Sir,
We read the article titled “Surgical outcomes of inverted internal limiting membrane flap technique for large macular hole” by Prabhushanker Mahalingam et al.,[1] recently published in your esteem journal with great interest and would like to congratulate the authors for their work.
We would like to contribute for the above said subject by sharing our experience of treating large/giant macular holes of various etiologies. We have performed vitrectomy, inverted flap internal limiting membrane (ILM) peeling and gas tamponade in 40 patients with the inclusion criteria being holes larger than 600 μm. Most patients had idiopathic macular hole (30 eyes - Fig. 1), others being vitreomacular traction syndrome (VMT) with associated macular hole (5 eyes), post cystoid macular edema (CME) (3 eyes) and post traumatic (2 eyes - Fig. 2) macular holes.
Figure 1.
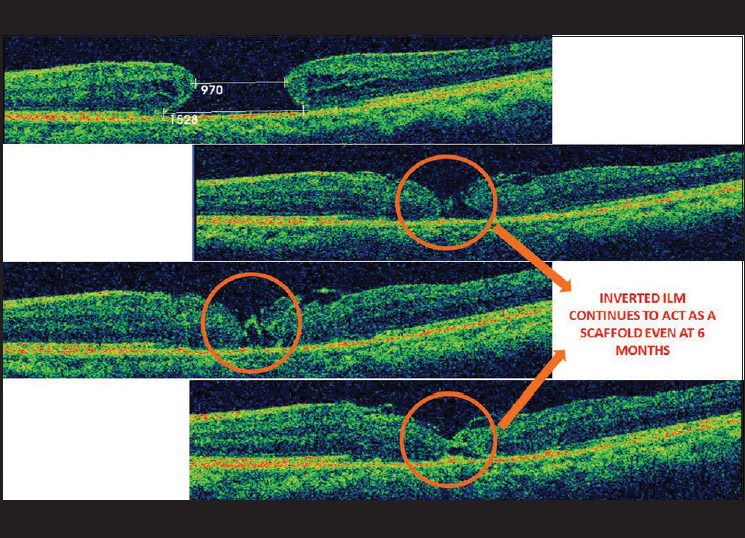
OCT scan of a stage 4 idiopathic macular hole of minimal diameter of 970 microns. The inverted ILM flap is well seen in the immediate and late post operative period persisting upto months with gradual closure of the macular hole
Figure 2.

A large macular hole of size 1.3 mm secondary to blunt trauma, successfully treated with inverted ILM peeling with good visual recovery
Of the 40 patients, 26 were phakic (23 had immature senile cataract, one had complicated cataract, one rosette cataract while the remaining one had a clear lens), and the remaining 14 were pseudophakic. Maximum pre-operative hole diameter was 1532 ± 168 μm. Fifteen of the 26 phakic eyes underwent combined cataract surgery, intraocular lens implantation along with macular hole surgery.
Type 1 macular hole closure was achieved in 100% of the eyes at 1 month follow-up and the holes remained closed at 6 months. Optical coherence tomography showed persistent outer layer defects in the neuro-sensory retina in 5 eyes at the end of 1 month, of which 2 persisted even at 3 months and 6 months.
The functional outcome in terms of visual improvement was noted in 25 eyes (62.5%). An increase of >4 lines was noted in 6 eyes, >2 lines in 13, <2 lines in 6 eyes while the remaining 15 maintained pre-operative vision. The mean pre-operative vision was 6/60 (1.00 LogMAR) which improved to 6/24 (0.602 LogMAR). Eyes with VMT associated macular hole improved the most with post-traumatic macular holes the least as compared to baseline. Visual improvement could be correlated with restoration of inner segment/outer segment (IS/OS) junction and this happened most in patients with VMT associated holes and idiopathic macular holes.
Thus, we can conclude that inverted ILM flap technique is effective in closing large holes, as been shown both in our study as well as the pilot study by Michalewska Z et al.,[2] irrespective of the etiology. Type 1 closure can be achieved in a large number of patients associated with a modest visual improvement.
References
- 1.Mahalingam P, Sambhav K. Surgical outcome of inverted internal limiting membrane flap technique for large macular hole. Indian J Ophthalmol. 2013;61:601–3. doi: 10.4103/0301-4738.121090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25. doi: 10.1016/j.ophtha.2010.02.011. [DOI] [PubMed] [Google Scholar]


