Abstract
Angioleiomyomas are benign smooth muscle tumors that originate from the tunica media of veins and arteries. They can occur anywhere in the body, but the preferential location of these tumors is the lower extremities. We describe a rare case of rectal angioleiomyoma and present our findings obtained by using computed tomography, magnetic resonance imaging, and histopathological analysis.
Keywords: Rectal angioleiomyoma, rectal vascular leiomyoma, computed tomography (CT), magnetic resonance imaging (MRI)
Introduction
Angioleiomyomas are formed by the proliferation of smooth muscle cells in the vascular wall. They appear as skin or subcutaneous nodules in the extremities (1) and rarely develop in organs other than the skin. To the best of our knowledge, only one case of rectal angioleiomyoma has been reported in the English literature (2); however, in that case, the tumor was not described radiologically. Therefore, our case report is the first description of the radiological findings of a rectal angioleiomyoma. Herein, we report the radiological imaging findings in a patient with a primary rectal angioleiomyoma histopathologically confirmed after surgery.
Case report
A 47-year-old man was referred to the Radiology Department of our hospital for further evaluation of a pelvic mass that was first noticed during an abdominal computed tomography (CT) examination as part of an evaluation for hematuria. He had no history of illness; a physical examination did not reveal any specific findings. The results of the laboratory analyses were within normal limits, except for a slight decrease in the hemoglobin level (10.9 g/dL) and a 2–3 red blood cell count of 2–3 million cells/mm red blood cell counts of 2–3 million cells/mm3on urinalysis.
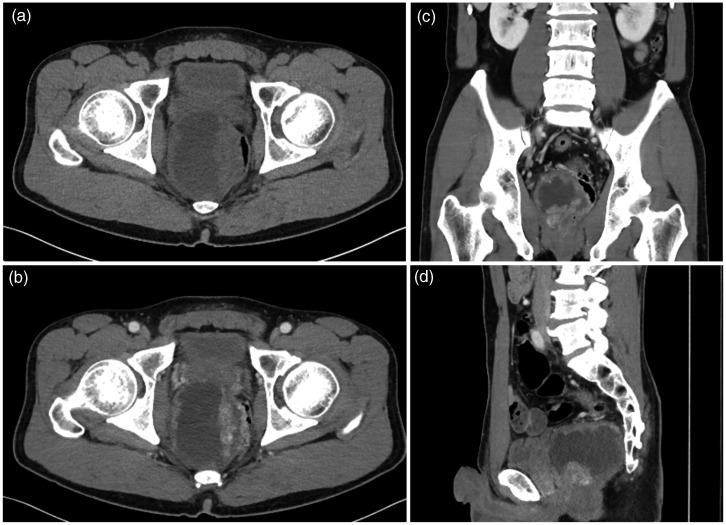
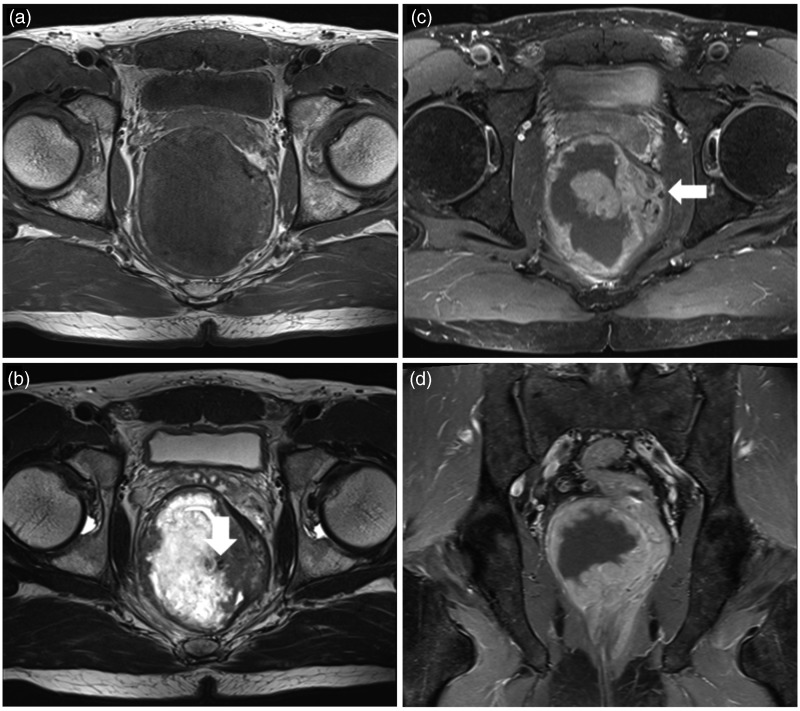
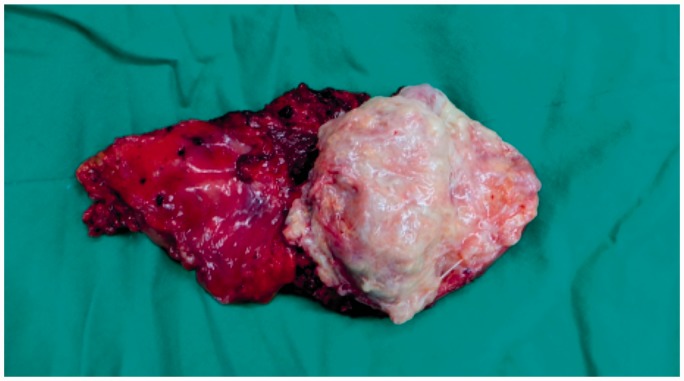
An unenhanced CT scan revealed a well-demarcated, heterogeneous large mass measuring 6 × 7 × 8 cm in the pelvis on the right side of the rectum (Fig. 1a). After i.v. injection of a contrast medium, the mass contained a non-enhanced, low-attenuated central area with a peripheral nodular-enhancing solid portion (Fig. 1b–d). Multiple avidly enhanced dot-like or tubular structures were also observed at the peripheral solid portions of the tumor. Suspecting a rectal or retroperitoneal tumor, we performed pelvic magnetic resonance imaging (MRI) with a 3-Tesla magnet (Magnetom Verio 3.0 T, Siemens Medical Systems, Erlangen, Germany) to better demonstrate the origin and extent of the mass. Magnetic resonance imaging (MRI) revealed that the tumor was located in the pelvic retroperitoneal space between the seminal vesicles and the rectum. A T1-weighted (T1W) MRI scan revealed a low-signal area at the central portion of the tumor with an area of iso-signal intensity at the peripheral portions compared with the intensity of the pelvic muscle (Fig. 2a). T2-weighted (T2W) MRI scans revealed that the outer margins of the tumor displayed a continuation of the hypointense layer of the muscularis propria of the rectum. In addition, the tumor had a beak sign on the surface in contact with the rectum. The tumor had well-defined margins and contained a central prominent high-intensity portion presumably due to myxoid or hyaline degeneration; it had a peripheral solid portion that showed slightly higher intensity than the pelvic muscles. The serpiginous curvilinear signal voidings were indicative of an abnormal increase in the vascularity at the peripheral solid portions of the mass (Fig. 2b). Postcontrast T1W MRI scans revealed peripheral enhancement of the tumor, except in the central areas of the presumed necrosis or the portion with hyaline degeneration (Fig. 2c and d). The differential diagnosis included a submucosal tumor or gastrointestinal stromal tumor (GIST) originating from either the rectum or a primary retroperitoneal tumor. Therefore, considering the positive beak sign with the continuation of the hypointense layer of the rectum, the diagnosis of a tumor in the rectum was made. The patient underwent surgery, which revealed an 8 × 5 × 4 cm whitish solid mass that was adhered to the rectum (Fig. 3).
Fig. 1.
Abdominal CT scan at the level of the pelvis showing a large mass at the right aspect of the rectum. The axial non-enhanced CT scan (a) shows a heterogeneous mass with a central low-attenuated portion and peripheral soft-tissue–attenuated components. The axial enhanced CT scans in the axial (b), coronal (c), and sagittal (d) planes show contrast enhancement at the peripheral solid portion, with an avidly enhanced dot-like or tubular structure suggesting a vascular component.
Fig. 2.
MRI scans of the pelvis obtained with a 3.0-T MRI instrument showing a large mass at the right aspect of the rectum. The axial T1W (a) and T2W (b) scans show a heterogeneous large mass. The mass has a hypersignal intense area on the T2W scan that suggests hyaline or myxoid changes. Tortuous and tubular signal void structures that represent a dilated tortuous vessel are visible at the peripheral solid portion of the mass (arrow). Contrast-enhanced MRI scans in the axial and coronal planes (c, d) showing peripheral enhancement of the mass with tubular or dot-like enhanced vascular structures. Some vessels show signal voiding because of their high flow (arrow).
Fig. 3.
Gross specimen of the resected tumor showing myxoid or hyaline change degeneration of the whitish central portion with prominent vascular structures.
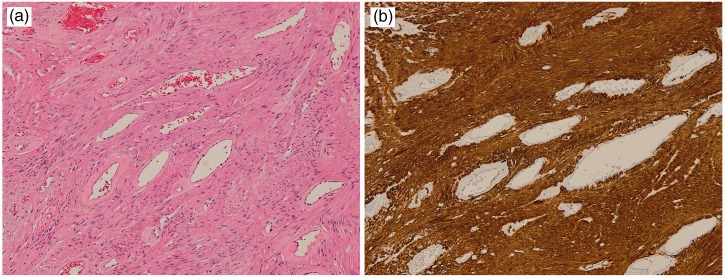
Histopathological examination revealed that the mass was located at the submucosal layer of the rectum with intact mucosa. The central portion of the tumor displayed myxoid change and hyalinization. Microscopic observation revealed the presence of numerous thick-walled blood vessels with intervening spindle cells. Mitotic activity and nuclear atypia were nearly absent, which indicated the benign nature of the tumor. Immunohistochemical analysis revealed that the cells of the thick-walled blood vessels and the myxoid intervascular components exhibited strong staining for smooth muscle actin, but were negative for C-kit, DOG1, and S-100 protein. The C-kit and DOG1 negativity excluded the diagnosis of GIST, whereas the S-100 protein negativity excluded a peripheral nerve sheath tumor. The numerous blood channels were clearly visualized by observing the positivity of the epithelioid cells for CD34 (Fig. 4). On the basis of these results, the tumor was diagnosed as an angioleiomyoma of the rectum.
Fig. 4.
(a) photomicrograph of a specimen showing numerous thickened vascular channels with proliferation of the smooth muscle cells. (b) photomicrograph of a specimen showing positive immunohistochemical staining for smooth muscle actin.
Discussion
Angioleiomyomas are benign tumors that can be interpreted as mixed tumors with muscular and vascular components. They originate from muscular tissue within the blood vessel wall, most often from the walls of veins. They can occur anywhere in the body, but they are most often observed in the extremities, particularly the lower leg. They usually occur as solitary subcutaneous lesions at the lower extremities of middle-aged women (3,4).
Primary angioleiomyomas are rare in the gastrointestinal tract; however, when they do occur, they mostly appear in the stomach and small intestine, but are much less common in the esophagus and colon. Primary angioleiomyomas of the rectum are even rarer. To the best of our knowledge, only one case of rectal angioleiomyoma has been reported in the English literature (2); however, that report did not describe any radiological findings.
Angioleiomyomas are histologically classified as solid, venous, and cavernous (5). The subdivisions are according to the degree of the smooth muscle distribution and vascular cavities of different shapes. The most common type is the solid type, which has closely compacted smooth muscles and many small, slit-like vascular channels. Myxoid and hyaline degeneration are sometimes observed because of circulatory disturbances (6).
Previous reported imaging findings of angioleiomyoma have been non-specific. According to a previous study, angioleiomyomas show mixed areas with slightly hyper- and iso-intense portions compared with the intensity of skeletal muscles on T2W MRI scans. After the intravenous administration of a contrast material, slightly hyperintense areas showed strong enhancement, although the iso-intense areas on the T2W MRI scans did not show enhancement. The hyperintense areas on the T2W MRI scans correspond to the smooth muscle bundle cells, and the iso-intense areas correlate with the fibrous tissue or intravascular thrombi. In addition, the well-defined peripheral hypointense area on the T2-weighted scans corresponding to the fibrous capsule (7). In another report, MRI findings revealed tortuous vascular channels surrounded by smooth muscle bundles that corresponded to the tortuous low-signal intensity on the T1W scans, suggestive of a diagnosis of angioleiomyoma (8).
Another characteristic finding in imaging studies of angioleiomyoma is the heterogeneity of the solid portion of the tumor on T2W scans. These findings are explained by the microscopic heterogeneity of the tumor with the presence of tortuous vascular channels surrounded by smooth muscle bundles and areas of myxoid change (9). The myxoid change or hyalinization show higher signal intensity on the T2W scans because the loose cellularity with edematous change may have prolong the relaxation time during T2W MRI. Similarly, in this case, the tumor showed heterogeneous high-signal intensity on the T2W scans because of the central portion of the myxoid change and the hyalinization. Serpiginous, curvilinear signal voiding vascular structures were also observed at the peripheral solid portion of the tumor.
Clinically, the major differential diagnosis of perirectal and retroperitoneal spaces includes a primary or secondary tumor arising from either the rectum or other primary retroperitoneal tumors.
In conclusion, rectal angioleiomyoma should be considered as a possible diagnosis when a well-demarcated mass of heterogeneous high-signal intensity and an adjacent tortuous vascular structure with a positive beak sign on the surface in contact with the rectum are seen in the perirectal and retroperitoneal spaces observed on T2W scans.
Conflict of interest
None declared.
References
- 1.Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer 1984; 54: 126–130. [DOI] [PubMed] [Google Scholar]
- 2.Stanojević GZ, Mihailović DS, Nestorović MD, et al. Case of rectal angioleiomyoma in a female patient. World J Gastroenterol 2013; 19: 2114–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freedman AM, Meland NB. Angioleiomyomas of the extremities: report of a case and review of the Mayo Clinic experience. Plast Reconstr Surg 1989; 83: 328–331. [PubMed] [Google Scholar]
- 4.Duhig JT, Ayer JP. Vascular leiomyoma: a study of 61 cases. Arch Pathol 1959; 68: 424–430. [PubMed] [Google Scholar]
- 5.Morimoto N. Angiomyoma. A clinicopathologic study. Med J Kagoshima Univ 1973; 24: 663–683. [Google Scholar]
- 6.Hasegawa T, Seiki K, Yang P, et al. Mechanism of pain and cytoskeletal properties in angioleiomyomas: an immunohistochemical study. Pathol Int 1994; 37: 61–64. [DOI] [PubMed] [Google Scholar]
- 7.Hwang JW, Ahn JM, Kang HS, et al. Vascular leiomyoma of an extremity: MR imaging-pathology correlation. Am J Roentgenol 1998; 171: 981–985. [DOI] [PubMed] [Google Scholar]
- 8.Kinoshita T, Ishii K, Abe Y, et al. Angiomyoma of the lower extremity: MR findings. Skeletal Radiol 1997; 26: 443–445. [DOI] [PubMed] [Google Scholar]
- 9.Yoo HJ, Choi JA, Chung JA, et al. Angioleiomyoma in soft tissue of extremities: MRI findings. Am J Roentgenol 2009; 192: W291–W294. [DOI] [PubMed] [Google Scholar]