Abstract
Background:
The abdomen remains a popular donor site for autologous tissue breast reconstruction. Recently, however, some authors have questioned whether the pedicled transverse rectus abdominis myocutaneous (TRAM) flap should remain a first-line reconstruction option.
Methods:
Between 1998 and 2009, 188 women underwent breast reconstruction with pedicled TRAM flaps by the senior author (J.A.A.). All TRAM flaps involved reinforcement of the abdominal wall repair with polypropylene mesh. Reconstruction was unilateral in 164 patients and bilateral in 24 patients, yielding a total of 212 flaps.
Results:
The mean follow-up period was 36 months. There were no complete flap losses. Overall hernia rate for the series was 1.6%, and overall abdominal bulge rate was 0.5%. When combining all types of morbidity, 38 unilateral (23.2%) and zero bilateral TRAM flap patients experienced flap site complications (P = 0.005), and 16 unilateral (9.8%) and 5 bilateral patients (20.8%) experienced donor site complications (P = 0.155). For morbidity that required a return to the operating room, the overall rate was 4.3% for unilateral TRAM flap patients and 4.2% for bilateral TRAM flap patients. Flap site morbidity was significantly associated with obesity, former or active smoking, and receiving 2 or more adjuvant therapies. Donor site morbidity was significantly associated with obesity.
Conclusions:
The pedicled TRAM flap continues to be an excellent option for breast reconstruction. Complication rates for both unilateral and bilateral TRAM flaps were low in this series, with no complete flap losses and just 4.3% of patients requiring a return to the operating room secondary to morbidity.
The transverse rectus abdominis myocutaneous (TRAM) flap is one of the most common methods of autologous tissue breast reconstruction.1 Since its development by Hartrampf et al2 in 1982, the TRAM flap procedure has been valued for its aesthetic outcomes, avoidance of a prosthetic implant, and high patient satisfaction. It remains one of the most popular methods of breast reconstruction today despite concerns regarding postoperative donor site morbidity.1–5
The purpose of this study is to address concerns regarding the pedicled TRAM flap by providing a detailed and up-to-date analysis of the morbidity associated with the procedure when polypropylene mesh is used to reinforce the abdominal wall repair. The study involves a series of 212 consecutive pedicled TRAM flaps performed in 188 patients by a single surgeon. This outcomes analysis includes a detailed review of flap and donor site morbidity and an assessment of relevant risk factors.
PATIENTS AND METHODS
Between December 1998 and December 2009, 188 patients underwent breast reconstruction with pedicled TRAM flaps by the senior author (J.A.A.) at the Columbia University Medical Center. All patients played an active role in the decision-making process and were provided the option of pedicled flaps, free flaps, or implant-based reconstruction.
The pedicled TRAM flap procedure was performed as described previously, employing an onlay polypropylene mesh to reinforce the abdominal wall closure.6,7 Reconstructions used the full width and a variable length of the rectus abdominis muscle. Patient charts were reviewed retrospectively for complications, including complete and partial flap loss, fat necrosis, infection, seroma, hematoma, abdominal hernia or bulge, skin loss, mesh removal, umbilical ischemia or stenosis, revision of the abdominal closure, and persistent abdominal wall discomfort requiring physical therapy referral.
Complete flap loss was defined as necrosis of 50% or more of the TRAM flap, whereas partial flap loss was defined as necrosis of less than 50% of the flap. Infection was defined as any signs of infection of the breast or abdomen requiring antibiotics or an incision and drainage procedure. Hernia was defined as any postoperative abdominal wall fascial defect. Abdominal bulge was defined as protrusion of the abdominal wall apparent on clinical examination but without an obvious fascial defect. Skin loss was defined as any full-thickness skin necrosis. Fat necrosis was defined as any subcutaneous tissue firmness persisting for at least 5 months following surgery that was treated with resection, either in the office or in the operating room, and was pathologically confirmed as fat necrosis. Seroma was any detectable collection of serous fluid.
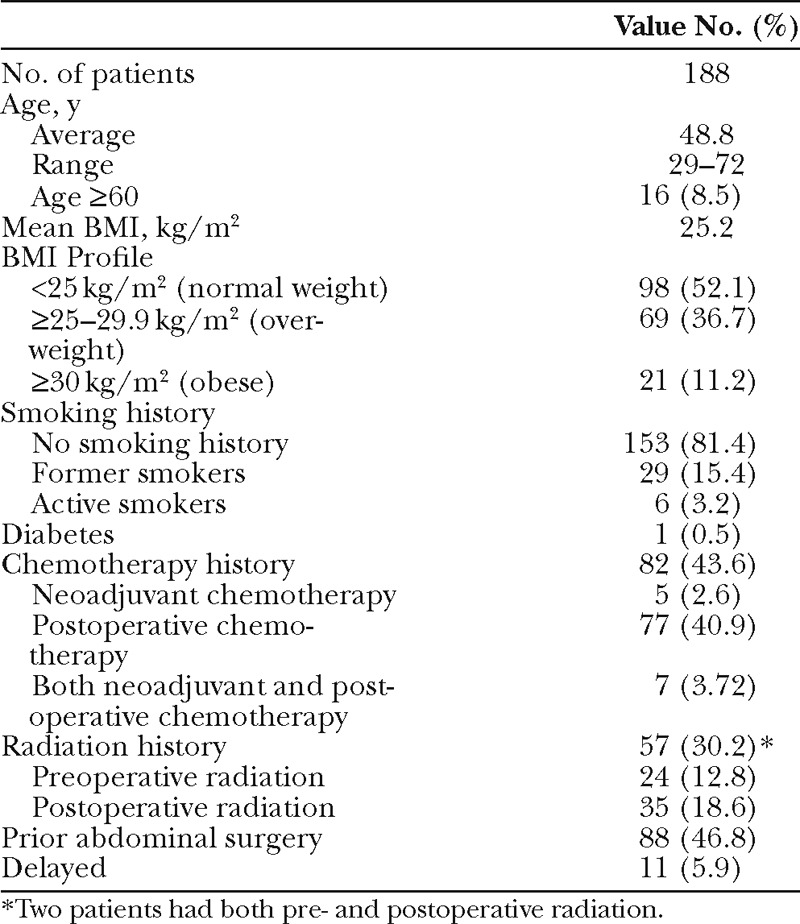
Data regarding patient demographics and possible risk factors were analyzed and included age, body mass index (BMI), diabetes, smoking history, previous abdominal surgery, radiation history, and chemotherapy history (Table 1). Patients were divided into age <60 or ≥60. BMI was categorized into normal (<25.0), overweight (≥25 and <30), or obese (≥30). Smoking history was subdivided into nonsmokers, former smokers (quit at least 4 weeks before surgery), or active smokers. Radiation history was divided into preoperative and postoperative radiation. Chemotherapy history was divided into neoadjuvant only, postoperative, and combined neoadjuvant and postoperative chemotherapy.
Table 1.
Patient Demographics and History
All statistical analyses were performed using the MedCalc statistics software (MedCalc Inc., Belgium), and statistical significance was defined as P < 0.05. In Tables 2 and 3, the 2-tailed Fisher’s exact test was used to compare bilateral and unilateral complication rates. The χ2 test was then used to determine independence of risk factors before regression analysis. Logistic regression analysis was performed to identify associations between potential risk factors and complications and is represented in Tables 4 and 5. Categories with a sample size greater than 10 were included in the regression models. Categorical variables were represented with dummy variables. Stepwise regression was performed in Table 5 with exclusion of risk factors resulting in P > 0.1 to strengthen the reproducibility of the regression model in identifying risk factor associations.
Table 2.
Flap Site Complications in Unilateral vs Bilateral TRAM Flap Patients
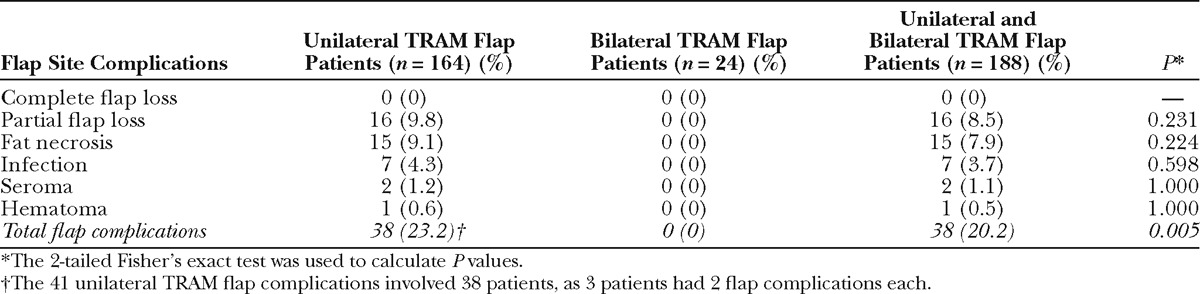
Table 3.
Donor Site Complications in Unilateral vs Bilateral TRAM Flap Patients
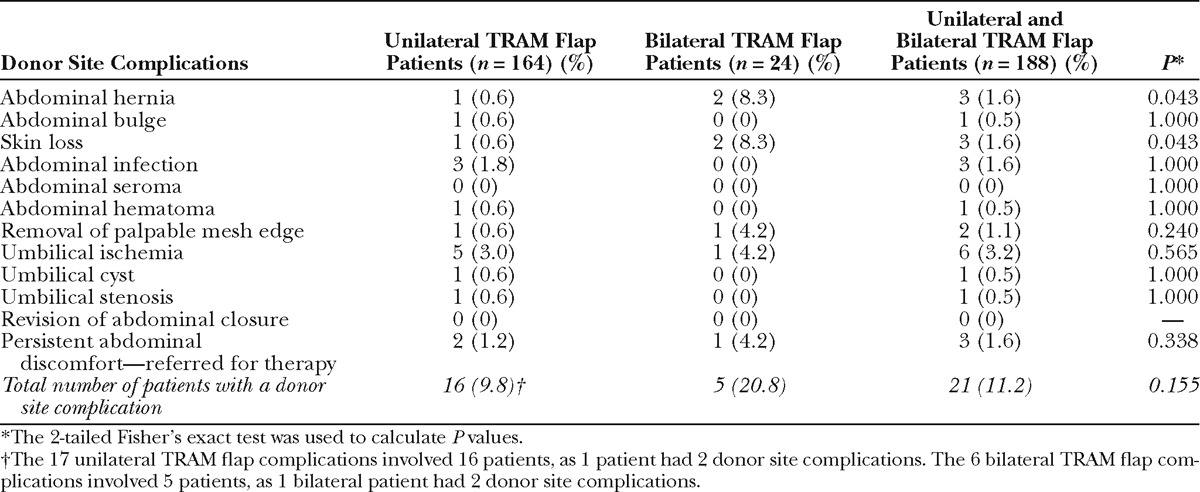
Table 4.
Multivariate Analysis of Independent Risk Factors for the Development of Flap Site, Donor Site, and Overall Complications after Pedicled TRAM Flap
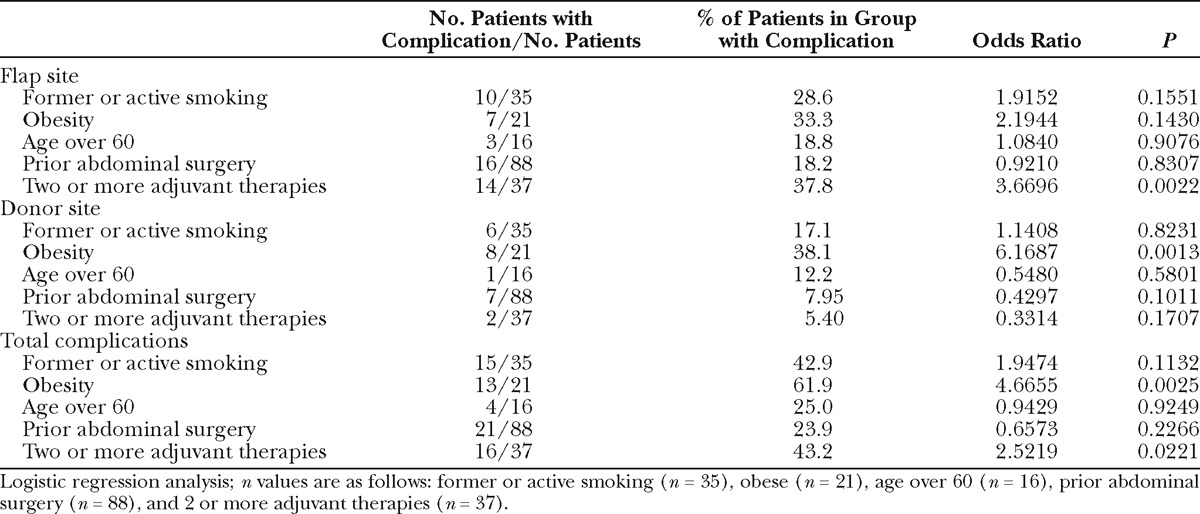
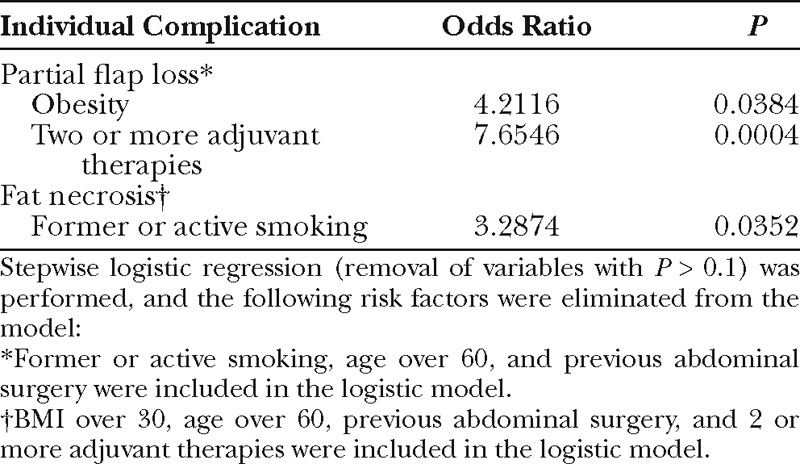
Table 5.
Multivariate Analysis of Selected Individual Complications by Significant Risk Factors
RESULTS
Patient Characteristics
During the study period, 188 patients underwent pedicled TRAM flap breast reconstruction by the senior author (J.A.A.). Unilateral pedicled TRAM flaps were performed in 164 patients, of which 148 were ipsilateral and 16 were contralateral. Bilateral procedures were performed on 24 patients. Immediate reconstruction after mastectomy was performed in 177 patients and delayed in 11 patients.
The mean follow-up period was 36 months, with a range of 3 months to 12 years, and the average length of hospital stay was 4 days. Patient demographics are summarized in Table 1. The mean patient age was 48.8 years, with a range of 29–72. Average BMI was 25.2, with 52.1% of patients classified as normal weight, 36.7% overweight, and 11.2% obese. Active smokers comprised 3.2%, and 15.4% of patients were former smokers. One patient had a history of diabetes. A total of 43.6% of patients received chemotherapy, and 30.2% received radiation. Prior abdominal surgery was reported by 46.8% of patients.
Unilateral vs Bilateral Complications
Flap site complications occurred in 38 patients (20.2%) (Table 2); however, the majority of these were treated in the office, and only 6 patients (3.7%) required a return to the operating room for a flap site-related complication. Furthermore, all of these flap complications occurred in unilateral TRAM flap patients, with a rate of 23.2% in the unilateral group vs 0% in the bilateral group (P = 0.005). Forty-one complications occurred in 38 patients, as 3 patients experienced 2 flap complications each. There were no complete flap losses. Partial flap loss occurred in 16 unilateral patients (9.8%) and zero bilateral patients (P = 0.231). Nearly all of the partial flap losses involved only a small portion of the flap (less than 15%). Four closed on their own, 11 were revised and closed in the office, and 1 was revised in the operating room. Fat necrosis occurred in 9.1% of unilateral patients, with none in the bilateral group (P = 0.224). Breast infection, seroma, and hematoma occurred in 4.3%, 1.2%, and 0.6% of unilateral patients, respectively, and in no bilateral patients (P = 0.598, 1.000, and 1.000).
Of the 3 patients who experienced 2 flap complications each, one was overweight and had undergone postoperative radiation therapy. She developed a breast hematoma and fat necrosis. Another patient was an obese woman with a 20 pack-year smoking history who quit smoking 1 month before surgery, and she experienced infection at the flap site and partial flap loss. The third patient was overweight, an active smoker, and underwent postoperative chemotherapy. She developed an infection at the flap site and fat necrosis.
Donor site morbidity occurred in 9.8% of unilateral and 20.8% of bilateral patients (P = 0.155) (Table 3). As with flap site-related complications, the majority of these donor site complications were relatively minor and were treated in the office. Only 1 bilateral patient (4.2%) and 2 unilateral patients (1.2%) required a return to the operating room for donor site morbidity. The 23 donor site complications involved 21 patients (11.2%), as 2 patients had 2 donor site complications. Three patients developed abdominal hernias, with 1 occurring after unilateral (0.6%) and 2 occurring after bilateral TRAM flap procedures (8.3%, P = 0.043). One of these bilateral patients who developed a hernia was obese and a former smoker with a history of previous abdominal surgery. When this small hernia was pointed out to the patient by the surgeon, she said she had not known it was there and declined the surgeon’s recommendation to have it fixed as she said she had never noticed it and it was asymptomatic. The other bilateral patient was normal weight and underwent repair of an abdominal hernia approximately 2 years following her TRAM flap operation. The unilateral TRAM flap patient was an obese woman, with a history of previous abdominal surgery and chemotherapy, who underwent repair of a ventral hernia approximately 10 years following her TRAM flap operation. An abdominal wall bulge was detected in 1 unilateral patient (0.6%) and in no bilateral TRAM flap patients (P = 1.000).
Donor site infection occurred in 3 unilateral patients (1.8%) and none of the bilateral patients (P = 1.000). Skin loss was higher in the bilateral group, with a rate of 0.6% in unilateral vs 8.3% in bilateral patients (P = 0.043). No patients developed an abdominal seroma, although 1 patient (0.6%) had an abdominal hematoma. One unilateral (0.6%) and 1 bilateral (4.2%) patient underwent removal of a palpable mesh edge (P = 0.240). No patient required mesh removal for infection. Umbilical ischemia occurred in 5 unilateral patients (3.0%) and 1 bilateral patient (4.2%, P = 0.565). An umbilical cyst developed in 1 unilateral patient (0.6%). Two unilateral patients (1.2%) and 1 bilateral (4.2%) patient experienced persistent abdominal discomfort requiring referral for physical therapy (P = 0.338).
Risk Factor Analysis
Rates of specific complications were compared between patients of varying age, BMI, smoking status, history of abdominal surgery, radiotherapy status, and chemotherapy status. Initial analysis revealed that chemotherapy and radiation history were not independent in our patients (χ2, P < 0.0001). Because we did not have adequate sample sizes and power to include all patients in mutually exclusive and comprehensively exhaustive treatment groups, as would be required to accurately separate the effects of chemotherapy and radiation in logistic regression, we chose to categorize patients by the number of adjuvant treatments received. We defined adjuvant treatments as pre- or postoperative radiation, neoadjuvant, or postoperative chemotherapy (eg, a patient receiving neoadjuvant chemotherapy and postoperative radiation was categorized as having 2 adjuvant treatments). Initial analysis found that an increasing number of adjuvant treatments was a significant risk factor for complications, with an inflection point found at 2 treatments; therefore, for the purpose of analysis, we use “2 or more adjuvant therapies” as a risk factor in our model.
A history of 2 or more adjuvant therapies for breast cancer was independently associated with overall flap site complications [odds ratio (OR), 3.67; P = 0.002] (Table 4). Of the specific flap site complications, partial flap loss was strongly associated with a history of 2 or more adjuvant therapies (OR, 7.65; P < 0.001) and obesity (OR, 4.211; P = 0.03) (Table 5). The odds of fat necrosis were greater in patients who were current or former smokers (OR, 3.28; P = 0.035). Age over 60 and prior abdominal procedures were not associated with a higher rate of flap site complications.
Obesity was significantly associated with donor site complications independent of other risk factor contributions (OR, 6.12; P = 0.001) (Table 4). A history of former or active smoking (P = 0.823), 2 or more adjuvant therapies (0.171), age over 60 (P = 0.580), and prior abdominal surgery (P = 0.101) were not associated with a higher rate of donor site complications.
Obesity had the greatest association with overall complications (OR, 4.67; P = 0.003) (Table 4). The rate of overall complications was higher in those who were former or active smokers (42.9%) compared to those who never smoked (26.1%), although the difference was not statistically significant (P = 0.113). Cancer treatment with 2 or more adjuvant therapies (OR, 2.52; P = 0.02) was independently associated with developing an overall complication. Overall morbidity was unaffected by age or a history of abdominal surgery.
DISCUSSION
Since the introduction of the pedicled TRAM flap procedure in 1982,2 much of the literature has focused on the procedure’s abdominal morbidity, particularly abdominal hernia and bulge formation. Very few studies comprehensively examine both the donor site and the flap site morbidity resulting from this procedure. Our study serves as a comprehensive assessment of complications in a large series of unilateral and bilateral pedicled TRAM flap procedures. Although outcomes data from the pedicled TRAM flap procedure showing low rates of abdominal morbidity have been previously reported, the use of the pedicled TRAM flap is still questioned; therefore, we believe it is important to present an updated outcomes study of patients undergoing this procedure to document the evidence for the safety of the pedicled TRAM flap.
Some surgeons have particularly questioned whether or not the bilateral pedicled TRAM flap remains a good reconstruction option for patients undergoing bilateral mastectomies. In our 24 bilateral patients, there were no intensive care unit stays, no blood transfusions, no partial or complete flap losses, and prolonged operating room times were avoided. Furthermore, only 1 bilateral patient (4.2%) returned to the operating room secondary to morbidity. We thus strongly believe that the data presented here do indeed document that bilateral pedicled TRAM flaps can be safely performed.
In our study, complication rates were relatively low in both unilateral and bilateral TRAM flap patients. Most importantly, when we looked at the more significant complications, those that required a return to the operating room, only 4.3% of unilateral TRAM flap patients (7/164) and only 4.2% of bilateral TRAM flap patients (1/24) required a return to the operating room when all types of morbidity were combined. Unilateral patients experienced more overall flap complications than bilateral patients (23.2% vs 0%), likely because unilateral flaps often included zone 4 with its associated decreased blood supply, whereas bilateral flaps included only tissue on the same side as the muscle pedicle.
Our rate of flap site complications of 20.2% in the total series is lower than the rates reported by Ducic et al,4 who found a 43.5% of flap complications after pedicled TRAM flaps. This may be attributed to our lower proportion of obese patients and active smokers, as these factors have been previously shown to increase the risk of flap complications after pedicled TRAM flap procedures.4,8,9 Historically, fat necrosis is the most commonly reported morbidity after pedicled TRAM flap reconstruction.10 In our study, fat necrosis occurred in 9.1% of unilateral patients and 0% of bilateral patients, values consistent with the literature.4–6,10
A history of treatment with 2 or more adjuvant therapies was significantly associated with overall flap morbidity in our study. Patients requiring at least 2 adjuvant treatments were nearly 4 times more likely to experience an overall flap complication and nearly 8 times more likely to experience partial flap loss. Considering the timing of postoperative radiation and chemotherapy in relation to surgery, this association is unlikely to be solely due to the treatments themselves. A possible explanation for this finding is the greater malignant burden, and therefore its effect on vascular physiology, in patients requiring at least 2 forms of adjuvant treatment.11
Although obesity and former or active smoking were not identified as risk factors for overall flap site morbidity, analysis of individual flap complications revealed that obesity was associated with partial flap loss, and a history of active or former smoking was associated with fat necrosis. When active smokers were excluded from this group, former smoking was not associated with fat necrosis. This likely indicates that the risk is attributable to the active smoking component; however, our sample size of active smokers (n = 6) was too low to investigate alone.
Our overall donor site complication rate was 11.2%, which compares favorably to previously reported donor site complication rates after free flap reconstruction.12 Rates of hernia and abdominal bulge development after pedicled TRAM flaps have varied in the literature, with reported hernia rates ranging from 0% to 16% and abdominal bulge rates from 3.6% to 82%.3,6,13,14 Our rates of abdominal hernia (1.6%) and bulge (0.5%) formation compare favorably with those reported after pedicled TRAM flap and free flap reconstruction.5,6,15,16 Two patients experiencing a hernia in our series of 188 patients underwent successful hernia repair and have had no secondary abdominal wall complications. We attribute these low rates to the use of an onlay polypropylene mesh to reinforce abdominal repairs. As no patient required mesh removal for infection, we believe that the use of mesh is well worth the small additional operating room time required to place it in all patients.
Obesity showed the greatest association with donor site morbidity, a finding consistent with the literature.8,17 Active smoking has been previously identified as a risk factor for donor site complications after pedicled TRAM flap reconstruction.9 In our series, patients who were former or active smokers had a higher rate of donor site complications compared to those who never smoked; however, this effect did not reach statistical significance.
Although our series investigates overall pedicled TRAM flap complications in a large number of consecutive patients, it also has limitations. Although all of our patients are offered the full range of reconstructive options, patients who are obese and active smokers are informed of their increased risk of complications after pedicled TRAM flaps. This may be a source of selection bias in our study. Additionally, before writing this article, we carefully reviewed the literature and found a multitude of definitions for fat necrosis. We chose our definition because it used an objective criterion that can be compared between different series, but there are certainly other valid definitions that have been selected by previous authors. Lastly, this is not a prospective, randomized, controlled study allowing for direct comparison between pedicled TRAM flaps and alternative methods of autologous breast reconstruction.
CONCLUSION
Despite continued concern regarding morbidity resulting from the pedicled TRAM flap, overall complication rates associated with both unilateral and bilateral pedicled TRAM flaps in this series were low and well within complication rates observed for other types of breast reconstruction using abdominal tissue. In properly selected patients, this procedure thus continues to be an excellent option for breast reconstruction after mastectomy.
Jeffrey A. Ascherman, MD
Division of Plastic Surgery
Columbia University Medical Center
161 Fort Washington Avenue, Suite 509
New York, NY 10032
E-mail: jaa7@columbia.edu.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Garvey PB, Buchel EW, Pockaj BA, et al. DIEP and pedicled TRAM flaps: a comparison of outcomes. Plast Reconstr Surg. 2006;117:1711–1719. doi: 10.1097/01.prs.0000210679.77449.7d. discussion 1720–1721. [DOI] [PubMed] [Google Scholar]
- 2.Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982;69:216–225. doi: 10.1097/00006534-198202000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109:2265–2274. doi: 10.1097/00006534-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Ducic I, Spear SL, Cuoco F, et al. Safety and risk factors for breast reconstruction with pedicled transverse rectus abdominis musculocutaneous flaps: a 10-year analysis. Ann Plast Surg. 2005;55:559–564. doi: 10.1097/01.sap.0000184463.90172.04. [DOI] [PubMed] [Google Scholar]
- 5.Chun YS, Sinha I, Turko A, et al. Outcomes and patient satisfaction following breast reconstruction with bilateral pedicled TRAM flaps in 105 consecutive patients. Plast Reconstr Surg. 2010;125:1–9. doi: 10.1097/PRS.0b013e3181c2a620. [DOI] [PubMed] [Google Scholar]
- 6.Ascherman JA, Seruya M, Bartsich SA. Abdominal wall morbidity following unilateral and bilateral breast reconstruction with pedicled TRAM flaps: an outcomes analysis of 117 consecutive patients. Plast Reconstr Surg. 2008;121:1–8. doi: 10.1097/01.prs.0000295378.43033.c4. [DOI] [PubMed] [Google Scholar]
- 7.Bartsich S, Ascherman JA. Posterior dissection of the rectus abdominis muscle during TRAM flap harvest for the preservation of medial row perforators. Plast Reconstr Surg. 2010;126:193e–195e. doi: 10.1097/PRS.0b013e3181ea928f. [DOI] [PubMed] [Google Scholar]
- 8.Spear SL, Ducic I, Cuoco F, et al. Effect of obesity on flap and donor-site complications in pedicled TRAM flap breast reconstruction. Plast Reconstr Surg. 2007;119:788–795. doi: 10.1097/01.prs.0000252003.14537.d2. [DOI] [PubMed] [Google Scholar]
- 9.Spear SL, Ducic I, Cuoco F, et al. The effect of smoking on flap and donor-site complications in pedicled TRAM breast reconstruction. Plast Reconstr Surg. 2005;116:1873–1880. doi: 10.1097/01.prs.0000191200.81375.8c. [DOI] [PubMed] [Google Scholar]
- 10.Buck DW, II, Fine NA. The pedicled transverse rectus abdominis myocutaneous flap: indications, techniques, and outcomes. Plast Reconstr Surg. 2009;124:1047–1054. doi: 10.1097/PRS.0b013e3181b457b2. [DOI] [PubMed] [Google Scholar]
- 11.Mandalà M, Tondini C. Adjuvant therapy in breast cancer and venous thromboembolism. Thromb Res. 2012;130(Suppl 1):S66–S70. doi: 10.1016/j.thromres.2012.08.280. [DOI] [PubMed] [Google Scholar]
- 12.Vyas RM, Dickinson BP, Fastekjian JH, et al. Risk factors for abdominal donor-site morbidity in free flap breast reconstruction. Plast Reconstr Surg. 2008;121:1519–1526. doi: 10.1097/PRS.0b013e31816b1458. [DOI] [PubMed] [Google Scholar]
- 13.Mizgala CL, Hartrampf CR, Jr, Bennett GK. Assessment of the abdominal wall after pedicled TRAM flap surgery: 5- to 7-year follow-up of 150 consecutive patients. Plast Reconstr Surg. 1994;93:988–1002. doi: 10.1097/00006534-199404001-00013. discussion 1003–1004. [DOI] [PubMed] [Google Scholar]
- 14.Fitoussi A, Le Taillandier M, Biffaud JC, et al. [Functional evaluation of the abdominal wall after raising a rectus abdominis myocutaneous flap]. Ann Chir Plast Esthet. 1997;42:138–146. [PubMed] [Google Scholar]
- 15.Suominen S, Asko-Seljavaara S, von Smitten K, et al. Sequelae in the abdominal wall after pedicled or free TRAM flap surgery. Ann Plast Surg. 1996;36:629–636. doi: 10.1097/00000637-199606000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Hamdi M, Weiler-Mithoff EM, Webster MH. Deep inferior epigastric perforator flap in breast reconstruction: experience with the first 50 flaps. Plast Reconstr Surg. 1999;103:86–95. doi: 10.1097/00006534-199901000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Rossetto LA, Abla LE, Vidal R, et al. Factors associated with hernia and bulge formation at the donor site of the pedicled TRAM flap. Eur J Plast Surg. 2010;33:203–208. doi: 10.1007/s00238-010-0418-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


