186/1471-2164-11-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lozano C, Aspiroz C, Ezpeleta AI, Gómez-Sanz E, Zarazaga M, Torres C. Empyema caused by MRSA ST398 with atypical resistance profile, Spain. Emerging Infect Dis. 2011 Jan;17(1):138–140. doi: 10.3201/eid1701.100307. Available from: http://dx.doi.org/10.3201/eid1701.100307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rasigade JP, Laurent F, Hubert P, Vandenesch F, Etienne J. Lethal necrotizing pneumonia caused by an ST398 Staphylococcus aureus strain. Emerg Infect Dis. 2010 Aug;16(8):1330. doi: 10.3201/eid1608.100317. Available from: http://dx.doi.org/10.3201/eid1608.100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Empfehlung zur Prävention und Kontrolle von Methicillin-resistenten Staphylococcus aureus-Stämmen (MRSA) in Krankenhäusern und anderen medizinischen Einrichtungen: MItteilung der Kommission Krankenhaushygiene und Infektionsprävention am RKI. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 1999;42:954–958. doi: 10.1007/s001030050227. Available from: http://dx.doi.org/10.1007/s001030050227. [DOI] [PubMed] [Google Scholar]
- 59.Robert Koch-Institut. Kommentar zu den Empfehlungen zur Prävention und Kontrolle von MRSA-Stämmen in Krankenhäusern und anderen medizinischen Einrichtungen". Epidemiol Bull. 2008;(42):363–364. Available from: http://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2008/Auschnitte/MRSA_2008_42.pdf. [Google Scholar]
- 60.Garcia-Graells C, Antoine J, Larsen J, Catry B, Skov R, Denis O. Livestock veterinarians at high risk of acquiring methicillin-resistant Staphylococcus aureus ST398. Epidemiol Infect. 2012 Mar;140(3):383–389. doi: 10.1017/S0950268811002263. Available from: http://dx.doi.org/10.1017/S0950268811002263. [DOI] [PubMed] [Google Scholar]
- 61.van Duijkeren E, Jansen MD, Flemming SC, de Neeling H, Wagenaar JA, Schoormans AH, van Nes A, Fluit AC. Methicillin-resistant Staphylococcus aureus in pigs with exudative epidermitis. Emerging Infect Dis. 2007 Sep;13(9):1408–1410. doi: 10.3201/eid1309.061268. Available from: http://dx.doi.org/10.3201/eid1309.061268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fessler A, Scott C, Kadlec K, Ehricht R, Monecke S, Schwarz S. Characterization of methicillin-resistant Staphylococcus aureus ST398 from cases of bovine mastitis. J Antimicrob Chemother. 2010 Apr;65(4):619–625. doi: 10.1093/jac/dkq021. Available from: http://dx.doi.org/10.1093/jac/dkq021. [DOI] [PubMed] [Google Scholar]
- 63.Haenni M, Galofaro L, Ponsin C, Bes M, Laurent F, Madec JY. Staphylococcal bovine mastitis in France: enterotoxins, resistance and the human Geraldine methicillin-resistant Staphylococcus aureus clone. J Antimicrob Chemother. 2011 Jan;66(1):216–218. doi: 10.1093/jac/dkq417. Available from: http://dx.doi.org/10.1093/jac/dkq417. [DOI] [PubMed] [Google Scholar]
- 64.Soares Magalhães RJ, Loeffler A, Lindsay J, Rich M, Roberts L, Smith H, Lloyd DH, Pfeiffer DU. Risk factors for methicillin-resistant Staphylococcus aureus (MRSA) infection in dogs and cats: a case-control study. Vet Res. 2010 Sep-Oct;41(5):55. doi: 10.1051/vetres/2010028. Available from: http://dx.doi.org/10.1051/vetres/2010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cordery RJ, Roberts CH, Cooper SJ, Bellinghan G, Shetty N. Evaluation of risk factors for the acquisition of bloodstream infections with extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella species in the intensive care unit; antibiotic management and clinical outcome. J Hosp Infect. 2008 Feb;68(2):108–115. doi: 10.1016/j.jhin.2007.10.011. Available from: http://dx.doi.org/10.1016/j.jhin.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 66.Kuster SP, Hasse B, Huebner V, Bansal V, Zbinden R, Ruef C, Ledergerber B, Weber R. Risks factors for infections with extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae at a tertiary care university hospital in Switzerland. Infection. 2010 Feb;38(1):33–40. doi: 10.1007/s15010-009-9207-z. Available from: http://dx.doi.org/10.1007/s15010-009-9207-z. [DOI] [PubMed] [Google Scholar]
- 67.Morosini MI, García-Castillo M, Coque TM, Valverde A, Novais A, Loza E, Baquero F, Cantón R. Antibiotic coresistance in extended-spectrum-beta-lactamase-producing Enterobacteriaceae and in vitro activity of tigecycline. Antimicrob Agents Chemother. 2006 Aug;50(8):2695–2699. doi: 10.1128/AAC.00155-06. Available from: http://dx.doi.org/10.1128/AAC.00155-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Carattoli A. Animal reservoirs for extended spectrum beta-lactamase producers. Clin Microbiol Infect. 2008 Jan;14 Suppl 1:117–123. doi: 10.1111/j.1469-0691.2007.01851.x. Available from: http://dx.doi.org/10.1111/j.1469-0691.2007.01851.x. [DOI] [PubMed] [Google Scholar]
- 69.Costa D, Poeta P, Briñas L, Sáenz Y, Rodrigues J, Torres C. Detection of CTX-M-1 and TEM-52 beta-lactamases in Escherichia coli strains from healthy pets in Portugal. J Antimicrob Chemother. 2004 Nov;54(5):960–961. doi: 10.1093/jac/dkh444. Available from: http://dx.doi.org/10.1093/jac/dkh444. [DOI] [PubMed] [Google Scholar]
- 70.Wang Y, He T, Han J, Wang J, Foley SL, Yang G, Wan S, Shen J, Wu C. Prevalence of ESBLs and PMQR genes in fecal Escherichia coli isolated from the non-human primates in six zoos in China. Vet Microbiol. 2012 Sep;159(1-2):53–59. doi: 10.1016/j.vetmic.2012.03.009. Available from: http://dx.doi.org/10.1016/j.vetmic.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 71.Literak I, Dolejska M, Janoszowska D, Hrusakova J, Meissner W, Rzyska H, Bzoma S, Cizek A. Antibiotic-resistant Escherichia coli bacteria, including strains with genes encoding the extended-spectrum beta-lactamase and QnrS, in waterbirds on the Baltic Sea Coast of Poland. Appl Environ Microbiol. 2010 Dec;76(24):8126–8134. doi: 10.1128/AEM.01446-10. Available from: http://dx.doi.org/10.1128/AEM.01446-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Literak I, Dolejska M, Radimersky T, Klimes J, Friedman M, Aarestrup FM, Hasman H, Cizek A. Antimicrobial-resistant faecal Escherichia coli in wild mammals in central Europe: multiresistant Escherichia coli producing extended-spectrum beta-lactamases in wild boars. J Appl Microbiol. 2010 May;108(5):1702–1711. doi: 10.1111/j.1365-2672.2009.04572.x. Available from: http://dx.doi.org/10.1111/j.1365-2672.2009.04572.x. [DOI] [PubMed] [Google Scholar]
- 73.Robert Koch-Institut. ESBL und AmpC:beta-Laktamasen als eine der Hauptursachen der Cephalosporin-Resistenz bei Enterobakterien. Epidemiol Bull; 2007;(28):247-50. p. Available from: http://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2007/Ausschnitte/ESBL_28_07.pdf. Available from: http://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2007/Ausschnitte/ESBL_28_07.pdf. [Google Scholar]
- 74.EFSA Panel on Biological Hazards (BIOHAZ) Scientific Opinion on the public health risks of bacterial strains producing extended-spectrum β-lactamases and/or AmpC β-lactamases in food and food-producing animals. EFSA J. 2011;9(8):2322. doi: 10.2903/j.efsa.2011.2322. Available from: http://dx.doi.org/10.2903/j.efsa.2011.2322. [DOI] [Google Scholar]
- 75.Geser N, Stephan R, Hächler H. Occurrence and characteristics of extended-spectrum β-lactamase (ESBL) producing Enterobacteriaceae in food producing animals, minced meat and raw milk. BMC Vet Res. 2012;8:21. doi: 10.1186/1746-6148-8-21. Available from: http://dx.doi.org/10.1186/1746-6148-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Falagas ME, Karageorgopoulos DE. Extended-spectrum beta-lactamase-producing organisms. J Hosp Infect. 2009 Dec;73(4):345–354. doi: 10.1016/j.jhin.2009.02.021. Available from: http://dx.doi.org/10.1016/j.jhin.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 77.Livermore DM, Canton R, Gniadkowski M, Nordmann P, Rossolini GM, Arlet G, Ayala J, Coque TM, Kern-Zdanowicz I, Luzzaro F, Poirel L, Woodford N. CTX-M: changing the face of ESBLs in Europe. J Antimicrob Chemother. 2007 Feb;59(2):165–174. doi: 10.1093/jac/dkl483. Available from: http://dx.doi.org/10.1093/jac/dkl483. [DOI] [PubMed] [Google Scholar]
- 78.Sayah RS, Kaneene JB, Johnson Y, Miller R. Patterns of antimicrobial resistance observed in Escherichia coli isolates obtained from domestic- and wild-animal fecal samples, human septage, and surface water. Appl Environ Microbiol. 2005 Mar;71(3):1394–1404. doi: 10.1128/AEM.71.3.1394-1404.2005. Available from: http://dx.doi.org/10.1128/AEM.71.3.1394-1404.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Raphael E, Wong LK, Riley LW. Extended-spectrum Beta-lactamase gene sequences in gram-negative saprophytes on retail organic and nonorganic spinach. Appl Environ Microbiol. 2011 Mar;77(5):1601–1607. doi: 10.1128/AEM.02506-10. Available from: http://dx.doi.org/10.1128/AEM.02506-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Locatelli C, Scaccabarozzi L, Pisoni G, Moroni P. CTX-M1 ESBL-producing Klebsiella pneumoniae subsp. pneumoniae isolated from cases of bovine mastitis. J Clin Microbiol. 2010 Oct;48(10):3822–3823. doi: 10.1128/JCM.00941-10. Available from: http://dx.doi.org/10.1128/JCM.00941-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Madec JY, Lazizzera C, Châtre P, Meunier D, Martin S, Lepage G, Ménard MF, Lebreton P, Rambaud T. Prevalence of fecal carriage of acquired expanded-spectrum cephalosporin resistance in Enterobacteriaceae strains from cattle in France. J Clin Microbiol. 2008 Apr;46(4):1566–1567. doi: 10.1128/JCM.02299-07. Available from: http://dx.doi.org/10.1128/JCM.02299-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dolejska M, Jurcickova Z, Literak I, Pokludova L, Bures J, Hera A, Kohoutova L, Smola J, Cizek A. IncN plasmids carrying bla CTX-M-1 in Escherichia coli isolates on a dairy farm. Vet Microbiol. 2011 May;149(3-4):513–516. doi: 10.1016/j.vetmic.2010.11.032. Available from: http://dx.doi.org/10.1016/j.vetmic.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 83.Costa D, Poeta P, Sáenz Y, Vinué L, Rojo-Bezares B, Jouini A, Zarazaga M, Rodrigues J, Torres C. Detection of Escherichia coli harbouring extended-spectrum beta-lactamases of the CTX-M, TEM and SHV classes in faecal samples of wild animals in Portugal. J Antimicrob Chemother. 2006 Dec;58(6):1311–1312. doi: 10.1093/jac/dkl415. Available from: http://dx.doi.org/10.1093/jac/dkl415. [DOI] [PubMed] [Google Scholar]
- 84.Bonnedahl J, Drobni M, Gauthier-Clerc M, Hernandez J, Granholm S, Kayser Y, Melhus A, Kahlmeter G, Waldenström J, Johansson A, Olsen B. Dissemination of Escherichia coli with CTX-M type ESBL between humans and yellow-legged gulls in the south of France. PLoS ONE. 2009;4(6):e5958. doi: 10.1371/journal.pone.0005958. Available from: http://dx.doi.org/10.1371/journal.pone.0005958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Briñas L, Moreno MA, Zarazaga M, Porrero C, Sáenz Y, García M, Dominguez L, Torres C. Detection of CMY-2, CTX-M-14, and SHV-12 beta-lactamases in Escherichia coli fecal-sample isolates from healthy chickens. Antimicrob Agents Chemother. 2003 Jun;47(6):2056–2058. doi: 10.1128/AAC.47.6.2056-2058.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Smet A, Martel A, Persoons D, Dewulf J, Heyndrickx M, Catry B, Herman L, Haesebrouck F, Butaye P. Diversity of extended-spectrum beta-lactamases and class C beta-lactamases among cloacal Escherichia coli Isolates in Belgian broiler farms. Antimicrob Agents Chemother. 2008 Apr;52(4):1238–1243. doi: 10.1128/AAC.01285-07. Available from: http://dx.doi.org/10.1128/AAC.01285-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Weill FX, Lailler R, Praud K, Kérouanton A, Fabre L, Brisabois A, Grimont PA, Cloeckaert A. Emergence of extended-spectrum-beta-lactamase (CTX-M-9)-producing multiresistant strains of Salmonella enterica serotype Virchow in poultry and humans in France. J Clin Microbiol. 2004 Dec;42(12):5767–5773. doi: 10.1128/JCM.42.12.5767-5773.2004. Available from: http://dx.doi.org/10.1128/JCM.42.12.5767-5773.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Girlich D, Poirel L, Carattoli A, Kempf I, Lartigue MF, Bertini A, Nordmann P. Extended-spectrum beta-lactamase CTX-M-1 in Escherichia coli isolates from healthy poultry in France. Appl Environ Microbiol. 2007 Jul;73(14):4681–4685. doi: 10.1128/AEM.02491-06. Available from: http://dx.doi.org/10.1128/AEM.02491-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dierikx C, van Essen-Zandbergen A, Veldman K, Smith H, Mevius D. Increased detection of extended spectrum beta-lactamase producing Salmonella enterica and Escherichia coli isolates from poultry. Vet Microbiol. 2010 Oct;145(3-4):273–278. doi: 10.1016/j.vetmic.2010.03.019. Available from: http://dx.doi.org/10.1016/j.vetmic.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 90.Bortolaia V, Guardabassi L, Trevisani M, Bisgaard M, Venturi L, Bojesen AM. High diversity of extended-spectrum beta-lactamases in Escherichia coli isolates from Italian broiler flocks. Antimicrob Agents Chemother. 2010 Apr;54(4):1623–1626. doi: 10.1128/AAC.01361-09. Available from: http://dx.doi.org/10.1128/AAC.01361-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cortés P, Blanc V, Mora A, Dahbi G, Blanco JE, Blanco M, López C, Andreu A, Navarro F, Alonso MP, Bou G, Blanco J, Llagostera M. Isolation and characterization of potentially pathogenic antimicrobial-resistant Escherichia coli strains from chicken and pig farms in Spain. Appl Environ Microbiol. 2010 May;76(9):2799–2805. doi: 10.1128/AEM.02421-09. Available from: http://dx.doi.org/10.1128/AEM.02421-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zou M, Keelara S, Thakur S. Molecular characterization of Salmonella enterica serotype Enteritidis isolates from humans by antimicrobial resistance, virulence genes, and pulsed-field gel electrophoresis. Foodborne Pathog Dis. 2012 Mar;9(3):232–238. doi: 10.1089/fpd.2011.1012. Available from: http://dx.doi.org/10.1089/fpd.2011.1012. [DOI] [PubMed] [Google Scholar]
- 93.Lavilla S, González-López JJ, Miró E, Domínguez A, Llagostera M, Bartolomé RM, Mirelis B, Navarro F, Prats G. Dissemination of extended-spectrum beta-lactamase-producing bacteria: the food-borne outbreak lesson. J Antimicrob Chemother. 2008 Jun;61(6):1244–1251. doi: 10.1093/jac/dkn093. Available from: http://dx.doi.org/10.1093/jac/dkn093. [DOI] [PubMed] [Google Scholar]
- 94.van den Bogaard AE, London N, Driessen C, Stobberingh EE. Antibiotic resistance of faecal Escherichia coli in poultry, poultry farmers and poultry slaughterers. J Antimicrob Chemother. 2001 Jun;47(6):763–771. doi: 10.1093/jac/dkn093. Available from: http://dx.doi.org/10.1093/jac/dkn093. [DOI] [PubMed] [Google Scholar]
- 95.Simon A, Gröger N, Engelhart S, Molitor G, Exner M, Bode U, Fleischhack G. Vancomycin-resistente Enterokokken (VRE) – Übersicht zu Bedeutung, Prävention und Management in der Pädiatrie. Hyg Med. 2004;29(7/8):259–275. [Google Scholar]
- 96.Haenni M, Saras E, Châtre P, Meunier D, Martin S, Lepage G, Ménard MF, Lebreton P, Rambaud T, Madec JY. vanA in Enterococcus faecium, Enterococcus faecalis, and Enterococcus casseliflavus detected in French cattle. Foodborne Pathog Dis. 2009 Nov;6(9):1107–1111. doi: 10.1089/fpd.2009.0303. Available from: http://dx.doi.org/10.1089/fpd.2009.0303. [DOI] [PubMed] [Google Scholar]
- 97.Galloway-Peña JR, Nallapareddy SR, Arias CA, Eliopoulos GM, Murray BE. Analysis of clonality and antibiotic resistance among early clinical isolates of Enterococcus faecium in the United States. J Infect Dis. 2009 Nov;200(10):1566–1573. doi: 10.1086/644790. Available from: http://dx.doi.org/10.1086/644790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Arthur M, Molinas C, Depardieu F, Courvalin P. Characterization of Tn1546, a Tn3-related transposon conferring glycopeptide resistance by synthesis of depsipeptide peptidoglycan precursors in Enterococcus faecium BM4147. J Bacteriol. 1993 Jan;175(1):117–127. doi: 10.1128/jb.175.1.117-127.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Heintz BH, Halilovic J, Christensen CL. Vancomycin-resistant enterococcal urinary tract infections. Pharmacotherapy. 2010 Nov;30(11):1136–1149. doi: 10.1592/phco.30.11.1136. Available from: http://dx.doi.org/10.1592/phco.30.11.1136. [DOI] [PubMed] [Google Scholar]
- 100.Weiss CA, 3rd, Statz CL, Dahms RA, Remucal MJ, Dunn DL, Beilman GJ. Six years of surgical wound infection surveillance at a tertiary care center: review of the microbiologic and epidemiological aspects of 20,007 wounds. Arch Surg. 1999 Oct;134(10):1041–1048. doi: 10.1001/archsurg.134.10.1041. Available from: http://dx.doi.org/10.1001/archsurg.134.10.1041. [DOI] [PubMed] [Google Scholar]
- 101.Zhanel GG, Laing NM, Nichol KA, Palatnick LP, Noreddin A, Hisanaga T, Johnson JL, Hoban DJ NAVRESS Group. Antibiotic activity against urinary tract infection (UTI) isolates of vancomycin-resistant enterococci (VRE): results from the 2002 North American Vancomycin Resistant Enterococci Susceptibility Study (NAVRESS) J Antimicrob Chemother. 2003 Sep;52(3):382–388. doi: 10.1093/jac/dkg352. Available from: http://dx.doi.org/10.1093/jac/dkg352. [DOI] [PubMed] [Google Scholar]
- 102.van den Bogaard AE, Jensen LB, Stobberingh EE. Vancomycin-resistant enterococci in turkeys and farmers. N Engl J Med. 1997 Nov;337(21):1558–1559. doi: 10.1056/NEJM199711203372117. Available from: http://dx.doi.org/10.1056/NEJM199711203372117. [DOI] [PubMed] [Google Scholar]
- 103.Klein G, Pack A, Reuter G. Antibiotic resistance patterns of enterococci and occurrence of vancomycin-resistant enterococci in raw minced beef and pork in Germany. Appl Environ Microbiol. 1998 May;64(5):1825–1830. doi: 10.1128/aem.64.5.1825-1830.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Butaye P, Devriese LA, Goossens H, Ieven M, Haesebrouck F. Enterococci with acquired vancomycin resistance in pigs and chickens of different age groups. Antimicrob Agents Chemother. 1999 Feb;43(2):365–366. doi: 10.1128/aac.43.2.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Van der Auwera P, Pensart N, Korten V, Murray BE, Leclercq R. Influence of oral glycopeptides on the fecal flora of human volunteers: selection of highly glycopeptide-resistant enterococci. J Infect Dis. 1996 May;173(5):1129–1136. doi: 10.1093/infdis/173.5.1129. Available from: http://dx.doi.org/10.1093/infdis/173.5.1129. [DOI] [PubMed] [Google Scholar]
- 106.Kirst HA, Thompson DG, Nicas TI. Historical yearly usage of vancomycin. Antimicrob Agents Chemother. 1998 May;42(5):1303–1304. doi: 10.1128/aac.42.5.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Klare I, Heier H, Claus H, Böhme G, Marin S, Seltmann G, Hakenbeck R, Antanassova V, Witte W. Enterococcus faecium strains with vanA-mediated high-level glycopeptide resistance isolated from animal foodstuffs and fecal samples of humans in the community. Microb Drug Resist. 1995;1(3):265–272. doi: 10.1089/mdr.1995.1.265. Available from: http://dx.doi.org/10.1089/mdr.1995.1.265. [DOI] [PubMed] [Google Scholar]
- 108.Wegener HC, Madsen M, Nielsen N, Aarestrup FM. Isolation of vancomycin resistant Enterococcus faecium from food. Int J Food Microbiol. 1997 Mar 18;35(1):57–66. doi: 10.1016/S0168-1605(96)01221-4. Available from: http://dx.doi.org/10.1016/S0168-1605(96)01221-4. [DOI] [PubMed] [Google Scholar]
- 109.Pantosti A, Del Grosso M, Tagliabue S, Macrì A, Caprioli A. Decrease of vancomycin-resistant enterococci in poultry meat after avoparcin ban. Lancet. 1999 Aug 28;354(9180):741–742. doi: 10.1016/S0140-6736(99)02395-8. Available from: http://dx.doi.org/10.1016/S0140-6736(99)02395-8. [DOI] [PubMed] [Google Scholar]
- 110.Heuer OE, Pedersen K, Jensen LB, Madsen M, Olsen JE. Persistence of vancomycin-resistant enterococci (VRE) in broiler houses after the avoparcin ban. Microb Drug Resist. 2002;8(4):355–361. doi: 10.1089/10766290260469624. Available from: http://dx.doi.org/10.1089/10766290260469624. [DOI] [PubMed] [Google Scholar]
- 111.Aarestrup FM. Characterization of glycopeptide-resistant enterococcus faecium (GRE) from broilers and pigs in Denmark: genetic evidence that persistence of GRE in pig herds is associated with coselection by resistance to macrolides. J Clin Microbiol. 2000 Jul;38(7):2774–2777. doi: 10.1128/jcm.38.7.2774-2777.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Eisner A, Feierl G, Gorkiewicz G, Dieber F, Kessler HH, Marth E, Köfer J. High prevalence of VanA-type vancomycin-resistant Enterococci in Austrian poultry. Appl Environ Microbiol. 2005 Oct;71(10):6407–6409. doi: 10.1128/AEM.71.10.6407-6409.2005. Available from: http://dx.doi.org/10.1128/AEM.71.10.6407-6409.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ramos S, Igrejas G, Rodrigues J, Capelo-Martinez JL, Poeta P. Genetic characterisation of antibiotic resistance and virulence factors in vanA-containing enterococci from cattle, sheep and pigs subsequent to the discontinuation of the use of avoparcin. Vet J. 2012 Jul;193(1):301–303. doi: 10.1016/j.tvjl.2011.12.007. Available from: http://dx.doi.org/10.1016/j.tvjl.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 114.Willems RJ, Top J, van den Braak N, van Belkum A, Mevius DJ, Hendriks G, van Santen-Verheuvel M, van Embden JD. Molecular diversity and evolutionary relationships of Tn1546-like elements in enterococci from humans and animals. Antimicrob Agents Chemother. 1999 Mar;43(3):483–491. doi: 10.1128/aac.43.3.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Biavasco F, Foglia G, Paoletti C, Zandri G, Magi G, Guaglianone E, Sundsfjord A, Pruzzo C, Donelli G, Facinelli B. VanA-type enterococci from humans, animals, and food: species distribution, population structure, Tn1546 typing and location, and virulence determinants. Appl Environ Microbiol. 2007 May;73(10):3307–3319. doi: 10.1128/AEM.02239-06. Available from: http://dx.doi.org/10.1128/AEM.02239-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Berchieri A. Intestinal colonization of a human subject by vancomycin-resistant Enterococcus faecium. Clin Microbiol Infect. 1999 Feb;5(2):97–100. doi: 10.1111/j.1469-0691.1999.tb00110.x. Available from: http://dx.doi.org/10.1111/j.1469-0691.1999.tb00110.x. [DOI] [PubMed] [Google Scholar]
- 117.Sørensen TL, Blom M, Monnet DL, Frimodt-Møller N, Poulsen RL, Espersen F. Transient intestinal carriage after ingestion of antibiotic-resistant Enterococcus faecium from chicken and pork. N Engl J Med. 2001 Oct;345(16):1161–1166. doi: 10.1056/NEJMoa010692. Available from: http://dx.doi.org/10.1056/NEJMoa010692. [DOI] [PubMed] [Google Scholar]
- 118.Lester CH, Frimodt-Møller N, Sørensen TL, Monnet DL, Hammerum AM. In vivo transfer of the vanA resistance gene from an Enterococcus faecium isolate of animal origin to an E. faecium isolate of human origin in the intestines of human volunteers. Antimicrob Agents Chemother. 2006 Feb;50(2):596–599. doi: 10.1128/AAC.50.2.596-599.2006. Available from: http://dx.doi.org/10.1128/AAC.50.2.596-599.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Larsen J, Schønheyder HC, Lester CH, Olsen SS, Porsbo LJ, Garcia-Migura L, Jensen LB, Bisgaard M, Hammerum AM. Porcine-origin gentamicin-resistant Enterococcus faecalis in humans, Denmark. Emerging Infect Dis. 2010 Apr;16(4):682–684. doi: 10.3201/eid1604.090500. Available from: http://dx.doi.org/10.3201/eid1604.090500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Freitas AR, Novais C, Ruiz-Garbajosa P, Coque TM, Peixe L. Clonal expansion within clonal complex 2 and spread of vancomycin-resistant plasmids among different genetic lineages of Enterococcus faecalis from Portugal. J Antimicrob Chemother. 2009 Jun;63(6):1104–1111. doi: 10.1093/jac/dkp103. Available from: http://dx.doi.org/10.1093/jac/dkp103. [DOI] [PubMed] [Google Scholar]
- 121.Becker K, Peters G. „Staphylococcaceae“, Micrococcaceae und Dermacoccaceae. In: Neumeister B, Geiss HK, Braun RW, Kimming P, editors. Mikrobiologische Diagnostik. 2nd ed. Stuttgart: Georg Thieme Verlag; 2009. pp. 333–351. [Google Scholar]
- 122.Marshall SA, Wilke WW, Pfaller MA, Jones RN. Staphylococcus aureus and coagulase-negative staphylococci from blood stream infections: frequency of occurrence, antimicrobial susceptibility, and molecular (mecA) characterization of oxacillin resistance in the SCOPE program. Diagn Microbiol Infect Dis. 1998 Mar;30(3):205–214. doi: 10.1016/S0732-8893(97)00212-5. Available from: http://dx.doi.org/10.1016/S0732-8893(97)00212-5. [DOI] [PubMed] [Google Scholar]
- 123.Pyörälä S, Taponen S. Coagulase-negative staphylococci-emerging mastitis pathogens. Vet Microbiol. 2009 Feb;134(1-2):3–8. doi: 10.1016/j.vetmic.2008.09.015. Available from: http://dx.doi.org/10.1016/j.vetmic.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 124.Unal N, Cinar OD. Detection of stapylococcal enterotoxin, methicillin-resistant and Panton-Valentine leukocidin genes in coagulase-negative staphylococci isolated from cows and ewes with subclinical mastitis. Trop Anim Health Prod. 2012 Feb;44(2):369–375. doi: 10.1007/s11250-011-0032-x. Available from: http://dx.doi.org/10.1007/s11250-011-0032-x. [DOI] [PubMed] [Google Scholar]
- 125.Watts JL, Ray CH, Washburn PJ. A convenient method for differentiation of coagulase-negative staphylococci isolated from bovine mammary glands. J Dairy Sci. 1991 Feb;74(2):426–428. doi: 10.3168/jds.S0022-0302(91)78186-1. Available from: http://dx.doi.org/10.3168/jds.S0022-0302(91)78186-1. [DOI] [PubMed] [Google Scholar]
- 126.Gentilini E, Denamiel G, Betancor A, Rebuelto M, Rodriguez Fermepin M, De Torrest RA. Antimicrobial susceptibility of coagulase-negative staphylococci isolated from bovine mastitis in Argentina. J Dairy Sci. 2002 Aug;85(8):1913–1917. doi: 10.3168/jds.S0022-0302(02)74267-7. Available from: http://dx.doi.org/10.3168/jds.S0022-0302(02)74267-7. [DOI] [PubMed] [Google Scholar]
- 127.Pitkälä A, Haveri M, Pyörälä S, Myllys V, Honkanen-Buzalski T. Bovine mastitis in Finland 2001--prevalence, distribution of bacteria, and antimicrobial resistance. J Dairy Sci. 2004 Aug;87(8):2433–2441. doi: 10.3168/jds.S0022-0302(04)73366-4. Available from: http://dx.doi.org/10.3168/jds.S0022-0302(04)73366-4. [DOI] [PubMed] [Google Scholar]
- 128.Sampimon OC, Vernooij JC, Mevius DJ, Sol J. Gevoeligheid voor diverse antibiotica van coagulase negatieve staphylococcen, geïsoleerd uit melkmonsters van Nederlands rundvee. [Sensitivity to various antibiotics of coagulase-negative staphylococci isolated from samples of milk from Dutch dairy cattle]. Tijdschr Diergeneeskd. 2007 Mar;132(6):200–204. [PubMed] [Google Scholar]
- 129.Zhang Y, Agidi S, LeJeune JT. Diversity of staphylococcal cassette chromosome in coagulase-negative staphylococci from animal sources. J Appl Microbiol. 2009 Oct;107(4):1375–1383. doi: 10.1111/j.1365-2672.2009.04322.x. Available from: http://dx.doi.org/10.1111/j.1365-2672.2009.04322.x. [DOI] [PubMed] [Google Scholar]
- 130.Kawano J, Shimizu A, Saitoh Y, Yagi M, Saito T, Okamoto R. Isolation of methicillin-resistant coagulase-negative staphylococci from chickens. J Clin Microbiol. 1996 Sep;34(9):2072–2077. doi: 10.1128/jcm.34.9.2072-2077.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Huber H, Ziegler D, Pflüger V, Vogel G, Zweifel C, Stephan R. Prevalence and characteristics of methicillin-resistant coagulase-negative staphylococci from livestock, chicken carcasses, bulk tank milk, minced meat, and contact persons. BMC Vet Res. 2011;7:6. doi: 10.1186/1746-6148-7-6. Available from: http://dx.doi.org/10.1186/1746-6148-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Huber H, Giezendanner N, Stephan R, Zweifel C. Genotypes, antibiotic resistance profiles and microarray-based characterization of methicillin-resistant Staphylococcus aureus strains isolated from livestock and veterinarians in Switzerland. Zoonoses Public Health. 2011 Aug;58(5):343–349. doi: 10.1111/j.1863-2378.2010.01353.x. Available from: http://dx.doi.org/10.1111/j.1863-2378.2010.01353.x. [DOI] [PubMed] [Google Scholar]
- 133.Haenni M, Châtre P, Boisset S, Carricajo A, Bes M, Laurent F, Madec JY. Staphylococcal nasal carriage in calves: multiresistant Staphylococcus sciuri and immune evasion cluster (IEC) genes in methicillin-resistant Staphylococcus aureus ST398. J Antimicrob Chemother. 2011 Aug;66(8):1927–1928. doi: 10.1093/jac/dkr196. Available from: http://dx.doi.org/10.1093/jac/dkr196. [DOI] [PubMed] [Google Scholar]
- 134.Wielders CL, Vriens MR, Brisse S, de Graaf-Miltenburg LA, Troelstra A, Fleer A, Schmitz FJ, Verhoef J, Fluit AC. In-vivo transfer of mecA DNA to Staphylococcus aureus [corrected] Lancet. 2001 May 26;357(9269):1674–1675. doi: 10.1016/S0140-6736(00)04832-7. Available from: http://dx.doi.org/10.1016/S0140-6736(00)04832-7. [DOI] [PubMed] [Google Scholar]
- 135.Hanssen AM, Kjeldsen G, Sollid JU. Local variants of Staphylococcal cassette chromosome mec in sporadic methicillin-resistant Staphylococcus aureus and methicillin-resistant coagulase-negative Staphylococci: evidence of horizontal gene transfer? Antimicrob Agents Chemother. 2004 Jan;48(1):285–296. doi: 10.1128/AAC.48.1.285-296.2004. Available from: http://dx.doi.org/10.1128/AAC.48.1.285-296.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Bloemendaal AL, Brouwer EC, Fluit AC. Methicillin resistance transfer from Staphylocccus epidermidis to methicillin-susceptible Staphylococcus aureus in a patient during antibiotic therapy. PLoS ONE. 2010;5(7):e11841. doi: 10.1371/journal.pone.0011841. Available from: http://dx.doi.org/10.1371/journal.pone.0011841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Barbier F, Ruppé E, Hernandez D, Lebeaux D, Francois P, Felix B, Desprez A, Maiga A, Woerther PL, Gaillard K, Jeanrot C, Wolff M, Schrenzel J, Andremont A, Ruimy R. Methicillin-resistant coagulase-negative staphylococci in the community: high homology of SCCmec IVa between Staphylococcus epidermidis and major clones of methicillin-resistant Staphylococcus aureus. J Infect Dis. 2010 Jul;202(2):270–281. doi: 10.1086/653483. Available from: http://dx.doi.org/10.1086/653483. [DOI] [PubMed] [Google Scholar]
- 138.Tulinski P, Fluit AC, Wagenaar JA, Mevius D, van de Vijver L, Duim B. Methicillin-resistant coagulase-negative staphylococci on pig farms as a reservoir of heterogeneous staphylococcal cassette chromosome mec elements. Appl Environ Microbiol. 2012 Jan;78(2):299–304. doi: 10.1128/AEM.05594-11. Available from: http://dx.doi.org/10.1128/AEM.05594-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Blot E, Escande MC, Besson D, Barbut F, Granpeix C, Asselain B, Falcou MC, Pouillart P. Outbreak of Clostridium difficile-related diarrhoea in an adult oncology unit: risk factors and microbiological characteristics. J Hosp Infect. 2003 Mar;53(3):187–192. doi: 10.1053/jhin.2002.1356. Available from: http://dx.doi.org/10.1053/jhin.2002.1356. [DOI] [PubMed] [Google Scholar]
- 140.Paltansing S, van den Berg RJ, Guseinova RA, Visser CE, van der Vorm ER, Kuijper EJ. Characteristics and incidence of Clostridium difficile-associated disease in The Netherlands, 2005. Clin Microbiol Infect. 2007 Nov;13(11):1058–1064. doi: 10.1111/j.1469-0691.2007.01793.x. Available from: http://dx.doi.org/10.1111/j.1469-0691.2007.01793.x. [DOI] [PubMed] [Google Scholar]
- 141.Zidaric V, Zemljic M, Janezic S, Kocuvan A, Rupnik M. High diversity of Clostridium difficile genotypes isolated from a single poultry farm producing replacement laying hens. Anaerobe. 2008 Dec;14(6):325–327. doi: 10.1016/j.anaerobe.2008.10.001. Available from: http://dx.doi.org/10.1016/j.anaerobe.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 142.Weese JS, Reid-Smith RJ, Avery BP, Rousseau J. Detection and characterization of Clostridium difficile in retail chicken. Lett Appl Microbiol. 2010 Apr;50(4):362–365. doi: 10.1111/j.1472-765X.2010.02802.x. Available from: http://dx.doi.org/10.1111/j.1472-765X.2010.02802.x. [DOI] [PubMed] [Google Scholar]
- 143.Rodriguez-Palacios A, Staempfli HR, Duffield T, Weese JS. Clostridium difficile in retail ground meat, Canada. Emerging Infect Dis. 2007 Mar;13(3):485–487. doi: 10.3201/eid1303.060988. Available from: http://dx.doi.org/10.3201/eid1303.060988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rodriguez-Palacios A, Stämpfli HR, Duffield T, Peregrine AS, Trotz-Williams LA, Arroyo LG, Brazier JS, Weese JS. Clostridium difficile PCR ribotypes in calves, Canada. Emerging Infect Dis. 2006 Nov;12(11):1730–1736. doi: 10.3201/eid1211.051581. Available from: http://dx.doi.org/10.3201/eid1211.051581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Aldeyab MA, Harbarth S, Vernaz N, Kearney MP, Scott MG, Funston C, Savage K, Kelly D, Aldiab MA, McElnay JC. Quasiexperimental study of the effects of antibiotic use, gastric acid-suppressive agents, and infection control practices on the incidence of Clostridium difficile-associated diarrhea in hospitalized patients. Antimicrob Agents Chemother. 2009 May;53(5):2082–2088. doi: 10.1128/AAC.01214-08. Available from: http://dx.doi.org/10.1128/AAC.01214-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.McDonald LC, Killgore GE, Thompson A, Owens RC, Jr, Kazakova SV, Sambol SP, Johnson S, Gerding DN. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med. 2005 Dec;353(23):2433–2441. doi: 10.1056/NEJMoa051590. Available from: http://dx.doi.org/10.1056/NEJMoa051590. [DOI] [PubMed] [Google Scholar]
- 147.Stubbs S, Rupnik M, Gibert M, Brazier J, Duerden B, Popoff M. Production of actin-specific ADP-ribosyltransferase (binary toxin) by strains of Clostridium difficile. FEMS Microbiol Lett. 2000 May;186(2):307–312. doi: 10.1111/j.1574-6968.2000.tb09122.x. Available from: http://dx.doi.org/10.1111/j.1574-6968.2000.tb09122.x. [DOI] [PubMed] [Google Scholar]
- 148.Freeman J, Bauer MP, Baines SD, Corver J, Fawley WN, Goorhuis B, Kuijper EJ, Wilcox MH. The changing epidemiology of Clostridium difficile infections. Clin Microbiol Rev. 2010 Jul;23(3):529–549. doi: 10.1128/CMR.00082-09. Available from: http://dx.doi.org/10.1128/CMR.00082-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pépin J, Valiquette L, Alary ME, Villemure P, Pelletier A, Forget K, Pépin K, Chouinard D. Clostridium difficile-associated diarrhea in a region of Quebec from 1991 to 2003: a changing pattern of disease severity. CMAJ. 2004 Aug;171(5):466–472. doi: 10.1503/cmaj.1041104. Available from: http://dx.doi.org/10.1503/cmaj.1041104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Weese JS. Clostridium difficile in food--innocent bystander or serious threat? Clin Microbiol Infect. 2010 Jan;16(1):3–10. doi: 10.1111/j.1469-0691.2009.03108.x. Available from: http://dx.doi.org/10.1111/j.1469-0691.2009.03108.x. [DOI] [PubMed] [Google Scholar]
- 151.Indra A, Schmid D, Huhulescu S, Hell M, Gattringer R, Hasenberger P, Fiedler A, Wewalka G, Allerberger F. Characterization of clinical Clostridium difficile isolates by PCR ribotyping and detection of toxin genes in Austria, 2006-2007. J Med Microbiol. 2008 Jun;57(Pt 6):702–708. doi: 10.1099/jmm.0.47476-0. Available from: http://dx.doi.org/10.1099/jmm.0.47476-0. [DOI] [PubMed] [Google Scholar]
- 152.Akerlund T, Alefjord I, Dohnhammar U, Struwe J, Noren T, Tegmark-Wisell K Swedish C. difficile Study Group. Geographical clustering of cases of infection with moxifloxacin-resistant Clostridium difficile PCR-ribotypes 012, 017 and 046 in Sweden, 2008 and 2009. Euro Surveill. 2011 Mar 10;16(10. pii):19813. doi: 10.2807/ese.16.10.19813-en. [DOI] [PubMed] [Google Scholar]
- 153.Stabler RA, Dawson LF, Valiente E, Cairns MD, Martin MJ, Donahue EH, Riley TV, Songer JG, Kuijper EJ, Dingle KE, Wren BW. Macro and micro diversity of Clostridium difficile isolates from diverse sources and geographical locations. PLoS ONE. 2012;7(3):e31559. doi: 10.1371/journal.pone.0031559. Available from: http://dx.doi.org/10.1371/journal.pone.0031559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Bauer MP, Notermans DW, van Benthem BH, Brazier JS, Wilcox MH, Rupnik M, Monnet DL, van Dissel JT, Kuijper EJ ECDIS Study Group. Clostridium difficile infection in Europe: a hospital-based survey. Lancet. 2011 Jan 1;377(9759):63–73. doi: 10.1016/S0140-6736(10)61266-4. Available from: http://dx.doi.org/10.1016/S0140-6736(10)61266-4. [DOI] [PubMed] [Google Scholar]
- 155.Keel K, Brazier JS, Post KW, Weese S, Songer JG. Prevalence of PCR ribotypes among Clostridium difficile isolates from pigs, calves, and other species. J Clin Microbiol. 2007 Jun;45(6):1963–1964. doi: 10.1128/JCM.00224-07. Available from: http://dx.doi.org/10.1128/JCM.00224-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Goorhuis A, Debast SB, van Leengoed LA, Harmanus C, Notermans DW, Bergwerff AA, Kuijper EJ. Clostridium difficile PCR ribotype 078: an emerging strain in humans and in pigs? J Clin Microbiol. 2008 Mar;46(3):1157. doi: 10.1128/JCM.01536-07. Available from: http://dx.doi.org/10.1128/JCM.01536-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hopman NE, Keessen EC, Harmanus C, Sanders IM, van Leengoed LA, Kuijper EJ, Lipman LJ. Acquisition of Clostridium difficile by piglets. Vet Microbiol. 2011 Apr;149(1-2):186–192. doi: 10.1016/j.vetmic.2010.10.013. Available from: http://dx.doi.org/10.1016/j.vetmic.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 158.Costa MC, Reid-Smith R, Gow S, Hannon SJ, Booker C, Rousseau J, Benedict KM, Morley PS, Weese JS. Prevalence and molecular characterization of Clostridium difficile isolated from feedlot beef cattle upon arrival and mid-feeding period. BMC Vet Res. 2012;8:38. doi: 10.1186/1746-6148-8-38. Available from: http://dx.doi.org/10.1186/1746-6148-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Cartman ST, Heap JT, Kuehne SA, Cockayne A, Minton NP. The emergence of 'hypervirulence' in Clostridium difficile. Int J Med Microbiol. 2010 Aug;300(6):387–395. doi: 10.1016/j.ijmm.2010.04.008. Available from: http://dx.doi.org/10.1016/j.ijmm.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 160.Norman KN, Harvey RB, Scott HM, Hume ME, Andrews K, Brawley AD. Varied prevalence of Clostridium difficile in an integrated swine operation. Anaerobe. 2009 Dec;15(6):256–260. doi: 10.1016/j.anaerobe.2009.09.006. Available from: http://dx.doi.org/10.1016/j.anaerobe.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 161.Weese JS, Wakeford T, Reid-Smith R, Rousseau J, Friendship R. Longitudinal investigation of Clostridium difficile shedding in piglets. Anaerobe. 2010 Oct;16(5):501–504. doi: 10.1016/j.anaerobe.2010.08.001. Available from: http://dx.doi.org/10.1016/j.anaerobe.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 162.Costa MC, Stämpfli HR, Arroyo LG, Pearl DL, Weese JS. Epidemiology of Clostridium difficile on a veal farm: prevalence, molecular characterization and tetracycline resistance. Vet Microbiol. 2011 Sep 28;152(3-4):379–384. doi: 10.1016/j.vetmic.2011.05.014. Available from: http://dx.doi.org/10.1016/j.vetmic.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 163.Debast SB, van Leengoed LA, Goorhuis A, Harmanus C, Kuijper EJ, Bergwerff AA. Clostridium difficile PCR ribotype 078 toxinotype V found in diarrhoeal pigs identical to isolates from affected humans. Environ Microbiol. 2009 Feb;11(2):505–511. doi: 10.1111/j.1462-2920.2008.01790.x. Available from: http://dx.doi.org/10.1111/j.1462-2920.2008.01790.x. [DOI] [PubMed] [Google Scholar]
- 164.Songer JG, Trinh HT, Killgore GE, Thompson AD, McDonald LC, Limbago BM. Clostridium difficile in retail meat products, USA, 2007. Emerging Infect Dis. 2009 May;15(5):819–821. doi: 10.3201/eid1505.081071. Available from: http://dx.doi.org/10.3201/eid1505.081071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Harvey RB, Norman KN, Andrews K, Norby B, Hume ME, Scanlan CM, Hardin MD, Scott HM. Clostridium difficile in retail meat and processing plants in Texas. J Vet Diagn Invest. 2011 Jul;23(4):807–811. doi: 10.1177/1040638711407893. Available from: http://dx.doi.org/10.1177/1040638711407893. [DOI] [PubMed] [Google Scholar]
- 166.de Boer E, Zwartkruis-Nahuis A, Heuvelink AE, Harmanus C, Kuijper EJ. Prevalence of Clostridium difficile in retailed meat in the Netherlands. Int J Food Microbiol. 2011 Jan;144(3):561–564. doi: 10.1016/j.ijfoodmicro.2010.11.007. Available from: http://dx.doi.org/10.1016/j.ijfoodmicro.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 167.Von Abercron SM, Karlsson F, Wigh GT, Wierup M, Krovacek K. Low occurrence of Clostridium difficile in retail ground meat in Sweden. J Food Prot. 2009 Aug;72(8):1732–1734. doi: 10.4315/0362-028x-72.8.1732. [DOI] [PubMed] [Google Scholar]
- 168.Jöbstl M, Heuberger S, Indra A, Nepf R, Köfer J, Wagner M. Clostridium difficile in raw products of animal origin. Int J Food Microbiol. 2010 Mar;138(1-2):172–175. doi: 10.1016/j.ijfoodmicro.2009.12.022. Available from: http://dx.doi.org/10.1016/j.ijfoodmicro.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 169.Rodriguez-Palacios A, Lejeune JT. Moist-heat resistance, spore aging, and superdormancy in Clostridium difficile. Appl Environ Microbiol. 2011 May;77(9):3085–3091. doi: 10.1128/AEM.01589-10. Available from: http://dx.doi.org/10.1128/AEM.01589-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Levy SB, FitzGerald GB, Macone AB. Spread of antibiotic-resistant plasmids from chicken to chicken and from chicken to man. Nature. 1976 Mar;260(5546):40–42. doi: 10.1038/260040a0. Available from: http://dx.doi.org/10.1038/260040a0. [DOI] [PubMed] [Google Scholar]
- 171.Gibbs SG, Green CF, Tarwater PM, Mota LC, Mena KD, Scarpino PV. Isolation of antibiotic-resistant bacteria from the air plume downwind of a swine confined or concentrated animal feeding operation. Environ Health Perspect. 2006 Jul;114(7):1032–1037. doi: 10.1289/ehp.8910. Available from: http://dx.doi.org/10.1289/ehp.8910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Literak I, Dolejska M, Rybarikova J, Cizek A, Strejckova P, Vyskocilova M, Friedman M, Klimes J. Highly variable patterns of antimicrobial resistance in commensal Escherichia coli isolates from pigs, sympatric rodents, and flies. Microb Drug Resist. 2009 Sep;15(3):229–237. doi: 10.1089/mdr.2009.0913. Available from: http://dx.doi.org/10.1089/mdr.2009.0913. [DOI] [PubMed] [Google Scholar]
- 173.Menschen können sich über den Kontakt mit Nutztieren mit Methicillin-resistenten Staphylococcus aureus (MRSA) infizieren. Stellungnahme Nr. 014/2009 des BfR vom 15. März 2009. Bundesinstitut für Risikobewertung; 2009. Available from: http://www.bfr.bund.de/cm/343/menschen_koennen_sich_ueber_den_kontakt_mit_nutztieren_mit_mrsa_infizieren.pdf. [Google Scholar]
- 174.GERMAP 2008. Antibiotika-Resistenz und -Verbrauch. Bericht über den Antibiotikaverbrauch und die Verbreitung von Antibiotikaresistenzen in der Human- und Veterinärmedizin in Deutschland. Rheinbach: Antiinfectives Intelligence Gesellschaft für klinisch-mikrobiologische Forschung und Kommunikation mbH; 2008. Available from: http://www.bvl.bund.de/SharedDocs/Downloads/08_PresseInfothek/Germap_2008.html. [Google Scholar]
- 175.Büchter B. Vorkommen und Charakterisierung von Extended-Spectrum-Beta-Laktamase (ESBL)-produzierenden Escherichia coli bei Lebensmittel liefernden Tieren [PhD-Thesis] Berlin: Institut für Mikrobiologie und Tierseuchen des Fachbereichs Veterinärmedizin der Freien Universität Berlin, Bundesamt für Verbraucherschutz und Lebensmittelsicherheit; 2010. Available from: http://www.diss.fu-berlin.de/diss/receive/FUDISS_thesis_000000020799. [Google Scholar]
- 176.Doi Y, Paterson DL, Egea P, Pascual A, López-Cerero L, Navarro MD, Adams-Haduch JM, Qureshi ZA, Sidjabat HE, Rodríguez-Baño J. Extended-spectrum and CMY-type beta-lactamase-producing Escherichia coli in clinical samples and retail meat from Pittsburgh, USA and Seville, Spain. Clin Microbiol Infect. 2010 Jan;16(1):33–38. doi: 10.1111/j.1469-0691.2009.03001.x. Available from: http://dx.doi.org/10.1111/j.1469-0691.2009.03001.x. [DOI] [PubMed] [Google Scholar]
- 177.Cohen Stuart J, van den Munckhof T, Voets G, Scharringa J, Fluit A, Hall ML. Comparison of ESBL contamination in organic and conventional retail chicken meat. Int J Food Microbiol. 2012 Mar;154(3):212–214. doi: 10.1016/j.ijfoodmicro.2011.12.034. Available from: http://dx.doi.org/10.1016/j.ijfoodmicro.2011.12.034. [DOI] [PubMed] [Google Scholar]
- 178.Gregova G, Kmetova M, Kmet V, Venglovsky J, Feher A. Antibiotic resistance of Escherichia coli isolated from a poultry slaughterhouse. Ann Agric Environ Med. 2012 Mar;19(1):75–77. [PubMed] [Google Scholar]
- 179.EARS-Net database. ECDC; [cited 2013 01.07.13]]. Available from: http://www.ecdc.europa.eu/en/activities/surveillance/EARS-Net/database/Pages/database.aspx. [Google Scholar]
- 180.GERMAP 2010. Antibiotika-Resistenz und -Verbrauch. Bericht über den Antibiotikaverbrauch und die Verbreitung von Antibiotikaresistenzen in der Human- und Veterinärmedizin in Deutschland. Rheinbach: Antiinfectives Intelligence Gesellschaft für klinisch-mikrobiologische Forschung und Kommunikation mbH; 2011. [cited 01.07.13]. Available from: http://www.p-e-g.org/aktuelles/497. [Google Scholar]
- 181.de Niederhäusern S, Bondi M, Messi P, Iseppi R, Sabia C, Manicardi G, Anacarso I. Vancomycin-resistance transferability from VanA enterococci to Staphylococcus aureus. Curr Microbiol. 2011 May;62(5):1363–1367. doi: 10.1007/s00284-011-9868-6. Available from: http://dx.doi.org/10.1007/s00284-011-9868-6. [DOI] [PubMed] [Google Scholar]
- 182.Khanna S, Pardi DS, Aronson SL, Kammer PP, Orenstein R, St Sauver JL, Harmsen WS, Zinsmeister AR. The epidemiology of community-acquired Clostridium difficile infection: a population-based study. Am J Gastroenterol. 2012 Jan;107(1):89–95. doi: 10.1038/ajg.2011.398. Available from: http://dx.doi.org/10.1038/ajg.2011.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Centers for Disease Control and Prevention (CDC) Severe Clostridium difficile-associated disease in populations previously at low risk--four states, 2005. MMWR Morb Mortal Wkly Rep. 2005 Dec;54(47):1201–1205. [PubMed] [Google Scholar]
- 184.Jangi S, Lamont JT. Asymptomatic colonization by Clostridium difficile in infants: implications for disease in later life. J Pediatr Gastroenterol Nutr. 2010 Jul;51(1):2–7. doi: 10.1097/MPG.0b013e3181d29767. Available from: http://dx.doi.org/10.1097/MPG.0b013e3181d29767. [DOI] [PubMed] [Google Scholar]
- 185.van Duijkeren E, Ikawaty R, Broekhuizen-Stins MJ, Jansen MD, Spalburg EC, de Neeling AJ, Allaart JG, van Nes A, Wagenaar JA, Fluit AC. Transmission of methicillin-resistant Staphylococcus aureus strains between different kinds of pig farms. Vet Microbiol. 2008 Jan;126(4):383–389. doi: 10.1016/j.vetmic.2007.07.021. Available from: http://dx.doi.org/10.1016/j.vetmic.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 186.Battisti A, Franco A, Merialdi G, Hasman H, Iurescia M, Lorenzetti R, Feltrin F, Zini M, Aarestrup FM. Heterogeneity among methicillin-resistant Staphylococcus aureus from Italian pig finishing holdings. Vet Microbiol. 2010 May;142(3-4):361–366. doi: 10.1016/j.vetmic.2009.10.008. Available from: http://dx.doi.org/10.1016/j.vetmic.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 187.Frick JE. Prävalenz Methicillin-resistener Staphyloccocus aureus (MRSA) in bayrischen Schweinebeständen [PhD-Thesis] München: Tierärztliche Fakultät der Ludwig-Maximilians-Universität; 2010. Available from: http://edoc.ub.uni-muenchen.de/11531/ [Google Scholar]
- 188.Broens EM, Graat EA, Van der Wolf PJ, Van de Giessen AW, De Jong MC. Prevalence and risk factor analysis of livestock associated MRSA-positive pig herds in The Netherlands. Prev Vet Med. 2011 Oct 1;102(1):41–49. doi: 10.1016/j.prevetmed.2011.06.005. Available from: http://dx.doi.org/10.1016/j.prevetmed.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 189.van Rijen MM, Van Keulen PH, Kluytmans JA. Increase in a Dutch hospital of methicillin-resistant Staphylococcus aureus related to animal farming. Clin Infect Dis. 2008 Jan;46(2):261–263. doi: 10.1086/524672. Available from: http://dx.doi.org/10.1086/524672. [DOI] [PubMed] [Google Scholar]
- 190.Mørk T, Jørgensen HJ, Sunde M, Kvitle B, Sviland S, Waage S, Tollersrud T. Persistence of staphylococcal species and genotypes in the bovine udder. Vet Microbiol. 2012 Sep 14;159(1-2):171–180. doi: 10.1016/j.vetmic.2012.03.034. Available from: http://dx.doi.org/10.1016/j.vetmic.2012.03.034. [DOI] [PubMed] [Google Scholar]