Abstract
BACKGROUND
Great strides have been made in improving heart health in the United States during the last 2 decades, yet these strides have not encompassed many ethnic minority populations. There are significant health disparity gaps stemming from both a paucity of valid research and a lack of culturally sensitive interventions. In particular, many Korean Americans with chronic illnesses encounter difficulty navigating the healthcare system because of limited health literacy.
METHODS
The effect of a multimodal Self-Help Intervention Program on the Control of High Blood Pressure (HBP) was tested in a community-based clinical trial for Korean American seniors. Of 440 seniors enrolled, 369 completed the study (184 in the intervention group and 185 in the control group; mean age = 70.9±5.3 years). The intervention group received 6 weekly educational sessions on HBP management skill building, including health literacy training, followed by telephone counseling and home blood pressure (BP) monitoring for 12 months.
RESULTS
Findings support that the Self-Help Intervention Program on the Control of HBP was effective in controlling BP in this ethnic/linguistic minority population. The BP control rates for the intervention and control groups were 49.5% vs. 43.2% at baseline, 58.5% vs. 42.4% at 6 months, 67.9% vs. 52.5% at 12 months, and 54.3% vs. 53.0% at 18 months. Significant changes were observed over time in some psychobehavioral outcomes, including self-efficacy for BP control, medication adherence behavior, HBP knowledge, and depression.
CONCLUSIONS
The study findings suggest that the multimodal Self-Help Intervention Program on the Control of HBP is effective at promoting optimal HBP control for this ethnic/linguistic minority population.
CLINICAL TRIALS REGISTRY
Keywords: behavioral intervention, blood pressure, community-based participatory research, health disparity, health literacy, high blood pressure, hypertension, Korean Americans.
Although improvements have been made in heart health in the United States during the last 2 decades, significant health disparities, stemming from insufficient research and a lack of culturally sensitive service infrastructure, remain for ethnic minority populations.1 Many ethnic minorities also suffer from insufficient health literacy, which severely limits their ability to “obtain, process, and understand basic health information and services to make appropriate health decisions.”2 Korean Americans, in particular, have encountered stiff language and cultural barriers to accessing the US healthcare system,3,4 and Korean American seniors have difficulties in managing chronic diseases such as high blood pressure (HBP).4 We therefore designed a multimodal HBP management program for Korean American seniors aimed at enhancing self-help management skills for HBP, which includes behavioral education5 and home blood pressure (BP) monitoring,6 followed by monthly counseling with community health workers7 and an extensive HBP management–related health literacy exercise component. Detailed information regarding each component of the intervention, including its theoretical underpinning, has been published elsewhere.5 The positive effect of our original community-based multifaceted HBP intervention program, which did not have a health literacy component, was demonstrated in our previous trials.5,6 To this intervention, we then added the HBP management–related health literacy exercise component as an important link between knowledge and health outcomes in self-help chronic disease management and to address a critical need of this target population, an elderly linguistic minority group with known low levels of health literacy.8–13 We present results of the clinical trial in which we tested the efficacy of our newly enhanced behavioral intervention for Korean American seniors. Specifically, we examine the effect of the intervention on (i) HBP management as a primary outcome and (ii) health literacy, self-efficacy, medication adherence, and psychological status (depression) as secondary outcomes.
METHODS
Study design
The multimodal Self-Help Intervention Program on the Control of HBP was presented in a prospective clinical controlled trial with Korean American senior participants from the Baltimore-Washington metropolitan area during the years 2007–2011. The intervention had 2 phases.
Planning.
In meetings with a community-based curriculum advisory committee, the intervention protocols were refined after pilot tests. The committee was comprised of Korean Americans from the greater Baltimore-Washington area, including Korean American seniors with HBP, healthcare providers, community leaders such as pastors, family members and caregivers of Korean American seniors with hypertension, nurse researchers, and social workers. Every effort was made to follow critical principles of participatory research,14 emphasizing mutuality and partnership between researchers and the target community. The planning resulted in our final Self-Help Intervention Program on the Control of HBP intervention protocol.
Testing.
To test the efficacy of the intervention protocol, we used a randomized clinical control trial with the intervention delayed for the control group. Using adaptive stratified randomization, we selected 22 Korean American churches and senior centers as intervention and control group sites, depending on size or location. Potential participants were screened, enrolled, and tested at each site.
Procedures
Sampling.
After approval by the Johns Hopkins Hospital Institutional Review Board, sites were selected and assigned for interventions or control groups. At baseline, a total of 633 Korean American seniors were screened; 440 were enrolled. Participants were aged 60 years or older with systolic BP ≥140mm Hg and/or diastolic BP ≥90mm Hg on 2 separate measurements or were on antihypertensive medication. After participants provided written informed consent, bilingual registered nurses (RNs) obtained 3 BP measurements, and trained bilingual research staff conducted face-to-face interviews for initial data collection. For both the intervention and control groups, data collection was repeated at 6, 12, and 18 months.
The control group received a brief educational brochure that also listed available resources in the community at baseline and an abbreviated educational session after all data were collected at 18 months. The intervention group received the following procedures: education and training, BP home monitoring, and telephone counseling.
Education and training.
The intervention group received 2-hour weekly educational sessions at the sites over 6 weeks, given by trained bilingual RNs and nutritionists to groups of 6–10 participants. The sessions covered (i) health literacy training and (ii) HBP management. Health literacy training focused on learning words and phrases relevant to care and control of HBP obtained from essential medical terminologies, prescriptions, and food labels, as well as practicing communication with healthcare providers regarding HBP.3 HBP management focused on (i) an overview of HBP and general HBP management guidelines, (ii) short- and long-term complications of uncontrolled BP, (iii) healthy diet and nutrition, (iv) food labels and exercise, (v) medications and food–drug interactions, and (vi) problem-solving skills. The process of cultural adaption of this multimodal HBP intervention in our previous studies has been published elsewhere.5
BP home monitoring.
After the instruction period, participants received a BP monitor (A&D UA-767, A&D Company Ltd, Tokyo, Japan)15 equipped with tele-transmission. The system was easy to use, but we provided instructions and technical assistance in Korean to ensure that participants followed the monitoring protocol.16 Participants were told that they should measure their BP at home twice a day (morning and evening) with 3 readings at each monitoring session. Additionally, they were asked to transmit accumulated BP data at least once a week to our contractor’s website. The contractor generated a monthly report, which counselors and participants shared for counseling and goal-setting.
Telephone counseling.
Trained bilingual community health workers conducted monthly telephone counseling for 12 months. The main goals of this counseling were to encourage the participants to maintain healthy behaviors, to address barriers to their obtaining adequate HBP care, and to assist them in problem solving if they encountered any difficulties. Bilingual RNs supervised the community health workers and contacted participants by phone when needed. For example, if a participant’s transmitted BP readings were ≥160/100mm Hg, an RN discussed this with the participant. If participants’ BP readings were ≥180/110mm Hg, the RN told them to contact their healthcare providers or visit a nearby urgent care center. At the same time, the RN contacted the consulting physician for the study. The selection and training of community health workers for HBP control and our working principles are detailed in our previous publication.7
Measurements
We collected individual sociodemographic characteristics at baseline, including length of stay in the United States, health insurance coverage, and medical history. We also collected BP readings and psychosocial outcome variables, including health literacy, HBP knowledge, self-efficacy, and depression at baseline, 6, 12, and 18 months.
BP was measured using a digital sphygmomanometer (A&D UA-767),15 which was checked regularly for precision and accuracy. Participants were instructed to refrain from using tobacco products, alcohol, or caffeine for 30 minutes before measurement. Participants sat quietly, resting the left arm on a flat surface (at the heart’s level) for at least 5 minutes before the first measurement. Three measurements were taken at 1-minute intervals; the second and third readings were averaged.
The HBP health literacy scale3 measured health literacy. The scale’s 43 items measure 2 domains—print literacy and functional health literacy for HBP management. Items are scored as correct or incorrect and then summed; higher scores indicate greater health literacy. The Kuder–Richardson reliability coefficient of the HBP health literacy scale was 0.98 in this study.
The 8-item Hill-Bone Medication Adherence scale for Korean Americans16 assessed adherence to BP medication. This 4-point Likert-type scale ranging from 1 (none of the time) to 4 (all the time) asks how often the participant has not complied with HBP medication therapy. Higher summed scores reflect poorer adherence. In this study, the Cronbach’s alpha reliability coefficient was 0.69.
HBP knowledge was assessed using a 26-item HBP knowledge questionnaire, combining the 12-item Check Your HBPIQ instrument17 with another 14 items based on our own intensive literature review. This scale was used with Korean Americans in our previous study.18 The items are scored as correct or incorrect and then summed; higher scores indicate greater HBP knowledge. The Kuder–Richardson reliability coefficient for this study was 0.62.
HBP self-efficacy was assessed using an 8-item questionnaire adapted from the HBP belief scale.19 The modified scale’s 4-point Likert-type items asked participants to rate from 1 (not confident at all) to 4 (very confident) how confident they felt about managing HBP in areas such as reducing salt intake, physical activity, and eating fewer fatty foods. Total scores were summed across the 8 items; higher scores indicate greater self-efficacy. The Cronbach’s alpha reliability coefficient in this study was 0.69.
Depression was measured using the Patient Health Questionnaire, which is comprised of 9 items that evaluate the presence of depressive symptoms over the past 2 weeks.20 Items are scored from 0 (not at all) to 3 (nearly every day); totals range from 0 to 27. The Patient Health Questionnaire cutpoints are 5, 10, 15, and 20 for mild, moderate, moderate severe, and severe depression, respectively. We used a total score of ≥5 as a cutpoint for presence of depressive symptoms. The Cronbach’s alpha reliability coefficient in this study was 0.81.
Analysis
We used χ2 tests to examine differences between the intervention and control groups in categorical outcome variables at each data collection point and t tests/Wilcoxon rank-sum tests for continuous variables.
We also used repeated measures analysis of variance to assess the effect of the intervention over time on the primary outcomes (systolic BP, diastolic BP, and BP control rates measured at baseline, 6, 12, and 18 months) and on the secondary outcomes, including HBP-specific health literacy, adherence to BP medication, HBP knowledge, HBP self-efficacy, and depression.
RESULTS
Enrollment, participation, and retention
We screened a total of 633 Korean American seniors and enrolled 440 (225 in the intervention group and 215 in the control group). Figure 1 presents a CONSORT diagram describing participants remaining in the program at each data collection time point. At 6, 12, and 18 months, the numbers of participants who stayed in the study were 379 (86.1%), 372 (84.5%), and 369 (83.9%); at 18 months, the distribution was nearly even (184 in the intervention group; 185 in the control group). Over the 18 months, 71 (16.1%) participants dropped out for reasons such as cessation of contact (phone disconnection, residence change), schedule conflict, personal problems, or physical conditions. Some dropped out because they thought their BP was not high enough to require rigorous management. There were no differences in sociodemographic characteristics between those who remained in the study and those who dropped out. Analysis included only those who completed the study.
Figure 1.
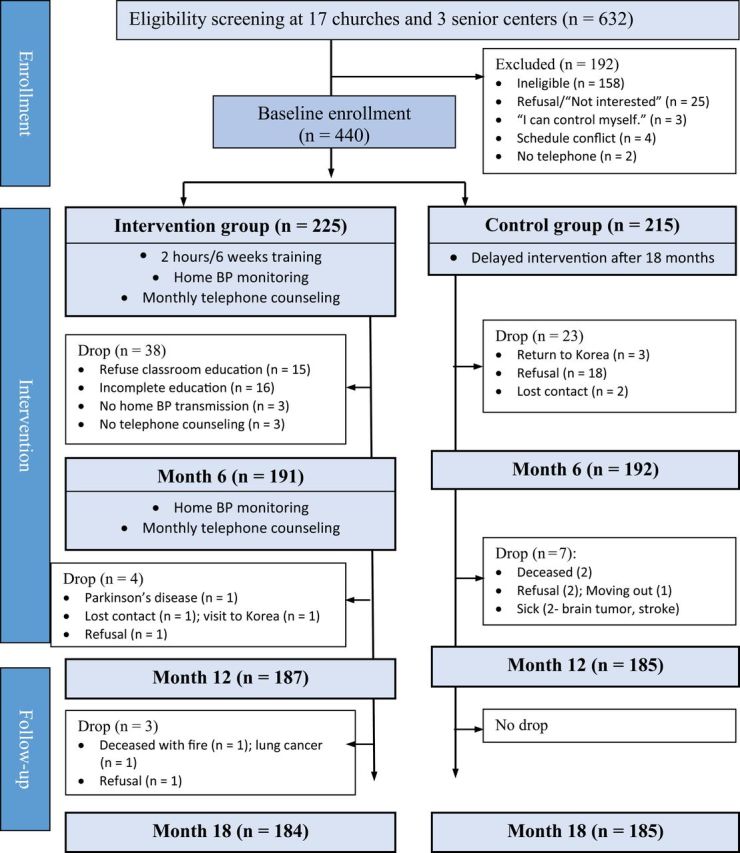
CONSORT chart.
Sociodemographic characteristics
Participants’ mean age was 70.9 years (±5.3; range = 60–89 years). There were almost 3 times more women (72.4%) than men, reflecting the sex distribution for the target population. The majority (65.6%) lacked education beyond high school and had been in the United States for 25 (±11) years on average (Table 1).
Table 1.
Sociodemographic characteristics of participants at baseline (n = 369)
| Characteristics | Total (n = 369) | Intervention (n = 184) | Control (n = 185) | P value |
|---|---|---|---|---|
| Age, y, mean (SD) | 70.9 (5.3) | 70.6 (5.0) | 71.2 (5.6) | 0.29 |
| ≤69, no. (%) | 155 (42.0) | 79 (42.9) | 76 (41.1) | |
| 70–79, no. (%) | 190 (51.5) | 97 (52.7) | 93 (50.3) | |
| ≥80, no. (%) | 24 (6.5) | 8 (4.3) | 16 (8.6) | |
| Sex | 0.29 | |||
| Male, no. (%) | 111 (30.1) | 60 (32.6) | 51 (27.6) | |
| Female, no. (%) | 258 (69.9) | 124 (67.4) | 134 (72.4) | |
| SBP, mm Hg, mean (SD) | 141 (19) | 141 (17) | 140 (20) | 0.69 |
| DBP, mm Hg, mean (SD) | 79 (11) | 79 (11) | 79 (11) | 0.91 |
| BMI, kg/m2, mean (SD) | 256 (3.2) | 25.5 (3.2) | 25.7 (3.3) | 0.70 |
| Education, y, mean (SD) | 11.2 (4.3) | 11.2 (4.2) | 11.1 (4.4) | 0.73 |
| ≤Middle school graduate, no. (%) | 138 (37.4) | 68 (37.0) | 70 (37.8) | |
| High school graduate, no. (%) | 104 (28.2) | 54 (29.3) | 50 (27.0) | |
| ≥Some college, no. (%) | 127 (34.4) | 62 (33.7) | 65 (35.1) | |
| Living in United States, y, mean (SD) | 25.0 (11.0) | 25.6 (10.5) | 24.4 (11.5) | 0.30 |
| Medical history | ||||
| Length of having HBP, y, mean (SD) | 9.8 (8.9) | 9.9 (8.7) | 9.7 (9.1) | 0.81 |
| On HBP medication, yes, no. (%) | 315 (85.4) | 163 (88.6) | 152 (82.2) | 0.08 |
| Family history of HTN, yes, no. (%) | 195 (52.8) | 105 (57.1) | 90 (48.6) | 0.11 |
| Comorbidities, yes, no. (%)a | 171 (46.3) | 91 (49.5) | 80 (43.2) | 0.23 |
| Controlled BP, yes, no. (%)b | 137 (37.1) | 62 (33.7) | 75 (40.5) | 0.17 |
| Healthcare utilization | ||||
| Having health insurance, yes, no. (%) | 305 (82.7) | 157 (85.3) | 148 (80.0) | 0.18 |
| Having PCP, yes, no. (%) | 311 (84.3) | 164 (89.1) | 147 (79.5) | 0.01 |
| Nonadherence to BP medication, mean (SD)c | 9.7 (2.4) | 9.7 (2.7) | 9.6 (2.0) | 0.61 |
| Self-efficacy for BP control, mean (SD) | 26.6 (3.5) | 26.4 (3.4) | 26.7 (3.6) | 0.45 |
| HBP knowledge, mean (SD) | 19.2 (3.2) | 19.4 (2.8) | 19.0 (3.6) | 0.24 |
| Depression (PHQ-9), mean (SD) | 2.9 (3.7) | 2.9 (3.5) | 2.9 (3.8) | 0.95 |
Abbreviations: BMI, body mass index; BP, blood pressure; DBP, diastolic blood pressure; HBP, high blood pressure; HTN, hypertension; PCP, primary care provider; PHQ-9, 9-item Patient Health Questionnaire; SBP, systolic blood pressure.
aDefined as having heart disease, angina, kidney disease, or diabetes.
bDefined as BP <140/90mm Hg (130/80mm Hg for patients with diabetes).
cParticipants who were not on medication were excluded.
Participants had been diagnosed with hypertension for an average of 9.6 (±8.8) years; 52.8% had a family history of hypertension, and 46.3% had ≥1 comorbid conditions. Approximately 85.4% reported being on antihypertension medication, but less than half (46.3%) had successfully controlled hypertension (BP <140/90mm Hg or <130/80mm Hg for those with diabetes). The intervention and control groups did not differ in these characteristics, although slightly more participants within the control group had a primary care provider.
Intervention dose received by participants
One hundred ten (60.0%) participants in the intervention group attended all 6 in-class education sessions, whereas others attended 3–5 sessions, with a mean of 5.4 (± 0.80) sessions. Approximately two-thirds (65.4%) of participants responded to all 12 telephone counseling sessions, with a mean of 11.5 (±0.86) sessions. During the 12-month project period, the intervention group transmitted a total of 164,279 BP measurements, averaging 2.5 measurements per person per day.
Effect of Self-Help Intervention Program on the Control of HBP on medication-taking behaviors
Because one of the main educational objectives of our intervention was to facilitate constructive patient–provider communication, including not delaying medical treatment of HBP (e.g., taking medication if recommended) and patients actively participating in their treatment plan with their provider, we monitored these patients’ medication-taking status throughout follow-up. At baseline, 10.3% (n = 19) of the intervention group and 18.4 % (n = 34) of the control group were delaying medical treatment and not taking HBP medication. The numbers of participants who were not taking any HBP medication steadily decreased for both groups over each follow-up period. At the end of the study, only 3.3% (n = 6) of the intervention group and 6.0% (n = 11) of the control group were not taking any HBP medication. Overall, the vast majority of study participants in both groups were on a stable medication regimen with relatively little changes during the study period (18 months). The changes in medication-taking behaviors measured by the Hill–Bone HBP compliance scale16 demonstrated that the mean level of non-adherence to BP medication within the intervention group decreased over time and also revealed the statistically significant difference between groups. The levels of non-adherence to BP medication were not different between the intervention and control groups at baseline.
Effect of Self-Help Intervention Program on the Control of HBP on primary outcomes
BP outcomes.
Figure 2 displays mean systolic BP and diastolic BP for the intervention and control groups from baseline to 18 months. Both measures dropped in these groups but rose in the intervention group at 18 months. BP decreases in the intervention group were steep at 6 months (9.1mm Hg for systolic BP; 3.9mm Hg for diastolic BP) (Table 2). The mean differences in systolic BP between the 2 groups at baseline, 6, 12, and 18 months were 0.8mm Hg (P = 0.69), −6.0mm Hg (P = 0.001), −6.1mm Hg (P = 0.002), and −2.9mm Hg (P = 0.12). The mean differences in diastolic BP were 0.2mm Hg (P = 0.91), −2.5mm Hg (P = 0.02), −2.9mm Hg (P = 0.01), and −0.9mm Hg (P = 0.37).
Figure 2.
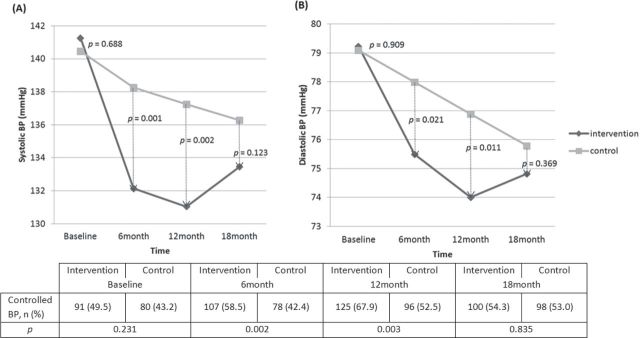
Changes in mean blood pressure (BP) over time and frequency of controlled BP between intervention and control groups.
Table 2.
Changes in mean blood pressure from baseline to 18 months (n = 369)
| Blood Pressure | Time | Intervention, | Control, | Source | F | P value |
|---|---|---|---|---|---|---|
| mean (SD) | mean (SD) | |||||
| Mean SBP | Baseline | 141 (17) | 140 (21) | Group | 5.532 | 0.02 |
| 6 mo | 132 (15) | 138 (21) | Time | 20.243 | 0.000 | |
| 12 mo | 131 (15) | 137 (22) | Group × Time | 5.662 | 0.001 | |
| 18 mo | 133 (16) | 136(19) | ||||
| Mean DBP | Baseline | 79 (11) | 79 (12) | Group | 2.812 | 0.09 |
| 6 mo | 75 (11) | 78 (11) | Time | 22.294 | 0.000 | |
| 12 mo | 74 (10) | 78 (11) | Group × Time | 3.648 | 0.01 | |
| 18 mo | 74 (10.1) | 76 (10) |
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure.
Health literacy changes.
Health literacy scores showed no difference between the two groups at 6 months, but there were significant differences in both print and functional health literacy scores at 12 and 18 months; scores for the intervention group were much higher (Table 3).
Table 3.
Changes in health literacy outcomes from baseline to 18 months (n = 369)
| Outcomes | Time | Intervention | Control | Source | F | P value |
|---|---|---|---|---|---|---|
| mean (SD) | mean (SD) | |||||
| Baseline | 17.9 (9.5) | 17.7 (11.2) | Group | 2.555 | 0.11 | |
| 6 mo | 19.8 (9.5) | 17.6 (10.6) | Time | 13.300 | 0.000 | |
| 12 mo | 20.1 (9.2) | 17.8 (10.6) | Group × Time | 7.684 | 0.000 | |
| 18 mo | 21.3 (8.4) | 18.2 (10.2) | ||||
| Functional | Baseline | 6.9 (3.5) | 6.8 (4.4) | Group | 3.278 | 0.07 |
| 6 mo | 7.9 (4.0) | 7.2 (4.0) | Time | 5.780 | 0.001 | |
| 12 mo | 8.3 (3.6) | 7.0 (3.7) | Group × Time | 2.675 | 0.046 | |
| 18 mo | 8.2 (3.7) | 7.1 (4.0) | ||||
| Total health literacy | Baseline | 24.7 (12.0) | 24.5 (14.8) | Group | 2.695 | 0.10 |
| 6 mo | 27.6 (12.7) | 24.8 (13.6) | Time | 15.153 | 0.000 | |
| 12 mo | 28.2 (12.1) | 24.9 (13.7) | Group × Time | 8.203 | 0.000 | |
| 18 mo | 29.4 (11.4) | 25.3 (13.4) |
Changes in psychosocial/behavioral outcomes.
Indicators of self-efficacy, medication adherence, HBP knowledge, and depression symptoms were improved over time in the intervention group, and the changes were statistically significant (P < 0.05). The intervention and control groups differed significantly in HBP knowledge and level of depression. The intervention group improved in HBP knowledge much more than did the control group (F = 6.89; P = 0.009), resulting in a significant interaction between group and time (F = 5.75; P = 0.001) (Table 4).
Table 4.
Changes in psychobehavioral outcomes from baseline to 18 months (n = 369)
| Outcomes | Time | Intervention | Control | Source | F | P value |
|---|---|---|---|---|---|---|
| mean (SD) | mean (SD) | |||||
| Nonadherence to BP medication, Hill–Bone | Baseline | 9.6 (2.0) | 9.6 (2.0) | Group | 3.470 | 0.06 |
| 6 mo | 9.1 (2.2) | 9.4 (1.9) | Time | 7.284 | 0.000 | |
| 12 mo | 9.1 (1.7) | 9.5 (2.0) | Group × Time | 0.653 | 0.57 | |
| 18 mo | 8.8 (1.4) | 9.2 (1.6) | ||||
| Self-efficacy for BP control | Baseline | 26.5 (3.4) | 26.7 (3.6) | Group | 0.370 | 0.54 |
| 6 mo | 26.6 (3.5) | 26.6 (4.0) | Time | 6.270 | 0.000 | |
| 12 mo | 26.6 (3.2) | 25.4 (3.7) | Group × Time | 5.268 | 0.001 | |
| 18 mo | 25.9 (3.7) | 26.1 (3.9) | ||||
| HBP knowledge | Baseline | 19.4 (2.8) | 18.9 (3.6) | Group | 6.892 | 0.009 |
| 6 mo | 20.1 (3.2) | 19.8 (3.5) | Time | 22.807 | 0.000 | |
| 12 mo | 20.8 (2.7) | 19.3 (3.7) | Group × Time | 5.754 | 0.001 | |
| 18 mo | 20.8 (2.8) | 20.1 (3.2) | ||||
| Depression, PHQ-9 | Baseline | 2.9 (3.5) | 3.0 (3.9) | Group | 1.699 | 0.19 |
| 6 mo | 2.5 (3.0) | 2.5 (3.3) | Time | 2.843 | 0.04 | |
| 12 mo | 2.1 (2.9) | 3.0 (3.0) | Group × Time | 2.809 | 0.04 | |
| 18 mo | 2.5 (3.3) | 2.9 (3.3) |
Abbreviations: BP, blood pressure; HBP, high blood pressure; PHQ-9, 9-item Patient Health Questionnaire.
DISCUSSION
The finding of this research indicated that our multi-modal Self-Help Intervention Program on the Control of HBP intervention had beneficial effects on BP control and management as well as psychosocial well-being in first-generation Korean American seniors. The intervention offers community-based, culturally sensitive HBP management protocols addressing not only urgent needs for education and counseling about HBP control but also practical skills in health literacy and self-care.
Significant BP reductions were found at 6 months in the intervention and control groups. Over 18 months, those reductions were sustained: for systolic BP, reductions of 7.8mm Hg and 4.1mm Hg in the intervention and control groups, respectively; for diastolic BP, reductions of 4.4mm Hg and 3.3mm Hg, respectively. Although these differential BP reductions were modest, a growing body of literature based on population data21,22 confirms the clinical significance of these improvements. For each 2–mm Hg difference in systolic BP, differences in coronary mortality, stroke mortality, and all mortality have been estimated as 4%, 6%, and 3%, respectively.21 When the systolic BP difference increased to 5mm Hg, the estimated reductions in mortality increased to 9%, 14%, and 7%, respectively.21
Significant improvements were also found in self-efficacy, HBP knowledge, and depression in the intervention group. Self-efficacy is important for HBP self-care skills. In one study of Korean American adults, self-efficacy was the most significant predictor of medication taking, weight control, exercise, and healthy diet.22 Self-efficacy has been significantly associated with adherence to medication, increased exercise, and eating a low-salt diet in blacks with HBP23 and with controlled HBP in a sample of Turkish adults.24 However, a longitudinal cohort study of 185 low-income blacks with HBP found that higher self-efficacy seemed to be partially helpful for smoking reduction and increases in physical activity but not for following a low-sodium diet.25 Thus, although self-efficacy may be an important predictor, by itself it may be insufficient for overcoming some barriers to positive HBP self-care. This is consistent with Bandura’s social cognitive theory,26 which depicts behaviors as dynamic, depending simultaneously on self-efficacy, personal attributes, and the environment, such that a change in 1 component has implications for the others. For ethnic minority populations with HBP, self-efficacy is clearly important. However, highly prevalent personal attributes, such as limited health literacy, can directly impact self-care behaviors.
Although knowledge alone may be insufficient for self-management of HBP, it is often basic to BP management and behavior modification, and knowledge improved significantly in the intervention group. Without adequate knowledge, cultural misconceptions about HBP might impede medication adherence and/or delay medical treatment. A study with Korean American adults reported that low knowledge was a strong predictor of intentional medication non adherence, including delay in taking HBP medication.19 The same study suggested that for information-deprived ethnic minority populations, such as new immigrant communities, interventions to improve knowledge about disease management, including possible side effects of medication as well as risks associated with nonadherence, would likely reduce intentional nonadherence to antihypertensive medication and ultimately help prevent devastating complications of uncontrolled HBP.
The improvements in depression in our intervention are also clinically relevant because depression can impact HBP in several ways. Those with depression are less likely to engage in adequate self-care; a secondary analysis of a trial to control HBP in black men found that those who were depressed were less likely to adhere to their medication.27 Depression is also associated with many risk factors for HBP, such as smoking, eating fewer fruits and vegetables, and less physical activity.28,29 Lastly, the lack of energy and exhaustion related to some forms of depression may be uniquely associated with proinflammatory pathways that lead to cardiovascular diseases.30
The positive findings in both primary and secondary outcomes of this study affirm the theoretical tenet of the Self-Help Intervention Program on the Control of HBP that improving HBP-related health literacy should not only improve one’s ability to retain HBP knowledge and BP outcomes but also improve self-efficacy and mood state (e.g., depression).31 Because the majority of Korean American seniors are older immigrants with limited English skills who often suffer from low self-esteem, low self-efficacy, and a high prevalence of depression because of the social isolation that accompanies language barriers, this is an ideal group for implementing this strategy.
Significant BP reductions at 6 months were sustained over 18 months. Until now, empirical evidence of long-term sustained reductions in BP resulting from structured behavioral interventions has been scarce.32 Our results are consistent with those of a previous study that yielded positive BP control using a short-term (6-week) intervention that combined group education, home BP monitoring, and tailored counseling.5 However, it was clear that the initial intervention effect that led to the 68% BP control rate in the intervention group at 12 months was not sustained at the 18-month follow-up: the improvement of BP control was most prominent for the first 12 months, during which the intervention was delivered. No intervention was given from 12 to 18 months, resulting in a 14% erosion of the BP control rate to 54% at 18 months. This finding may suggest a critical time point for booster interventions to sustain the intervention effect.
Another noteworthy finding was that many participants in the control group (10%) also demonstrated lower BP(s) and improved BP control. A possible explanation for this phenomenon might be related to our rigorous outreach efforts to minimize drop-outs in follow-up evaluations. Specifically, answering exhaustive behavioral questionnaires on hypertension knowledge and self-care behaviors also served as an influential intervention in itself for many participants. In fact, a significant number of participants in the control group (n = 23) who were delaying medical treatment and were not on any hypertensive medication at baseline started a medication regimen after they enrolled and had repeated opportunities to respond on those questionnaires at each follow-up data collection. It is reasonable to speculate that these repeated opportunities to consider and evaluate their hypertension management behaviors made them realize that they needed to begin hypertension treatment. This phenomenon, modest but non-negligible improvement of BP outcomes in the control participants, has been observed in other studies.33 When behavioral trials are conducted with resource-scarce communities, such as a low-income ethnic minorities, the very act of being in a study can act as a powerful intervention for some control participants.33
A key and unique feature of our multimodal intervention is the addition of health literacy training. Both print and functional health literacy improved significantly in the intervention group at 6 months and continued to improve incrementally at 12 and 18 months. This contrasts with most other intervention effects, where large gains seen after the first interval are followed by a plateau.
A possible explanation for such incremental improvements is that it takes time for an adult to develop literacy skills in a second or third language. This may be why previous cross-sectional34 and short-term35 studies have fallen short of identifying a direct relationship between health literacy and primary health outcomes. Given time, health literacy skills should produce significant results. Collectively, our findings support the effectiveness of multicomponent strategies in sustaining positive BP outcomes, as well as the long-term benefits of health literacy–enhanced interventions for this vulnerable group.
Nevertheless, this study has several limitations. It was designed as a single-center trial with 1 ethnic minority group. Although this ensured cultural sensitivity, future efforts need to include other ethnic groups to enhance external validity. Because this was translational research done in a community setting, it was also difficult to design a complex factorial study to test independent effects of each intervention component. Specifically, the inability to delineate a precise independent effect of the newly added component of health literacy training may be considered a weakness of this study. In addition, because our heightened interest in examining the process variables, we used a treatment-received analytical model rather than applying the traditional intent-to-treat analysis, which is the gold standard for the statistical reporting of clinical trials. Although we obtained a relatively small noncompliance rate from our intervention group participants and thus the statistical differences that would be obtained in an intent-to-treat analysis might be minimal, we acknowledge that an intent-to-treat analysis might be a more conservative approach for an effectiveness trial regarding outcome evaluation. Lastly, the study lacks cost data: community health workers were an effective way to reach out to participants in the community, and the use of community health workers as primary counselors (with bilingual RN back-up) was expected to reduce the total cost of HBP management in the community. Future studies on cost-effectiveness of using community health workers as interventionists are warranted.
Despite these limitations, our Self-Help Intervention Program on the Control of HBP sheds some light on HBP management strategies in ethnic/linguistic communities. Our study is one of the first community-based HBP behavioral intervention trials to include health literacy skill building for an ethnic/linguistic minority population. Linguistic minorities in the United States are often excluded from intervention research because of their insufficient English skills and low health literacy. Second, our study demonstrates that the appropriate use of community health workers in community-based HBP management programs is a feasible, effective option for strengthening community health infrastructure in some resource-scarce communities.
Given that the US population is becoming more ethnically diverse and older, the findings and methodological lessons from this study should be helpful to clinicians and researchers who are dealing with patients with HBP from many linguistically or culturally isolated ethnic minority communities.
DISCLOSURE
The authors declared no conflict of interest.
ACKNOWLEDGMENTS
This work was supported by a grant from the National Heart, Lung, and Blood Institute (R01 HL085567; Clinical Trials Registry NCT00406614). The authors are grateful for substantial editorial assistance provided by Dr John Bellquist at the Cane Center for Nursing Research, University of Texas at Austin. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1. Stuart-Shor EM, Berra KA, Kamau MW, Kumanyika SK. Behavioral strategies for cardiovascular risk reduction in diverse and underserved racial/ethnic groups. Circulation 2012; 125:171–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Institute of Medicine. Health Literacy: A Prescription to End Confusion. National Academies Press: Washington, DC: The National Academies, 2004 [PubMed] [Google Scholar]
- 3. Kim MT, Song HJ, Han HR, Song Y, Nam S, Nguyen TH, Lee HC, Kim KB. Development and validation of the high blood pressure-focused health literacy scale. Patient Educ Couns 2012; 87:165–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kang JH, Han HR, Kim KB, Kim MT. Barriers to care and control of high blood pressure in Korean-American elderly. Ethn Dis 2006; 16:145–151 [PubMed] [Google Scholar]
- 5. Kim MT, Han HR, Park HJ, Lee H, Kim KB. Constructing and testing a self-help intervention program for high blood pressure control in Korean American seniors-a pilot study. J Cardiovasc Nurs 2006; 21:77––84 [DOI] [PubMed] [Google Scholar]
- 6. Kim MT, Han HR, Hedlin H, Kim J, Song HJ, Kim KB, Hill MN. Teletransmitted monitoring of blood pressure and bilingual nurse counselling-sustained improvements in blood pressure control during 12 months in hypertensive Korean Americans. J Clin Hypertens 2011; 13:605–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Han HR, Kim KB, Kim MT. Evaluation of the training of Korean community health workers for chronic disease management. Health Educ Res 2007; 22:513–521 [DOI] [PubMed] [Google Scholar]
- 8. Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med 2004; 19:1228–1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011; 155:97–107 [DOI] [PubMed] [Google Scholar]
- 10. Loke YK, Hinz I, Wang X, Salter C. Systematic review of consistency between adherence to cardiovascular or diabetes medication and health literacy in older adults. Ann Pharmacother 2012; 46:863–872 [DOI] [PubMed] [Google Scholar]
- 11. Dominick GM, Dunsiger SI, Pekmezi DW, Marcus BH. Health literacy predicts change in physical activity self-efficacy among sedentary Latinas. J Immigr Minor Health 2013; 15:533–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rowlands GP, Mehay A, Hampshire S, Phillips R, Williams P, Mann A, Steptoe A, Walters P, Tylee AT. Characteristics of people with low health literacy on coronary heart disease GP registers in South London: a cross-sectional study. BMJ Open 2013; 3: 1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sentell T, Braun KL. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J Health Commun 2012; 17:82–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 1998; 19:173–202 [DOI] [PubMed] [Google Scholar]
- 15. Rogoza AN, Pavlova TS, Sergeeva MV. Validation of A&D UA-767 device for the self-measurement of blood pressure. Blood Press Monit 2000; 5:227–231 [DOI] [PubMed] [Google Scholar]
- 16. Kim J, Han HR, Song H, Lee J, Kim KB, Kim MT. Compliance with home blood pressure monitoring among middle-aged Korean Americans with hypertension. J Clin Hypertens 2010; 12:253–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. National Heart, Lung, and Blood Institute. Check Your HBPIQ. NIH Publication No. 94–3671. US Government Printing Office: Bethesda, MD, 1994.
- 18. Kim EY, Han HR, Jeong S, Kim KB, Park H, Kang E, Shin HS, Kim MT. Does knowledge matter? Intentional medication nonadherence among middle-aged Korean Americans with high blood pressure. J Cardiovasc Nurs 2007; 22:397–404 [DOI] [PubMed] [Google Scholar]
- 19. Bandura A. Self-efficacy: The Exercise of Control. WH Freeman: New York, 1997 [Google Scholar]
- 20. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stamler R. Implications of the INTERSALT study. Hypertension 1991; 17: I16–I20 [DOI] [PubMed] [Google Scholar]
- 22. Lee JE, Han HR, Song H, Kim J, Kim KB, Kim MT. Correlates of self-care behaviors for managing hypertension among Korean Americans: a questionnaire survey. Int J Nurs Stud 2010; 47:411–417 [DOI] [PubMed] [Google Scholar]
- 23. Warren-Findlow J, Seymor RB, Brunner Huber LR. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health 2012; 37:15–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gozum S, Hacihasanoglu R. Reliability and validity of the Turkish adaptation of medication adherence self-efficacy scale in hypertensive patients. Eur J Cardiovasc Nurs 2009; 8:129–136 [DOI] [PubMed] [Google Scholar]
- 25. Mansyur CL, Pavlik VN, Hyman DJ, Taylor WC, Goodrick GK. Self-efficacy and barriers to multiple behavior change in low-income African Americans with hypertension. J Behav Med 2013; 36:75–85 [DOI] [PubMed] [Google Scholar]
- 26. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977; 84:191–215 [DOI] [PubMed] [Google Scholar]
- 27. Lewis LM, Schoenthaler AM, Ogedegbe G. Patient factors, but not provider and health care system factors, predict medication adherence in hypertensive black men. J Clin Hypertens 2012; 14:250–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Artinian NT, Washington OG, Flack JM, Hockman EM, Jen KL. Depression, stress, and BPin urban African-American women. Prog Cardiovasc Nurs 2006; 21:68–75 [DOI] [PubMed] [Google Scholar]
- 29. Mikkelsen SS, Tolstrup JS, Flachs EM, Mortensen EL, Schnohr P, Flensborg-Madsen TA cohort study of leisure time physical activity and depression. Prev Med 2010; 51:471–475 [DOI] [PubMed] [Google Scholar]
- 30. Davidson KW. Depression and coronary heart disease. ISRN Cardiol 2012; 2012:743813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kim MT, Han HR, Hill MN, Rose L, Roary M. Depression, substance use, adherence behaviors, and BP in urban hypertensive black men. Ann Behav Med. 2003; 26:24–31 [DOI] [PubMed] [Google Scholar]
- 32. Ogedegbe G, Tobin JN, Fernandez S, Gerin W, Diaz-Gloster M, Cassells A, Khalida C, Pickering T, Schoenthaler A, Ravenell J. Counseling African Americans to Control Hypertension (CAATCH) trial: a multi-level intervention to improve BP control in hypertensive blacks. Circ Cardiovasc Qual Outcomes 2009; 2:249–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hill MN, Han HR, Dennison CR, Kim MT, Roary MC, Blumenthal RS, Bone LR, Levine DM, Post WS. Hypertension care and control in underserved urban African American men: behavioral and physiologic outcomes at 36 months. Am J Hypertens 2003; 16:906–913 [DOI] [PubMed] [Google Scholar]
- 34. Powers BJ, Olsen MK, Oddone EZ, Thorpe CT, Bosworth HB. Literacy and blood pressure-do healthcare systems influence this relationship? A cross-sectional study. BMC Health Serv Res 2008; 8:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther 2011; 13:335–341 [DOI] [PMC free article] [PubMed] [Google Scholar]


