Abstract
Objective
To compare cross-sectional and longitudinal side-differences in thigh muscle anatomical cross-sectional areas (ACSAs), muscle strength, and specific strength (strength/ACSA), between knees with early radiographic change vs. knees without radiographic knee osteoarthritis (RKOA), in the same person.
Design
55 (of 4796) Osteoarthritis Initiative participants fulfilled the inclusion criteria of early RKOA in one limb (definite tibiofemoral osteophytes; no radiographic joint space narrowing [JSN]) vs. no RKOA (no osteophyte; no JSN) in the contralateral limb. ACSAs of the thigh muscles and quadriceps heads were determined using axial MRIs at 33%/30% femoral length (distal to proximal). Isometric extensor and flexor muscle strength were measured (Good Strength Chair). Baseline quadriceps ACSA and extensor (specific) strength represented the primary analytic focus, and two-year changes of quadriceps ACSAs the secondary focus.
Results
No statistically significant side-differences in quadriceps (or other thigh muscle) ACSAs, muscle strength, or specific strength were observed between early RKOA vs. contralateral limbs without RKOA (p≥0.44), neither in men nor in women. The two-year reduction in quadriceps ACSA in limbs with early RKOA was −0.9±6% (mean ± standard deviation) vs. −0.5±6% in limbs without RKOA (statistical difference p=0.85).
Conclusion
Our results do not provide evidence that early unilateral radiographic changes, i.e. presence of osteophytes, are associated with cross-sectional or longitudinal differences in quadriceps muscle status compared with contralateral knees without RKOA. At the stage of early unilateral RKOA there thus appears to be no clinical need for countervailing a potential dys-balance in quadriceps ACSAs and strength between both knees.
Introduction
Quadriceps strength is an important determinant of physical disability, and quadriceps weakness is commonly observed in radiographic knee osteoarthritis (RKOA) (1). In a recent between-knee, within-person comparison, we found smaller quadriceps anatomical cross-sectional areas (ACSAs) and isometric extensor muscle strength in limbs with frequent knee pain compared with contralateral limbs without pain with the same RKOA stage (2). In contrast, baseline quadriceps ACSAs or strength did not differ between limbs with advanced RKOA (i.e. joint space narrowing [JSN]) vs. contralateral ones without JSN, nor did longitudinal changes in ACSAs and strength (3). These data have suggested that muscle status may be associated with knee pain, but not with advanced RKOA status.
Other work has proposed that a reduction in thigh muscle mass and strength may be primarily associated with the onset of the early stages of RKOA (4;5), and our study in JSN vs. no-JSN limbs may have missed these, because the potential time window during which discordant muscle status was present had already passed. Whereas previous work studied whether reduction in muscle strength (as an independent exposure variable of risk) is associated with the onset or progression of RKOA as an outcome (4–6), the current study focuses on cross-sectional differences in thigh muscle status between knees with an early radiographic stage of knee OA vs. contralateral knees without RKOA (within-person comparison), and on two-year changes in muscle ACSAs (the dependent variable) of knees with and without early RKOA (the independent variable). We considered presence of an osteophyte and absence of JSN as an early stage of RKOA, because cartilage thickness is not yet reduced in these knees (7). We tested the following hypotheses:
Quadriceps ACSAs, strength, and specific strength are lower in knees displaying early RKOA (i.e. definite osteophytes, no JSN) compared to contralateral knees without any radiographic change.
The two-year decrease in muscle ACSAs is greater in early RKOA compared to contralateral no-RKOA knees.
Methods
Participants
Participants were drawn from the Osteoarthritis Initiative (OAI) participants (n=4796 http://www.oai-ucsf.edu/datarelease/) (7;8). The inclusion criteria were early RKOA of the tibiofemoral joint (i.e. definite tibial or femoral marginal osteophytes according to the Osteoarthritis Research Society International atlas) in one knee, no signs of RKOA in the contralateral knee, and no joint space narrowing (JSN) in either knee at baseline. Radiographic readings were taken from the OAI data base, identifying 84 subjects fulfilling the above criteria; these were confirmed by an experienced musculoskeletal radiologist (F.R.) in 61 cases (7). Pain was not an inclusion criterion, but WOMAC pain scores (3.1 Likert scale; 0–20; 20 being the worst) and Physical Activity Scale for the Elderly (PASE) scores were exported from the OAI data base. Further, participants needed to have baseline T1-weighted axial spin-echo MRI images of the thigh available (imaging data set 0.E.1), which was the case for 55 participants. Of these 38 also had 2-year follow-up MRI (3.E.2) available.
Evaluation of anatomical cross-sectional areas (ACSAs) and strength
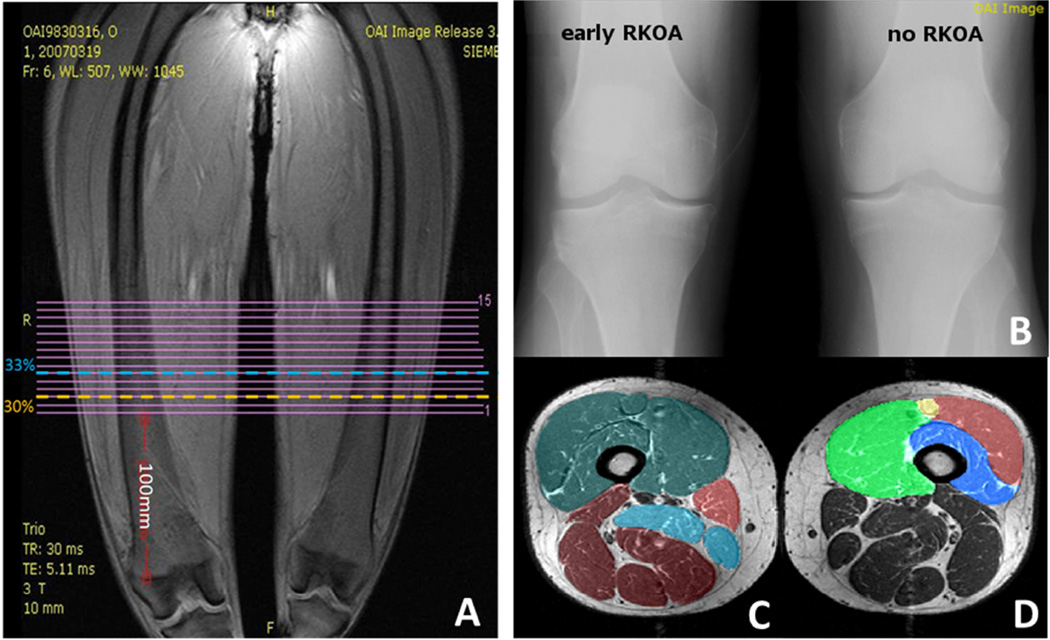
ACSAs of the quadriceps, hamstrings, and adductors were manually segmented at anatomically consistent locations (33% femoral length; distal to proximal), and individual quadriceps heads at 30% (2;3) (Figure 1). Isometric knee extensor and flexor strength was measured using the “Good Strength Chair” (Metitur Oy, Jyvaskyla, Finland) at 60° knee flexion (2;3). Strength data was available for 49 of the 55 participants; specific strength was calculated as strength per unit ACSA (N/cm2).
Figure 1.
A Coronal localizer image: 15 continuous axial slices of the thigh have been acquired. B. Participants (right top). For the current study we selected participants with early radiographic knee osteoarthritis (RKOA) in one knee and no RKOA in the contralateral knee on fixed-flexion X-rays (right top). C–D. Axial cross-sectional MRIs with segmented muscles. Anatomical cross-sectional areas of the quadriceps (pink), hamstrings (red), and adductors (yellow) have been segmented at 33% of femoral length (from distal to proximal) (C). ACSAs of the individual quadriceps heads vastus medialis (brown), vastus intermedius (turquoise), vastus lateralis (yellow), and rectus femoris (purple) have been segmented at 30% of femoral length (from proximal to distal) (D).
Statistical analyses
The cross-sectional between-knee within-person comparison of quadriceps ACSAs, strength, and specific strength (early RKOA vs. no-RKOA) was considered the primary analytic focus; the two-year changes in quadriceps ACSAs within limbs and between early RKOA vs no-RKOA limbs were the secondary analytic focus; differences between knees were tested using paired t-tests and statistical significance was considered as p<0.05. Other tests were considered exploratory. Given reports on the reduction of muscle strength to be associated with knee OA in women, but not in men (5;9), sensitivity analyses were performed between both sexes. Pearson’s correlation coefficients were calculated for quadriceps ACSAs vs. extensor strength, hamstring ACSAs vs. flexor strength, and for two-year change in quadriceps ACSAs vs. two-year change in PASE scores.
Results
Demographics
The 55 OAI participants (53% women) meeting the inclusion criteria were 60.6 6±9.8 (mean ±standard deviation) years old (BMI 27.7±4.8 kg/m2). The 49 participants (51% women) with baseline strength data were 60.0±10.1 years old (BMI 27.7±4.8 kg/m2) and the 38 participants (58% women) with two-year follow-up MRIs were 59.8±9.8 years old (BMI 27.6±4.9 kg/m2). There was no statistically significant difference in the age and BMI of those included in the longitudinal analysis vs. those not included (p≥0.52; unpaired t-tests). 73% of the 55 participants had medial (5 femoral; 35 tibial) and 49% lateral (7 femoral, 20 tibial) definite marginal osteophytes. The early RKOA limb was from the dominant limb in 27 participants (25×right, 2×left), and from the non-dominant in 23 participants (19×right, 4×left); 5 participants replied to have no dominant leg (OAI question: “Which leg do you use to kick a ball?”). Baseline WOMAC pain scores tended to be greater (2.16±3.4) in early RKOA than in no-RKOA knees (1.51±3.0), but the difference did not attain statistical significance (p=0.10). At two-year follow-up, WOMAC knee pain scores were 1.35±2.2 in early RKOA and 1.77±2.7 in no-RKOA knees. PASE scores were 162.3±91.3 at baseline (n=55), and 160.7±78.5 at follow-up (n=38).
Cross-sectional comparisons
There were no statistically significant side-differences in quadriceps ACSAs or extensor (specific) strength between knees with early RKOA vs. contralateral knees without RKOA (p≥0.11; Table 1). Further, no statistically significant side-differences were observed in other muscles, and results were similar when stratifying for men and women (Supplementary Online Tables 1&2). The correlation between quadriceps ACSAs with extensor strength was 0.66 (95% confidence interval 0.46–0.79) and that between hamstring ACSAs with flexor strength 0.55 (0.32–0.72) in early RKOA knees, and 0.63 (0.43–0.78) and 0.66 (0.46–0.79) in no-RKOA knees, respectively.
Table 1.
Baseline absolute (mean [95% CI]) and mean percent (%) differences in thigh muscle anatomical cross-sectional areas (ACSAs) and (specific) strength between knees with early vs. knees without radiographic knee osteoarthritis (RKOA)
| Early RKOA n=55 |
no RKOA n=55 |
Early vs. no RKOA Absolute Diffs [95% CI] |
Mean % Differences |
p-value Early vs. no RKOA |
|
|---|---|---|---|---|---|
| Muscle cross-sectional areas (cm2) | |||||
| Quadriceps | 53.2 ± 16.1 | 52.8 ± 15.1 | −0.45 [−1.64, 0.75] | −0.1 | 0.46 |
| Hamstrings | 32.5 ± 9.0 | 32.7 ± 9.0 | +0.24 [−0.37, 0.85] | +1.1 | 0.44 |
| Adductors | 13.5 ± 7.2 | 13.6 ± 7.6 | +0.06 [−0.75, 0.87] | +0.3 | 0.89 |
| VM | 18.7 ± 5.3 | 18.9 ± 5.2 | +0.23 [−0.38, 0.83] | +2.2 | 0.46 |
| VL | 14.8 ± 5.1 | 14.1 ± 4.6 | −0.71 [−1.60, 0.17] | −2.1 | 0.11 |
| VIM | 14.3 ± 4.4 | 14.2 ± 4.3 | −0.08 [−0.49, 0.32] | +0.2 | 0.68 |
| RF | 2.5 ± 1.4 | 2.5 ± 1.3 | +0.01 [−0.14, 0.16] | +7.3 | 0.91 |
| Strength (Newton)* | |||||
| Extensors | 387.2 ± 136.8 | 383.8 ± 134.1 | −3.35 [−23.7, 17.0] | +0.5 | 0.74 |
| Flexors | 157.2 ± 78.6 | 160.9 ± 79.4 | +3.69 [−7.9, 15.2] | +7.8 | 0.52 |
| Specific Strength (N/cm2)* | |||||
| Extensors | 7.3 ± 2.1 | 7.3 ± 2.0 | +0.01 [−0.32, 0.33] | +1.1 | 0.97 |
| Flexors | 4.7 ± 1.8 | 4.8 ± 1.9 | +0.12 [−0.21, 0.46] | +6.4 | 0.47 |
CI=confidence interval; Diffs= Differences ; VM=vastus medialis; VL=vastus lateralis; VIM=vastus intermedius; RF=rectus femoris;
Muscle (specific) strength data were available for 49 (out of 55) participants
Longitudinal comparisons
Early RKOA knees showed a 0.9% reduction, and contralateral no-RKOA knees a 0.5% reduction in quadriceps ACSAs over two years (Supplementary Online Table 3). These changes were not statistically significantly different from each other. The same applied to the other thigh muscles (p≥0.10; Supplementary Online Table 3). No significant correlation was observed between two-year change in quadriceps ACSAs with those in the PASE score, neither in RKOA nor in no-RKOA knees (p≥0.08; data not shown)
Discussion
This is the first study to examine thigh muscle status in early RKOA vs. no-RKOA, using a between-knee, within-person study design. The study differs from our previous work (2;3) in that it specifically examines thigh muscle status in knees with discordant early RKOA vs. no RKOA status. These knees were in a state at which osteophyte formation had already taken place, but no radiographic JSN or reduction in cartilage thickness was yet present (7). Further, no structural progression was detectable in these knees over a one-year period, either with MRI (cartilage thickness) or with radiography (loss in joint space) (10). This stage of RKOA has been suggested to be of particular relevance in context of interaction between muscle status and RKOA (4;5). However, we did not find statistically significant side-differences in thigh muscle cross-sectional areas and (specific) strength between early RKOA and no-RKOA limbs in either sex, and no statistically significant differences in the two-year change of the quadriceps ACSAs between these knees.
A limitation of the study is the relatively small sample size. This was due to the specific inclusion criteria of this between-knee, within-person design (7). This study design, however, has the advantage that it circumvents between-person confounders (such as differences in age, height, weight, physical activity etc., which may be independently associated with muscle status), and that paired statistical tests can be applied. Our results are in contrast to those of a previous between-knee, within-person comparison, in which we identified differences in quadriceps ACSAs and strength between painful vs painless knees with the same RKOA status (2). This previous study had a smaller sample size (n=48) and was successful in detecting a significant (6%) side-difference (2). A further limitation of our study may be that it was not restricted to participants without pain, but only 17 participants had bilateral WOMAC pain=0. Although baseline WOMAC pain scores were somewhat greater in early RKOA than in no-RKOA limbs (2.2±3.4 vs. 1.5±3.0), this difference (0.6) was lower than the minimal clinically important difference (MCID) of 4 points reported for WOMAC pain (11). It also was smaller than that in our previous between-knee study of painful vs. contralateral painless knees (4.4±3.5 vs. 0.6±1.7) (2) and smaller than that in a recent comparison of asymptomatic (WOMAC=0) vs. symptomatic OAI participants (WOMAC≥5) (12). Both cross-sectional studies (2;12) found statistically significant pain-related differences in muscle strength, independent of RKOA status, and the between-knee comparison (2) also reported significant side-differences in quadriceps ACASs.
We resume that side-differences in pain have a stronger relationship with those in muscle status than side-differences in structural (radiographic) knee OA. These findings appear to not only apply to later stages of RKOA where JSN is present (3), but also to the earliest RKOA stages where osteophytes have formed, but no JSN is present yet. Further, it appears that side-differences in pain need to exceed a certain threshold to lead to measurable differences in muscle ACSAs and strength. Still, the current results should be interpreted in light of RKOA often being a bilateral disease: Although the contralateral (control) knees had no sign of RKOA, they still shared the same (person-specific) risk factors. Therefore, they cannot necessarily be regarded as perfectly healthy.
We are aware that we applied a relatively large number of statistical tests in an exploratory context; however, the primary and secondary outcomes were defined a priori and the analytic focus was tailored to these specific measures. We purposely did not adjust for parallel tests, because quadriceps ACSAs and (specific) strength are highly co-linear. The correlations of ACSAs with isometric strength in the current study are comparable with those reported previously in painful and painless knees (2), and in knees with and without advanced RKOA (3). Yet, the only moderate correlations suggest that other factors such as age, sex, BMI, and neuromuscular activation influence thigh muscle strength beyond that of muscle mass alone.
Our analysis of two-year changes in muscle status was confined to differences in muscle ACSAs, as these are more sensitive to change than those in muscle strength (13). The two-year changes in quadriceps ACSA were small, and although they appeared greater in early RKOA knees than in contralateral no-RKOA knees (−0.9 vs. −0.5%), the between-person variability was relatively large and the difference did not attain statistical significance. These changes were slightly smaller than those observed in a convenience sample of RKOA (−2.1%) and no-RKOA knees (−1.5%) (14). They also were smaller than those in limbs with JSN knees (−1.1%) (3) and in limbs with progressive knee OA (−2.8%) or matched RKOA knees without structural progression (−1.8%) (13), with the same measurement methodology used in the current and in the latter studies (3;13).
Current OARSI guidelines recommend muscle strengthening exercise in the clinical management of knee OA (15). However, there exists little evidence that these therapeutic measures are effective in preventing the progression of change in radiographic joint structure. A recent prospective study did not find changes in thigh muscle strength to precede or to be associated with radiographic progression (i.e. reduction in JSW) in knees without and with early RKOA (6). In the current study, in which muscle ACSAs were regarded as the dependent and early RKOA status as the independent factor, we also did not find any evidence for a relationship between both variables.
In conclusion, our results do not provide evidence that early radiographic change, i.e. presence of osteophytes, is associated with cross-sectional or longitudinal differences in quadriceps muscle status compared with contralateral knees without RKOA. At the stage of early unilateral RKOA there thus appears to be no clinical need for countervailing a potential dys-balance in quadriceps ACSAs and strength between both knees.
Supplementary Material
Acknowledgements
We would like to thank the OAI participants, OAI investigators and OAI Clinical Center’s staff for generating this publicly available image data set. The images were acquired by the OAI, a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institute of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners of the OAI include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institute of Health. This manuscript has received the approval of the OAI Publications Committee based on a review of its scientific content and data interpretation.
The image analysis was supported by funds from the Paracelsus Medical University Research Fund (PMU FFF E-11/14/073-WIR).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author’s Contribution
All authors have made substantial contributions to: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Role of the funding source
The funding sources took no active part of influence on the analysis of the data and in drafting or revising the article. However, the manuscript received the approval of the OAI Publications Committee based on a review of its scientific content and data interpretation.
Competing interest statement
Felix Eckstein is CEO and co-owner of Chondrometrics GmbH, a company providing MR image analysis services. He provides consulting services to MerckSerono, Novartis, and Sanofi Aventis. Torben Dannhauer and Sebastian Cotofana have part-time appointments with Chondrometrics GmbH. Wolfgang Wirth has a part-time appointment with Chondrometrics GmbH and is co-owner of Chondrometrics GmbH. Frank Roemer is co-owner of Boston Core Imaging Lab and provides consulting services for NIH and Merck Serono. Michael Nevitt and Anja Ruhdorfer have no competing interests.
Contributor Information
T Dannhauer, Email: torben.dannhauer@pmu.ac.at.
W Wirth, Email: wolfgang.wirth@pmu.ac.at.
S Cotofana, Email: sebastian.cotofana@pmu.ac.at.
F Roemer, Email: Frank.Roemer@klinikum-augsburg.de.
M Nevitt, Email: MNevitt@psg.ucsf.edu.
F Eckstein, Email: felix.eckstein@pmu.ac.at.
Reference List
- 1.Petterson SC, Barrance P, Buchanan T, Binder-Macleod S, Snyder-Mackler L. Mechanisms underlying quadriceps weakness in knee osteoarthritis. Med Sci Sports Exerc. 2008;40(3):422–427. doi: 10.1249/MSS.0b013e31815ef285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sattler M, Dannhauer T, Hudelmaier M, Wirth W, Sanger AM, Kwoh CK, et al. Side differences of thigh muscle cross-sectional areas and maximal isometric muscle force in bilateral knees with the same radiographic disease stage, but unilateral frequent pain - data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2012;20(6):532–540. doi: 10.1016/j.joca.2012.02.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruhdorfer A, Dannhauer T, Wirth W, Hitzl W, Kwoh CK, Guermazi A, et al. Thigh muscle cross-sectional areas and strength in advanced versus early painful osteoarthritis-An exploratory between-knee, within-person comparison in osteoarthritis initiative participants. Arthritis Care Res (Hoboken) 2013:10. doi: 10.1002/acr.21965. [DOI] [PubMed] [Google Scholar]
- 4.Thorstensson CA, Petersson IF, Jacobsson LT, Boegard TL, Roos EM. Reduced functional performance in the lower extremity predicted radiographic knee osteoarthritis five years later. Ann Rheum Dis. 2004;63(4):402–407. doi: 10.1136/ard.2003.007583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Segal NA, Glass NA. Is quadriceps muscle weakness a risk factor for incident or progressive knee osteoarthritis? Phys Sportsmed. 2011;39(4):44–50. doi: 10.3810/psm.2011.11.1938. [DOI] [PubMed] [Google Scholar]
- 6.Eckstein F, Hitzl W, Duryea J, Kent KC, Wirth W. Baseline and longitudinal change in isometric muscle strength prior to radiographic progression in osteoarthritic and pre-osteoarthritic knees - data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2013;21(5):682–690. doi: 10.1016/j.joca.2013.02.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cotofana S, Buck R, Wirth W, Roemer F, Duryea J, Nevitt M, et al. Cartilage thickening in early radiographic human knee osteoarthritis - within-person, between-knee comparison. Arthritis Care Res (Hoboken) 2012 doi: 10.1002/acr.21719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eckstein F, Wirth W, Nevitt MC. Recent advances in osteoarthritis imaging-the Osteoarthritis Initiative. Nat Rev Rheumatol. 2012:10. doi: 10.1038/nrrheum.2012.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Segal NA, Glass NA, Torner J, Yang M, Felson DT, Sharma L, et al. Quadriceps weakness predicts risk for knee joint space narrowing in women in the MOST cohort. Osteoarthritis Cartilage. 2010;18(6):769–775. doi: 10.1016/j.joca.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cotofana S, Buck R, Dreher D, Wirth W, Roemer F, Duryea J, et al. Longitudinal (1-year) change in cartilage thickness in knees with early knee osteoarthritis: A within-person between-knee comparison-data from the OAI. Arthritis Care Res (Hoboken) 2013 doi: 10.1002/acr.22172. [DOI] [PubMed] [Google Scholar]
- 11.Escobar A, Garcia PL, Herrera-Espineira C, Aizpuru F, Sarasqueta C, Gonzalez Saenz de TM, et al. Total knee replacement; minimal clinically important differences and responders. Osteoarthritis Cartilage. 2013;21(12):2006–2012. doi: 10.1016/j.joca.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Ruhdorfer A, Wirth W, Hitzl W, Nevitt M, Eckstein F. Thigh muscle strength is associated with knee symptoms but not with radiographic disease stage of osteoarthritis - data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 2014 doi: 10.1002/acr.22317. [DOI] [PubMed] [Google Scholar]
- 13.Dannhauer T, Sattler M, Wirth W, Hunter DJ, Kwoh CK, Eckstein F. Longitudinal sensitivity to change of MRI-based muscle cross-sectional area versus isometric strength analysis in osteoarthritic knees with and without structural progression: pilot data from the Osteoarthritis Initiative. MAGMA. 2013 doi: 10.1007/s10334-013-0418-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beattie KA, Macintyre NJ, Ramadan K, Inglis D, Maly MR. Longitudinal changes in intermuscular fat volume and quadriceps muscle volume in the thighs of women with knee osteoarthritis. Arthritis Care Res (Hoboken) 2012;64(1):22–29. doi: 10.1002/acr.20628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16(2):137–162. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.