Abstract
We report a rare case of Aspergillus terreus endogenous endophthalmitis in an immunocompetent patient with subretinal abscess and also review the reported cases. A 50-year-old healthy male presented with sudden painful loss of vision in right eye. He was diagnosed with endogenous endophthalmitis and underwent urgent vitrectomy. Aspergillus terreus growth was obtained in culture. At final follow-up, there was complete resolution of the infection but visual acuity was poor due to macular scar. Aspergillus terreus is a rare cause of endophthalmitis with usually poor outcomes. Newer antifungals like Voriconazole can be sometimes associated with better prognosis.
Keywords: Aspergillus terreus, endogenous endophthalmitis, immunocompetent, subretinal abscess
Fungal endogenous endophthalmitis is usually associated with immunocompromised states. Aspergillus terreus is a rare cause of endogenous endophthalmitis with only six reported cases.[1,2,3,4,5,6] We report a rare case of A terreus endogenous endophthalmitis in an immunocompetent patient and review the other cases which have been reported. This is the first case report of A terreus endogenous endophthalmitis from India.
Case Report
A 50-year-old healthy non diabetic male presented with sudden painful decrease in vision in right eye (OD) since one week. The patient gave history of a bout of gastroenteritis 2 weeks back. On examination, best corrected visual acuity (BCVA) in OD was perception of light with accurate projection of rays. Anterior segment examination showed circumciliary congestion, corneal haze, anterior chamber cells 3+, clear lens, and 3+ vitreous cells. Intraocular pressure was 10 mm of Hg. Indirect ophthalmoscopy showed grade 3 vitritis with central yellowish sub retinal lesion [Fig. 1a]. The retina appeared attached. BCVA in the left eye was 6/6, N6. Left eye was normal. Ultrasonography confirmed the presence of a subretinal lesion. A provisional diagnosis of endogenous endophthalmitis in OD was made and the patient was advised urgent surgical intervention. A complete systemic examination which included HIV testing, urine, and blood culture along with a physician evaluation was done.
Figure 1.

(a) Colour fundus photograph of OD at presentation, showing vitreous haze and subretinal abscess at the posterior pole (white arrow). (b) Colour fundus photograph of OD at final follow up, showing scarred subretinal abscess (white star) and persistent subretinal fluid inferiorly (white arrowhead)
The patient underwent 20 G Pars Plana Vitrectomy. Undiluted vitreous aspirate was sent for microbiological tests. The patient received intravitreal Vancomycin (1 mg/0.1ml), Ceftazidime (2.25 mg/0.1 ml), and Voriconazole (50 μg/0.1ml) at the end of the procedure. Microscopy of the wet mount preparation with 10% KOH and Calcofluor white under fluorescent microscope revealed plenty of septate filamentous fungal elements which were branched in acute angle [Fig. 2a]. Examination of the tease mount preparation from the culture revealed conidiophores of variable length, biseriate compactly columnar phialides covering the entire vesicle, which shows morphological characteristics of Aspergillus terreus [Fig. 2b]. In culture, velvety colonies were obtained with a characteristic cinnamon brown color, with brown pigmentation in the reverse [Fig. 3a] A broad ranged panfungal polymerase chain reaction (PCR) targeting the Internal Transcribed Spacer II (ITS II) region was also positive, thereby confirming the presence of fungi in the sample [Fig. 3b]. All other microbiological investigations like blood culture, urine culture, and HIV testing were negative. No active systemic foci of infection was detected.
Figure 2.
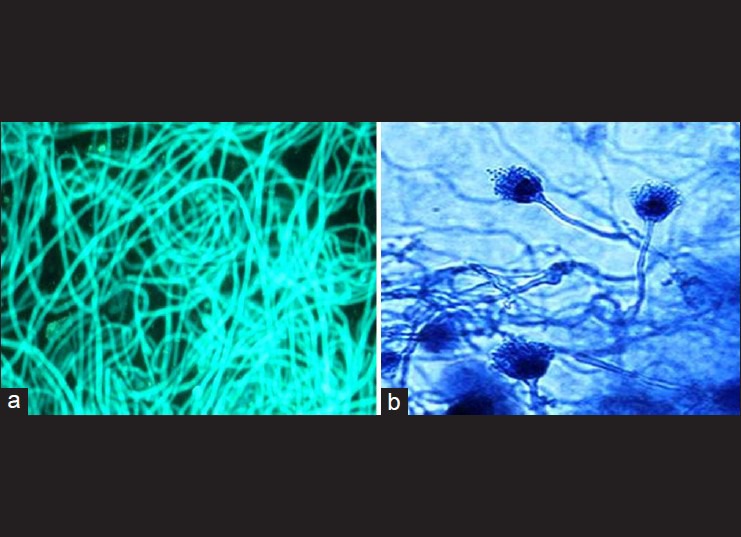
(a) KOH mount prepared from the vitreous aspirate examined under fluorescent microscope after staining with calcofluor white reveals characteristic septate, branched, filamentous fungi (Magnification ×40) (b) Tease mount preparation stained with Lactophenol cotton blue reveals characteristic biseriate sterigmata on dome shaped vesicles characteristic of Aspergillus terreus (magnification ×40)
Figure 3.
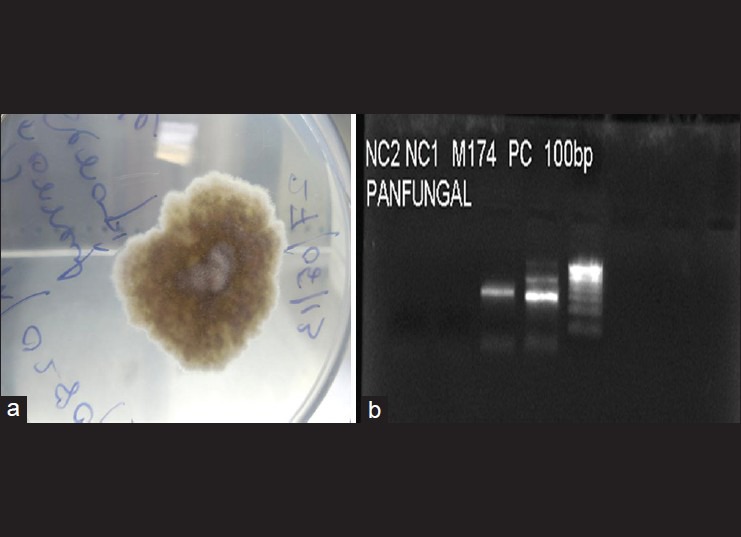
(a) Photograph of the culture plate showing characteristic velvety, cinnamon-coloured colonies of A. terreus (b) Gel picture showing amplified products (ITS 2 region) of a pan-fungal PCR at the appropriate position (255 bp) NC1- negative control is round, NC2- negative control 2nd round PC- positive control, 100 bp molecular ladder
In the postoperative period the patient received six injections of intravitreal Voriconazole. Three weeks following the surgery, he developed total retinal detachment which required revitrectomy with endolaser and silicon oil tamponade. At final follow-up after 2 months, right eye vision was perception of light (PL) only. Anterior chamber was quiet. Vitreous cavity was clear with a macular scar and persistent subretinal fluid inferiorly [Fig. 1b]. The patient was advised resurgery which he refused. He was prescribed oral Voriconazole 200 mg twice daily for 2 months.
Discussion
A terreus is a saprophytic fungus occurring in the soil and is occasionally pathogenic. Out of six reports of A terreus endogenous endophthalmitis [as summarized in Table 1], majority have been associated with immunosupression.[1,2,3,4,5] Only one report by Ng et al.,[6] of A terreus endogenous endophthalmitis in immunocompetent individual exists in literature. Three cases of postoperative and 1 case of posttraumatic endophthalmitis have been reported.[7,8,9] Riddell et al.,[10] have reported the ocular manifestations of endogenous Aspergillus endophthalmitis. Patients present with sudden painful unilateral blurring of vision, variable amount of circumciliary congestion, AC reaction and hypopyon. Fundoscopy reveals vitritis, exudative lesions in the posterior pole, pre and intraretinal hemorrhages. Pseudohypopyon (pre-retinal layering of exudates), pathognomic of Aspergillus endophthalmitis, has been reported. Our patient presented with subretinal abscess in the macular area which eventually formed a scar. A detailed microbiological analysis is necessary in all cases. However, the sensitivity of identifying the organism from vitreous aspirates, PCR, and vitrectomy specimen is 50, 72 and 90% respectively.[6]
Table 1.
Clinical characteristics of patients with Aspergillus terreus endophthalmitis

Systemic and intravitreal Amphotericin-B has been the main stay of treatment of Aspergillus endophthalmitis and has been reported to result in good outcomes.[1,7] However, A terreus has been reported to exhibit resistance to Amphotericin–B in 98% of the isolates, which is a cause of concern. Alternative antifungal like Voriconazole, with an oral bioavailability of 96% and good aqueous and vitreous concentrations, is being used these days. Kramer et al.[4] were the first to report the successful use of intravitreal Voriconazole in A terreus endogenous endophthalmitis. In the present case, though the infection was controlled with intravitreal and systemic Voriconazole, however, the final visual outcome was poor because of the central macular scar. Our patient had no previous ocular trauma, surgery or medical history which could explain the present condition. The exact source of infection could not be determined inspite of our best efforts.
Conclusion
To conclude, our study adds to the body of literature available on A terreus endogenous endophthalmitis. A terreus endogenous endophthalmitis with subretinal abscess usually have a dismal prognosis. A high index of suspicion along with prompt medical and surgical intervention may result in better outcomes.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Dave VP, Majji AB, Suma N, Pappuru RR. A rare case of Aspergillus terreus endogenous endophthalmitis in a patient of acute lymphoid leukemia with good clinical outcome. Eye. 2011;25:1094–6. doi: 10.1038/eye.2011.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalina PH, Campbell RJ. Aspergillus terreus endophthalmitis in a patient with chronic lymphocytic leukemia. Arch Ophthalmol. 1991;109:102–3. doi: 10.1001/archopht.1991.01080010104040. [DOI] [PubMed] [Google Scholar]
- 3.Gross JG. Endogenous Aspergillus-induced endophthalmitis, successful treatment without systemic antifungal medication. Retina. 1992;12:341–5. [PubMed] [Google Scholar]
- 4.Kramer M, Kramer MR, Blau H. Intravitreal voriconazole for the treatment of endogenous Aspergillus endophthalmitis. Ophthalmology. 2006;113:1184–6. doi: 10.1016/j.ophtha.2006.01.059. [DOI] [PubMed] [Google Scholar]
- 5.Bradley JC, George JG, Sarria JC, Kimbrough RC, Mitchell KT. Aspergillus terreus endophthalmitis. Scand J Infect Dis. 2005;37:529–31. doi: 10.1080/00365540510036598. [DOI] [PubMed] [Google Scholar]
- 6.Ng J, Ho S, Krishnan P, Teoh SC. Aspergillus terreus endogenous endophthalmitis in a nonimmuno compromised patient with a history of bronchiectasis. Ocul Immunol Inflamm. 2013;21:231–3. doi: 10.3109/09273948.2012.754907. [DOI] [PubMed] [Google Scholar]
- 7.Das T, Vyas P, Sharma S. Aspergillus terreus postoperative endophthalmitis. Br J Ophthalmol. 1993;77:386–7. doi: 10.1136/bjo.77.6.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garg P, Mahesh S, Bansal AK, Gopinathan U, Rao GN. Fungal infection of sutureless self-sealing incision for cataract surgery. Ophthalmology. 2003;110:2173–7. doi: 10.1016/S0161-6420(03)00861-3. [DOI] [PubMed] [Google Scholar]
- 9.Moinfar N, Smiddy WE, Miller D, Miller D, Herschel K. Posttraumatic Aspergillus terreus endophthalmitis masquerading as dispersed lens fragments. J Cataract Refract Surg. 2007;33:739–40. doi: 10.1016/j.jcrs.2006.11.031. [DOI] [PubMed] [Google Scholar]
- 10.Riddell J, McNeil SA, Johnson MT, Bradley SF, Kazanjian PH, Kauffman CA. Endogenous aspergillus endophthalmitis, report of 3 cases and review of literature. Medicine (Baltimore) 2002;81:311–20. doi: 10.1097/00005792-200207000-00007. [DOI] [PubMed] [Google Scholar]


