Abstract
Introduction:
Pain and tobacco smoking are both highly prevalent and comorbid conditions, and there is reason to believe that pain may pose a barrier to smoking cessation. Although motivation to quit smoking and abstinence self-efficacy have been shown to predict future quit attempts and smoking cessation outcomes, little is known about how these factors may differ as a function of pain status. The goal of the current study was to test cross-sectional relations between past-month pain and self-reported motivation to quit smoking, recent difficulty quitting, and current abstinence self-efficacy.
Methods:
Current daily smokers were recruited from the local community to participate in a laboratory study that included a baseline assessment of recent pain and smoking history.
Results:
Approximately 59% of 132 smokers endorsed past-month pain. Consistent with hypotheses, smokers who endorsed past-month pain reported lower confidence in their ability to remain abstinent and having experienced greater difficulty during their most recent quit attempt (ps < .03). Smokers in pain also endorsed greater motivation to quit and were more than twice as likely (odds ratio = 2.74, 95% confidence interval = 1.28–5.84) to be classified in the contemplation/preparation (vs. precontemplation) stages, relative to pain-free smokers.
Conclusions:
To our knowledge, this is the first study to demonstrate an association between positive pain status, recent difficulty quitting smoking, and reduced self-efficacy for future smoking abstinence. These findings support the utility of assessing pain among all smokers and may help to inform future intervention efforts aimed at helping persons in pain quit smoking.
INTRODUCTION
Pain and tobacco smoking are both highly prevalent and comorbid conditions that are of increasing empirical interest (Ditre, Brandon, Zale, & Meagher, 2011). The prevalence of smoking among persons in pain (e.g., 49%–68%; Jamison, Stetson, & Parris, 1991; Michna et al., 2004) may be greater than twice that observed in the general population (19%; CDC, 2012), and there is some evidence that pain may pose a barrier to smoking cessation. For example, pain has been shown to be a potent motivator of smoking (Ditre & Brandon, 2008), pain patients have readily endorsed smoking to cope with pain (Hooten et al., 2011; Patterson et al., 2012), and there is some evidence that recurring pain may be prospectively linked to poorer abstinence-related outcomes (Waldie, McGee, Reeder, & Poulton, 2008).
Tobacco dependence has been conceptualized as a chronic, relapsing disorder that often requires multiple quit attempts (Fiore et al., 2008). Self-reported motivation to quit smoking has been shown to reliably predict the initiation of quit attempts (e.g., Vangeli, Stapleton, Smit, Borland, & West, 2011), and self-reported confidence in quitting (i.e., abstinence self-efficacy) has been shown to reliably predict duration of smoking abstinence (e.g., Gwaltney, Metrik, Kahler, & Shiffman, 2009; Ockene et al., 2000). Initial evidence suggests that smokers in pain may be no less motivated to quit (Hahn, Rayens, Kirsh, & Passik, 2006) and may be equally likely to engage a quit attempt (Zale & Ditre, 2013), relative to their pain-free counterparts. However, we are not aware of any research that has examined motivation to quit, abstinence self-efficacy, and recent difficulty quitting as a function of past-month pain.
The goal of the current study was to test cross-sectional relations between past-month pain and motivation to quit, abstinence self-efficacy, and recent difficulty quitting, among a sample of daily tobacco smokers recruited from the local community. We hypothesized that smokers who endorsed past-month pain (vs. no past-month pain) would report lower abstinence self-efficacy and having experienced greater difficulty during their most recent quit attempt. Given previous null findings (Hahn et al., 2006), we did not generate an a priori hypothesis with regard to motivation to quit smoking. Finally, we conducted exploratory mediation analyses to test whether recent difficulty quitting may mediate the hypothesized relation between past-month pain and lower abstinence self-efficacy.
METHODS
Participants
The sample consisted of 132 daily tobacco smokers (50% female) who were recruited to participate in a laboratory pain study (Ditre, Heckman, Butts, & Brandon, 2010). Participants were required to be 18–65 years of age, smoke ≥15 cigarettes/day, provide pre-session expired carbon monoxide concentration ≥8 ppm, and not currently using prescription pain medications.
Measures
Pain
Past-month pain was assessed with a single item (“did you (yes/no) experience any bodily pain in the past 4 weeks?”) from the Medical Outcomes Survey (Sherbourne, 1992), which has demonstrated utility as a brief screen for pain among community populations (Greendale, Huang, Karlamangla, Seeger, & Crawford, 2009). Participants who endorsed past-month pain were asked to rate the average intensity of their pain over the past 4 weeks using a 0–10 scale.
Motivation to Quit Smoking
Motivation to quit was assessed via both the contemplation ladder (Biener & Abrams, 1991) and the stages of change (SOC) algorithm (DiClemente et al., 1991). The contemplation ladder is a visual analogue scale, with response options ranging from 0 (no thought of quitting) to 10 (taking action to quit). The SOC algorithm comprises three questions assessing number of past-year quit attempts lasting greater than 24hr and serious consideration of quitting in the next 6 months and 30 days. SOC classifications include precontemplation (no consideration of quitting), contemplation (consideration of quitting in the next 6 months or 30 days, but no past-year 24-hr quit attempt), and preparation (≥1 past-year 24-hr quit attempt and consideration of quitting in the next 30 days). Given the small number of participants who classified in preparation (n = 15), and consistent with previous research (Hahn et al., 2006), the contemplation and preparation groups were combined to produce a dichotomous variable (precontemplation vs. contemplation/preparation).
Abstinence Self-Efficacy
Participants were asked to rate their confidence in remaining abstinent from smoking for 1 week, 1 month, and 1 year, on scales that ranged from 0 (no confidence) to 4 (extremely confident). Responses were averaged to create a composite score of abstinence self-efficacy (e.g., Bandura, Cioffi, Taylor, & Brouillard, 1988).
Recent Difficulty Quitting Smoking
Participants were asked to rate how difficult it was for them to quit smoking during their most recent quit attempt. Responses choices ranged from 0 (easy) to 3 (very difficult). This item has been used in previous research to assess the degree of difficulty experienced by smokers during prior quit attempts (Griffin & Sayette, 2008).
Smoking Characteristics
Participants were asked to report the number of cigarettes smoked per day and the number of years they had been daily smokers. Tobacco dependence was assessed via the widely used Fagerström Test for Nicotine Dependence (Heatherton, Kozlowski, Frecker, & Fagerström, 1991).
Data Analytic Plan
Group differences in smoking and sociodemographic characteristics were tested using t tests and chi-square analyses for continuous and categorical variables, respectively. Participants with past-month pain (vs. no pain) were more likely to be female (χ2 = 8.02, p < .01), and no other differences in sociodemographic or smoking characteristics were observed (ps > .18). Given the observed association with pain status, gender was retained as a covariate in all models. Separate analyses of covariance (controlling for gender) were then conducted with past-month pain status entered as the fixed factor, and contemplation ladder scores, abstinence self-efficacy, and recent difficulty quitting entered as the respective dependence variables. Logistic regression (controlling for gender) was employed to test the association between past-month pain status and SOC (precontemplation vs. contemplation/preparation). Although we tested a gender × pain interaction in each of the models, no interactions were significant (ps > .41), and the gender × pain interaction term was not retained. Finally, mediation analyses were conducted using the INDIRECT macro for SPSS (Preacher & Hayes, 2008) in order to test whether recent difficulty quitting mediated the association between past-month pain and abstinence self-efficacy. The mediation analysis employed a bootstrapping approach with 5,000 resamples and gender as a covariate.
RESULTS
Sample Characteristics
Participants were predominantly White (65.9%) with mean age of 39.58 (SD = 9.91) years. On average, participants reported smoking 25 cigarettes/day (SD = 13.23) and were moderately to highly dependent on tobacco (M = 6.68, SD = 2.06). Approximately 59% of the sample endorsed past-month pain, with an average pain intensity rating of 2.46 (SD = 1.26, range: 0–5). Complete sample characteristics are presented in Table 1.
Table 1.
Sociodemographic and Smoking Characteristics by Pain Status
| Participant characteristics | No past-month pain | Past-month pain | Total sample |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Gender** | |||
| Male | 35 (64.8) | 31 (39.7) | 66 (50.0) |
| Female | 19 (35.2) | 47 (60.3) | 66 (50.0) |
| Race/ethnicity | |||
| White | 33 (61.1) | 54 (69.2) | 87 (65.9) |
| Black | 21 (38.9) | 22 (28.2) | 43 (32.6) |
| American Indian/Alaskan Native | 0 (0) | 2 (2.6) | 2 (1.5) |
| Marital status | |||
| Single | 32 (59.3) | 34 (43.6) | 66 (50.0) |
| Married | 6 (11.1) | 16 (20.5) | 22 (16.7) |
| Separated | 2 (3.7) | 6 (7.7) | 8 (6.1) |
| Widowed | 14 (25.9) | 19 (24.4) | 33 (25.0) |
| Divorced | 0 (0) | 3 (3.8) | 3 (2.3) |
| Education | |||
| Did not graduate high school | 6 (11.1) | 8 (10.3) | 14 (10.6) |
| Graduated high school | 22 (40.7) | 30 (38.5) | 52 (39.4) |
| Some college | 11 (20.4) | 21 (26.9) | 32 (24.2) |
| Technical/associates degree | 12 (22.2) | 14 (17.9) | 26 (19.7) |
| Four years of college | 3 (5.6) | 5 (6.4) | 8 (6.1) |
| Household income | |||
| <20,000 | 49 (37) | 32 (41.1) | 49 (37.1) |
| 20,000–39,999 | 15 (27.8) | 17 (21.8) | 32 (24.2) |
| >40,000 | 8 (14.9) | 13 (16.8) | 21 (15.8) |
| SOC* | |||
| Precontemplation | 29 (53.7) | 26 (33.3) | 55 (41.7) |
| Contemplation/preparation | 25 (46.3) | 52 (66.7) | 77 (58.3) |
| M (SD) | M (SD) | M (SD) | |
| Age | 40.02 (9.70) | 39.27 (10.10) | 39.58 (9.91) |
| Cigarettes/day | 25.48 (13.07) | 24.26 (13.40) | 24.76 (13.23) |
| FTND | 6.52 (2.16) | 6.81 (2.00) | 6.69 (2.06) |
| Years daily smoking | 21.86 (9.33) | 20.90 (10.59) | 21.29 (10.07) |
| Number of past-year 24-hr quit attempts | 1.91 (2.56) | 1.59 (2.32) | 1.72 (2.41) |
| Exhaled CO | 25.07 (10.41) | 26.41 (11.38) | 25.86 (10.97) |
Note. SOC = stages of change; FTND = Fagerström Test for Nicotine Dependence; CO = carbon monoxide measured in parts per million. Household income was not provided by 30 respondents.
*χ2 significant at p < .05. **χ2 significant at p < .01.
Motivation to Quit Smoking
Results indicated that smokers who endorsed past-month pain (vs. no pain) reported greater motivation to quit. Specifically, smokers with past-month pain scored higher on the contemplation ladder (M = 5.60, SD = 2.81) relative to smokers without past-month pain (M = 4.59, SD = 2.77), F(1, 130) = 5.66, p = .02. Smokers in pain were also more than twice as likely to be classified into contemplation/preparation stages, relative to the precontemplation stage (odds ratio = 2.74, 95% CI = 1.28–5.84, p = .01).
Abstinence Self-Efficacy
Self-reported abstinence self-efficacy was observed to be lower among smokers who endorsed past-month pain (M = 0.79, SD = 0.93), relative to smokers who did not endorse past-month pain (M = 1.25, SD = 1.19), F(1, 130) = 5.11, p = .03.
Recent Difficulty Quitting Smoking
Smokers who endorsed past-month pain reported having experienced greater difficulty during their most recent quit attempt (M = 2.51, SD = 0.72), relative to pain-free smokers (M = 2.17, SD = 0.97), F(1, 130) = 4.80, p = .03.
Exploratory Mediation Analyses
As presented in Figure 1, greater difficulty of the most recent quit attempt mediated the association between past-month pain and lower abstinence self-efficacy, 95% CI = (−0.32, −0.01), F(3,128) = 5.33, R 2 = .11, p = .002. Specifically, past-month pain was positively associated with recent difficulty quitting, which, in turn, was negatively associated with self-efficacy for future smoking abstinence. The association between past-month pain and abstinence self-efficacy was reduced to nonsignificance after controlling for recent difficulty quitting.
Figure 1.
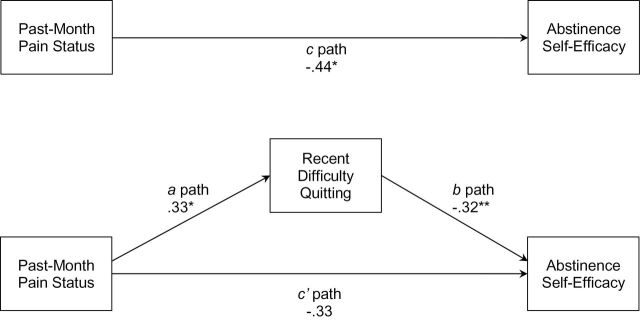
Greater difficulty of the most recent quit attempt as a mediator of the association between positive past-month pain status and lower self-efficacy for future smoking abstinence. The mediational model includes gender as a covariate. The c coefficient represents the total negative association between past-month pain and abstinence self-efficacy. The a and b coefficients represent the mediated path of reduced abstinence self-efficacy through greater difficulty quitting. The c' coefficient represents the nonsignificant association between past-month pain and abstinence self-efficacy, after controlling for the mediated path.**p < .01; *p < .05. All regression coefficients are unstandardized.
DISCUSSION
The goal of the current study was to test cross-sectional relations between past-month pain status and several factors relevant to the initiation and maintenance of smoking cessation. Results indicated that smokers who endorsed past-month pain (relative to no past-month pain) also endorsed greater motivation to quit smoking, having experienced greater difficulty during their most recent quit attempt, and lower confidence in their ability to remain abstinent from smoking. Mediation analyses provided preliminary evidence that previous difficulty quitting may help to explain, in part, why smokers in pain also reported having less confidence in their ability to abstain during future quit attempts. Although mediation analyses were deemed exploratory due to the cross-sectional nature of these data, this interpretation is consistent with evidence that past smoking cessation failures can erode self-efficacy for future quit attempts (Carey & Carey, 1993; Kirchner, Shiffman, & Wileyto, 2012).
These findings are also consistent with previous research indicating that although pain may not diminish motivation to quit smoking (Hahn et al., 2006; Hooten et al., 2011; Zale & Ditre, 2013), some smokers in pain hold concerns about their ability to cope with the additional “stress” of quitting (Hooten et al., 2011). Smokers with comorbid pain disorders readily endorse using tobacco to cope with their pain (Hooten et al., 2011; Patterson et al., 2012), and it is possible that smokers in pain may experience greater difficulty quitting in the absence of more adaptive approaches to pain management (Cooper, Russell, & George, 1988). It is also possible that pain may deplete resources needed to cope with quitting and the early stages of nicotine withdrawal (e.g., Heckman, Ditre, & Brandon, 2012), thus making it more difficult for persons in pain to maintain smoking abstinence.
Strengths of the current study include the assessment of recent pain among a community sample of daily tobacco smokers, biochemical verification of smoking status, and the assessment of several constructs that are relevant to the process of smoking cessation. Several limitations also bear noting. First, the use of cross-sectional data precludes causal interpretations. Second, only past-month pain was assessed, and current use of prescription analgesics was a basis for exclusion. Thus, the current sample may not be representative of smokers with chronic pain, though it may represent a broader segment of the smoking population. Indeed, the prevalence of past-month pain in the current sample (59%) was consistent with previous reports of pain among smokers in the general population (e.g., 56% past-year low-back pain; Palmer, Syddall, Cooper, & Coggon, 2003), and these findings provide additional support for the utility of assessing pain among all smokers, regardless of chronic pain status (e.g., Ditre & Brandon, 2008; Hahn et al., 2006). Third, although we detected statistically significant differences in self-reported motivation to quit, recent difficulty quitting, and abstinence self-efficacy as a function of past-month pain status, some mean differences appear to be small, and the clinical significance of these findings is not yet clear (e.g., Carpenter, Hughes, Solomon, & Callas, 2004).
This is the first study, to our knowledge, to demonstrate associations between pain, recent difficulty quitting, and reduced self-efficacy to abstain from smoking during future quit attempts. These results are largely consistent with the predictions of a reciprocal model of pain and smoking, which posits that both conditions may interact in the manner of a positive feedback loop, resulting in the maintenance of tobacco addiction (Ditre et al., 2011). Future studies would benefit from examining prospective relations between pain, abstinence self-efficacy, and smoking cessation outcomes. Such an approach would allow for the identification of potential mechanisms of action and would further inform intervention development efforts. Indeed, these data suggest that smokers in pain may benefit from interventions designed to enhance abstinence self-efficacy in the context of acute or recurring pain, possibly by enhancing their ability to cope with pain in the absence of smoking.
FUNDING
This work was supported by grant R21DA034285 awarded to JWD by the National Institute on Drug Abuse .
DECLARATION OF INTERESTS
None declared.
REFERENCES
- Bandura A., Cioffi D., Taylor C. B., Brouillard M. E. (1988). Perceived self-efficacy in coping with cognitive stressors and opioid activation. Journal of Personality and Social Psychology, 55, 479–488. 10.1037//0022-3514.55.3.479 [DOI] [PubMed] [Google Scholar]
- Biener L., Abrams D. B. (1991). The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology, 10, 360–365. 10.1037//0278-6133.10.5.360 [DOI] [PubMed] [Google Scholar]
- Carey K. B., Carey M. P. (1993). Changes in self-efficacy resulting from unaided attempts to quit smoking. Psychology of Addictive Behaviors, 7, 219–224. 10.1037/0893-164x.7.4.219 [Google Scholar]
- Carpenter M. J., Hughes J. R., Solomon L. J., Callas P. W. (2004). Both smoking reduction with nicotine replacement therapy and motivational advice increase future cessation among smokers unmotivated to quit. Journal of Consulting and Clinical Psychology, 72, 371–381. 10.1037/0022-006X.72.3.371 [DOI] [PubMed] [Google Scholar]
- CDC. (2012). Current cigarette smoking among adults - United States 2011. Morbidity and Mortality Weekly Report, 61, 889–894 [PubMed] [Google Scholar]
- Cooper M. L., Russell M., George W. H. (1988). Coping, expectancies, and alcohol abuse: A test of social learning formulations. Journal of Abnormal Psychology, 97, 218–230. 10.1037//0021-843X.97.2.218 [DOI] [PubMed] [Google Scholar]
- DiClemente C. C., Prochaska J. O., Fairhurst S. K., Velicer W. F., Velasquez M. M., Rossi J. S. (1991). The process of smoking cessation: An analysis of precontemplation, contemplation, and preparation stages of change. Journal of Consulting and Clinical Psychology, 59, 295–304. 10.1037//0022-006X.59.2.295 [DOI] [PubMed] [Google Scholar]
- Ditre J. W., Brandon T. H. (2008). Pain as a motivator of smoking: Effects of pain induction on smoking urge and behavior. Journal of Abnormal Psychology, 117, 467–472. 10.1037/0021-843X.117.2.467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditre J. W., Brandon T. H., Zale E. L., Meagher M. M. (2011). Pain, nicotine, and smoking: Research findings and mechanistic considerations. Psychological Bulletin, 137, 1065–1093. 10.1037/a0025544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditre J. W., Heckman B. W., Butts E. A., Brandon T. H. (2010). Effects of expectancies and coping on pain-induced motivation to smoke. Journal of Abnormal Psychology, 119, 524–533. 10.1037/a0019568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore M. C., Jaen C. R., Baker T. B., Bailey W. C., Benowitz N. L., Curry S. J., Dorfman S. F. (2008). Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service [Google Scholar]
- Greendale G. A., Huang M. H., Karlamangla A. S., Seeger L., Crawford S. (2009). Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: Results of a randomized controlled trial. Journal of the American Geriatrics Society, 57, 1569–1579. 10.1111/j.1532-5415.2009.02391.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin K. M., Sayette M. A. (2008). Facial reactions to smoking cues relate to ambivalence about smoking. Psychology of Addictive Behaviors, 22, 551–556. 10.1037/0893-164X.22.4.551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwaltney C. J., Metrik J., Kahler C. W., Shiffman S. (2009). Self-efficacy and smoking cessation: A meta-analysis. Psychology of Addictive Behaviors, 23, 56–66. 10.1037/a0013529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn E. J., Rayens M. K., Kirsh K. L., Passik S. D. (2006). Brief report: Pain and readiness to quit smoking cigarettes. Nicotine & Tobacco Research, 8, 473–480. 10.1080/14622200600670355 [DOI] [PubMed] [Google Scholar]
- Heatherton T. F., Kozlowski L. T., Frecker R. C., Fagerström K.-O. (1991). The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction, 86, 1119–1127. 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- Heckman B. W., Ditre J. W., Brandon T. H. (2012). The restorative effects of smoking upon self-control resources: A negative reinforcement pathway. Journal of Abnormal Psychology, 121, 244–249. 10.1037/a0023032 [DOI] [PubMed] [Google Scholar]
- Hooten W. M., Vickers K. S., Shi Y., Ebnet K. L., Townsend C. O., Patten C. A., Warner D. O. (2011). Smoking cessation and chronic pain: Patient and pain medicine physician attitudes. Pain Practice, 11, 552–563. 10.1111/j.1533-2500.2011.00462.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamison R. N., Stetson B. A., Parris W. C. (1991). The relationship between cigarette smoking and chronic low back pain. Addictive Behaviors, 16, 103–110. 10.1016/0306-4603(91)90002-Y [DOI] [PubMed] [Google Scholar]
- Kirchner T. R., Shiffman S., Wileyto E. P. (2012). Relapse dynamics during smoking cessation: Recurrent abstinence violation effects and lapse-relapse progression. Journal of Abnormal Psychology, 121, 187–197. 10.1037/a0024451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michna E., Ross E. L., Hynes W. L., Nedeljkovic S. S., Soumekh S., Janfaza D, … Jamison R. N. (2004). Predicting aberrant drug behavior in patients treated for chronic pain: Importance of abuse history. Journal of Pain and Symptom Management, 28, 250–258. 10.1016/j.jpainsymman.2004.04.007 [DOI] [PubMed] [Google Scholar]
- Ockene J. K., Emmons K. M., Mermelstein R. J., Perkins K. A., Bonollo D. S., Voorhees C. C., Hollis J. F. (2000). Relapse and maintenance issues for smoking cessation. Health Psychology, 19, 17–31. 10.1037//0278-6133.19.Suppl1.17 [DOI] [PubMed] [Google Scholar]
- Palmer K. T., Syddall H., Cooper C., Coggon D. (2003). Smoking and musculoskeletal disorders: Findings from a British national survey. Annals of the Rheumatic Diseases, 62, 33–36. 10.1136/ard.62.1.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson A. L., Gritzner S., Resnick M. P., Dobscha S. K., Turk D. C., Morasco B. J. (2012). Smoking cigarettes as a coping strategy for chronic pain is associated with greater pain intensity and poorer pain-related function. The Journal of Pain, 13, 285–292. 10.1016/j.jpain.2011.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K. J., Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Sherbourne C. D. (1992). Pain measures. In Stewart A. L., Ware J. E. (Eds.), Measuring functioning and well-being: The medical outcomes study approach (pp. 220–234). Durham, NC: Duke University Press [Google Scholar]
- Vangeli E., Stapleton J., Smit E. S., Borland R., West R. (2011). Predictors of attempts to stop smoking and their success in adult general population samples: A systematic review. Addiction (Abingdon, England), 106, 2110–2121. 10.1111/j.1360-0443.2011.03565.x [DOI] [PubMed] [Google Scholar]
- Waldie K. E., McGee R., Reeder A. I., Poulton R. (2008). Associations between frequent headaches, persistent smoking, and attempts to quit. Headache, 48, 545–552. 10.1111/j.1526-4610.2007.01037.x [DOI] [PubMed] [Google Scholar]
- Zale E. L., Ditre J. W. (2013). Associations Between Chronic Pain Status, Attempts to Quit Smoking, and Use of Pharmacotherapy for Smoking Cessation. Psychology of Addictive Behaviors. Advance online publication. 10.1037/a0032515 [DOI] [PMC free article] [PubMed] [Google Scholar]


