Abstract
Key Clinical Message
A preterm infant at the age of 9 months with severe bronchopulmonary dysplasia (BPD) and large lobar emphysema, compromising ventilation into adjacent lobes with respiratory failure under maximal conservative treatment and pulmonary arterial hypertension recovered initially well after bilateral lung volume reduction surgery, but progressed 2 years later into respiratory failure. The initial imaging with Magnetic-Resonance-Imaging (MRI)-Angiography and decision-making was difficult and interdisciplinary treatment was essential.
Keywords: Bronchopulmonary dysplasia, emphysema, prematurity, surgery
Introduction
Some preterm infants with bronchopulmonary dysplasia (BPD) develop acquired lobar emphysema (ALE) with high mortality and morbidity 1,2.
Currently, there is no satisfactory way to improve lobar emphysema in infants, especially when the formation of bullae has lead to mechanical problems in ventilation, pulmonary hypertension, and compresses adjacent lobes. In severe emphysema in adults, one of the most promising approaches is lung volume reduction surgery (LVRS), in which large bullae or lobar emphysema is resected to allow adjacent lung tissue to expand and improve respiratory function 3.
Experiences with children are limited; cases are reported of successful LVRS for interstitial emphysema 4 and bullae after congenital diaphragmatic hernia (CDH) 5.
In addition to a case we reported earlier 6 of a female patient who was successfully treated with surgical lung volume reduction, we would like to share a recent case that was referred to us at 9 months of age, much later than our previous experiences.
Patient
The patient was born at 25 + 1 weeks of gestation with a birth weight of 790 g after premature rupture of membrane. Initially, he presented with second-degree respiratory distress syndrome and pronounced pulmonary hypertension. After standard initial treatment including surfactant twice, he was treated with high-frequency oscillation (HFO) for 12 days, repeated surfactant administration, and inhaled nitric oxide (iNO, max 20 ppm). Extubation was accomplished on the 37th day of life.
He was discharged at the age of 6 months with home oxygen 0.2–1 L/min via nasal insufflation. To quantify pulmonary hypertension, a catheter investigation was performed at the age of 7 months. A pronounced pulmonary artery hypertension (pulmonary artery pressure 42/16 mmHg, 2/3 systemic pressure under FiO2 100%) was found, which was not improved by NO or Ilomedin (pulmonary vascular resistance was 7.8 WExm²).
Result/Course at Our Hospital
After referral (pCO2 85 mmHg, 4–5 L O2/min), the patient was stabilized with diuretics (furosemide, thiazide), sedation, theophylline, inhaled iloprost, inhalative bronchodilators, and systemic glucocorticoids. Chest radiographs revealed two massive bullae in both lower lobes (Fig.1).
Figure 1.

Initial chest X-ray. Massive deformed thorax with dominant lower lobe bullae.
The decision for LVRS on the right side was interdisciplinary, based on computer tomography (CT) and MR Angiography, because conservative prognosis was limited. Informed consent was obtained and the situation was explained in detail to the parents.
Spiral CT showed 50% emphysematous deformations, 20% compressed, and 30% normal parts of the right lung, and 40% emphysematous deformations, 20% compressed, and 40% normal parts of the left lung, respectively (Fig.2). MR angiography confirmed the CT findings, that is, an impaired perfusion of the right lower lobe (Fig.3A).
Figure 2.
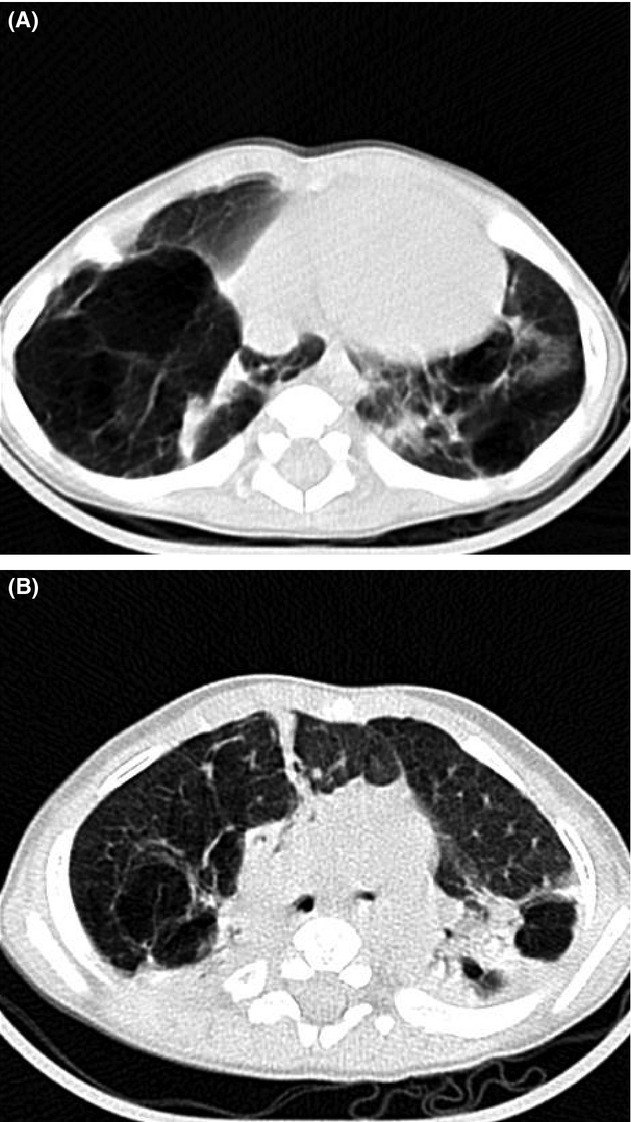
(A/B) Preoperative HRCT. Huge bullae bilaterally in lower lobes with compressed adjacent lung tissue, atelectasis, and herniation of left lung toward right.
Figure 3.
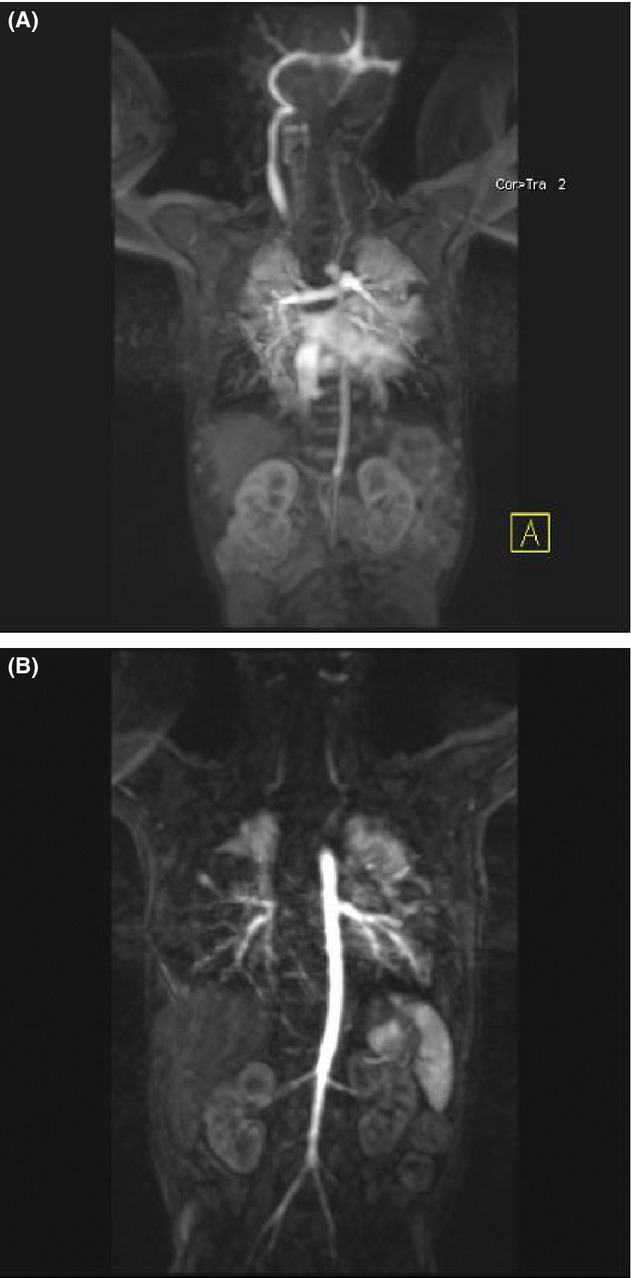
(A/B) MRI angiography with contrast preoperative/postoperative. In comparison, better perfusion on left, but recurrent bulla in right lower lobe.
As a first step, an atypical lower lobe resection on the right side was performed via lateral thoracotomy. Intraoperatively, the middle lobe seemed normal. The upper lobe was compressed, but extended after resection of the bulla in the lower lobe. Extubation on day 3 was successful after a short course of iNO.
In between surgeries, we established full enteral feeding with good weight gain (catch up growth to 10th percentile and improvement of psychomotor development and minimal oxygen requirement). In the following echocardiography, signs of pulmonary hypertension persisted.
Four weeks after the first surgery, atypical excision of the bulla in the left lower lobe was performed without complications. A postoperative MRI showed good ventilation of all lobes, but a reappearance of bullae in the right lower lobe (Fig.3).
We could discharge the patient with minimal oxygen supplementation (0.1–0.2 L/min) and good enteral feeding partially via percutaneous gastrostomy catheter leading to weight gain and growth parallel to the 10th percentile. Neurobehavioral development was assessed by Griffith Score at age of 14 months: motor skills, personal/social, auditory/voice 8 months, and general performance 7–8 months.
Eighteen months after discharge from the hospital and outpatient follow-up, the patient presented again with acute infectious exacerbation and respiratory failure. On initial CT, a recurrence of large emphysematous areas in the right lower lobe was diagnosed with compression of upper lobe tissue (Fig.4).
Figure 4.
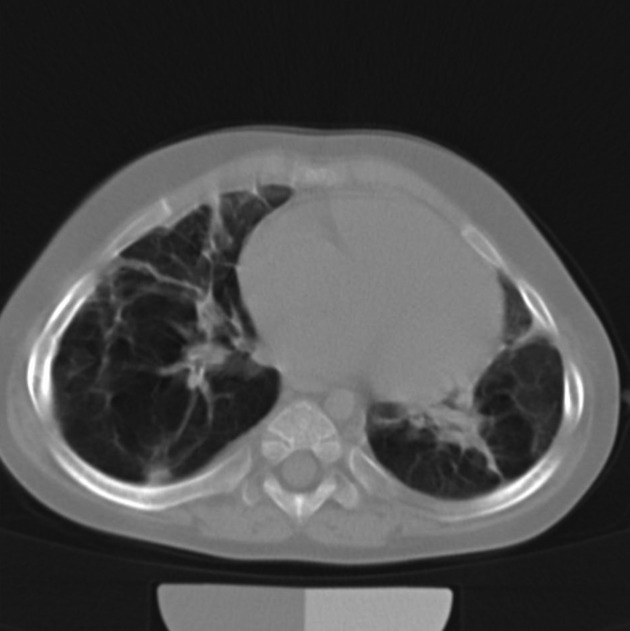
CT on readmission in acute infectious exacerbation.
The patient's clinical situation deteriorated under maximal conservative therapy and the parents decided together with the team of our ICU to limit further therapeutic escalation. The patient died in the arms of his parents 4 weeks after admission to the ICU.
Comment
LVRS has posed a therapeutic option for severe ALE when conservative treatment does not yield satisfactory results. We reported a case at our hospital that was treated with LVRS successfully 10 years ago and is still well on follow-up with perfectly normal development 6.
In adults, successful studies were undertaken to define specific criteria to identify patients who benefit from LVRS 7,8. So far, there are no criteria to identify infants that benefit from surgery. Due to structural lung development within the first 2-(4-6) years of life, surgery should probably not be withheld too long to provide time for pulmonary adaptation 9.
Initial imaging was difficult; high-resolution CT has been shown to be weakly predictive for postoperative outcome 10 and ventilation–perfusion scans have also been used with moderate predictive value in adults and even neonates 11. In the pediatric population, MRI has been discussed as gold-standard imaging of bronchopulmonary dysplasia, providing additional valuable information 12.
Due to the small number of patients, it will be hard to implement good studies to evaluate patients with deterioration under maximal conservative therapy for surgery, but indications for LVRS in infants need to be defined and cases like this need to be communicated.
Conflict of Interest
None declared.
Funding Information
No funding information provided.
References
- Azizkhan RG, Grimmer DL, Askin FB, Lacey SR, Merten DF. Wood RE. Acquired lobar emphysema (overinflation): clinical and pathological evaluation of infants requiring lobectomy. J. Pediatr. Surg. 1992;27:1145–1151. doi: 10.1016/0022-3468(92)90577-t. ; discussion 1151–1152. [DOI] [PubMed] [Google Scholar]
- Wong PM, Lees AN, Louw J, Lee FY, French N, Gain K, et al. Emphysema in young adult survivors of moderate-to-severe bronchopulmonary dysplasia. Eur. Respir. J. 2008;32:321–328. doi: 10.1183/09031936.00127107. [DOI] [PubMed] [Google Scholar]
- Criner GJ. Mamary AJ. Lung volume reduction surgery and lung volume reduction in advanced emphysema: who and why? Semin. Respir. Crit. Care Med. 2010;31:348–364. doi: 10.1055/s-0030-1254075. [DOI] [PubMed] [Google Scholar]
- Messineo A, Fusaro F, Mognato G, Sabatti M, D'Amore ES. Guglielmi M. Lung volume reduction surgery in lieu of pneumonectomy in an infant with severe unilateral pulmonary interstitial emphysema. Pediatr. Pulmonol. 2001;31:389–393. doi: 10.1002/ppul.1063.abs. [DOI] [PubMed] [Google Scholar]
- Yonekura T, Hirooka S, Kubota A, Hoki M, Kosumi T, Yamauchi K, et al. Surgical intervention for emphysematous pulmonary regions in a postoperative infant with congenital diaphragmatic hernia. J. Pediatr. Surg. 2000;35:1820–1821. doi: 10.1053/jpsu.2000.19268. [DOI] [PubMed] [Google Scholar]
- Siaplaouras J, Heckmann M, Reiss I, Schaible T, Waag KL. Gortner L. Lung volume reduction surgery in bronchopulmonary dysplasia. Acta Paediatr. 2003;92:754–756. doi: 10.1111/j.1651-2227.2003.tb00613.x. [DOI] [PubMed] [Google Scholar]
- Ginsburg ME, Thomashow BM, Yip CK, Dimango AM, Maxfield RA, Bartels MN, et al. Lung volume reduction surgery using the NETT selection criteria. Ann. Thorac. Surg. 2011;91:1556–1561. doi: 10.1016/j.athoracsur.2011.01.054. [DOI] [PubMed] [Google Scholar]
- Berger RL, Decamp MM, Criner GJ. Celli BR. Lung volume reduction therapies for advanced emphysema: an update. Chest. 2010;138:407–417. doi: 10.1378/chest.09-1822. [DOI] [PubMed] [Google Scholar]
- Burri PH. Structural aspects of postnatal lung development – alveolar formation and growth. Biol. Neonate. 2006;89:313–322. doi: 10.1159/000092868. [DOI] [PubMed] [Google Scholar]
- Washko GR, Martinez FJ, Hoffman EA, Loring SH, Estepar RS, Diaz AA, et al. Physiological and computed tomographic predictors of outcome from lung volume reduction surgery. Am. J. Respir. Crit. Care Med. 2010;181:494–500. doi: 10.1164/rccm.200906-0911OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonidas JC, Moylan FM, Kahn PC. Ramenofsky ML. Ventilation-perfusion scans in neonatal regional pulmonary emphysema complicating ventilatory assistance. AJR Am. J. Roentgenol. 1978;131:243–246. doi: 10.2214/ajr.131.2.243. [DOI] [PubMed] [Google Scholar]
- Ley-Zaporozhan J, Puderbach M. Kauczor HU. MR for the evaluation of obstructive pulmonary disease. Magn. Reson. Imaging Clin. N. Am. 2008;16:291–308. doi: 10.1016/j.mric.2008.02.014. ix. [DOI] [PubMed] [Google Scholar]


