Abstract
A 54-year-old man was admitted to our hospital for further examination following a chest radiographic screening test. He was asymptomatic but had an elevated serum concentration of alpha-fetoprotein. Chest computed tomography (CT) and magnetic resonance imaging showed a posterior mediastinal mass in the left thoracic paravertebral region. CT-guided percutaneous needle biopsy was performed, and the histological findings confirmed nonseminomatous germ cell tumor (NSGCT). Gonadal examination and F-18 fluorodeoxyglucose positron emission tomography findings indicated the posterior mediastinum as the origin of the disease. Reports of primary NSGCT in the posterior mediastinum are extremely rare.
Keywords: Alpha-fetoprotein, germ cell tumor, mediastinal tumor, neurogenic tumor
Introduction
Radiographic features and the location of mediastinal tumors usually enable the correct diagnosis to be made. In the posterior mediastinum, neurogenic tumors and bronchogenic cysts predominate. Primary malignant germ cell tumors of the mediastinum are rare, accounting for only 10%–15% of all mediastinal tumors, and usually involve the anterior mediastinum [1]. Primary malignant germ cell tumors, such as seminoma or teratoma, in the posterior mediastinum have been reported but these are extremely rare [2, 3]. Here, we present a case of extragonadal nonseminomatous germ cell tumor (NSGCT) arising in the posterior mediastinum.
Case Report
A 54-year-old man undergoing health screening was found to have a chest radiographic abnormality and was admitted to our hospital for further examination. He did not have any clinical symptoms. On admission, the results of physical examination were normal. In addition, no testicular abnormalities were detected by palpation or ultrasonography. Laboratory findings on admission indicated that serum alpha-fetoprotein (AFP) was markedly elevated (60,500 ng/mL), but chorionic gonadotropin beta subunit level was normal. Chest computed tomography (CT) showed a homogeneous mass in the posterior mediastinum along the left vertebral area (Fig. 1A and B). Chest axial magnetic resonance imaging revealed a tumor in the posterior mediastinum with relatively low intensity on T1-weighted magnetic resonance angiography (Fig. 1C) and high intensity on T2-weighted magnetic resonance imaging (Fig. 1D). The patient underwent CT-guided percutaneous needle biopsy, and the histological findings and immunochemical staining for AFP confirmed an NSGCT (yolk sac tumor) (Fig. 2). 18F-Fluorodeoxy glucose positron emission tomography revealed abnormal accumulation in the posterior lesion without any other lesions. The patient was treated with chemotherapy followed by surgery.
Figure 1.
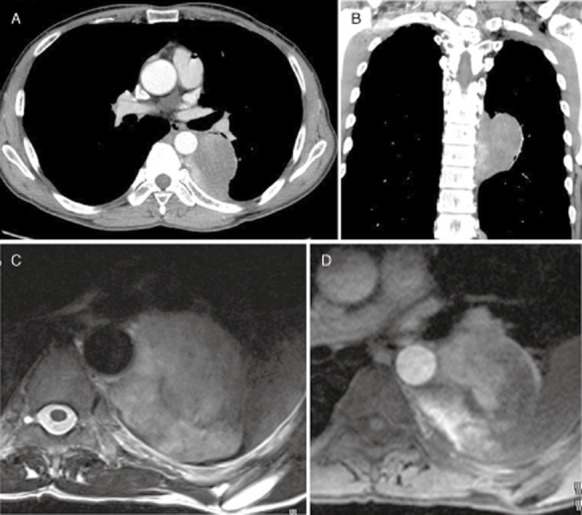
Chest computed tomography showed a mass in the posterior mediastinum along the left paravertebral area (A, axial view; B, coronal view). The mass was heterogeneous with irregular margins. Chest axial magnetic resonance imaging showed a tumor of relatively low intensity in the posterior mediastinum on T1-weighted magnetic resonance angiography (C) and of high intensity on T2-weighted magnetic resonance imaging (D).
Figure 2.
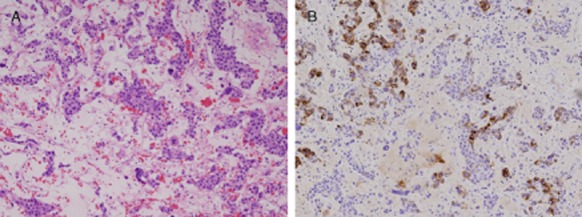
Photomicrograph of needle biopsy specimen. Hematoxylin-eosin stained sections revealed diffuse malignant cells (A 100×) and immunostaining was positive for anti–alpha-fetoprotein (B 100×).
Discussion
Primary mediastinal NSGCT usually occurs in the anterior mediastinum and presents in young adulthood [1]. Although the precise histogenesis of mediastinal NSGCT has not been determined, it has been postulated that primordial germ cells stray into midline extragonadal areas in the migration during embryonic development. As primordial germ cells pursue a dorsal route along the midline, it is surprising that mediastinal seminomas outside the anterior mediastinum are so rare. Indeed, several cases of seminoma in the posterior mediastinum have been reported in the literature [2, 3]. However, to our knowledge, only two cases of primary NSGCT in the posterior mediastinum have been reported to date [4, 5]. One case initially presented neurological signs of brain metastasis, and the surgical resection of the brain tumor revealed choriocarcinoma. The primary tumor was found to be located on posterior mediastinum in autopsy. Another case developed a dumbbell type of extension, and the tumor was located in left posterior mediastinum. The pathological examination by the surgical resection via laminectomy showed yolk sac carcinoma. Serum tumor markers including AFP and human chorionic gonadotropin were elevated, respectively. It is well known that these tumor markers are important to be an initial evaluation or differential diagnosis of NSGCTs, especially in patients with anterior mediastinal masses [5]. Increased AFP was observed in the present case. If tumor markers had not been checked in the present case, the patient would have undergone a primary resection of the posterior mediastinal tumor surrounding the descending aorta.
Neurogenic tumors are most common in the posterior mediastinum and account for 75% of primary neoplasms observed in this region. Schwannoma and neurofibroma arising from peripheral nerves are the most common neurogenic tumors in adults. Tumors of nerve sheath origin are usually spherical and lobulated masses with sharp margins. The mass may be fairly homogeneous or heterogeneous. The low attenuation on radiographic analysis is correlated with pathological areas of hypocellularity, cystic changes, and hemorrhage within the tumor. Typical magnetic resonance imaging signal intensity in the mass shows low intensity on T1-weighted images and intermediate to high intensity on T2-weighted images. These characteristics of neurogenic tumors correspond to those in the present case. In the present case, the mass extended along the paravertebral area, but the tumor was an irregular mass on axial view and no radiographic signs extended through the intervertebral foramen. These findings seem to be slightly inconsistent with those of neurogenic tumors showing a spindle-shaped soft tissue mass. However, we think that it is difficult for chest clinicians or radiologists to estimate the possibility of mediastinal NSGCT from the radiological findings in the present case. Thus, when the tumor in posterior mediastinum shows a rapid growing or untypical radiographic appearances with neurogenic tumors, we should examine AFP and human chorionic gonadotropin as a possibility of mediastinal NSGCTs.
In conclusion, our case demonstrated that mediastinal NSGCT does not always occur in the anterior mediastinum. In cases in which radiological findings are atypical for neurogenic tumors, we should consider the possibility of NSGCT and examine the tumor markers.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
References
- 1.Nichols CR. Mediastinal germ cell tumors. Clinical features and biologic correlates. Chest. 1991;99:472–479. doi: 10.1378/chest.99.2.472. [DOI] [PubMed] [Google Scholar]
- 2.Ravenel JG, Gordon LL, Block MI, et al. Primary posterior mediastinal seminoma. Am. J. Roentgenol. 2004;183:1835–1837. doi: 10.2214/ajr.183.6.01831835. [DOI] [PubMed] [Google Scholar]
- 3.Sinclair DS, Bolen MA. King MA. Mature teratoma within the posterior mediastinum. J. Thorac. Imaging. 2003;18:53–55. doi: 10.1097/00005382-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Yamashita S, Ohyama C, Nakagawa H, et al. Primary choriocarcinoma in the posterior mediastinum. J. Urol. 2002;167:1789. [PubMed] [Google Scholar]
- 5.Thomas C, Kalifa C, Couannet D, et al. An uncommon site of malignant germ cell tumor secreting alpha fetoprotein: the posterior mediastinum. Arch. Fr. Pediatr. 1993;50:879–881. [PubMed] [Google Scholar]


