Abstract
Meningioma rarely gives rise to metastases outside the brain and meninges. We report here a case of a patient who was treated for anaplastic brain meningioma with surgery and fractionated radiation therapy without any recurrence until 5 years after the operation, when she developed vertebral metastases.
Keywords: MR imaging, radiation therapy, brain, spine
Meningiomas are neoplasms of the central nervous system derived from meningothelial cells. These neoplasms account for 14–19% of intracranial tumors (1). Most meningiomas are benign and surgery is curative in the majority of cases. However, malignant meningiomas are more aggressive (with 5-year survival rates in the range of 50–60% versus 90–100% in benign meningiomas), tend to recur earlier, and invade the surrounding structures of the scull and the brain (with interval to recurrence estimated at 3.5 years versus 7.5 years in benign meningiomas) (2). Despite their malignancy, extracranial metastases of malignant meningiomas are rare with an estimated incidence of 1–5 out of 1000 cases (2). Only 7% involve vertebrae and just a few cases have been reported in the literature (3). We present here an unusual case of a patient who was treated for an anaplastic brain meningioma originally diagnosed in 2007 and treated by complete surgical resections and radiotherapy, with complete recovery for 5 years, after which she developed vertebral metastases.
Case report
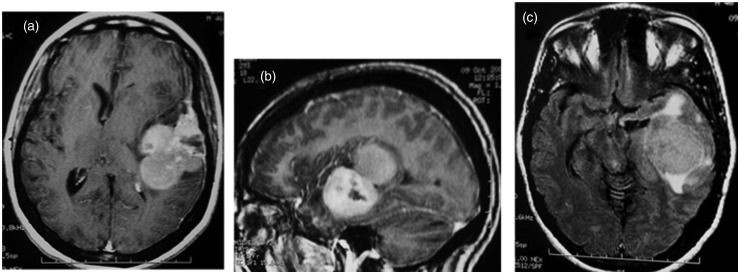
The report involves a 51-year-old woman who presented in 2007 with a clinical history of headache, nausea, and vomiting. The initial cranial computed tomography (CT) and magnetic resonance imaging (MRI) showed a left parieto-temporal dural-based infiltrating tumor. The mass was mushrooming on the outer edge and had a heterogenous enhancement (Fig. 1a and b) with necrosis, central calcifications, marked edema (Fig. 1c), and bone destruction.
Fig. 1.
MRI: left parieto-temporal dural-based infiltrating tumor. The mass had an heterogenous enhancement (a, b) with necrosis, and marked edema (c).
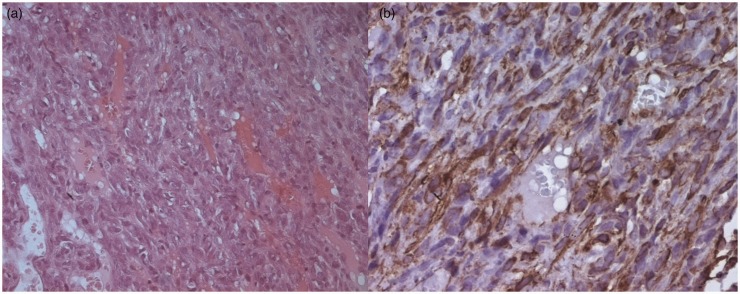
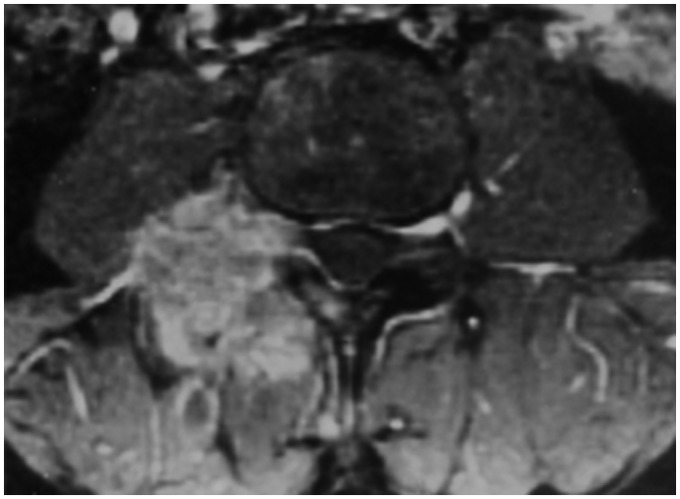
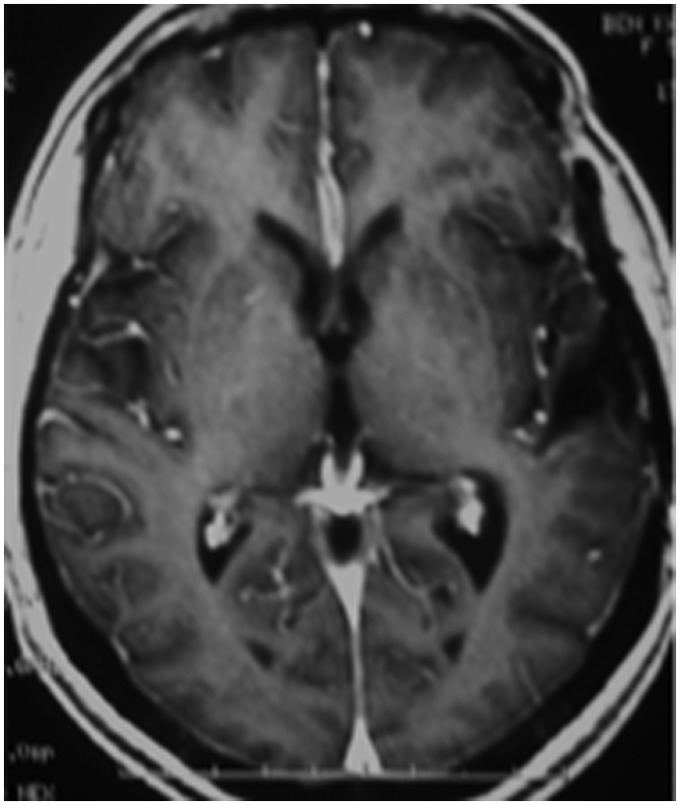
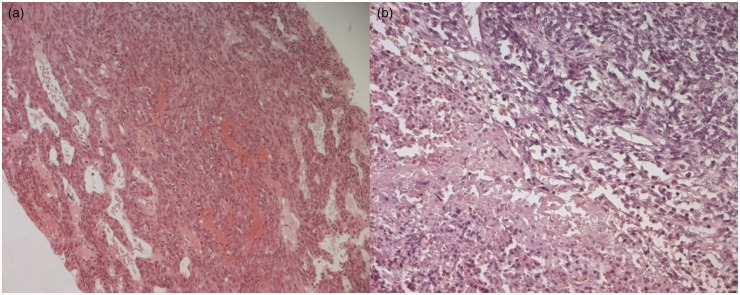
The patient underwent a complete surgical resection. Histological diagnosis revealed an anaplastic meningioma (World Health Organization [WHO] grade III) with hypercellularity and a prominent mitotic activity with around 32 mitoses per 10 high power fields (hpf) (Fig. 2a and b). The postoperative course was uneventful and the patient was discharged. The operation was followed by fractionated radiation therapy. At the follow-up during the next 4 years, the patient presented in good condition and MRI showed no tumor recurrence. In March 2012, the patient developed a progressively invalidating lumbar pain. Spinal MRI showed a slightly circumscribed mass within the right transverse process of the third thoracic vertebra (T3) with paravertebral extension to surrounding soft tissue (Fig. 3). Brain MRI showed no recurrence of the intracranial meningioma (Fig. 4).
Fig. 2.
Histological diagnosis (hematoxylin and eosin HE x 200) anaplastic meningioma with hypercellularity and a prominent mitotic activity with around 32 mitoses per 10 hpf (a). Tumor cells display strong immunoreactivity for CD 99 (b).
Fig. 3.
Spinal MRI: circumscribed mass within the right transverse process of the third thoracic vertebra (T3) with paravertebral extension to the soft tissues.
Fig. 4.
Brain MRI: no recurrence of the intracranial meningioma.
A percutaneous transpedicular biopsy was performed and the histological findings were identical to those found in 2007 (Fig. 5a and b). The patient was given palliative radiotherapy for bone metastases but she died 3 months later due to pulmonary embolism.
Fig. 5.
The CT-guided biopsy of the vertebral mass revealed a metastasis of a meningioma: hypercellularity with prominent mitotic activity (hematoxylin and eosin HE x 100) with area of necrosis.
Discussion
Meningioma is one of the most frequently encountered tumors of the central nervous system consisting of meningoepithelial cells and it generally originates from intracranial meninges (4). These tumors are most commonly reported in elderly patients with peak incidence in the seventh decade of life. There is a clear bias towards women with a female:male ratio of about 2:1. Less common subtypes and high-grade meningiomas are over-represented in men and children. Jaaskelainen et al. found in their study of 936 patients that meningiomas with histologic anaplasia occurred in 12% of the men versus 4% of the women (5). In children, 7–16% of meningiomas are malignant, and the prevalence of malignancy decreases with increasing age (6). Although most meningiomas are benign, they have a broad spectrum of clinical characteristics, and histologically distinct subsets are associated with high risk of recurrence, even after apparent complete resection. In rare instances, meningiomas are malignant (7). According to WHO criteria, there are three grades of histopathological subtypes of meningiomas: meningioma; atypical meningioma; and malignant meningioma. Atypical and malignant meningiomas (only 1.7–4.2% of all meningiomas) differ from benign lesions according to several histological features, such as increased mitotic activity (>4 mitotic figures in atypical and >20 mitoses in malignant, per 10 hpf), increased cell density, presence of nuclear pleomorphism, loss of architectural cell disposition, existence of tumoral necrosis and brain invasion, papillary transformation and carcinoma, melanoma, or sarcomatous appearance (Table 1). Type II (atypical, clear cell, and choroid variants) and III (rhabdoid, papillary, and anaplastic variants), and the presence of brain invasion in either benign or malignant meningiomas, seem to favor metastatic spread (8,9). Immunohistochemical analyses of a nuclear protein related to cell proliferation, Ki-67 proliferative index, or of molecular markers such as CDKN2A deletion, along with a 9p21 deletion, are also useful in evaluating the potential of meningioma recurrence and/or metastases (4). In addition to proliferative index, primary tumor appearance on imaging may be useful. Some radiological indicators such as mushrooming, non-homogenous enhancement, peritumoral edema, osteolysis, intrinsic cyst-like areas, and indistinct tumor-brain borders have been proposed as providing important clues about the malignancy (10,11).
Table 1.
Summary of the 2007 WHO grading scheme for meningiomas (4).
| WHO grade | Histological subtype | Histological features |
|---|---|---|
| I (benign) | Meningothelial, fibroblastic, transitional, angiomatous, microcystic, secretory, lymphoplasmacytic metaplastic, psammamatous | Does not fulfill criteria for grades II or III |
| II (atypical) | Chordoid, clear cell | Four or more mitotic cells per 10 hpf and/or three or more of the following: increased cellularity, small cells, necrosis, prominent nucleoli, sheeting and/or brain invasion in an otherwise grade I tumor |
| III (anaplastic/malignant) | Papillary, rhabdoid | Twenty or more mitoses per 10 hpf and/or obviously malignant cytological characteristics such that tumor cell resembles carcinoma, sarcoma, or melanoma |
Extracranial metastases of meningiomas are rare. The most common sites of metastases of meningiomas are the lungs (60%) (12), followed by the abdomen and liver (34%), cervical lymph nodes (18%), long bones, pelvis and skull (11%), pleura (9%), central nervous system (7%), and mediastinum (5%). The kidneys, bladder, thyroid, breasts, thymus, heart, skin, vulva, adrenal glands, and eyes are only occasionally affected (13, 14). Only 7% occur in the vertebrae. A few cases of spinal metastases have been published to date. Some of them were intra-arachnoidian and others were intraosseous; located in C-2 (15), T-1 (16), T-10 (17), T-11 (8), L-2 (17), L-5 (18), and sacrum (19). They can even be multiple. Distant metastases from benign meningiomas are extremely rare (1,20). However, the rate of distant metastases could reach 5% for atypical and 30% for anaplastic or malignant meningiomas (1,2,11). The mechanism of systemic spread is not yet known, but a passage of tumor through venous sinuses and channel is discussed in the literature (8,11,17). Surgical removal may also increase the risk of iatrogenic metastases of meningiomas with atypical histology, and malignant meningiomas could even disseminate without previous surgery (21,22). An intracranial lesion usually recurs locally several times before it metastasizes. This interval appears to be shorter for atypical and malignant tumors (about 1 year) compared to benign lesions (>5 years). The explanation for this variety remains unclear. There is quite a variable latency period between the diagnosis of the intracranial tumor and the appearance of the metastasis, ranging from a few months to >20 years (8). In our case, there were 5 years between the tumor resection and the vertebral metastasis.
Our case report is unusual because the patient developed distance metastases without intracranial recurrence of the meningioma. Factors that suggest the ability to metastasize include previous intracranial surgery and especially malignant histological grading.
Currently, to our knowledge, no consensus guidelines exist for treatment of metastasizing meningiomas (23). Treatment options available for metastatic disease of the spine include medical therapy, surgery, and radiation. Operative intervention is most often palliative with pain control, maintenance of neurologic function, and spinal stability as primary goals. For years, many considered that surgery is the best initial therapy, with the goal of gross total resection. Realistically, such an aggressive approach requires en bloc resection: it is rarely indicated in vertebral metastases, but can be considered for single lesions with a good prognosis (8,24,25). There is no proven effective chemotherapy agent for treating metastasizing meningiomas. In some studies irinotecan and hydroxyurea have had a marginal response. Progress in identifying alternative forms of therapy for patients with these metastases has been limited by poor understanding of the molecular pathogenesis of meningiomas and of the critical molecular changes driving tumor growth, as well as by the lack of meningioma cell lines and tumor models for preclinical studies (26). Extracranial bone metastases and multiple extracranial metastases of meningiomas predict poor prognosis (2).
In conclusion, although uncommon, vertebral metastases of meningiomas should always be included in the differential diagnosis in patients with a history of meningioma who developed lesions suggestive of distant metastases, especially patients who had malignant intracranial meningioma.
References
- 1.Abboud M, Haddad G, Kattar M, et al. Extraneural metastases from cranial meningioma: a case report. Radiat Oncol 2009; 4: 20–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Modha A, Gutin PH. Diagnosis and treatment of atypical and anaplastic meningiomas: a review. Neurosurgery 2005; 57: 538–550 [DOI] [PubMed] [Google Scholar]
- 3.Enam SA, Abdulrauf S, Mehta B, et al. Metastasis in meningioma. Acta Neurochir 1996; 138: 1172–1178 [DOI] [PubMed] [Google Scholar]
- 4.Fabi A, Nuzzo C, Vidiri A, et al. Bone and lung metastases from intracranial meningioma. Anticancer Res 2006; 26: 3835–7383 [PubMed] [Google Scholar]
- 5.Jaaskelainen J, Haltia M, Servo A. Atypical and anaplastic meningiomas: radiology, surgery, radiotherapy, and outcome. Surg Neurol 1986; 25: 233–242 [DOI] [PubMed] [Google Scholar]
- 6.Greenberg SB, Schneck MJ, Faerber EN, et al. Malignant meningioma in a child: CT and MR findings. Am J Roentgenol 1993; 160: 1111–1112 [DOI] [PubMed] [Google Scholar]
- 7.Riemenschneider MJ, Perry A, Reifenberger G. Histological classification and molecular genetics of meningiomas. Lancet Neurol 2006; 5: 1045–1054 [DOI] [PubMed] [Google Scholar]
- 8.López D, Martín-Velasco V, Díez C, et al. Metastatic meningioma to the eleventh dorsal vertebral body: total en bloc spondylectomy. Case report and review of the literature. Neurocirugia 2006; 17: 240–249 [DOI] [PubMed] [Google Scholar]
- 9.Yang SY, Park CK, Park SH, et al. Atypical and anaplastic meningiomas: prognostic implications of clinicopathological features. J Neurol Neurosurg Psychiatry 2008; 79: 574–580 [DOI] [PubMed] [Google Scholar]
- 10.Azene EM, Gai QW, Tabar SP, et al. Metastasis of a histologically benign–appearing meningioma to the iliac bone. J Clin Oncol 2008; 26: 4688–4690 [DOI] [PubMed] [Google Scholar]
- 11.Chan Lee G, Choi SW, Seon-Hwan K, et al. Multiple Extracranial Metastases of Atypical Meningiomas. J Korean Neurosurg Soc 2009; 45: 107–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yekeler E, Dursun M, Yilmazbayhan D, et al. Multiple pulmonary metastases from intracranial meningioma: MR imaging findings (case report). Diagn Interv Radiol 2005; 11: 28–30 [PubMed] [Google Scholar]
- 13.Figueroa BE, Quint DJ, Keever PE, et al. Extracranial metastatic meningioma. Br J Radiol 1999; 72: 513–516 [DOI] [PubMed] [Google Scholar]
- 14.Yacoub M, Naccache JM, Kujas M, et al. Isolated pleural metastases from an atypical meningioma. Rev Mal Respir 2003; 20: 433–436 [PubMed] [Google Scholar]
- 15.Tominaga T, Koshu K, Narita N, et al. Metastatic meningioma to the second cervical vertebral body: a case report. Neurosurgery 1994; 34: 538–540 [DOI] [PubMed] [Google Scholar]
- 16.Fuentes S, Metellus P, Bouvier C, et al. Metastatic meningioma to the first thoracic vertebral body. A case report and review of the literature. Neurochirurgie 2002; 48: 53–56 [PubMed] [Google Scholar]
- 17.Tournat H, Huchet A, Ouhabrache N, et al. Bone metastatic evolution of a recurrent meningioma: case report. Cancer/Radiothérapie 2006; 10: 590–594 [DOI] [PubMed] [Google Scholar]
- 18.Palmer JD, Cook PL, Ellison DW. Extracranial osseous metastases from intracranial meningioma. Br J Neurosurg 1994; 8: 215–218 [DOI] [PubMed] [Google Scholar]
- 19.Lee YY, Wen-Wei H, Huang TJ, et al. Metastatic meningioma in the sacrum: a case report. Spine 2002; 27: 100–103 [DOI] [PubMed] [Google Scholar]
- 20.Som PM, Sacher M, Strenger SW, et al. “Benign” metastasizing meningiomas. Am J Neuroradiol 1987; 8: 127–130 [PMC free article] [PubMed] [Google Scholar]
- 21.Cramer P, Thomale UW, Okuducu AF, et al. An atypical spinal meningioma with CSF metastasis: fatal progression despite aggressive treatment. Case report. J Neurosurg Spine 2005; 3: 153–158 [DOI] [PubMed] [Google Scholar]
- 22.Garcia-Conde M, Roldan-Delgado H, Martel-Barth-Hansen D, et al. Anaplastic transformation of an atypical intraventricular meningioma with metastases to the liver: case report. Neurocirugia 2009; 20: 541–549 [PubMed] [Google Scholar]
- 23.Taieb G, Campello C, Renard D, et al. Multifocal extracranial meningioma metastases. Arch Neurol 2011; 68: 388–389 [DOI] [PubMed] [Google Scholar]
- 24.Ecker RD, Endo T, Wetjen NM, et al. Diagnosis and treatment of vertebral column metastases. Mayo Clin Proc 2005; 80: 1177–1186 [DOI] [PubMed] [Google Scholar]
- 25.Gasbarrini A, Cappuccio M, Mirabile L, et al. Spinal metastases: treatment evaluation algorithm. Eur Rev Med Pharmacol Sci 2004; 8: 265–274 [PubMed] [Google Scholar]
- 26.Norden AD, Drappatz J, Wen PY. Targeted drug therapy for meningiomas. Neurosurg Focus 2007; 23: 12–12 [DOI] [PubMed] [Google Scholar]