Abstract
Introduction
In 2009, the International Society for Sexual Medicine (ISSM) convened a select panel of experts to develop an evidence-based set of guidelines for patients suffering from lifelong premature ejaculation (PE). That document reviewed definitions, etiology, impact on the patient and partner, assessment, and pharmacological, psychological, and combined treatments. It concluded by recognizing the continually evolving nature of clinical research and recommended a subsequent guideline review and revision every fourth year. Consistent with that recommendation, the ISSM organized a second multidisciplinary panel of experts in April 2013, which met for 2 days in Bangalore, India. This manuscript updates the previous guidelines and reports on the recommendations of the panel of experts.
Aim
The aim of this study was to develop clearly worded, practical, evidenced-based recommendations for the diagnosis and treatment of PE for family practice clinicians as well as sexual medicine experts.
Method
A comprehensive literature review was performed.
Results
This article contains the report of the second ISSM PE Guidelines Committee. It offers a new unified definition of PE and updates the previous treatment recommendations. Brief assessment procedures are delineated, and validated diagnostic and treatment questionnaires are reviewed. Finally, the best practices treatment recommendations are presented to guide clinicians, both familiar and unfamiliar with PE, in facilitating treatment of their patients.
Conclusion
Development of guidelines is an evolutionary process that continually reviews data and incorporates the best new research. We expect that ongoing research will lead to a more complete understanding of the pathophysiology as well as new efficacious and safe treatments for this sexual dysfunction. We again recommend that these guidelines be reevaluated and updated by the ISSM in 4 years. Althof SE, McMahon CG, Waldinger MD, Serefoglu EC, Shindel AW, Adaikan PG, Becher E, Dean J, Giuliano F, Hellstrom WJG, Giraldi A, Glina S, Incrocci L, Jannini E, McCabe M, Parish S, Rowland D, Segraves RT, Sharlip I, and Torres LO. An update of the International Society of Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation (PE). Sex Med 2014;2:60–90.
Keywords: Premature Ejaculation, Definition of PE, Diagnosis of PE, Etiology of PE, Pharmacotherapy of PE, Prevalence of PE, Psychotherapy of PE
Introduction
In 2009, the International Society for Sexual Medicine (ISSM) convened a select panel of experts to develop an evidence-based set of guidelines for patients suffering from lifelong premature ejaculation (LPE) [1]. That document reviewed definitions, etiology, impact on the patient and partner, assessment, and pharmacological, psychological, and combined treatments. It concluded by recognizing the continually evolving nature of clinical research and recommended a subsequent guideline review and revision every fourth year.
Consistent with that recommendation, the ISSM organized a second multidisciplinary panel of experts in April 2013, which met for 2 days in Bangalore, India. The committee members were selected to assure diversity of discipline, balance of opinion, knowledge, gender, and geography. Twenty members consisting of nine urologists, three psychiatrists, three psychologists, one family practice physician, one endocrinologist, one sexual medicine physician, one radiation oncologist, and one pharmacologist comprised the group. The committee was chaired by Chris McMahon, MD.
Prior to the meeting, the committee members received a comprehensive literature review and were asked to critically assess the previous guidelines. Members were assigned specific topic for presentation, and a writing committee was chosen to craft this document. Quality of evidence and the strength of recommendation were graded using the Oxford Centre of Evidence-Based Medicine system [2].
The meeting was supported by an unrestricted grant from Johnson & Johnson (New Brunswick, NJ, USA), the manufacturer of dapoxetine. ISSM required complete independence from industry; there were no industry representatives at the meeting and there was no attempt by industry to influence the writing process at any time [3]. Members were required to declare in advance any conflicts of interests.
Definitions of Premature Ejaculation (PE)
Several definitions for PE exist, having been drafted by various professional organizations or professionals 4–11 (see Table 1), and most include the PE subtypes of lifelong and acquired (PE symptoms beginning after a period of normal ejaculatory function). The major criticisms of the extant definitions included their failure to be evidence based, lack of specific operational criteria, excessive vagueness, and reliance on the subjective judgment of the diagnostician [12]. Nonetheless, three common constructs underlie most definitions of PE: (i) a short ejaculatory latency; (ii) a perceived lack of control or inability to delay ejaculation, both related to the broader construct of perceived self-efficacy; and (iii) distress and interpersonal difficulty to the individual and/or partner (related to the ejaculatory dysfunction) [12].
Table 1.
Definitions of premature ejaculation established through consensus committees and/or professional organizations
| Definition | Source |
|---|---|
| A male sexual dysfunction characterized by ejaculation that always or nearly always occurs prior to or within 1 minute of vaginal penetration, either present from the first sexual experience or following a new bothersome change in ejaculatory latency, and the inability to delay ejaculation on all or nearly all vaginal penetrations, and negative personal consequences, such as distress, bother, frustration, and/or the avoidance of sexual intimacy. | International Society of Sexual Medicine, 2013 |
| A. Persistent or recurrent pattern of ejaculation occurring during partnered sexual activity within approximately 1 minute following vaginal penetration and before the individual wishes it (Note: Although the diagnosis of premature [early] ejaculation may be applied to individuals engaged in non-vaginal sexual activities, specific duration criteria have not been established for these activities). | DSM-5, 2013 |
| B. The symptom in Criterion A must have been present for at least 6 months and must be experienced on almost all or all ( approximately 75%–100%) occasions of sexual activity (in identified situational contexts or, if generalized, in all contexts). | |
| C. The symptom in Criteria A causes clinically significant distress in the individual. | |
| D. The sexual dysfunction is not better explained by a nonsexual mental disorder or as a consequence of severe relationship distress or other significant stressors and is not attributable to the effects of a substance/medication or another medical disorder. | |
| Persistent or recurrent ejaculation with minimal sexual stimulation, before, on or shortly after penetration and before the person wishes it. The condition must also cause marked distress or interpersonal difficulty and cannot be due exclusively to the direct effects of a substance. | DSM-IV-TR, 2000 |
| For individuals who meet the general criteria for sexual dysfunction, the inability to control ejaculation sufficiently for both partners to enjoy sexual interaction, manifest as either the occurrence of ejaculation before or very soon after the beginning of intercourse (if a time limit is required, before or within 15 seconds) or the occurrence of ejaculation in the absence of sufficient erection to make intercourse possible. The problem is not the result of prolonged absence from sexual activity. | International Statistical Classification of Disease, 10th Edition, 1994 |
| The inability to control ejaculation for a “sufficient” length of time before vaginal penetration. It does not involve any impairment of fertility, when intravaginal ejaculation occurs. | European Association of Urology. Guidelines on Disorders of Ejaculation, 2001 |
| Persistent or recurrent ejaculation with minimal stimulation before, on, or shortly after penetration, and before the person wishes it, over which the sufferer has little or no voluntary control, which causes the sufferer and/or his partner bother or distress. | International Consultation on Urological Diseases, 2004 |
| Ejaculation that occurs sooner than desired, either before or shortly after penetration, causing distress to either one or both partners. | American Urological Association Guideline on the Pharmacologic Management of Premature Ejaculation, 2004 |
DSM-5 definition reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, (Copyright ©2013). American Psychiatric Association. All Rights Reserved.
Because of the discontent with the existing PE definitions, as well as pressure from regulatory agencies concerning the inadequacy of the definitions, the ISSM convened in 2007 and again in 2013, a meeting of experts to develop a definition grounded in clearly definable scientific criteria [12]. After carefully reviewing the literature, the committee proposed a unified definition of both LPE and acquired PE (APE): It “is a male sexual dysfunction characterized by:
ejaculation that always or nearly always occurs prior to or within about 1 minute of vaginal penetration from the first sexual experience (LPE), OR a clinically significant reduction in latency time, often to about 3 minutes or less (acquired premature ejaculation);
the inability to delay ejaculation on all or nearly all vaginal penetrations; and
negative personal consequences, such as distress, bother, frustration, and/or the avoidance of sexual intimacy.” Level of evidence (LOE 1a)
The definition applies to both LPE and APE but is limited to intravaginal sexual activity, as correlations between coital, oral sex, and masturbatory latencies are not consistently high. In addition, it does not define PE when men have sex with men. The committee concluded that there was insufficient information available to extend the definition to these other situations or groups. (LOE 5d)
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [13] definition of premature (early) ejaculation, published in 2013, is consistent with the ISSM definition and includes the approximately 1-minute intravaginal ejaculatory latency time (IELT) criteria as well as the inclusion of distress. It also asks the clinician to specify the subtypes of lifelong and acquired, generalized, or situational as well as the severity of the dysfunction.
Anteportal ejaculation is the term applied to men who ejaculate prior to vaginal penetration and is considered the most severe form of PE. Such men or couples typically present when they are having difficulty conceiving children. It is estimated that between 5% and 20% of men with LPE suffer from anteportal PE [14].
The committee recognized that some men who self-diagnose PE and present for treatment fail to fulfill the ISSM criteria for PE. Waldinger has proposed two additional “subtypes” of men who are distressed about their ejaculatory function but do not meet the diagnostic criterion for PE. He designated them as variable PE (VPE) and subjective PE (SPE) [10,15]. These subtypes should be considered provisional; however, we believe these categories may help health care professionals (HCPs) address the concerns of men who do not qualify for the diagnosis of PE but are seeking help. VPE is characterized by short ejaculatory latency that occurs irregularly and inconsistently with some subjective sense of diminished control of ejaculation. This subtype is not considered a sexual dysfunction but rather a normal variation in sexual performance. SPE is characterized by one or more of the following: (i) subjective perception of consistent or inconsistent short IELT; (ii) preoccupation with an imagined short ejaculatory latency or lack of control over the timing of ejaculation; (iii) actual IELT in the normal range or even of longer duration (i.e., an ejaculation that occurs after 5 minutes); (iv) ability to control ejaculation (i.e., to withhold ejaculation at the moment of imminent ejaculation) that may be diminished or lacking; and (v) the preoccupation that is not better accounted for by another mental disorder. (LOE 5d)
Epidemiology
PE has been recognized as a syndrome for well over 100 years [16]. Despite this long history, the prevalence of the condition remains unclear. This ambiguity derives in large part from the difficulty defining what constitutes clinically relevant PE. Vague definitions without specific operational criteria, different modes of sampling, and nonstandardized data acquisition have led to tremendous variability in estimated prevalence 1,12,17–19. The sensitive nature of PE further hampers the reliability of epidemiologic studies; the small fraction of the male population willing to answer questions concerning their sexual lives may not be representative of the larger population of men [20,21]. In addition, some men with genuinely rapid ejaculation times may be reluctant to report this complaint due to worry about social stigmatization [22]. Conversely, healthy individuals may report PE because of the incentives provided by researchers, the belief that they will benefit from participation in a survey [22], or a misunderstanding of what is typical with respect to ejaculatory latency in real-world sexual encounters [8]. Aside from difficulties with definitions and sampling, there is marked variability in distress related to early ejaculation between individual men and across cultures [8]. It is likely that some men may report early ejaculation when asked a single-item question on an epidemiological survey while not experiencing bother sufficient to justify medical attention. Based on the absence of distress, such men would not meet the current criteria for PE [12,23].
Peer-reviewed studies on the prevalence of PE published prior to March 2013 are summarized in Table 2 26,27,29,30,33–35,37–41,43–46,48–59. Most of these studies utilized the DSM, Fourth Edition, Text Revision (IV-TR) definition and characterized PE as the “most common male sexual dysfunction,” with a prevalence rate of 20–30% 20–22. As the DSM-IV-TR definition lacks objective diagnostic criteria, the high prevalence of PE reported in many of these surveys is a source of ongoing debate [30,33,40,46,53,55,58,59]. It is, however, unlikely that the PE prevalence is as high as 20–30% based on the relatively low number of men who present for treatment of PE [21,54,57].
Table 2.
The prevalence rates of premature ejaculation
| Date | Author | Method of data collection | Method of sample recruitment | Specific operational criteria | Prevalence rate | Number of men |
|---|---|---|---|---|---|---|
| 1998 | Dunn et al. [24] | General practice registers—random stratification | Having difficulty with ejaculating prematurely | 14% (past 3 months) | 617 | |
| 31% (lifetime) | 618 | |||||
| 1999 | Laumann et al. (NHSLS) [22] | Interview | NA | Climaxing/ejaculating too rapidly during the past 12 months | 31% | 1,410 |
| 2002 | Fugl-Meyer and Fugl-Meyer [25] | Interview | Population register | NA | 9% | 1,475 |
| 2004 | Rowland et al. [26] | Mailed questionnaire | Internet panel | DSM-IV | 16.3% | 1,158 |
| 2004 | Nolazco et al. [27] | Interview | Invitation to outpatient clinic | Ejaculating fast or prematurely | 28.3% | 2,456 |
| 2005 | Laumann et al. (GSSAB) [20] | Telephone-personal interview/mailed questionnaires | Random (systematic) sampling | Reaching climax too quickly during the past 12 months | 23.75% (4.26% frequently) | 13,618 |
| 2005 | Basile Fasolo et al. [28] | Clinician based | Invitation to outpatient clinic | DSM-IV | 21.2% | 12,558 |
| 2005 | Stulhofer et al. [29] | Interview | Stratified sampling | Often ejaculating in less than 2 minutes | 9.5% | 601 |
| 2007 | Porst et al. (PEPA) [21] | Web-based survey Self-report | Internet panel | Control over ejaculation Distress | 22.7% | 12,133 |
| 2008 | Shindel et al. [30] | Questionnaire | Male partners of infertile couples under evaluation | Self report premature ejaculation | 50% | 73 |
| 2009 | Brock et al. [31] | Telephone interview | Web-based survey | DSM-III | 16% | 3,816 |
| Control | 26% | |||||
| Distress | 27% | |||||
| 2010 | Traeen and Stigum [32] | Mailed questionnaire + Internet | Web interview + randomization | NA | 27% | 11,746 + 1,671 |
| 2010 | Son et al. [33] | Questionnaire | Internet panel (younger than 60) | DSM-IV | 18.3% | 600 |
| 2010 | Amidu et al. [34] | Questionnaire | NA | NA | 64.7% | 255 |
| 2010 | Liang et al. [35] | NA | NA | ISSM | 15.3% | 1,127 |
| 2010 | Park et al. [36] | Mailed questionnaire | Stratified sampling | Suffering from PE | 27.5% | 2,037 |
| 2010 | Vakalopoulos et al. [37] | One-on-one survey | Population-based cohort | EED | 58.43% | 522 |
| ISSM lifelong PE | 17.7% | |||||
| 2010 | Hirshfeld et al. [38] | Web-based survey | Online advertisement in the United States and Canada | Climaxing/ejaculating too rapidly during the past 12 months | 34% | 7,001 |
| 2011 | Christensen et al. [39] | Interview + questionnaire | Population register (random) | NA | 7% | 5,552 |
| 2011 | Serefoglu et al. [40] | Interview | Stratified sampling | Complaining about ejaculating prematurely | 20.0% | 2,593 |
| 2011 | Son et al. [33] | Questionnaire | Internet panel | Estimated IELT ≤5 minutes, inability to control ejaculation, distress | 10.5% | 334 |
| 2011 | Tang and Khoo [41] | Interview | Primary care setting | PEDT ≥ 9 | 40.6% | 207 |
| 2012 | Mialon et al. [42] | Mailed questionnaire | Convenience sampling (18–25 years old) | Control over ejaculation Distress | 11.4% | 2,507 |
| 2012 | Shaeer and Shaeer [43] | Web-based survey | Online advertisement in Arabic countries | Ejaculate before the person wishes to ejaculate at least sometimes | 83.7% | 804 |
| 2012 | Shindel et al. [44] | Web-based survey | Online advertisement targeted to MSM + distribution of invitation to organizations catering to MSM | PEDT ≥ 9 | 8–12% | 1,769 |
| 2012 | McMahon et al. [45] | Computer-assisted interviewing, online, or in-person self-completed | NA | PEDT ≥ 11 | 16% | 4,997 |
| Self-reported (always/nearly-always) | 13% | |||||
| 2012 | Lotti et al. [46] | Interview | Men seeking medical care for infertility | PEDT ≥ 9 | 15.6% | 244 |
| 2013 | Zhang et al. [47] | Interview | Random stratified sample of married men aged 30–60 | Self-reported premature ejaculation | 4.7% | 728 |
| 2013 | Lee et al. [48] | Interview | Stratified random sampling | PEDT ≥ 11 | 11.3% | 2,081 |
| Self-reported | 19.5% | |||||
| IELT < 1 minute | 3% | 1,035 | ||||
| 2013 | Shaeer [49] | Web-based survey | Online advertisement in the United States | PEDT ≥ 11 | 50% | 1,133 |
| Self-report any PE | 78% | |||||
| Self-reported “always” or “mostly” | 14% | |||||
| 2013 | Gao et al. [50] | Interview | Random stratified sample of monogamous heterosexual men in China | Self-reported premature ejaculation | 25.8% | 3,016 |
| 2013 | Hwang et al. [51] | Survey of married couples | Married heterosexual couples in Korea | Estimated IELT < 2 minutes | 21.7% | 290 |
| PEDT ≥ 11 | 12.1% | |||||
| 2013 | Vansintejan et al. [52] | Web-based survey | Online and flyer advertisements to Belgian men who have sex with men (only HIV+ men in this study) | IPE score ≤ 50% of total possible IPE score ≤ 66% of total possible | 4% 18% | 72 |
DSM = Diagnostic and Statistical Manual of Mental Disorders; EED = early ejaculatory dysfunction; GSSAB = Global Study of Sexual Attitudes and Behaviors; HIV = human immunodeficiency virus; IELT = intravaginal ejaculatory latency time; ISSM = International Society of Sexual Medicine; IPE = Index of Premature Ejaculation; MSM = men who have sex with men; NA = North American; NHSLS = National Health and Social Life Survey; PE = premature ejaculation; PEDT = Premature Ejaculation Diagnostic Tool; PEPA = premature ejaculation prevalence and attitudes
In two online surveys, one of Arabic-speaking men in the Middle East, the second of US men, 82.6% and 78% of participants, respectively, reported some degree of PE [43,49]. This high rate of PE is best accounted for by the inclusion of men with VPE or SPE. In the Middle Eastern study, only 15.3% of men reported that they “always” ejaculated before they wished, while 46% and 21% described themselves, respectively, as “sometimes” or “mostly” ejaculating before they wished. In the US study, the 78% of men acknowledging some degree of PE decreased to 14.4% when combining the “always' or “mostly” group.
In two five-nation (Turkey, United States, United Kingdom, the Netherlands, and Spain) studies of IELT in men from the general population, the median IELT was 5.4 minutes (range 0.55–44.1 minutes) and 6.0 minutes (range 0.1–52.7 minutes), respectively [8,56]. In these samples, 2.5% of men had an IELT of less than 1 minute and 6% of less than 2 minutes PE [1,8,56]. These percentages are not necessarily equivalent to the prevalence of LPE because there was no assessment of distress or chronicity [8,56].
Based on these data and the ISSM and DSM-5 definition of PE, in terms of an IELT of about 1 minute, the prevalence of LPE is unlikely to exceed 4% of the general population. (LOE 3b)
Serefoglu et al. were the first to report prevalence rates for the four PE subtypes [40,58,59] as described by Waldinger and Schweitzer [10,15,23] A 2010 study reported the distribution of PE subtypes in PE patients admitted to a urology outpatient clinic in Turkey, while a subsequent 2011 study reported the prevalence of PE subtypes in the general male population in Turkey randomly selected by a proportional sampling method according to postal code [40,58]. This research design was replicated by Zhang et al. [53] and Gao et al. [50] in a Chinese population. In both these studies, a relatively high proportion of men (20.0% in Turkey and 25.8% in China) acknowledged a concern with ejaculating too quickly, consistent with previously reported prevalence studies of PE [21]. Employing Waldinger's definition [10,23], in the general male population of both countries, the prevalence of LPE was 2.3% and 3%, whereas the prevalence of APE was 3.9% and 4.8%, respectively [40,50]. The prevalence of VPE and SPE was 8.5% and 5.1% in Turkey and 11% and 7% in China, respectively [40,50].
An approximately 5% prevalence of APE and LPE in general populations is consistent with epidemiological data indicating that around 5% of the population have an ejaculation latency less than 2 minutes. (LOE 3b)
There are significant differences between PE prevalence rates in the general population and clinic settings because the majority of men with PE do not seek treatment. Of patients presenting for treatment, 36% to 63% have LPE and 16% to 28% have APE [53,58]. The prevalence of VPE and SPE among these clinic patients was 14.5% and 6.9% in the Turkish clinic and 12.7% and 23.5% in the Chinese clinic patients [53,58].
Etiology
Early PE investigators did not often differentiate between APE and LPE, nor were there objective criteria for what constituted PE in general [4,6]. With the development of the ISSM definition [12] and two new PE syndromes VPE and SPE [15,57], it is increasingly important to clarify which syndrome is being addressed in etiological studies.
Historical ambiguity on what constitutes early ejaculation has led to a diverse list of potential and established etiological factors [1]. Classically, PE was thought to be psychologically or interpersonally based, due in large part to anxiety or conditioning toward rapid ejaculation based on rushed early sexual experiences [6,60]. Over the past two decades, somatic and neurobiological etiologies for early ejaculation have been hypothesized. Myriad biological factors have been proposed to explain PE including: hypersensitivity of the glans penis [61], robust cortical representation of the pudendal nerve [62], disturbances in central serotonergic neurotransmission [63,64], erectile difficulties and other sexual comorbidities [65,66], prostatitis [67], detoxification from prescribed medications [68,69], recreational drugs [70], chronic pelvic pain syndrome (CPPS) [71], and thyroid disorders [72,73]. It is noteworthy that none of these etiologies has been confirmed in large scale studies.
Neurobiology of PE
Serotonin is the neurotransmitter of greatest interest in the control of ejaculation and has the most robust data in animal and human models. Waldinger hypothesized that lifelong early ejaculation in humans may be explained by a hyposensitivity of the 5-HT2C and/or hypersensitivity of the 5-HT1A receptors [19]. As serotonin tends to delay ejaculation, men low in 5-HT neurotransmission and/or 5-HT2C receptor hyposensitivity may have intrinsically lower ejaculatory thresholds. (LOE 3b)
Serotonin dysregulation as an etiological hypothesis for LPE has been postulated to explain only a small percentage (2–5%) of complaints of PE in the general population [74]. (LOE 2a)
Dopamine and oxytocin also appear to play important roles in ejaculation; the biology of these neurotransmitters in relation to ejaculation is less well studied, but in animal studies, both appear to have a stimulatory effect on ejaculation [75,76]. (LOE 3b)
In the spinal cord, lumbar spinothalamic neurons have been implicated as essential to the ejaculatory reflex in rats 77–80 constituting a spinal generator of ejaculation [81] (LOE2a). There is also preliminary evidence that such a neural organization also exists in humans [82]. The relevance of these findings to PE is not yet apparent, but this remains a fertile area for further translational research.
Genetics of PE
Genetic variations have been proposed to bring about differences in the neurobiological factors associated with PE. A genetic cause for PE was first hypothesized in 1943 based on family prevalence studies [60]. Waldinger et al. confirmed this finding by surveying family members of 14 men with a lifelong IELT less than 1 minute. Data on ejaculation latency in these male relatives were obtained by interview (n = 11) or “family history” (n = 6). Lifelong IELT of less than 1 minute was found in 88% of these first-degree male relatives of men with LPE [83].
In 2007, Jern et al. reported on genetic and environmental risk factors for ejaculation disturbances in 1,196 Finnish twins [84]. Modeling of etiological factors for early ejaculation (based on a subjective symptom scale) suggested a moderate additive genetic influence on propensity toward early ejaculation; however, a large portion of the variance in the frequency of early ejaculation was related to non-shared environmental variance, suggesting that genetic influences may create a diathesis or predisposition to PE rather than a direct cause-and-effect relationship [84].
The first DNA-based study on PE was performed by Janssen et al. in 89 Dutch men with LPE (confirmed by stopwatch IELT) compared with a cohort of mentally and physically healthy Dutch Caucasian men [85]. The target of this assessment was a gene polymorphism for the serotonin transporter protein (5-HTTLPR). This polymorphism has long (L) and short (S) allelic variants; the L alleles lead to greater transcriptional activity and hence decreased synaptic serotonin. In the LPE group, men homozygous for the L allele had ejaculation latencies that were half as long as men with the SL or SS genotypes. Given that the L allele leads to reduced synaptic serotonin, this finding is consistent with our current understanding of the influence of serotonin on ejaculation latency [85]. However, there was no difference in the prevalence of the LL, SL, and SS genotypes in men with LPE compared with their prevalence in the general male Dutch population, which suggests that this polymorphism alone cannot account for PE [85]. Follow-up studies on this same gene locus from other investigators have been mixed, with one report [86] being consistent with Janssen et al.'s findings, another reporting no association between 5-HTTLPR allele type and early ejaculation [87], and another study finding the exact opposite relationship between ejaculation latency and L vs. S allele carries [88].
A new body of research on tandem repeats of the dopamine transporter gene (DAT-1) as a modulator of ejaculation latency has emerged 89–91. Men with longer tandem repeat lengths have greater transcription of the transporter and hence, less synaptic dopamine activity [89]. Santtila et al. reported that men with longer tandem repeats were more likely to endorse symptoms consistent with early ejaculation [89]. A few studies, mainly performed in general male twin studies, have investigated polymorphism receptors for serotonin, oxytocin, and/or vasopressin [92]. Preliminary findings have not indicated a marked preponderance of any one genetic polymorphism in men with symptoms of early ejaculation 92–94.
The current body of evidence suggests that individual genetic polymorphisms exert a minor, if any, effect on ejaculation latency. Men with numerous genetic variants may be predisposed to development of PE, but data remain scant and controversial. (LOE 2a)
Special Patient Populations
Thyroid Hormones
Data from animal studies suggest anatomic and physiologic interactions between brain dopamine and serotonin systems and the hypothalamic-pituitary thyroid axis 95–97. Corona et al. and Carani et al. reported a significant correlation between APE and suppressed thyroid-stimulating hormone and high thyroid hormone values in andrological and sexological patients [72,73]. After normalizing thyroid function in hyperthyroid men, the prevalence of APE fell from 50% to 15% [72]. These data have been confirmed in several other reports 72,98–101. However, no link has been found between thyroid hormones and PE in a large cohort of men with LPE [102].
Hyperthyroidism (an acquired condition) has no role in LPE and has been found to be associated with APE in extremely few patients [103]. (LOE 2a)
Other Hormones
Although it is well established that male reproduction and sexuality are hormonally regulated, the endocrine control of the ejaculatory reflex is still not completely clarified. Recent studies on large populations indicate that the endocrine system is involved in the control of ejaculatory function and that prolactin (PRL) and testosterone play independent roles [100]. In particular, in a consecutive series of 2,531 outpatients consulting for sexual dysfunctions, PRL in the lowest quartile levels is associated with APE and anxiety symptoms [104]. Additionally, higher testosterone levels correlate with PE, while lower androgenization is related to delayed ejaculation [105].
Both hypoprolactinemia and relatively high testosterone levels cannot be considered etiologies of APE. The relationship between these hormonal abnormalities and PE is unclear. (LOE 2a)
Prostatitis
Twenty-six to 77% of men with chronic prostatitis (CP) or CPPS report early ejaculation [71,106,107]. Prostatic inflammation and chronic bacterial prostatitis have been reported as common findings in men with APE [67,108]. Considering the role of the prostate in the ejaculatory mechanism, a direct influence of the local inflammation in the pathogenesis of a few cases of APE seems possible [109].
The mechanism linking CP and PE is unknown, and there are some methodological limitations of the existing data. While physical and microbiological examination of the prostate expression in men with painful ejaculation or CP/CPPS is recommended, there is insufficient evidence to support routine screening of men with PE for this condition. (LOE 3a)
Erectile Dysfunction
Patients may mislabel or confuse the syndromes of PE and erectile dysfunction (ED). Examples include patients who say they have ED because they are unable to rapidly achieve a second erection after ejaculation. Similarly, some men with ED may self-report having PE because they rush intercourse to prevent loss of their erection and consequently ejaculate rapidly. This may be compounded by the presence of high levels of performance anxiety related to their ED, which serves to worsen their prematurity.
PE and ED may be comorbid conditions in some men [66]. In a global study of 11,205 men from 29 countries, Laumann et al. reported that a history of “sometimes” or “frequently” experiencing difficulty attaining and maintaining erections was independently predictive of “sometimes” or “frequently” experiencing early ejaculation within the past year. This relationship occurred across all regions, with odds ratios ranging from 3.7 to 11.9 [20]. Smaller studies from general and clinic populations have also reported this association between self-reported PE and self-reported ED 31,35,43,45,110–112, as determined by ED and PE patient-reported outcomes (PROs) [41,45,48]. Conversely, some population studies have not detected an association between ED and PE [30,32,44,46,113].
In an integrated analysis of two double-blind placebo controlled trials of dapoxetine for PE (DSM criteria and IELT < 2 minutes), the prevalence of ED was higher in men with APE vs. LPE (24% vs. 15%) [114]. Men with mild ED had less control over ejaculation compared with men with no ED and LPE [114]. This relationship was most pronounced in men with LPE and mild ED.
Comorbid ED is associated with more severe PE symptoms. In a stopwatch study of 78 men with LPE, McMahon reported that men with a normal Sexual Health Inventory for Men (SHIM, a metric for assessment of ED risk) had a significantly greater geometric mean IELT compared with men with an abnormal SHIM suggestive of ED (18 seconds vs. 11 seconds, respectively) [115].
As in so many other areas of PE research, interpretation of data on the association between ED and PE is limited by varied definitions of PE and the means employed to assess PE.
While ED is unlikely as a comorbidity or etiological factor for LPE, there are data to support that APE is associated with ED 114,116–119 (LOE 3b). In such cases, men may experience rapid ejaculation due to performance anxiety, or due to deliberate intensification of stimulation so as to complete ejaculation before loss of tumescence (LOE 5).
Men with comorbid ED and PE may manifest a more severe variant of each disorder; furthermore, such men may experience lower sexual satisfaction and diminished response to treatment of PE [114]. (LOE 2a)
PE in Men Who Have Sex with Men
Data on the prevalence of PE in men who have sex with men (MSM) are relatively sparse. Existing studies suggest that a substantial proportion of MSM report PE and associated sexual bother. In some cases, ejaculatory dysfunction in MSM has been associated with higher risk of sexual behavior and/or social recrimination [120]. Most contemporary studies suggest a similar prevalence of concern about early ejaculation in MSM when compared with men who have sex with women only (MSW) [44]. Some older studies have suggested that the rate of distressing ejaculation problems in MSM is lower than in MSW [121]. However, differences in relationships and sexual activities may be responsible for some of these purported differences [122].
There are no stopwatch studies of ejaculation latency in MSM with or without ejaculation concerns. While there is no compelling evidence that MSM experience ejaculatory dysfunction differently than their MSW counterparts, more research is needed.
Psychological Factors
Psychological and interpersonal factors may cause or exacerbate PE. These factors may be developmental (e.g., sexual abuse, attitudes toward sex internalized during childhood), individual psychological factors (e.g., body image, depression, performance anxiety, alexithymia), and/or relationship factors (e.g., decreased intimacy, partner conflict) 123–125. There has been limited research on causality; most studies have been cross-sectional and hence can only report association. Obviously, developmental variables are likely to predate clinical PE, but it is conceivable that an intermediate factor secondary to the developmental history mediates the development of PE.
It is plausible that psychological factors may lead to PE or vice versa. It is likely that for many men, the relationship is reciprocal with either PE or the other factor causing exacerbation of the other. For example, performance anxiety may lead to PE, which then further exacerbates the original performance anxiety. (LOE 5d)
Importance of Partners and the Impact of PE on the Partner's Sexual Function
Inclusion of the partner in the treatment process is an important but not a mandatory ingredient for treatment success [118,126]. Some patients may not understand why clinicians wish to include the partner, and some partners may be reluctant to join the patient in treatment. However, if partners are not involved in treatment, they may be resistant to changing the sexual interaction. A cooperative partner augments the power of the treatment, and this likely leads to an improvement in the couple's sexual relationship, as well as the broader aspects of their relationship. There are no controlled studies on the impact of involving partners in treating PE. However, a review of treatment studies for ED demonstrates the important role of including a focus on interpersonal factors on treatment success [127].
Men with PE have been shown to have more interpersonal difficulties than men without PE, as well as partners of men with PE reporting higher levels of relationship problems compared with partners of men without PE [59,128,129]. Men with PE feel that they are “letting their partner down” by having PE and that the quality of their relationship would improve if they did not have PE [31].
Rosen and Althof reviewed 11 observational, noninterventional studies from 1997 to 2007 that reported on the psychosocial and quality of life consequences of PE on the man, his partner, and the relationship [130]. These studies employed different methodologies and outcome measures and consisted of both qualitative and quantitative investigations. All studies consistently confirmed a high level of personal distress reported by men with PE and their female partners. Men with PE have significantly lower scores on self-esteem and self-confidence than non-PE men, and one-third of men with PE report anxiety connected to sexual situations [131]. The negative impact on single men with PE may be greater than on men in relationships as PE serves as a barrier to seeking out and becoming involved in new relationships [132].
There is evidence of the negative impact of PE on the female partner's sexuality. This has been confirmed in several epidemiological studies where PE has been found to be correlated to overall female sexual dysfunction (FSD), sex not being pleasurable, desire, arousal, and orgasmic problems as well as low sexual satisfaction and sexual distress 128,129,131,133–139. FSD may also increase the risk of the partner having PE. For example, Dogan and Dogan [140] found that 50% of the partners of women with vaginismus were found to have PE, but it was not possible to determine whether PE was actually a consequence of the vaginismus.
Both men and their partners demonstrate negative effects and interpersonal difficulty related to their PE and an overall reduction in their quality of life. (LOE 1a–3a)
Assessment of PE
History
Patients want clinicians to inquire about their sexual health [141]. Often patients are too embarrassed, shy, and/or uncertain to initiate a discussion of their sexual complaints in the HCP's office [142]. Inquiry by the HCP into sexual health gives patients permission to discuss sexual concerns and also screens for associated health risks (e.g., cardiovascular risk and ED).
Table 3 lists recommended and optional questions that patients who complain of PE should be asked [1]. The recommended questions establish the diagnosis and direct treatment considerations, and the optional questions gather detail for implementing treatment. Finally, the committee recommends that HCPs take a medical and psychosocial history. (LOE 5d)
Table 3.
Recommended and optional questions to establish the diagnosis of PE and direct treatment
| Recommended questions for diagnosis | What is the time between penetration and ejaculation (cumming)? Can you delay ejaculation? Do you feel bothered, annoyed, and/or frustrated by your premature ejaculation? |
| Optional questions: Differentiate lifelong and acquired PE | When did you first experience premature ejaculation? Have you experienced premature ejaculation since your first sexual experience on every/almost every attempt and with every partner? |
| Optional questions: Assess erectile function | Is your erection hard enough to penetrate? Do you have difficulty in maintaining your erection until you ejaculate during intercourse? Do you ever rush intercourse to prevent loss of your erection? |
| Optional questions: Assess relationship impact | How upset is your partner with your premature ejaculation? Does your partner avoid sexual intercourse? Is your premature ejaculation affecting your overall relationship? |
| Optional question: Previous treatment | Have you received any treatment for your premature ejaculation previously? |
| Optional questions: Impact on quality of life | Do you avoid sexual intercourse because of embarrassment? Do you feel anxious, depressed, or embarrassed because of your premature ejaculation? |
PE = premature ejaculation
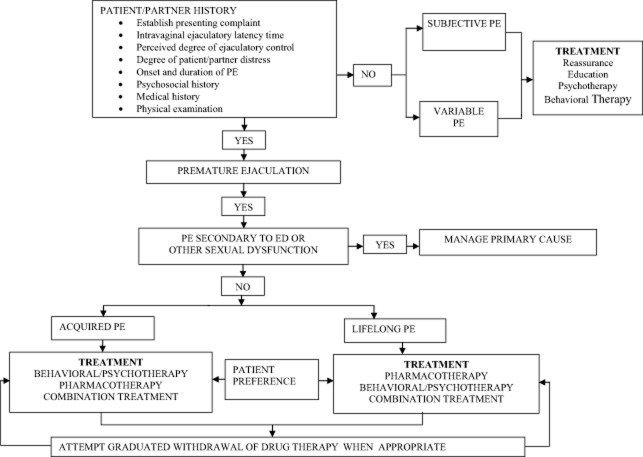
Figure 1 is a flowchart devised by Rowland et al., detailing the assessment and treatment options for subjects complaining of PE [143].
Figure 1.
Algorithm for the management of PE (with permission of D. Rowland). ED = erectile dysfunction; PE = premature ejaculation
Physical Examination
For LPE, a physical examination is advisable but not mandatory. Some patients find it reassuring for the physician to perform a hands-on physical examination. For APE, a targeted physical examination is advisable but not mandatory. The purpose of a targeted physical examination for the patient with APE is to assess for comorbidities, risk factors, and etiologies.
Stopwatch Assessment of Ejaculatory Latency (IELT)
Stopwatch measures of IELT are widely used in clinical trials and observational studies of PE, but have not been recommended for use in routine clinical management of PE [144]. Despite the potential advantage of objective measurement, stopwatch measures have the disadvantage of being intrusive and potentially disruptive of sexual pleasure or spontaneity [145]. Several studies have indicated that patient or partner self-report of ejaculatory latency correlates relatively well with objective stopwatch latency and might be useful as a proxy measure of IELT 146–148.
Because patient self-report is the determining factor in treatment seeking and satisfaction, it is recommended that self-estimation by the patient and partner of ejaculatory latency be accepted as the method for determining IELT in clinical practice. (LOE 2b)
Use of Assessment Instruments
Standardized assessment measures for PE include the use of validated questionnaires, in addition to stopwatch measures of ejaculatory latency [149]. These measures are all relatively new and were developed primarily for use as research tools. However, they may serve as valuable adjuncts for clinical screening and assessment.
Several PE questionnaires assessing lifelong and acquired subtypes have been described in the literature 150–155, although only a small number have undergone extensive psychometric testing and validation. Five validated questionnaires have been developed and published to date. Currently, there are two questionnaires that have extensive databases and meet most of the criteria for test development and validation: The Premature Ejaculation Profile (PEP) and the Index of Premature Ejaculation (IPE) [150,152]. A third brief diagnostic measure (Premature Ejaculation Diagnostic Tool [PEDT]) has also been developed, has a modest database, and is available for clinical use [154]. Two other measures (Arabic and Chinese PE questionnaires) have minimal validation or clinical trial data available [151,155]. These latter measures are not recommended for clinical use. Table 4 details these instruments in terms of number of questions, domains, and psychometric properties. The IPE, PEP, and PEDT can be found in Appendix 1.
Table 4.
Recommended patient reported outcomes for PE
| Name | Number of questions | Domain names | Reliability studies | Validity studies | Advantages | Limitations |
|---|---|---|---|---|---|---|
| Premature Ejaculation Profile (PEP) | 4 | 1. Perceived control over ejaculation 2. Satisfaction with sexual intercourse 3. Personal distress related to ejaculation 4. Interpersonal difficulty related to ejaculation | Yes | Yes | Assesses outcome Brief, easy to administer Evaluates the subjective and clinically relevant component domains | Lack of validated cutoff scores Only one question per domain |
| Index of Premature Ejaculation (IPE) | 10 | 1. Control 2. Sexual satisfaction 3. Distress | Yes | Yes | Assesses outcome Relatively brief and easy to administer Evaluates the subjective and clinically relevant domains | Lacks norms and diagnostic cutoffs |
| Premature Ejaculation Diagnostic Tool (PEDT) | 5 | None | Yes | Yes | Screening questionnaire with cutoff scores Brief and easy to administer |
PE = premature ejaculation
Depending on the specific need, the PEP or IPE continue to be the preferred questionnaire measures for assessing lifelong or acquired subtypes of PE, particularly when monitoring responsiveness to treatment. Overall, these measures may serve as useful adjuncts but should not substitute for a detailed sexual history performed by a qualified clinician. (LOE 2b).
Psychological/Behavioral, Combined Medical and Psychological, and Educational Interventions
Psychotherapy for men and couples suffering from PE has two overlapping goals. First, psychological interventions aim to help men develop sexual skills that enable them to delay ejaculation while broadening their sexual scripts, increasing sexual self-confidence, and diminishing performance anxiety. The second goal focuses on resolving psychological and interpersonal issues that may have precipitated, maintained, or be the consequence of the PE symptom for the man, partner, or couple 156–158.
Present day psychotherapy for rapid ejaculation is an integration of psychodynamic, systems, behavioral, and cognitive approaches within a short-term psychotherapy model 7,157,159–161. Treatment may be provided in an individual, couples, or group format. Unfortunately, the majority of the psychotherapy treatment outcome studies are uncontrolled, unblinded trials; few meet the requirements for evidence-based studies [156]. Most studies employed small to moderately sized cohorts who received different varieties of psychological interventions with limited or no follow-up. Additionally, the inclusion criteria utilized by these studies varied widely and included men who would not meet the ISSM PE definition.
The most frequently used behavioral treatments are the squeeze or stop–start techniques [6,162]. Both of these therapies were designed to help men recognize mid-level ranges of excitement. Men gain skills at identifying mid-level excitement by a series of graduated exercises beginning with self-stimulation, moving on to partner-hand stimulation, then to intercourse without movement, and finally to stop/start thrusting. This process gradually leads to an increase in IELT, sexual confidence, and self-esteem; although there are few controlled studies to support this claim.
Older uncontrolled studies on the squeeze technique report a failure rate of 2.2% immediately after therapy and 2.7% at the 5-year follow-up [6]. These results have not been replicated; other studies have found success rates of between 60% and 90% [163]. De Carufel and Trudel demonstrated an eightfold increase in IELT among men treated with behavioral techniques compared with a wait-list control condition [164]. A previous study found that bibliotherapy with and without phone contact as well as sex therapy (three separate groups) experienced a sixfold increase in IELT compared with a control group [165]. Treatment gains were maintained at the 3 months follow-up.
There have been two recent meta-analytic reports and one systematic review on psychotherapy for sexual dysfunctions 166–168. The first reviewed only one PE psychotherapy article and three PE combination medical and psychotherapy studies [167]. The authors concluded that “there is weak and inconsistent evidence regarding the effectiveness of psychological interventions for the treatment of premature ejaculation.” Similarly, the second study [166] only reviewed the same report and concluded that “there was no evidence for the efficacy of psychological interventions on symptom severity in patients suffering from PE.” The third review found evidence that behavioral interventions were effective in treating PE [168]. Because these meta-analyses had such stringent inclusion criterion, the majority of the PE psychotherapy studies were not included and thus the conclusions were based on a small number of studies. The PE Guidelines Committee continues to believe that psychotherapy offers men, women, and couples benefit, including the development of sexual skills, delay of ejaculation, improving relationship concerns, and sexual self-confidence.
There is some evidence to support the efficacy of psychological and behavioral interventions in the treatment of PE (LOE 2b). Future well-designed studies on the efficacy of psychotherapy are needed.
Men with VPE (irregular and inconsistent rapid ejaculation with a diminished sense of subjective control of ejaculation) should be educated and reassured. Men with SPE (those whose IELT is within the normal range but who are preoccupied by their ejaculatory control) may require a referral for psychotherapy [10]. More research is necessary to better define the efficacy of reassurance, education, and psychotherapy with these provisional subtypes.
HCPs and mental health professionals have differing levels of interest and training in treating PE. In general, all clinicians should be able to diagnose, offer support, and prescribe behavioral exercises. When the situation is complex and/or patients are not responsive to the initial intervention, clinicians should consider referring to a sexual health specialist.
Online Treatment Programs
A recent development in the psychological treatment of male and female sexual dysfunction has been the adaptation of strategies used in face-to-face treatment to online treatment packages. McCabe et al. [169] evaluated their six-session online treatment for ED and found it to be an effective treatment for ED and a suitable alternative to face-to-face therapy. Similar findings have been obtained for Internet-based treatment for FSD [170]. Although there are currently no Internet-based programs available specifically for PE, these other programs could serve as a model for the development of such online interventions. As for other sexual disorders, this would be an extremely useful future development in the treatment of PE.
Pharmacological Treatment
Several forms of pharmacotherapy have been used in the treatment of PE [171]. These include the use of topical local anesthetics (LA) [172], selective serotonin reuptake inhibitors (SSRIs) [57,174], tramadol [175], phosphodiesterase type 5 inhibitors (PDE5i) [176], and alpha adrenergic blockers [177]. The use of topical LA, such as lidocaine, prilocaine, or benzocaine, alone or in association, to diminish the sensitivity of the glans penis is the oldest known pharmacological treatment for PE [60]. The introduction of the SSRIs paroxetine, sertraline, fluoxetine, citalopram, and the tricyclic antidepressant (TCA) clomipramine has revolutionized the treatment of PE. These drugs block axonal reuptake of serotonin from the synaptic cleft of central serotonergic neurons by 5-HT transporters, resulting in enhanced 5-HT neurotransmission and stimulation of postsynaptic membrane 5-HT receptors.
Treatment with SSRIs and TCAs
PE can be treated with on-demand SSRIs such as dapoxetine or off-label clomipramine, paroxetine, sertraline, and fluoxetine, or with daily dosing of off-label paroxetine, clomipramine, sertraline, fluoxetine, or citalopram 63,178–187.
Dapoxetine
Dapoxetine has received approval for the treatment of PE in over 50 countries worldwide. It is a rapid-acting and short half-life SSRI with a pharmacokinetic profile supporting a role as an on-demand treatment for PE [181,182,184,188,189]. No drug–drug interactions associated with dapoxetine, including phosphodiesterase inhibitor drugs, have been reported [190]. In randomized controlled trials (RCTs), dapoxetine 30 mg or 60 mg taken 1–2 hours before intercourse is more effective than placebo from the first dose, resulting in a 2.5 and 3.0-fold increases in IELT, increased ejaculatory control, decreased distress, and increased satisfaction. Dapoxetine was comparably effective both in men with LPE and APE [114,184,191] and was similarly effective and well tolerated in men with PE and comorbid ED treated with PDE5i drugs [192]. Treatment-related side effects were uncommon, dose dependent, and included nausea, diarrhea, headache, and dizziness [184,189]. They were responsible for study discontinuation in 4% (30 mg) and 10% (60 mg) of subjects. There was no indication of an increased risk of suicidal ideation or suicide attempts and little indication of withdrawal symptoms with abrupt dapoxetine cessation [193].
There is Level 1a evidence to support the efficacy and safety of on-demand dosing of dapoxetine for the treatment of lifelong and APE. (LOE 1a)
Off-Label SSRIs and TCAs
Daily treatment with off-label paroxetine 10–40 mg, clomipramine 12.5–50 mg, sertraline 50–200 mg, fluoxetine 20–40 mg, and citalopram 20–40 mg is usually effective in delaying ejaculation 178–180,183,186,194. A meta-analysis of published data suggests that paroxetine exerts the strongest ejaculation delay, increasing IELT approximately 8.8-fold over baseline [195].
Ejaculation delay usually occurs within 5–10 days of starting treatment, but the full therapeutic effect may require 2–3 weeks of treatment and is usually sustained during long-term use [196]. Adverse effects are usually minor, start in the first week of treatment, and may gradually disappear within 2–3 weeks. They include fatigue, yawning, mild nausea, diarrhea, or perspiration. There are anecdotal reports that decreased libido and ED are less frequently seen in nondepressed PE men treated by SSRIs compared with depressed men treated with SSRIs [197]. Men wishing to impregnate their partners should be advised that SSRIs may affect the motility of spermatozoa and therefore should not begin treatment with an SSRI, or if on an SSRI, gradually discontinue taking it [198]. Neurocognitive adverse effects include significant agitation and hypomania in a small number of patients, and treatment with SSRIs should be avoided in men with a history of bipolar depression [199].
Systematic analysis of RCTs of antidepressants (SSRIs and other drug classes) in patients with depressive and/or anxiety disorders indicates a small increase in the risk of suicidal ideation or suicide attempts in youth but not adults 200–202. In contrast, such risk of suicidal ideation has not been found in trials with SSRIs in nondepressed men with PE 200–202. Caution is suggested in prescribing SSRIs to young adolescents with PE aged 18 years or less and to men with PE and a comorbid depressive disorder, particularly when associated with suicidal ideation [200]. Patients should be advised to avoid sudden cessation or rapid dose reduction of daily dosed SSRIs, which may be associated with an SSRI withdrawal syndrome [203].
On-demand administration of clomipramine, paroxetine, sertraline, and fluoxetine 3–6 hours before intercourse is modestly efficacious and well tolerated but is associated with substantially less ejaculatory delay than daily treatment in most studies [185,187,204,205]. On-demand treatment may be combined with either an initial trial of daily treatment or concomitant low-dose daily treatment [185].
Patients are often reluctant to begin off-label treatment of PE with SSRIs. Salonia et al. reported that 30% of patients refused to begin treatment (paroxetine 10 mg daily for 21 days followed by 20 mg as needed) and another 30% of those that began treatment discontinued it [206]. Similarly, Mondaini et al. reported that in a clinic population, 90% of subjects either refused to begin or discontinued dapoxetine within 12 months of beginning treatment [207]. Reasons given included not wanting to take an antidepressant, treatment effects below expectations, and cost.
There is Level 1a evidence to support the efficacy and safety of off-label daily dosing of the SSRIs paroxetine, sertraline, citalopram, fluoxetine, and the serotonergic tricyclic clomipramine, and off-label on-demand dosing of clomipramine, paroxetine, and sertraline for the treatment of LPE and APE. (LOE 1a)
The decision to treat PE with either on-demand dosing of dapoxetine (where available) or daily dosing of off-label SSRIs should be based upon the treating physician's assessment of individual patient requirements. Although many men with PE who engage in sexual intercourse infrequently may prefer on-demand treatment, many men in established relationships may prefer the convenience of daily medication [208]. Well-designed preference trials will provide additional insight into the role of on-demand dosing.
In some countries, off-label prescribing may present difficulties for the physician as the regulatory authorities strongly advise against prescribing for indications in which a medication is not licensed or approved. Obviously, this complicates treatment in countries where there is no approved medication and the regulatory authorities advise against off-label prescription.
Topical Local Anesthetics
The use of topical LA such as lidocaine and/or prilocaine as a cream, gel, or spray is well established and is moderately effective in delaying ejaculation 172,173,209–211. Data suggest that diminishing the glans sensitivity may inhibit the spinal reflex arc responsible for ejaculation [212]. Dinsmore et al. reported on the use of PSD502, a lidocaine–prilocaine spray currently in clinical trials that is applied to the penis at least 5 minutes before intercourse. The treated group reported a 6.3-fold increase in IELT and associated improvements in PRO measures of control and sexual satisfaction [172]. Carson et al. reported similar results in a second Phase 3 randomized controlled trial. There were minimal reports of penile hypoanesthesia and transfer to the partner due to the unique formulation of the compound [172]. Other topical anesthetics are associated with significant penile hypoanesthesia and possible transvaginal absorption, resulting in vaginal numbness and resultant female anorgasmia unless a condom is used [210].
There is Level 1a evidence to support the efficacy and safety of off-label on-demand label topical anesthetics in the treatment of LPE. (LOE 1a)
PDE5i
PDE5i, sildenafil, tadalafil, and vardenafil are effective treatments for ED. Several authors have reported using PDE5is alone or in combination with SSRIs as a treatment for PE 176,213–215. Although systematic reviews of multiple studies have failed to provide robust evidence to support a role for PDE5i in the treatment of PE, with the exception of men with PE and comorbid ED [216,217], recent well-designed studies do support a potential role for these agents suggesting a need for further evidence-based research [176,216].
There is some evidence to support the efficacy and safety of off-label on-demand or daily dosing of PDE5is in the treatment of LPE in men with normal erectile function (LOE 4d). Treatment of LPE with PDE5is in men with normal erectile function is not recommended, and further evidence-based research is encouraged to understand conflicting data.
Table 5 is a summary of recommended pharmacological treatments for PE.
Table 5.
Summary of recommended pharmacological treatments for premature ejaculation
| Drug | Daily dose/on demand | Dose | IELT fold increase | Side effects | Status | Level of evidence |
|---|---|---|---|---|---|---|
| Oral Therapies | ||||||
| Dapoxetine [184] | On demand | 30–60 mg | 2.5–3 | Nausea Diarrhea Headache Dizziness | Approved in some countries | 1a |
| Paroxetine [186] | Daily dose | 10–40 mg | 8 | Fatigue Yawning Nausea Diarrhea Perspiration Decreased Sexual Desire Erectile Dysfunction | Off label | 1a |
| Clomipramine [178,180] | Daily dose | 12.5–50 mg | 6 | Off label | 1a | |
| Sertraline [183] | Daily dose | 50–200 mg | 5 | Off label | 1a | |
| Fluoxetine [194] | Daily dose | 20–40 mg | 5 | Off label | 1a | |
| Citalopram [179] | Daily dose | 20–40 mg | 2 | Off label | 1a | |
| Paroxetine [185] | Daily dose for 30 days and then on demand | 10–40 mg | 11.6 | Off label | 1a | |
| Paroxetine [185] | On demand | 10–40 mg | 1.4 | Off label | 1a | |
| Clomipramine [187] | On demand | 12.5–50 mg | 4 | Off label | 1a | |
| Topical therapy | ||||||
| Lidocaine/Prilocaine [210] | On demand | 25 mg/gm lidocaine 25 mg/gm prilocaine | 4–6.3 | Penile numbness Partner genital numbness Skin irritation Erectile dysfunction | Off label | 1a |
Other Pharmacological Treatments
Tramadol
Tramadol has been investigated as a potential off-label therapy for PE, with several studies demonstrating efficacy. The major metabolite, M1, has a 200-fold increased affinity for the μ-opioid receptor, which likely accounts for the analgesic effects achieved [218]. Because of the relatively long half-lives of tramadol (6 hours) and the M1 metabolite (9 hours), patients may be at decreased risk of developing addiction compared with other μ-opioid receptor agonists. These pharmacokinetic properties require dose adjustment in patients with hepatic or renal impairments. Although the mechanism of action is not completely described, the efficacy of tramadol may be secondary to anti-nociceptive and anesthetic-like effects, as well as via central nervous system modulation through inhibition of serotonin and noradrenaline reuptake 218–220.
Several studies have demonstrated improved IELTs with varying doses of daily or on-demand tramadol therapy. The first reported use of on demand tramadol for PE evaluated 64 patients in a blinded, randomized trial. A 50 mg dose vs. placebo was administered 2 hours prior to anticipated sexual activity over an 8-week period [219]. Results demonstrated an absolute increase in IELT from 19–21 seconds pretreatment to 243 seconds posttreatment (placebo 34 seconds, P < 0.001). Satisfaction was similarly improved with tramadol over placebo, as measured by the satisfaction domain of the International Index of Erectile Function questionnaire (14 vs. 10, P < 0.05).
Three subsequent investigations evaluated on-demand tramadol using blinded, crossover, and placebo-controlled study designs [175,221,222]. Following administration of 25–50 mg of tramadol over an 8–12-week period, patients experienced a 4–7.3-fold increase in IELT from baseline compared with a 1.7-1.8 fold increase with placebo (absolute change from 36–70 to 155–442 seconds) [175,222]. Alghobary and colleagues further investigated temporal benefits of therapy and reported slight attenuation of efficacy over time [221]. Results demonstrated a 7.2-fold increase (18 seconds pretreatment to 130 seconds) at 6 weeks of tramadol 50 mg, which decreased to 5.7-fold increase (102 seconds) at 12 weeks (P = 0.02 between time points). In comparing efficacy with paroxetine, patients receiving daily paroxetine achieved an 11.1-fold improvement (6 weeks), which further increased to 22.1-fold improvement (12 weeks). These findings suggest a need for further long-term and comparative evaluations to assess the efficacy of tramadol over time and against alternative therapies.
In the largest, blinded, placebo-controlled randomized trial performed to date, Bar-Or and colleagues evaluated the efficacy of orally disintegrating tramadol (62 mg and 89 mg) administered within 2 minutes of anticipated intercourse [223]. Results from 604 patients over 12 weeks of therapy demonstrated a clinically small, although statistically significant improvement in IELT (1.6, 2.4, and 2.5-fold increases for placebo, 62 mg and 89 mg, respectively) (P < 0.001 for all comparisons). A more recent study, evaluating 300 patients randomized to tramadol hydrochloride capsules 25, 50, or 100 mg demonstrated a dose-response effect [224]. Reported IELT increased from a mean of 174 seconds pretreatment to 790 (25 mg), 1,405 (50 mg), and 2,189 (100 mg) seconds, equating to a 4.5, 8.1, and 12.6-fold increase, respectively. Although the absolute increase in IELT was significantly elevated compared with other contemporary studies, this may be secondary to higher baseline IELTs with the study population (mean 174 seconds, standard deviation 54 seconds). See Table 6 for a summary of available studies evaluating the efficacy of tramadol on demand for the off-label treatment of PE.
Table 6.
Summary table of studies evaluating the efficacy of tramadol for the treatment of premature ejaculation
| Study | N | Design | Dosage (mg) | Duration (weeks) | Pre-tx IELT (sec) | Post-tx IELT (sec) | Mean change (sec) | Fold increase |
|---|---|---|---|---|---|---|---|---|
| Safarinejad (2006) [219] | 64 | RCT, placebo, blinded | 50 | 8 | 19 | 243 | 224 | 13 |
| Salem (2008) [222] | 60 | Crossover, placebo, blinded | 25 | 8 | 70 | 442 | 372 | 6.3 |
| Alghobary (2010) [221] | 35 | Crossover, comparison (paroxetine) | 50 | 12 | 36 | 180, 133 | 144, 97 | 7.3, 5.7 |
| Kaynar (2012) [175] | 60 | Crossover, placebo, blinded | 25 | 8 | 39 | 155 | 116 | 4 |
| Bar-Or (2012) [223] | 604 | RCT, placebo, blinded | 62, 89 | 12 | 58 | 134, 151 | 76, 93 | 2.4, 2.5 |
| Eassa (2013) [224] | 300 | Randomized, dose response | 25, 50, 100 | 24 | 174 | 790, 1,405, 2,189 | 616, 1,231, 2,015 | 4.5, 8.1, 12.6 |
RCT = randomized controlled trial; tx = treatment
Tramadol may be an effective option for the treatment of PE. However, it may be considered when other therapies have failed because of the risk of addiction and side effects. It should not be combined with an SSRI because of the risk of serotonin syndrome, a potentially fatal outcome [225]. Further well-controlled studies are required to assess the efficacy and safety of tramadol in the treatment of PE patients. (LOE2)
Oxytocin
Oxytocin has been found to shorten ejaculation latency and post-ejaculatory refractory period when it is infused into the cerebral ventricle of male rats and increases latencies of mount and intromission when administered into the intracerebroventricular space [226,227]. Similar to central administration, systemic oxytocin administration is demonstrated to shorten ejaculation latency and post-ejaculatory interval in sexually active male rats [226,227]. These findings suggested a potential role for anti-oxytocin drugs in treatment of PE. Argiolas et al. demonstrated that central administration of a selective oxytocin receptor antagonist inhibits sexual behavior, including ejaculation, in male rats [228]. Clement et al. confirmed that intraventricular administration of oxytocin antagonist dose-dependently inhibited sexual responses, whereas they also found that systemic administration of oxytocin antagonist did not make a significant change [229]. In a recent study, the same group demonstrated that a highly selective, non-peptide oxytocin antagonist (GSK557296) inhibits ejaculation when administered both peripherally and centrally [75]. The authors concluded that targeting central oxytocin receptors with a highly selective antagonist might be a promising approach for the treatment of PE.
A double-blind, placebo control study of epelsiban, a selective oxytocin receptor antagonist, failed to show either clinical or statistical differences in IELT from placebo in men with PE [230]. In an attempt to investigate the effects of polymorphisms in oxytocin and vasopressin receptor genes on ejaculatory function, Jern et al. could not detect any clear-cut gene variant revealing ejaculatory dysfunction and concluded that oxytocin receptor genes are unlikely targets for future pharmaceutical treatment of PE [92].
Intraventricular administration of oxytocin antagonist inhibits sexual behavior in animal studies; however in one human study, an oxytocin antagonist failed to clinically or statistically improve IELT. Further human studies are necessary. (LOE 4)
Cryoablation and Neuromodulation of the Dorsal Penile Nerve
Ablation and modulation of the dorsal penile nerve, which is the main afferent somatosensory pathway of the penis [231], have been suggested to be an effective treatment option for PE [232,233]. David Prologo et al. [232] reported on the unilateral computed tomography-guided percutaneous cryoablation of the dorsal penile nerve on IELT and PEP outcomes in 24 men with PE. Baseline average IELT significantly increased (from 54.7 ± 7.8 to 140.9 ± 83.6 at the end of the first year, P < 0.001) and PEP results were also improved. The authors noted that the majority of the subjects said that they would undergo the procedure again.
In another study, Basal et al. [233] investigated the clinical utility of percutaneous pulsed radiofrequency ablation of bilateral dorsal penile nerves in 15 patients with LPE. The authors described a significant increase in the mean IELT 3 weeks after the procedure (18.5 ± 17.9 vs. 139.9 ± 55.1 seconds) and PRO measures improved. However, further expanded clinical trials are necessary before such modalities can be recommended for treating PE.
Neuromodulation of the dorsal penile nerve is an invasive and irreversible procedure, which is associated with an increase in the IELT. However, safety of this treatment modality needs to be determined before this procedure can be recommended for treating PE patients. (LOE 4)
Intracavernosal Injection for PE
There is limited evidence regarding the efficacy of intracavernosal vasoactive drug injection for the treatment of PE. In one study, which included eight PE patients, a mixture of phentolamine mesylate (1.0 mg/mL) and papaverine hydrochloride (30 mg/mL) was injected. All patients reported satisfaction with the results of this treatment, but ejaculation delay was not objectively measured [234].
Intracavernosal injection of vasoactive drugs is not recommended for the treatment of PE. (LOE 4)
Acupuncture
One randomized placebo-controlled clinical study compared effectiveness of acupuncture therapy (twice a week) with paroxetine (20 mg/day) and placebo (sham acupuncture) in the treatment of PE [235]. The authors included 90 patients with PE and demonstrated that acupuncture had a significantly stronger ejaculation delaying effect than placebo (65.7 vs. 33.1 seconds), although it was less effective than daily paroxetine (82.7 seconds) (P = 0.001). Similarly, the PRO measures showed an improvement in the acupuncture and paroxetine groups.
There are limited positive data regarding the effectiveness of acupuncture therapy. (LOE 3b)
Preclinical Studies for PE
Several agents have been studied in animal models for treating PE. A potent SSRI (DA-8031) significantly inhibited ejaculation after oral and intravenous administration in both para-chloroamphetamine and meta-chlorophenylpiperazine-mediated ejaculation rat models [236]. In another study using a rat model, DA-8031 administration resulted in inhibition of the expulsion phase of ejaculation by bulbospongiosus muscle activity modulation and impairment of the emission phase by blocking the seminal vesicular pressure rise [237].
Modafinil (diphenylmethyl sulphinyl-2-acetamide) is an agent that is used for the treatment of narcolepsy. In a behavioral rat model, Marson et al. [238] demonstrated that modafinil (30 mg/kg and 100 mg/kg) produced a significant delay in ejaculation. The delay in ejaculation was accompanied by an increase in the number of intromissions without any change in the mount or intromission latency.
Because the bulbospongiosus muscle plays a pivotal role in the expulsion phase of ejaculation, decreasing its contractile activity with injection of botulinum toxin may be of benefit in treating PE [239]. In an animal model Serefoglu et al. [240] demonstrated that botulinum toxin A injection (0.5–1 U/mL) into the bulbospongiosus muscle bilaterally significantly increased ejaculatory latency in male rats.
Combining Psychological and Pharmacological Treatment
Combining medical and psychological interventions harnesses the power of both therapies to provide patients with rapid symptom amelioration, while the psychological and interpersonal issues that either precipitated or maintained the symptom are addressed [143,157,241,242]. There are three studies reporting on combined pharmacological and behavioral treatment for PE 243–245 and one study reporting on consecutive treatment with pharmacotherapy followed by behavior therapy [246]. Each study used a different medication—sildenafil, citalopram, clomipramine, or paroxetine (in the consecutive study). Pharmacotherapy was given in conjunction with a behavioral treatment and compared with pharmacotherapy alone. In all three studies, combination therapy was superior to pharmacotherapy alone on either IELT and/or the Chinese IPE.
For ED, combined treatments have also been found to be more effective than either medical or psychological treatments alone [167,247,248]. Factors that are not addressable by pharmacotherapy alone can be attended to such as: (i) patient factors (performance anxiety, self-confidence); (ii) partner factors (partner sexual dysfunction); (iii) relationship factors (conflict, lack of communication); (iv) sexual factors in the relationship (sexual scripts, sexual satisfaction); and (v) contextual factors (life stressors).
Combining a medical and psychological approach may be especially useful in men with APE where there is a clear psychosocial precipitant or lifelong cases where the individual or couple's issues interfere in the medical treatment and success of therapy. Similarly, in men with PE and comorbid ED, combination therapy may also be helpful to manage the psychosocial aspects of these sexual dysfunctions. (LOE 2a)
Role of Education and Coaching
Education (or coaching) on PE may be useful to attend to aspects of PE that are not treated with medication [157,241,242,249]. Providing education on the prevalence of PE and general population IELT may help to dispel myths. Additionally, education may help men with PE to not avoid sexual activity, to discuss issues with their partner, or limit their sexual repertoire.
Educational or coaching strategies are designed to give the man the confidence to try the medical intervention, reduce performance anxiety, and modify his maladaptive sexual scripts. (LOE 5d)
Lifelong PE
As LPE is likely to have an organic etiology, a medical intervention with basic psycho-education is initially recommended [10,250].
If the PE has resulted in psychological and relationship concerns, graded levels of patient and couple counseling, guidance, and/or relationship therapy may be a useful adjunct to the medical intervention. (LOE 1a)
Acquired PE
It is recommended that HCPs utilize a combination medical and psychological approach where feasible [251]. Men desire an immediate effect from therapy; therefore pharmacotherapy and amelioration of associated disease factors such as ED will be extremely helpful.
Education on the nature of PE, helping men improve ejaculatory control with behavioral exercises, addressing restricted/narrow sexual behavioral patterns, and resolving interpersonal issues are likely to be of significant help to men with APE. Once the man's self confidence and sense of control have improved, it may then be possible to reduce or discontinue the medical intervention. (LOE 5d)
Role of the Primary Care Clinician
Primary care providers are usually the first line of contact for a patient with the health care system, including for the diagnosis and management of sexual problems. This role includes (i) initial recognition and evaluation of any undiagnosed sign, symptom, or health concern (the “undifferentiated” patient); (ii) health promotion including disease prevention, health maintenance, counseling, patient education, chronic illness management, and patient advocacy; and (iii) coordination of care promoting effective communication with patients and encouraging the patient to be a partner in health [252]. This model of care is not limited by problem origin, organ system, or diagnosis.
Primary care providers (PCP) are the ideal group to assist the patient with sexual difficulties for several reasons including: (i) the value of the longitudinal and personal relationships with patients; (ii) the multifactorial issues around sexual problems that can be appropriately evaluated by a generalist clinician; and (iii) the long-term follow-up routine in primary care is well suited to being certain that a sexual dysfunction is resolved. The main responsibility of the PCP is to recognize PE and enable the patient to feel comfortable about getting help, either in the primary care setting or through an effective referral. PCPs can normalize and universalize the inquiry about sexual concerns and then use screening questions to identify PE. PCPs who have effective communication skills regarding sexual function and who are knowledgeable about first-line treatments can initiate the workup and treatment plan.
A urologist can be useful when the patient presents with a difficult or complex problem, with a genital anatomic problem, with prostatitis or lower urinary tract symptom, or with ED or painful intercourse due to a structural condition such as phimosis. The endocrinologist is useful in the presence of sexual dysfunctions comorbid with hormonal and metabolic abnormalities. A mental health professional with experience in sexual problems can work collaboratively with the clinician by: (i) resolving the sexual difficulty; (ii) teasing out important history; (iii) educating the patient and partner; (iv) suggesting sexual enhancement techniques; and (v) helping the couple resolve individual as well as relationship problems.
Referral to or collaboration with a psychologist or sexual health specialist may be appropriate at various times when managing a man with PE. The major factors in determining when a consultation is needed include (i) the PCP's comfort in discussing PE and managing treatment options; (ii) the depth of the psychosocial and sexual issues involved; and (iii) the success or failure of the PCPs initial intervention efforts. Specific instances in which subspecialty assistance is often useful include (i) treatment failure; (ii) anatomic or complex hormonal issues; (iii) complex issues around sex and/or partnerships; (iv) severe psychological problems; or (v) anytime the treating physician feels that help is needed.
The management algorithm “ALLOW,” an outgrowth of the PLISSIT model (permission, limited information, specific suggestions, and intensive therapy) [253] can help PCPs talk with their patients about sexual health problems and refer patients when appropriate [254]. The physician begins by “Asking” about a patient's sexual life and “Legitimizing” the importance and potential impact of sexual problems to the patient. The physician then considers his/her “Limitations” with regard to managing the sexual dysfunction and may refer the patient to a sexual health specialist for further evaluation and management. Conversely, if the physician feels comfortable managing the patient's issue(s), he or she then “Opens” up the issue(s) for further discussion, and the physician and the patient “Work together to develop a management plan.” This methodical approach to giving the patient permission to discuss sexual issues can be accomplished in as brief or as long a time as the physician has available.
Comanagement by the less experienced PCP along with an appropriate sexual health specialist is an excellent way to manage the patient's issues and to increase the PCPs understanding of PE. Good communication between clinicians can improve patient outcomes and understanding of planned treatments and monitoring measures. Comanagement can be optimized by a clear understanding between the PCP and the sexual health specialist about who will do what. This kind of communication can be ensured by creating “referral agreements” in which a specific referral guideline is used and the responsibilities and activities of each clinician are clearly spelled out [255].
Conclusion
In 2009, the ISSM convened a select panel of experts to develop an evidence-based set of guidelines for patients suffering from LPE [1]. That document concluded by recognizing the continually evolving nature of clinical research and recommended a subsequent guideline review and revision every fourth year.
As per that recommendation, the ISSM convened a second multidisciplinary panel of experts in April 2013. This manuscript summarizes the committee's work in reviewing and updating the original recommendations. Table 7 lists all the relevant recommendations promulgated by the second PE Guidelines Committee including issues of definition, prevalence, subtypes, etiology, assessment, and treatment.
Table 7.
Summary of PE guideline recommendations
| Topic | Recommendation |
|---|---|
| Definition of lifelong PE | A male sexual dysfunction characterized by ejaculation that always or nearly always occurs prior to or within about 1 minute of vaginal penetration, either present from the first sexual experience or following a new bothersome change in ejaculatory latency, and the inability to delay ejaculation on all or nearly all vaginal penetrations, and negative personal consequences, such as distress, bother, frustration, and/or the avoidance of sexual intimacy. |
| Prevalence of PE | Based on these data and the ISSM and DSM-5 definition of PE, in terms of an IELT of about 1 minute, the prevalence of lifelong PE is unlikely to exceed 4% of the general population. |
| Average ejaculatory latency | In multinational studies, the median IELT is 5.4 minutes. Median IELT may differ between countries. |
| Quality of life | Negative effects on quality of life and interpersonal difficulty related to their PE have been consistently been reported by men and their partners. |
| Etiology | The etiology of premature ejaculation is not known. To date, no biological factor has been shown to be causative in the majority of men with PE. |
| Assessment | The committee agreed that there was inadequate evidence to recommend screening or case finding for PE, either in a general population or in any subpopulation. However, it is recommended that men with ED be screened for PE. |
| It is recommended that clinicians utilize the screening questions in Table 3 and that clinicians take a medical and psychosocial history. | |
| Because patient self-report is the determining factor in treatment seeking and satisfaction, it has been recommended that self-estimation by the patient and partner of ejaculatory latency be routinely assessed in clinical practice when PE is present. | |
| The PEP or IPE are currently the preferred questionnaire measures for assessing PE, particularly in the context of monitoring responsiveness to treatment. | |
| For lifelong PE, a physical examination is highly advisable but not mandatory and should be conducted in most if not all patients. | |
| For acquired PE, a targeted physical examination is mandatory to assess for associated/causal diseases such as ED, thyroid dysfunction, or prostatitis. | |
| Treatment | There is robust evidence to support the efficacy and safety of on-demand dosing of dapoxetine for the treatment of lifelong and acquired PE. It has been approved in some countries. |
| There is robust evidence to support the efficacy and safety of off-label daily dosing of the SSRIs paroxetine, sertraline, citalopram, fluoxetine, and the serotonergic tricyclic clomipramine, and off-label on-demand dosing of clomipramine, paroxetine, and sertraline for the treatment of lifelong and acquired PE. | |
| There is good evidence to support the efficacy and safety of off-label on-demand topical anesthetics in the treatment of lifelong PE. | |
| There is some evidence to support the efficacy and safety of off-label on-demand or daily dosing of PDE5is in the treatment of lifelong PE in men with normal erectile function. Treatment of lifelong PE with PDE5is in men with normal erectile function is not recommended, and further evidence-based research is encouraged to further understand conflicting data. | |
| Tramadol may be an effective option for the treatment of PE. However, it may be considered when other therapies have failed because of the risk of addiction and side effects. It should not be combined with an SSRI because of the risk of serotonin syndrome, a potentially fatal outcome. Further, well-controlled studies are required to assess the efficacy and safety of tramadol in the treatment of PE patients. | |
| There is modest evidence supporting the efficacy of psychological/behavioral interventions in the treatment of PE. | |
| Combining pharmacological and psychological/behavioral treatments may be especially useful in men with acquired premature ejaculation where there is a clear psychosocial precipitant or lifelong cases where the individual or couple's responses to PE are likely to interfere in the medical treatment and ultimate success of therapy. Similarly, in men with PE and comorbid ED, combination therapy may also be helpful to manage the psychosocial aspects of these sexual dysfunctions. | |
| There is reliable evidence to support the treatment of PE and comorbid ED with ED pharmacotherapy. There is Level 3c evidence to support the treatment of PE and comorbid ED with ED pharmacotherapy in combination with PE pharmacotherapy. | |
| Selective dorsal nerve neurotomy or glans penis augmentation using hyaluronic acid gel may be associated with permanent loss of sexual function and is not recommended in the management of PE. | |
| Outcome | Treatment outcome can be addressed in one simple, brief, and validated question known as the Clinical Global Impression of Change (CGIC). It asks patients, “Compared to before starting treatment, would you describe your premature ejaculation problem as: much worse, worse, slightly worse, no change, slightly better, better, or much better?” |
DSM-5 = Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; ED = erectile dysfunction; IELT = intravaginal ejaculatory latency time; ISSM = International Society of Sexual Medicine; IPE = Index of Premature Ejaculation; PDE5i = phosphodiesterase type 5 inhibitor; PE = premature ejaculation; PEP = Premature Ejaculation Profile; SSRI = selective serotonin reuptake inhibitor
Development of guidelines is an evolutionary process that continually reviews data and incorporates the best new research. We expect that future research will lead to a more complete understanding of the pathophysiology as well as new efficacious and safe treatments for this sexual dysfunction. Therefore, it is strongly recommended that these guidelines again be reevaluated and updated in 4 years.
Finally, it is important to keep in mind that PE causes significant personal and interpersonal distress to the man, his partner, and the couple. We are hopeful that these guidelines will assist clinicians in accurately diagnosing and managing their patients who present with complaints of PE.
Appendix 1
Index of Premature Ejaculation (IPE)
These questions ask about the effects your sexual problems have had on your sex life over the past 4 weeks. Please answer the following questions as honestly and clearly as possible. In answering these questions, the following definitions apply:
Sexual intercourse is defined as vaginal penetration (you entered your partner).
Ejaculation is the ejection of semen from the penis.
Control is ejaculating when you are ready.
Distress means how frustrated, disappointed, or bothered you are by your premature ejaculation.
Mark only one box per question.
-
Over the past 4 weeks, when you had sexual intercourse, how often did you have control over when you ejaculated?
□ No sexual intercourse (not applicable)
□ Almost always or always
□ More than half the time
□ About half the time
□ Less than half the time
□ Almost never or never
-
Over the past 4 weeks, when you had sexual intercourse, how much confidence did you have over when you ejaculated?
□ No sexual intercourse (not applicable)
□ High confidence
□ Moderately high confidence
□ Neither high nor low confidence
□ Moderately low confidence
□ Low confidence
-
Over the past 4 weeks, when you had sexual intercourse, how often was it satisfactory for you?
□ No sexual intercourse (not applicable)
□ Almost always or always
□ More than half the time
□ About half the time
□ Less than half the time
□ Almost never or never
-
Over the past 4 weeks, when you had sexual intercourse, how satisfied were you with your sense of control over when you ejaculated?
□ No sexual intercourse (not applicable)
□ Very satisfied
□ Somewhat satisfied
□ Neither satisfied nor dissatisfied
□ Somewhat dissatisfied
□ Very dissatisfied
-
Over the past 4 weeks, when you had sexual intercourse, how satisfied were you with the length of intercourse before ejaculation?
□ No sexual intercourse (not applicable)
□ Very satisfied
□ Somewhat satisfied
□ Neither satisfied nor dissatisfied
□ Somewhat dissatisfied
□ Very dissatisfied
-
Over the past 4 weeks, how satisfied have you been with your sex life overall?
□ No sexual intercourse (not applicable)
□ Very satisfied
□ Somewhat satisfied
□ Neither satisfied nor dissatisfied
□ Somewhat dissatisfied
□ Very dissatisfied
-
Over the past 4 weeks, how satisfied have you been with your sexual relationship with your partner?
□ No sexual intercourse (not applicable)
□ Very satisfied
□ Somewhat satisfied
□ Neither satisfied nor dissatisfied
□ Somewhat dissatisfied
□ Very dissatisfied
-
Over the past 4 weeks, how much pleasure has sexual intercourse given you?
□ No sexual intercourse (not applicable)
□ High pleasure
□ Moderate high pleasure
□ Neither high nor low pleasure
□ Moderately low pleasure
□ Low pleasure
-
Over the past 4 weeks, how distressed (frustrated) were you by how long you lasted before you ejaculated?
□ No sexual intercourse (not applicable)
□ Extremely distressed
□ Very distressed
□ Moderately distressed
□ Slightly distressed
□ Not at all distressed
-
Over the past 4 weeks, how distressed (frustrated) have you been about your control over ejaculation?
□ No sexual intercourse (not applicable)
□ Extremely distressed
□ Very distressed
□ Moderately distressed
□ Slightly distressed
□ Not at all distressed
Premature Ejaculation Profile (PEP Items)
| Over the past month, was your control over ejaculation during sexual intercourse: | ||||
| □ Very poor | □ Poor | □ Fair | □ Good | □ Very good |
| Over the past month, was your satisfaction with sexual intercourse: | ||||
| □ Very poor | □ Poor | □ Fair | □ Good | □ Very good |
| Over the past month, how distressed were you by how fast you ejaculated during sexual intercourse? | ||||
| □ Not at all | □ A little | □ Moderately | □ Quite a bit | □ Extremely |
| Over the past month, to what extent did how fast you ejaculated during sexual intercourse cause difficulty in your relationship with your partner? | ||||
| □ Not at all | □ A little | □ Moderately | □ Quite a bit | □ Extremely |
PE Diagnostic Tool (PEDT)
Patient Instructions
This next questionnaire is designed to help identify men who may have a problem with ejaculating too soon during sexual activity. Even if you do not have difficulties, please answer all the questions:
Please mark X in the box that best represented you answer for each of the questions below.
Please mark only one box for each question.
While your experiences may change from time to time, please report your general experiences with intercourse.
Definition: Ejaculation here refers to ejaculation (release of semen) after penetration (when your penis enters your partner).
| Not difficult at all | Somewhat difficult | Moderately difficult | Very difficult | Extremely difficult | |
|---|---|---|---|---|---|
| 1) How difficult is it for you to delay ejaculation? | □ 0 | □ 1 | □ 2 | □ 3 | □ 4 |
| Almost never or never (0%) | Less than half the time (25%) | About half the time (50%) | More than half the time (75%) | Almost always or always (100%) | |
| 2) Do you ejaculate before you wish? | □ 0 | □ 1 | □ 2 | □ 3 | □ 4 |
| 3) Do you ejaculate with very little stimulation? | □ 0 | □ 1 | □ 2 | □ 3 | □ 4 |
| Not at all | Slightly | Moderately | Very | Extremely | |
| 4) Do you feel frustrated because of ejaculating before you want to? | □ 0 | □ 1 | □ 2 | □ 3 | □ 4 |
| 5) How concerned are you that your time to ejaculation leaves your partner sexually unfulfilled? | □ 0 | □ 1 | □ 2 | □ 3 | □ 4 |
Conflict of Interest
| Stanley E. Althof | Allergan, Consultant, Advisory Board, Principal Investigator |
| Abvie, Consultant | |
| Eli Lilly, Consultant | |
| Ixchelsis, Consultant | |
| Menarini, Speaker | |
| Palitan, Advisory Board | |
| Plethora, Consultant | |
| Sprout, Advisory Board, Consultant | |
| Trimel, Principal Investigator | |
| Chris G. McMahon | Johnson & Johnson, Consultant, Principal Investigator, Advisory Board Member, Speaker |
| Menarini Group, Principal Investigator, Advisory Board Member, Speaker | |
| Bayer Schering, Investigator, Advisory Board, Speaker | |
| Plethora Solutions, Advisory Board, Speaker | |
| Ixchelsis, Consultant | |
| Marcel D. Waldinger | Emotional Brain B.V., Advisory Board |
| Menarini Netherlands, Advisory Board | |
| Pound International Ltd., Advisory Board | |
| Ege Can Serefoglu | Allergan, Consultant |
| Alan Shindel | Elsevier |
| International Society of Sexual Medicine | |
| International Society for the Study of Women's Sexual Health | |
| Sexual Medicine Society of North America | |
| Strategic Science and Technology, LLC | |
| Ganesh Adaikan | Menarini, Consultant |
| Asia-Pacific Men's Health Council | |
| Edgardo Becher | Eli Lilly, Speaker, Investigator |
| GSK, Speaker, Advisory Board | |
| Pfizer, Speaker | |
| John Dean | Plethora Pharmaceuticals, Consultant or Lecturer |
| The Urology Company, Consultant or Lecturer | |
| Shianogi Pharmaceuticals, Consultant or Lecturer | |
| Repros Pharmaceuticals, Consultant or Lecturer - | |
| Emotional Brain BV (The Netherlands), Consultant or Lecturer | |
| Spimaco (Saudi Arabia), Consultant or Lecturer | |
| Francois Giuliano | Pfizer, Lecturer |
| Eli Lilly, Lecturer, Investigator and Consultant | |
| Menarini, Lecturer | |
| Allergan, Consultant | |
| Menarini, Consultant | |
| Sanofi, Consultant | |
| Bayer-Schering, Investigator and Consultant | |
| Johnson & Johnson, Investigator and Consultant | |
| GSK, Investigator and Consultant | |
| Wayne J.G. Hellstrom | American Medical Systems, Consultant or Advisor |
| Andromedical, Consultant or Advisor | |
| Auxilium, Meeting Participant, Lecturer, Consultant, Investigator, Advisor | |
| Allergan, Consultant or Advisor, Scientific Study or Trial | |
| Coloplast, Consultant or Advisor, Investigator | |
| Cook, Consultant or Advisor, Lecturer | |
| Endo, Consultant or Advisor, Investigator, Lecturer | |
| Johnson & Johnson, Consultant or Advisor, Meeting Participant or Lecturer, Investigator | |
| Lilly, USA, Consultant or Advisor, Lecturer; NIH – Board Member, Officer, Trustee | |
| Slate Pharmaceuticals, Inc., Lecturer, Advisor, and Investigator | |
| Theralogix, Board Member, Officer, Trustee | |
| VIVUS, Advisor/Consultant, Investigator, Lecturer | |
| Annamaria Giraldi | Eli Lilly, Speaker |
| Emotional Brain, Advisory Board; | |
| Apricus Bioscience, Advisory Board | |
| Sidney Glina | Eli Lilly, Principal Investigator, Speaker, Advisory Board |
| Astra Zeneca, Principal Investigator | |
| Bayer, Speaker | |
| Pfizer, Speaker | |
| Besins, Advisory Board | |
| Luca Incrocci | No conflicts to report. |
| Emmanuele Jannini | Bayer, Speaker, Consultant, Grant Recipient |
| Bessins, Speaker, Consultant, Grant Recipient | |
| Isba, Speaker, Consultant, Grant Recipient | |
| Lilly, Speaker, Consultant, Grant Recipient | |
| Menarini, Speaker, Consultant, Grant Recipient | |
| Pfizer, Speaker, Consultant, Grant Recipient | |
| Marita McCabe | Menarini, Advisory Board |
| Sharon Parish | Emotional Brain, Advisory Board |
| Shinogi, Advisory Board | |
| Apricus, Advisory Board | |
| Strategic Science and Technology, Advisory Board | |
| Pfizer, Advisory Board | |
| David Rowland | No conflicts to report. |
| R. Taylor Segraves | S1Biopharm, Advisor and Investor |
| Ira Sharlip | Aborption Pharmaceuticals, Consultant |
| Eli Lilly, Speaker and Consultant | |
| Plethora, Consultant | |
| Pfizer, Speaker and Consultant | |
| Luis Otavio Tores | Eli Lilly, Speaker and Advisory Board |
| GSK, Speaker | |
| Janssen, Speaker | |
| Pfizer, Speaker |
References
- 1.Althof S, Abdo C, Dean J, Hackett G, McCabe M, McMahon CG, Rosen RC, Sadovsky R, Waldinger MD, Becher E, Broderick G, Buvat J, Goldstein I, El-Meliegy A, Giuliano F, Hellstrom W, Incrocci L, Jannini EA, Park K, Parish S, Porst H, Rowland D, Segraves R, Sharlip I, Simonelli C, Tan HM. International Society for Sexual Medicine's Guidelines for the diagnosis and treatment of premature ejaculation. J Sex Med. 2010;7:2947–2969. doi: 10.1111/j.1743-6109.2010.01975.x. [DOI] [PubMed] [Google Scholar]
- 2.Centre for Evidence Based Medicine. Oxford Centre for Evidence Based Medicine levels of evidence. 2001. Available at: http://www.cebm.net (accessed August 5, 2013)
- 3.Jannini E, Eardley I, Sand M, Hackett G. Clinical and basic science research in sexual medicine must rely, in part, on pharmaceutical funding? J Sex Med. 2010;7:2331–2337. doi: 10.1111/j.1743-6109.2010.01898.x. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th edition, text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 5.Colpi G, Weidner W, Jungwirth A, Pomerol J, Papp G, Hargreave T, Dohle G. EAU guidelines on ejaculatory dysfunction. Eur Urol. 2004;46:555–558. doi: 10.1016/j.eururo.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 6.Masters W, Johnson V. Human sexual inadequacy. Boston: Little, Brown; 1970. [Google Scholar]
- 7.Metz M, McCarthy B. Coping with premature ejaculation: How to overcome PE, please your partner & have great sex. Oakland: New Harbinger Publications; 2003. [Google Scholar]
- 8.Waldinger M, Quinn P, Dilleen M, Mundayat R, Schweitzer D, Boolell M. A multinational population survey of intravaginal ejaculation latency time. J Sex Med. 2005;2:292–297. doi: 10.1111/j.1743-6109.2005.00070.x. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. International classification of diseases and related health problems. 10th edition. Geneva: WHO; 1994. [Google Scholar]
- 10.Waldinger M. Premature ejaculation: Different pathophysiologies and etiologies determine its treatment. J Sex Marital Ther. 2008;34:1–13. doi: 10.1080/00926230701640355. [DOI] [PubMed] [Google Scholar]
- 11.Jannini E, Lenzi A. Ejaculatory disorders: Epidemiology and current approaches to definition, classification and subtyping. World J Urol. 2005;23:68–75. doi: 10.1007/s00345-004-0486-9. [DOI] [PubMed] [Google Scholar]
- 12.McMahon CG, Althof SE, Waldinger MD, Porst H, Dean J, Sharlip I, Adaikan PG, Becher E, Broderick GA, Buvat J, Dabees K, Giraldi A, Giuliano F, Hellstrom WJ, Incrocci L, Laan E, Meuleman E, Perelman MA, Rosen RC, Rowland DL, Segraves R. An evidence-based definition of lifelong premature ejaculation: Report of the International Society for Sexual Medicine (ISSM) ad hoc committee for the definition of premature ejaculation. J Sex Med. 2008;5:1590–1606. doi: 10.1111/j.1743-6109.2008.00901.x. [DOI] [PubMed] [Google Scholar]
- 13.American Psychiatric Association. The diagnostic and statistical manual of mental disorders, 5th edition. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 14.Pagani E, Rodrigues O, Torselli M, Genari D. Characterization of 305 men with complaints of premature ejaculation. Int J Impot Res. 1996;8:172. [Google Scholar]
- 15.Waldinger M. Pathophysiology of lifelong premature ejaculation. In: Jannini EA, McMahon CM, Waldinger MD, editors. Premature ejaculation from etiology to diagnosis and treatment. Italia: Springer-Verlag; 2013. pp. 71–80. [Google Scholar]
- 16.Gross S. Practical treatise on impotence and sterility and allied disorders of the male sexual organs. Edinburg: YJ Pentland; 1887. [Google Scholar]
- 17.Carson C, Gunn K. Premature ejaculation: Definition and prevalence. Int J Impot Res. 2006;18:S5–13. doi: 10.1038/sj.ijir.3901507. [DOI] [PubMed] [Google Scholar]
- 18.Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, Vardi Y, Wespes E. Guidelines on male sexual dysfunction: Erectile dysfunction and premature ejaculation. Eur Urol. 2010;57:804–814. doi: 10.1016/j.eururo.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 19.Waldinger M. The neurobiological approach to premature ejaculation. J Urol. 1998;168:2359–2367. doi: 10.1016/S0022-5347(05)64146-8. [DOI] [PubMed] [Google Scholar]
- 20.Laumann EO, Nicolosi A, Glasser DB, Paik A, Gingell C, Moreira E, Wang T. Sexual problems among women and men aged 40–80 y: prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int J Impot Res. 2005;17:39–57. doi: 10.1038/sj.ijir.3901250. [DOI] [PubMed] [Google Scholar]
- 21.Porst H, Montorsi F, Rosen RC, Gaynor L, Grupe S, Alexander J. The premature ejaculation prevalence and attitudes (PEPA) survey: Prevalence, comorbidities and professional help-seeking. Eur Urol. 2007;51:816–824. doi: 10.1016/j.eururo.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Laumann E, Paik A, Rosen R. Sexual dysfunction in the United States: Prevalence and predictors. J Am Med Assoc. 1999;281:537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 23.Waldinger M, Schweitzer D. Changing paradigms from a historical DSM-III and DSM-IV view toward an evidence-based definition of premature ejaculation. Part II- proposals for DSM-V and ICD-11. J Sex Med. 2006;3:693–705. doi: 10.1111/j.1743-6109.2006.00276.x. [DOI] [PubMed] [Google Scholar]
- 24.Dunn KM, Croft PR, Hackett GI. Sexual problems: A study of the prevalence and need for health care in the general population. Fam Pract. 1998;15:519–524. doi: 10.1093/fampra/15.6.519. [DOI] [PubMed] [Google Scholar]
- 25.Fugl-Meyer K, Fugl-Meyer AR. Sexual disabilities are not singularities. Int J Impot Res. 2002;14:487–493. doi: 10.1038/sj.ijir.3900914. [DOI] [PubMed] [Google Scholar]
- 26.Rowland D, Perelman M, Althof S, Barada J, McCullough A, Bull S, Jamieson C, Ho KF. Self-reported premature ejaculation and aspects of sexual functioning and satisfaction. J Sex Med. 2004;1:225–232. doi: 10.1111/j.1743-6109.2004.04033.x. [DOI] [PubMed] [Google Scholar]
- 27.Nolazco C, Bellora O, Lopez M, Surur D, Vazquez J, Rosenfeld C, Becher E, Mazza O. Prevalence of sexual dysfunctions in Argentina. Int J Impot Res. 2004;16:69–72. doi: 10.1038/sj.ijir.3901140. [DOI] [PubMed] [Google Scholar]
- 28.Basile Fasolo C, Mirone V, Gentile V, Parazzini F, Ricci E. Premature ejaculation: Prevalence and associated conditions in a sample of 12,558 men attending the andrology prevention week 2001—A study of the Italian Society of Andrology (SIA) J Sex Med. 2005;2:376–382. doi: 10.1111/j.1743-6109.2005.20350.x. [DOI] [PubMed] [Google Scholar]
- 29.Stulhofer A, Bajic Z. Prevalence of erectile and ejaculatory difficulties among men in Croatia. Croat Med J. 2006;47:114–124. [PMC free article] [PubMed] [Google Scholar]
- 30.Shindel AW, Nelson CJ, Naughton CK, Mulhall JP. Premature ejaculation in infertile couples: Prevalence and correlates. J Sex Med. 2008;5:485–491. doi: 10.1111/j.1743-6109.2007.00690.x. [DOI] [PubMed] [Google Scholar]
- 31.Brock GB, Benard F, Casey R, Elliott SL, Gajewski JB, Lee JC. Canadian male sexual health council survey to assess prevalence and treatment of premature ejaculation in Canada. J Sex Med. 2009;6:2115–2123. doi: 10.1111/j.1743-6109.2009.01362.x. [DOI] [PubMed] [Google Scholar]
- 32.Traeen B, Stigum H. Sexual problems in 18–67-year-old Norwegians. Scand J Public Health. 2010;38:445–456. doi: 10.1177/1403494810371245. [DOI] [PubMed] [Google Scholar]
- 33.Son H, Song SH, Kim SW, Paick JS. Self-reported premature ejaculation prevalence and characteristics in Korean young males: Community-based data from an internet survey. J Androl. 2010;31:540–546. doi: 10.2164/jandrol.110.010355. [DOI] [PubMed] [Google Scholar]
- 34.Amidu N, Owiredu WK, Woode E, Addai-Mensah O, Gyasi-Sarpong KC, Alhassan A. Prevalence of male sexual dysfunction among Ghanaian populace: Myth or reality? Int J Impot Res. 2010;22:337–342. doi: 10.1038/ijir.2010.24. [DOI] [PubMed] [Google Scholar]
- 35.Liang CZ, Hao ZY, Li HJ, Wang ZP, Xing JP, Hu WL, Zhang TF, Ge WW, Zhang XS, Zhou J, Li Y, Zhou ZX, Tang ZG, Tai S. Prevalence of premature ejaculation and its correlation with chronic prostatitis in Chinese men. Urology. 2010;76:962–966. doi: 10.1016/j.urology.2010.01.061. [DOI] [PubMed] [Google Scholar]
- 36.Park HJ, Park JK, Park K, Lee SW, Kim SW, Yang DY, Moon du G, Min KS, Moon KH, Yang SK, Hyun JS, Park NC. Prevalence of premature ejaculation in young and middle-aged men in Korea: A multicenter internet-based survey from the Korean Andrological Society. Asian J Androl. 2010;12:880–889. doi: 10.1038/aja.2010.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vakalopoulos I, Dimitriadis G, Varnava C, Herodotou Y, Gkotsos G, Radopoulos D. Prevalence of ejaculatory disorders in urban men: Results of a random-sample survey. Andrologia. 2011;43:327–333. doi: 10.1111/j.1439-0272.2010.01079.x. [DOI] [PubMed] [Google Scholar]
- 38.Hirshfield S, Chiasson MA, Wagmiller RL, Jr, Remien RH, Humberstone M, Scheinmann R, Grov C. Sexual dysfunction in an Internet sample of U.S. men who have sex with men. J Sex Med. 2010;7:3104–3114. doi: 10.1111/j.1743-6109.2009.01636.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Christensen BS, Gronbaek M, Osler M, Pedersen BV, Graugaard C, Frisch M. Sexual dysfunctions and difficulties in Denmark: Prevalence and associated sociodemographic factors. Arch Sex Behav. 2011;40:121–132. doi: 10.1007/s10508-010-9599-y. [DOI] [PubMed] [Google Scholar]
- 40.Serefoglu EC, Yaman O, Cayan S, Asci R, Orhan I, Usta MF, Ekmekcioglu O, Kendirci M, Semerci B, Kadioglu A. Prevalence of the complaint of ejaculating prematurely and the four premature ejaculation syndromes: Results from the Turkish Society of Andrology Sexual Health Survey. J Sex Med. 2011;8:540–548. doi: 10.1111/j.1743-6109.2010.02095.x. [DOI] [PubMed] [Google Scholar]
- 41.Tang WS, Khoo EM. Prevalence and correlates of premature ejaculation in a primary care setting: A preliminary cross-sectional study. J Sex Med. 2011;8:2071–2078. doi: 10.1111/j.1743-6109.2011.02280.x. [DOI] [PubMed] [Google Scholar]
- 42.Mialon A, Berchtold A, Michaud PA, Gmel G, Suris JC. Sexual dysfunctions among young men: Prevalence and associated factors. J Adolesc Health. 2012;51:25–31. doi: 10.1016/j.jadohealth.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 43.Shaeer O, Shaeer K. The Global Online Sexuality Survey (GOSS): Ejaculatory function, penile anatomy, and contraceptive usage among Arabic-speaking Internet users in the Middle East. J Sex Med. 2012;9:425–433. doi: 10.1111/j.1743-6109.2011.02338.x. [DOI] [PubMed] [Google Scholar]
- 44.Shindel AW, Vittinghoff E, Breyer BN. Erectile dysfunction and premature ejaculation in men who have sex with men. J Sex Med. 2012;9:576–584. doi: 10.1111/j.1743-6109.2011.02585.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McMahon CG, Lee G, Park JK, Adaikan PG. Premature ejaculation and erectile dysfunction prevalence and attitudes in the Asia-Pacific region. J Sex Med. 2012;9:454–465. doi: 10.1111/j.1743-6109.2011.02507.x. [DOI] [PubMed] [Google Scholar]
- 46.Lotti F, Corona G, Rastrelli G, Forti G, Jannini EA, Maggi M. Clinical correlates of erectile dysfunction and premature ejaculation in men with couple infertility. J Sex Med. 2012;9:2698–2707. doi: 10.1111/j.1743-6109.2012.02872.x. [DOI] [PubMed] [Google Scholar]
- 47.Zhang H, Yip AW, Fan S, Yip PS. Sexual dysfunction among Chinese married men aged 30–60 years: A population-based study in Hong Kong. Urology. 2013;81:334–339. doi: 10.1016/j.urology.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 48.Lee SW, Lee JH, Sung HH, Park HJ, Park JK, Choi SK, Kam SC. The prevalence of premature ejaculation and its clinical characteristics in Korean men according to different definitions. Int J Impot Res. 2013;25:12–17. doi: 10.1038/ijir.2012.27. [DOI] [PubMed] [Google Scholar]
- 49.Shaeer O. The Global Online Sexuality Survey (GOSS): The United States of America in 2011 chapter III-premature ejaculation among English-speaking male internet users. J Sex Med. 2013;10:1882–1888. doi: 10.1111/jsm.12187. [DOI] [PubMed] [Google Scholar]
- 50.Gao J, Zhang X, Su P, Liu J, Xia L, Yang J, Shi K, Tang D, Hao Z, Zhou J, Liang C. Prevalence and factors associated with the complaint of premature ejaculation and the four premature ejaculation syndromes: A large observational study in china. J Sex Med. 2013;10:1874–1881. doi: 10.1111/jsm.12180. [DOI] [PubMed] [Google Scholar]
- 51.Hwang I, Yang DO, Park K. Self-reported prevalence of and attitudes toward premature ejaculation in a community-based study of married couples. World J Mens Health. 2013;31:70–75. doi: 10.5534/wjmh.2013.31.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vansintejan J, Janssen J, Van De Vijver E, Vandevoorde J, Devroey D. The gay men sex studies: prevalence of sexual dysfunctions in Belgian HIV(+) gay men. HIV AIDS (Auckl) 2013;5:89–96. doi: 10.2147/HIV.S43962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang X, Gao J, Liu J, Yip PS. Distribution and factors associated with four premature ejaculation syndromes in outpatients complaining of ejaculating prematurely. J Sex Med. 2013;10:1603–1611. doi: 10.1111/jsm.12123. [DOI] [PubMed] [Google Scholar]
- 54.Simons JS, Carey MP. Prevalence of sexual dysfunctions: results from a decade of research. Arch Sex Behav. 2001;30:177–219. doi: 10.1023/a:1002729318254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Waldinger M. History of premature ejaculation. In: Jannini EA, McMahon C, Waldinger M, editors. Premature ejaculation: From etiology to diagnosis and treatment. Italia: Springer-Verlag; 2013. pp. 5–24. [Google Scholar]
- 56.Waldinger M, McIntosh J, Schweitzer DH. A five-nation survey to assess the distribution of the intravaginal ejaculatory latency time among the general male population. J Sex Med. 2009;6:2888–2895. doi: 10.1111/j.1743-6109.2009.01392.x. [DOI] [PubMed] [Google Scholar]
- 57.Waldinger MD. Recent advances in the classification, neurobiology and treatment of premature ejaculation. Adv Psychosom Med. 2008;29:50–69. doi: 10.1159/000126624. [DOI] [PubMed] [Google Scholar]
- 58.Serefoglu EC, Cimen HI, Atmaca AF, Balbay MD. The distribution of patients who seek treatment for the complaint of ejaculating prematurely according to the four premature ejaculation syndromes. J Sex Med. 2010;7:810–815. doi: 10.1111/j.1743-6109.2009.01570.x. [DOI] [PubMed] [Google Scholar]
- 59.Serefoglu EC, Yaman O, Cayan S, Asci R, Orhan I, Usta MF, Ekmekcioglu O, Kendirci M, Semerci B, Kadioglu A. The comparison of premature ejaculation assessment questionnaires and their sensitivity for the four premature ejaculation syndromes: results from the Turkish society of andrology sexual health survey. J Sex Med. 2011;8:1177–1185. doi: 10.1111/j.1743-6109.2010.02183.x. [DOI] [PubMed] [Google Scholar]
- 60.Schapiro B. Premature ejaculation, a review of 1130 cases. J Urol. 1943;50:374–379. [Google Scholar]
- 61.Xin ZC, Choi YD, Rha KH, Choi HK. Somatosensory evoked potentials in patients with primary premature ejaculation. J Urol. 1997;158:451–455. [PubMed] [Google Scholar]
- 62.Fanciullacci F, Colpi G, Beretta G. Cortical evoked potentials in subjects with true premature ejaculation. Andrologia. 1988;20:326–330. [PubMed] [Google Scholar]
- 63.Waldinger M, Berendsen HH, Blok BF, Olivier B, Holstege G. Premature ejaculation and serotonergic antidepressants-induced delayed ejaculation: The involvement of the serotonergic system. Behav Brain Res. 1998;92:111–118. doi: 10.1016/s0166-4328(97)00183-6. [DOI] [PubMed] [Google Scholar]
- 64.Giuliano F. 5-Hydroxytryptamine in premature ejaculation: Opportunities for therapeutic intervention. Trends Neurosci. 2007;30:79–84. doi: 10.1016/j.tins.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 65.Chia S. Management of premature ejaculation—A comparison of treatment outcome in patients with and without erectile dysfunction. Int J Androl. 2002;25:301–305. doi: 10.1046/j.1365-2605.2002.00368.x. [DOI] [PubMed] [Google Scholar]
- 66.Jannini EA, Lombardo F, Lenzi A. Correlation between ejaculatory and erectile dysfunction. Int J Androl. 2005;28(suppl 2):40–45. doi: 10.1111/j.1365-2605.2005.00593.x. [DOI] [PubMed] [Google Scholar]
- 67.Screponi E, Carosa E, Di Stasi SM, Pepe M, Carruba G, Jannini EA. Prevalence of chronic prostatitis in men with premature ejaculation. Urology. 2001;58:198–202. doi: 10.1016/s0090-4295(01)01151-7. [DOI] [PubMed] [Google Scholar]
- 68.Adson DE, Kotlyar M. Premature ejaculation associated with citalopram withdrawal. Ann Pharmacother. 2003;37:1804–1806. doi: 10.1345/aph.1D214. [DOI] [PubMed] [Google Scholar]
- 69.O'Flynn R, Michael A. Reboxetine-induced spontaneous ejaculation. Br J Psychiatry. 2000;177:567–568. doi: 10.1192/bjp.177.6.567-b. [DOI] [PubMed] [Google Scholar]
- 70.Peugh J, Belenko S. Alcohol, drugs and sexual function: A review. J Psychoactive Drugs. 2001;33:223–232. doi: 10.1080/02791072.2001.10400569. [DOI] [PubMed] [Google Scholar]
- 71.Gonen M, Kalkan M, Cenker A, Ozkardes H. Prevalence of premature ejaculation in Turkish men with chronic pelvic pain syndrome. J Androl. 2005;26:601–603. doi: 10.2164/jandrol.04159. [DOI] [PubMed] [Google Scholar]
- 72.Carani C, Isidori AM, Granata A, Carosa E, Maggi M, Lenzi A, Jannini EA. Multicenter study on the prevalence of sexual symptoms in male hypo- and hyperthyroid patients. JCEM. 2005;90:6472–6479. doi: 10.1210/jc.2005-1135. [DOI] [PubMed] [Google Scholar]
- 73.Corona G, Petrone L, Mannucci E, Jannini E, Mansani R, Magini A, Giommi R, Forti G, Maggi M. Psycho-biological correlates of rapid ejaculation in patients attending an andrologic unit for sexual dysfunctions. Eur Urol. 2004;46:615–622. doi: 10.1016/j.eururo.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 74.Waldinger M, Schweitzer DH. The use of old and recent DSM definitions of premature ejaculation in observational studies: A contribution to the present debate for a new classification of PE in the DSM-V. J Sex Med. 2008;5:1079–1087. doi: 10.1111/j.1743-6109.2008.00789.x. [DOI] [PubMed] [Google Scholar]
- 75.Clement P, Bernabe J, Compagnie S, Alexandre L, McCallum S, Giuliano F. Inhibition of ejaculation by the non-peptide oxytocin receptor antagonist GSK557296: A multi-level site of action. Br J Pharmacol. 2013;169:1477–1485. doi: 10.1111/bph.12198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Clement P, Pozzato C, Heidbreder C, Alexandre L, Giuliano F, Melotto S. Delay of ejaculation induced by SB-277011, a selective dopamine D3 receptor antagonist, in the rat. J Sex Med. 2009;6:980–988. doi: 10.1111/j.1743-6109.2008.01173.x. [DOI] [PubMed] [Google Scholar]
- 77.Borgdorff AJ, Bernabe J, Denys P, Alexandre L, Giuliano F. Ejaculation elicited by microstimulation of lumbar spinothalamic neurons. Eur Urol. 2008;54:449–456. doi: 10.1016/j.eururo.2008.03.043. [DOI] [PubMed] [Google Scholar]
- 78.Borgdorff AJ, Rossler AS, Clement P, Bernabe J, Alexandre L, Giuliano F. Differences in the spinal command of ejaculation in rapid ejaculating rats. J Sex Med. 2009;6:2197–2205. doi: 10.1111/j.1743-6109.2009.01308.x. [DOI] [PubMed] [Google Scholar]
- 79.Truitt W, Coolen L. Identification of a potential ejaculation generator in the spinal cord. Science. 2002;297:1566–1569. doi: 10.1126/science.1073885. [DOI] [PubMed] [Google Scholar]
- 80.Coolen L, Allard J, Truitt W, McKenna K. Central regulation of ejaculation. Physiol Behav. 2004;83:203–215. doi: 10.1016/j.physbeh.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 81.Staudt MD, Truitt WA, McKenna KE, de Oliveira CV, Lehman MN, Coolen LM. A pivotal role of lumbar spinothalamic cells in the regulation of ejaculation via intraspinal connections. J Sex Med. 2012;9:2256–2265. doi: 10.1111/j.1743-6109.2011.02574.x. [DOI] [PubMed] [Google Scholar]
- 82.Chehensse C, Bahrami S, Denys P, Clement P, Bernabe J, Guiliano F. The spinal control of ejaculation revisited. A systematic review and meta-analysis of anejaculation in spinal cord injured patients. Hum Reprod Update. 2013;19:507–526. doi: 10.1093/humupd/dmt029. [DOI] [PubMed] [Google Scholar]
- 83.Waldinger M, Rietschel M, Nothen N, Hengeveld MW, Olivier B. Familial occurrence of primary premature ejaculation. Psychiatr Genet. 1998;8:37–40. doi: 10.1097/00041444-199800810-00007. [DOI] [PubMed] [Google Scholar]
- 84.Jern P, Santtila P, Alanko K, Harlaar N, Johansson A, von der Pahlen B, Araojen M, Vilstrom N, Algars M, Sandnabba K. Premature and delayed ejaculation: Genetic and environmental effects in a population-based sample of Finnish twins. J Sex Med. 2007;4:1739–1749. doi: 10.1111/j.1743-6109.2007.00599.x. [DOI] [PubMed] [Google Scholar]
- 85.Janssen P, Bakker S, Rethelyi J, Zwinderman AH, Touw DJ. Olivier B, Waldinger MD. Serotonin transporter promoter region (5-HTTLPR) polymorphism is associated with the intravaginal ejaculation latency time in Dutch men with lifelong premature ejaculation. J Sex Med. 2009;6:276–284. doi: 10.1111/j.1743-6109.2008.01033.x. [DOI] [PubMed] [Google Scholar]
- 86.Zuccarello D, Ghezzi M, Pengo M, Forzan M, Frigo AC, Ferlin A, Foresta C. No difference in 5-HTTLPR and Stin2 polymorphisms frequency between premature ejaculation patients and controls. J Sex Med. 2012;9:1659–1668. doi: 10.1111/j.1743-6109.2012.02715.x. [DOI] [PubMed] [Google Scholar]
- 87.Jern P, Eriksson E, Westberg L. A reassessment of the possible effects of the serotonin transporter gene linked polymorphism 5-HTTLPR on premature ejaculation. Arch Sex Behav. 2013;42:45–49. doi: 10.1007/s10508-012-9991-x. [DOI] [PubMed] [Google Scholar]
- 88.Ozbek E, Tasci A, Tugcu V, Ilbey YO, Simsek A, Ozcan L, Polat EC, Koksal V. Possible association of the 5-HTTLPR serotonin transporter promoter gene polymorphism with PE in a Turkish population. Asian J Androl. 2009;11:1–5. doi: 10.1038/aja.2008.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Santtila P, Jern P, Westberg L, Walum H, Pedersen CT, Eriksson E, Sandnabba N. The dopamine transporter gene (DAT1) polymorphism is associated with premature ejaculation. J Sex Med. 2010;7:1538–1546. doi: 10.1111/j.1743-6109.2009.01696.x. [DOI] [PubMed] [Google Scholar]
- 90.Van Dyck C, Malison R, Jacobson L, Seibyl JP, Staley JK, Laruelle M, Baldwin RM, Innis RB, Gelernter J. Increased dopamine transporter availability associated with the 9-repeat allele of the SLC6A3 gene. J Nucl Med. 2005;46:745–751. [PubMed] [Google Scholar]
- 91.Van Ness S, Owens M, Kilts C. The variable number of tandem repeats element in DAT1 regulates in vitro dopamine transporter density. BMC Genet. 2005;6:55. doi: 10.1186/1471-2156-6-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jern P, Westberg L, Johansson A, Jonsson L, Corander J, Sandnabba NK, Santtila P. Are single nucleotide polymorphisms in the oxytocin and vasopressin 1A/1B receptor genes likely candidates for variation in ejaculatory function? BJU Int. 2012;110:E1173–1180. doi: 10.1111/j.1464-410X.2012.11419.x. [DOI] [PubMed] [Google Scholar]
- 93.Jern P, Westberg L, Johansson A, Gunst A, Eriksson E, Sandnabba K, Santtila P. A study of possible associations between single nucleotide polymorphisms in the serotonin receptor 1A, 1B, and 2C genes and self-reported ejaculation latency time. J Sex Med. 2012;9:866–872. doi: 10.1111/j.1743-6109.2011.02618.x. [DOI] [PubMed] [Google Scholar]
- 94.Luo S, Lu Y, Wang F, Xie Z, Huang X, Dong Q, Zhang S. Association between polymorphisms in the serotonin 2C receptor gene and premature ejaculation in Han Chinese subjects. Urol Int. 2010;85:204–208. doi: 10.1159/000314528. [DOI] [PubMed] [Google Scholar]
- 95.Carosa E, Di Sante S, Rossi S, Castri A, D'Adamo F, Gravina GL, Ronchi P, Kostrouch Z, Dolci S, Lenzi A, Jannini EA. Ontogenetic profile of the expression of thyroid hormone receptors in rat and human corpora cavernosa of the penis. J Sex Med. 2010;7:1381–1390. doi: 10.1111/j.1743-6109.2009.01701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kulikov AV, Maksyutova AV, Ivanova EA, Khvorostov IB, Popova NK. The effect of thyroidectomy on the expression of the mRNA of 5-HT2A serotonin receptors in the rat frontal cortex. Dokl Biochem Biophys. 2002;383:116–118. doi: 10.1023/a:1015387818916. [DOI] [PubMed] [Google Scholar]
- 97.Kulikov AV, Zubkov EA. Chronic thyroxine treatment activates the 5-HT2A serotonin receptor in the mouse brain. Neurosci Lett. 2007;416:307–309. doi: 10.1016/j.neulet.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 98.Cihan A, Demir O, Demir T, Aslan G, Comlekci A, Esen A. The relationship between premature ejaculation and hyperthyroidism. J Urol. 2009;181:1273–1280. doi: 10.1016/j.juro.2008.10.150. [DOI] [PubMed] [Google Scholar]
- 99.Cihan A, Murat N, Demir O, Aslan G, Comlekci A, Esen A. An experimental approach to the interrelationship between hyperthyroidism and ejaculation latency time in male rats. J Urol. 2009;181:907–912. doi: 10.1016/j.juro.2008.10.061. [DOI] [PubMed] [Google Scholar]
- 100.Corona G, Jannini EA, Lotti F, Boddi V, De Vita G, Forti G, Lenzi A, Mannucci E, Maggi M. Premature and delayed ejaculation: Two ends of a single continuum influenced by hormonal milieu. Int J Androl. 2011;34:41–48. doi: 10.1111/j.1365-2605.2010.01059.x. [DOI] [PubMed] [Google Scholar]
- 101.Ozturk MI, Koca O, Tuken M, Keles MO, Ilktac A, Karaman MI. Hormonal evaluation in premature ejaculation. Urol Int. 2012;88:454–458. doi: 10.1159/000336137. [DOI] [PubMed] [Google Scholar]
- 102.Waldinger MD, Zwinderman AH, Olivier B, Schweitzer DH. Thyroid-stimulating hormone assessments in a Dutch cohort of 620 men with lifelong premature ejaculation without erectile dysfunction. J Sex Med. 2005;2:865–870. doi: 10.1111/j.1743-6109.2005.00142.x. [DOI] [PubMed] [Google Scholar]
- 103.Corona G, Jannini EA, Vignozzi L, Rastrelli G, Maggi M. The hormonal control of ejaculation. Nat Rev Urol. 2012;9:508–519. doi: 10.1038/nrurol.2012.147. [DOI] [PubMed] [Google Scholar]
- 104.Corona G, Mannucci E, Jannini E, Lotti F, Ricca V, Monami M, Boddi V, Bandini E, Balercia G, Forti G, Maggi M. Hypoprolactinemia: A new clinical syndrome in patients with sexual dysfunction. J Sex Med. 2009;6:1457–1466. doi: 10.1111/j.1743-6109.2008.01206.x. [DOI] [PubMed] [Google Scholar]
- 105.Corona G, Jannini E, Mannucci E, Fisher AD, Lotti F, Petrone L, Balercia G, Bandini E, Chiarini V, Forti G, Maggi M. Different testosterone levels are associated with ejaculatory dysfunction. J Sex Med. 2008;5:1991–1998. doi: 10.1111/j.1743-6109.2008.00803.x. [DOI] [PubMed] [Google Scholar]
- 106.Liang CZ, Zhang XJ, Hao ZY, Shi HQ, Wang KX. Prevalence of sexual dysfunction in Chinese men with chronic prostatitis. BJU Int. 2004;93:568–570. doi: 10.1111/j.1464-410x.2003.04662.x. [DOI] [PubMed] [Google Scholar]
- 107.Trinchieri A, Magri V, Cariani L, Bonamore R, Restelli A, Garlaschi MC, Perletti G. Prevalence of sexual dysfunction in men with chronic prostatitis/chronic pelvic pain syndrome. Arch Ital Urol Androl. 2007;79:67–70. [PubMed] [Google Scholar]
- 108.Shamloul R, el-Nashaar A. Chronic prostatitis in premature ejaculation: A cohort study in 153 men. J Sex Med. 2006;3:150–154. doi: 10.1111/j.1743-6109.2005.00107.x. [DOI] [PubMed] [Google Scholar]
- 109.Lotti F, Corona G, Mancini M, Biagini C, Colpi G, Innocenti SD, Filmberti E, Gacci M, Krausz C, Sforza A, Forti G, Mannucci E, Maggi M. The association between varicocele, premature ejaculation and prostatitis symptoms: possible mechanisms. J Sex Med. 2009;6:2878–2887. doi: 10.1111/j.1743-6109.2009.01417.x. [DOI] [PubMed] [Google Scholar]
- 110.el-Sakka AI. Efficacy of sildenafil citrate in treatment of erectile dysfunction: impact of associated premature ejaculation and low desire. Urology. 2006;68:642–647. doi: 10.1016/j.urology.2006.03.070. [DOI] [PubMed] [Google Scholar]
- 111.Malavige LS, Jayaratne SD, Kathriarachchi ST, Sivayogan S, Fernando DJ, Levy JC. Erectile dysfunction among men with diabetes is strongly associated with premature ejaculation and reduced libido. J Sex Med. 2008;5:2125–2134. doi: 10.1111/j.1743-6109.2008.00907.x. [DOI] [PubMed] [Google Scholar]
- 112.Shaeer O, Shaeer K. The Global Online Sexuality Survey (GOSS): The United States of America in 2011. Chapter I: Erectile dysfunction among English-speakers. J Sex Med. 2012;9:3018–3027. doi: 10.1111/j.1743-6109.2012.02976.x. [DOI] [PubMed] [Google Scholar]
- 113.Hwa JS, Kam SC, Choi JH, Do JM, Seo DH, Hyun JS. Impact of erectile function and age in men with lower urinary tract symptoms on ejaculatory dysfunction and premature ejaculation. Int J Impot Res. 2012;24:101–105. doi: 10.1038/ijir.2012.1. [DOI] [PubMed] [Google Scholar]
- 114.Porst H, McMahon C, Althof S, Sharlip I, Bull S, Rivas DA. Baseline characteristics and treatment outcomes for men with acquired or lifelong premature ejaculation with mild or no erectile dysfunction: Integrated analysis of two phase III dapoxetine trials. J Sex Med. 2010;7:2231–2242. doi: 10.1111/j.1743-6109.2010.01820.x. [DOI] [PubMed] [Google Scholar]
- 115.McMahon CG. Screening for erectile dysfunction in men with lifelong premature ejaculation—Is the Sexual Health Inventory for Men (SHIM) reliable? J Sex Med. 2009;6:567–573. doi: 10.1111/j.1743-6109.2008.01092.x. [DOI] [PubMed] [Google Scholar]
- 116.Cahangirov A, Cihan A, Murat N, Demir O, Aslan G, Gidener S, Esen AA. Investigation of the neural target level of hyperthyroidism in premature ejaculation in a rat model of pharmacologically induced ejaculation. J Sex Med. 2011;8:90–96. doi: 10.1111/j.1743-6109.2010.02042.x. [DOI] [PubMed] [Google Scholar]
- 117.Cooper AJ, Cernovsky ZZ, Colussi K. Some clinical and psychometric characteristics of primary and secondary premature ejaculators. J Sex Marital Ther. 1993;19:276–288. doi: 10.1080/00926239308404371. [DOI] [PubMed] [Google Scholar]
- 118.Jannini EA, Porst H. A practical approach to premature ejaculation. J Sex Med. 2011;8(suppl 4):301–303. doi: 10.1111/j.1743-6109.2011.02456.x. [DOI] [PubMed] [Google Scholar]
- 119.Ozturk B, Cetinkaya M, Saglam H, Adsan O, Akin O, Memis A. Erectile dysfunction in premature ejaculation. Arch Ital Urol Androl. 1997;69:133–136. [PubMed] [Google Scholar]
- 120.Lau J, Kim J, Tsui H. Prevalence and sociocultural predictors of sexual dysfunction among Chinese men who have sex with men in Hong Kong. J Sex Med. 2008;5:2766–2779. doi: 10.1111/j.1743-6109.2008.00892.x. [DOI] [PubMed] [Google Scholar]
- 121.Bancroft J, Carnes L, Janssen E, Goodrich D, Long JS. Erectile and ejaculatory problems in gay and heterosexual men. Arch Sex Behav. 2005;34:285–297. doi: 10.1007/s10508-005-3117-7. [DOI] [PubMed] [Google Scholar]
- 122.Jern P, Santtila P, Johansson A, Alanko K, Salo B, Sandnabba NK. Is there an association between same-sex sexual experience and ejaculatory dysfunction? J Sex Marital Ther. 2010;36:303–312. doi: 10.1080/0092623X.2010.488102. [DOI] [PubMed] [Google Scholar]
- 123.Althof S, McCabe M, Assalian P, Chevret-Measson M, Leiblum S, Simonelli C, Wylie K. Psychological and interpersonal dimensions of sexual function and dysfunction. In: Montorsi F, Basson R, Adaikan G, Becher E, Clayton A, Giuliano F, Khory S, Sharlip I, editors. Sexual Medicine: Sexual dysfunctions in men and women. Editions 21. Paris: Editions 21; 2010. pp. 121–182. [Google Scholar]
- 124.McCabe M. The development and maintenance of sexual dysfunction: An explanation based on cognitive theory. Sex Marital Ther. 1991;6:254–260. [Google Scholar]
- 125.Michetti P, Rossi R, Bonanno D, DeDominicis C, Lori F, Simonelli C. Dysregulation of emotions and premature ejaculation (PE): Alexithymia in 100 outpatients. J Sex Med. 2007;17:18–23. doi: 10.1111/j.1743-6109.2007.00564.x. [DOI] [PubMed] [Google Scholar]
- 126.Graziottin A, Althof S. What does premature ejaculation mean to the man, the woman, and the couple? J Sex Med. 2011;8(suppl 4):304–309. doi: 10.1111/j.1743-6109.2011.02426.x. [DOI] [PubMed] [Google Scholar]
- 127.Mohr D, Bentler L. Erectile dysfunction: A review of diagnostic and treatment procedures. Clin Psychol Rev. 1990;10:123–150. [Google Scholar]
- 128.Patrick DL, Althof SE, Pryor JL, Rosen R, Rowland DL, Ho KF, McNulty P, Rothman M, Jamieson C. Premature ejaculation: An observational study of men and their partners. J Sex Med. 2005;2:358–367. doi: 10.1111/j.1743-6109.2005.20353.x. [DOI] [PubMed] [Google Scholar]
- 129.Giuliano F, Patrick DL, Porst H, La Pera G, Kokoszka A, Merchant S, Rothman M, Gagnon DD, Polverejan E. Premature ejaculation: Results from a five-country European observational study. Eur Urol. 2008;53:1048–1057. doi: 10.1016/j.eururo.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 130.Rosen R, Althof S. Impact of premature ejaculation: The psychological quality of life and sexual relationship consequences. J Sex Med. 2008;5:1296–1307. doi: 10.1111/j.1743-6109.2008.00825.x. [DOI] [PubMed] [Google Scholar]
- 131.Rowland D, Patrick D, Rothman M, Gagnon D. The psychological burden of premature ejaculation. J Urol. 2007;177:1065–1070. doi: 10.1016/j.juro.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 132.Symonds T, Roblin D, Hart K, Althof S. How does premature ejaculation effect a man's life. J Sex Marital Ther. 2003;29:361–370. doi: 10.1080/00926230390224738. [DOI] [PubMed] [Google Scholar]
- 133.Escajadillo-Vargas N, Mezones-Holguin E, Castro-Castro J, Cordova-Marcelo W, Blumel JE, Perez-Lopez FR, Chedraui P. Sexual dysfunction risk and associated factors in young Peruvian university women. J Sex Med. 2011;8:1701–1709. doi: 10.1111/j.1743-6109.2011.02259.x. [DOI] [PubMed] [Google Scholar]
- 134.Hobbs K, Symonds T, Abraham L, May K, Morris MF. Sexual dysfunction in partners of men with premature ejaculation. Int J Impot Res. 2008;20:512–517. doi: 10.1038/ijir.2008.34. [DOI] [PubMed] [Google Scholar]
- 135.Limoncin E, Tomassetti M, Gravina GL, Ciocca G, Carosa E, Di Sante S, Gentile V, Mirone V, Montorsi F, Lenzi A, Jannini EA. Premature ejaculation results in female sexual distress: Standardization and validation of a new diagnostic tool for sexual distress. J Urol. 2013;189:1830–1835. doi: 10.1016/j.juro.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 136.Oberg K, Sjogren Fugl-Meyer K. On Swedish women's distressing sexual dysfunctions: Some concomitant conditions and life satisfaction. J Sex Med. 2005;2:169–180. doi: 10.1111/j.1743-6109.2005.20226.x. [DOI] [PubMed] [Google Scholar]
- 137.Riley A, Riley E. Premature ejaculation: Presentation and associations. An audit of patients attending a sexual problems clinic. Int J Clin Pract. 2005;59:1482–1487. doi: 10.1111/j.1368-5031.2005.00730.x. [DOI] [PubMed] [Google Scholar]
- 138.Shaeer O, Shaeer K, Shaeer E. The Global Online Sexuality Survey (GOSS): Female sexual dysfunction among Internet users in the reproductive age group in the Middle East. J Sex Med. 2012;9:411–424. doi: 10.1111/j.1743-6109.2011.02552.x. [DOI] [PubMed] [Google Scholar]
- 139.Zhang H, Yip PS. Female sexual dysfunction among young and middle-aged women in Hong Kong: Prevalence and risk factors. J Sex Med. 2012;9:2911–2918. doi: 10.1111/j.1743-6109.2012.02773.x. [DOI] [PubMed] [Google Scholar]
- 140.Dogan S, Dogan M. The frequency of sexual dysfunctions in male partners of women with vaginismus in a Turkish sample. Int J Impot Res. 2008;20:218–221. doi: 10.1038/sj.ijir.3901615. [DOI] [PubMed] [Google Scholar]
- 141.Schein M, Zyzanski SJ, Levine S, Medalie JH, Dickman RL, Alemagno SA. The frequency of sexual problems among family practice patients. Fam Pract Res J. 1988;7:122–134. [PubMed] [Google Scholar]
- 142.Humphrey S, Nazareth I. GP's view on their management of sexual dysfunction. Fam Pract. 2001;18:516–518. doi: 10.1093/fampra/18.5.516. [DOI] [PubMed] [Google Scholar]
- 143.Rowland D, McMahon C, Abdo C, Chen J, Jannini E, Waldinger MD, Ahn TY. Disorders of orgasm and ejaculation in men. J Sex Med. 2010;7:1668–1686. doi: 10.1111/j.1743-6109.2010.01782.x. [DOI] [PubMed] [Google Scholar]
- 144.Jannini E, Maggi M, Lenzi A. Evaluation of premature ejaculation. J Sex Med. 2011;8:328–334. doi: 10.1111/j.1743-6109.2011.02289.x. [DOI] [PubMed] [Google Scholar]
- 145.Serefoglu EC, Cimen HI, Ozdemir AT, Symonds T, Berktas M, Balbay MD. Turkish validation of the premature ejaculation diagnostic tool and its association with intravaginal ejaculatory latency time. Int J Impot Res. 2009;21:139–144. doi: 10.1038/ijir.2008.58. [DOI] [PubMed] [Google Scholar]
- 146.Althof SE. Evidence based assessment of rapid ejaculation. Int J Impot Res. 1998;10(suppl 2):S74–76. discussion S77–9. [PubMed] [Google Scholar]
- 147.Pryor JL, Broderick GA, Ho KF, Jamieson C, Gagnon D. Comparison of estimated versus measured intravaginal ejaculatory latency time in men with and without premature ejaculation. J Sex Med. 2005;3:54. [Google Scholar]
- 148.Rosen R, McMahon C, Niederberger C, Broderick G, Jamieson C, Gagnon DD. Correlates to the clinical diagnosis of premature ejaculation: Results from a large observational study of men and their partners. J Urol. 2007;177:1059–1064. doi: 10.1016/j.juro.2006.10.044. [DOI] [PubMed] [Google Scholar]
- 149.Corona G, Jannini E, Maggi M. Inventories for male and female sexual dysfunctions. Int J Impot Res. 2006;18:236–250. doi: 10.1038/sj.ijir.3901410. [DOI] [PubMed] [Google Scholar]
- 150.Althof S, Rosen R, Symonds T, Mundayat R, May K, Abraham L. Development and validation of a new questionnaire to assess sexual satisfaction, control and distress associated with premature ejaculation. J Sex Med. 2006;3:465–475. doi: 10.1111/j.1743-6109.2006.00239.x. [DOI] [PubMed] [Google Scholar]
- 151.Arafa M, Shamloul R. Development and validation of the Arabic Index of Premature Ejaculation (AIPE) J Sex Med. 2007;4:1750–1756. doi: 10.1111/j.1743-6109.2006.00213.x. [DOI] [PubMed] [Google Scholar]
- 152.Patrick DL, Giuliano F, Ho KF, Gagnon DD, McNulty P, Rothman M. The premature ejaculation profile: Validation of self-reported outcome measures for research and practice. BJU Int. 2008;103:358–367. doi: 10.1111/j.1464-410X.2008.08041.x. [DOI] [PubMed] [Google Scholar]
- 153.Symonds T, Perelman M, Althof S, Giuliano F, Martin M, Abraham L, Crossland A, Morris M, May K. Further evidence of the reliability and validity of the premature ejaculation diagnostic tool. Int J Impot Res. 2007;19:521–525. doi: 10.1038/sj.ijir.3901567. [DOI] [PubMed] [Google Scholar]
- 154.Symonds T, Perelman M, Althof S, Giuliano F, Martin M, May K, Abraham L, Crossland A, Morris M. Development and validation of a premature ejaculation diagnostic tool. Eur Urol. 2007;52:565–573. doi: 10.1016/j.eururo.2007.01.028. [DOI] [PubMed] [Google Scholar]
- 155.Yuan Y, Xin ZC, Jiang J, Guo YJ, Liu WJ, Tian L, Zhu JC. Sexual function of premature ejaculation patients assayed with the Chinese Index of Premature Ejaculation. Asian J Androl. 2004;6:121–126. [PubMed] [Google Scholar]
- 156.Althof S. Psychological approaches to the treatment of rapid ejaculation. J Mens Health Gend. 2006;3:180–186. [Google Scholar]
- 157.Althof S. Treatment of rapid ejaculation: Psychotherapy, pharmacotherapy, and combined therapy. In: Leiblum S, editor. Principles and practice of sex therapy. 4th edition. New York: Guilford Press; 2007. pp. 212–240. [Google Scholar]
- 158.Jannini E, Simonelli C, Lenzi A. Sexological approach to ejaculatory dysfunction. Int J Androl. 2002;25:317–323. doi: 10.1046/j.1365-2605.2002.00371.x. [DOI] [PubMed] [Google Scholar]
- 159.Kaplan HS. The new sex therapy. New York: Bruner Mazel; 1974. [Google Scholar]
- 160.Levine SB. Sexual life: A clinician's guide. New York: Plenum; 1992. [Google Scholar]
- 161.McCarthy B. Cognitive behavioral strategies and techniques in the treatment of early ejaculation. In: Leiblum S, Rosen R, editors. Principles and practice of sex therapy: Update for the 1990s. New York: Guilford Press; 1990. pp. 141–167. [Google Scholar]
- 162.Semans J. Premature ejaculation. South Med J. 1956;49:352–358. doi: 10.1097/00007611-195604000-00008. [DOI] [PubMed] [Google Scholar]
- 163.Hawton K. Treatment of sexual dysfunctions by sex therapy and other approaches. Br J Psychiatry. 1995;167:307–314. doi: 10.1192/bjp.167.3.307. [DOI] [PubMed] [Google Scholar]
- 164.De Carufel F, Trudel G. Effects of a new functional sexological treatment for premature ejaculation. J Sex Marital Ther. 2006;32:97–114. doi: 10.1080/00926230500442292. [DOI] [PubMed] [Google Scholar]
- 165.Trudel G, Proulx S. Treatment of premature ejaculation by bibliotherapy: An experimental study. Sex Marital Ther. 1987;2:163–167. [Google Scholar]
- 166.Fruhauf S, Gerger H, Schmidt HM, Munder T, Barth J. Efficacy of psychological interventions for sexual dysfunction: A systematic review and meta-analysis. Arch Sex Behav. 2013;42:915–933. doi: 10.1007/s10508-012-0062-0. [DOI] [PubMed] [Google Scholar]
- 167.Melnik T, Althof S, Atallah Á, Puga MS, Glina S, Riera R. Psychosocial interventions for premature ejaculation. Cochrane Database Syst Rev. 2010;1 doi: 10.1002/14651858.CD008195.pub2. CD008195. [DOI] [PubMed] [Google Scholar]
- 168.Berner M, Gunzler C. Efficacy of psychosocial interventions in men and women with sexual dysfunctions—A systematic review of controlled clinical trials: Part 1-the efficacy of psychosocial interventions for male sexual dysfunction. J Sex Med. 2012;9:3089–3107. doi: 10.1111/j.1743-6109.2012.02970.x. [DOI] [PubMed] [Google Scholar]
- 169.McCabe M, Price E, Piterman L, Lording D. Evaluation of a internet based psychological intervention for the treatment of erectile dysfunction. Int J Impot Res. 2008;20:324–330. doi: 10.1038/ijir.2008.3. [DOI] [PubMed] [Google Scholar]
- 170.Jones L, McCabe M. The effectiveness of an internet-based psychological treatment program for female sexual dysfunction. J Sex Med. 2011;8:2781–2792. doi: 10.1111/j.1743-6109.2011.02381.x. [DOI] [PubMed] [Google Scholar]
- 171.Giuliano F, Clement P. Pharmacology for the treatment of premature ejaculation. Pharmacol Rev. 2012;64:621–644. doi: 10.1124/pr.111.004952. [DOI] [PubMed] [Google Scholar]
- 172.Dinsmore W, Wylie M. PSD502 improves ejaculatory latency, control and sexual satisfaction when applied topically 5 minutes before intercourse in men with premature ejaculation: Results of a phase III, multicentre, double-blind, placebo-controlled study. BJU Int. 2009;103:940–949. doi: 10.1111/j.1464-410X.2009.08456.x. [DOI] [PubMed] [Google Scholar]
- 1001.Carson C, Wylie M. Improved ejaculatory latency, control and sexual satisfaction when PSD502 is applied topically in men with premature ejaculation: Results of a phase III, double-blind, placebo-controlled study. J Sex Med. 2010;7:3179–3189. doi: 10.1111/j.1743-6109.2010.01913.x. [DOI] [PubMed] [Google Scholar]
- 174.McMahon C. Clinical trial methodology in premature ejaculation observational, interventional and treatment preference studies- Part 1- Defining and selecting the study population. J Sex Med. 2008;6:1805–1816. doi: 10.1111/j.1743-6109.2008.00836.x. [DOI] [PubMed] [Google Scholar]
- 175.Kaynar M, Kilic O, Yurdakul T. On-demand tramadol hydrochloride use in premature ejaculation treatment. Urology. 2012;79:145–149. doi: 10.1016/j.urology.2011.09.031. [DOI] [PubMed] [Google Scholar]
- 176.Aversa A, Pili M, Francomano D, Bruzziches R, Spera E, La Pera G, Spera G. Effects of vardenafil administration on intravaginal ejaculatory latency time in men with lifelong premature ejaculation. Int J Impot Res. 2009;21:221–227. doi: 10.1038/ijir.2009.21. [DOI] [PubMed] [Google Scholar]
- 177.Cavallini G. Alpha-1 blockade pharmacotherapy in primitive psychogenic premature ejaculation resistant to psychotherapy. Eur Urol. 1995;28:126–130. doi: 10.1159/000475036. [DOI] [PubMed] [Google Scholar]
- 178.Althof S, Levine S, Corty E, Risen C, Stern E, Kurit D. Clomipramine as a treatment for rapid ejaculation: A double-blind crossover trial of fifteen couples. J Clin Psychiatry. 1995;56:402–407. [PubMed] [Google Scholar]
- 179.Atmaca M, Kuloglu M, Tezcan E, Semercioz A. The efficacy of citalopram in the treatment of premature ejaculation: A placebo-controlled study. Int J Impot Res. 2002;14:502–505. doi: 10.1038/sj.ijir.3900918. [DOI] [PubMed] [Google Scholar]
- 180.Goodman RE. An assessment of clomipramine (Anafranil) in the treatment of premature ejaculation. J Int Med Res. 1980;8:53–59. [PubMed] [Google Scholar]
- 181.Hellstrom WJ, Althof S, Gittelman M, Streidle C, Ho KF, Kell S, Nilson-Beijber A. Dapoxetine for the treatment of men with premature ejaculation (PE): Dose-finding analysis. J Urol. 2005;173:238. abstract 877. [Google Scholar]
- 182.McMahon C, Kim S, Park N, Chang C, Rivas D, Tesfaye F, Rothman M, Aquilina J. Treatment of premature ejaculation in the Asia-Pacific region: Results from a phase III double-blind, parallel-group study of dapoxetine. J Sex Med. 2009;7:256–268. doi: 10.1111/j.1743-6109.2009.01560.x. [DOI] [PubMed] [Google Scholar]
- 183.McMahon CG. Treatment of premature ejaculation with sertraline hydrochloride: A single-blind placebo controlled crossover study. J Urol. 1998;159:1935–1938. doi: 10.1016/S0022-5347(01)63201-4. [DOI] [PubMed] [Google Scholar]
- 184.McMahon CG, Althof SE, Kaufman JM, Buvat J, Levine SB, Aquilina JW, Tesfaye F, Rothman M, Rivas DA, Porst H. Efficacy and safety of dapoxetine for the treatment of premature ejaculation: Integrated analysis of results from five phase 3 trials. J Sex Med. 2011;8:524–539. doi: 10.1111/j.1743-6109.2010.02097.x. [DOI] [PubMed] [Google Scholar]
- 185.McMahon CG, Touma K. Treatment of premature ejaculation with paroxetine hydrochloride as needed: 2 single-blind placebo controlled crossover studies. J Urol. 1999;161:1826–1830. [PubMed] [Google Scholar]
- 186.Waldinger MD, Hengeveld MW, Zwinderman AH. Paroxetine treatment of premature ejaculation: A double-blind, randomized, placebo-controlled study. Am J Psychiatry. 1994;151:1377–1379. doi: 10.1176/ajp.151.9.1377. [DOI] [PubMed] [Google Scholar]
- 187.Waldinger MD, Zwinderman AH, Olivier B. On-demand treatment of premature ejaculation with clomipramine and paroxetine: A randomized, double-blind fixed-dose study with stopwatch assessment. Eur Urol. 2004;46:510–515. doi: 10.1016/j.eururo.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 188.Buvat J, Tesfaye F, Rothman M, Rivas DA, Giuliano F. Dapoxetine for the treatment of premature ejaculation: Results from a randomized, double-blind, placebo-controlled phase 3 trial in 22 countries. Eur Urol. 2009;55:957–967. doi: 10.1016/j.eururo.2009.01.025. [DOI] [PubMed] [Google Scholar]
- 189.Pryor JL, Althof SE, Steidle C, Rosen RC, Hellstrom WJ, Shabsigh R, Miloslavsky M, Kell S. Efficacy and tolerability of dapoxetine in treatment of premature ejaculation: An integrated analysis of two double-blind, randomised controlled trials. Lancet. 2006;368:929–937. doi: 10.1016/S0140-6736(06)69373-2. [DOI] [PubMed] [Google Scholar]
- 190.Dresser MJ, Desai D, Gidwani S, Seftel AD, Modi NB. Dapoxetine, a novel treatment for premature ejaculation, does not have pharmacokinetic interactions with phosphodiesterase-5 inhibitors. Int J Impot Res. 2006;18:104–110. doi: 10.1038/sj.ijir.3901420. [DOI] [PubMed] [Google Scholar]
- 191.Jannini EA. Editorial comment on: Dapoxetine for the treatment of premature ejaculation: Results from a randomized, double-blind, placebo-controlled phase 3 trial in 22 countries. Eur Urol. 2009;55:967–968. doi: 10.1016/j.eururo.2009.01.026. [DOI] [PubMed] [Google Scholar]
- 192.McMahon CG, Giuliano F, Dean J, Hellstrom WJ, Bull S, Tesfaye F, Sharma O, Rivas D, Aquilina J. Efficacy and safety of dapoxetine in men with premature ejaculation and concomitant erectile dysfunction treated with a phosphodiesterase type 5 inhibitor: Randomized, placebo-controlled, phase III study. J Sex Med. 2013;10:2312–2325. doi: 10.1111/jsm.12236. [DOI] [PubMed] [Google Scholar]
- 193.Levine L. Evaluation of Withdrawal Effects with Dapoxetine in the Treatment of Premature Ejaculation (PE). Poster presented at SMSNA 2006.
- 194.Kara H, Aydin S, Yucel M, Agargun MY, Odabas O, Yilmaz Y. The efficacy of fluoxetine in the treatment of premature ejaculation: A double-blind placebo controlled study. J Urol. 1996;156:1631–1632. [PubMed] [Google Scholar]
- 195.Waldinger M, Zwinderman A, Schweitzer D, Oliver B. Relevance of methodological design for the interpretation of efficacy of drug treatment of premature ejaculation: A systematic review and metaanalysis. Int J Impot Res. 2004;16:1–13. doi: 10.1038/sj.ijir.3901172. [DOI] [PubMed] [Google Scholar]
- 196.McMahon CG. Long term results of treatment of premature ejaculation with selective serotonin re-uptake inhibitors. Int J Impot Res. 2002;14:S19. [Google Scholar]
- 197.Waldinger MD. Premature ejaculation: Definition and drug treatment. Drugs. 2007;67:547–568. doi: 10.2165/00003495-200767040-00005. [DOI] [PubMed] [Google Scholar]
- 198.Tanrikut C, Feldman AS, Altemus M, Paduch DA, Schlegel PN. Adverse effect of paroxetine on sperm. Fertil Steril. 2010;94:1021–1026. doi: 10.1016/j.fertnstert.2009.04.039. [DOI] [PubMed] [Google Scholar]
- 199.Marangell L, Dennehy E, Wisniewski S, Bauer MS, Miyahara S, Allen MH, Martinez M, Al Jurdi RK, Thase ME. Case-control analyses of the impact of pharmacotherapy on prospectively observed suicide attempts and completed suicides in bipolar disorder: findings from STEP-BD. J Clin Psychiatry. 2008;69:916–922. doi: 10.4088/jcp.v69n0605. [DOI] [PubMed] [Google Scholar]
- 200.Khan A, Khan S, Kolts R, Brown WA. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: Analysis of FDA reports. Am J Psychiatry. 2003;160:790–792. doi: 10.1176/appi.ajp.160.4.790. [DOI] [PubMed] [Google Scholar]
- 201.Mann J, Emslie G, Baldessarini R, Beardslee W, Fawcett J, Goodwin FK, Leon AC, Meltzer HY, Ryan ND, Shaffer D, Wagner KD. ACNP Task Force report on SSRIs and suicidal behavior in youth. Neuropsychopharmacology. 2006;31:473–492. doi: 10.1038/sj.npp.1300958. [DOI] [PubMed] [Google Scholar]
- 202.Stone M, Laughren T, Jones ML, Levenson M, Holland PC, Hughes A, Hammad TA, Temple R, Rochester G. Risk of suicidality in clinical trials of antidepressants in adults: Analysis of proprietary data submitted to US Food and Drug Administration. Br Med J. 2009;339:2880–2890. doi: 10.1136/bmj.b2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Black K, Shea CA, Dursun S, Kutcher S. Selective serotonin reuptake inhibitor discontinuation syndrome: Proposed diagnostic criteria. J Psychiatry Neurosci. 2000;25:255–261. [PMC free article] [PubMed] [Google Scholar]
- 204.Kim SW, Paick JS. Short-term analysis of the effects of as needed use of sertraline at 5 PM for the treatment of premature ejaculation. Urology. 1999;54:544–547. doi: 10.1016/s0090-4295(99)00187-9. [DOI] [PubMed] [Google Scholar]
- 205.Strassberg DS, de Gouveia Brazao CA, Rowland DL, Tan P, Slob AK. Clomipramine in the treatment of rapid (premature) ejaculation. J Sex Marital Ther. 1999;25:89–101. doi: 10.1080/00926239908403982. [DOI] [PubMed] [Google Scholar]
- 206.Salonia A, Rocchini L, Sacca A, Pellucchi F, Ferrari M, Del Carro U, Ribotto P, Gallina A, Zanni G, Deho F, Regatti P, Montorsi F. Acceptance of and discontinuation rate from paroxetine treatment in patients with lifelong premature ejaculation. J Sex Med. 2009;6:2868–2877. doi: 10.1111/j.1743-6109.2009.01404.x. [DOI] [PubMed] [Google Scholar]
- 207.Mondaini N, Fusco F, Cai T, Benemei S, Mirone V, Bartoletti R. Dapoxetine treatment in patients with lifelong premature ejaculation: The reasons of a “waterloo”. Urology. 2013;82:620–624. doi: 10.1016/j.urology.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 208.Waldinger MD, Zwinderman AH, Olivier B, Schweitzer DH. The majority of men with lifelong premature ejaculation prefer daily drug treatment: An observation study in a consecutive group of Dutch men. J Sex Med. 2007;4:1028–1037. doi: 10.1111/j.1743-6109.2007.00528.x. [DOI] [PubMed] [Google Scholar]
- 209.Berkovitch M, Keresteci AG, Koren G. Efficacy of prilocaine-lidocaine cream in the treatment of premature ejaculation. J Urol. 1995;154:1360–1361. [PubMed] [Google Scholar]
- 210.Busato W, Galindo CC. Topical anaesthetic use for treating premature ejaculation: A double-blind, randomized, placebo-controlled study. BJU Int. 2004;93:1018–1021. doi: 10.1111/j.1464-410X.2003.04773.x. [DOI] [PubMed] [Google Scholar]
- 211.Pu C, Yang L, Liu L, Yuan H, Wei Q, Han P. Topical anesthetic agents for premature ejaculation: A systematic review and meta-analysis. Urology. 2013;81:799–804. doi: 10.1016/j.urology.2012.12.028. [DOI] [PubMed] [Google Scholar]
- 212.Wieder JA, Brackett NL, Lynne CM, Green JT, Aballa TC. Anesthetic block of the dorsal penile nerve inhibits vibratory-induced ejaculation in men with spinal cord injuries. Urology. 2000;55:915–917. doi: 10.1016/s0090-4295(99)00608-1. [DOI] [PubMed] [Google Scholar]
- 213.Jannini EA, McMahon C, Chen J, Aversa A, Perelman M. The controversial role of phosphodiesterase type 5 inhibitors in the treatment of premature ejaculation. J Sex Med. 2011;8:2135–2143. doi: 10.1111/j.1743-6109.2011.02401.x. [DOI] [PubMed] [Google Scholar]
- 214.McMahon CG, Stuckey B, Andersen ML. Efficacy of Viagra: Sildenafil citrate in men with premature ejaculation. J Sex Med. 2005;2:368–375. doi: 10.1111/j.1743-6109.2005.20351.x. [DOI] [PubMed] [Google Scholar]
- 215.Salonia A, Maga T, Colombo R, Scattoni V, Briganti A, Cestari A, Guazzoni G, Rigatti P, Montorsi F. A prospective study comparing paroxetine alone versus paroxetine plus sildenafil in patients with premature ejaculation. J Urol. 2002;168:2486–2489. doi: 10.1016/S0022-5347(05)64174-2. [DOI] [PubMed] [Google Scholar]
- 216.Asimakopoulos AD, Miano R, Finazzi Agro E, Vespasiani G, Spera E. Does current scientific and clinical evidence support the use of phosphodiesterase type 5 inhibitors for the treatment of premature ejaculation? A systematic review and meta-analysis. J Sex Med. 2012;9:2404–2416. doi: 10.1111/j.1743-6109.2011.02628.x. [DOI] [PubMed] [Google Scholar]
- 217.McMahon CG, McMahon CN, Leow LJ, Winestock CG. Efficacy of type-5 phosphodiesterase inhibitors in the drug treatment of premature ejaculation: A systematic review. BJU Int. 2006;98:259–272. doi: 10.1111/j.1464-410X.2006.06290.x. [DOI] [PubMed] [Google Scholar]
- 218.Frink MC, Hennies HH, Englberger W, Haurand M, Wilffert B. Influence of tramadol on neurotransmitter systems of the rat brain. Arzneimittelforschung. 1996;46:1029–1036. [PubMed] [Google Scholar]
- 219.Safarinejad MR, Hosseini SY. Safety and efficacy of tramadol in the treatment of premature ejaculation: A double-blind, placebo-controlled, fixed-dose, randomized study. J Clin Psychopharmacol. 2006;26:27–31. doi: 10.1097/01.jcp.0000195110.79027.3f. [DOI] [PubMed] [Google Scholar]
- 220.Szkutnik-Fiedler D, Kus K, Balcerkiewicz M, Grzeskowiak E, Nowakowska E, Burda K, Ratajczak P, Sadowski C. Concomitant use of tramadol and venlafaxine—Evaluation of antidepressant-like activity and other behavioral effects in rats. Pharmacol Rep. 2012;64:1350–1358. doi: 10.1016/s1734-1140(12)70932-5. [DOI] [PubMed] [Google Scholar]
- 221.Alghobary M, El-Bayoumy Y, Mostafa Y, Mahmoud el HM, Amr M. Evaluation of tramadol on demand versus daily paroxetine as a long-term treatment of lifelong premature ejaculation. J Sex Med. 2010;7:2860–2867. doi: 10.1111/j.1743-6109.2010.01789.x. [DOI] [PubMed] [Google Scholar]
- 222.Salem EA, Wilson SK, Bissada NK, Delk JR, Hellstrom WJ, Cleves MA. Tramadol HCL has promise in on-demand use to treat premature ejaculation. J Sex Med. 2008;5:188–193. doi: 10.1111/j.1743-6109.2006.00424.x. [DOI] [PubMed] [Google Scholar]
- 223.Bar-Or D, Salottolo KM, Orlando A, Winkler JV. A randomized double-blind, placebo-controlled multicenter study to evaluate the efficacy and safety of two doses of the tramadol orally disintegrating tablet for the treatment of premature ejaculation within less than 2 minutes. Eur Urol. 2011;61:736–743. doi: 10.1016/j.eururo.2011.08.039. [DOI] [PubMed] [Google Scholar]
- 224.Eassa BI, El-Shazly MA. Safety and efficacy of tramadol hydrochloride on treatment of premature ejaculation. Asian J Androl. 2013;15:138–142. doi: 10.1038/aja.2012.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Takeshita J, Litzinger M. Serotonin syndrome associated with tramadol. Prim Care Companion J Clin Psychiatry. 2009;11:273. doi: 10.4088/PCC.08l00690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Arletti R, Bazzani C, Castelli M, Bertolini A. Oxytocin improves male copulatory performance in rats. Horm Behav. 1985;19:14–20. doi: 10.1016/0018-506x(85)90002-9. [DOI] [PubMed] [Google Scholar]
- 227.Stoneham MD, Everitt BJ, Hansen S, Lightman SL, Todd K. Oxytocin and sexual behaviour in the male rat and rabbit. J Endocrinol. 1985;107:97–106. doi: 10.1677/joe.0.1070097. [DOI] [PubMed] [Google Scholar]
- 228.Argiolas A, Collu M, D'Aquila P, Gessa GL, Melis MR, Serra G. Apomorphine stimulation of male copulatory behavior is prevented by the oxytocin antagonist d(CH2)5 Tyr(Me)-Orn8-vasotocin in rats. Pharmacol Biochem Behav. 1989;33:81–83. doi: 10.1016/0091-3057(89)90433-4. [DOI] [PubMed] [Google Scholar]
- 229.Clement P, Peeters M, Bernabe J, Denys P, Alexandre L, Giuliano F. Brain oxytocin receptors mediate ejaculation elicited by 7-hydroxy-2-(di-N-propylamino) tetralin (7-OH-DPAT) in anaesthetized rats. Br J Pharmacol. 2008;154:1150–1159. doi: 10.1038/bjp.2008.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Shinghal R, Barnes A, Mahar K, Stier B, Giancaterino L, Condreay LD, Black L, McCallum SW. Safety and efficacy of epelsiban in the treatment of men with premature ejaculation: A randomized, double-blind, placebo-controlled, fixed-dose study. J Sex Med. 2013;10:2506–2517. doi: 10.1111/jsm.12272. discussion 16–7. [DOI] [PubMed] [Google Scholar]
- 231.Yang CC, Bradley WE. Peripheral distribution of the human dorsal nerve of the penis. J Urol. 1998;159:1912–1916. doi: 10.1016/S0022-5347(01)63194-X. [DOI] [PubMed] [Google Scholar]
- 232.David Prologo J, Snyder LL, Cherullo E, Passalacqua M, Pirasteh A, Corn D. Percutaneous CT-guided cryoablation of the dorsal penile nerve for treatment of symptomatic premature ejaculation. J Vasc Interv Radiol. 2013;24:214–219. doi: 10.1016/j.jvir.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 233.Basal S, Goktas S, Ergin A, Yildirim I, Atim A, Tahmaz L, Dayanc M. A novel treatment modality in patients with premature ejaculation resistant to conventional methods: The neuromodulation of dorsal penile nerves by pulsed radiofrequency. J Androl. 2010;31:126–130. doi: 10.2164/jandrol.108.007344. [DOI] [PubMed] [Google Scholar]
- 234.Fein RL. Intracavernous medication for treatment of premature ejaculation. Urology. 1990;35:301–303. doi: 10.1016/0090-4295(90)80149-h. [DOI] [PubMed] [Google Scholar]
- 235.Sunay D, Sunay M, Aydogmus Y, Bagbanci S, Arslan H, Karabulut A, Emir L. Acupuncture versus paroxetine for the treatment of premature ejaculation: A randomized, placebo-controlled clinical trial. Eur Urol. 2011;59:765–771. doi: 10.1016/j.eururo.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 236.Jeon HJ, Kim HS, Lee CH, Lee YG, Choi SM, Sohn YS, Shin CY, Kim J, Shim HJ, Kang KK, Ahn BO, Kim SH. Candidate molecule for premature ejaculation, DA-8031: In vivo and in vitro characterization of DA-8031. Urology. 2011;77:e17–21. doi: 10.1016/j.urology.2010.11.046. [DOI] [PubMed] [Google Scholar]
- 237.Kang KK, Ahn GJ, Sung JH, Kim SH, Kim H, Lee S. Ejaculatory responses are inhibited by a new chemical entity, DA-8031, in preclinical rodent models of ejaculation. Urology. 2013;81:e13–18. doi: 10.1016/j.urology.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 238.Marson L, Yu G, Farber NM. The effects of oral administration of d-modafinil on male rat ejaculatory behavior. J Sex Med. 2010;7:70–78. doi: 10.1111/j.1743-6109.2009.01509.x. [DOI] [PubMed] [Google Scholar]
- 239.Serefoglu EC, Silay MS. Botulinum toxin-A injection may be beneficial in the treatment of life-long premature ejaculation. Med Hypotheses. 2010;74:83–84. doi: 10.1016/j.mehy.2009.07.038. [DOI] [PubMed] [Google Scholar]
- 240.Serefoglu ECHW, Lesker GF, Grissom EM, Sikka SC, Dohanich GP, Hellstrom WJG. Effect of botulinum—A toxin injection into Bulbospongiosus muscle on ejaculatory latency time in male rats. In: Goldstein I, editor. World meeting on sexual medicine. Chicago: Wiley-Blackwell; 2012. p. 331. [Google Scholar]
- 241.Althof S. Sex therapy in the age of pharmacotherapy. Annu Rev Sex Res. 2006:116–132. [Google Scholar]
- 242.Perelman M. A new combination treatment for premature ejaculation. A sex therapist's perspective. J Sex Med. 2006;3:1004–1012. doi: 10.1111/j.1743-6109.2006.00238.x. [DOI] [PubMed] [Google Scholar]
- 243.Li P, Zhy G, Xu P, Sun J, Wang P. Interventional effect of behavioral psychotherapy on patients with premature ejaculation [Chinese] Zhonghua nan ke xue = Natl J Androl. 2006;12:717–719. [PubMed] [Google Scholar]
- 244.Tang W, Ma L, Zhao L, Liu Y, Chen Z. Clinical efficacy of viagra with behavior therapy against premature ejaculation [Chinese] Zhonghua nan ke xue = Natl J Androl. 2004;10:366–367. [PubMed] [Google Scholar]
- 245.Yuan P, Dai J, Yang Y, Guo J, Liang R. A comparative study on treatment for premature ejaculation: citalopram used in combination with behavioral therapy versus either citalopram or behavioral therapy alone [Chinese] Chin J Androl. 2008;22:35–38. [Google Scholar]
- 246.Steggall M, Fowler C, Pryce A. Combination therapy for PE: Results of a small-scale study. Sex Relat Ther. 2008;23:365–376. [Google Scholar]
- 247.Abdo CH, Afif-Abdo J, Otani F, Machado AC. Sexual satisfaction among patients with erectile dysfunction treated with counseling, sildenafil, or both. J Sex Med. 2008;5:1720–1726. doi: 10.1111/j.1743-6109.2008.00841.x. [DOI] [PubMed] [Google Scholar]
- 248.Aubin S, Heiman J, Berger R, Murallo A, Yung-Wen L. Comparing sildenafil alone versus sildenafil plus brief couple sex therapy on erectile dysfunction and couples' sexual and marital quality of life: A pilot study. J Sex Marital Ther. 2009;35:122–143. doi: 10.1080/00926230802712319. [DOI] [PubMed] [Google Scholar]
- 249.Perelman M. Sex coaching for physicians: Combination treatment for patient and partner. Int J Impot Res. 2003;15:S67–74. doi: 10.1038/sj.ijir.3901075. [DOI] [PubMed] [Google Scholar]
- 250.McMahon C, Abdo C, Incrocci L, Perelman M, Rowland D, Stuckey B, Waldinger M, Xin ZC. Disorders of orgasm and ejaculation in men. In: Lue T, Basson R, Rosen R, editors. Sexual medicine: Sexual dysfunctions in men and women (2nd International Consultation on Sexual Dysfunctions) Paris: Health Publications; 2004. pp. 409–468. [Google Scholar]
- 251.Jannini E, Isidori A, Aversa A, Lenzi A, Althof SE. Which first? The controversial issue of precedence in the treatment of male sexual dysfunctions. J Sex Med. 2013;10:2359–2369. doi: 10.1111/jsm.12315. [DOI] [PubMed] [Google Scholar]
- 252.American Academy of Family Physicians. Definition of Primary Care. Available at: http://www.aafp.org/online/en/home/policy/policies/p/primarycare.html (accessed November 11, 2009)
- 253.Annon J. Behavioral treatment of sexual problems: Brief therapy. Hagerstown, MD: Harper & Row; 1976. [Google Scholar]
- 254.Sadowsky R. The role of the primary care clinician in the management of erectile dysfunction. Rev Urol. 2002;4:S54–63. [PMC free article] [PubMed] [Google Scholar]
- 255.Murray M. Reducing waits and delays in the referral process. Fam Pract Manag. 2002;9:39–42. [PubMed] [Google Scholar]