Abstract
Objective
The present study examined trajectories of individual DSM-IV symptoms of ADHD and ODD across the preschool years in children with ADHD. It also evaluated whether preschool symptoms vary in their ability to discriminate children who later meet criteria for ADHD from typically developing children.
Method
ADHD and ODD symptoms were assessed annually in 75 ethnically diverse children (46 boys) who presented with behavior problems at age 3 and met criteria for ADHD 3 years later, and in 51 typically developing children (26 boys).
Results
Children with ADHD generally exhibited stable levels of hyperactivity/impulsivity, but increases in several symptoms of inattention. Most ADHD symptoms showed at least fair utility in discriminating children with and without ADHD; however, three symptoms of inattention (carelessness, losing things, and forgetfulness) and one symptom of hyperactivity/impulsivity (blurting out answers) had relatively poor utility. These symptoms demonstrated only somewhat greater utility at age 4, but by the age of 5 were better able to classify children. Children with ADHD exhibited increases in several ODD symptoms, including symptoms related to negative affect.
Conclusions
Although most symptoms of hyperactivity/impulsivity appear to extend well down to age 3, more developmentally appropriate symptoms of inattention may be required to develop more sensitive assessments for 3- and 4-year-old children.
Keywords: inattention, hyperactivity, ODD, trajectories, preschool
Longitudinal Changes in Individual Symptoms Across the Preschool Years in Children with ADHD
Attention-deficit/hyperactivity disorder (ADHD) is characterized by difficulties with inattention and hyperactivity/impulsivity (American Psychiatric Association, 2013), and there is growing evidence that this disorder often emerges during the preschool years. ADHD is estimated to occur in 2 to 8% of preschoolers (Egger, Condo, & Angold, 2006; Lavigne, LeBailly, Hopkins, Gouze, & Binns, 2009; Wichstrøm, et al., 2012) and demonstrates high continuity from preschool to school-age (Harvey, Youngwirth, Thakar, & Errazuriz, 2009; Bufferd, Dougherty, Carlson, Rose, & Klein, 2012; Lahey et al., 2004; Riddle et al., 2013). Guidelines for diagnosing ADHD have therefore recently been expanded by the American Academy of Pediatrics to include children as young as 4 years of age (Subcommittee on Attention-Deficit/Hyperactivity Disorder, Steering Committee on Quality Improvement and Management, 2011). However, it is not yet clear whether extending the existing Diagnostic and Statistical Manual of Mental Disorders (DSM) ADHD nosology to preschoolers is optimal in providing developmentally sensitive diagnoses. This uncertainty has resulted in calls for research to inform our understanding of the clinical phenomenology of ADHD in early childhood (Chacko, Wakschlag, Hill, Danis, & Espy, 2009), including explorations of how symptoms develop over time in preschoolers (Purpura, Wilson, & Lonigan, 2010). Two important steps in this process are to prospectively examine trajectories of individual symptoms of ADHD during the preschool years in children with ADHD and to identify which symptoms best discriminate these children from typically developing children. These lines of research may provide insight into the patterns of symptom emergence during the early development of ADHD, thus informing developmentally sensitive early assessments.
Longitudinal Studies of Preschool Behavior Problems
Although some studies have prospectively examined trajectories of inattention and hyperactivity/impulsivity averaging across symptoms (Galéra et al., 2011; Lahey, Pelham, Loney, Lee, & Willcutt, 2005; LeBlanc et al., 2008; Romano, Tremblay, Farhat, & Cote, 2006; Shaw, Lacourse, & Nagin, 2005), few studies have tracked individual DSM ADHD symptoms over time in preschoolers (Willoughby et al., 2012). However, a larger body of longitudinal research on behavior problems provides an important context for the current investigation. A number of longitudinal studies on behavior problems have been conducted with both community (e.g., Bufferd et al., 2012) and clinical preschool samples (e.g., Lahey et al., 2005; Lavigne et al., 1998; Riddle et al., 2013), and generally indicate that children with early behavior problems are likely to continue to have problems over time. Although groundbreaking, many of these studies focused on externalizing behavior broadly or assessed children only once during the preschool years. Assessing ADHD symptomatology more specifically across multiple time points during the preschool years can advance our understanding of the early course of these disorders.
A few studies (Galéra et al., 2011; Lahey et al., 2005; LeBlanc et al., 2008; Romano et al., 2006; Shaw et al., 2005; Willoughby et al., 2012) have examined trajectories of hyperactivity and inattention during the preschool years in community samples. Findings have generally suggested that children in community samples who initially demonstrated the highest levels of hyperactivity showed flat trajectories from preschool to school age, followed by a slight decline beginning at about 6 or 8 years old (Leblanc et al., 2008; Shaw et al., 2005; Galéra et al., 2011), although Romano et al. (2006) reported that children with the highest levels of hyperactivity demonstrated slight increases from age 2 to 7. Galéra et al. (2011) also found that children with initially high levels of inattention showed steady increases in inattention from age 1.5 to age 6 before leveling off from age 6 to age 8. Finally, Lahey et al. (2005) reported that 4- to 6-year-old children with ADHD demonstrated declining levels of hyperactivity/impulsivity and inattention over an 8 year period. Research is needed to build on these studies to better understand how inattention and hyperactivity/impulsivity change in general across development in children with ADHD, as well as how change varies across specific symptoms within each of these domains.
Implications of Typical Developmental Changes for Symptom Trajectories
A number of developmental changes that occur during the preschool years may determine when different symptoms emerge and influence the overall pattern of change in symptoms. Behavior problems should generally decrease across the preschool years as children’s frontal lobes develop, resulting in increased inhibitory control (Bell, Wolfe, & Adkins, 2007). Greater inhibition is likely to result in greater motor and attentional control, and therefore fewer symptoms of ADHD. In addition, as children’s verbal and cognitive skills develop, symptom expression may shift from being more non-verbally based (e.g., seems “on the go”) to more verbally based (e.g., talkativeness), and children may engage in more complex and indirect forms of symptom expression. Finally, contextual changes may contribute to symptom expression. As children move through the preschool years, they may engage in more complex activities, spend more time with peers and in school settings, and expectations for their behavior may shift. Thus, for example, one might expect increases in symptoms that are more readily observed in school contexts (e.g., leaves seat, blurts out answers). These rapid shifts in cognitive development and contexts may result not only in changes in symptom expression, but also in the psychometric properties of symptoms across the preschool years. Indeed, cross-study comparisons of the psychometric properties of ADHD symptoms using item-response theory in preschoolers (Purpura et al., 2010), elementary school-aged children (Gomez, 2008), and adolescents (Gomez, 2012) suggest that although most symptoms of ADHD show similar properties, there may be some important shifts in the relative utility of certain symptoms across development.
Evidence Suggesting That Symptom Expression May Change Across Development
Although individual symptoms of ADHD exhibit high levels of internal consistency (Burns, Walsh, Owen, & Snell, 1997) and similar predictive power in older children (Frick, Lahey, Applegate, & Kerdyck, 1994), a handful of studies suggest that individual symptoms might show different patterns of change and discriminability across the preschool years; however, no published studies have directly examined this possibility. First, retrospective reports suggest that individual DSM symptoms of ADHD vary in their age of onset (Loeber, Green, Lahey, Christ, & Frick, 1992). If symptoms emerge at different points in development, one would expect symptom trajectories and their ability to identify ADHD to vary accordingly. For example, a symptom that typically emerges in the early preschool years may remain high in frequency across the preschool years, resulting in a high, but relatively flat trajectory, whereas a symptom that does not emerge until the later preschool years would exhibit lower frequency during the early preschool years and higher frequency during the later preschool years, resulting in an upward trajectory. Similarly, because symptoms that occur infrequently in children with ADHD may be less likely to demonstrate high accuracy in classifying children with ADHD, predictive power may vary depending on when symptoms emerge, with symptoms having less potential for predictive power when the are less frequent among children with ADHD. Second, cross-sectional research suggests that ADHD symptoms vary in their utility for discriminating children with and without ADHD in older children (Frick et al., 1994) and in preschoolers (Purpura et al., 2010). Third, there is evidence that DSM symptoms of ADHD, particularly inattentive symptoms, vary in their frequency among preschoolers (Byrne, Bawden, Beattie, & DeWolfe, 2000; Willoughby et al., 2012). It is therefore possible that rises in broad measures of inattention that have been documented (Galéra et al., 2011) may be driven by specific symptoms that are less common during the preschool years and emerge slightly later in development. Longitudinal studies are needed to test this possibility.
Symptom Trajectories of Comorbid Oppositional Defiant Disorder
Approximately half of children with ADHD also meet criteria for oppositional defiant disorder (ODD; Waschbusch, 2002) and research suggests that this comorbidity may develop during the preschool years (Bufferd et al., 2012; Harvey, Metcalfe, Herbert, & Fanton, 2011; Lavigne et al., 2009). Examining early trajectories of individual ODD symptoms in children with ADHD may provide important insights into the early development of comorbidity between these disorders. This may be particularly important because children with comorbid ADHD and ODD have poorer prognoses than children with ADHD alone (Waschbusch, 2002).
Although studies have prospectively examined trajectories of conduct problems (e.g., NICHD Early Child Care Research Network [ECCRN], 2004; Shaw, Gilliom, Ingoldsby, & Nagin, 2003; Shaw et al., 2005), no published studies have tracked individual DSM ODD symptoms over time in preschoolers. However, it is likely that normal developmental changes also impact trajectories of ODD symptoms. For example, increasing inhibitory control is likely to result in improved emotion regulation (Barkley, 1997), and therefore improvement in ODD symptoms involving negative affect. Symptoms of ODD may also improve over time as children develop a greater capacity for moral reasoning and empathy (Kerig & Wenar, 2006). Children’s changing verbal and cognitive skills also result in shifts in how they express their growing sense of autonomy during the preschool years (Kuczynski & Kochanska, 1990). Non-verbal and less complex ODD symptoms (e.g., temper tantrums) may be more evident in younger children, whereas verbal (e.g., arguing) or more complex (e.g., spiteful) symptoms may emerge later in development. Research is needed to explore these possibilities and gain a better understanding of how individual ODD symptoms unfold over time in children with ADHD.
The Present Study
The primary goal of the present study was to examine trajectories of individual hyperactivity/impulsivity and inattention symptoms across the preschool years among children who later meet criteria for ADHD1. Of interest was whether symptoms vary in frequency during the preschool years and how this variability changes over time. This study also sought to examine the predictive power of individual symptoms of ADHD during the preschool years to discriminate children who later meet criteria for ADHD from typically developing children. A secondary goal of the study was to examine trajectories of individual ODD symptoms among children with ADHD. The following questions were examined:
How do average levels of inattention and hyperactivity/impulsivity change across the preschool years in children who later meet criteria for ADHD?
Although the primary goal of this study was to examine individual variation in symptoms, this study also sought to replicate and extend previous studies that have examined changes in average ADHD symptoms in children with ADHD. Studies that have examined multiple time points across the preschool years suggest that children with high levels of hyperactivity/impulsivity follow a flat trajectory (Galéra et al., 2011; Leblanc et al., 2008; Shaw et al., 2005), with declines beginning in the early elementary years. In contrast, previous research suggests that inattention is likely to increase across the preschool years (Galéra et al., 2011). Thus it was predicted that hyperactivity/impulsivity would remain stable, whereas inattention would increase across the preschool years in children who later meet criteria for ADHD.
How do individual ADHD symptoms vary in their trajectories across the preschool years in children who later meet criteria for ADHD?
Theory and research point to three sets of potential factors that may determine variation in symptom trajectories. First, changes in children’s cognitive and language abilities suggest that verbally based and cognitively complex symptoms (e.g., difficulty organizing tasks, talks excessively) may show different trajectories than non-verbally based, less complex symptoms (e.g., easily distracted, being “on the go”). Nonverbal symptoms may be evident by an early age and show a flat, high trajectory path; however, more complex verbally based symptoms may be infrequent early in development, but steadily increase across the preschool years as children's skills developed. Second, changing contexts and expectations as children develop could mean that symptoms that may be more evident in school settings and symptoms that are less accepted in older children (e.g., blurts out answers, leaves seat, loses things) may show different trajectories than symptoms that may be less context and age dependent (e.g., doesn’t listen, difficulty playing quietly). Finally, although ADHD symptoms have generally been found to be internally consistent, dimensions within this domain (e.g., hyperactivity vs. impulsivity vs. inattention) may show different patterns of change over time. Teasing apart the influence of these three sets of factors is difficult, in part because they may exert opposing forces that counteract one another, and in part because some symptoms may be more easily classified along these dimensions than others. However, these factors do provide a basis for predicting that individual symptoms should demonstrate different patterns of change. The direction of those differences remains an open question; exploring these differences represents a first step towards understanding symptom changes across the preschool years.
Do individual symptoms of ADHD during the preschool years vary in their ability to discriminate children who later meet criteria for ADHD from typically developing children?
In an earlier set of analyses with the present sample, we (Harvey et al., 2009) found that average preschool symptoms of ADHD demonstrated good power in predicting future ADHD. However, of interest in the present study was whether some symptoms discriminate children with and without ADHD better than others. As described previously, the developmental and contextual changes across the preschool years are likely to result in different symptoms emerging at different points in development. It is therefore expected that predictive power may vary across symptoms and across time points; however, the specific ways in which symptoms might differ remains an open question.
How do individual ODD symptoms vary in their trajectories across the preschool years in children who later meet criteria for ADHD?
To better understand the early emergence of ODD symptoms in children with ADHD, this study also examined trajectories of ODD symptoms in children who later meet criteria for ADHD. Theory suggests that children with ADHD are likely to elicit negative reactions from their environment, which in turn may lead to the development of ODD (Barkley, 1990). These processes likely begin during the early preschool years when ADHD symptoms are thought to first emerge (e.g., Bufferd et al., 2012), and continue throughout the preschool years. It was therefore predicted that ODD symptoms would generally increase among children with ADHD across the preschool years, reflecting the cumulative effects of the negative environmental reactions to children's ADHD symptoms. However, the same developmental and contextual changes that might cause ADHD symptoms to emerge at different time points are also likely to result in trajectory variability across ODD symptoms. Thus, it was predicted that ODD symptoms would vary in their trajectories across the preschool years, but the precise nature of this variability remains an open question.
Method
Participants
Participants were 126 children (75 with ADHD and 51 without) and their mothers who were drawn from a larger sample of children who participated in a longitudinal study beginning at age 3. The larger sample consisted of two groups of children: (a) 199 children who were identified as having externalizing problems at age 3, and (b) 59 children who were identified as not having significant externalizing problems at age 3. Among children in the externalizing group, 168 completed diagnostic assessments at 3-year follow-up, 75 of whom met criteria for ADHD. Among children in the nonproblem group, 55 completed diagnostic assessments at 3-year follow-up, 51 of whom did not meet criteria for ADHD at follow-up. The 75 children with ADHD and 51 children without ADHD were the focus of the current study. Children from the larger sample who did not complete follow-up assessments (31 from the externalizing group and 4 from the nonproblem group), children from the nonproblem group who met criteria for ADHD (n = 4), and children from the externalizing group who did not meet criteria for ADHD (n = 93) were not included in the present study. Children were all 3 years old at the time of screening and were 37 to 50 months (M = 44.15, SD = 3.55) at the first home visit. The sample consisted of 55% European American children, 22% Latino children, 9.5% African American children, and 13.5% multiethnic children. The median family income at the first time point was $47,108. Most mothers (87%) were high school graduates and 29% of mothers also had bachelor’s degrees.
Procedure
All participants were recruited over a 3-year period (2000 to 2003) from 3-year-old children (n = 1752) whose parents completed a screening packet, which they received through the mail (via state birth records), pediatrician offices, child care centers, and community centers throughout western Massachusetts in the United States. The questionnaire packet contained an informed consent form; a Behavior Assessment System for Children-Parent Rating Scale (BASC-PRS; Reynolds & Kamphaus, 1992); and a questionnaire assessing for exclusion criteria, parental concern about externalizing symptoms, and demographic information. Criteria for all participants included no evidence of intellectual disability, deafness, blindness, language delay, cerebral palsy, epilepsy, autism, or psychosis. Criteria for the externalizing group were: (a) parent responded “yes” or “possibly” to the question, “Are you concerned about your child’s activity level, defiance, aggression, or impulse control?” and (b) BASC-PRS hyperactivity and/or aggression subscale T scores fell at or above 65 (1.5 SDs above the mean; approximately 92nd percentile)2. Criteria for the nonproblem control group were: (a) parent responded “no” to the question, “Are you concerned about your child’s activity level, defiance, aggression, or impulse control?” and (b) T scores on the BASC-PRS hyperactivity, aggression, attention problems, anxiety, and depression subscales fell at or below 60. Parents whose children met criteria for either the externalizing group or nonproblem group (who were matched on age, gender, and maternal education) were invited to participate in home visit assessments at age 3 (T1) and again at 1-year (T2; mean age = 56 months, SD = 3.7), 2-year (T3; mean age = 69 months, SD = 4.5), and 3-year (T4; mean age = 80 months, SD = 5.3) follow-up visits. Fifty-nine percent of externalizing problem children and 72% of non-problem children whom we sought to recruit participated. Families were paid for their participation. Written informed consent was obtained from all parents who participated and verbal assent was obtained from children. The study was conducted in compliance with the authors' Institutional Review Board.
Measures
Disruptive Behavior Rating Scale (DBRS)
Mothers completed the DBRS-Parent Version (Barkley & Murphy, 1998) at each time point. This 26-item scale includes items related to the 18 DSM-IV symptoms for ADHD and 8 DSM-IV symptoms for ODD. Mothers rated whether each symptom occurred not at all (0), sometimes (1), often (2), or very often (3) in the past 6 months. This scale has demonstrated good reliability and validity in preschoolers (Friedman-Weieneth, Doctoroff, Harvey, & Goldstein, 2009). Cronbach’s alphas for the ADHD sample ranged from .83 to .88 across time points for hyperactivity/impulsivity, .80 to .86 for inattention, and .87 to .88 for ODD items.
Diagnostic interview
At Times 1, 2, and 3, the ADHD section of the NIMH-Diagnostic Interview Schedule for Children-IV (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) were administered to mothers, with minor modification to school-related questions. Fathers also participated in the interviews for 56% of children at Time 1, 38% at Time 2, and 22% at Time 3 in this sample. Mothers’ responses were used in the rare case of open disagreement between mother and father. The presence or absence of each of the 18 ADHD symptoms at each time point was used in the present study to examine each symptom’s ability to discriminate children with and without ADHD. Kuder-Richardson 20 ranged from .82 to .86 across time points for hyperactivity/impulsivity items and .84 to .88 for inattention items.
T4 ADHD diagnoses
Clinicians who conducted the T4 home visits assigned diagnoses of ADHD and ODD based on the following measures collected at T4: DISC-IV (Shaffer et al., 2000), a psychosocial interview, and parent- and teacher-completed BASCs and DBRSs. All clinicians were clinical or school psychology graduate students who had taken graduate courses on child assessment and were trained by the first author to conduct these assessments. Clinicians did not review data collected at earlier time points in making diagnoses. Clinician-based DSM-IV diagnoses guided by structured interview and rating scale data were used as recommended by experts in the assessment of these disorders (Barkley, 1990) to maximize generalizability of the findings to clinical settings. In making diagnoses, clinicians examined symptom counts based on the DISC-IV and DBRS, elevations on BASC hyperactivity and aggression subscales (T scores at or above 65), and evidence of impairment based on the DISC-IV and psychosocial interview. Convergent evidence of developmentally deviant symptoms was necessary to make diagnoses (elevations on most, but not necessarily all, measures). To be consistent with previous longitudinal studies of preschool ADHD (Lahey et al., 2005), and because it may take some time before ADHD symptoms become fully evident at school for some young children, ADHD diagnoses were given if clinically significant symptoms were evident at home or at school. Children who displayed symptoms primarily at home did not differ significantly from children who displayed symptoms at home and school on any of the DBRS subscales at any of the time points, all ps > .05. A second clinician reviewed T4 materials and made independent diagnoses. Discrepancies were discussed and a consensus diagnosis was reached. Kappa was .78 for ADHD. Of the 168 externalizing problem children who completed T4, 36 met criteria for ADHD only, 39 for ADHD and ODD, and 22 for ODD only. Of the 75 children who met criteria for ADHD, 6 met criteria for ADHD predominantly inattentive type, 13 for ADHD predominantly hyperactive/impulsive type, and 56 for ADHD combined type. Of the 55 control children who completed T4 home visits, 51 did not met criteria for ADHD3. ADHD diagnoses were not made before T4, because at the time of data collection, there was not yet sufficient support for making ADHD diagnoses in preschool-aged children.
Data Analyses
DBRS frequency ratings of individual symptoms were used to assess ADHD and ODD symptom trajectories, because they provided continuous (0 to 3) data for each symptom, which is better suited than dichotomous data for estimating trajectories. In contrast, DISC-IV symptom endorsements were used to examine predictive power of symptoms, because dichotomous scores (presence or absence of each symptom) were more conducive to this set of analyses. The DBRS and DISC-IV items are quite similar to one another, although not identical. Using these two different measures allowed us to better match the type of analyses to the form of data, and provided converging evidence regarding the relative frequency of various symptoms.
HLM was used to estimate symptom trajectories. A Level 1 model was estimated for individual j’s repeated measures of DBRS scores across multiple time points (from 1 to i): DBRSij = β0j+ β1j(timeLINEARij)+ β2j(timeQUADij) + rij
HLM allows for missing data at Level 1, so all 75 children with ADHD were included. Time was centered at T1; time was coded as 0 at T1, 1 at T2, 2 at T3, and 3 at T4. If the quadratic term (time squared) was significant, then it was retained in the model for that symptom. These models yield an intercept (β0) which represents the average symptom score at T1, a slope (β1) which represents the average rate of change per year in the symptom score, and a quadratic term (β2) which represents the rate of change in the slope over time (curvature).
Classification analyses were conducted to evaluate the predictive power of ADHD DISC-IV symptoms at T1, T2, and T3 for discriminating children with and without ADHD at T4. Sensitivity, specificity, positive predictive power, negative predictive power, overall predictive power, and relative improvement over chance (RIOC, which takes into account chance and base rates; Copas & Loeber, 1990) were calculated to evaluate each symptom’s power to discriminate children with and without ADHD. DISC-IV symptom frequencies were available for all 126 children at T1, for 74 children with ADHD and 50 children without ADHD at T2, and for 61 children with ADHD and 46 children without ADHD at T3. Because there was a higher rate of missing data at T3, ANOVAs were conducted to compare children with and without complete data at T3 on T1 and T4 DISC-IV hyperactivity/impulsivity and inattention symptom counts. No significant differences were found in either group, with ps ranging from .19 to .72 for children without ADHD and from .42 to .90 for children with ADHD.
Results
Descriptive Statistics
Children with ADHD did not differ significantly from children without ADHD on age, F (1, 124) = 1.36, p = .25, or sex, X2(1) = 1.33, p = .25. Mothers of children with ADHD had significantly fewer years of education (M = 12.89, SD = 2.88) than mothers of children without ADHD (M = 13.94, SD = 2.25), F (1, 124) = 4.76, p = .03. Table 1 presents means and standard deviations for DBRS symptoms at each time point.
Table 1.
Means and Standard Deviations of DBRS Symptoms Across Time
| Symptom |
Time 1 M (SD) N = 75 |
Time 2 M (SD) N = 74 |
Time 3 M (SD) N = 69 |
Time 4 M (SD) N = 74 |
|---|---|---|---|---|
| Inattention | ||||
| 1. Fails to pay close attention to details/careless mistakes | 1.17 (0.76) | 1.26 (0.81) | 1.43 (0.76) | 1.47 (0.80) |
| 2. Difficulty sustaining attention | 1.31 (0.92) | 1.26 (0.86) | 1.33 (0.83) | 1.61 (0.90) |
| 3. Doesn’t listen when spoken to directly | 1.65 (0.81) | 1.65 (0.90) | 1.59 (0.83) | 1.66 (0.82) |
| 4. Doesn’t follow through on instructions | 1.65 (0.81) | 1.61 (0.90) | 1.49 (0.89) | 1.62 (0.81) |
| 5. Difficulty organizing tasks | 1.17 (0.91) | 1.14 (0.91) | 1.28 (0.95) | 1.26 (0.85) |
| 6. Avoids, dislikes activities that require sustained effort | 1.13 (1.10) | 1.23 (1.05) | 1.20 (0.88) | 1.30 (0.96) |
| 7. Loses things necessary for tasks or activities | 1.21 (0.89) | 1.34 (0.91) | 1.33 (0.82) | 1.41 (0.91) |
| 8. Easily distracted | 1.85 (0.88) | 1.95 (0.98) | 1.93 (0.93) | 2.15 (0.87) |
| 9. Forgetful in daily activities | 0.95 (0.91) | 1.04 (0.91) | 1.20 (0.98) | 1.39 (0.98) |
| Hyperactivity/impulsivity | ||||
| 1. Fidgets with hands or feet or squirms in seat | 1.81 (0.93) | 1.95 (0.98) | 2.10 (0.88) | 2.18 (0.88) |
| 2. Leaves seat | 2.01 (0.91) | 1.77 (1.03) | 1.84 (0.87) | 1.73 (1.02) |
| 3. Seems restless | 1.59 (0.89) | 1.46 (0.91) | 1.42 (0.91) | 1.62 (0.99) |
| 4. Difficulty engaging in leisure activities quietly | 1.36 (0.97) | 1.12 (0.96) | 1.25 (0.98) | 1.23 (0.93) |
| 5. Seems “on the go” or “driven by a motor” | 2.08 (1.02) | 2.04 (0.93) | 1.94 (1.04) | 1.97 (1.01) |
| 6. Talks excessively | 1.88 (1.04) | 2.01 (1.01) | 1.94 (0.97) | 1.99 (0.93) |
| 7. Blurts out answers | 1.00 (0.92) | 1.15 (0.98) | 1.35 (0.95) | 1.50 (0.95) |
| 8. Has difficulty awaiting turn | 1.93 (0.98) | 1.96 (0.87) | 1.91 (0.89) | 1.93 (0.94) |
| 9. Interrupts or intrudes on others | 2.07 (0.92) | 2.03 (0.81) | 2.07 (0.83) | 2.07 (0.85) |
| ODD | ||||
| 1. Loses temper | 1.89 (0.97) | 1.97 (0.74) | 1.77 (0.91) | 1.84 (0.86) |
| 2. Argues with adults | 1.85 (0.98) | 1.99 (0.90) | 1.84 (0.96) | 1.91 (0.97) |
| 3. Actively defies or refuses to comply with adults’ requests or rules | 1.84 (0.89) | 1.70 (0.95) | 1.68 (1.09) | 1.55 (1.00) |
| 4. Deliberately annoys people | 1.13 (0.96) | 1.28 (0.96) | 1.29 (0.99) | 1.50 (0.93) |
| 5. Blames others for his/her mistakes or misbehavior | 1.23 (1.09) | 1.61 (1.00) | 1.65 (1.11) | 1.51 (0.93) |
| 6. Touchy or easily annoyed by others | 1.15 (0.97) | 1.42 (0.94) | 1.51 (0.99) | 1.62 (0.98) |
| 7. Angry or resentful | 0.88 (0.89) | 1.01 (0.85) | 1.09 (0.94) | 1.14 (0.96) |
| 8. Spiteful or vindictive | 0.57 (0.86) | 0.69 (0.81) | 0.64 (0.82) | 0.72 (0.84) |
Trajectories of Average Levels of Inattention and Hyperactivity/Impulsivity in Children Who Later Meet Criteria for ADHD
Trajectory parameters for average inattention and hyperactivity/impulsivity are shown in Table 2. Intercepts represent average symptom levels at Time 1, and slopes provide a measure of average linear change over time. Averaging across symptoms, children demonstrated significant increases in inattention over time, but showed flat trajectories of hyperactivity/impulsivity.
Table 2.
Symptom Trajectories for DBRS Inattention, Hyperactivity/Impulsivity, and ODD Symptoms
| Symptom | Intercept B0(SE) |
Slope B1(SE) |
Quadratic B2(SE) |
|---|---|---|---|
| Inattention | 1.34 (0.06)*** | 0.07 (0.02)* | |
| 1. Fails to pay close attention to details/careless mistakes | 1.17 (0.08)*** | 0.11 (0.04)* | |
| 2. Difficulty sustaining attention | 1.31 (0.11)*** | −0.16 (0.14) | 0.09 (0.04)* |
| 3. Doesn’t listen when spoken to directly | 1.64 (0.08)*** | −0.00 (0.04) | |
| 4. Doesn’t follow through on instructions | 1.62 (0.09)*** | −0.01 (0.04) | |
| 5. Difficulty organizing tasks | 1.15 (0.10)*** | 0.04 (0.04) | |
| 6. Avoids, dislikes activities that require sustained effort | 1.14 (0.12)*** | 0.05 (0.05) | |
| 7. Loses things necessary for tasks or activities | 1.23 (0.10)*** | 0.06 (0.05) | |
| 8. Easily distracted | 1.84 (0.09)*** | 0.10 (0.04)* | |
| 9. Forgetful in daily activities | 0.92 (0.10)*** | 0.15 (0.04)** | |
| Hyperactivity/Impulsivity | 1.73 (0.07)*** | 0.02 (0.03) | |
| 1. Fidgets with hands or feet or squirms in seat | 1.82 (0.10)*** | 0.12 (0.05)* | |
| 2. Leaves seat | 1.95 (0.11)*** | −0.07 (0.05) | |
| 3. Seems restless | 1.60 (0.10)*** | −0.26 (0.12)* | 0.09 (0.04)* |
| 4. Difficulty engaging in leisure activities quietly | 1.27 (0.10)*** | −0.02 (0.04) | |
| 5. Seems “on the go” or “driven by a motor” | 2.07 (0.11)*** | −0.04 (0.04) | |
| 6. Talks excessively | 1.92 (0.11)*** | 0.03 (0.04) | |
| 7. Blurts out answers | 0.99 (0.11) | 0.18 (0.05)** | |
| 8. Has difficulty awaiting turn | 1.94 (0.10)*** | 0.00 (0.04) | |
| 9. Interrupts or intrudes on others | 2.05 (0.09)*** | 0.01 (0.05) | |
| ODD | 1.36 (0.08)*** | 0.05 (0.03) | |
| 1. Loses temper | 1.92 (0.10)*** | −0.03 (0.05) | |
| 2. Argues with adults | 1.90 (0.11)*** | 0.01 (0.05) | |
| 3. Actively defies or refuses to comply with adults’ requests or rules | 1.82 (0.10)*** | −0.08 (0.04)* | |
| 4. Deliberately annoys people | 1.13 (0.11)*** | 0.11 (0.04)* | |
| 5. Blames others for his/her mistakes or misbehavior | 1.23 (0.12)*** | 0.52 (0.16)** | −0.14 (0.05)** |
| 6. Touchy or easily annoyed by others | 1.20 (0.11)*** | 0.16 (0.05)** | |
| 7. Angry or resentful | 0.90 (0.09)*** | 0.08 (0.05)† | |
| 8. Spiteful or vindictive | 0.60 (0.09)*** | 0.04 (0.04) |
Note: Symptoms were rated from 0 (not at all) to 3 (very often).
p< .10,
p< .05,
p< .01,
p< .001
Trajectories of Individual Symptoms of Inattention and Hyperactivity/Impulsivity in Children Who Later Meet Criteria for ADHD
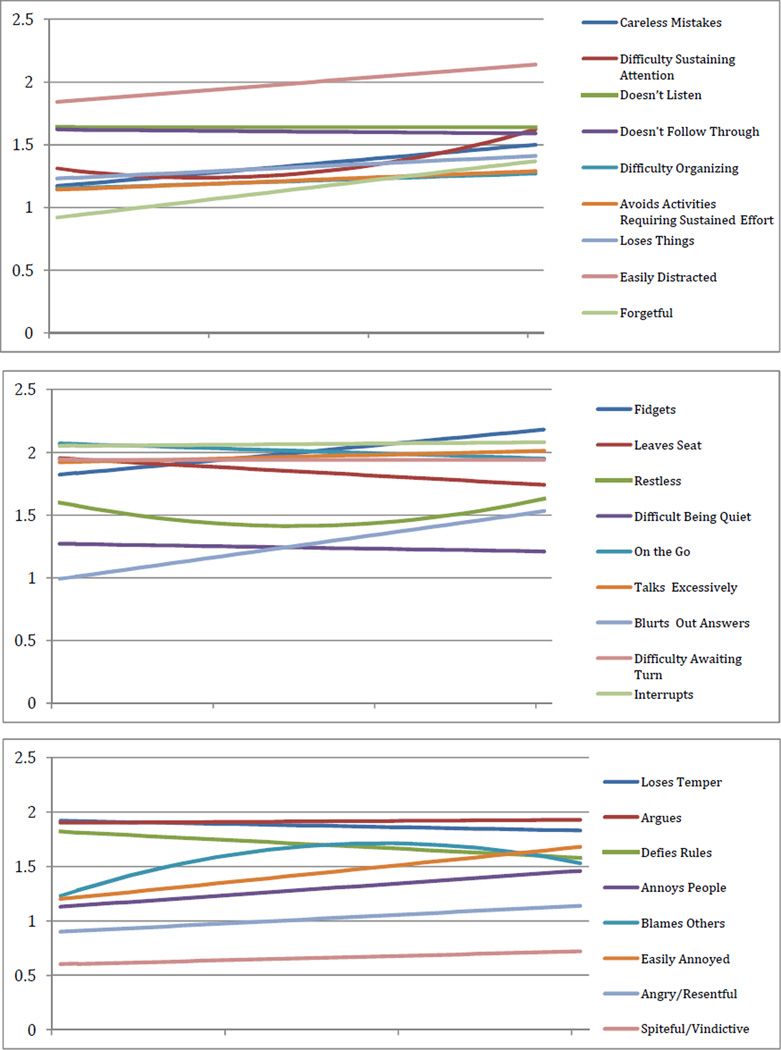
Individual symptom trajectories are presented in Table 2 and Figure 1. With respect to inattention, children with ADHD began with relatively low levels of difficulty organizing tasks, avoiding activities requiring sustained effort, losing things, paying attention to details/making careless mistakes, and being forgetful. These symptoms showed some increase over time, but only the latter two demonstrated significant increases. Children with ADHD also began with modest difficulty in sustaining attention, which initially decreased, but ultimately increased over time. In contrast, not listening and having difficulty following through began at high levels and remained high over time, and being easily distracted also began at high levels and increased even further over time.
Figure 1.
Symptom trajectories for children with ADHD
Most of the nine hyperactive/impulsive symptoms demonstrated flat trajectories for children with ADHD, with important exceptions. Fidgeting and blurting out answers significantly increased over time, although fidgeting began at a higher frequency than blurting out answers. Restlessness showed significant curvature, with an initial decrease followed by a comparable increase. It is important to note that the wording of this symptom on the DBRS corresponds to only part of the description in the DSM-IV/V and omits mention of running or climbing. Leaving one’s seat, being “on the go,” talking excessively, having difficulty waiting one’s turn, and interrupting all began at high levels and remained stable over time. Difficulty engaging in leisure activities quietly began at a modest level and remained stable over time.
Predictive Power of ADHD Symptoms in Discriminating Children Who Later Meet Criteria for ADHD from Typically Developing Children
Tables 3 and 4 present the predictive power statistics of symptom at T1, T2, and T3 for distinguishing between children with and without ADHD at T4. We considered predictive power above .8 as high, .7 to .8 as good, .6 to .7 as fair, and less than .6 as poor (Grodzinsky & Barkley, 1999). All 18 symptoms significantly discriminated between children with and without ADHD, as measured by the odds ratios, and positive predictive power was fairly consistently strong, suggesting that a high proportion of children exhibiting each symptom later met criteria for ADHD. However, symptoms varied considerably in their ability to classify children.
Table 3.
Predictive Powerof DISC-IV Inattentive Symptoms to Discriminate Children With and Without ADHD at T4
| T1 | T2 | T3 | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Sens | Spec | PPP | NPP | OPP | RIOC | OR | Sens | Spec | PPP | NPP | OPP | RIOC | OR | Sens | Spec | PPP | NPP | OPP | RIOC | OR |
| 1. Fails to pay close attention to details/careless mistakes | .29 | .98 | .96 | .49 | .57 | .14 | 20.75*** | .39 | .98 | .97 | .52 | .63 | .20 | 31.58*** | .46 | 1.00 | 1.00 | .58 | .69 | .27 | -- |
| 2. Difficulty sustaining attention | .47 | .98 | .97 | .56 | .67 | .25 | 43.75*** | .58 | .90 | .90 | .59 | .71 | .32 | 12.48*** | .62 | .98 | .97 | .66 | .78 | .41 | 74.35*** |
| 3. Doesn’t listen | .72 | .80 | .84 | .66 | .75 | .43 | 10.54*** | .77 | .74 | .81 | .69 | .76 | .47 | 9.54*** | .74 | .72 | .78 | .68 | .73 | .43 | 7.36*** |
| 4. Doesn’t follow through | .85 | .69 | .80 | .76 | .79 | .60 | 12.73*** | .86 | .72 | .82 | .78 | .81 | .64 | 16.46*** | .80 | .72 | .79 | .74 | .77 | .54 | 10.68*** |
| 5. Difficulty organizing tasks | .37 | .88 | .82 | .49 | .58 | .14 | 4.47** | .53 | .94 | .93 | .57 | .69 | .28 | 17.46*** | .62 | .83 | .83 | .63 | .71 | .34 | 8.05*** |
| 6. Avoids, dislikes activities requiring sustained effort | .59 | .92 | .92 | .60 | .72 | .33 | 16.68*** | .65 | .88 | .89 | .63 | .74 | .38 | 13.54*** | .61 | .98 | .97 | .65 | .77 | .39 | 69.38*** |
| 7. Loses things | .40 | .90 | .86 | .51 | .60 | .17 | 6.13** | .53 | .82 | .81 | .54 | .65 | .23 | 5.08*** | .59 | .89 | .88 | .63 | .72 | .34 | 12.10*** |
| 8. Easily distracted | .80 | .84 | .88 | .74 | .82 | .57 | 21.50*** | .72 | .82 | .85 | .66 | .76 | .43 | 11.50*** | .75 | .85 | .87 | .72 | .79 | .51 | 17.09*** |
| 9. Forgetful | .29 | .94 | .88 | .48 | .56 | .12 | 6.64** | .42 | .86 | .82 | .50 | .60 | .16 | 4.43** | .51 | .96 | .94 | .60 | .70 | .29 | 23.25*** |
Note. T1 = Time 1; T2 = Time 2; T3 = Time 3; T4 = Time 4; Sens = Sensitivity; Spec = Specificity; PPP = Positive Predictive Power; NPP = Negative Predictive Power; OPP = Overall Predictive Power; RIOC = Relative Improvement Over Chance; OR = odds ratio. Significance of OR was calculated using Fischer’s Exact Test.
p< .01;
p< .001
Table 4.
Predictive Power of DISC-IV Hyperactive/Impulsive Symptoms to Discriminate Children With and Without ADHD at T4
| T1 | T2 | T3 | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Sens | Spec | PPP | NPP | OPP | RIOC | OR | Sens | Spec | PPP | NPP | OPP | RIOC | OR | Sens | Spec | PPP | NPP | OPP | RIOC | OR |
| 1. Fidgets | .60 | .92 | .92 | .61 | .73 | .35 | 17.63*** | .73 | .90 | .92 | .69 | .80 | .48 | 24.30*** | .74 | .85 | .87 | .71 | .79 | .49 | 15.67*** |
| 2. Leaves seat | .80 | .76 | .83 | .72 | .79 | .53 | 13.00*** | .78 | .72 | .81 | .69 | .76 | .48 | 9.32*** | .75 | .85 | .87 | .72 | .79 | .51 | 17.09*** |
| 3. Runs/climbs/restless | .97 | .67 | .81 | .94 | .85 | .91 | 73.00*** | .95 | .62 | .79 | .89 | .81 | .81 | 28.55*** | .93 | .66 | .78 | .89 | .81 | .80 | 27.61*** |
| 4. Difficulty engaging in leisure activities quietly | .52 | .96 | .95 | .58 | .70 | .29 | 26.54*** | .47 | .98 | .97 | .56 | .68 | .26 | 43.97*** | .51 | .93 | .91 | .59 | .69 | .28 | 14.81*** |
| 5. Seems “on the go” or “driven by a motor” | .69 | .82 | .85 | .65 | .75 | .41 | 10.55*** | .77 | .80 | .85 | .70 | .78 | .50 | 13.41*** | .69 | .87 | .88 | .68 | .77 | .44 | 14.74*** |
| 6. Talks excessively | .64 | .55 | .68 | .51 | .60 | .18 | 2.16* | .69 | .58 | .71 | .56 | .65 | .26 | 3.06** | .64 | .67 | .72 | .58 | .65 | .27 | 3.66** |
| 7. Blurts out answers | .27 | .98 | .95 | .48 | .56 | .12 | 18.18*** | .46 | .84 | .81 | .51 | .61 | .18 | 4.46** | .62 | .85 | .84 | .63 | .72 | .35 | 9.44*** |
| 8. Has difficulty awaiting turn | .77 | .78 | .84 | .70 | .78 | .50 | 12.41*** | .74 | .86 | .89 | .69 | .79 | .49 | 17.78*** | .80 | .87 | .89 | .77 | .83 | .60 | 27.22*** |
| 9. Interrupts or intrudes on others | .95 | .45 | .72 | .85 | .75 | .75 | 14.58*** | .95 | .44 | .71 | .85 | .74 | .74 | 13.75*** | .97 | .40 | .67 | .90 | .72 | .83 | 19.33*** |
Note. T1 = Time 1; T2 = Time 2; T3 = Time 3; T4 = Time 4; Sens = Sensitivity; Spec = Specificity; PPP = Positive Predictive Power; NPP = Negative Predictive Power; OPP = Overall Predictive Power; RIOC = Relative Improvement Over Chance; OR = odds ratio. Significance of OR was calculated using Fischer’s Exact Test.
p< .01;
p< .01;
p< .001
A number of symptoms of inattention demonstrated high specificity (proportion of typically developing children who did not display the symptom), but low sensitivity (proportion of children with later ADHD who displayed the symptom) at age 3, including making careless mistakes, difficulty organizing tasks, losing things, and being forgetful. These symptoms showed only modest ability to distinguish children with and without ADHD, with poor overall predictive power (see Table 3). Although making careless mistakes was the least common symptom, with lowest sensitivity, it had some utility because it rarely occurred in children without ADHD (2%), and therefore had high specificity. Moreover, the utility of this symptom increased over time, as sensitivity increased without a drop in specificity. Thus, although this symptom was uncommon, when it did occur it was highly indicative of ADHD. Similarly, among children with later ADHD, having difficulty sustaining attention was reported in just 47% of children at age 3; however, this symptom showed high specificity, so it also demonstrated high utility, which only increased over time. Being easily distracted, not listening, and not following through were the most common symptoms in children with ADHD across the preschool years, and therefore showed high sensitivity. These symptoms demonstrated good to high predictive power that remained fairly stable over time.
Symptoms of hyperactivity/impulsivity were also somewhat variable in their ability to distinguish children with and without ADHD. Leaving one’s seat, climbing/running/restlessness, having difficulty waiting one’s turn, and interrupting were common across the preschool years in children with ADHD, with sensitivity ranging from .74 and .97 (Table 4). Although these symptoms also occurred in typically developing children, they were generally much less frequent than in children with ADHD and therefore showed good discriminability across the preschool years. Fidgeting, difficulty engaging in activities quietly, and being “on the go,” occurred with moderate frequency in children with ADHD across the preschool years, with sensitivity ranging from .47 to .77. These symptoms were much less common in typically developing children, resulting in generally good discriminability across time, with good overall predictive power and high positive predictive power (proportion of children who displayed the symptom who later met criteria for ADHD), but poor to fair negative predictive power (proportion of children who did not display the symptom who later did not meet criteria for ADHD). In contrast, talking excessively was also moderately common in children with ADHD, with sensitivity ranging from .64 to .69, but specificity was lower than other symptoms, because it was more common in typically developing children, resulting in only fair predictive power across time. Finally, blurting out answers demonstrated the lowest sensitivity at T1 (.27), but was also very uncommon in typically developing children (2%), and therefore showed high specificity. Thus, although this symptom was uncommon, when it did occur it was fairly highly indicative of ADHD, with very high positive predictive power (.95) and an odds ratio of over 18. However, because it occurred infrequently, it correctly classified only 56% of children at T1. By T3, however, blurting out answers was much more common in children with ADHD, resulting in greater sensitivity (.62) and correctly classifying 72% of children.
Trajectories of ODD Symptoms in Children Who Later Meet Criteria for ADHD
Trajectories for ODD symptoms are shown in Table 2 and Figure 1. Averaging across symptoms, children showed flat trajectories of ODD symptoms across the preschool years, but there was substantial variability across symptoms. Deliberately annoying people, being touchy/easily annoyed, and blaming others all began at relatively low levels and significantly increased over time, although the trajectory for blaming others was curvilinear, with an initially large increase that tapered off over time. An increase in being angry/resentful was also observed at a probability level that approached significance. In contrast, defiance began at a very high level but decreased significantly over time. Arguing and losing one’s temper began as the highest symptoms and remained high throughout the preschool years. Being spiteful/vindictive began at a low level and remained low over time.
Discussion
This study examined trajectories of DSM-IV symptoms of ADHD across the preschool years in children who later met criteria for ADHD, and evaluated the utility of individual symptoms for discriminating these children from typically developing children. This study also explored trajectories of individual ODD symptoms in children who later met criteria for ADHD, to better understand the early emergence of comorbid ODD in children with ADHD. Results suggested both commonalities and differences in individual symptom trajectories and ability to discriminate children with and without ADHD across the preschool years.
Trajectories of ADHD Symptoms
Inattention
Consistent with Galéra et al. (2011), children who later met criteria for ADHD demonstrated increases in average levels of inattention over time; however, there was substantial variability in symptom levels and trajectories. Carelessness, difficulty organizing tasks, avoiding activities requiring sustained effort, losing things, and being forgetful began at relatively low levels at age 3 in children who later met criteria for ADHD, and these symptoms were remarkably similar to those reported to be relatively infrequent in preschoolers with ADHD (Byrne et al., 2000) and in community samples (Egger et al., 2006; Willoughby et al., 2012). The present study extends Byrne and colleagues’ (2000) cross-sectional research and demonstrates that at least some of these less frequently endorsed symptoms increase across the preschool years in children with later ADHD, and “catch up” to most of the more frequently endorsed symptoms of inattention by school-age. Examination of the content of these items suggests that the observed pattern may be due to changing expectations related to school demands. In early elementary school, there are likely greater expectations regarding attention to detail/working carefully and remembering tasks than during the preschool years, which may account for the rising frequency of carelessness and forgetfulness in children with ADHD. In contrast, other inattentive symptoms appeared to be well in place at the age of 3, and showed flat trajectories over time. These included not listening and not following through on instructions. Interestingly, the most highly rated symptom at age 3, being easily distracted, increased significantly across time, suggesting that early distractibility emerges early and only deteriorates over time in children with ADHD.
Hyperactivity/Impulsivity
Consistent with previous studies that have assessed children at multiple time points across the preschool years (Galera et al., 2011; Leblanc et al., 2008; Shaw et al., 2005), children with ADHD showed flat trajectories of hyperactivity/impulsivity. However, previous research that has followed preschool children beyond age 6 (e.g., Lahey et al., 2005), suggests that although hyperactivity/impulsivity seems to remain flat across the preschool years, symptoms may begin to decline shortly thereafter. Most individual symptoms of hyperactivity/impulsivity began at high levels and were stable or increased over time. However, there were important exceptions. Consistent with Byrne et al. (2000), blurting out answers began at a relatively low level at age 3, but increased over time. Changes in blurting out answers are likely due to increases in structure from preschool to early elementary school. With a shift away from play toward didactic teaching, there are likely more opportunities for blurting out answers. Fidgeting/squirming in one’s seat began at a high level and increased even further over time. It is possible that this change represents a developmental change in behavioral control, as children shift from large motor hyperactivity to fine motor hyperactivity. Observed decreases in symptoms of gross motor activity (leaves seat, being “on the go”) were not significant, but the magnitude of the decline in these two symptoms together was comparable to the significant increase in fidgeting. Difficulty engaging in activities quietly remained relatively infrequent across the preschool years. This finding is consistent with evidence that difficulty playing quietly is also infrequent in older children in the U.S. (Frick et al., 1994), although inconsistent with Byrne et al. (2000), who reported high rates of endorsement of this symptom in preschoolers from Canada.
Predictive Power of ADHD Symptoms
Inattention
Inattentive symptoms varied considerably in their utility at age 3 to discriminate children with and without ADHD. Difficulty organizing tasks, losing things, and being forgetful were endorsed for approximately one-third of children with ADHD at age 3, and were able to correctly classify just over half of children. However, by age 5, these symptoms were more common in children with ADHD and correctly classified over 70% of children. Although carelessness also occurred in less than one-third of children with ADHD at age 3, the specificity of this symptom was high with between 0 and 2% of typically developing children displaying this symptom over time. Thus, although carelessness did not occur commonly, when it did occur, it was highly indicative of ADHD, and therefore of some utility. The remaining symptoms of inattention generally displayed good utility in distinguishing children with and without ADHD across the preschool years.
Hyperactivity/impulsivity
Compared to symptoms of inattention, symptoms of hyperactivity/impulsivity demonstrated somewhat higher sensitivity (i.e., were more frequently endorsed in children with ADHD), but also had somewhat lower specificity (i.e., they were also more common in typically developing children), so discriminability was only somewhat better. Across the preschool years climbing/running/restlessness showed the highest utility for discriminating children with and without ADHD; over 80% of children were correctly classified using this symptom alone. In contrast, talking excessively and blurting out answers had poor discriminability at age 3, classifying 60% and 55% of children, respectively. This finding is consistent with Purpura et al., (2010) who found that these two symptoms provided little utility in assessing hyperactivity in a community sample of preschoolers. The lower discriminative ability of these two symptoms may be due to the fact that they involve verbal behavior, whereas symptoms that showed high discriminative ability tended to involve motor behavior. Because language is still undergoing substantial development among young preschool children, verbally based hyperactivity items may have less utility. Interestingly, interrupt/intrudes can also involve verbal behavior, but nonetheless demonstrated good overall predictive power. However, it may be that younger preschoolers may exhibit this symptom in nonverbal ways. Research investigating the different ways in which individual symptoms are expressed across development would be useful in evaluating this possibility.
Trajectories of ODD Symptoms
Children with ADHD showed flat trajectories of ODD symptoms over time, but there was substantial variability across symptoms. Losing one’s temper and arguing with adults appeared early in development and remained high across the preschool years. Defiance was also common early in development, but improved over time for children who later met criteria for ADHD. This may reflect normal developmental changes in children’s expression of autonomy, as children shift from active defiance to more adaptive strategies of asserting their will (Kuczynski & Kochanska, 1990). Increases in blaming others and annoying people may indicate children’s greater capacity for engaging in more complex social behaviors that allow for more proactive forms of verbal aggression to be added to their repertoire of reactive behaviors (e.g., arguing).
Perhaps one of the most important findings in this study was that children with ADHD exhibited increases in symptoms related to negative affect (being touchy/easily annoyed and to a lesser extent being angry/resentful). These symptoms began at moderate levels and increased over time in children who later met criteria for ADHD. Temper tantrums, which also involve negative affect, did not show the same increase over time. However, because temper tantrums are characteristic of the early preschool years (Bhatia, Dhar, Singhal, & Nigam, 1990; Wakschlag et al., 2012), they typically decrease with age (Loeber, Lahey, & Thomas, 1991; Wakschlag et al., 2012). The finding that they did not decrease in this sample together with the observed increases in anger and annoyance suggests that preschool children with ADHD may be failing to acquire emotion regulation skills at the same rate as typically developing preschoolers.
Limitations
These findings should be interpreted in the context of several limitations of this study. First, like most previous studies of ADHD and ODD trajectories, symptoms were assessed primarily using maternal report. Although maternal reports of preschoolers’ behavior are typically central to the assessment process, further research is needed to examine trajectories of teacher-reported, father-reported, and observed behavior. Second, individual symptoms were measured with single items, which are likely less reliable than variables measured with multiple items. Third, although the sample was ethnically diverse, the sample size was not sufficiently large to evaluate whether ethnicity moderated findings of the present study. Fourth, ADHD diagnoses were available only at Time 4. It would have been useful to know how many children classified as ADHD in this study met criteria at earlier time points as well. Because all children with ADHD were identified as having behavior problems at age 3, it is likely that most would have met criteria, but their early diagnostic status remains unknown. Similarly, because only children with ADHD who had significant behavior problems at age 3 were included in this study, these findings may not generalize to children who do not develop significant symptoms of ADHD until later in development. Fifth, only a small number of children met criteria for ADHD predominantly inattentive type, so results may not generalize to that population. Finally, there is some evidence that the optimal frequency threshold for determining the presence of a symptom may vary across symptoms (Purpura et al., 2010); for example, for some items, occasional presence of the symptom might be indicative of a disorder, whereas for other items, more frequent occurrence of a symptom would be needed. The diagnostic interview used in the present study indicated only whether symptoms occurred often or not, so we were not able to address this issue.
Implications for Research and Practice
Despite these limitations, the results of this study add to mounting evidence (Egger et al., 2006; Lavigne et al., 2009; Wichstrøm, et al., 2012) that children with ADHD can show symptoms as early as age 3. Moreover, our finding that all 18 ADHD symptoms significantly discriminated children with and without ADHD throughout the preschool years provides some support for the validity of these symptoms. However, three symptoms of inattention (carelessness, losing things, and forgetfulness) and one symptom of hyperactivity/impulsivity (blurting out answers) had relatively lower utility at age 3, because they were relatively uncommon in children with ADHD. These symptoms became only somewhat more common at age 4, but by the age of 5 were better able to classify children. Although it is clear that ADHD symptoms are evident in young preschoolers, it may be necessary to replace some of the existing symptoms with poor utility with symptoms that better discriminate 3- and 4-year-old children with (or at risk for) ADHD from typically developing children. Although the current set of 18 symptoms may be adequate, they do not appear to be ideal for children under the age of 5. Finally, the finding that children with ADHD demonstrate an increase in a number of ODD symptoms during the preschool years, including symptoms of irritability and proactive verbal aggression, suggests that early identification and intervention for children with ADHD may be crucial in preventing the development of ODD. This highlights the importance of developing more sensitive methods of identifying young preschoolers who are at risk for developing ADHD.
Acknowledgments
This research was supported by a grant from the National Institutes of Health (MH60132) awarded to the first author.
Footnotes
An equally interesting question is how symptoms change following a preschool diagnosis of ADHD. Because we were interested in the emergence of symptoms as early as age 3, and ADHD diagnoses are infrequently made in children under 4 (3 year old children fall outside of the age range recommended by the American Academy of Pediatrics), our focus was on examining preschool symptom trajectories leading up to the diagnosis of ADHD.
We did not screen for Attention Problems because research suggested a later onset of ADHD Predominantly Inattentive Type. In fact, in an ancillary study, we attempted to also screen for children who only showed elevations on the Attention Problems scale and were only able to obtain a relatively small number of children.
We considered including the 4 control children who developed ADHD together with the 75 children from the externalizing group. However, because this small group of children was unlikely to influence the overall pattern of findings even if they showed very different symptom trajectories, we thought it better to focus on a more homogenous group of children so that it was clear which population the results would generalize to: children with ADHD whose symptoms begin to develop during the preschool years.
Contributor Information
Elizabeth A. Harvey, Department of Psychology, University of Massachusetts Amherst
Claudia I. Lugo-Candelas, Department of Psychology, University of Massachusetts Amherst
Rosanna P. Breaux, Department of Psychology, University of Massachusetts Amherst
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: Fifth edition. Washington, DC: Authors; 2013. [Google Scholar]
- Barkley RA. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. New York, NY: Guilford Press; 1990. [Google Scholar]
- Barkley RA. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR. Attention-deficit hyperactivity disorder: A clinical workbook. 2nd ed. New York, NY: Guilford Press; 1998. [Google Scholar]
- Bell MA, Wolfe CD, Adkins DR. Frontal lobe development during infancy and childhood: Contributions of brain electrical activity, temperament, and language to individual differences in working memory and inhibitory control. In: Coch D, Dawson G, Fischer KW, editors. Human behavior and the developing brain Typical development (2nd ed.): Typical development. New York, NY: Guilford Press; 2007. pp. 247–276. [Google Scholar]
- Bhatia MS, Dhar NK, Singhal PK, Nigam VR. Temper tantrums: Prevalence and etiology in a non-referral outpatient setting. Clinical Pediatrics. 1990;29:311–315. doi: 10.1177/000992289002900603. [DOI] [PubMed] [Google Scholar]
- Bufferd SJ, Dougherty LR, Carlson GA, Rose S, Klein DN. Psychiatric disorders in preschoolers: Continuity from ages 3 to 6. The American Journal of Psychiatry. 2012;169:1157–1164. doi: 10.1176/appi.ajp.2012.12020268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns GL, Walsh JA, Owen SM, Snell J. Internal validity of attention deficit hyperactivity disorder, oppositional defiant disorder, and overt conduct disorder symptoms in young children: Implications from teacher ratings for a dimensional approach to symptom validity. Journal of Clinical Child Psychology. 1997;26:266–275. doi: 10.1207/s15374424jccp2603_5. [DOI] [PubMed] [Google Scholar]
- Byrne JM, Bawden HN, Beattie TL, DeWolfe NA. Preschoolers classified as having attention-deficit hyperactivity disorder (ADHD): DSM-IV symptom endorsement pattern. Journal of Child Neurology. 2000;15:533–538. doi: 10.1177/088307380001500807. [DOI] [PubMed] [Google Scholar]
- Chacko A, Wakschlag L, Hill C, Danis B, Espy KA. Viewing preschool disruptive behavior disorders and attention-deficit/hyperactivity disorder through a developmental lens: What we know and what we need to know. Child and Adolescent Psychiatric Clinics of North America. 2009;18:627–643. doi: 10.1016/j.chc.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copas JB, Loeber R. Relative improvement over chance (RIOC) for 2 × 2 tables. British Journal of Mathematical and Statistical Psychology. 1990;43:293–307. [Google Scholar]
- Egger H, Kondo D, Angold A. The epidemiology and diagnostic issues in preschool attention-deficit/ hyperactivity disorder: A review. Infants & Young Children. 2006;19:109–122. [Google Scholar]
- Frick PJ, Lahey BB, Applegate B, Kerdyck L. DSM-IV field trials for the disruptive behavior disorders: Symptom utility estimates. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:529–539. doi: 10.1097/00004583-199405000-00011. [DOI] [PubMed] [Google Scholar]
- Friedman-Weieneth J, Doctoroff GL, Harvey EA, Goldstein LH. The Disruptive Behavior Rating Scale—Parent Version (DBRS-PV): Factor analytic structure and validity among young preschool children. Journal of Attention Disorders. 2009;13:42–55. doi: 10.1177/1087054708322991. [DOI] [PubMed] [Google Scholar]
- Galéra C, Côté SM, Bouvard MP, Pingault J, Melchior M, Michel G, Tremblay RE. Early risk factors for hyperactivity-impulsivity and inattention trajectories from age 17 months to 8 years. Archives of General Psychiatry. 2011;68:1267–1275. doi: 10.1001/archgenpsychiatry.2011.138. [DOI] [PubMed] [Google Scholar]
- Gomez R. Item response theory analyses of the parent and teacher ratings of the DSM-IV ADHD Rating Scale. Journal of Abnormal Child Psychology. 2008;36:865–885. doi: 10.1007/s10802-008-9218-8. [DOI] [PubMed] [Google Scholar]
- Gomez R. Item response theory analyses of adolescent self-ratings of the ADHD symptoms in the Disruptive Behavior Rating Scale. Personality and Individual Differences. 2012;53:963–968. [Google Scholar]
- Grodzinsky GM, Barkley RA. The predictive power of frontal lobe tests for the diagnosis of attention deficit hyperactivity disorder. Clinical Neuropsychologist. 1999;13:12–21. doi: 10.1076/clin.13.1.12.1983. [DOI] [PubMed] [Google Scholar]
- Harvey EA, Metcalfe LA, Herbert SD, Fanton JH. The role of family experiences and ADHD in the early development of oppositional defiant disorder. Journal of Consulting and Clinical Psychology. 2011;79:784–795. doi: 10.1037/a0025672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey EA, Youngwirth SD, Thakar DA, Errazuriz PA. Predicting attention-deficit/hyperactivity disorder and oppositional defiant disorder from preschool diagnostic assessments. Journal of Consulting and Clinical Psychology. 2009;77:349–354. doi: 10.1037/a0014638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kerig PK, Wenar C. Developmental Psychopathology. 5th edition. New York, NY: McGraw Hill; 2006. [Google Scholar]
- 22.Kuczynski L, Kochanska G. Development of children's noncompliance strategies from toddlerhood to age 5. Developmental Psychology. 1990;26:398–408. [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Kipp H, Ehrhardt A, Lee SS, Massetti G. Three-year predictive validity of DSM-IV attention deficit hyperactivity disorder in children diagnosed at 4–6 years of age. The American Journal of Psychiatry. 2004;161:2014–2020. doi: 10.1176/appi.ajp.161.11.2014. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Arend R, Rosenbaum D, Binns HJ, Christoffel KK, Gibbons RD. Psychiatric disorders with onset in the preschool years: II. Correlates and predictors of stable case status. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1255–1261. doi: 10.1097/00004583-199812000-00008. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, LeBailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child and Adolescent Psychology. 2009;38:315–328. doi: 10.1080/15374410902851382. [DOI] [PubMed] [Google Scholar]
- Leblanc N, Boivin M, Dionne G, Brendgen M, Vitaro F, Tremblay RE, Pérusse D. The development of hyperactive–impulsive behaviors during the preschool years: The predictive validity of parental assessments. Journal of Abnormal Child Psychology. 2008;36:977–987. doi: 10.1007/s10802-008-9227-7. [DOI] [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB, Christ MA, Frick PJ. Developmental sequences in the age of onset of disruptive child behaviors. Journal of Child and Family Studies. 1992;1:21–41. [Google Scholar]
- Loeber R, Lahey BB, Thomas C. Diagnostic conundrum of oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology. 1991;100:379–390. doi: 10.1037//0021-843x.100.3.379. [DOI] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. Trajectories of physical aggression from toddlerhood to middle childhood. Monographs of the Society for Research in Child Development. 2004;69(4):vii, 129. doi: 10.1111/j.0037-976x.2004.00312.x. [DOI] [PubMed] [Google Scholar]
- Purpura DJ, Wilson SB, Lonigan CJ. Attention-deficit/hyperactivity disorder symptoms in preschool children: Examining psychometric properties using item response theory. Psychological Assessment. 2010;22:546–558. doi: 10.1037/a0019581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW. Behavior Assessment System for Children manual. Circle Pines, MN: American Guidance Service; 1992. [Google Scholar]
- Riddle MA, Yershova K, Lazzaretto D, Paykina N, Yenokyan G, Greenhill L, Posner K. The Preschool Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS) 6-year follow-up. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:264e2–278e2. doi: 10.1016/j.jaac.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano E, Tremblay RE, Farhat A, Côté S. Development and prediction of hyperactive symptoms from 2 to 7 years in a population-based sample. Pediatrics. 2006;117:2101–2110. doi: 10.1542/peds.2005-0651. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Gilliom M, Ingoldsby EM, Nagin DS. Trajectories leading to school-age conduct problems. Developmental Psychology. 2003;39:189–200. doi: 10.1037//0012-1649.39.2.189. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Lacourse E, Nagin DS. Developmental trajectories of conduct problems and hyperactivity from ages 2 to 10. Journal of Child Psychology and Psychiatry. 2005;46:931–942. doi: 10.1111/j.1469-7610.2004.00390.x. [DOI] [PubMed] [Google Scholar]
- Subcommittee on Attention-Deficit/Hyperactivity Disorder, Steering Committee on Quality Improvement and Management. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Choi SW, Carter AS, Hullsiek H, Burns J, McCarthy K, Briggs-Gowan MJ. Defining the developmental parameters of temper loss in early childhood: Implications for developmental psychopathology. Journal of Child Psychology and Psychiatry. 2012;53:1099–1108. doi: 10.1111/j.1469-7610.2012.02595.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waschbusch DA. A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletin. 2002;128:118–150. doi: 10.1037/0033-2909.128.1.118. [DOI] [PubMed] [Google Scholar]
- Wichstrøm L, Berg-Nielsen T, Angold A, Egger H, Solheim E, Sveen T. Prevalence of psychiatric disorders in preschoolers. Journal of Child Psychology and Psychiatry. 2012;53:695–705. doi: 10.1111/j.1469-7610.2011.02514.x. [DOI] [PubMed] [Google Scholar]
- Willoughby MT, Pek J, Greenberg MT the Family Life Project Investigators. Parent-reported attention deficit/hyperactivity symptomatology in preschool-aged children: Factor structure, developmental change, and early risk factors. Journal of Abnormal Child Psychology. 2012;40:1301–1312. doi: 10.1007/s10802-012-9641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]