Abstract
Corticosteroid hypersensitivity is a rare, but troublesome condition often mimicking the symptoms of the underlying disease and therefore probably underdiagnosed. Our objective is to underline the importance of increased awareness of corticosteroid hypersensitivity and of determining the tolerability to other corticosteroid preparations and thus identify a safe treatment alternative. We report a case of corticosteroid hypersensitivity in a 65-year-old woman with a history of difficult-to-treat asthma and systemic corticosteroid allergy admitted with increasing dyspnea and dry cough. The patient was diagnosed with hypereosinophilia, apical fibrosis, and basal pulmonary infiltrations. A prick test and a prolonged challenge test were performed to find a suitable corticosteroid to treat her hypereosinophilia. In conclusion, it is compulsory to perform cutaneous prick and intradermal test, but many cases will only be diagnosed correctly by intravenous or oral challenge test.
Keywords: Allergy, corticosteroid, hypersensitivity, steroids
Introduction
Corticosteroid sensitivity is a rare and probably underdiagnosed condition and symptoms can easily be mistaken to be caused by the underlying disease [1, 2]. Corticosteroids are widely used in the treatment of severe asthma and chronic obstructive pulmonary disease, severe allergic reactions, organ transplant recipients, and autoimmune disorders often with symptoms mimicking allergic reactions.
Corticosteroids have a wide range of adverse effects, but considering the frequent use of corticosteroids, hypersensitivity reactions are rare. Previous studies have found a frequency of less than 1% for systemic treatment [1]. Topically administered corticosteroids have a higher prevalence of hypersensitivity reactions ranging from 0.5 to 5% but tend to cause less severe reactions than systemic corticosteroids [1].
Systemic corticosteroid hypersensitivity reactions are a heterogeneous group of immediate and non-immediate reactions in some cases due to the steroid itself, in others due to salts and diluents/preservatives in the corticosteroid preparations with symptoms ranging from urticaria to cardiovascular collapse and death [1, 2]. Immediate reactions are probably mediated by specific IgE antibodies in a classical type I allergy with onset of symptoms within less than 1 h. Non-immediate allergic reactions are T-cell-mediated type IV allergic reactions with delayed symptoms up to 48 h after administration of the suspected allergen. Methylprednisolone and hydrocortisone are the drugs most often involved in immediate hypersensitivity reactions while betamethasone is the most frequent in non-immediate reactions followed by dexamethasone and triamcinolone [1, 2].
Coopman classified corticosteroids into four groups based on chemical structure and patch test results [1]. The classification applies to topical steroids and provides a structured overview of cross-reactivity, but it does unfortunately not seem to apply to systemic corticosteroids [1, 3].
Case Report
We report a 65-year-old woman with a history of difficult-to-treat asthma, pulmonary embolisms, non-steroidal anti-inflammatory drug (NSAID) allergy, and adverse reactions to systemic corticosteroids admitted with increasing dyspnea and dry cough for 14 days and severe desaturation at the time of admittance.
The patient's history strongly suggested corticosteroid hypersensitivity, as she had previously developed skin itching, vomiting, urticaria, and dyspnea shortly after both oral and intravenous administration of prednisolone, methylprednisolone, and two other corticosteroids.
At admission she was diagnosed with hypereosinophilia with an eosinophil count of 4.7 and a high-resolution computed scanning of her lungs showed apical fibrosis and basal pulmonary infiltrations (Fig. 1). There were no signs of parasitic infection.
Figure 1.
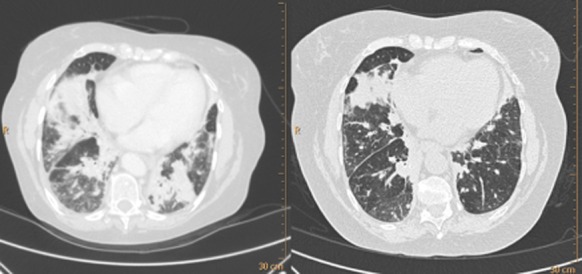
Patient chest computed tomography scan before (left panel) and after hydrocortisone therapy.
In order to treat her hypereosinophilia, we first tested her for hypersensitivity to hydrocortisone-succinate by performing a prick test, which was negative, followed by a prolonged challenge test with increasing doses of intravenous hydrocortisone-succinate over the course of 2 h (5, 10, 25 and, lastly, 50 mg with 30 min between all doses). The patient tolerated the challenge test and therefore started continuous treatment of 100 mg hydrocortisone-succinate intravenously twice daily. On this treatment, the eosinophil count normalized.
In order to substitute from intravenous to oral corticosteroids, her tolerability to alternative corticosteroid preparations was tested. She was given 5 mg prednisolone under the cover of the hydrocortisone-succinate. The patient developed a rash, diarrhea, headache, and dyspnea within 2 h of administration, which we considered diagnostic of prednisolone allergy. She was then treated with hydrocortisone 5 mg without any adverse reaction. The dose of hydrocortisone was soon increased to 20 mg three times daily with simultaneous tapering of hydrocortisone-succinate.
The patient's clinical condition as well as her pulmonary function test (initial FEV1 1.03 [44%], ratio 69%, after treatment FEV1 1.31 [56%], ratio 77%) improved remarkably on the corticosteroid treatment and she was discharged in good condition. The hydrocortisone was later tapered but due to reoccurrence of hypereosinophilia a dose of 10 mg twice daily was continued and was well tolerated for more than a year.
Discussion
Although corticosteroid hypersensitivity is rare, our case underscores that it can be associated with severe adverse events, thus complicating optimal treatment of patients.
Many cases of corticosteroid hypersensitivity remains probably undiagnosed because the symptoms often mimic the symptoms of the underlying disease [4]. Our patient received substandard care until her corticosteroid allergy was confirmed and skin and challenge tests were done in order to determine her tolerability to other corticosteroid preparations to find a suitable alternative.
Early studies did not identify significant host factors associated with corticosteroid allergy [2], but more recent works have found several risk factors [4]. Our patient was at high risk of corticosteroid allergy having some of the recently identified risk factors: a diagnosis of asthma with frequent corticosteroid use and repeated high-dose boluses as well as NSAID hypersensitivity. Other risk factors are renal transplantation, a history of nephritis, and high percutaneous absorption caused by sweat, cutaneous infections, and atopic dermatitis [4].
Cases of cross-reactivity have been described [3, 4], but similar to our case, previous case reports have shown that hypersensitivity to a corticosteroid in one group does not rule out the safe use of other corticosteroids in the same group [5].
Although the Coopman classification does not apply to systemic corticosteroids [3], it can guide doctors in their efforts to choose a replacement corticosteroid, but it cannot replace a systematic evaluation of the individual patient sensitivity and tolerability.
It is compulsory to perform cutaneous prick and intradermal test, but many cases will only be diagnosed correctly by intravenous or oral challenge test. A challenge test should always be carried out to determine the tolerability to other corticosteroid preparations and thus identify a safe treatment alternative if skin tests are negative.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
References
- 1.Torres MJ, Canto G. Hypersensitivity reactions to corticosteroids. Curr. Opin. Allergy Clin. Immunol. 2010;10(4):273–279. doi: 10.1097/ACI.0b013e32833b1f34. [DOI] [PubMed] [Google Scholar]
- 2.Butani L. Corticosteroid-induced hypersensitivity reactions. Ann. Allergy Asthma Immunol. 2002;89(5):439–445. doi: 10.1016/S1081-1206(10)62077-7. quiz 445-446, 502. [DOI] [PubMed] [Google Scholar]
- 3.Venturini M, Lobera T, del Pozo MD, et al. Immediate hypersensitivity to corticosteroids. J. Investig. Allergol. Clin. Immunol. 2006;16(1):51–56. [PubMed] [Google Scholar]
- 4.Vatti RR, Ali F, Teuber S, et al. Hypersensitivity reactions to corticosteroids. Clin. Rev. Allergy Immunol. 2013 doi: 10.1007/s12016-013-8365-z. doi: 10.1007/s12016-013-8365-z. [DOI] [PubMed] [Google Scholar]
- 5.Aranda A, Mayorga C, Ariza A, et al. IgE-mediated hypersensitivity reactions to methylprednisolone. Allergy. 2010;65(11):1376–1380. doi: 10.1111/j.1398-9995.2010.02386.x. [DOI] [PubMed] [Google Scholar]


