Abstract
Rothia spp. are gram-positive pleomorphic bacteria that are part of the normal oral microflora. They are associated with dental and periodontal disease, although systemic infections have also been reported. We describe the case of a 75-year-old lady with rheumatoid arthritis who presented with prosthetic knee joint infection due to Rothia aeria. We discuss its identification and the evidence regarding association of dental disease with Rothia spp. joint infections based on available literature.
Keywords: Identification, infection, joint, prosthetic, Rothia aeria, treatment
Introduction
Rothia spp. are gram-positive pleomorphic bacteria that are part of the normal oral microflora. They are associated with dental and periodontal disease [1,2]. The first description of disease in humans due to Rothia species was reported in 1975 in a case of peri-appendiceal abscess [3].
More recently a number of case reports have described Rothia species as causing native and prosthetic endocarditis [4,5] and other rare infections, including endophthalmitis [6,7], corneal infections [8], peritoneal infections [9] and sepsis in an immunocompromised patient [10] and a neonate [11].
Case Report
A 75-year-old lady with a history of seronegative erosive rheumatoid arthritis since 1972 presented with painful swelling of the right knee. She had bilateral knee replacements. The right knee replacement was carried out in 1993 and the left one in 2003. Her other co-morbidities included asthma, arterial hypertension and chronic kidney disease. She was on drug therapy for treatment for the above conditions and also on methotrexate 12.5 mg once weekly and prednisolone 7.5 mg once a day, for more than 10 years. She had also undergone multiple hand and wrist surgeries. She did not have any history of trauma or previous knee infections.
On examination, body temperature was 38°C. Examination showed swelling, erythema and tenderness of the knee and upper calf. The initial blood tests showed white blood cells = 25.7 × 109/L, neutrophils = 24.4 × 109/L, C-reactive protein = 144 mg/L (normal <10 mg/L). Joint fluid aspirate contained 49 600 × 106 white blood cells/L with 90% neutrophils. Microscopy showed gram-positive bacilli and a culture grew bacteria (Fig. 1). Identification of this isolate was performed by API Coryne (Biomérieux, Marcy l'Etoile, France). The isolate was initially identified as Rothia dentocariosa with a profile of 7050121. This isolate was then sent to the Health Protection Agency Regional reference laboratory in Colindale, London, UK and was identified as Rothia aeria by 16S rRNA sequencing.
Figure 1.
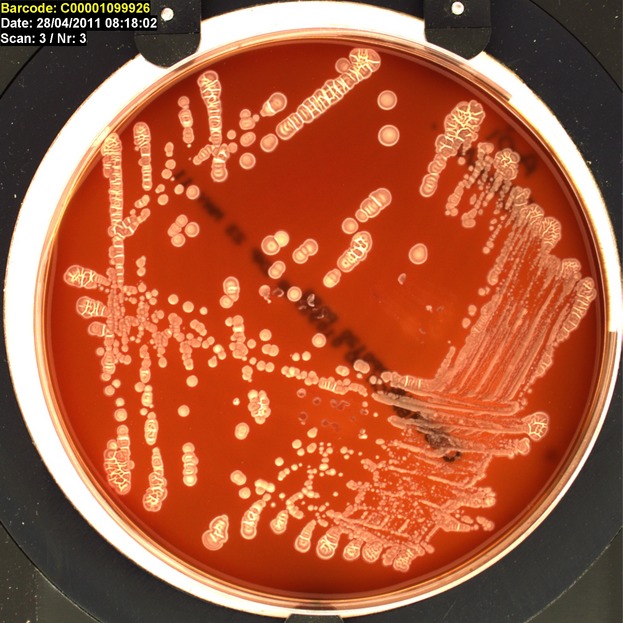
Appearance of Rothia aeria on the culture plates.
A two-stage revision procedure was undertaken. At the first stage, all the metallic prosthetic components were extracted and spacers shaped like the prosthetic components (Biomet, Warsaw, IN, USA) were implanted. Vancomycin was mixed into the cement. 2 g of vancomycin was used per 40 g of cement. Four out of seven specimens grew R. aeria, suggesting that this was a significant organism. The patient was treated with intravenous ceftriaxone (2 g once daily) for approximately 2 weeks and then with teicoplanin (600 mg once daily) for a further 4 weeks. Inflammatory markers showed a steady decline during this period. The patient underwent a re-implantation of the metallic prostheses 12 weeks following the first stage of the revision procedure.
After 4 months following the revision the patient was doing well with good functional joint and normal blood markers. A subsequent review at the maxillofacial clinic at the hospital identified some retained roots and dental caries that were removed 5 months after surgery. Although the knee infection was successfully treated, this patient unfortunately died of Clostridium difficile diarrhoea 6 months after the antibiotic course.
Discussion
In 1967, Georg and Brown proposed the genus Rothia [12] for a group of coccoid to diphtheroid to filamentous gram-positive organisms isolated from the human oral cavity, naming the genus after Roth [13], who had performed basic studies on these organisms.
The taxonomic position of the genus Rothia has undergone a number of changes since Georg and Brown first assigned it to the family Actinomycetaceae and proposed R. dentocariosa as the type (and only) species [12]. Possible assignments to the genera Actinomyces and Nocardia were rejected on chemotaxonomic, metabolic and biochemical grounds. More recent molecular studies placed the genus in the family Micrococcaceae, suborder Micrococcineae, order Actinomycetales, subclass Actinobacteridae, class Actinobacteria [14]. It is therefore in the same family as the genera Micrococcus, Arthrobacter, Kocuria, Nesterenkonia, Renibacterium and Stomatococcus, all of which show characteristic signature nucleotides in their 16S rDNA sequences [14]. Subsequently, Stomatococcus mucilaginosus, the only species in the genus Stomatococcus, was reclassified as Rothia mucilaginosa on the basis of 16S rRNA gene sequence and whole-cell protein pattern [15]. Genomic heterogeneity within R. dentocariosa has been observed [16].
Further, Rothia nasimurium, recovered from the nose of a mouse [15], and Rothia amarae, recovered from sludge [17], have been described and are both distinct phenotypically from R. dentocariosa.
More recently, phylogenetic analysis of a gram-positive bacterium strain A1-17BT isolated from Russian space station air samples showed that it grouped with unofficially named R. dentocariosa genomovar II, [18]. As a result of a polyphasic taxonomic study, the isolate was proposed to be classified as the novel species Rothia aeria sp. nov. [18].
After an extensive literature search we have been able to review six previously reported cases of Rothia joint infections (Table 1).
Table 1.
Seven reported cases of Rothia genus joint infections (most recent first)
| First author | Organism | Age (years) | Joint | Dental disease | RA | Immunosuppression | Treatment | Duration | Outcome successful |
|---|---|---|---|---|---|---|---|---|---|
| Mahobia et al. | Rothia aeria | 75 | Right prosthetic knee | Yes | Yes | Methotrexate, prednisolone | Hardware removed, IV ceftriaxone 2 g once daily | 2 weeks | Yes |
| Teicoplanin 600 mg once daily | 4 weeks | ||||||||
| Trivedi et al. [19] | Rothia species not known | 53 | Left prosthetic knee | Yes | Yes | No | Hardware removed,ertapenem 1 g daily + amoxicillin-clavulanate | 8 weeks | Yes |
| Oral amoxicillin-clavulanate | 4 months | ||||||||
| Kaasch et al. [20] | Rothia mucilaginosa | 73 | Right native knee | Unknown | Yes | Prednisolone | Moxifloxacin 400 mg once daily | 2 weeks | Yes |
| Ampicillin plus sulbactam 375 mg twice daily | 7 weeks | ||||||||
| Verrall et al. [21] | Rothia aeria | 88 | Both native shoulders | Yes | Yes | Methotrexate, prednisolone, hydrocortisone | IV penicillin 2.4 g/day infusion | 2 weeks | Yes |
| Favero et al. [22] | Rothia dentocariosa | 46 | Right native knee | Yes | Yes | Etanercept 25 mg twice weekly, oxaprozin | Levofloxacin, clarithromycin | Unknown | Yes |
| Michels et al. [23] | Rothia mucilaginosa | 59 | Right prosthetic hip | Yes | No | No | Hardware removed, vancomycin | 6 weeks | Yes |
| Klingler et al. [24] | Rothia dentocariosa | 44 | Right prosthetic knee | Yes | No but OA | Zidovudine, lamivudine (HIV) | Patient declined hardware removal, IV cefazolin | 6 weeks | Yes |
| Oral amoxicillin-clavulanate | Indefinitely |
IV, intravenous; OA, osteoarthritis; RA, rheumatoid arthritis.
It is evident from the above mentioned cases that significant rheumatological disease and orthopaedic surgeries are a significant risk factor for joint infections. Of the seven patients studied, all but one [20] had dental disease. It is also interesting that the two patients who had Rothia spp. joint infections despite being immunocompetent had a history of dental problems.
Of the seven Rothia spp. joint infections reported to date, four were prosthetic joint infections and three were native joint infections. In three of the four prosthetic joint infections all the hardware was removed. In one of these cases [23] hardware was removed only after treatment failure with antibiotics and resection. In the fourth case [24], where hardware was not removed, amoxicillin-clavulanate was continued indefinitely.
To the best of our knowledge, our case is the first report of an R. aeria prosthetic joint infection. Rothia aeria has been identified as a rare colonizing organism in the oral cavity of healthy individuals [25].
Ko et al. [26] studied the identification of Rothia isolates from human patients and one of their conclusions was that two strains which had previously been supposed to be R. dentocariosa according to the API Coryne system, were identified as R. aeria by 16S rRNA gene analysis. Two other case reports highlighted similar observations regarding the identification of Rothia spp. in their report [21,27]. This was also demonstrated in our case. This would suggest that routine biochemical tests may misidentify R. aeria as R. dentocariosa.
To date only six cases of systemic infections caused by R. aeria have been reported (excluding the current case). In these cases, R. aeria identification was performed using the 16S rRNA gene analysis [11,21,27–30].
Tarumoto et al. [28] reported the most recent case of R. aeria invasive infection. The report described a case of infective endocarditis in a 40-year-old Japanese man with a history of smoking but no history of medical problems. Unfortunately this case had a fatal outcome after cerebral haemorrhagic infarction. The other reported cases of R. aeria infection include a neck abscess in a patient with chronic granulomatous disease [29], multifocal nodular pneumonia [30], bronchitis [27], septic arthritis [21] and sepsis [11].
Falcone et al. [29] described the case of an R. aeria neck abscess in a patient with chronic granulomatous disease. The infection was aggressive, requiring two surgeries as well as prolonged antibiotics for complete resolution. Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) using a MALDI-TOF MicroFlex LT mass spectrometer (Bruker Daltonics, Billerica, MA, USA) identified it as Rothia species with best match to R. aeria. Full 16S rRNA gene sequencing confirmed the species level identification with a 99.8% match to the R. aeria type strain.
We took the opportunity to run the isolate from our case (previously identified as R. aeria by 16S rRNA gene analysis) through MALDI-TOF MS. The MALDI-TOF confirmed the isolate as Rothia spp. with best match to R. aeria.
Rothia aeria is susceptible to many antibiotics [11,21,27,28,30]. However, it reportedly demonstrates intermediate susceptibility to clindamycin and vancomycin [21,28]. Resistance to clindamycin [11,30], aztreonam [30] and ofloxacin [27] has also been reported.
Conclusion
Rothia spp. joint infections are rare. Genetic identification down to the level of species is important because species of Rothia can cause severe infections and certain species are not susceptible to some antibiotics. Evidence suggests that 16S rRNA sequencing or MALDI-TOF MS provide reliable identification of species. Failure of antibiotic treatment has been reported in the absence of complete removal of hardware.
Acknowledgments
We thank Louise Hill-King (Microbiology Department, Frimley) for the laboratory support and picture.
Conflict of Interest
None.
References
- Peltroche-Llacsahuanga H, Reichhart E, Schmitt W, Lutticken R, Haase G. Investigation of infectious organisms causing pericoronitis of the mandibular third molar. J Oral Maxillofac Surg. 2000;58:611–616. [PubMed] [Google Scholar]
- Lesher RJ, Gerencser VF, Morrison DJ. Presence of Rothia dentocariosa strain 477 serotype 2 in gingiva of patients with inflammatory periodontal disease. J Dent Res. 1977;56:189. doi: 10.1177/00220345770560021801. [DOI] [PubMed] [Google Scholar]
- Scharfen J. Untraditional glucose fermenting actinomycetes as human pathogens. Part II: Rothia dentocariosa as a cause of abdominal actinomycosis and a pathogen for mice. Zentralbl Bakteriol. 1975;233:80–92. [PubMed] [Google Scholar]
- Pape J, Singer C, Kiehn TE, Lee BJ, Armstrong D. Infective endocarditis caused by Rothia dentocariosa. Ann Intern Med. 1979;91:746–747. doi: 10.7326/0003-4819-91-5-746. [DOI] [PubMed] [Google Scholar]
- Sudduth EJ, Rozich JD, Farrar WE. Rothia dentocariosa endocarditis complicated by perivalvular abscess. Clin Infect Dis. 1993;17:772–775. doi: 10.1093/clinids/17.4.772. [DOI] [PubMed] [Google Scholar]
- MacKinnon MM, Amezaga MR, MacKinnon JR. A case of Rothia dentocariosa endophthalmitis. Eur J Clin Microbiol Infect Dis. 2001;20:756–757. doi: 10.1007/s100960100589. [DOI] [PubMed] [Google Scholar]
- Partner AM, Bhattacharya S, Scott RAH, Stavrou P. Rothia genus endophthalmitis following penetrating injury in a child. Eye. 2006;20:502–503. doi: 10.1038/sj.eye.6701902. [DOI] [PubMed] [Google Scholar]
- Morley AM, Tuft SJ. Rothia dentocariosa isolated from a corneal ulcer. Cornea. 2006;25:1128–1129. doi: 10.1097/01.ico.0000226362.11431.81. [DOI] [PubMed] [Google Scholar]
- Morris SK, Nag S, Suh KN, Evans GA. Recurrent chronic ambulatory peritoneal dialysis-associated infection due to Rothia dentocariosa. Can J Infect Dis Med Microbiol. 2004;15:171–173. doi: 10.1155/2004/823463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiesmayr S, Stelzmueller I, Berger N, et al. Rothia dentocariosa sepsis in a pediatric renal transplant recipient having post-transplant lymphoproliferative disorders. Pediatr Transplant. 2006;10:377–379. doi: 10.1111/j.1399-3046.2005.00472.x. [DOI] [PubMed] [Google Scholar]
- Monju A, Shimizu N, Yamamoto M, Oda K, Kawamoto Y, Ohkusu K. First case report of sepsis due to Rothia aeria in a neonate. J Clin Microbiol. 2009;47:1605–1606. doi: 10.1128/JCM.02337-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georg LK, Brown JM. Rothia, gen. nov., an aerobic genus of the family Actinomycetaceae. Int J Syst Bacteriol. 1966;17:79–88. [Google Scholar]
- Roth GD. Proteolytic organisms of carious lesions. Oral Surg Oral Med Oral Pathol. 1957;10:1105–1117. doi: 10.1016/0030-4220(57)90063-4. [DOI] [PubMed] [Google Scholar]
- Stackebrandt E, Rainey FA, Ward-Rainey NL. Proposal for a hierarchic classification system, Actinobacteria classis nov. Int J Syst Bacteriol. 1997;47:479–491. [Google Scholar]
- Collins MD, Hutson RA, Baverud V, Falsen E. Characterization of a Rothia-like organism from a mouse: description of Rothia nasimurium sp. nov. and reclassification of Stomatococcus mucilaginosus as Rothia mucilaginosa comb. nov. Int J Syst Evol Microbiol. 2000;50:1247–1251. doi: 10.1099/00207713-50-3-1247. [DOI] [PubMed] [Google Scholar]
- von Graevenitz A. Rothia dentocariosa: taxonomy and differential diagnosis. Clin Microbiol Infect. 2004;10:399–402. doi: 10.1111/j.1469-0691.2004.00784.x. [DOI] [PubMed] [Google Scholar]
- Fan Y, Jin Z, Tong J, et al. Rothia amarae sp. nov. from sludge of a foul water sewer. Int J Syst Evol Microbiol. 2002;52:2257–2260. doi: 10.1099/00207713-52-6-2257. [DOI] [PubMed] [Google Scholar]
- Li Y, Kawamura Y, Fujiwara N, et al. Rothia aeria sp. nov., Rhodococcus baikonurensis sp. nov. and Arthrobacter russicus sp. nov., isolated from air in the Russian space laboratory. Int J Syst Evol Microbiol. 2004;54:827–835. doi: 10.1099/ijs.0.02828-0. [DOI] [PubMed] [Google Scholar]
- Trivedi MN, Malhotra P. Rothia prosthetic knee joint infection. J Microbiol Immunol Infect. 2013;pii:S1684-1182(12)00243–S1684-1182(12)00245. doi: 10.1016/j.jmii.2012.12.001. [DOI] [PubMed] [Google Scholar]
- Kaasch AJ, Saxler G, Seifert H. Septic arthritis due to Rothia mucilaginosa. Infection. 2011 Feb;39:81–82. doi: 10.1007/s15010-010-0065-5. [DOI] [PubMed] [Google Scholar]
- Verrall AJ, Robinson PC, Tan CE, Mackie WG, Blackmore TK. Rothia aeria as a cause of sepsis in a native joint. J Clin Microbiol. 2010 Jul;48:2648–2650. doi: 10.1128/JCM.02217-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favero M, Raffeiner B, Cecchin D, Schiavon F. Septic arthritis caused by Rothia dentocariosa in a patient with rheumatoid arthritis receiving etanercept therapy. J Rheumatol. 2009;36:2846–2847. doi: 10.3899/jrheum.090276. [DOI] [PubMed] [Google Scholar]
- Michels F, Colaert J, Gheysen F, Scheerlinck T. Late prosthetic joint infection due to Rothia mucilaginosa. Acta Orthop Belg. 2007;73:263–267. [PubMed] [Google Scholar]
- Klingler ET, Verma P, Harris A. Infection of a total knee arthroplasty with Rothia dentocariosa: brief report and review of the literature. Infect Dis Clin Pract. 2005;13:195–199. [Google Scholar]
- Haraszthy VI, Zambon JJ, Sreenivasan PK, et al. Identification of oral bacterial species associated with halitosis. J Am Dent Assoc. 2007;138:1113–1120. doi: 10.14219/jada.archive.2007.0325. [DOI] [PubMed] [Google Scholar]
- Ko KS, Lee MY, Park YK, Peck KR, Song J-H. Molecular identification of clinical Rothia isolates from human patients: proposal of a novel Rothia Species, Rothia arfidiae sp. nov. J Bacteriol Virol. 2009;39:159–164. [Google Scholar]
- Michon J, Jeulin D, Lang JM, Cattoir V. Rothia aeria acute bronchitis: the first reported case. Infection. 2010;38:335–337. doi: 10.1007/s15010-010-0012-5. [DOI] [PubMed] [Google Scholar]
- Tarumoto N, Sujino K, Yamaguchi T, et al. A first report of Rothia aeria endocarditis complicated by cerebral hemorrhage. Intern Med. 2012;51:3295–3299. doi: 10.2169/internalmedicine.51.7946. [DOI] [PubMed] [Google Scholar]
- Falcone EL, Zelazny AM, Holland SM. Rothia aeria neck abscess in a patient with chronic granulomatous disease: case report and brief review of the literature. J Clin Immunol. 2012;32:1400–1403. doi: 10.1007/s10875-012-9726-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiyamuta H, Tsuruta N, Matsuyama T, Satake M, Ohkusu K, Higuchi K. First case report of respiratory infection with Rothia aeria. Nihon Kokyuki Gakkai Zasshi. 2010;48:219–223. [PubMed] [Google Scholar]


