Abstract
Key Clinical Message
Norovirus (NoV) and rotavirus (RV) gastroenteritis are usually self-limiting. However, few pediatric cases of bowel perforation and no duodenal perforation with NoV gastroenteritis were reported. We describe two children with duodenal perforation due to NoV or RV gastroenteritis. Suspicion for this association enables prompt intervention, preventing lethal outcomes of these common infections.
Keywords: Bowel perforation, duodenum, viral gastroenteritis
Introduction
Norovirus (NoV) and rotavirus (RV) are the most common causes of epidemic gastroenteritis in children 1,2. Gastroenteritis due to NoV and RV is usually self-limiting. However, diarrhea-associated death in children under 5 years of age is high (20%) in developing countries 2. Few pediatric cases of bowel perforation associated with gastroenteritis due to these viruses including a case of duodenal perforation in an infant with RV gastroenteritis have also been reported 3–5. However, to our knowledge, duodenal perforation associated with NoV gastroenteritis has not been described in children. In this report, we describe one pediatric case of duodenal perforation associated with NoV and another one with RV gastroenteritis. In the absence of any other apparent cause, complication due to the underlying viral gastroenteritis was deemed to be the most likely etiology.
Patient 1
A 2-year-old previously healthy boy with a 3-day history of vomiting and diarrhea presented to our hospital because of fever, lethargy, and continuous vomiting and diarrhea. He was pale and severely dehydrated but had normal blood pressure. Physical examination revealed no bruise or scar of burns to suggest child abuse. The abdomen was soft and not distended, and bowel sounds were absent. Laboratory investigations revealed normal hematocrit, serum electrolytes and amylase, but leucocytosis and positive C-reactive protein. Stool cultures did not reveal pathogenic bacteria. A plain X-ray showed free subdiaphragmatic air. Abdominal computed tomography confirmed free peritoneal gas and fluid retention. The patient was transferred to the Ishikawa Prefecture Central Hospital for further surgical management.
On admission, the stool analysis was positive for NoV. At laparotomy, there was a 1-cm diameter perforation at the anterior duodenal bulb (Fig.1A). The intestinal wall around the perforated site was edematous, but there was no mural thinning or thickening, necrosis, ulcerative lesions, or intramural hematoma. The perforated site was surgically closed with an omental patch. Postsurgical recovery was uneventful. He was discharged on day 14 after surgery.
Figure 1.
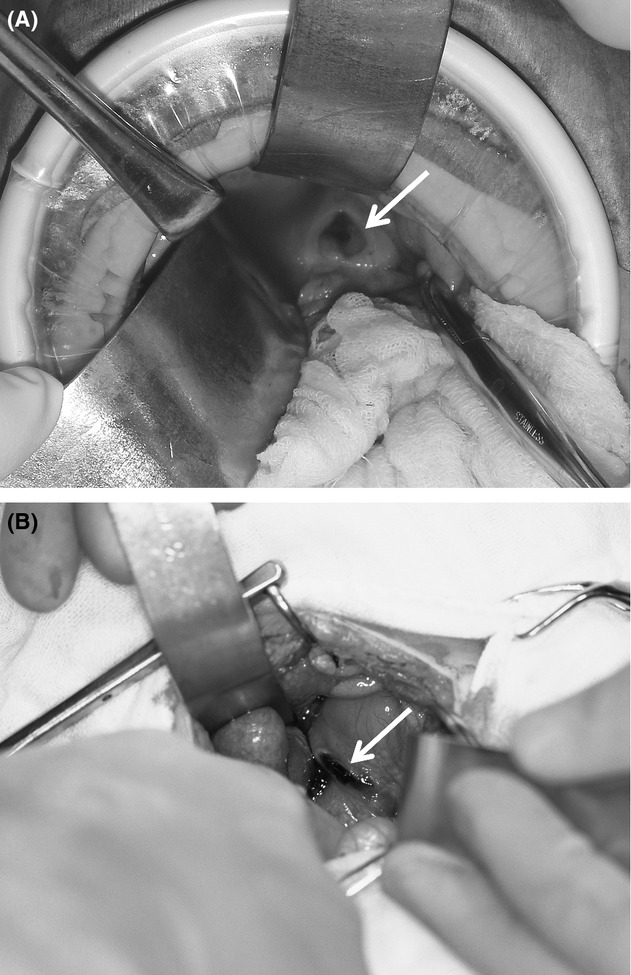
A laparotomy revealed a perforation 1 cm in diameter (A, arrow) and 1.5 cm in diameter (B, arrow) at the anterior duodenal bulb in children with norovirus and rotavirus gastroenteritis, respectively.
Patient 2
A 1-year-old previously healthy boy presented to a local hospital with a 2-day history of vomiting and diarrhea. He was found to have RV gastroenteritis because of positive RV antigen in the stool specimens. The following day, he began to vomit ground coffee-like materials and passed dark stool that was positive for occult blood. Due to deterioration of his condition, he was transferred to the Ishikawa Prefecture Central Hospital. On admission, he was pale, drowsy, and in preshock condition with severe dehydration. Physical examination revealed slightly distended abdomen with generalized guarding. There were no signs to suggest child abuse. Laboratory investigations revealed leucocytosis and mild anemia, but no electrolyte abnormalities were found. The patient was immediately taken up for laparotomy and a 1.5-cm diameter perforation at the anterior duodenal bulb was noted (Fig.1B). The perforated site showed no mural thinning or thickening, necrosis, ulcerative lesions, or intramural hematoma. The perforation was surgically closed. Subsequent clinical course in the hospital was uneventful. He was discharged on day 22 after surgery, and continues to be in good health.
Discussion
The most common causes for duodenal perforation in young children are accidental injury or trauma caused by child abuse 6. These were not found in the above-mentioned two cases. Thus, we conclude that the underlying NoV and RV gastroenteritis were the most likely causes leading to duodenal perforation. Our observation adds to the existing limited literature that duodenal perforation can be an uncommon yet severe manifestation of gastroenteritis due to common viruses such as NoV or RV in infants and young children.
It is believed that gastroenteritis due to NoV and RV typically causes minor intestinal inflammation 1,2. However, the information on intestinal pathology in those patients who had severe intestinal complications associated with epidemic viral gastroenteritis is scarce. Mural thickening, fibrosis, and necrosis of the intestine have been documented in three preterm babies with colonic perforation associated with NoV gastroenteritis 3. As was the case in the patients reported above, perforations of the stomach and duodenum without any associated pathological changes around the perforation sites have been reported in two infants with RV gastroenteritis 4,5. On the other hand, one report on spontaneous bowel perforation in children with acute viral gastroenteritis has described mucosal lesions such as focal ulcer or diffuse inflammation and necrosis around the perforation sites 7.
All reported pediatric cases of bowel perforation associated with NoV and RV gastroenteritis, including our cases, have been described in children less than 2 years of age. Both viruses infect mature enterocytes of the duodenal villi 1,2, and the host's inability to eliminate the viruses due to limited systemic and intestinal immunity at this age may be one responsible factor for an association of bowel perforation with NoV and RV gastroenteritis in the young. Severe dehydration associated with acute diarrhea may cause severe acute bowel ischemia, leading to bowel perforation 3,7. Although no ischemic or necrotic lesions were found at perforation sites, it is possible that acute and transient ischemia of the small intestine caused by severe dehydration could have triggered duodenal perforation. In addition, mucosal blood flow has been shown to be lower at anterior duodenal bulb than posterior bulb 8, suggesting that anterior duodenal bulb may be more susceptible to ischemia, resulting in severe mucosal and mural inflammation and reduced regeneration of the tissues. In fact, the perforation site was found at the anterior duodenal bulb in the above-mentioned patients. Furthermore, the ability to repair the mucosal inflammation of small intestine may be impaired in the young 9. These factors may contribute to duodenal perforation associated with severe Nov and RV gastroenteritis in the young.
In summary, our observation suggests that duodenal perforation can be a potential complication in infants and young children with the viral gastroenteritis due to NoV or RV. A high index of suspicion for this complication is required when the patients have sudden deterioration of clinical condition. Timely clinical intervention can prevent severe or lethal outcomes in children with this uncommon complication of a common clinical entity.
Acknowledgments
We thank H. Iwayama and S. Refetoff, The University of Chicago, Chicago, IL, USA, for their helpful advice in the revision of this manuscript.
Conflict of Interest
None declared.
Funding Information
No funding information provided.
References
- Karst SM. Pathogenesis of noroviruses, emerging RNA viruses. Viruses. 2010;2:748–781. doi: 10.3390/v2030748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundgren O. Svensson L. Pathogenesis of rotavirus diarrhea. Microbes Infect. 2001;3:1145–1156. doi: 10.1016/S1286-4579(01)01475-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelizzo G, Nakib G, Goruppi I, Fusillo M, Scorletti F, Mencherini S, et al. Isolated colon ischemia with norovirus infection in preterm babies: a case series. J. Med. Case Rep. 2013;7:108. doi: 10.1186/1752-1947-7-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu T, Horiuchi T, Hirooka S, Yonekura T. Tamai H. Idiopathic gastric rupture in a 3-month-old girl. Acta Paediatr. 2003;92:628–630. doi: 10.1080/08035250310002650. [DOI] [PubMed] [Google Scholar]
- Stabell N, Klingenberg C. Rushfeldt C. Duodenal perforation in an infant with rotavirus gastroenteritis. 2013. BMJ Case Rep 2013. doi: 10.1136/bcr-2012-008421. [DOI] [PMC free article] [PubMed]
- Gaines BA, Shultz BS, Morrison K. Ford HR. Duodenal injuries in children: beware of child abuse. J. Pediatr. Surg. 2004;39:600–602. doi: 10.1016/j.jpedsurg.2003.12.010. [DOI] [PubMed] [Google Scholar]
- Chen JC, Chen CC, Liang JT. Huang SF. Spontaneous bowel perforation in infants and young children: a clinicopathologic analysis of pathogenesis. J. Pediatr. Gastroenterol. Nutr. 2000;30:432–435. doi: 10.1097/00005176-200004000-00016. [DOI] [PubMed] [Google Scholar]
- Hentati N, Fournier HD, Papon X, Aube C, Vialle R. Mercier P. Arterial supply of the duodenal bulb: an anatomoclinical study. Surg. Radiol. Anat. 1999;21:159–164. doi: 10.1007/BF01630893. [DOI] [PubMed] [Google Scholar]
- Vieten D, Corfield A, Carroll D, Ramani P. Spicer R. Impaired mucosal regeneration in neonatal necrotising enterocolitis. Pediatr. Surg. Int. 2005;21:153–160. doi: 10.1007/s00383-004-1312-6. [DOI] [PubMed] [Google Scholar]


