Abstract
Purpose
The introduction of volar plating has dramatically changed the operative treatment of distal radius fractures (DRFs). However, the factors that influence the adoption of new techniques remain unclear. Therefore, the purpose of this study is to determine the extent to which surgeon age influences treatment patterns for DRFs. We hypothesize that younger surgeons perform ORIF for DRFs among elderly individuals more frequently than older surgeons, who employ a wider range of treatment modalities.
Methods
We identified 61,314 Medicare beneficiaries who suffered DRFs and the 12,823 surgeons who performed ORIF, external fixation, pinning or closed reduction on them during the year of 2007. We examined the effect of surgeon age on DRF treatment pattern, controlling for patient characteristics and other surgeon factors using multinomial logistic regression. We then stratified our analysis by ASSH membership to more closely examine the influence of surgeon specialization on the association between surgeon age and DRF treatment.
Results
Surgeons aged 40 and younger were more likely to perform ORIF and less likely to choose external fixation and percutaneous pinning to treat DRFs compared with older surgeons. Surgeon specialization mitigated this relationship, and ASSH members were more likely to choose ORIF compared with non-members. However, surgeon age remained a significant predictor of treatment choice after controlling for other factors and surgeon specialization.
Discussion
Younger surgeons are more likely to perform ORIF for DRFs among Medicare beneficiaries over 65 years old. Given the lack of evidence supporting any single treatment option for DRF, understanding the factors that drive dissemination of operative techniques may provide insight into treatment disparities within the Medicare population.
Keywords: Distal radius fractures, Medicare, physical attributes, practice patterns
Introduction
Despite the prevalence of distal radius fractures in the United States, the optimal treatment for unstable fractures remains unclear. (1, 2) Previous research demonstrates that variation in treatment is related to patient attributes, such as socioeconomic status, and surgeon characteristics, such as specialization in hand surgery. (2-4) Nonetheless, technologic advances in fracture fixation develop at a rapid pace, and it is challenging for surgeons to discern the comparative effectiveness of any single treatment strategy. Understanding the surgeon-related factors that drive variation in practice can provide insight into how new techniques are disseminated into clinical practice and adopted by surgeons into their treatment algorithm.
Physician age is correlated with practice patterns and treatment outcomes for a variety of conditions. (6-13) For example, in a national study, younger physicians are more aggressive in choosing operative treatment in treating orthopedic fractures compared with older surgeons. (14) Younger surgeons may also be more likely to integrate technologic advances into practice. For example, younger surgeons use laparoscopic techniques more frequently compared with older surgeons, possibly due to differences in exposure to these techniques during training. (15) The effect of age on treatment patterns and performance is not linear, however, and lack of experience and surgeon youth is also correlated with poorer outcomes.(16, 17) Although these age-related differences have been described among a variety of fields, the effect of surgeon age on the management of orthopedic fractures has not been described. For hand surgery, training pathways are variable, and many different types of providers may perform hand surgery. For example, orthopedic, plastic, and general surgeons may perform hand surgery procedures. The training and scope of practice for each of these surgeons can vary widely, and are represented by different professional organizations. For many upper extremity procedures, each patient and injury pattern is unique, and few procedures have a dogmatic, “cook-book” approach.
The purpose of this study is to examine the effect of surgeon age on treatment patterns following distal radius fractures among a cohort of Medicare beneficiaries in 2007. We hypothesize that younger surgeons more frequently perform ORIF for distal radius fractures, whereas older surgeons more frequently utilize alternative strategies, such as percutaneous pinning, external fixation, or closed reduction and immobilization.
Methods
Patient Sample
Using Medicare MedPAR, Carrier, and Outpatient files, we identified all beneficiaries diagnosed in 2007 with fracture of the distal radius with or without an associated ulna fracture who underwent open reduction and internal fixation (ORIF), external fixation, percutaneous pinning, closed reduction and cast immobilization or splinting within two weeks of diagnosis. Only patients who continuously enrolled in Medicare Part A and B were included in the study cohort. Patients who were younger than 65, enrolled in a Health Maintenance Organization (HMO) plan, or who had a diagnosis of bone cancer were excluded from the study sample. Owing to potential differences in fracture severity, we excluded all the patients whose most invasive fracture treatment was cast immobilization or splinting without closed reduction. (Figure 1) We obtained approval from Institutional Review Board in our University for conducting the study before access to Medicare data.
Figure 1.
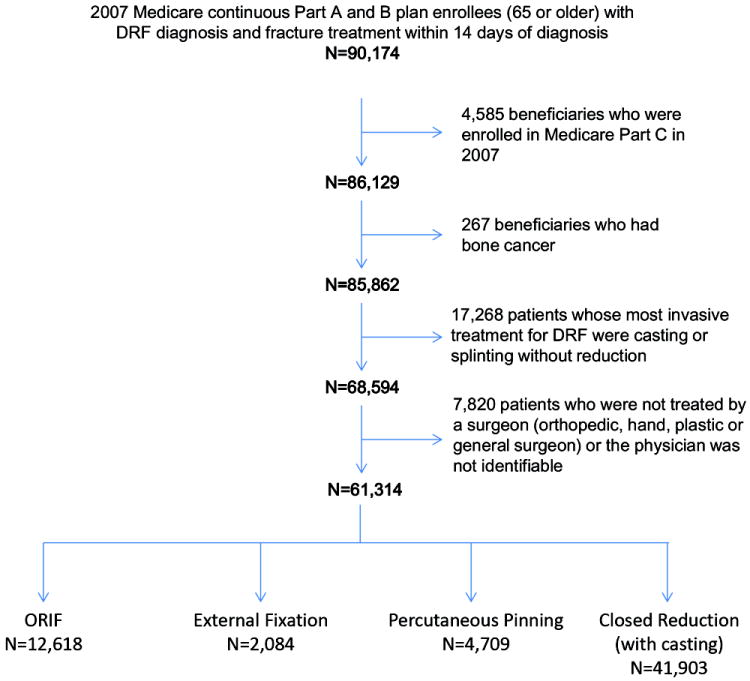
Cohort flowchart and DRF treatment in the study cohort
We obtained demographic information from the Medicare Denominator File including age, race, gender, and socioeconomic status (SES). Nine-digit residence zip code was used to construct SES according to 2000 US Census data on income, education and occupation based on previously described methods. (18) We examined comorbid conditions using International Classification of Diseases, Ninth Revision (ICD-9) codes in Elixhauser’s index through the year of 2007 for each patient drawn from the MedPAR, Outpatient, and Carrier files. (19) Elixhauser’s index is a list of thirty comorbidity conditions associated with increased length of hospital stay, charges, and overall mortality, such as congestive heart failure, chronic pulmonary disease, hypertension and diabetes. Finally, we examined concomitant injuries occurring on the date of DRF diagnosis including other fractures, neurologic condition (traumatic brain injury, subdural hematoma, and epidural hematoma), solid organ injury (liver laceration/contusion, spleen laceration/contusion, bowel injury, diaphragmatic rupture, and kidney laceration/contusion) and other injuries (pneumothorax, hemothorax).
Surgeon Sample
We identified physicians managing each patient from the Medicare Outpatient and Carrier files using Unique Physician Identification Numbers (UPIN). We designated the physician linked with the most invasive treatment within 2 weeks of DRF diagnosis as the surgeon for each patient. Surgeon age in 2007 was obtained by linking UPIN to the American Medical Association Physician Masterfile, a national registry of physicians practicing in the United States. (20) The age of surgeons was categorized as less than 40 years of age, 41 to 50 years, 51 to 60 years, and 60 years and older, based on prior work. (21)
In order to examine the effect of surgeon specialization on the relationship between surgeon age and DRF treatment, we examined surgeon membership in the American Society for Surgery of the Hand (ASSH) by matching UPIN to active members of ASSH during 2007. Only patients who were treated by a surgeon with UPIN entered the final study cohort. (Figure 1) Finally, we included the number of DRF patients treated during the year of 2007 by each surgeon as a measure of surgeon volume. We categorized surgeon volume by quintiles, and included this variable in our analysis based on previous studies demonstrating the interaction between surgeon age and operative volume.(21)
Statistical analysis
We used multinomial logistic regression in order to examine the effect of surgeon age on DRF treatment, with DRF treatments (ORIF, external fixation, percutaneous pinning and closed reduction) as the dependent variable and surgeon age as the primary predictor. In the model, closed reduction was set as the reference level for the outcome and the age of 41-50 years old was used as the reference group for surgeon age. To control the effect of other surgeon factors (ASSH membership and DRF patient volume) and patient characteristics (patient age, gender, race, SES, comorbidity and concomitant injuries) that potentially can influence DRF treatment pattern, we added all these covariates into our model for adjustment.(4)
We then included surgeon ASSH membership into each model in order to examine the effect of surgeon specialization on the relationship between surgeon age and DRF treatment. Based on statistical significance of this interaction term, we further stratified our multinomial logistic model by ASSH membership. We calculated odds ratios of ORIF performance among different surgeon age groups (40 and younger, 51 to 60 and 61 and older vs. 41 to 50, respectively) for ASSH members and non-members separately and then, compared the odds ratios between ASSH members and non-members to present the modified effect of surgeon age by ASSH membership.
Results
DRF treatment
In this cohort, 61,314 DRF patients were treated by 12,823 surgeons. The characteristics of the patient and surgeon sample are detailed in Table 1 and Table 2. Table 3 displays the influence of surgeon attributes on DRF treatment patterns, adjusted for patient age, gender, race, SES, comorbidity and concurrent injury. Adjusted rates DRF treatment by surgeon age were calculated and displayed in Figure 2.
Table 1. Characteristics of Medicare beneficiaries suffered distal radius fracture in 2007.
| Characteristics | Number of Individuals | Percent |
|---|---|---|
| Total | 61,314 | 100% |
| Age | ||
| 65-69 | 11,216 | 18.3% |
| 70-74 | 11,596 | 18.9% |
| 75-79 | 13,257 | 21.6% |
| 80-84 | 12,825 | 20.9% |
| 85 and older | 12,420 | 20.3% |
| Sex | ||
| Male | 8,729 | 14.2% |
| Female | 52,585 | 85.8% |
| Race | ||
| White | 58,893 | 96.1% |
| Black | 1,205 | 2.0% |
| Other | 1,165 | 1.9% |
| SES | ||
| Low | 10,257 | 16.7% |
| Medium | 16,723 | 27.3% |
| High | 32,372 | 52.8% |
| Missing | 1,962 | 3.2% |
| Comorbidity | ||
| 0-1 | 17,407 | 28.4% |
| 2-3 | 22,401 | 36.5% |
| >=4 | 21,506 | 35.1% |
| Concurrent Injury | ||
| None | 42,937 | 70.0% |
| 1 | 14,750 | 24.1% |
| >=2 | 3,627 | 5.9% |
Table 2. Characteristics of the surgeons who provided DRF treatments on the study cohort.
| Characteristics | Number of Individuals | Percent |
|---|---|---|
| Total | 12,823 | 100% |
| Surgeon Age | ||
| 40 and younger | 2,652 | 20.8% |
| 41 to 50 | 4,338 | 34.0% |
| 51 to 60 | 3,793 | 29.7% |
| 61 and older | 1,981 | 15.5% |
| ASSH Membership | ||
| No | 11,629 | 90.9% |
| Yes | 1,194 | 9.1% |
| DRF Patient Volume | ||
| 1-3 patients | 5,626 | 43.9% |
| 4-5 patients | 2,439 | 19.0% |
| 6-8 patients | 2,351 | 18.3% |
| 9-12 patients | 1,456 | 11.4% |
| 13 and more patients | 951 | 7.4% |
Table 3. Adjusted odds ratios of DRF treatment by surgeon characteristics. ¥.
| Adjusted Odds Ratios of Distal Radius Fracture Treatment | |||
|---|---|---|---|
| Internal Fixation | External Fixation | Percutaneous Pinning | |
| Surgeon Age | |||
| 41 to 50 | 1 | 1 | 1 |
| 40 and younger | 1.36 (1.29, 1.43)* | 0.58 (0.51, 0.68)* | 0.70 (0.64, 0.77)* |
| 51 to 60 | 0.72 (0.68, 0.76)* | 1.02 (0.92, 1.14) | 0.97 (0.90, 1.04) |
| 61 and older | 0.62 (0.57, 0.67)* | 1.00 (0.87, 1.16) | 0.92 (0.83, 1.01) |
| ASSH Membership | |||
| No | 1 | 1 | 1 |
| Yes | 2.73 (2.59, 2.89)* | 0.50 (0.41, 0.61)* | 0.76 (0.68, 0.86)* |
| DRF Patient Volume | |||
| 1-3 patients | 1 | 1 | 1 |
| 4-5 patients | 1.12 (1.03, 1.21)* | 1.08 (0.93, 1.27) | 0.98 (0.88, 1.08) |
| 6-8 patients | 1.12 (1.04, 1.20)* | 0.99 (0.86, 1.14) | 0.90 (0.81, 0.98)* |
| 9-12 patients | 1.04 (0.96, 1.11) | 1.10 (0.95, 1.27) | 0.73 (0.66, 0.81)* |
| 13 and more patients | 1.12 (1.05, 1.21)* | 1.03 (0.89, 1.19) | 0.79 (0.72, 0.88)* |
P value < 0.05.
Odds ratios were calculated controlling for surgeon self-reported specialty, patient age, gender, race, SES, comorbidity and concurrent injury.
Figure 2.
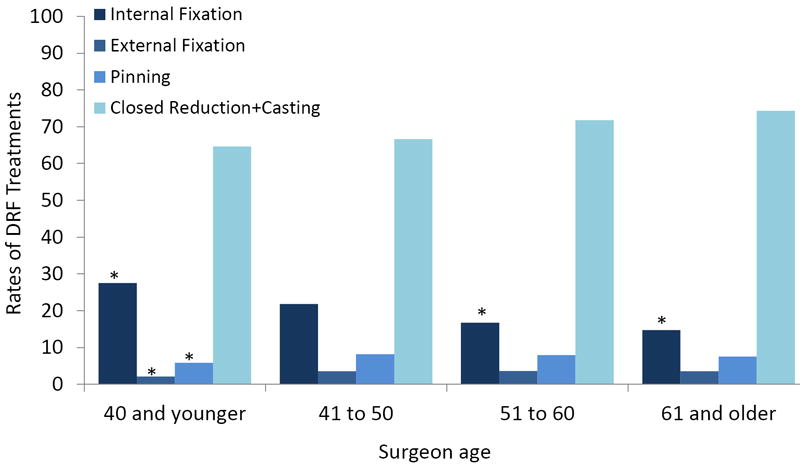
Adjusted rate of DRF treatment on patients by surgeon age among a cohort of Medicare beneficiaries in 2007. ¥
*: P value <0.001
¥: The rates are calculated controlling for surgeon ASSH membership, DRF volume and patient age, gender, race, SES, comorbidity and concurrent injury.
After adjusting all other surgeon and patient characteristics, surgeon age was significantly correlated with surgical techniques used for distal radius fractures. Younger surgeons were more likely to perform ORIF than older surgeons. (Table 3) Furthermore, the rates of ORIF utilization linearly decreased with the rising of surgeon age. (Figure 2) As for other surgical techniques, the youngest surgeon group (surgeons who were 40 or younger) performed significantly less external fixation and percutaneous pinning compared to surgeons in any older age groups. (Figure 2)
Other surgeon factors such as ASSH membership and DRF patient volume during the year also were correlated with fracture treatment. ASSH members were 2.73 times more likely to perform ORIF compared to non-members, and surgeons with higher patient volume had slightly higher ORIF rate than surgeons treated only 1 to 3 DRF patients during the year. As for other surgical techniques, ASSH members performed significantly less external fixation and percutaneous pinning than non-members, and the rate of percutaneous pinning utilization decreased with increasing surgeon volume. (Table 3)
ASSH members vs. non-members
Figure 3 illustrates the relationship between surgeon age and DRF treatment, controlling for patient characteristics and stratified by ASSH membership, and differences in DRF treatment by surgeon age persist in both ASSH members and non-members. However, ASSH membership significantly modified the relationship between surgeon age and DRF treatment by substantially reducing the effect of surgeon age on ORIF performance. (Table 4) For example, among non-members, surgeons 40 and younger were 1.41 times (p<0.05) more likely to perform ORIF compared to the reference group (surgeons aged 41 to 50 years), compared with 1.19 among ASSH members. (Table 4)
Figure 3.
Adjusted rate of DRF treatment on patients by surgeon age among Medicare beneficiaries in 2007, stratified by ASSH membership. ¥
*: P<0.05
**: p<0.001
¥ The rates are calculated controlling for surgeon ASSH membership, DRF volume and patient age, gender, race, SES, comorbidity and concurrent injury.
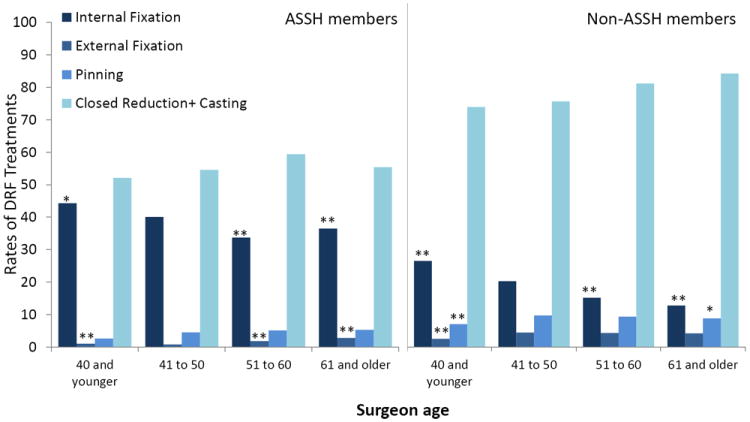
Table 4. Comparison of adjusted odds ratios of ORIF by surgeon age between ASSH members and non-members. ¥.
| Surgeon Age | Adjusted Odds Ratios of internal fixation | P values | |
|---|---|---|---|
| ASSH members | Non-ASSH members | ||
| 41 to 50 | 1 | 1 | - |
| 40 and younger | 1.19 (1.06,1.33) | 1.41 (1.33,1.50) | <0.001 |
| 51 to 60 | 0.76 (0.68, 0.87) | 0.72 (0.67,0.76) | 0.91 |
| 61 and older | 0.86 (0.70,1.04) | 0.58 (0.54,0.64) | <0.001 |
Odds ratios were calculated from multinomial logistic regression model controlling for surgeon self-reported specialty, patient age, gender, race, SES, comorbidity and concurrent injury.
Finally, we performed a subgroup analysis of patients with 4 or more comorbid conditions in order to further assess treatment patterns by surgeon age (Table 5). In this subgroup analysis, the effect of surgeon age and ORIF persisted, and younger surgeons were more likely to perform ORIF even among patients with numerous comorbid conditions.
Table 5. Adjusted odds ratios of DRF treatment by surgeon age among patients with four or more than four comorbid conditions. ¥.
| Adjusted Odds Ratios of Distal Radius Fracture Treatment | |||
|---|---|---|---|
| Internal Fixation | External Fixation | Percutaneous Pinning | |
| Surgeon Age | |||
| 41 to 50 | 1 | 1 | 1 |
| 40 and younger | 1.38(1.26, 1.52)* | 0.68 (0.55, 0.86)* | 0.77 (0.66, 0.89)* |
| 51 to 60 | 0.73 (0.66, 0.80)* | 0.99 (0.83, 1.19) | 0.96 (0.85, 1.09) |
| 61 and older | 0.63 (0.55, 0.72)* | 0.95 (0.75, 1.22) | 0.99 (0.84, 1.16) |
P value < 0.05.
Odds ratios were calculated controlling for surgeon self-reported specialty, patient age, gender, race, SES, comorbidity and concurrent injury.
Discussion
In this cohort of Medicare beneficiaries who suffered distal radius fractures, closed reduction with casting remained the most common treatment. Younger surgeons were more likely to perform ORIF for DRF, whereas older surgeons more frequently used percutaneous pinning, external fixation, or closed reduction and casting. Surgeon specialization mitigated the effect of surgeon age on treatment, and ASSH members were more likely to perform ORIF. After adjusting for specialization, younger surgeons remained more likely to perform ORIF compared with older surgeons, however, ASSH membership modified the age-related differences, and the difference in ORIF utilization rates among surgeons with different age were less pronounced among ASSH members.
Although our study does not address potential mechanisms of the relationship of surgeon age on treatment patterns, several reasons may explain this effect. In recent years, the advent of volar plates with locking screws has heightened popularity for internal fixation. (22-24) Changing practice patterns may influence the techniques that surgical trainees are exposed to, and recent graduates may have greater familiarity with internal fixation. (25) (14) In our study, ASSH membership modified these age-related differences, and the difference in ORIF utilization rates among surgeons with different age were weakened among ASSH members. Specialized surgeons may have greater exposure to evidence regarding the relative effectiveness of treatment strategies for DRFs. They may also have increased exposure to new fixation techniques due to differences in marketing strategies by biomedical companies toward subspecialty groups. Despite these theories, a deeper understanding of the mechanisms that underlie how surgeons adopt new techniques into practice must await future studies.
This study has several notable limitations. First, this study is cross-sectional in nature, and we cannot comment on the causality of the associations we observed. In addition, our findings are drawn from administrative data, which is limited in its ability to capture fracture severity. (1,2,4) However, we expect that fracture severity would remain evenly distributed among surgeons of different ages, and would not likely alter the associations that we observed. Furthermore, DRF patient volume of surgeons during the study period only consisted of Medicare beneficiaries, which may underestimate practice volume. Finally, Medicare claims designated only a single primary specialty, and it is difficult to ascertain surgeons truly specialized in hand surgery from CMS data alone. However, we have matched each surgeon with records indicating ASSH membership in order to identify those surgeons who are specialized in hand surgery in order to better examine its effect on surgeon age and treatment patterns.
Despite these limitations, this study has important implications for surgeons in practice. First, given the popularity of internal fixation techniques, particularly volar plating, younger surgeons may lack adequate exposure to other treatment strategies, and may be less inclined to utilize these in practice. Although there are distinct advantages to internal fixation, there are specific scenarios in which external fixation or percutaneous pinning is desirable, and knowledge of alternative techniques is beneficial.(26) Therefore, ensuring broad exposure during training is critical, and surgeons early in practice may benefit from continuing medical education courses regarding fracture management. Additionally, it is important to consider the ways in which individuals acquire new information and skills, which changes with the aging process. For example, compared to younger surgeons, older individuals retain information more efficiently with written material than video and computerized presentations, and are more adept at self-paced and self-directed learning than proctored learning. (27-30) Designing information to introduce new surgical techniques and concepts should consider these phenomena in order to provide the most efficient strategy to education surgeons. Finally, it is important to ensure that new evidence regarding the comparative effectiveness of DRFs treatment is available to all surgeons who are choosing a treatment plan for their patients.
Surgeon age is correlated with DRF treatment, and older surgeons are more likely to utilize a broader array of treatment strategies. Future, population-based studies that examine DRF outcomes by surgical option and the adoption of surgical techniques into practice by surgeon attributes will provide insight into the reasons for the wide variation in care of these common fractures.
Acknowledgments
Conflict of interest statement:
The institution of the authors has received funding from:
R01 #AR062066. National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Diseases (to Dr. Chung)
2012 Clinical Research Grant funded by the American Foundation for Surgery of the Hand (to Dr. Waljee)
K24 #AR053120. The National Institute of Arthritis and Musculoskeletal and Skin Diseases (To Dr. Chung)
Footnotes
Level of Evidence: level III – Therapeutic
Ethical Review Committee Statement:
This study is approved by the Institutional Review Board [HUM00061645]. Current IRB Approval period is 10/16/2012 to 10/15/2013. A copy of approval letter will be uploaded with the manuscript.
Statement of Location:
All the work has been done at University of Michigan, North Campus Research Complex.
Contributor Information
Lin Zhong, Email: zhonglin@med.umich.edu.
Melissa Shauver, Email: mshauver@med.umich.edu.
Kevin C. Chung, Email: kecchung@med.umich.edu.
References
- 1.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91(8):1868–1873. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung KC, Shauver MJ, Yin H, Kim HM, et al. Variations in the use of internal fixation for distal radial fracture in the United States medicare population. J Bone Joint Surg Am. 2011;93(23):2154–2162. doi: 10.2106/JBJS.J.012802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fanuele J, Koval KJ, Lurie J, et al. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg Am. 2009;91(6):1313–1319. doi: 10.2106/JBJS.H.00448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung KC, Shauver MJ, Yin H. The relationship between ASSH membership and the treatment of distal radius fracture in the United States Medicare population. The Journal of hand surgery. 2011;36(8):1288–1293. doi: 10.1016/j.jhsa.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 5.Bjork B, Roos A, Lauri M. Scientific journal pubishing: yearly volume and open access availability. Information Research. 2009;14(1) [Google Scholar]
- 6.Ayanian JZ, Hauptman PJ, Guadagnoli E, et al. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. New England Journal of Medicine. 1994;331(17):1136–1142. doi: 10.1056/NEJM199410273311707. [DOI] [PubMed] [Google Scholar]
- 7.Salem-Schatz SR, Avorn J, Soumerai SB. Influence of clinical knowledge, organizational context, and practice style on transfusion decision making. JAMA: the journal of the American Medical Association. 1990;264(4):476–483. [PubMed] [Google Scholar]
- 8.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Annals of internal medicine. 2005 Feb 15;142(4):260–273. doi: 10.7326/0003-4819-142-4-200502150-00008. [DOI] [PubMed] [Google Scholar]
- 9.Beaulieu MD, Blais R, Jacques A, et al. Are patients suffering from stable angina receiving optimal medical treatment? Qjm. 2001;94(6):301–308. doi: 10.1093/qjmed/94.6.301. [DOI] [PubMed] [Google Scholar]
- 10.Stolley PD, Becker MH, Lasagna L, McEvilla JD, Sloane LM. The relationship between physician characteristics and prescribing appropriateness. Medical care. 1972;10(1):17–28. doi: 10.1097/00005650-197201000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Hartz AJ, Kuhn EM, Pulido J. Prestige of training programs and experience of bypass surgeons as factors in adjusted patient mortality rates. Medical care. 1999;37(1):93. doi: 10.1097/00005650-199901000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Ramsey PG, Carline JD, Inui TS, et al. Changes over time in the knowledge base of practicing internists. JAMA : the journal of the American Medical Association. 1991 Aug 28;266(8):1103–1107. [PubMed] [Google Scholar]
- 13.Cruft GE, Humphreys JW, Jr, Hermann RE, et al. Recertification in surgery, 1980. Archives of Surgery. 1981;116(8):1093. doi: 10.1001/archsurg.1981.01380200089020. [DOI] [PubMed] [Google Scholar]
- 14.Ansari U, Adie S, Harris IA, Naylor JM. Practice variation in common fracture presentations: a survey of orthopaedic surgeons. Injury. 2011 Apr;42(4):403–407. doi: 10.1016/j.injury.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Moloo H, Haggar F, Martel G, et al. The adoption of laparoscopic colorectal surgery: a national survey of general surgeons. Can J Surg. 2009 Dec;52(6):455–462. [PMC free article] [PubMed] [Google Scholar]
- 16.Prystowsky JB. Are young surgeons competent to perform alimentary tract surgery? Arch Surg. 2005 May;140(5):495–500. doi: 10.1001/archsurg.140.5.495. discussion 500-492. [DOI] [PubMed] [Google Scholar]
- 17.Prystowsky JB, Bordage G, Feinglass JM. Patient outcomes for segmental colon resection according to surgeon’s training, certification, and experience. Surgery. 2002 Oct;132(4):663–670. doi: 10.1067/msy.2002.127550. discussion 670-662. [DOI] [PubMed] [Google Scholar]
- 18.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001 Jul 12;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 19.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Survey AMA, Resources D. Physician characteristics and Distribution in the US: Survey & Data Resources. American Medical Association; 2010. [Google Scholar]
- 21.Waljee JF, Greenfield LJ, Dimick JB, et al. Surgeon age and operative mortality in the United States. Annals of surgery. 2006;244(3):353–362. doi: 10.1097/01.sla.0000234803.11991.6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004 Jan;29(1):96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 23.Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003;27(1):1–6. doi: 10.1007/s00264-002-0393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002;27(2):205–215. doi: 10.1053/jhsu.2002.32081. [DOI] [PubMed] [Google Scholar]
- 25.Blasier RB. The problem of the aging surgeon: when surgeon age becomes a surgical risk factor. Clinical Orthopaedics and Related Research®. 2009;467(2):402–411. doi: 10.1007/s11999-008-0587-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Margaliot Z, Haase SC, Kotsis SV, et al. A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J Hand Surg Am. 2005 Nov;30(6):1185–1199. doi: 10.1016/j.jhsa.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Ackerman PL, Beier ME, Boyle MO. Working memory and intelligence: the same or different constructs? Psychol Bull. 2005;131(1):30–60. doi: 10.1037/0033-2909.131.1.30. [DOI] [PubMed] [Google Scholar]
- 28.Masunaga H, Horn J. Expertise and age-related changes in components of intelligence. Psychology and aging. 2001;16(2):293–311. [PubMed] [Google Scholar]
- 29.Radvansky GA, Copeland DE. Working memory and situation model updating. Mem Cognit. 2001;29(8):1073–1080. doi: 10.3758/bf03206375. [DOI] [PubMed] [Google Scholar]
- 30.Roberson D, Merriam S. The Self-Directed Learning Process of Older, Rural Adults. Adult Education Quarterly. 2005;55(4):269–287. [Google Scholar]


