Abstract
Background: South African alcohol-serving establishments (i.e., shebeens) offer unique opportunities to reduce HIV risks among men who drink. Purpose: To test an individual- and a social structural-level HIV prevention intervention for men who drink in shebeens. Methods: Twelve matched pairs of township neighbourhoods were randomized to receive either (i) an HIV prevention intervention (guided by Social Action Theory) to reduce sexual risk and increase risk reduction communication in social networks, or (ii) an attention-matched control intervention that focused on the prevention of relationship violence. At the individual level, the interventions delivered skills building workshops focused on sexual risk reduction. At the social structural level, the intervention aimed to increase conversations about safer sex among men in the shebeens, distributed small media and implemented community educational events. Individual-level outcomes were assessed by following the workshop cohorts for 1 year (N = 984), and community-level outcomes were examined through cross-sectional community surveys conducted for 1 year in the shebeens (N = 9,678). Results: Men in the HIV prevention workshops demonstrated greater condom use, more HIV prevention-oriented conversations and greater perceptions of safer sex norms than men in the comparison workshops. Changes at the community level demonstrated significant differences in condom use, although the pattern was not consistent over time. Conclusions: Multi-level interventions that target men who drink in South African shebeens may help reduce risks for HIV and other sexually transmitted infections.
Introduction
Southern Africa is home to two-thirds of people living with HIV in the world.1 In South Africa, men who drink alcohol are at particularly high risk for HIV and other sexually transmitted infections (STIs).2–4 Informal drinking venues (i.e., shebeens) located in urban townships fuel the generalized HIV epidemic in South Africa by serving as an intersection between high-risk sexual networks and the general population.4 The majority of men who drink alcohol in shebeens also meet sex partners in these venues.5,6 Meeting sex partners in shebeens is associated with higher rates of unprotected sexual behaviours and less frequent condom use.3,7 Sexual risks for HIV transmission are amplified by alcohol use and can be facilitated by the social environment of drinking venues.8 However, the social relationships in shebeens also offer opportunities for peer influence interventions to prevent the spread of HIV. Shifting community norms to foster condom use acceptance may, for example, increase consistent safer sex practices. Social relationships and conversations between network members can shape behavioural norms and are an important target of interventions.
Previous HIV prevention interventions based on social diffusion models of behaviour change delivered in drinking venues have increased condom use among men in US gay bars and female sex workers at drinking venues in the Philippines.9,10 In southern Africa, however, such social-structural HIV prevention interventions have not yet shown positive outcomes.11,12 The structure of social environments can support risk behaviours and hamper individual efforts to reduce risks. Therefore, altering the social context of risk environments by increasing HIV protective conversations can shift social norms and promote long-term behaviour changes.13
The purpose of the present study was to advance community-level HIV prevention interventions in southern Africa by testing a multi-level individual and social structural intervention to reduce sexual risks of men who drink in South African shebeens. We aimed to systematically saturate the social environments of shebeens with men who participated in prevention workshops with the intent of increasing conversations and shifting social norms to support sustained changes in protective behaviours.14 We engaged men from shebeens to attend intervention workshops and encouraged the men to act as agents of change by raising consciousness regarding HIV risks in their community.15,16
We hypothesized that men engaged in alcohol and sexual risk reduction intervention workshops would demonstrate significantly fewer sexual risk behaviours over a sustained period compared with men in a control condition. We also hypothesized that the intervention workshops would encourage discussion of HIV preventive actions, and increase protective attitudes in the men who participated. Finally, we hypothesized that the impact of the intervention would diffuse to men in the broader shebeen community who were not directly engaged in the workshops.
Methods
Participants
Participants were residents living in 12 sections of four large Xhosa townships in Cape Town, South Africa.
Ethical review
The University of Connecticut, Syracuse University and the Human Sciences Research Council of South Africa’s institutional review boards approved all procedures.
Overview of trial design
The study used a two-condition cluster randomized trial designed to test an experimental multi-level alcohol–HIV risk reduction intervention contrasted with an attention-matched control intervention focused on preventing relationship violence. Both interventions had two components: individual-level workshops and community-level activation. The two conditions were time matched, structurally equivalent and attention controlled, and they differed only with respect to the public health problem that was targeted. The outcome assessment also occurred at both individual and community levels (figure 1).
Figure 1.
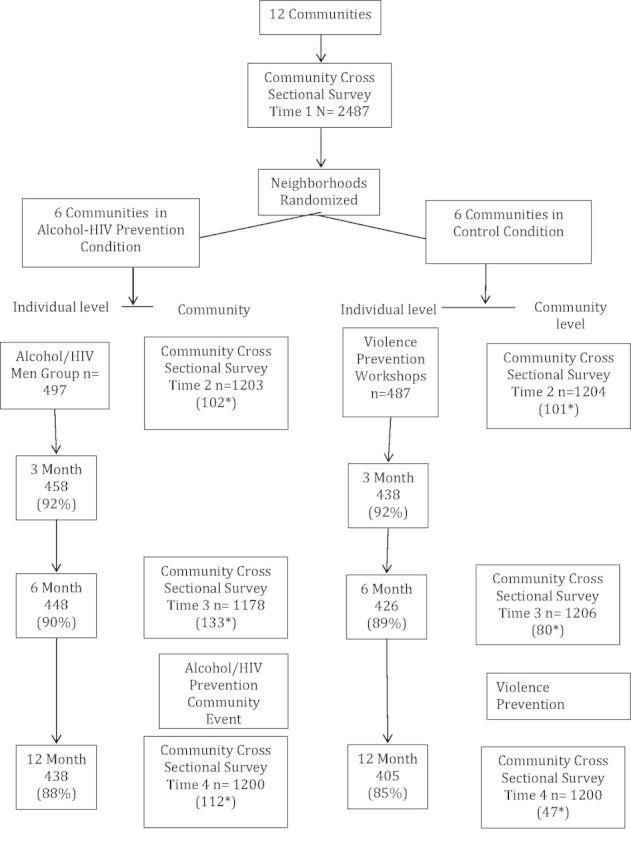
Flow of individual- and community-level participants in the community-level randomized trial. Note values with asterisk represent number of men in a cross-sectional survey time point who attended intervention workshops and were removed from analyses
At the individual level, we recruited an initial 10 men (e.g., seeds) from each venue to participate in the first set of workshops. Specifically, we asked owners and servers to recommend 10 men who come to the shebeen on a regular basis and were 18 years of age or older. The shebeen owners and servers therefore identified the initial seeds. The seeds then attended the first series of three workshops. After the workshops, each seed was asked to identify a male friend from the shebeen and invite him to participate in the next set of workshops. There were no exclusion criteria and the only inclusion criteria were age 18 or older and invited to participate in the project by a man who had already been enrolled. This procedure for recruitment was modelled after methods used in respondent-driven sampling.16
Groups of 8–10 men participated in three 3-hour workshops (9 hours of contact) conducted by one male and one female trained group facilitator. Seven consecutive waves of intervention workshops were performed to accrue approximately 70 men to saturate shebeens with men who were directly engaged in the intervention workshops.9,12,17 Men who participated in the workshops were subsequently followed at 3, 6 and 12 months after intervention assessments.
At the community level, we first conducted cross-sectional behavioural monitoring surveys to establish baseline rates of behaviours and social norms. We repeated the community-level monitoring surveys 4, 8 and 12 months after the baseline. Nine months after the initial set of individual-level workshops, we implemented a community-level event at each shebeen to deliver an informational performance and included lunch. These events, along with increased conversations among men, constituted the community-level intervention.
Shebeen selection and randomization
We used methods described by Weir et al.14,15 to perform rapid community assessments to identify 12 shebeens separated by at least 1 km from each other. All shebeens were confirmed by visits, and we interviewed owners, managers and patrons to determine whether the shebeens served sufficient, at least 75, patrons per week. Owners were asked to participate in the project on the basis of playing a positive role in the community and were offered R500 South African Rand (approximately US$50) three times over the course of the year as a thank you for the use of their shebeens.
Based on the rapid assessment results, shebeens were matched on the median age, education and employment status of patrons; number of adjacent shebeens; number of patrons served during a typical day; the proportion of men relative to women and the types of alcohol sold. Within each matched pair, shebeens were randomized to conditions by the toss of a coin.
Intervention conditions
Experimental alcohol and HIV risk reduction individual-level workshops
The alcohol–HIV risk reduction intervention tested in this trial was grounded in Social Action Theory, a conceptual model that invokes individual, social and environmental factors to explain health behaviour change.18,19 The intervention was designed to directly influence men’s individual sexual decisions and conversations. As suggested by the Social Action Theory, we aimed to change individual sex practices and simultaneously shift safer sex supportive social norms in the broader community context. The workshops therefore had two major components: (i) building individual sexual risk reduction skills for lowering HIV risks and (ii) enhancing interpersonal communication skills to promote safer sex conversations in social networks.
The individual-level behaviour change elements of the intervention concentrated on correcting misconceptions about HIV, recognizing the signs and symptoms of STIs, sensitizing men to HIV risks, reducing numbers of sex partners and increasing condom use.20–23 We addressed alcohol use by integrating the World Health Organization’s brief alcohol counselling model.24 Role-play exercises involving behavioural rehearsal were used to increase risk reduction skills. Proper male and female condom use was instructed and modelled, allowing participants to practice condom application with corrective feedback from the group facilitators.
The social environmental component of the workshops addressed interpersonal and contextual influences on behaviour.25–27 Participants discussed their roles as men in their community and what they can do to make a difference. The focus was on alcohol use, sexual risks and HIV prevention. Participants were asked to select another man from the shebeen who they wanted to ‘teach’ about HIV and set a goal to talk with that man before the next group session. Strategies for talking with friends included selecting the best time and place, preparing to initiate conversations and preparing for resistance.
Experimental alcohol and HIV risk reduction community activation
We implemented community events at the shebeens with the goal of creating an environment conducive for safer sex conversations and supportive of HIV risk reduction. We placed small media (e.g., posters, brochures and flyers) in the shebeens as part of the community-level intervention. We also contracted with a local non-governmental organization to conduct an indigenous community programme on the grounds of the shebeen. Events were conducted once at each shebeen approximately 9 months after the start of the individual-level workshops. The educational-theatrical performance conveyed safer sex and HIV prevention messages. The events lasted an average of 2 hours and served food, with an average of 125 community members attending.
Control relationship violence individual intervention and community activation
We used a matched time and attention workshop intervention focused on relationship violence prevention for communities randomized to the control condition. We also implemented small media materials and non-governmental organizations facilitated community-level educational performance events, with their content directed toward relationship violence prevention.
Assessment procedures
Measures were administered using paper–pencil printed in English and Xhosa. Measures were constructed at a primary school reading level and provided participants with assistance when needed (<5%).
Individual-level intervention outcomes
Measures were collected at the research site using an instructor-guided self-administration procedure in groups of four to eight persons. Assessments were conducted at baseline and at 3, 6 and 12 months’ follow-up. Participants were shown page-by-page how to complete the measures by using an enlarged facsimile, ensuring that instructions for each instrument were carefully described and that participants were given privacy when responding.
Community-level monitoring surveys
We surveyed communities at four time points, every 4 months, over the course of 12 months. Field workers approached men on the streets adjacent to the shebeens as well as individuals socializing and drinking in the shebeens. Individuals who agreed (95%) were given a nine-page anonymous survey that required 10–15 minutes to complete. Equal numbers of participants were surveyed inside and on the adjacent street of selected shebeens. We included an item asking whether the survey participant had attended an intervention workshop. Participants were compensated for taking the time to complete the survey with a keychain or shopping bag. Surveys were not reviewed in the field and names were not collected to protect participant anonymity.
Demographic characteristics and alcohol use
Participants reported their age, race, cultural heritage, education, marital status, employment status and whether they had been treated for an STI and tested for HIV. Frequency of drinking was measured by asking participants how often they drank alcohol in the past month.
Primary outcomes
Sexual behaviours
Participants reported the number of male and female sex partners they had and the number of specific sex acts in which they engaged (vaginal and anal intercourse with and without condoms). Sex behaviour questions were asked with regard to the past 3 months for the individual-level workshop participants to provide a seamless record of individuals’ behaviour and with regard to the past month (30 days) in the cross-sectional community surveys to reflect behaviour most proximal to the survey time. Sexual behaviour measures used an open response format, where participants wrote a number in a blank space.28 We calculated the percent of intercourse occasions protected by condoms (condom-protected intercourse/total intercourse occasions).
HIV protective conversations
Participants reported whether they had a conversation with someone about AIDS and whether they gave advice to use a condom. Responses indicated whether each behaviour had occurred (yes/no) in the previous 30 days.
Secondary outcomes
Individual-level attitudes
To assess risk reduction attitudes, we asked men in the workshops how they ‘personally feel about’ these targeted behaviours: (i) having more than one sex partner, (ii) having sex without a condom and (iii) meeting sex partners in shebeens. Responses were made on 4-point scales, 1 = strongly disapprove and 4 = strongly approve.
Community-level social norms
To assess perceived norms, men in the community-level monitoring surveys were asked ‘How do the men in your community feel about’ these target behaviours: (i) having more than one sex partner, (ii) having sex without a condom and (iii) meeting sex partners in shebeens. Responses we made on 4-point scales, 1 = strongly disapprove and 4 = strongly approve.
Statistical analyses
The primary and secondary outcome analyses tested hypotheses regarding intervention effects on sexual behaviours, conversations, attitudes and norms. Analyses were performed using generalized estimating equations (GEE) for longitudinal workshop intervention outcomes and generalized linear modelling (GZLM) for cross-sectional community-level outcomes.29 GEE corrects for the intraclass correlation, expected as a result of our nested design.30 Poisson distribution or negative binomial distribution was used for variables that were over-dispersed, specifically continuous count data (e.g., sexual partners, sexual behaviours); binomial distributions were used for whether conversations occurred and linear distributions were used for attitudes. GEE models included baseline measures of primary and secondary outcome variables and controlled for demographic characteristics that were significantly different at baseline. Men who participated in the individual-level workshops were removed from the community-level analyses. In all GEE and GZLM models, we controlled for the relationship between condition and outcome variables within paired communities. We report Wald’s X2 tests for model effects on primary and secondary outcomes. All analyses assumed missing data occurred at random and defined statistical significance as P < .05.
Results
Initial analyses found few differences in demographic characteristics between experimental and control communities (table 1). For men in the workshops, the only significant baseline difference occurred for education level; men in the comparison shebeens had less education.
Table 1.
Baseline characteristics of men participating in the intervention workshops and men completing community-level venue surveys
| Characteristic | Men participating in workshops |
||||
|---|---|---|---|---|---|
| Alcohol–HIV intervention |
Control condition |
||||
| (n = 497) |
(n = 478) |
||||
| M | SD | M | SD | t | |
| Age | 29.8 | 8.7 | 30.5 | 9.1 | 1.1 |
| Educationa | 2.4 | 0.6 | 2.3 | 0.6 | 2.7** |
| Alcohol frequency | 4.2 | 1.7 | 4.2 | 1.7 | 0.5 |
| Alcohol intoxication | 2.9 | 1.8 | 2.8 | 1.9 | 0.9 |
| Heavy drinking episodes | 3.9 | 1.8 | 3.8 | 1.8 | 1 |
| N | % | n | % | X2 | |
| Employed | 17 | 3 | 22 | 4 | 0.9 |
| Married | 35 | 7 | 40 | 8 | 0.3 |
| Ethnicity black African | 488 | 98 | 469 | 98 | 0.2 |
| Ever diagnosed with STI | 158 | 31 | 135 | 28 | 1.4 |
| Ever tested for HIV | 314 | 63 | 303 | 63 | 0.1 |
| Tested HIV positive | 26 | 5 | 19 | 4 | 0.8 |
| Men surveyed in and around shebeensb |
|||||
| (n = 3155) |
(n = 3006) |
||||
| M | SD | M | SD | t | |
| Age | 32.5 | 9.7 | 32 | 9.5 | 2.0* |
| Education | 2.5 | 0.7 | 2.6 | 0.7 | 2.7** |
| Alcohol frequency | 3.7 | 2 | 3.7 | 1.9 | 0.3 |
| Alcohol intoxication | 2 | 1.5 | 2 | 1.5 | 0.4 |
| Heavy drinking episodes | 2.9 | 1.9 | 3.1 | 1.9 | 4.8** |
| N | % | n | % | X2 | |
| Employed | 1628 | 51 | 1574 | 52 | 0.32 |
| Married | 793 | 25 | 674 | 22 | 6.3* |
| Ethnicity Black African | 3128 | 99 | 2963 | 98 | 4.6* |
| Ever diagnosed with STI | 2047 | 44 | 1900 | 42 | 6.0** |
| Ever tested for HIV | 3207 | 70 | 3219 | 71 | 1.8 |
| Tested HIV positive | 251 | 5 | 251 | 5 | 0.1 |
aEducation assessed on scale: 1 = No schooling, 2 = grades 1 through 11 completed, 3 = matriculated, 4 = college.
bMen in workshops excluded.
*P < .05, **P < .01.
Individual-level primary outcomes
Table 2 shows the primary sexual behaviour outcomes for men in the experimental and control workshops. Models controlling for baseline and education showed that groups did not differ in the number of sex partners reported or the rates of unprotected intercourse. However, there was a significant effect of the intervention on proportion of intercourse occasions protected by condoms; the experimental HIV prevention groups demonstrated significantly greater use of condoms over the follow-up period. Also, men in the intervention condition engaged in more conversations within their communities about HIV/AIDS and trended toward giving more advice to use condoms.
Table 2.
Individual-level behavioural and attitudinal outcomes reported by men in workshops from the communities receiving the alcohol–HIV prevention and comparison interpersonal violence interventions
| Behavior | Alcohol–HIV Intervention (n = 497) |
Control Condition (n = 478) |
Wald X2 | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Number of sex partners | 0.12 | ||||
| Baseline | 5.7 | 12.9 | 4.5 | 7.2 | |
| 3 months | 4.1 | 11.7 | 4 | 8.6 | |
| 6 months | 3.9 | 7.8 | 3.7 | 5.9 | |
| 12 months | 3.5 | 5.1 | 3.7 | 8.5 | |
| Unprotected sex | 2.18 | ||||
| Baseline | 6.7 | 16.4 | 5.1 | 13 | |
| 3 months | 3.6 | 12.2 | 4.2 | 10.5 | |
| 6 months | 3.6 | 10 | 4.3 | 13.6 | |
| 12 months | 3.4 | 8.3 | 3.6 | 8.2 | |
| % protected sex | 5.23** | ||||
| Baseline | 73 | 33 | 75 | 34 | |
| 3 months | 83 | 27 | 78 | 31 | |
| 6 months | 81 | 29 | 77 | 31 | |
| 12 months | 83 | 28 | 81 | 30 | |
| N | % | N | % | ||
| Talked with people in your community about HIV/AIDS | 23.2** | ||||
| Baseline | 161 | 32 | 136 | 28 | |
| 3 months | 264 | 58 | 191 | 43 | |
| 6 months | 247 | 55 | 180 | 42 | |
| 12 months | 184 | 41 | 126 | 31 | |
| Advised someone to use condoms | 3.6* | ||||
| Baseline | 256 | 51 | 216 | 45 | |
| 3 months | 288 | 62 | 225 | 51 | |
| 6 months | 286 | 64 | 248 | 58 | |
| 12 months | 261 | 59 | 223 | 56 | |
| Attitude | |||||
| How do you feel about having more than one sex partner at a time? | 0.24 | ||||
| Baseline | 2.02 | 1.02 | 1.89 | 0.97 | |
| 3 months | 1.91 | 1 | 1.87 | 1 | |
| 6 months | 1.95 | 1.01 | 1.83 | 0.96 | |
| 12 months | 1.82 | 0.97 | 1.82 | 0.98 | |
| How do you feel about having sex without a condom? | 6.52** | ||||
| Baseline | 0.83 | 0.99 | 0.79 | 1 | |
| 3 months | 0.54 | 0.87 | 0.67 | 0.93 | |
| 6 months | 0.55 | 0.92 | 0.71 | 0.99 | |
| 12 months | 0.59 | 0.89 | 0.65 | 0.94 | |
| How do you feel about meeting sex partners at shebeens? | 5.66** | ||||
| Baseline | 1.76 | 0.9 | 1.64 | 0.84 | |
| 3 months | 1.71 | 0.85 | 1.81 | 0.94 | |
| 6 months | 1.76 | 0.9 | 1.82 | 0.96 | |
| 12 months | 1.67 | 0.82 | 1.76 | 0.91 | |
Behaviours reported for past 3 months; Condition effects from GEE models controlling for education and baseline values. Attitude item responses on 4-point scale, 1 = Strongly disapprove, 4 = Strongly approve; *P = .06; **P < .01
Individual-level secondary outcomes
Analyses controlling for baseline and education showed that men who participated in the experimental HIV prevention workshops demonstrated more positive attitudes toward condom use and less favourable attitudes toward meeting sex partners in shebeens than did men in the control condition (table 2).
Community-level primary outcomes
Models controlling for education found that communities differed at the initial assessment for rates of unprotected intercourse and condom use; the experimental HIV prevention communities had higher rates of unprotected sex and lower proportions of condom use (table 3). Results showed that baseline differences were not present at the second follow-up assessment and reversed to show intervention effects at the third assessment for the percent intercourse occasions protected. In addition, men in the experimental communities reported fewer sex partners at the third assessment. However, there were no differences between the experimental and comparison communities by the final community-level assessments.
Table 3.
Community-level behavioural and perceived social norm outcomes reported by men in the communities receiving the alcohol–HIV prevention and comparison interpersonal violence interventions
| Behavior | Alcohol–HIV intervention |
Control condition |
|||
|---|---|---|---|---|---|
| M | SD | M | SD | Wald X2 | |
| Number of sex partners | |||||
| Baseline | 1.63 | 1.65 | 1.71 | 1.89 | 0.12 |
| 4 months | 1.67 | 1.79 | 1.77 | 2.15 | 0.24 |
| 8 months | 1.46 | 1.36 | 1.66 | 1.69 | 4.01* |
| 12 months | 1.39 | 1.17 | 1.52 | 1.95 | 3.35 |
| Unprotected sex | |||||
| Baseline | 7.13 | 8.61 | 5.92 | 8.37 | 13.71** |
| 4 months | 6.06 | 9.38 | 6.35 | 7.4 | 0.01 |
| 8 months | 5.81 | 8.37 | 6.25 | 7.54 | 1.01 |
| 12 months | 5.34 | 6.32 | 4.88 | 6.43 | 2.14 |
| % protected sex | |||||
| Baseline | 54 | 42 | 60 | 42 | 7.92** |
| 4 months | 57 | 42 | 57 | 42 | 0.06 |
| 8 months | 59 | 43 | 53 | 42 | 6.16* |
| 12 months | 54 | 42 | 57 | 44 | 1.62 |
| n | % | n | % | ||
| Talked with people in your community about HIV/AIDS | |||||
| Baseline | 270 | 40 | 243 | 40 | 0.01 |
| 4 months | 261 | 47 | 266 | 50 | 0.65 |
| 8 months | 270 | 45 | 270 | 49 | 0.64 |
| 12 months | 338 | 53 | 270 | 47 | 5.09* |
| Advised someone to use condoms | |||||
| Baseline | 333 | 56 | 313 | 61 | 2.32 |
| 4 months | 342 | 68 | 318 | 62 | 3.86* |
| 8 months | 375 | 65 | 328 | 62 | 1.21 |
| 12 months | 387 | 64 | 382 | 63 | 0.12 |
| How do men in your community feel about having more than one sex partner at a time? | |||||
| Baseline | 2.84 | 1.06 | 2.87 | 1.03 | 0.02 |
| 4 months | 2.89 | 1 | 2.88 | 0.98 | 0.02 |
| 8 months | 2.93 | 1.02 | 3.01 | 1 | 2.6 |
| 12 months | 2.93 | 0.95 | 3.07 | 0.9 | 7.73** |
| How do men in your community feel about having sex without a condom? | |||||
| Baseline | 2.72 | 0.89 | 2.68 | 0.89 | 0.2 |
| 4 months | 2.71 | 0.86 | 2.71 | 0.93 | 0.08 |
| 8 months | 2.75 | 0.82 | 2.77 | 0.73 | 0.31 |
| 12 months | 2.71 | 0.79 | 2.87 | 0.8 | 15.91** |
| How do men in your community feel about meeting sex partners at shebeens? | |||||
| Baseline | 2.73 | 1 | 2.82 | 0.98 | 2.74 |
| 4 months | 2.79 | 0.96 | 2.72 | 1.08 | 1.54 |
| 8 months | 2.74 | 0.99 | 2.82 | 0.99 | 2.78 |
| 12 months | 2.84 | 0.95 | 2.85 | 0.94 | 0.03 |
Note: Behaviours reported for past 30 days; Condition effects from GZLM models controlling for education and baseline values. Social norm item responses on 4-point scale, 1 = Strongly disapprove, 4 = Strongly approve; *P < .05, **P < .01
For conversational outcomes, we found that men in the experimental communities were significantly more likely to report having advised someone to use condoms at the second assessment, and had talked with people in the community about AIDS at the final cross-sectional assessment (table 3).
Community-level secondary outcomes
With respect to perceived social norms at the community-level assessments, we found that at the final 12-month assessment, men in the experimental HIV prevention communities reported less perceived support for having multiple sex partners and less perceived support for not using condoms than men in the control communities. There were no differences between conditions for perceived norms for meeting sex partners in shebeens (table 3).
Discussion
The current community-level prevention trial tested an alcohol-related HIV prevention intervention that targeted South African men who drink in shebeens. The intervention aimed to reduce men’s sexual risks and sustain risk reduction behaviour change by altering the social context in which men drink. Participants in the HIV risk reduction and communication skills training workshops demonstrated significantly greater use of condoms than participants in the control communities. Confirming our hypotheses, individual-level changes in behaviour were sustained over 12 months. Results at the community-level were less consistent, with men surveyed from the HIV prevention shebeens evidencing greater condom use only at the third assessment. At the community level, condom use increased 9.2% at the third assessment (8 months from baseline) in the experimental communities, compared with an 11.6% decrease in the control communities. This effect did not occur at the second or fourth community surveys. Thus, the intervention had its greatest impact on condom use at the individual level, with a more modest and inconsistent effect observed in the broader community.
We also observed greater conversations about HIV and condoms reported by men in the experimental alcohol–HIV prevention workshops than men who participated in the control workshops. Differences between conditions in preventive communications were accompanied by changes in protective attitudes. Consistent with the condom use and attitudinal outcomes, we observed changes in conversations and perceived social norms at the community level. Analyses at the community level suggest modest shebeen-level changes may have occurred as a result of social diffusion.12,17
The current study adds to the growing literature on social structural interventions for HIV prevention. It has long been known that personal behaviour change is difficult to achieve without environmental support. Social and environmental cues such as those that occur in conversations can lead to relapse to risk behaviour.31,32 Drinking venues are cue-rich environments for sexual risk behaviour.33 Changes in the social context of shebeens that we observed through men’s conversations and perceived norms may have fostered sustained condom use among men in the intervention workshops and the diffusion of behaviour changes observed among men in the broader community. Like other multi-level drinking venue interventions,34 the pattern of individual- and community-level changes in behaviour, conversations and norms in this trial may have synergistic effects.
These findings should be interpreted in light of the study limitations. Our intervention emphasized condom use to a greater degree than other potential risk reduction strategies, including reductions in numbers of partners. Although our intervention addressed these options, condoms were the focus of skills training. The study was also limited by our reliance on self-report measures for behavioural outcomes. Self-reported sexual behaviours are influenced by social biases, including social desirability. In addition, behavioural measures were collected using a proximal timeframe of 1-month recall at the community level and a wider timeframe of 3 months for individual-level data, prohibiting direct comparisons of changes in rates of behaviour. Our study is also limited by not including a disease end point, such as incident STI. Finally, the magnitude of intervention effects at the individual and community levels was modest and should be considered one potential facet of more comprehensive approaches to HIV risk reduction in alcohol-serving venues. With these limitations in mind, we believe that our findings offer new directions for HIV prevention in South African drinking venues.
Alcohol use is a reliable predictor of sexual risks for HIV infection. Indeed, countries with the greatest per-capita consumption of alcohol have among the greatest prevalence rates of HIV.35 Findings from the current trial build on previous research with other populations in vastly different settings to suggest that shebeens, typically considered risk environments, can serve as platforms for HIV prevention.36 Additional research is needed to test multi-level interventions that target a broader spectrum of risk reduction behaviours beyond condom use for men in shebeens. Shifting social perceptions of shebeens away from being viewed as risk environments toward places that support protective behaviours will help sustain long-term individual efforts toward behaviour change.
Funding
This project was supported by National Institute on Alcohol Abuse and Alcoholism Grants R01-AA017399.
Conflicts of interest: None declared.
Key points.
Informal drinking venues in South Africa offer unique opportunities for HIV prevention interventions conducted at the community level.
A randomized community-level HIV prevention intervention trial targeting men in South African drinking venues demonstrated modest effects on increased condom use and shifts in risk reduction social norms.
Individual-level intervention effects were sustained over 1-year follow-up in conjunction with modest shifts in risk reduction supportive social norms.
References
- 1.UNAIDS. UNAIDS World AIDS Day Report 2011. 2011. [Google Scholar]
- 2.Kalichman SC, Simbayi LC, Vermaak R, et al. HIV/AIDS risks among men and women who drink at informal alcohol serving establishments (Shebeens) in Cape Town, South Africa. Prev Sci. 2008;9:55–62. doi: 10.1007/s11121-008-0085-x. [DOI] [PubMed] [Google Scholar]
- 3.Morojele NK, Kachieng’a MA, Mokoko E, et al. Alcohol use and sexual behaviour among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Soc Sci Med. 2006;62:217–27. doi: 10.1016/j.socscimed.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 4.Kalichman SC, Simbayi LC, Kaufman M, et al. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8:141–51. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- 5.Weir SS, Morroni C, Coetzee N, et al. A pilot study of a rapid assessment method to identify places for AIDS prevention in Cape Town, South Africa. Sex Transm Infect. 2002;78(Suppl I):106–13. doi: 10.1136/sti.78.suppl_1.i106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weir SS, Pailman C, Mahlalela X, et al. From people to places: focusing AIDS prevention efforts where it matters most. AIDS. 2003;17:895–903. doi: 10.1097/01.aids.0000050809.06065.e0. [DOI] [PubMed] [Google Scholar]
- 7.Kalichman SC, Simbayi LC, Vermaakk R, et al. HIV/AIDS risks among men and women who drink at informal alcohol serving establishments (Shebeens) in Cape Town, South Africa. Prev Sci. 2008;9:55–62. doi: 10.1007/s11121-008-0085-x. [DOI] [PubMed] [Google Scholar]
- 8.Carey KB, Scott-Sheldon LA, Carey MP, et al. Community norms for HIV risk behaviors among men in a South African township. J Behav Med. 2011;34:32–40. doi: 10.1007/s10865-010-9284-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly JA, Murphy DA, Sikkema KJ, et al. Randomized, controlled, community-level HIV prevention intervention for sexual risk behaviour among homosexual men in US cities. Lancet. 1997;350:1500–5. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- 10.Morisky DE, Stein JA, Chiao C, et al. Impact of a social influence intervention on condom use and sexually transmitted infections among establishment-based female sex workers in the Philippines: a multilevel analysis. Health Psychol. 2006;25:595–603. doi: 10.1037/0278-6133.25.5.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fritz K, McFarland W, Wyrod R, et al. Evaluation of a peer network-based sexual risk reduction intervention for men in beer halls in Zimbabwe: results from a randomized controlled trial. AIDS Behav. 2011;15:1732–44. doi: 10.1007/s10461-011-9922-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rogers E. Diffusion of Innovations. 5th edn. New York: Free Press; 1995. [Google Scholar]
- 13.Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol. 2003;22:332–9. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- 14.Kincaid DL. From innovation to social norm: bounded normative influence. J Health Commun. 2004;9(Suppl 1):37–57. doi: 10.1080/10810730490271511. [DOI] [PubMed] [Google Scholar]
- 15.Heckathorn D, editor. Cognitive Psychology, Social Networks, and AIDS. The workshop on social and behavioral science base HIV prevention. Washington, DC, 1995: [Google Scholar]
- 16.Ramirez-Valles J, Heckathorn DD, Vázquez R, et al. From networks to populations: the development and application of respondent-driven sampling among IDUs and Latino gay men. AIDS Behav. 2005;9:387–402. doi: 10.1007/s10461-005-9012-3. [DOI] [PubMed] [Google Scholar]
- 17.Kelly JA, St Lawrence JS, Diaz YE, et al. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Public Health. 1991;81:168–71. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ewart C. Social action theory for a public health psychology. Am Psychol. 1991;465:931–46. doi: 10.1037//0003-066x.46.9.931. [DOI] [PubMed] [Google Scholar]
- 19.Ewart C. How integrative behavioral theory can improve health promotion and disease prevention. In: Boll TJ, Frank RG, Baum A, Wallander J, editors. Handbook of Health Psychology. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- 20.Latkin CA, Donnell D, Metzger D, et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Soc Sci Med. 2009;68:740–8. doi: 10.1016/j.socscimed.2008.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelly JA, Kalichman SC. Behavioral research in HIV/AIDS primary and secondary prevention: recent advances and future directions. J Consult Clin Psychol. 2002;70:626–39. [PubMed] [Google Scholar]
- 22.Carey MP, Maisto SA, Kalichman SC, et al. Enhancing motivation to reduce risk for HIV infection for economically disadvantaged urban women. J Consult Clin Psychol. 1997;65:531–41. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carey KB, Scott-Sheldon LA, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: a meta-analytic review. Addict Behav. 2007;32:2469–94. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addictions. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 25.Latkin C, Sherman S, Knowlton A. HIV prevention among drug users: outcomes of a network-oriented peer outreach intervention. Health Psychol. 2003;22:332–9. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- 26.Kelly JA, Amirkhanian YA, Kabakchieva E, et al. Prevention of HIV and sexually transmitted diseases in high risk social networks of young Roma (Gypsy) men in Bulgaria: randomised controlled trial. BMJ. 2006;333:1098. doi: 10.1136/bmj.38992.478299.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trotter RT, Bowen AM, Baldwin JA, Price LJ. The efficacy of network-based HIV/AIDS risk reduction programs in midsized towns in the United States. J Drug Issues. 1996;26:591–605. [Google Scholar]
- 28.Napper LE, Fisher DG, Reynolds GL, Johnson ME. HIV risk behavior self-report reliability at different recall periods. AIDS Behav. 2009;14:152–61. doi: 10.1007/s10461-009-9575-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pan W. Akaike's information criterion in generalized estimating equations. Biometrics. 2001;57:120–5. doi: 10.1111/j.0006-341x.2001.00120.x. [DOI] [PubMed] [Google Scholar]
- 30.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–60. [PubMed] [Google Scholar]
- 31.Brownell KD, Marlatt GA, Lichtenstein E, Wilson GT. Understanding and preventing relapse. Am Psychol. 1986;41:765–82. doi: 10.1037//0003-066x.41.7.765. [DOI] [PubMed] [Google Scholar]
- 32.Marlatt GA. Cue exposure and relapse prevention in the treatment of addictive behaviors. Addict Behav. 1990;15:395–9. doi: 10.1016/0306-4603(90)90048-3. [DOI] [PubMed] [Google Scholar]
- 33.Kelly JA, Kalichman SC, Kauth MR, et al. Situational factors associated with AIDS risk behavior lapses and coping strategies used by gay men who successfully avoid lapses. Am J Public Health. 1991;81:1335–8. doi: 10.2105/ajph.81.10.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morisky DE, Stein JA, Chiao C, et al. Impact of a social influence intervention on condom use and sexually transmitted infections among establishment-based female sex workers in the Philippines: a multilevel analysis. Health Psychol. 2006;25:595–603. doi: 10.1037/0278-6133.25.5.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fritz K, Morojele N, Kalichman S. Alcohol: the forgotten drug in HIV/AIDS. Lancet. 2010;376:398–400. doi: 10.1016/S0140-6736(10)60884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Latkin CA, Knowlton AR. Micro-social structural approaches to HIV prevention: a social ecological perspective. AIDS Care. 2005;17(Suppl 1):S102–13. doi: 10.1080/09540120500121185. [DOI] [PubMed] [Google Scholar]


