Abstract
Purpose
While the addition of radiation to chemotherapy improves survival in patients with locally advanced pancreatic cancer, more effective therapies are urgently needed. Thus, we investigated the radiosensitizing efficacy of the novel drug combination of Wee1 and PARP1/2 [poly (ADP-ribose) polymerase 1/2] inhibitors (AZD1775 and olaparib, respectively) in pancreatic cancer.
Experimental Design
Radiosensitization of AsPC-1 or MiaPaCa-2 human pancreatic cancer cells was assessed by clonogenic survival and tumor growth assays. Mechanistically, the effects of AZD1775, olaparib, and radiation on cell cycle, DNA damage (γH2AX) and HRR (homologous recombination repair) were determined.
Results
Treatment of AsPC-1 and MiaPaCa-2 cells with either AZD1775 or olaparib caused modest radiosensitization while treatment with the combination significantly increased radiosensitization. Radiosensitization by the combination of AZD1775 and olaparib was associated with G2 checkpoint abrogation and persistent DNA damage. In addition, AZD1775 inhibited HRR activity and prevented radiation-induced Rad51 focus formation. Finally, in vivo, in MiaPaCa-2-derived xenografts, olaparib did not radiosensitize, while AZD1775 produced moderate, yet significant, radiosensitization (P<0.05). Importantly, the combination of AZD1775 and olaparib produced highly significant radiosensitization (P<0.0001) evidenced by a 13-day delay in tumor volume doubling (vs radiation alone) and complete eradication of 20% of tumors.
Conclusions
Taken together, these results demonstrate the efficacy of combined inhibition of Wee1 and PARP inhibitors for radiosensitizing pancreatic cancers and support the model that Wee1 inhibition sensitizes cells to PARP inhibitor-mediated radiosensitization through inhibition of HRR and abrogation of the G2 checkpoint, ultimately resulting in unrepaired, lethal DNA damage and radiosensitization.
Keywords: pancreatic cancer, Wee1, PARP1/2, radiosensitization, homologous recombination repair
Introduction
Radiation is in an important component of therapy for locally advanced pancreatic cancer and in combination with concurrent gemcitabine or 5-fluorouracil is the standard of care for locally advanced disease. In combination with gemcitabine, radiation significantly improves patient survival compared to gemcitabine treatment alone (1). While recent studies from our group and others suggest that intensification of highly conformal radiation may extend survival in locally advanced patients beyond the approximate one year survival associated with standard chemoradiation therapies, more effective therapies are urgently needed (2, 3). Since approximately 30% of pancreatic cancer patients die from local disease progression (4), management of local disease is a critical issue. Thus, in the present study we have focused on a strategy to improve therapy for local disease by using a novel combination of molecularly targeted agents as radiation sensitizers in pancreatic cancers.
Inhibition of the DNA damage response is a promising strategy for sensitizing cancer cells to the lethal DNA DSBs (double strand breaks) induced by ionizing radiation(5). We have previously shown that inhibition of Chk1 (checkpoint kinase 1) sensitizes pancreatic cancer cells and xenografts to radiation by mechanisms involving abrogation of the radiation-induced G2 checkpoint (via Cdc25A stabilization and Cdk1 activation) and inhibition of HRR (6). Furthermore, we have shown this sensitization is even greater in the presence of gemcitabine-based chemoradiation (7). Similar to Chk1, the Wee1 kinase has also been identified as a therapeutic target. Wee1 inhibition by the small molecule AZD1775 (formerly MK1775) radiosensitizes TP53 mutant solid tumors (8, 9). Inhibition of Wee1 has been shown to cause abrogation of the radiation-induced G2 checkpoint (via activation of Cdk1) and in addition, lead to impaired HRR (10) as well as to the induction of replication stress and DNA DSBs (the latter, regulated by Mus81-Eme1 endonuclease) (11, 12). The tumor cell selectivity of sensitization by Chk1 or Wee1 inhibitors is based, in part, on the presence of TP53 mutation (13–15). TP53 mutant tumor cells are more sensitive to G2 checkpoint abrogation due to their lack a G1 checkpoint, whereas p53 wild type normal cells are protected from G2 checkpoint abrogation by their intact G1 checkpoint. Since pancreatic cancers have a high incidence of TP53 mutation (16), inhibition of Wee1 is a promising approach for selectively sensitizing pancreatic tumors to radiation.
While the use of single molecularly targeted agents has demonstrated modest therapeutic benefits, there is growing interest in targeting multiple pathways or multiple steps within a single pathway to produce even more effective cancer therapies. In this context, combinations of agents which target the DNA damage response are an exciting new area of investigation. The combination of Chk1 and Wee1 inhibitors, for example, has synergistic anti-tumor activity through mechanisms involving both premature mitotic entry and increased DNA damage (17, 18). Given the synthetic lethality of PARP inhibitors in BRCA1/2 mutant or HRR defective cancers (19), combining PARP inhibitors with agents that inhibit HRR is another major area of investigation. Since radiosensitization by PARP inhibition is also more effective in DSB repair-defective tumor cells (20, 21), this strategy has been extended to radiation studies as well (22, 23). While direct inhibitors of HRR are in the very early stages of development (24), there are a few agents which have been shown to indirectly inhibit HRR, including small molecules targeting Chk1, Wee1, PP2A, Hsp90, and EGFR (7, 10, 22, 25, 26). For example, by reducing Rad51 and BRCA2 protein levels, the Hsp90 inhibitor 17-AAG has been shown to inhibit HRR and thus cause additive radiosensitization in combination with PARP inhibition (22). In addition, we have previously shown that the combination of a Chk1 inhibitor with olaparib produces highly significant radiosensitization preferentially in TP53 mutant cancers through mechanisms that involve HRR inhibition and G2 checkpoint abrogation (23).
In this study we sought to test the combination of the Wee1 inhibitor AZD1775, a first-in-class agent currently in Phase I/II clinical trials, and the PARP1/2 inhibitor olaparib, currently in Phase III clinical trials, as a radiosensitizing strategy in pancreatic cancers. We hypothesized that Wee1 and PARP inhibitors would interact to produce greater radiosensitization than either agent alone. To test this hypothesis, we assessed radiation survival in pancreatic cancer cells treated with AZD1775 and olaparib. When we found that simultaneous inhibition of Wee1 and PARP produced highly significant radiosensitization in pancreatic cancers, we went on to investigate the contributions of cell cycle checkpoint abrogation and HRR to the mechanisms of radiosensitization. In addition, we tested the ability of AZD1775 and olaparib to sensitize in vivo in human pancreatic cancer xenograft models.
Materials and Methods
Cell Culture and Drug Solutions
MiaPaCa2 and AsPC-1 cells were obtained from and authenticated (via short tandem repeat profiling) by the American Type Culture Collection (2009 and 2011, respectively). Cells used for this study were cryopreserved within 6 months of authentication. Cells were grown in DMEM (MiaPaCa2) or RPMI 1640 (AsPC-1) supplemented with 10% Fetal Bovine Serum (Life Technologies), 2 mM L-Glutamine (Sigma), and antibiotics. For in vitro experiments, AZD1775 (Axon Medchem) and olaparib (AstraZeneca) were each dissolved in dimethyl sulfoxide (Sigma) and stored in aliquots at −20°C. For in vivo experiments, AZD1775 was suspended in 0.5% methylcellulose (Sigma) and stored for a maximum of 5 days at room temperature with constant stirring, and olaparib was diluted as needed in 10% 2-hydroxypropyl-β-cyclodextrin (Sigma).
Clonogenic Survival Assyas
Cells treated with drugs or radiation were processed for clonogenic survival as previously described (27, 28). The radiation enhancement ratio was calculated as the ratio of the mean inactivation dose under control conditions divided by the mean inactivation dose after drug exposure (29). A value significantly greater than 1 indicates radiosensitization.
Flow Cytometry
Cells were trypsinized, washed with ice-cold PBS, and fixed at a concentration of 2 × 106 cells/mL in ice-cold 70% ethanol. For γH2AX analysis, samples were incubated with a mouse anti-γH2AX-specific antibody (clone JBW301; Millipore) overnight at 4°C followed by incubation with a FITC-conjugated secondary antibody (Sigma) as previously described (30). For quantification of γH2AX positivity, a gate was arbitrarily set on the control, untreated sample to define a region of positive staining for γH2AX of approximately 5%. This gate was then overlaid on the drug/radiation-treated samples. For pHistone H3 analysis, cells were processed as described above, then incubated with a rabbit anti-pHistone H3 (S10) antibody (Millipore) as previously described (31). Samples for both analyses were stained with propidium iodide to measure total DNA content and analyzed on a FACScan flow cytometer (Becton Dickinson) with FlowJo software (Tree Star).
Immunoblotting
Whole cell lysates were prepared in cold SDS lysis buffer (10mM Tris, 2% SDS) supplemented with PhosSTOP phosphatase inhibitor and Complete protease inhibitor cocktail tablets (Roche) as previously described (27). The following antibodies were used: Cdk1, pCdk1 (Y15), GAPDH (Cell Signaling Technology), pHistone H3 (S10), PAR (Millipore), Wee1 (Santa Cruz Biotechnology), pRPA32 (S4/8) (Bethyl) and RPA32 (Abcam). Immunoblots were quantitated using ImageJ (NIH).
Homologous Recombination Repair
MiaPaCa-2 cells stably expressing a DR-GFP reporter plasmid (32) were used to measure HRR of a DNA double strand break as previously described (6). In brief, double strand breaks were induced by adenoviral-mediated expression of the restriction enzyme I-SceI, which cleaves the defective DR-GFP gene. Homologous recombination repair of this break restores GFP expression. Beginning 18 hours post-transfection, cells were treated with drug for 24 hours. The extent of double strand break repair by HRR was then quantified by flow cytometric analysis of GFP expression.
Immunofluorescence
For immunofluorescence experiments, cells were grown and treated on cover slips in 12-well dishes. Following treatment, cells were fixed and stained as previously described (33) with a mouse monoclonal Rad51 antibody (GeneTex) and DAPI (4′,6-diamidino-2-phenylindole). Samples were imaged with an Olympus IX71 FluoView confocal microscope (Olympus America) with a 60x oil objective. Fields were chosen at random based on DAPI staining. For quantitation of Rad51 foci, at least 100 cells from each of three independent experiments were visually scored for each condition. Cells with 5 or more Rad51 foci were scored as positive.
Irradiation
Irradiations were performed using a Philips RT250 (Kimtron Medical) at a dose rate of ~2 Gy/min in the University of Michigan Comprehensive Cancer Center Experimental Irradiation Core. Dosimetry was performed using an ionization chamber connected to an electrometer system that is directly traceable to a National Institute of Standards and Technology calibration. For tumor irradiation, animals were anesthetized with isoflurane and positioned such that the apex of each flank tumor was at the center of a 2.4cm aperture in the secondary collimator, with the rest of the mouse shielded from radiation.
Tumor Growth Studies
Animals were handled in accordance with protocols approved by the University of Michigan Committee for Use and Care of Animals. MiaPaCa-2 cells (5×106) were suspended in a 1:1 mixture of 10%FBS-DMEM/Matrigel (BD Biosciences) and injected subcutaneously, bilaterally into the flanks of 3–5 week old, female athymic nude mice (Harlan). Treatment was initiated when the average tumor volume reached 100 mm3 and consisted of AZD1775 (60mg/kg; BID; 1h pre- and 4h post-RT; Mon–Fri), olaparib (60mg/kg, QD, 1h pre-RT; Mon–Fri), and radiation (1.8Gy/fraction; Mon–Fri) for one cycle. AZD1775 was administered via oral gavage; olaparib was administered via intraperitoneal injection. Tumor size was measured two times per week. Tumor volume (TV) was calculated according to the equation: TV = π/6 (ab2), where a and b are the longer and shorter dimensions of the tumor, respectively. Measurements were made until day 90 or until the tumor volume increased by approximately a factor of 5.
Statistics
Statistically significant differences for the clonogenic survival and immunofluorescence assays were determined by one-way ANOVA with the Tukey post-comparison test in GraphPad PRISM version 5 (GraphPad software). For homologous recombination repair assays, a Student’s, two-tailed, T-test was performed in GraphPad PRISM. For tumor growth experiments, the time required for tumor volume doubling was determined for each xenograft by identifying the earliest day on which it was at least twice as large as on the first day of treatment. The Kaplan-Meier method was used to analyze the doubling times. Log rank test (PROC LIFETEST in SAS) was used to compare the doubling times between any two treatment groups. In addition, the Bayesian hierarchical changepoint model (34) was used to compare tumor regression rates, regression periods, and regrowth rates between any two treatment groups.
Results
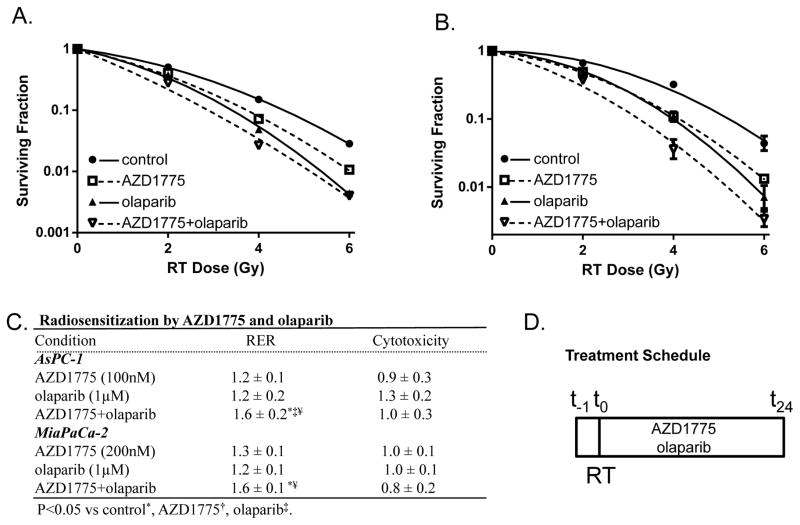
In order to determine whether combined Wee1 and PARP inhibition might interact to enhance radiosensitization, we treated pancreatic cancer cells with AZD1775 and olaparib, small molecule inhibitors of Wee1 and PARP1/2, respectively, under a treatment schedule optimized for radiosensitization with related inhibitors of the DNA damage response (Fig. 1D) (23). Treatment with non-toxic drug concentrations of either AZD1775 or olaparib for one hour prior to, and 24 hours post-radiation led to modest radiosensitization in both AsPC-1 and MiaPaCa-2 pancreatic cancer cell lines (Fig. 1A–C). More importantly, the combination of AZD1775 and olaparib significantly radiosensitized both cell lines, with radiation enhancement ratios of 1.6±0.2 and 1.6±0.1 (P<0.05), respectively. These data demonstrate that simultaneous inhibition of Wee1 and PARP improves radiosensitization over that afforded by inhibition of either Wee1 or PARP alone in pancreatic cancer cells.
Figure 1. Radiosensitization by combined Wee1 and PARP inhibition.
AsPC-1 (A) and MiaPaCa-2 (B) pancreatic cancer cell lines were treated with AZD1775 (100nM), olaparib (1μM), and radiation (0–6Gy) according to the schedule illustrated (D). At the end of treatment cells were processed for clonogenic survival. Data are from a single representative experiment (A–B) or are the mean radiation enhancement ratio (RER) ± SE for n = 3 independent experiments (C). Cytotoxicity in the absence of radiation treatment was calculated by normalizing the plating efficiencies of drug treated-cells to non-drug treated cells where plating efficiencies for non-drug treated AsPC-1 and MiaPaCa-2 cells were 0.2 and 0.3, respectively (C). Statistical significance (P<0.05) is indicated vs control*, AZD1775‡, and olaparib¥.
To begin to establish the mechanisms of radiosensitization in response to combined inhibition of Wee1 and PARP, we first investigated the effects of AZD1775 and olaparib on their respective downstream targets, phosphorylated-Cdk1 (Y15) and PAR [poly (ADP-ribose)], in MiaPaCa-2 cells. As anticipated, olaparib (1μM) significantly decreased PAR levels, a result consistent with inhibition of PARP-mediated protein poly-ADP-ribosylation, and AZD1775 (200nM) significantly reduced pCdk1 (Y15) levels, a result consistent with inhibition of Wee1-mediated phosphorylation at this site (Fig. 2). The redistribution of Cdk1 from an inactive, Y15-phosphorylated form to the dephosphorylated, and presumably active form, corresponded with an increase in levels of the mitotic marker, pHistone H3 in AZD1775-treated cells. Interestingly, AZD1775 also caused a significant increase in PAR levels in response to radiation (16 hours post-radiation; Fig. 2B), suggesting prolonged Wee1 inhibition following radiation increases PARP activity. Since Wee1 inhibition has previously been shown to cause aberrant replication origin firing leading to replication stress (11), we examined the effects of AZD1775, olaparib, and radiation on phosphorylated-RPA (S4/8) which accumulates on single-stranded DNA formed in association with replication stress and/or HRR-mediated resection of DNA DSBs (35, 36). Consistent with the induction of replication stress by AZD1775, pRPA (S4/8) levels were increased in response to AZD1775 alone or in combination with olaparib and radiation at both early and late time points.
Figure 2. The effects of AZD1775 and olaparib on DNA damage response signaling.
MiaPaCa-2 cells were treated with AZD1775 and olaparib for 1 hour pre- and 6 or 16 hours post-RT (6Gy). At the end of drug treatment cells were analyzed by immunoblotting for the indicated proteins. Data are from a single representative experiment (A) or are the mean fold-change in PAR or pCdk1 (Y15) levels relative to control ± SE at 16 hours post-RT from 3 independent experiments (B–C). Statistical significance (P<0.05) is indicated vs control* and radiation†.
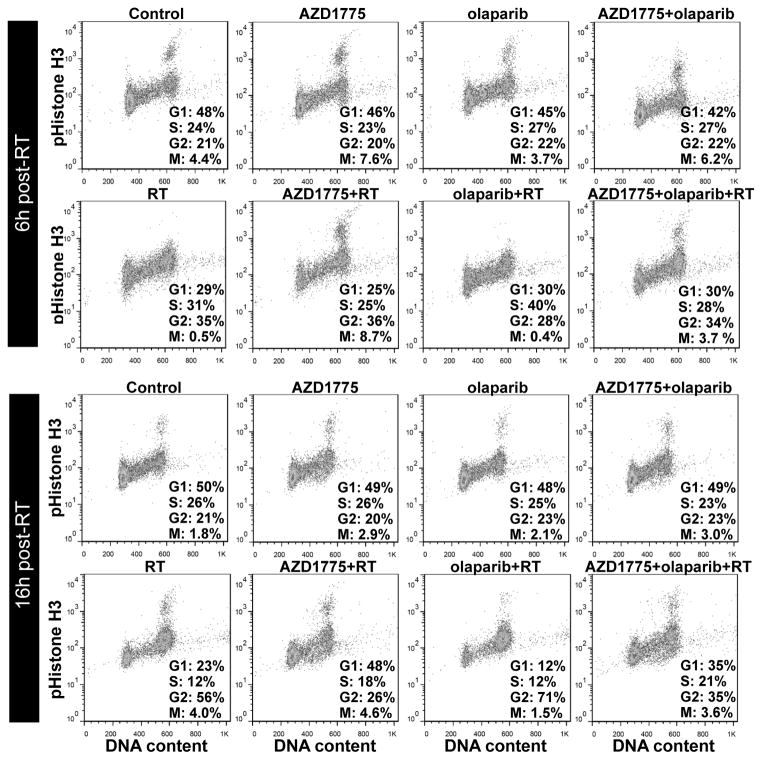
To further investigate the mechanisms of radiosensitization by combined Wee1 and PARP inhibition in MiaPaCa-2 cells, we next assessed the effects of AZD1775, olaparib, and radiation on the cell cycle. Based on previous results (8) and the data presented in Figure 2, we hypothesized that AZD1775-mediated Wee1 inhibition would abrogate the radiation-induced G2 checkpoint. As expected, we found that AZD1775 alone increased mitotic entry and abrogated the radiation-induced G2 checkpoint, as evidenced by an increase in pHistone H3-positive, mitotic cells at the 6 hour time point and a redistribution of irradiated cells from G2 to G1 at the 16 hour time point (Fig. 3; Suppl. Fig. 1). In addition, we found that olaparib treatment prolonged the radiation-induced G2 checkpoint at the 16 hour time point, as evidenced by an increase in the percentage of cells in G2 and corresponding decreases in the percentages of cells in mitosis and G1. Importantly, AZD1775 given in combination with olaparib and radiation abrogated this G2 checkpoint, as evidenced by an increase in the percentage of cells in mitosis and a redistribution of cells from G2 to G1. In addition, assessment of sub-G1 DNA content suggested that AZD1775 and olaparib do not induce apoptosis in response to radiation (Suppl. Fig. 2). Taken together, these data demonstrate that AZD1775 abrogates the G2 checkpoint induced by the combination of olaparib and radiation and suggest that the G2 checkpoint may be a mechanism of interaction between Wee1 and PARP inhibition on radiosensitization.
Figure 3. Abrogation of olaparib and radiation-induced G2 checkpoint by AZD1775.
MiaPaCa-2 cells were treated with AZD1775/olaparib (200nM/1uM, respectively) for 1 hour pre- and 6 (top) or 16 (bottom) hours post-RT (6Gy) and then analyzed for pHistone H3 and DNA content by flow cytometry. The percentages of cells in each phase of the cell cycle are indicated. Data are from single representative experiments. A summary of n=2 independent experiments is included in Suppl. Fig. 1.
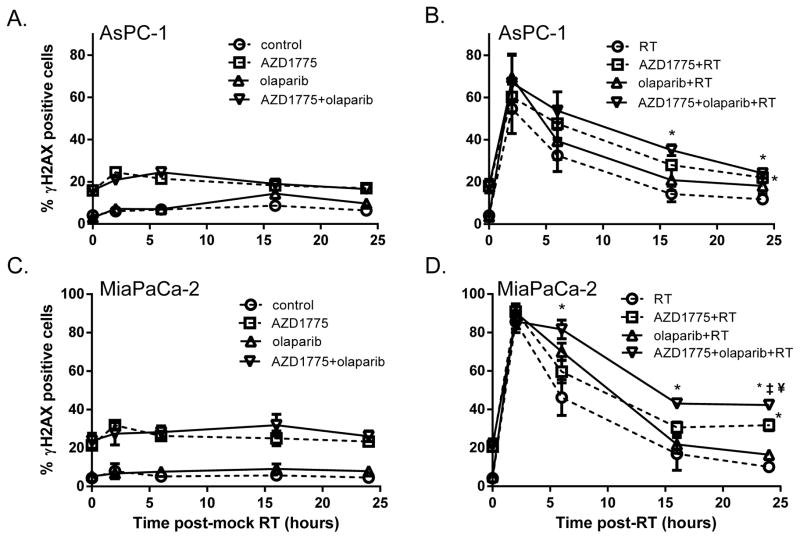
Given that abrogation of the G2 checkpoint forces cells with incompletely repaired DNA damage to progress through the cell cycle with persistent, and often lethal, DNA damage (37), we next assessed the effects of AZD1775 and olaparib on radiation-induced DNA damage. In the absence of radiation, AZD1775 (alone or in combination with olaparib), caused a rapid (within 1 hour) induction of γH2AX, an established marker of DNA DSBs (38) in both MiaPaCa-2 and AsPC-1 cells (Fig. 4A, C). This effect persisted throughout the drug-treatment period and is consistent with previous reports of replication stress and consequent Mus81-Eme1 endonuclease-induced DNA DSBs upon Wee1 inhibition (11, 12). In response to radiation alone, γH2AX levels peaked within 2 hours post-radiation, with substantial resolution occurring by 6 hours, and complete resolution by 24 hours in both cell lines (Fig. 4B, D). Treatment with AZD1775 led to persistent radiation-induced DNA damage in both cell lines evidenced by elevated γH2AX at 24 hours. More importantly, treatment with the combination of AZD1775 and olaparib resulted in significantly greater γH2AX at 16 and 24 hours post-radiation (compared to radiation alone) in AsPC-1 cells (Fig. 4B). The effects of AZD1775 and/or olaparib on γH2AX were more pronounced in MiaPaCa-2 cells. While olaparib treatment caused a transient delay in the repair of radiation-induced DNA DSBs in MiaPaCa-2 cells (46% vs 70% γH2AX-positive cells, 6 hours post-radiation vs olaparib+radiation, respectively), γH2AX expression persisted for 24 hours post-radiation in cells treated with AZD1775. More importantly, the greatest levels of residual DNA damage were found in cells treated with the combination of AZD1775 and olaparib with radiation, a result consistent with the increased radiosensitization found in cells treated with this combination of agents.
Figure 4. Combined inhibition of Wee1 and PARP causes persistent radiation-induced DNA damage.
AsPC-1 (A) and MiaPaCa-2 (B) cells were treated with AZD1775/olaparib for 1 hour pre- and for the indicated times post-RT. At each time point post-RT, cells were fixed for flow cytometric analysis and analyzed for γH2AX positivity and DNA content. Data shown are the mean percentage of γH2AX positive cells ± SE from n=3–4 independent experiments. Statistical significance (P<0.05) is indicated vs RT*, AZD1775+RT‡, and olaparib+RT¥.
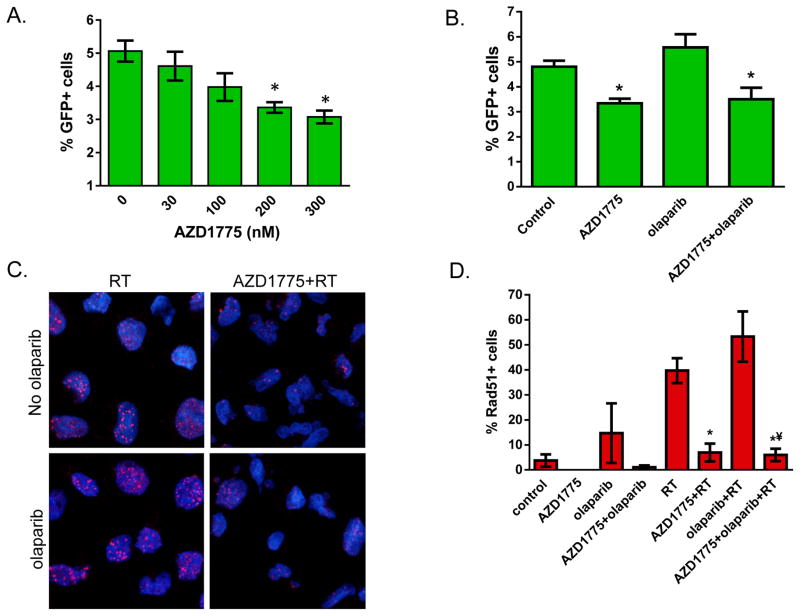
Based on our finding that Wee1 inhibition results in persistent radiation-induced DNA damage (Fig. 4), and a previous study demonstrating a role for Wee1 in HRR (10), we next assessed the effects of AZD1775 on HRR in MiaPaCa-2 cells. Given the radiosensitizing efficacy of PARP inhibitors in DNA DSB repair-defective cells (20, 21), we hypothesized that inhibition of HRR by AZD1775 may contribute to the greater radiosensitization afforded by combined Wee1 and PARP inhibition. Using MiaPaCa-2 cells transfected to express a reporter construct for homology-directed repair of an I-Sce1-induced DSB (32), we found a concentration-dependent decrease in HRR activity with increasing, though non-toxic, concentrations of AZD1775 (Fig. 5A). Consistent with previous reports, olaparib had no effect on either HRR activity or on AZD1775-mediated inhibition of HRR (23, 39) (Fig. 5B). To further characterize the effect of Wee1 inhibition on HRR, we assessed the effects of AZD1775 on Rad51, a key intermediary in HRR (40). Using immunofluorescent staining, we found significant Rad51 staining 24 hours after radiation in MiaPaCa-2 cells (Fig. 5C, D). As expected, AZD1775 significantly inhibited this response (40% vs 7% Rad51-positive cells in response to radiation vs AZD1775+radiation, respectively, P<0.05). Taken together, these data support the model that Wee1 inhibition by AZD1775 sensitizes cells to PARP inhibitor-mediated radiosensitization through inhibition of HRR and abrogation of the G2 checkpoint, ultimately resulting in unrepaired, lethal DNA damage.
Figure 5. Inhibition of HRR and Rad51 focus formation by AZD1775.
(A, B) MiaPaCa-2 cells stably expressing the DR-GFP homologous recombination repair reporter were infected with I-SceI-expressing adenovirus and treated for 24 hours with increasing concentrations of AZD1775 (A) or 200nM AZD1775 and 1μM olaparib (B) and assayed for GFP positivity by flow cytometry. Data are the mean percentage ± SE of n=3–4 independent experiments performed in duplicate. Statistical significance (P<0.05) is indicated vs control*. C and D, MiaPaCa-2 cells were treated with AZD1775 (200nM) and olaparib (1μM) for 1 hour pre- and 24 hours post-RT (6Gy). At the end of treatment, cells were stained for Rad51 (red) and with DAPI (blue). Images are from a single representative experiment (C). Data are the mean percentage ± SE of Rad51 positive cells (cells containing 5 or more Rad51 foci) from n=3 independent experiments. Statistical significance (P<0.05) is indicated vs RT* and olaparib+RT¥.
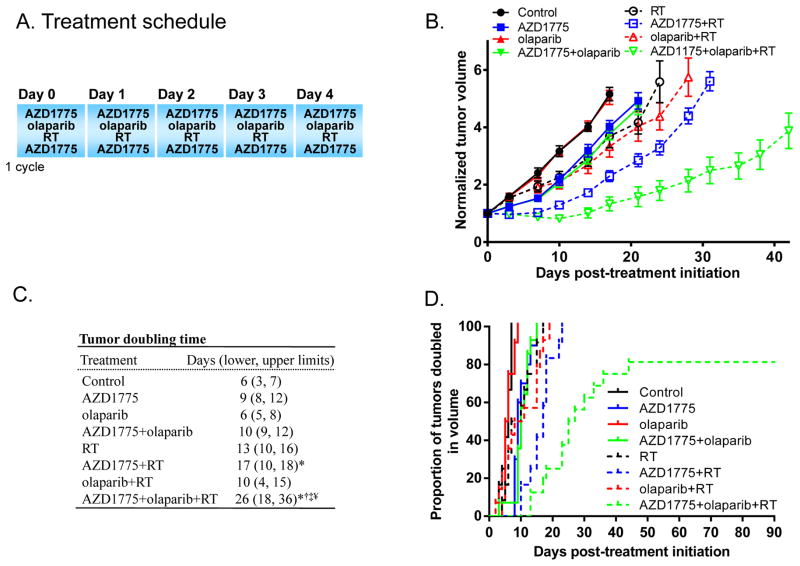
Based on the radiosensitization observed in vitro in response to Wee1 and PARP inhibition, we next addressed the question whether AZD1775 and olaparib would radiosensitize human tumor xenografts in vivo. Mice bearing sub-cutaneous MiaPaCa-2 tumor xenografts were treated daily with AZD1775, olaparib, and radiation for one cycle as depicted in Figure 6A. We found that, in the absence of radiation, neither AZD1775 nor olaparib had a significant effect on tumor growth, although mice receiving AZD1775 tended to have slightly longer tumor doubling times (Fig. 6B–D). In combination with fractionated radiation, AZD1775 produced significant radiosensitization, as evidenced by a 4-day delay in tumor doubling time relative to radiation alone (P<0.05), while olaparib produced no radiosensitization. The combination of AZD1775 and olaparib, however, produced highly significant radiosensitization (P<0.0001 vs radiation alone) that was also significantly greater than that achieved by either AZD1775 (P<0.002) or olaparib (P<0.0001), with 9- and 16-day delays in tumor doubling time, respectively. In addition, within the AZD1775, olaparib, radiation treatment group,3 tumors completely regressed during the first two weeks following therapy initiation, and remained undetectable for the duration of the study (90 days; Fig. 6D). Comprehensive statistical analysis of these data by the Bayesian hierarchical change point model (34) illustrated that the combination of AZD1775, olaparib, and radiation caused significant tumor regression for an average of 8 days (90% confidence interval: 3–14 days) whereas other treatments resulted in either stable disease (AZD1775+RT) or growth during treatment (RT and olaparib+RT). Furthermore, analysis with this model revealed that tumors treated with the combination of AZD1775, olaparib, and radiation had significantly slower tumor regrowth rates following the regression period, compared to tumors from other radiation-treatment groups. Finally, treatment with the combination of AZD1775, olaparib, and radiation caused no obvious systemic toxicity as assessed by weight loss (Suppl. Fig. 3). Taken together, these in vivo data indicate that AZD1775 and olaparib are well tolerated when administered together and produce highly significant radiosensitization in human pancreatic tumor models.
Figure 6. Radiosensitization of pancreatic tumor xenografts by combined treatment with AZD1775 and olaparib.
Athymic nude mice bearing bilateral, flank MiaPaCa-2 xenografts were treated with AZD1775 (60mg/kg; BID; 1h pre- and 4h post-RT; Mon–Fri), olaparib (60mg/kg, QD, 1h pre-RT; Mon–Fri), and radiation (RT; 1.8Gy/fraction; Mon–Fri) for one cycle as illustrated (A). B, Tumor volumes were normalized to the first day of treatment (day 0) and are the mean ± SE of 10–16 tumors per treatment group. Data shown are for the latest time point (17–42 days) before censoring occurred due to animals being removed from study due to tumor burden. C, The median time required for tumor volume doubling is illustrated with lower and upper limits in parentheses. Statistical significance (P<0.05) is indicated vs control*, RT†, AZD1775+RT‡, and olaparib+RT¥. C, The Kaplan-Meier plot illustrates the proportion of tumors doubled in volume within the full 90 day monitoring period.
Discussion
In this study, we have found that combined inhibition of Wee1 and PARP produces significantly more radiosensitization in pancreatic cancer cells than inhibition of either Wee1 or PARP alone. Mechanistically, we show that Wee1 inhibition by AZD1775 both inhibits HRR as well as abrogates a prolonged G2 checkpoint induced by the combination of olaparib with radiation. These findings suggest that Wee1 and PARP inhibitors interact to affect both HRR and the G2 checkpoint leading to dramatic radiosensitization. Consistent with this hypothesis, we observed little to no radiosensitization of pancreatic tumors by PARP inhibition alone, but substantial radiosensitization resulting in some durable, complete tumor regressions when PARP inhibition was combined with Wee1 inhibition. Taken together, our data suggest that the combination of PARP inhibitors with targeted agents which impair HRR and/or abrogate the G2 checkpoint may induce synthetic lethality in combination with radiation.
Radiosensitization by PARP inhibitors such as olaparib is thought to be mediated by inhibition of base excision repair, resulting in delayed repair of SSBs that upon collision with progressing replication forks are converted to 1-ended DSBs which in turn require homologous recombination for repair. Supporting this model, PARP inhibition in combination with radiation produces greater growth inhibition in BRCA2-deficient than in BRCA2-proficient breast cancers(21). In addition, radiosensitization by PARP inhibition is enhanced in the context of a variety of DSB repair deficiencies including those involving Artemis, Ligase IV, and ATM (20). Consistent with these reports, we found that olaparib produced little to no radiosensitization in pancreatic cancer cells and tumors with intact DSB repair. However, radiosensitization was significantly increased when olaparib was combined with the Wee1 inhibitor AZD1775, which is likely attributable to the HRR inhibition and G2 checkpoint abrogation induced by AZD1775. Although HRR inhibition represents a plausible mechanism of interaction between PARP and Wee1 inhibitors, G2 checkpoint abrogation may also be a key mechanism as repair of the 1-ended DSBs induced by PARP inhibition likely proceeds with slower kinetics that would require an intact G2 checkpoint to accommodate the DSB repair process. The current model suggests that for tumors without innate DSB repair defects, maximal radiosensitization by PARP inhibitors will require the addition of a second agent to inhibit the DNA damage response.
In addition to effects on the G2 checkpoint and HRR, Wee1 and PARP may also interact to regulate replication stress. Wee1 inhibition or depletion has been shown to cause replication stress resulting from deregulated Cdk1 activity, increased origin firing, subsequent nucleotide depletion, and slowed replication fork progression (11, 12). In addition, Wee1 negatively regulates the Mus81-Eme1 endonuclease. Thus, another consequence of Wee1 inhibition by AZD1775 would be Mus81-Eme1-mediated DNA DSBs at sites of aberrant replication structures (41). These studies are consistent with our finding that AZD1775 causes an early increase in the levels of pRPA (S4/8) and γH2AX, markers of replication stress and DNA DSBs, respectively (Figs. 2 and 4). PARP inhibition may also be detrimental to cells encountering replication stress, since PARP functions at sites of stalled replication forks to mediate replication restart and to protect stalled forks from Mre11-mediated degradation (42, 43). Taken together these findings suggest that PARP activity may mitigate the effects of replication stress induced by Wee1 inhibition. Future studies are required to determine whether replication stress contributes to radiosensitization following Wee1 and PARP inhibition.
Although this is the first study to investigate the combination of Wee1 and PARP inhibitors, significant interest lies in finding combinations of drugs that cooperate to induce synthetic lethality selectively in cancer cells. Others have investigated the combination of Chk1 and Wee1 inhibitors and demonstrated synergistic effects on DNA damage, apoptosis, and cytotoxicity in tumor cells (17, 18). In addition, we observed dramatic radiosensitization of tumor cells in response to combined Chk1 and Wee1 inhibition. This radiosensitization, however, was accompanied by substantial cytotoxicity (5). Thus, although combined inhibition of Chk1 and Wee1 represents a highly active therapy in tumor cells, the normal tissue toxicity and mechanisms of tumor cell selectivity have not yet been established, as TP53 mutation does not appear to confer selectivity (17). Furthermore, the combination of Chk1 and Wee1-targeted agents appears to require dose de-escalation to approximately half of the maximum tolerated doses for each of the single agents (44). In contrast, our group has previously shown that combined inhibition of Chk1 and PARP results in preferential radiosensitization of TP53-mutant cancer cells, with little to no cytotoxicity or radiosensitization of normal cells (23). This selectivity is likely related to the ability of cells with intact p53 to arrest in G1 and repair DNA damage through non-homologous end joining negating the effects of both G2 checkpoint abrogation (45) and HRR inhibition (46), respectively. Based on the similarities between Chk1 and Wee1, both of which when inhibited selectively sensitize TP53-mutant tumor cells (14, 15); it is likely that TP53 mutation is also a mechanism of tumor cell selectivity for the combination of Wee1 and PARP inhibitors. The tumor cell selectivity of Wee1 and PARP inhibitors is suggested in the present study by the tolerability of the combination of agents at the doses previously established for the single agents (8, 47). In future studies, it will be important to further evaluate the mechanisms of tumor cell selectivity and the therapeutic indices of these novel agent combinations.
Chemoradiation is the standard therapy for the majority of inoperable, locally advanced cancers. The addition of molecularly targeted agents to chemoradiation represents a promising strategy for improving chemoradiation efficacy and is the focus of our current clinical trial combining AZD1775 with gemcitabine-radiation in locally advanced pancreatic cancer patients. In general, however, chemoradiation therapy is associated with considerable toxicity. This limitation motivates the investigation of novel combinations of targeted agents which may be less toxic than chemotherapy, in lieu of chemotherapy in chemoradiation regimens (5). Whether novel combinations of targeted agents could ultimately replace cytotoxic chemotherapy in chemoradiation regimens requires extensive investigation. Initial clinical studies in breast cancer however, have shown combinations of targeted agents can approach the efficacy of chemotherapy (48). In addition, the findings presented in this study demonstrate tumor radiosensitization by combined Wee1 and PARP inhibition that is greater than that achieved in our previous studies by chemoradiation only but comparable to that achieved by combining a single targeted agent with chemoradiation in similar pancreatic tumor models (6, 7). While it is an intriguing concept that combinations of targeted agents with radiation might someday alleviate the need for conventional chemotherapy in chemoradiation regimens, the development of these therapies will require careful preclinical investigation in future studies.
Supplementary Material
Statement of Translational Relevance.
Although chemoradiation is superior to chemotherapy alone in locally advanced pancreatic cancers, more effective therapies are urgently needed. Combinations of targeted agents, which have the potential to be efficacious and less toxic than standard chemotherapy, with radiation are an exciting area of investigation. In this study, our findings that combined inhibition of Wee1 and PARP produces greater radiosensitization than either agent alone and, in some cases, complete regression of pancreatic tumors illustrate the therapeutic benefit of this combination of agents. Since Wee1 inhibition is currently under clinical investigation with gemcitabine-radiation in locally advanced pancreatic cancers, this study represents the preclinical foundation for the next generation of clinical trials, using combinations of targeted agents with radiation or chemoradiation for locally advanced pancreatic cancers.
Acknowledgments
Grant support: This work was funded by NIH Grants R01CA163895, P50CA130810, Cancer Center Core Grant P30 CA046592, and an Alfred B. Taubman Scholarship.
Abbreviations
- DSB
double strand break
- HRR
homologous recombination repair
- PARP
poly (ADP-ribose) polymerase
- PAR
poly (ADP-ribose)
- RER
radiation enhancement ratio
- RT
radiation
Footnotes
Disclosure of potential conflicts of interest: None
References
- 1.Loehrer PJ, Sr, Feng Y, Cardenes H, Wagner L, Brell JM, Cella D, et al. Gemcitabine alone versus gemcitabine plus radiotherapy in patients with locally advanced pancreatic cancer: an eastern cooperative oncology group trial. J Clin Oncol. 2011;29:4105–12. doi: 10.1200/JCO.2011.34.8904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ben-Josef E, Schipper M, Francis IR, Hadley S, Ten-Haken R, Lawrence T, et al. A Phase I/II Trial of Intensity Modulated Radiation (IMRT) Dose Escalation With Concurrent Fixed-dose Rate Gemcitabine (FDR-G) in Patients With Unresectable Pancreatic Cancer. Int J Radiat Oncol Biol Phys. 2012 doi: 10.1016/j.ijrobp.2012.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crane CH, Varadhachary GR, Yordy JS, Staerkel GA, Javle MM, Safran H, et al. Phase II trial of cetuximab, gemcitabine, and oxaliplatin followed by chemoradiation with cetuximab for locally advanced (T4) pancreatic adenocarcinoma: correlation of Smad4 (Dpc4) immunostaining with pattern of disease progression. J Clin Oncol. 2011;29:3037–43. doi: 10.1200/JCO.2010.33.8038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iacobuzio-Donahue CA, Fu B, Yachida S, Luo M, Abe H, Henderson CM, et al. DPC4 gene status of the primary carcinoma correlates with patterns of failure in patients with pancreatic cancer. J Clin Oncol. 2009;27:1806–13. doi: 10.1200/JCO.2008.17.7188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgan MA, Parsels LA, Maybaum J, Lawrence TS. Improving the efficacy of chemoradiation with targeted agents. Cancer Discov. 2014;4:280–91. doi: 10.1158/2159-8290.CD-13-0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morgan MA, Parsels LA, Zhao L, Parsels JD, Davis MA, Hassan MC, et al. Mechanism of radiosensitization by the Chk1/2 inhibitor AZD7762 involves abrogation of the G2 checkpoint and inhibition of homologous recombinational DNA repair. Cancer Res. 2010;70:4972–81. doi: 10.1158/0008-5472.CAN-09-3573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Engelke CG, Parsels LA, Qian Y, Zhang Q, Karnak D, Robertson JR, et al. Sensitization of Pancreatic Cancer to Chemoradiation by the Chk1 Inhibitor MK8776. Clin Cancer Res. 2013;19:4412–21. doi: 10.1158/1078-0432.CCR-12-3748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bridges KA, Hirai H, Buser CA, Brooks C, Liu H, Buchholz TA, et al. MK-1775, a novel Wee1 kinase inhibitor, radiosensitizes p53-defective human tumor cells. Clin Cancer Res. 2011;17:5638–48. doi: 10.1158/1078-0432.CCR-11-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarcar B, Kahali S, Prabhu AH, Shumway SD, Xu Y, Demuth T, et al. Targeting radiation-induced G(2) checkpoint activation with the Wee-1 inhibitor MK-1775 in glioblastoma cell lines. Mol Cancer Ther. 2011;10:2405–14. doi: 10.1158/1535-7163.MCT-11-0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krajewska M, Heijink AM, Bisselink YJ, Seinstra RI, Sillje HH, de Vries EG, et al. Forced activation of Cdk1 via wee1 inhibition impairs homologous recombination. Oncogene. 2012 doi: 10.1038/onc.2012.296. [DOI] [PubMed] [Google Scholar]
- 11.Beck H, Nahse-Kumpf V, Larsen MS, O’Hanlon KA, Patzke S, Holmberg C, et al. Cyclin-dependent kinase suppression by WEE1 kinase protects the genome through control of replication initiation and nucleotide consumption. Mol Cell Biol. 2012;32:4226–36. doi: 10.1128/MCB.00412-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dominguez-Kelly R, Martin Y, Koundrioukoff S, Tanenbaum ME, Smits VA, Medema RH, et al. Wee1 controls genomic stability during replication by regulating the Mus81-Eme1 endonuclease. J Cell Biol. 2011;194:567–79. doi: 10.1083/jcb.201101047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zabludoff SD, Deng C, Grondine MR, Sheehy AM, Ashwell S, Caleb BL, et al. AZD7762, a novel checkpoint kinase inhibitor, drives checkpoint abrogation and potentiates DNA-targeted therapies. Mol Cancer Ther. 2008;7:2955–66. doi: 10.1158/1535-7163.MCT-08-0492. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell JB, Choudhuri R, Fabre K, Sowers AL, Citrin D, Zabludoff SD, et al. In vitro and in vivo radiation sensitization of human tumor cells by a novel checkpoint kinase inhibitor, AZD7762. Clin Cancer Res. 2010;16:2076–84. doi: 10.1158/1078-0432.CCR-09-3277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rajeshkumar NV, De Oliveira E, Ottenhof N, Watters J, Brooks D, Demuth T, et al. MK-1775, a potent Wee1 inhibitor, synergizes with gemcitabine to achieve tumor regressions, selectively in p53-deficient pancreatic cancer xenografts. Clin Cancer Res. 2011;17:2799–806. doi: 10.1158/1078-0432.CCR-10-2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rozenblum E, Schutte M, Goggins M, Hahn SA, Panzer S, Zahurak M, et al. Tumor-suppressive pathways in pancreatic carcinoma. Cancer Res. 1997;57:1731–4. [PubMed] [Google Scholar]
- 17.Guertin AD, Martin MM, Roberts B, Hurd M, Qu X, Miselis NR, et al. Unique functions of CHK1 and WEE1 underlie synergistic anti-tumor activity upon pharmacologic inhibition. Cancer Cell Int. 2012;12:45. doi: 10.1186/1475-2867-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carrassa L, Chila R, Lupi M, Ricci F, Celenza C, Mazzoletti M, et al. Combined inhibition of Chk1 and Wee1: in vitro synergistic effect translates to tumor growth inhibition in vivo. Cell Cycle. 2012;11:2507–17. doi: 10.4161/cc.20899. [DOI] [PubMed] [Google Scholar]
- 19.Rouleau M, Patel A, Hendzel MJ, Kaufmann SH, Poirier GG. PARP inhibition: PARP1 and beyond. Nat Rev Cancer. 2010;10:293–301. doi: 10.1038/nrc2812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Loser DA, Shibata A, Shibata AK, Woodbine LJ, Jeggo PA, Chalmers AJ. Sensitization to radiation and alkylating agents by inhibitors of poly(ADP-ribose) polymerase is enhanced in cells deficient in DNA double-strand break repair. Mol Cancer Ther. 2010;9:1775–87. doi: 10.1158/1535-7163.MCT-09-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evers B, Drost R, Schut E, de Bruin M, van der Burg E, Derksen PW, et al. Selective inhibition of BRCA2-deficient mammary tumor cell growth by AZD2281 and cisplatin. Clin Cancer Res. 2008;14:3916–25. doi: 10.1158/1078-0432.CCR-07-4953. [DOI] [PubMed] [Google Scholar]
- 22.Dungey FA, Caldecott KW, Chalmers AJ. Enhanced radiosensitization of human glioma cells by combining inhibition of poly(ADP-ribose) polymerase with inhibition of heat shock protein 90. Mol Cancer Ther. 2009;8:2243–54. doi: 10.1158/1535-7163.MCT-09-0201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vance S, Liu E, Zhao L, Parsels JD, Parsels LA, Brown JL, et al. Selective radiosensitization of p53 mutant pancreatic cancer cells by combined inhibition of Chk1 and PARP1. Cell Cycle. 2011;10:4321–9. doi: 10.4161/cc.10.24.18661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Budke B, Logan HL, Kalin JH, Zelivianskaia AS, Cameron McGuire W, Miller LL, et al. RI-1: a chemical inhibitor of RAD51 that disrupts homologous recombination in human cells. Nucleic Acids Res. 2012;40:7347–57. doi: 10.1093/nar/gks353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wei D, Parsels LA, Karnak D, Davis MA, Parsels JD, Marsh AC, et al. Inhibition of Protein Phosphatase 2A Radiosensitizes Pancreatic Cancers by Modulating CDC25C/CDK1 and Homologous Recombination Repair. Clin Cancer Res. 2013;19:4422–32. doi: 10.1158/1078-0432.CCR-13-0788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li L, Wang H, Yang ES, Arteaga CL, Xia F. Erlotinib attenuates homologous recombinational repair of chromosomal breaks in human breast cancer cells. Cancer Res. 2008;68:9141–6. doi: 10.1158/0008-5472.CAN-08-1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morgan MA, Parsels LA, Kollar LE, Normolle DP, Maybaum J, Lawrence TS. The combination of epidermal growth factor receptor inhibitors with gemcitabine and radiation in pancreatic cancer. Clin Cancer Res. 2008;14:5142–9. doi: 10.1158/1078-0432.CCR-07-4072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lawrence TS. Ouabain sensitizes tumor cells but not normal cells to radiation. Int J Radiat Oncol Biol Phys. 1988;15:953–8. doi: 10.1016/0360-3016(88)90132-0. [DOI] [PubMed] [Google Scholar]
- 29.Fertil B, Dertinger H, Courdi A, Malaise EP. Mean inactivation dose: a useful concept for intercomparison of human cell survival curves. Radiat Res. 1984;99:73–84. [PubMed] [Google Scholar]
- 30.Huang X, Halicka HD, Darzynkiewicz Z. Detection of histone H2AX phosphorylation on Ser-139 as an indicator of DNA damage (DNA double-strand breaks) Curr Protoc Cytom. 2004;Chapter 7(Unit 7):27. doi: 10.1002/0471142956.cy0727s30. [DOI] [PubMed] [Google Scholar]
- 31.Morgan MA, Parsels LA, Parsels JD, Lawrence TS, Maybaum J. The relationship of premature mitosis to cytotoxicity in response to checkpoint abrogation and antimetabolite treatment. Cell Cycle. 2006;5:1983–8. doi: 10.4161/cc.5.17.3184. [DOI] [PubMed] [Google Scholar]
- 32.Pierce AJ, Johnson RD, Thompson LH, Jasin M. XRCC3 promotes homology-directed repair of DNA damage in mammalian cells. Genes Dev. 1999;13:2633–8. doi: 10.1101/gad.13.20.2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parsels LA, Morgan MA, Tanska DM, Parsels JD, Palmer BD, Booth RJ, et al. Gemcitabine sensitization by checkpoint kinase 1 inhibition correlates with inhibition of a Rad51 DNA damage response in pancreatic cancer cells. Mol Cancer Ther. 2009;8:45–54. doi: 10.1158/1535-7163.MCT-08-0662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao L, Morgan MA, Parsels LA, Maybaum J, Lawrence TS, Normolle D. Bayesian hierarchical changepoint methods in modeling the tumor growth profiles in xenograft experiments. Clin Cancer Res. 2011;17:1057–64. doi: 10.1158/1078-0432.CCR-10-1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shi W, Feng Z, Zhang J, Gonzalez-Suarez I, Vanderwaal RP, Wu X, et al. The role of RPA2 phosphorylation in homologous recombination in response to replication arrest. Carcinogenesis. 2010;31:994–1002. doi: 10.1093/carcin/bgq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yajima H, Fujisawa H, Nakajima NI, Hirakawa H, Jeggo PA, Okayasu R, et al. The complexity of DNA double strand breaks is a critical factor enhancing end-resection. DNA Repair (Amst) 2013;12:936–46. doi: 10.1016/j.dnarep.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 37.Carrassa L, Damia G. Unleashing Chk1 in cancer therapy. Cell Cycle. 2011;10:2121–8. doi: 10.4161/cc.10.13.16398. [DOI] [PubMed] [Google Scholar]
- 38.Redon CE, Nakamura AJ, Zhang YW, Ji JJ, Bonner WM, Kinders RJ, et al. Histone {gamma}H2AX and Poly(ADP-Ribose) as Clinical Pharmacodynamic Biomarkers. Clin Cancer Res. 2010;16:4532–42. doi: 10.1158/1078-0432.CCR-10-0523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang Z, Wang F, Tang T, Guo C. The role of PARP1 in the DNA damage response and its application in tumor therapy. Front Med. 2012;6:156–64. doi: 10.1007/s11684-012-0197-3. [DOI] [PubMed] [Google Scholar]
- 40.Krejci L, Altmannova V, Spirek M, Zhao X. Homologous recombination and its regulation. Nucleic Acids Res. 2012;40:5795–818. doi: 10.1093/nar/gks270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martin Y, Dominguez-Kelly R, Freire R. Novel insights into maintaining genomic integrity: Wee1 regulating Mus81/Eme1. Cell Div. 2011;6:21. doi: 10.1186/1747-1028-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bryant HE, Petermann E, Schultz N, Jemth AS, Loseva O, Issaeva N, et al. PARP is activated at stalled forks to mediate Mre11-dependent replication restart and recombination. EMBO J. 2009;28:2601–15. doi: 10.1038/emboj.2009.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ying S, Hamdy FC, Helleday T. Mre11-dependent degradation of stalled DNA replication forks is prevented by BRCA2 and PARP1. Cancer Res. 2012;72:2814–21. doi: 10.1158/0008-5472.CAN-11-3417. [DOI] [PubMed] [Google Scholar]
- 44.Russell M, Levin K, Rader J, Belcastro L, Li Y, Martinez D, et al. Combination Therapy Targeting the Chk1 and Wee1 Kinases Demonstrates Therapeutic Efficacy in Neuroblastoma. Cancer Res. 2012 doi: 10.1158/0008-5472.CAN-12-2669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ma CX, Janetka JW, Piwnica-Worms H. Death by releasing the breaks: CHK1 inhibitors as cancer therapeutics. Trends Mol Med. 2010 doi: 10.1016/j.molmed.2010.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rieckmann T, Kriegs M, Nitsch L, Hoffer K, Rohaly G, Kocher S, et al. p53 modulates homologous recombination at I-SceI-induced double-strand breaks through cell-cycle regulation. Oncogene. 2013;32:968–75. doi: 10.1038/onc.2012.123. [DOI] [PubMed] [Google Scholar]
- 47.Senra JM, Telfer BA, Cherry KE, McCrudden CM, Hirst DG, O’Connor MJ, et al. Inhibition of PARP-1 by olaparib (AZD2281) increases the radiosensitivity of a lung tumor xenograft. Mol Cancer Ther. 2011;10:1949–58. doi: 10.1158/1535-7163.MCT-11-0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Prat A, Baselga J. Dual Human Epidermal Growth Factor Receptor 2 (HER2) Blockade and Hormonal Therapy for the Treatment of Primary HER2-Positive Breast Cancer: One More Step Toward Chemotherapy-Free Therapy. J Clin Oncol. 2013;31:1703–6. doi: 10.1200/JCO.2012.48.4998. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.