Abstract
Aims:
The aim was to evaluate the long-term surgical outcomes of endoillumination assisted scleral buckling (EASB) in primary rhegmatogenous retinal detachment (RRD).
Methods:
Twenty-five eyes of 25 patients with primary RRD and proliferative vitreoretinopathy ≤C2 where any preoperative break could not be localised, were included. All patients underwent 25 gauge endoilluminator assisted rhegma localisation. Successful break determination was followed by cryopexy and standard scleral buckling under surgical microscope. Anatomical and functional outcomes were evaluated at the end of 2 years.
Results:
At least one intraoperative break could be localized in 23 of 25 (92%) eyes. Median age of these patients was 46 years (range: 17-72). Thirteen eyes (56.52%) were phakic, 8 (34.78%) were pseudophakic and 2 (8.6%) were aphakic. Anatomical success (attachment of retina) was achieved in 22 (95.63%) of 23 eyes with EASB. All eyes remained attached at the end of 2 years. Significant improvement in mean visual acuity (VA) was achieved at the end of follow-up (1.09 ± 0.46 log of the minimum angle of resolution [logMAR]) compared with preoperative VA (1.77 ± 0.28 logMAR) (P < 0.001).
Conclusion:
EASB can be considered an effective alternative to vitreoretinal surgery in simple retinal detachment cases with the added advantage of enhanced microscopic magnification and wide field illumination.
Keywords: Endoilluminator, results, scleral buckling
Despite better visual outcomes with scleral buckling (SB) in both phakic and pseudophakic eyes in comparison to vitrectomy, it is declining in popularity among vitreo-retinal surgeons.[1] We describe our results with endoillumination assisted SB (EASB) to achieve retinal attachment.
Methods
This was a prospective interventional case series of consecutive patients who presented to retina services from March 2010 to September 2011 with primary rhegmatogenous retinal detachment (RRD) and proliferative vitreoretinopathy (PVR) grade < C2 where breaks were not localized preoperatively on indirect ophthalmoscopy (IO) with scleral indentation. A written informed consent from all patients was taken and approval from Institutional Review Board was obtained. Patients unwilling to participate and detachments with PVR ≥ C3 grade were excluded. Baseline characteristics including age, etiological diagnosis, duration of detachment, preoperative visual acuity (VA), lens status and PVR grade were recorded.
A 360° peritomy and extraocular muscle bridling was followed by placement of 25 gauge self-retaining endoilluminator either in a quadrant opposite to the suspected break or else in inferotemporal quadrant. Under high microscopic magnification and through volk Reinverting Operating Lens Systemand wide angle viewing system (WAVS), break was localised using indentation, marked and cryopexy was performed[2] [Fig. 1]. Endoilluminator was removed and sclerotomy was closed using 7-0 vicryl. Conventional nondrainage buckling was then performed using silicon-based scleral buckle and encirclage and height of buckle was adjusted according to break buckle relationship under observation of indirect ophthalmoscope. Multiple paracentesis helped stabilise intraocular pressure (IOP); and peritomy was closed after a gentamicin wash. Patients were assessed for anatomical retinal attachment and VA change at 1st day, 1 and 4 weeks, 3 months and 3 monthly thereafter till 2 years. Statistical analysis was performed using the SPSS version 17.0 (SPSS, Chicago, Illionis, USA). Paired t-test was used to evaluate significant change in log of the minimum angle of resolution VA. P < 0.05 was considered as significant.
Figure 1.
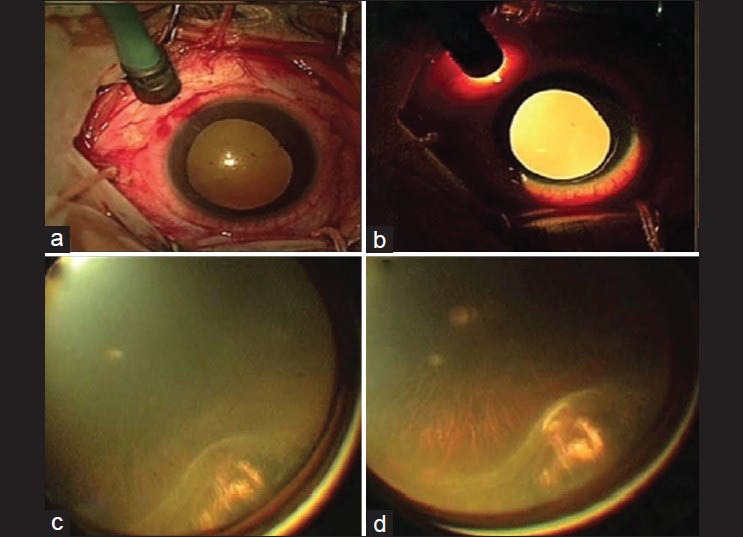
(a) 25-guage self-retaining endoilluminator is placed into the vitreous cavity; (b) Intense internal illumination is obtained after switching on the endoilluminator and switching off the microscope light; (c) the cryo probe is adjusted, so that the break is located at the apex of the indentation and (d) cryopexy is completed
Results
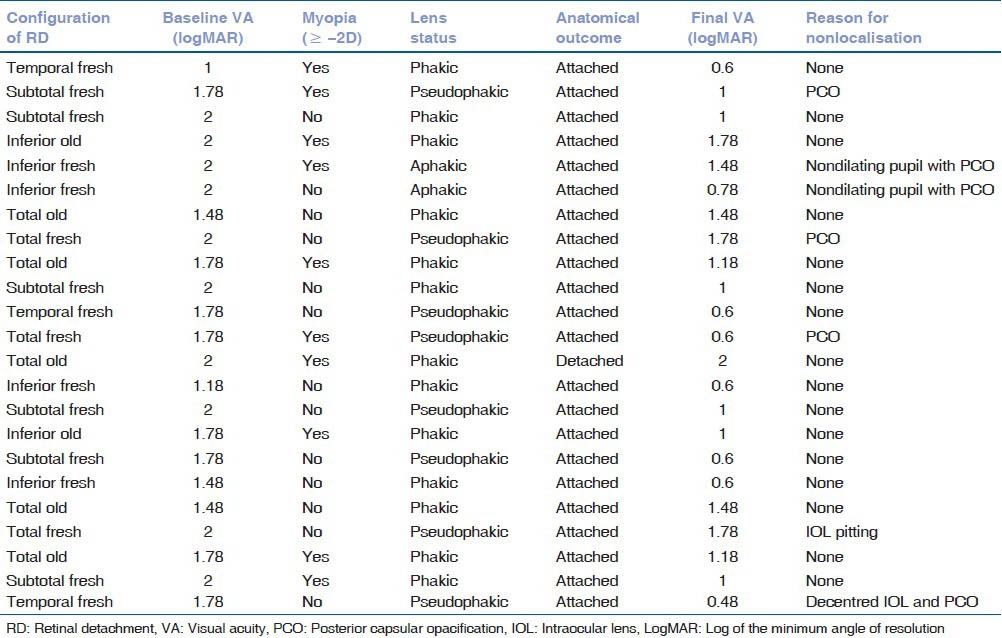
Of 25 eyes (25 patients) recruited at least one intraoperative break could be localized in 23 of 25 (92%) eyes; and multiple breaks (≥ 2) were found in four patients. All 23 patients underwent EASB and pars plana vitrectomy was performed in two patients where break was not localized intraoperatively. Median age of these 23 patients was 46 years (range: 17-72); 14 were males. Among pseudophakic eyes, five of eight eyes had cataract surgery-related problems, which precluded preoperative break localization [Table 1] None of the patients had fix folds in our series; however, three patients had subretinal bands in two quadrants. Initial retinal attachment in EASB group could be achieved in 22 of 23 eyes (95.6%); 23 gauge pars plana vitrectomy and silicon oil injection was performed for eye, which had failed EASB. Retina remained attached in all eyes at 2 years. Mean preoperative and postoperative VA was 1.77 + 0.28 and 1.09 + 0.46 (P < 0.0001, Paired t-test). None developed endoilluminator site break, cataract or significant IOP rise until 2 years follow-up.
Table 1.
Demonstrating baseline clinical characteristics, anatomical outcome and final visual acuity
Discussion
Peroperative determination of retinal tear(s) is time consuming, requires lifting the microscope and wearing the headband of IO and an unobstructed view of peripheral retina. In contrast, chances of missing retinal tear are minimal with vitrectomy due to advanced endoilluminator technology, WAVS and high microscopic magnification; albeit with an increased risk of cataract progression, iatrogenic tears, complications of vitreous substitutes and prolonged time for visual rehabilitation.[3] Several series have reported anatomic retinal attachment rates at 70% to 90% after vitrectomy and 75-91% after SB in cases with RRD.[4] However, redetachment is higher after vitrectomy due to contraction of residual vitreous and epiretinal membrane.[5] EASB combines advantages of both SB and vitrectomy to provide us with good surgical outcomes.
In our series, posterior capsule opacification, small pupil and thin atrophic breaks in far periphery in myopes precluded preoperative rhegma localisation; whereas these factors hampered visibility in EASB minimally. Despite a limited sample size, 95.6% success rate of EASB at 2 years is encouraging and the technique could be used as a standard protocol in selected cases.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Häring G, Wiechens B. Long-term results after scleral buckling surgery in uncomplicated juvenile retinal detachment without proliferative vitreoretinopathy. Retina. 1998;18:501–5. doi: 10.1097/00006982-199806000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Venkatesh P, Garg S. Endoillumination-assisted scleral buckling: A new approach to retinal detachment repair. Retin Physician. 2012;9:34–7. [Google Scholar]
- 3.Heimann H, Bartz-Schmidt KU, Bornfeld N, Weiss C, Hilgers RD, Foerster MH, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: A prospective randomized multicenter clinical study. Ophthalmology. 2007;114:2142–54. doi: 10.1016/j.ophtha.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 4.Heimann H, Zou X, Jandeck C, Kellner U, Bechrakis NE, Kreusel KM, et al. Primary vitrectomy for rhegmatogenous retinal detachment: An analysis of 512 cases. Graefes Arch Clin Exp Ophthalmol. 2006;244:69–78. doi: 10.1007/s00417-005-0026-3. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz SG, Kuhl DP, McPherson AR, Holz ER, Mieler WF. Twenty-year follow-up for scleral buckling. Arch Ophthalmol. 2002;120:325–9. doi: 10.1001/archopht.120.3.325. [DOI] [PubMed] [Google Scholar]


