Abstract
Objective
To compare the rate and sensitivity to change of quantitative cartilage thickness change with MRI across specific radiographic strata of knee osteoarthritis (KOA) from central expert readings of the Osteoarthritis Initiative (OAI). Specifically, we explored whether Kellgren Lawrence grade (KLG) 2 knees with radiographic joint space narrowing (JSN) displayed greater cartilage loss than those without JSN, and whether knees with medial JSN grade2 had greater loss than those with grade1.
Methods
One-year femorotibial cartilage thickness change was obtained for 836 knees, 112 without, and 724 with definite radiographic KOA based on baseline site readings. The maximum subregional cartilage loss, and cartilage thickness change in the total femorotibial joint and medial compartment (MFTC) were analyzed across different radiographic strata (central vs. site readings).
Results
The maximum subregional rate of change was significantly greater in central_KLG2 knees with than in those without JSN (172±152 vs. 134±100µm; p=0.03). In contrast, the rate did not differ significantly between central_KLG1 knees with and without JSN. MFTC cartilage loss in central_medial_grade2 JSN knees was substantially and significantly greater than in grade1 knees (−70±159 vs. −31±126µm; p=0.02). For comparison, the loss in grade3 knees was −72±122µm.
Conclusions
In KLG2 knees, presence of radiographic JSN was associated with significantly and substantially greater rates of subregional cartilage loss. Differentiating knees with mild vs. moderate medial JSN, and definite radiographic OA knees with vs. without JSN is important in predicting structural progression of KOA, and for planning clinical trials testing the efficacy of disease modifying drugs (DMOADs).
Keywords: Knee Osteoarthritis, Cartilage, Magnetic Resonance Imaging, Radiography, Sensitivity to change
INTRODUCTION
The Osteoarthritis Initiative (OAI) is an ongoing multi-center study (http://www.oai.ucsf.edu) targeted at identifying sensitive (imaging) biomarkers for onset and progression of knee osteoarthritis (1). 4674 participants with all grades of radiographic knee osteoarthritis (RKOA) and 122 healthy participants without symptoms, signs and risk factors of RKOA were studied annually over 48 months and longer (1), using fixed flexion radiography (2) and magnetic resonance imaging (MRI) (1,3).
We previously reported quantitative cartilage thickness loss in a large subsample of the OAI and reported rates and sensitivity to change across different radiographic strata (i.e Kellgren Lawrence grades [KLG]) (4). This analysis relied on the radiographic readings from the four clinical OAI sites available then. Healthy reference and KLG2 knees displayed minimal cartilage thickness loss; KLG3 and 4 knees displayed significantly greater loss than KLG2 knees. Since, central readings from experts at Boston University have been made available (1), and it has been found that central radiographic grading may differ substantially from that at the clinical sites, because different thresholds exist between readers for scoring osteophytes and radiographic joint space narrowing (JSN) (5). The central readings used the traditional KLG classification (6) as well as Osteoarthritis Research Society International (OARSI) osteophyte and JSN scores (7) and applied the full spectrum of OARSI JSN grades 1–3 (7), whereas the site readings had collapsed grades 1–2 into a single grade.
The purpose of this report was therefore to compare the rate and sensitivity to change of quantitative cartilage thickness loss between specific RKOA strata of central OAI readings, and to list those side-to-side with previously published site-reading strata (4). Specifically, we tested whether knees classified centrally as KLG 2 (and 1) display greater cartilage loss with presence of JSN, and whether medial JSN grade2 knees display greater medial cartilage loss than JSN grade1 knees.
METHODS
MRI acquisition and analysis
The OAI (1), the subsample studied, its demographics, and the MRI acquisition and image analysis technology have been described previously (4). Fixed flexion radiographs were acquired using a Synaflexer frame (2), and 3T double oblique coronal FLASH MRIs (Online Fig. 1) according to the OAI protocol (http://www.oai.ucsf.edu/) (1,3). The longitudinal analysis of femorotibial cartilage thickness change in this subsample was funded by a consortium of industry partners, the OAI coordinating center, and an image analysis company (Chondrometrics GmbH). Segmentation of baseline and year-1 follow-up images (Online Fig. 1) was performed with blinding to time-point (4). The number of segmented slices of each cartilage plate was matched between time points, but no prospective or retrospective registration was performed. To minimize differences between readers, all segmentations were quality controlled by one expert (S.M.). The mean cartilage thickness (ThCtAB.Me) was computed in the medial and lateral tibia and weight-bearing femoral condyles (4) (Online Fig. 1), and in 16 femorotibial subregions (8), for which the test-retest errors (RMS SD) have been reported to range from 19µm to 84µm. Non-location dependent rates of subregional cartilage loss were determined using an ordered value (OV) approach (4,9). In each knee, subregional rates of change were ranked to determine OV1, i.e. the rate of cartilage thickness loss (in µm) in the subregion with the greatest loss (4,9). OV1 is a location-independent measure and has been associated similarly with medial or lateral JSN (10).
Online Figure 1. Knees from a OAI participants with different radiographic status: fixed flexion radiographs shown on the left, coronal MR images without segmentation shown in the middle; coronal MR images with segmentation of the femorotibial cartilages shown on the right.
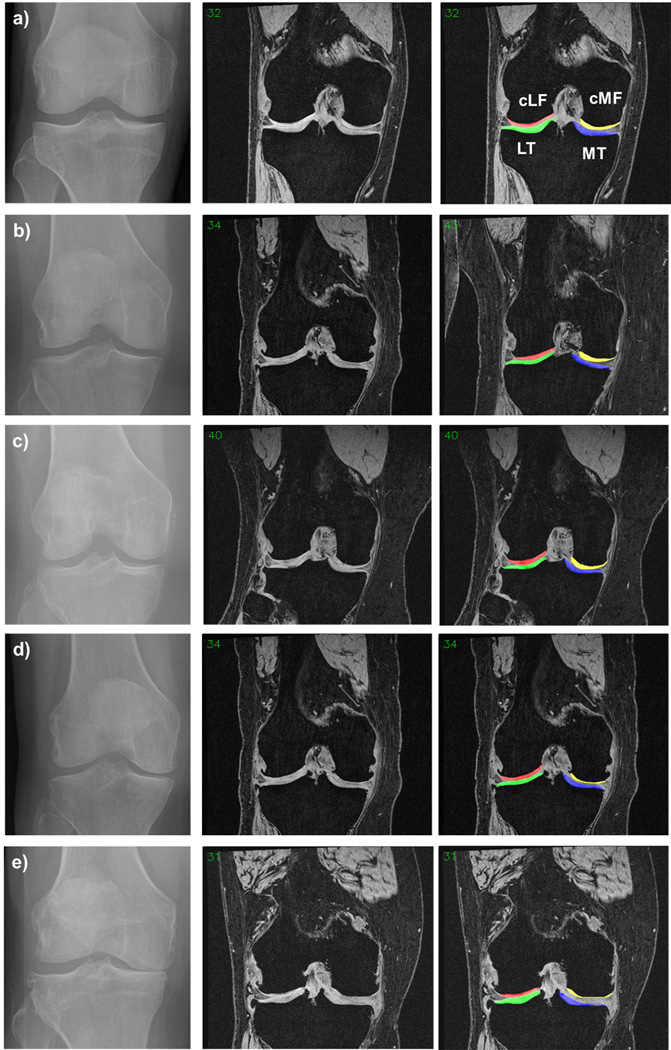
a) Healthy reference cohort knee
b) Central KLG1 knee
c) Central KLG2 knee without JSN
d) Central KLG2 knee with JSN
e) Central KLG3 knee
MT = medial tibial cartilage; cMF = medial weight-bearing femoral cartilage; LT = lateral tibial cartilage, cLF = lateral weight-bearing femoral cartilage
Radiographic strata
The previous study relied on baseline KLGs assigned by centrally trained and certified readers (one to three validated radiologists or rheumatologist) at each of four clinical OAI sites (4). KLGs were “calculated” from OARSI atlas osteophyte and JSN grades (7). Readers assessed each knee for presence/absence of definite marginal osteophytes (OARSI atlas grade 1–3, any medial and lateral, tibial and femoral osteophytes), and medial and lateral OAI JSN grades 1 (OARSI atlas grades1–2) or 2 (OARSI atlas grade3). The siteKLG was defined as: 0= osteophytes and JSN scores=0; 1= questionable osteophyte and OAI JSN grade0–1 (or grade0 osteophyte and OAI JSN grade1); 2= definite osteophyte and OAI JSN grade0 (or no/questionable osteophyte and OAI JSN grade2); 3= definite osteophyte and OAI JSN grade1; 4 = definite osteophyte and OAI JSN grade2, OAI JSN grade1 corresponding to “definite mild” and not to “possible or uncertain” JSN.
In the present analysis central radiographic readings (release 0.5) by three expert radiologists or rheumatologists at Boston University were used (https://oai.epi-ucsf.org/datarelease/SASDocs/kXR_SQ_BU_descrip.pdf). KLGs were assigned pertinent to the original description (6), independent of OARSI atlas osteophyte and JSN grades (Online Fig. 1) (7). Knees with presence of doubtful osteophytes and possible JSN were graded KLG1 (Fig. 1B), those with definite osteophytes and possible JSN KLG2 (Fig. 1C/D), and those with presence of moderate multiple osteophytes, definite JSN, subchondral sclerosis, and (possible) deformity of the bone KLG3 or 4 (Fig. 1E).
Study sample
Cartilage thickness measurements were available for 837 knees from 837 participants (one knee from each). The selection criteria were reported previously (4). One knee that had been assigned KLG3 by the site had no central reading performed and was hence not included in the current analysis. Our previous study (4) reported results for 831 knees: 112 from the healthy reference sample, 310 sKLG2, 300 sKLG3, and 109 sKLG4. Six knees with JSN but without definite osteophytes had not been included in the previous analysis (4), but were included in the current study, because the central readings did not confirm the above findings.
Statistical analysis
The mean, standard deviation (SD) and 95% confident intervals of change in cartilage thickness (ThCtAB; µm) between baseline and year-1 follow-up was determined, and the standardized response mean (SRM=mean/SD change) was used as a measure of the sensitivity to change. OV1 and FTJ rates of change were compared between KLG2 knees with and without JSN, using an unpaired Student’s t-test. The same comparison was made for KLG1 knees. The same procedure was used to test whether medial OARSI JSN grade2 knees displayed greater cartilage loss than grade1 knees. Analysis of variance (ANOVA) was then used to confirm whether the inferences would hold after accounting for age, sex, and BMI. MFTC cartilage change was used here, because medial JSN was associated with cartilage loss in the medial but not in the lateral compartment (10). No statistical comparisons were made between site- and central reading strata in order to avoid issues of multiple parallel testing on readings with different constructs.
RESULTS
Of 836 study participants, the 112 from the healthy reference cohort were [mean±SD] 55±7.7 years (BMI 24.3±3.0), whereas the 724 knees with RKOA (site readings) were 63±9.3 years (BMI 29.6±4.7). Of the 112 healthy reference subjects with bilateral siteKLG0, 101 had bilateral normal knees based on central radiographic reading (Table 1). Of 724 knees with siteKLG2–4, the central readings reported 93 to be centKLG0, 101 centKLG1 (OARSI JSN grade0/1=61/40), 308 centKLG2 (JSN grade0/1/2=98/209/1), 161 centKLG3 (all JSN grade 2), and 61 centKLG4 (all JSN grade 3).
Table 1.
Rates of one-year change in the femorotibial subregion with the greatest change in each knee (OV1), according to radiographic strata based on the OAI site and central readings
| Site readings | Central readings (Boston Univ.) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n= | OV1 MC | FTJ MC | FTJ | n= | OV1 MC | FTJ MC | FTJ | |||||
| (µm) | CI 95% | (µm) | CI 95% | SRM | (µm) | CI 95% | (µm) | CI 95% | SRM | |||
| Healthy | 112 | −115 | [−126; −105] | 9 | [−17;35] | 0.07 | 101 | −111 | [−122; −100] | 13 | [−15;40] | 0.09 |
| KLG0 | n.a. | - | - | - | 93 | −120 | [−132; −108] | −12 | [−35;10] | −0.11 | ||
| KLG1 | n.a. | - | - | - | 101 | −138 | [−156; −120] | −33 | [−67;2] | −0.19 | ||
| KLG1 −JSN | 61 | −150 | [−176; −125] | −55 | [−101; −10] | −0.30 | ||||||
| KLG1 +JSN | 40 | −119 | [−143; −95] | 1 | [−50;52] | 0.01 | ||||||
| KLG2 | 308 | −136 | [−148; −125] | −20 | [−37; −4] | −0.14 | 308 | −160 | [−176; −145] | −40 | [−59; −20] | −0.23 |
| KLG2 −JSN | 98 | −134 | [−155; −115] | −25 | [−54;5] | −0.16 | ||||||
| KLG2 +JSN | 210 | −172 | [−193; −152] | −46 | [−72; −21] | −0.25 | ||||||
| KLG3 | 299 | −180 | [−197; −164] | −69 | [−91; −47] | −0.35 | 161 | −203 | [−225; −181] | −109 | [−142; −77] | −0.52 |
| KLG4 | 111 | −201 | [−222; −179] | −107 | [−147; −67] | −0.50 | 61 | −195 | [−223; −166] | −84 | [−137; −32] | −0.40 |
MC = mean change; CI 95% = [lower bound; upper bound] of the 95 confidence interval; SRM = standardized response mean = mean/SD change; KLG = Kellgren Lawrence grade of radiographic knee osteoarthritis; JSN = OARSI grade of (medial or lateral) radiographic joint space narrowing The numbers of site readings (n = 830) and central readings (n = 825) differ, because 6 cases were not classified in our previous paper on the site readings, but were here. In addition we found that from the healthy reference subjects only 101 had bilateral normal knees according to the central readings, explaining the total difference of n = 5.
The rates of OV1 change were of similar magnitude between healthy reference cohorts defined by site vs. central readings and appeared to increase with greater KLGs (Table 1). centKLG2 knees with JSN displayed significantly (p=0.03) greater rates of OV1 cartilage thickness change than those without JSN (Table 1). Similar difference in means was found after adjusting for age, sex and BMI (p=0.03). In contrast, the OV1 rates of change did not differ significantly between centKLG1 knees with and without JSN (p=0.09) (Table 1). Similar qualitative observations were made for total femorotibial joint (FTJ) cartilage thickness change (i.e. the sum of medial and lateral compartment change), the SRM in centKLG2 knees with JSN being more negative than in those without JSN, although the difference did not reach statistical significance (p=0.31 without, p=0.43 with adjustment).
Knees with greater medial centJSN grades tended to displayed greater rates of MFTC cartilage loss (Table2). MFTC cartilage loss in OARSI medial centJSN grade2 knees was significantly (p=0.02) greater than that in grade1 knees (Table 2), and the conclusion and difference in means were the same after adjusting for age, sex and BMI (p=0.02). The observed rate of MFTC change in centJSN grade2 appeared to be similar to that in grade3 knees (p=0,96) (Table 2).
Table 2.
Rates of one-year change in the medial femorotibial compartment (MFTC), according to radiographic strata based on the OAI site and central readings
| Site readings | Central readings (BU) | |||||||
|---|---|---|---|---|---|---|---|---|
| n= | MFTC MC | n= | MFTC MC | |||||
| (µm) | CI 95% | SRM | (µm) | CI 95% | SRM | |||
| Healthy | 112 | +2 | [−10;20] | 0.02 | 101 | +2 | [−10;20] | 0,02 |
| medJSN 0 | 428 | −15 | [−25; −5] | −0,14 | 356 | −14 | [−30;1] | −0,13 |
| medJSN 1 | 217 | −43 | [−60; −26] | −0,34 | 209 | −31 | [−50; −13] | −0,25 |
| medJSN 2 | (collapsed with gr. 1) | 116 | −70 | [−99; −41] | −0,44 | |||
| medJSN 3 | 73 | −86 | [−121; −51] | −0,57 | 43 | −72 | [−108; −35] | −0,59 |
MC = mean change; CI 95% = [lower bound; upper bound] of the 95 confidence interval; SRM = standardized response mean = mean/SD change; medJSN = OARSI grade of medial radiographic joint space narrowing
DISCUSSION
This study presents, for the first time, rates of cartilage loss in specific RKOA strata defined by central OAI readings, namely KLG2 knees with and without radiographic JSN, and knees with medial OARSI JSN grade 2 vs. 1. We find the maximum subregion change (OV1) to be greater in centKLG2 knees with than in those without JSN. Clinical trials that aim at determining risk factors of structural progression, or the effect of a DMOAD on cartilage loss, should hence preferably include KLG2 knees with JSN, if significantly cartilage loss (in the placebo group) is to be observed over acceptable observation periods. The observed rates of MFTC cartilage loss in medial grade2 centJSN knees were more than 2-fold greater than in grade1 knees. From a prognostic perspective, therefore, OARSI JSN grades 1 and 2 knees should thus not be collapsed into the same grade, as done for recruitment purposes by the OAI site readings. MFTC cartilage loss in medial JSN grade2 and 3 knees, in contrast, were observed to be relatively similar.
It is surprising to what extent the radiographic classification differed between site and central readings, particularly in view of the site readers having been trained for this purpose. Almost ¼ of siteKLG≥2 knees turned out to not display definite RKOA in central readings, and approx. 14% were classified to not have any radiographic change at all. Enrollment for the OAI extended over a 2-year period, and this may have involved drift within and between the site readers. Further, different thresholds were noted between expert and trained readers for scoring osteophytes and radiographic JSN (5).
Radiographic strata other than centKLG2 (and centKLG1) with and without JSN, and medial centJSN grade2 vs. 1, were not compared statistically, to avoid issues of multiple parallel testing. However, further interesting observations can be made at a descriptive level: Exclusion of knees from the healthy reference cohort by central reading did not have a noticeable impact on the observed rate of cartilage loss. centKLG0 knees (with risk factors of RKOA) only had very marginally greater rates of change than healthy reference knees. The OV1 rate of change in centKLG1 knees was in between that of centKLG0 and centKLG2, but was almost identical to that of centKLG2 knees without JSN. Although the observed rate of change in KLG1 subjects without JSN was greater than those with JSN, this difference was not statistically significant. The rate and also the SD of change in centKLG2 knees without JSN was almost identical to that of siteKLG2 knees (who did not have JSN by definition); further, removal of KLG0 and 1 knees by the central readings from the pool of siteKLG2 knees did not appear to increase the sensitivity to change (SRM). However, centKLG2 knees with JSN displayed greater sensitivity of femorotibial cartilage loss (SRM −0.25) than those without JSN (SRM −0.16).
Given that JSN was identified to be a potent predictor of subsequent cartilage loss (10–12), the finding that centKLG2 knees with JSN display greater rates of cartilage loss than those without was not unexpected. A recent clinical trial (13) used change in medial radiographic joint space width (JSW) as an outcome and specifically recruited KLG2 knees with JSN. The trial reported a significant reduction in JSW (−0.13±0.36mm) over one year in the placeo group, using a highly controlled (i.e. modified Lyon Schuss) radiographic technique (13), with the SRM being similar to that observed for medial compartment cartilage thickness loss in knees with medial OARSI grade1 JSN in our present study.
In conclusion, presence of radiographic JSN within KLG2 (but not within KLG1) knees was associated with significantly greater rates of cartilage loss and greater longitudinal sensitivity to change. Differentiating knees with mild (OARSI grade1) vs. moderate (grade2) medial JSN, and KLG2 knees with and without JSN, is hence important from a prognostic perspective of predicting structural progression in KOA. The findings reported have important implications for designing clinical trials that test the efficacy of disease modifying drugs (DMOADs).
ACKNOWLEDGEMENTS
We thank the OAI participants, investigators, funders, coordinating center, readers at Boston University, and readers at Chondrometrics GmbH for their support. Further, we thank Robert Buck, PhD (StatAnswers Consulting LLC, Minneapolis, MN, USA) for statistical advice and analysis.
FUNDING SOURCES
The study and image acquisition was supported by the Osteoarthritis Initiative (OAI), a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Pfizer, Inc.; Novartis Pharmaceuticals Corporation; Merck Research Laboratories; and GlaxoSmithKline. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. The image analysis of this study was funded by an industry consortium consisting of Pfizer Inc., Eli Lilly & Co, Merck Serono SA, Glaxo Smith Kline Inc., Wyeth Research, Centocor Research and Development, Inc, and Novartis Pharma AG and by the OAI coordinating center (UCSF).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONTRIBUTIONS
All authors made substantial contributions to all three sections: (1) the conception and design of the study, data acquisition, analysis and interpretation; (2) drafting the article or revising it critically; (3) final approval of the version to be submitted.
COMPETING INTERESTS
Susanne Maschek and Wolfgang Wirth have part time appointments with Chondrometrics GmbH and are co-owners of Chondrometrics GmbH, a company providing quantitative MR image analysis services. Felix Eckstein is CEO and co-owner of Chondrometrics GmbH. He has provided consulting services to MerckSerono, Novartis and Abbvie. He has received funding support for this study from Pfizer, Eli Lilly, Novartis, MerckSerono, Glaxo Smith Kline, Wyeth, and Contocor. He has received funding support not related to this study from Stryker, Abbvie, Kolon, and Synarc. Christoph Ladel is employed by Merck KGaA, Darmstadt, Germany. Marie-Pierre Hellio Le Graverand is employed by Pfizer Development Japan, Tokyo, Japan.
Reference List
- 1.Eckstein F, Wirth W, Nevitt MC. Recent advances in osteoarthritis imaging-the Osteoarthritis Initiative. Nat Rev Rheumatol. 2012;8:622–630. doi: 10.1038/nrrheum.2012.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nevitt MC, Peterfy C, Guermazi A, Felson DT, Duryea J, Woodworth T, et al. Longitudinal performance evaluation and validation of fixed-flexion radiography of the knee for detection of joint space loss. Arthritis Rheum. 2007;56:1512–1520. doi: 10.1002/art.22557. [DOI] [PubMed] [Google Scholar]
- 3.Peterfy CG, Schneider E, Nevitt M. The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthritis Cartilage. 2008;16:1433–1441. doi: 10.1016/j.joca.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eckstein F, Nevitt M, Gimona A, Picha K, Lee JH, Davies RY, et al. Rates of change and sensitivity to change in cartilage morphology in healthy knees and in knees with mild, moderate, and end-stage radiographic osteoarthritis: Results from 831 participants from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2011;63:311–319. doi: 10.1002/acr.20370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guermazi A, Hunter DJ, Li L, Benichou O, Eckstein F, Kwoh CK, et al. Different thresholds for detecting osteophytes and joint space narrowing exist between the site investigators and the centralized reader in a multicenter knee osteoarthritis study--data from the Osteoarthritis Initiative. Skeletal Radiol. 2012;41:179–186. doi: 10.1007/s00256-011-1142-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):1–56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Wirth W, Eckstein F. A technique for regional analysis of femorotibial cartilage thickness based on quantitative magnetic resonance imaging. IEEE Trans Med Imaging. 2008;27:737–744. doi: 10.1109/TMI.2007.907323. [DOI] [PubMed] [Google Scholar]
- 9.Wirth W, Buck R, Nevitt M, Le Graverand MP, Benichou O, Dreher D, et al. MRI-based extended ordered values more efficiently differentiate cartilage loss in knees with and without joint space narrowing than region-specific approaches using MRI or radiography--data from the OA initiative. Osteoarthritis Cartilage. 2011;19:689–699. doi: 10.1016/j.joca.2011.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wirth W, Nevitt M, Le Graverand MP, Lynch J, Maschek S, Hudelmaier M, et al. Lateral and Medial Joint Space Narrowing Predict Subsequent Cartilage Loss in the Narrowed, but not in the Non-narrowed Femorotibial Compartment - Data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2013 doi: 10.1016/j.joca.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Le Graverand MP, Buck RJ, Wyman BT, Vignon E, Mazzuca SA, Brandt KD, et al. Change in regional cartilage morphology and joint space width in osteoarthritis participants versus healthy controls: a multicentre study using 3.0 Tesla MRI and Lyon-Schuss radiography. Ann Rheum Dis. 2010;69:155–162. doi: 10.1136/ard.2008.099762. [DOI] [PubMed] [Google Scholar]
- 12.Eckstein F, Le Graverand MP, Charles HC, Hunter DJ, Kraus VB, Sunyer T, et al. Clinical, radiographic, molecular and MRI-based predictors of cartilage loss in knee osteoarthritis. Ann Rheum Dis. 2011;70:1223–1230. doi: 10.1136/ard.2010.141382. [DOI] [PubMed] [Google Scholar]
- 13.Hellio Le Graverand MP, Clemmer RS, Brunell RM, Hayes CW, Miller CG, Vignon E. Considerations when designing a disease-modifying osteoarthritis drug (DMOAD) trial using radiography. Semin Arthritis Rheum. 2013;43:1–8. doi: 10.1016/j.semarthrit.2012.11.006. [DOI] [PubMed] [Google Scholar]


