Abstract
A human factors approach to healthcare system redesign emphasizes the involvement of multiple healthcare stakeholders (e.g., patients and families, healthcare providers) in the redesign process. This study explores the experience of multiple stakeholders with collaboration in a healthcare system redesign project. Interviews were conducted with ten stakeholder representatives who participated in the redesign of the family-centered rounds process in a pediatric hospital. Qualitative interview data were analyzed using a phenomenological approach. A model of collaborative healthcare system redesign was developed, which defined four phases (i.e., setup of the redesign team, preparation for meetings, collaboration in meetings, follow-up after meetings) and two outcomes (i.e., team outcomes, redesign outcomes) of the collaborative process. Challenges to multi-stakeholder collaboration in healthcare system redesign, such as need to represent all relevant stakeholders, scheduling of meetings and managing different perspectives, were identified.
Keywords: collaboration, healthcare system redesign, multiple stakeholders, family-centered rounds, pediatric hospital
1. Introduction
Human Factors and Ergonomics (HFE) principles can be used to redesign healthcare work systems so that patient care is safe and effective and meets the needs of patients (Carayon, 2011; Carayon, Wetterneck, et al., 2014; Carayon et al., 2013; Holden et al., 2013; Institute of Medicine Committee on Quality of Health Care in America, 2001; Reid et al., 2005). An overarching HFE principle is to involve “stakeholders,” who affect or are affected by the healthcare work system, in the redesign process (Carayon et al., 2012). Stakeholders have varied values, norms, responsibilities, experience, tasks, skills, and priorities; therefore, they possess heterogeneous perspectives regarding care processes and their quality and safety (Carayon et al., 2012). These different perspectives are invaluable and need to be considered and integrated in any healthcare system redesign process (Manias et al., 2007; Tregunno et al., 2004). In particular, in response to the call for patient/family-centered care (Institute of Medicine Committee on Quality of Health Care in America, 2001), an HFE approach to healthcare system redesign should integrate the perspective of patients and families through their participation in the redesign process (Johnson et al., 2008).
We define “collaborative healthcare system redesign” as the involvement of different stakeholders in the process of healthcare system redesign. Based on Patel et al. (2012), we conceptualize collaborative healthcare system redesign as a complex team process in which stakeholders interact in a single event or series of events to redesign healthcare work systems and processes with the goal of improving patient, employee and organizational outcomes. Studies on the impact of healthcare collaboration on quality of care (Horbar et al., 2001) and patient safety (Clemmer et al., 1999) show that the effectiveness of collaborative initiatives is dependent on the quality of collaboration between stakeholders (Hackman, 1987; Kozlowski and Ilgen, 2006). Inadequate or poor collaboration between stakeholders can limit team progress, create bad feelings, and result in either a “safe solution” degenerating to the lowest common denominator or a “biased solution” ignoring certain perspectives, and therefore, impair the quality of the redesign (Eisenhardt et al., 1997; Katzenbach and Smith, 1994; Kyng, 1998; Wilson and Haines, 1997).
Stakeholder collaboration in healthcare system redesign can be framed in the input-process-output team model (Salas et al., 2007). In a comparison of two multidisciplinary teams performing healthcare failure mode and effects analysis (FMEA), Wetterneck et al. (2009) found that FMEA team performance was associated with team inputs (e.g., team composition, team objectives, organizational support) and processes (e.g., team dynamics, attendance, team progress). In a similar vein, Gray and Wood (1991) proposed a general model of collaboration consisting of three elements: preconditions, process and outcomes. Understanding these three elements and how they influence each other is important to facilitate stakeholder collaboration in healthcare system redesign.
A number of studies have described preconditions of (or input to) collaboration (e.g., Bronstein, 2003; Mattessich and Monsey, 1992). The framework of collaborative work system design by Patel et al. (2012) includes seven categories of factors influencing collaboration: context, support, tasks, interaction processes, teams, individuals, and overarching factors. While the preconditions of collaboration are well documented, the process of collaboration is less understood (Gray and Wood, 1991; Thomson and Perry, 2006). Specifically, no study has examined how multiple stakeholders collaborate in healthcare system redesign. Healthcare involves different groups of stakeholders (e.g., patients and families, healthcare providers, management) who play different roles (e.g., actors, designers, decision makers, influencers) in healthcare system redesign (Dul et al., 2012; Edwards and Jensen, 2014). To optimize collaborative redesign, we need to understand the needs of these stakeholders and the collaborative redesign process through which they can integrate their needs and perspectives (Détienne, 2006; Xie et al., 2012).
The objective of this study is to examine the collaboration of multiple stakeholders in a specific project aimed to redesign the family-centered rounds (FCR) process. Specifically, this study aims to understand (1) the process of collaborative healthcare system redesign and (2) challenges to collaboration associated with the participation of multiple stakeholders.
2. Context of the Study: Collaboration in FCR Process Redesign
FCR are “interdisciplinary work rounds at the bedside in which the patient and family share in the control of the management plan as well as in the evaluation of the process itself” (Sisterhen et al., 2007). During FCR, the healthcare team, consisting of physicians, nurses and other healthcare providers, meets with the hospitalized patient and his/her family to communicate clinical information and, ideally, make joint decisions on daily and discharge care. In the pediatric setting, FCR are recommended as standard practice to engage families in the care of hospitalized children (Committee on Hospital Care and Institute for Patient- and Family-Centered Care, 2012). Various work system barriers (e.g., disruption of workflow, healthcare team size, physical room constraints), however, can hinder family engagement in FCR (Carayon et al., 2011; Mittal et al., 2010). To improve family engagement in FCR, these system barriers need to be addressed and the FCR process and related work system need to be redesigned (Kelly et al., 2013).
FCR were implemented at the American Family Children’s Hospital (AFCH) in Madison, Wisconsin at its inception in 2007. While AFCH leadership was strongly supportive of family-centered care and committed to FCR, gaps existed in the extent to which families were engaged in FCR and effective interventions to improve family engagement in FCR. To bridge these gaps, a five-year research project funded by the Agency for Healthcare Research and Quality was initiated, in which a participatory ergonomics approach was used to redesign the FCR process on one hematology/oncology and one hospitalist service at AFCH. An Intervention Implementation Team (IIT) was formed to facilitate the redesign process, consisting of five researchers (four HFE professionals and one pediatric attending physician) and ten FCR stakeholder representatives:
One parent from the AFCH Patient and Family Advisory Council
A medical administrator at AFCH
Two nurse managers
Two nurses
Two attending physicians
Two senior resident physicians.
Table 1 describes the stages and involvement of researchers and FCR stakeholders in the redesign process. Six IIT meetings were held over a 10-month period (from January to October, 2012). Two researchers (the physician and one of the HFE professionals) facilitated the discussion at each meeting, while the other three researchers recorded meeting notes and managed meeting logistics. In addition, researchers carried out decisions made by the IIT in between meetings and met regularly with the steering committee of the overall research project to report progress and gather feedback. Stakeholder representatives on the IIT were expected to actively participate in the meetings and communicate with their colleagues in between meetings. Other FCR stakeholders who did not participate in the IIT were able to voice their opinions and contribute to the redesign process through different mechanisms, e.g., interviews (Carayon et al., 2011; Carayon, Li, et al., 2014; Kelly et al., 2013), surveys (Xie et al., 2012) and the pilot study of the intervention (Li et al., 2013).
Table 1.
Summary of FCR process redesign
| Timeline | Activities | Participants*
|
||
|---|---|---|---|---|
| R | SR | OS | ||
| Before meeting 1 | - Observe FCR process on different inpatient services | X | ||
| - Interview FCR stakeholders to identify facilitators, barriers and strategies for improving family engagement in FCR | X | X | ||
| - Survey FCR stakeholders to evaluate impact of identified strategies on family engagement in FCR | X | X | ||
|
| ||||
| Meeting 1 | - Share team members’ experience with FCR | X | X | |
| - Review survey data on impact of strategies on family engagement | X | X | ||
| - Categorize strategies into “should be addressed by the intervention”, “might be addressed by the intervention”, and “should not be addressed by the intervention” | X | X | ||
| - Brainstorm intervention ideas for each strategy in the “should be addressed by the intervention” category | X | X | ||
|
| ||||
| Between meetings 1 and 2 | - Summarize proposed intervention ideas | X | ||
| - Survey FCR stakeholders to evaluate feasibility of implementing intervention ideas | X | X | ||
|
| ||||
| Meeting 2 | - Share team members’ experience with proposed intervention ideas | X | X | |
| - Review survey data on feasibility of intervention ideas | X | X | ||
| - Categorize intervention ideas into yes, maybe, no | X | X | ||
| - Select the intervention, i.e., the FCR checklist of best practices for FCR | X | X | ||
|
| ||||
| Between meetings 2 and 3 | - Observe FCR process on different inpatient services | X | ||
| - Review HFE literature on checklist design, implementation and challenges | X | |||
|
| ||||
| Meeting 3 | - Review summary of HFE literature on checklist design | X | X | |
| - Discuss the FCR checklist design (e.g., content, format, roles, workflow) | X | X | ||
|
| ||||
| Between meetings 3 and 4 | - Create prototypes of FCR checklist | X | X | X |
| - Revise prototypes of FCR checklist | X | X | X | |
|
| ||||
| Meeting 4 | - Review summary of HFE literature on checklist implementation | X | X | |
| - Discuss FCR checklist implementation plan (e.g., pilot study) | X | X | ||
|
| ||||
| Between meetings 4 and 5 | - Pilot test prototypes of FCR checklist | X | X | X |
| - Finalize the FCR checklist | X | X | X | |
|
| ||||
| Meeting 5 | - Review findings from pilot study (e.g., lessons learned, data on checklist item performance) | X | X | |
| - Discuss FCR checklist implementation plan (e.g., training) | X | X | ||
|
| ||||
| Between meetings 5 and 6 | - Pilot test final version of FCR checklist | X | X | X |
| - Provide training to healthcare team members | X | X | X | |
| - Hold information sessions with other healthcare providers | X | X | X | |
|
| ||||
| Meeting 6 | - Discuss challenges to implementation of FCR checklist | X | X | |
| - Share team members’ experience as champions | X | X | ||
R=researchers; SR=stakeholder representatives on the IIT; OS=other stakeholders
A checklist of FCR best practices was developed by the IIT and implemented on the two inpatient services in October 2012, along with training and other implementation activities. An evaluation of the impact of the intervention on care processes (e.g., use of the FCR checklist) and patient outcomes (e.g., family/patient engagement) is being conducted. These data will be reported in forthcoming manuscripts.
3. Methods
Using a phenomenological approach (Creswell, 2013; Moustakas, 1994; van Manen, 1990), we conducted semi-structured interviews with the ten stakeholder representatives on the IIT. The goal of the interviews was to explore IIT members’ experience with the collaborative redesign process (or the phenomenon). This exploratory research study aimed to examine “entities from many sides, angles, and perspectives until a unified vision of the essences of a phenomenon or experience is achieved” (Moustakas, 1994).
3.1 Participants
The Institutional Review Board at the University of Wisconsin-Madison approved this study. All ten IIT members representing parents, healthcare team members (e.g., physicians, nurses) and hospital management (e.g., nurse managers, medical administrator) participated voluntarily.
3.2 Data collection
An information sheet was emailed to IIT members with an invitation to participate in the study. One week before the interview, we sent a summary table of the six IIT meetings to the participant to help him/her recall what happened in the meetings. The summary table listed participants attending the meeting, activities performed, and decisions made.
Using a semi-structured interview guide, a team of two researchers conducted face-to-face interviews. At the beginning of the interview, researchers reviewed the summary table with the participant. The participant was then asked to talk about his/her experience with: (1) the collaborative redesign process (e.g., “What was your experience in working with other IIT members in meetings? Pluses? Minuses?”), (2) the participation of different groups of stakeholders (e.g., “What do you think of the participation of the parent/nurses/nurse managers/attending physicians/resident physicians/medical administrator?”), and (3) factors influencing collaboration (e.g., “What was it that facilitated or hindered the collaboration with members of the team?”). Follow-up questions based on key elements of collaboration (e.g., communication, decision making, coordination, learning) (Patel et al., 2012) were asked to fully understand the participant’s views on the collaborative redesign process (e.g., “How did we make decisions on the categorization of intervention ideas in the second meeting?”). Elements of the work system model (e.g., people, tasks, tools and technologies, organization, environment) (Carayon, 2009; Smith and Carayon-Sainfort, 1989) were used to elicit factors influencing collaboration (e.g., “What is it about the physical environment that facilitated or hindered your collaboration?”).
A total of ten interviews were conducted between March and June 2013, i.e. four to seven months after the end of the redesign process. Interviews ranged from 30 to 45 minutes, and were all audio-recorded and transcribed.
3.3 Data Analysis
Using the phenomenological analysis method of Moustakas (1994), we performed a qualitative analysis of the interview transcripts in an inductive way. All researchers on the IIT participated in the iterative data analysis process, which included the following steps:
To fully understand the experience of participants and to “bracket” the preconceptions of researchers regarding the phenomenon, all researchers described their personal experience with the collaborative healthcare system redesign.
Two researchers (AX and PC) read each transcript several times to make sense of the data. While reading the transcripts, marginal notes were taken to keep track of phrases, ideas and concepts that occurred to the researchers.
Two researchers (AX and PC) discussed their perceptions of the data and selected five transcripts from different stakeholders (i.e., transcripts from the parent, one attending physician, one senior resident physician, one nurse manager and one nurse) to create a preliminary list of themes.
One researcher (AX) wrote a summary of the selected transcripts and identified significant statements related to collaborative healthcare system redesign. Another researcher (PC) reviewed the summaries and provided feedback.
One researcher (AX) grouped significant statements into a preliminary list of themes and sub-themes, and discussed it with other researchers (PC, MK, RC and YL).
Steps 4 and 5 were repeated for the rest of the transcripts; the list of themes and sub-themes was finalized.
One researcher (AX) re-read the transcripts to identify links between themes; a model of collaborative healthcare system redesign was created based on the themes and links. Other researchers (PC, MK, RC and YL) reviewed the model and provided feedback.
One researcher (AX) re-read the transcripts and identified challenges to collaboration associated with the participation of multiple stakeholders. Other researchers (PC, MK, RC and YL) reviewed the challenges and provided feedback.
To ensure quality of data analysis and meet the criteria of credibility, dependability and confirmability (Devers, 1999), we used the following strategies:
Searching for negative cases to refine the analysis (credibility, confirmability);
Keeping a reflective journal of data analysis (e.g., changes and modifications to the themes and sub-themes, decisions made during data analysis); this allowed to document how researchers influenced data analysis (dependability, confirmability);
Asking other researchers with broad experience and training in interview and qualitative data analysis to do skeptical peer review of the analysis (dependability, confirmability) (Devers, 1999; Mays and Pope, 2000).
4. Results
4.1 Model of collaborative healthcare system redesign
Figure 1 shows the model of collaborative healthcare system redesign based on significant statements identified from the interviews. The main phases of the collaborative redesign process are: setup of the redesign team, preparation for meetings, collaboration in meetings, and follow-up after meetings. Outcomes of the collaborative redesign process include redesign outcomes and team outcomes.
Figure 1.
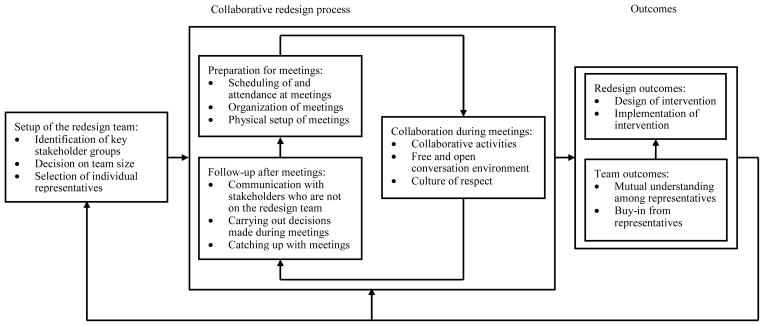
Model of multi-stakeholder collaboration in healthcare system redesign
4.1.1 Setup of the redesign team
The IIT was at the core of the collaborative redesign process. Three issues about the IIT set-up were mentioned in the interviews: identification of key stakeholder groups, decision on team size, and selection of individual representatives.
Heterogeneity was an important criterion for identifying key stakeholders to involve in the redesign process. For instance, the IIT involved stakeholders from different clinical services (e.g., hematology/oncology, hospitalist), which have different patient populations and approaches to FCR:
Different patient populations: “Hematology/oncology is a different population than everyone else … because [patients] are in the hospital for so much longer.”
Different approaches to FCR: “Most of hematology/oncology rounds take place outside of the patient room, which changes the dynamic of how [rounds] work.”
The IIT also involved stakeholders from different professional groups (e.g., physician, nurse) who have different workflows and roles on FCR:
Different workflows: “It was nice to talk about … what might work for doctors and what might work for nurses, because our workflow is very different.”
Different roles on FCR: “The [nurse] managers know, but the floor nurses really know. They are the ones who are actually doing it, as opposed to overseeing it.”
In addition, “the parent brought things to the table that none of the healthcare providers would consider,” while the medical administrator “set the stage for saying that this is a really important issue and this is what we are going to devote energy and resources to.”
Team size was a concern as the number of key stakeholders and the number of representatives from each stakeholder group could be quite high. While “it was not feasible to have everybody at the table,” selected representatives were invited to participate in the IIT. The selection of individual representatives may influence the number of representatives required from each stakeholder group. For instance, “[XXX] was accustomed to being in groups of people and making [herself] heard and understood;” therefore, “[being the only representative of her group on the IIT] was not an issue for her, but may be an issue for someone else.”
4.1.2 Preparation for meetings
Effort was put in the preparation of meetings, including scheduling, organization, and physical setup.
Scheduling of meetings was important as it influenced stakeholder attendance and, therefore, collaboration: “Scheduling was certainly difficult, and nurses could not be there for every meeting.” To allow more stakeholders to attend, the IIT meetings were scheduled far enough ahead of time: “For many of these meetings, we knew [the schedule] far enough ahead.” When scheduling IIT meetings, the following issues were considered:
Total number of meetings: “Six meetings are a lot of meetings. But looking back on it, it is hard to eliminate any one of those meetings.”
Duration of meeting: “Two hours was about right. Four hours was a little on the long side but necessary.”
Interval between meetings: “We had good space in between the meetings.”
Meeting time: “The meetings happened during normal business hours, which is when I am expected to be at work with clinical duties.”
The research team also spent time organizing the meetings, such as defining goals of the redesign process and specific objectives for each meeting, establishing a timeline of the redesign process, and creating meeting agendas: “You had spent a great deal of time clearly thinking about what we want to accomplish and what are our reasonable goals.” In addition, physical setup was planned right before each meeting: “It was nice that we were in a table where everyone was facing each other and having a name card.”
4.1.3 Collaboration in meetings
The core of the redesign process involved collaboration of stakeholder representatives during IIT meetings, which had three elements: collaborative activities, free and open conversation environment, and culture of respect.
Collaborative activities described by stakeholder representatives included the following:
Sharing experience, knowledge, opinions and ideas with each other: “The thought sharing was good. There was pretty good flow of ideas.” For instance, as part of meetings 1 and 2, each stakeholder representative was asked to talk about his/her experience with FCR and intervention ideas. They were also asked to brainstorm intervention ideas for improving the FCR process.
Learning about the FCR process: “I learned a lot about rounds by attending those meetings. The whole process was very instructive. It affected how I worked.” For instance, stakeholder representatives learned about FCR from each other and from observation, interview and survey data (e.g., FCR process map, strategies for improving family engagement in FCR, impact of strategies and feasibility of intervention ideas) that were collected in between meetings.
Discussing differences between clinical services and professional groups: “There was enough opportunity to discuss how hematology/oncology and hospitalist perceived FCR differently.” For instance, at meeting 1, stakeholder representatives discussed differences between hematology/oncology and hospitalist services. By understanding why hematology/oncology teams would not conduct rounds in the patient room (e.g., to protect vulnerable hematology/oncology patients from infection), stakeholder representatives finally agreed on not prescribing the location of rounds but, instead, asking patients and families for their preference on the location.
Making group decisions on the design and implementation of the intervention: “We reviewed different potential interventions. … I felt very comfortable contributing to the group and making decisions.” For instance, at meeting 1, stakeholder representatives discussed strategies for improving family engagement in FCR, and voted to categorize them into “should be addressed by the intervention”, “might be addressed by the intervention”, and “should not be addressed by the intervention”. A similar process was used to categorize intervention ideas.
Collaboration also required a free and open conversation environment, in which stakeholder representatives had an open mind and did not push their own agenda: “There were times when I said something, and someone said, ‘I am not seeing that’ or ‘I do not agree.’ That was totally okay. It was not about ego. It was about how we get to the best product that works for families and providers.” Free and open conversation was depicted as a closed communication loop consisting of:
Expressing: “I felt very comfortable with voicing my concerns, and I think everybody else did too.”
Listening: “Everyone was really listening to everybody else.”
Responding: “Everyone listened to and valued everyone else’s input and actually responded so that it is a discussion”
Considering: “I thought that was very good, say it, hear a reaction, and consider the reaction, oh, maybe there is something there.”
To create a free and open conversation environment during IIT meetings, ground rules (e.g., only one person talks at a time, participate and listen actively, there are no right or wrong answers) were described in the IIT charter and reviewed with stakeholder representatives at the beginning of each meeting.
Finally, it was important to have a culture of respect, which was developed based on the understanding of who the stakeholders were and what they brought to the IIT: “Everybody was respectful of everyone else, both as individuals and the roles they held. … When [XXX] talked, pretty much everyone listened, because she could provide a view that none of the rest of us had. Her viewpoint was valued.”
4.1.4 Follow-up after meetings
Follow-up actions were taken after meetings, such as communication with other stakeholders, carrying out decisions made during meetings, and catching up with people who missed a meeting (see Table 1).
After each IIT meeting, stakeholder representatives communicated with their colleagues to:
Share information learned at the meeting: “In our unit council, we could talk about this is what is happening, be aware that this is coming.” For instance, representatives of nurse managers and nurses regularly presented outcomes of IIT meetings at the nursing councils.
Obtain a broader perspective from other stakeholders: “We did ask families in surveys; so they were represented that way.” For instance, after meeting 2, we summarized proposed intervention ideas, and surveyed different stakeholders to evaluate the feasibility of implementing these intervention ideas.
Researchers were responsible for carrying out decisions made during the meetings and moving things forward in between meetings: “It would have been very frustrating if nothing was happening in between. I thought you did a nice job.” For instance, researchers created prototypes of the FCR checklist and the family preference system after meeting 3 and piloted them after meeting 4 based on stakeholder representatives’ discussion at the meetings.
If a stakeholder representative did not participate in a meeting, different methods were used to help them catch up, such as:
Talking to people who participated in the meeting: “I missed so much on the two that I was not there, but I felt like I could catch up by talking to folks as well.”
Reading meeting minutes: “It was easy to look back at the notes and be able to understand the process that occurred at that meeting.”
4.1.5 Outcomes
The outcomes of the collaborative redesign process were twofold: redesign outcomes and team outcomes.
The main outcomes of the collaborative redesign process were the design and implementation of the intervention to improve family engagement in FCR. The main element of the intervention was a FCR checklist that could be applied across clinical services and worked for healthcare professionals as well as patients and families: “If you make a tool too prohibitive, such that you cannot apply it across many, then it does not help.” In addition, the collaborative redesign process facilitated the implementation of the FCR checklist: “Involving everybody in the redesign from the beginning … made the rollout of the intervention easier and more accepted.”
The collaborative redesign process also resulted in team outcomes, including:
A mutual understanding among stakeholders: “You have everybody, you understand everybody’s workflow at the table.”
Buy-in to the FCR process: “Having all those stakeholders present is huge, because you really do need buy-in from everybody.”
These team outcomes influenced the redesign outcomes. For instance, the buy-in from different groups of stakeholders (e.g., physicians, nurse managers, nurses) was critical to implementing the intervention:
Physicians: “Physicians are huge drivers to make sure FCR are actually completed. If they are not leading this and buying into this and seeing the value of it, then it will not sustain over time.”
Nurse managers: “It was very important that the nurse managers were involved, because they had to promote and support it.”
Nurses: “If nurses were not there, then this probably would not work.”
Team outcomes also influenced the collaborative redesign process through feedback loops: “It was nice to meet multiple times so that you could get used to everyone, build confidence a little bit, build a rapport with everyone … and be able to put your two cents in.”
4.2 Challenges to multi-stakeholder collaboration
The collaborative redesign process faced unique challenges associated with the participation of multiple stakeholders (see Table 2 for a summary).
Table 2.
Challenges to multi-stakeholder collaboration
| Collaboration phases | Challenges |
|---|---|
| Setup of the redesign team |
|
| Preparation for meetings |
|
| Collaboration during meetings |
|
A challenge to setting up the IIT was to represent all relevant stakeholders and involve enough representatives from each stakeholder group while considering team size. The IIT was a large team with ten representatives of different services (e.g., hematology/oncology, hospitalist) and different stakeholder groups (e.g., parents, physicians, nurse managers, nurses): “It was a fairly big team, but you had to have those people. You really needed to have the different attendings, a couple of residents, parents and the managers. Because we are talking about two different units, you needed both managers and both nurses.” However, some stakeholders (e.g., medical specialists, pharmacists) were missing from the IIT: “It would have been not bad to have one of the other specialists, who are running all over the place and are fairly disruptive for the operation to happen in a predictable way for the families.” Some IIT members suggested to have enough nurses and parents to balance the representation of different stakeholder groups: “If you are going to have many physicians, make sure you have multiple nurses there as well as more family members.”
A challenge to preparing for IIT meetings was to accommodate the schedules of different stakeholder representatives. Scheduling of meetings can be extremely challenging when they involve representatives of different stakeholder groups: “The scheduling component was the hardest. But that’s going to be the hardest whenever you have a diverse group like that.”
Two main reasons are:
Different groups of stakeholders had different work schedules: “From the staff nurse perspective, the four-hour meeting was ideal, because it was easier to work into their schedule. … For the physicians and nurse managers, four hours was really hard, because that was a big chunk of the day to do.”
Different groups of stakeholders used different scheduling systems: “One thing that would help all of us for the scheduling is if we all had the same type of scheduling procedure. Some of us use Outlook calendar, some use something else.”
A related challenge was to keep stakeholder representatives consistently attending the IIT meetings: “Having the members there consistently as much as possible is challenging with having so many people from so many places trying to get together.” For instance, only two of the ten stakeholder representatives attended all six IIT meetings, and no IIT meeting had all stakeholder representatives attend. If a stakeholder representative could not attend meetings consistently, it was suggested to have at least one representative from each stakeholder group at each meeting: “Trying to make sure that you have a representative from each group at each meeting is really important.”
A challenge to multi-stakeholder collaboration during IIT meetings was to manage different perspectives and make decisions that would satisfy all stakeholders: “This process involves everybody. You realize not everybody is going to be 100% happy all the time.” This was difficult when stakeholder representatives had different objectives: “If you have one person whose goal is to get patients out as quickly as possible and not necessarily provide excellent care, that detractor can really take away from the group-think process and dominate the group in a negative way.” In order to achieve consensus, stakeholder representatives sometimes had to compromise: “Everybody is there, together picking the important things and ultimately agreeing on them. That is what compromise is.” However, there were also circumstances when consensus could not be achieved: “One of the more uncomfortable discussions that we had was how we sustain [FCR] on weekends when there is less physician staff there. We did make progress, but I do not think we have reached our full potential.” In these cases, stakeholder representatives needed to further discuss their differences and integrate their perspectives: “I can think of one time when [XXX] and I had a question, and she was like, well, no, we cannot. I could have taken that as, oh, I probably should just shut up. But, no, it was more of an opportunity to discuss why we cannot do that or why it is different.”
5. Discussion
This study examined the collaboration of multiple stakeholders in a healthcare system redesign project. A model of collaborative healthcare system redesign was developed, which extends the collaborative redesign process beyond collaboration during meetings and emphasizes the elements of team setup, meeting preparation and follow-up. Our model of collaborative healthcare system redesign has some similarities with the collaborative process of Gray (1989) that has three phases: (1) problem setting (e.g., common definition of problem, commitment to collaborate, identification of stakeholders), (2) direction setting (e.g., establishing ground rules, agenda setting, organizing subgroups), and (3) implementation (e.g., dealing with constituencies, structuring, monitoring the agreement and compliance). While phase three corresponds with stakeholder collaboration during meetings, phases one and two highlight activities that occur before meetings.
On the other hand, our model of collaborative healthcare system redesign goes beyond that of Gray (1989) by stressing the importance of following up after meetings. During the meetings, stakeholder representatives shared their perspectives, discussed their differences, and made decisions as a group. Decisions made during meetings needed to be carried out after the meetings. Meeting outcomes were communicated with other stakeholders after the meetings to collect feedback and gain buy-in from a broader perspective. If stakeholder representatives did not consistently participate in meetings, they could use the time in between meetings to catch up and be prepared for future meetings. Stakeholder collaboration in healthcare system redesign needs to be conceptualized as a continuous process through which stakeholders establish mutual understanding, get involved in and accept the redesign, and further improve their collaboration.
We described challenges to collaboration associated with the participation of multiple stakeholders. Setting up the redesign team is challenging because there is no clear, easy rule for determining team size and identifying the right stakeholders to be involved in the redesign process. Decisions should be made based on the specific healthcare system to be redesigned (e.g., who are the key stakeholders in the healthcare system) and available resources (e.g., who can represent each stakeholder group). Similarly, there is no easy way to schedule meetings with different stakeholders. Organizational support (e.g., providing incentive) is necessary to facilitate attendance to meetings. To manage different perspectives, stakeholders need to establish common ground and clarify their differences (Détienne, 2006), which can be achieved stepwise through the continuous collaborative redesign process.
While all stakeholder representatives performed critical functions in the collaboration process, the involvement of the parent representative was especially essential. As a member of the AFCH Patient and Family Advisory Council, the parent representative was able to communicate with other parents on the council and gather feedback. Despite being the only parent on the IIT, she was able to participate fully in the meetings and collaborate with other IIT members for multiple reasons: (1) she was a professional accustomed to working with groups of people; (2) she had relevant inpatient experience at AFCH and was conversant in the language and practices of clinical staff; (3) she participated in several healthcare quality improvement projects and is an experienced stakeholder advocate; and (4) she was familiar with other IIT members.
Researchers on the IIT also played an important role in the collaboration process. Their involvement is not a necessary condition for successful collaboration in healthcare system redesign. However, someone has to take on the role of coordination and management of the collaborative redesign process. Specifically, a coordinator (or coordination team) needs to perform the following tasks: (1) project management (e.g., designing and planning the collaborative redesign process; establishing the redesign team; scheduling meetings), (2) meeting facilitation (e.g., assuring everyone feels comfortable participating; assuring everyone’s ideas are heard; assuring decisions are made by the team), (3) data collection and analysis (e.g., collecting feedback from stakeholders through observations, interviews and surveys; analyzing and preparing data to be presented at meetings), and (4) intervention development and testing (e.g., creating and piloting prototypes of the intervention; revising the intervention based on feedback from stakeholders). A coordinator also needs to have at the minimum basic knowledge of HFE and the healthcare environment, which are incorporated in the redesign. While a structure (e.g., objectives, timeline, work plan) is important to the collaborative redesign process, a coordinator needs to be flexible and continuously adapt to the needs of the redesign team (Haims and Carayon, 1998).
This study has several limitations. First, we reported a case study focusing on a complex care process at a single, academic children’s hospital, which limits the generalizability of the results to other settings. However, the proposed model of collaborative healthcare system redesign and the challenges to multi-stakeholder collaboration are supported by previous work (Détienne, 2006; Gray, 1989; Patel et al., 2012) and expected to be “generalizable to theoretical propositions” (Yin, 1994). Future research may rely on a multiple case study research design where cases in various contexts are studied and compared to validate the collaboration model. Second, we conducted retrospective interviews to collect data on the experience of stakeholders with collaboration. Compared to concurrent data collection (e.g., naturalistic observation, audio- or video-recording), the validity of data collected by retrospective interviews may be affected by biases and limitations of human cognition (Schwarz and Sudman, 1994). To enhance the validity of retrospective interview data, we used a summary table with activities and decisions for each IIT meeting to help participants recollect what happened in the meetings. This “aided-recall” technique can help with the problem of forgetting, but does not address potential memory distortion (Singleton et al., 1988). Third, this study relies solely on a qualitative research approach and does not provide any quantitative information regarding collaboration. Further research could develop and use survey measures of collaboration and provide a comprehensive analysis by mixing qualitative and quantitative data on collaboration (Creswell, 2009). For instance, our qualitative data suggested a feedback loop from outcomes to the process of collaborative healthcare system redesign. Quantitative data could have been collected at the beginning and end of the redesign process to examine whether stakeholder collaboration was improved through the redesign process; therefore, providing information on the feedback loop in the collaboration model. Finally, it might be interesting to know if different groups of stakeholders have different opinions regarding their collaboration. However, due to the small number of participants, we de-identified the interview data and did not report the specific stakeholder group for various quotes.
6. Conclusion
There is growing recognition among healthcare professionals, leaders and researchers that healthcare stakeholders, including patients and their families, should be actively involved in healthcare system redesign. This study explores the experience of multiple stakeholders with collaboration in FCR redesign. A model of collaborative healthcare system redesign was developed, and challenges to collaboration associated with the participation of multiple stakeholders were described. To facilitate future collaborative redesign efforts, work system factors (Carayon, 2009; Smith and Carayon-Sainfort, 1989) influencing collaboration (e.g., experience and aspiration of stakeholder representatives, culture of the redesign team, use of communication technologies, physical environment of meetings) should be identified and related to the collaborative redesign process. Strategies and principles for guiding collaborative healthcare system redesign (e.g., establishing informal relationships among stakeholder representatives, creating a culture of collaboration, securing management support, designing and managing the collaborative redesign process) should also be developed, which should facilitate further implementation and dissemination of HFE in healthcare (Carayon, 2010).
Highlights.
We explored stakeholder experience with collaboration in healthcare system redesign.
We proposed a model of stakeholder collaboration in healthcare system redesign.
We identified challenges to stakeholder collaboration in healthcare system redesign.
Acknowledgments
This study was supported by an AHRQ Health Services Research Demonstration and Dissemination grant, R18 HS018680 (Cox, PI), and the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant # 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS) grant # 9U54TR000021. The authors would like to thank Betty Chewning, Michael J. Smith, Tosha B. Wetterneck and Douglas A. Wiegmann for their comments and feedback, and Ann Schoofs Hundt for her help with some of the interviews.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bronstein LR. A model for interdisciplinary collaboration. Social Work. 2003;48:297–306. doi: 10.1093/sw/48.3.297. [DOI] [PubMed] [Google Scholar]
- Carayon P. The balance theory and the work system model … Twenty years later. International Journal of Human-Computer Interaction. 2009;25:313–327. [Google Scholar]
- Carayon P. Human factors in patient safety as an innovation. Applied Ergonomics. 2010;41:657–665. doi: 10.1016/j.apergo.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2. CRC Press; Boca Raton, FL: 2011. [Google Scholar]
- Carayon P, Alyousef B, Xie A. Human factors and ergonomics in health care. In: Salvendy G, editor. Handbook of Human Factors and Ergonomics. 4. John Wiley and Sons; New York: 2012. pp. 1574–1595. [Google Scholar]
- Carayon P, DuBenske LL, McCabe BC, Shaw B, Gaines ME, Kelly MM, Orne J, Cox ED. Work system barriers and facilitators to family engagement in rounds in a pediatric hospital. In: Albolino S, Bagnara S, Bellandi T, Llaneza J, Rosal-Lopez G, Tartaglia R, editors. Healthcare Systems Ergonomics and Patient Safety 2011: Proceedings on the International Conference on Healthcare Systems Ergonomics and Patient Safety (HEPS 2011) CRC Press; Oviedo, Spain: 2011. [Google Scholar]
- Carayon P, Li Y, Kelly MM, DuBenske LL, Xie A, McCabe BC, Orne J, Cox ED. Stimulated recall methodology for assessing work system barriers and facilitators in family-centered rounds in a pediatric hospital. Applied Ergonomics. 2014;45:1540–1546. doi: 10.1016/j.apergo.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, Gurses AP. Human factors systems approach to healthcare quality and patient safety. Applied Ergonomics. 2014;45:14–25. doi: 10.1016/j.apergo.2013.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Quality and Safety. 2013;23:196–205. doi: 10.1136/bmjqs-2013-001812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemmer TP, Spuhler VJ, Oniki TA, Horn SD. Results of a collaborative quality improvement program on outcomes and costs in a tertiary critical care unit. Critical Care Medicine. 1999;27:1768–1774. doi: 10.1097/00003246-199909000-00011. [DOI] [PubMed] [Google Scholar]
- Committee on Hospital Care Institute for Patient- Family-Centered Care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129:394–404. doi: 10.1542/peds.2011-3084. [DOI] [PubMed] [Google Scholar]
- Creswell JW. Research Design - Qualitative, Quantitative, and Mixed Methods Approaches. 3. Sage Publications; Thousand Oaks, CA: 2009. [Google Scholar]
- Creswell JW. Qualitative Inquiry and Research Design: Choosing among Five Approaches. Sage Publications; Thousand Oaks, CA: 2013. [Google Scholar]
- Détienne F. Collaborative design: Managing task interdependencies and multiple perspectives. Interacting with Computers. 2006;18:1–20. [Google Scholar]
- Devers KJ. How will we know “good” qualitative research when we see it? Beginning the dialogue in health services research. Health Services Research. 1999;34:1153–1188. [PMC free article] [PubMed] [Google Scholar]
- Dul J, Bruder R, Buckle P, Carayon P, Falzon P, Marras WS, Wilson JR, van der Doelen B. A strategy for human factors/ergonomics: developing the discipline and profession. Ergonomics. 2012;55:377–395. doi: 10.1080/00140139.2012.661087. [DOI] [PubMed] [Google Scholar]
- Edwards K, Jensen PL. Design of systems for productivity and well being. Applied Ergonomics. 2014;45:26–32. doi: 10.1016/j.apergo.2013.03.022. [DOI] [PubMed] [Google Scholar]
- Eisenhardt KM, Kahwajy JL, Bourgeois LJ., III Conflict and strategic choice: How top management teams disagree. California Management Review. 1997;39:42–62. [Google Scholar]
- Gray B. Collaborating: Finding Common Ground for Multiparty Problems. Jossey-Bass; San Francisco, CA: 1989. [Google Scholar]
- Gray B, Wood DJ. Collaborative alliances: moving from practice to theory. The Journal of Applied Behavioral Science. 1991;27:3–22. [Google Scholar]
- Hackman JR. The design of work team. In: Lorsch J, editor. Handbook of Organizational Behavior. Prentice Hall; New York: 1987. pp. 315–342. [Google Scholar]
- Haims MC, Carayon P. Theory and practice for the implementation of ‘in-house’, continuous improvement participatory ergonomic programs. Appl Ergon. 1998;29:461–472. doi: 10.1016/s0003-6870(98)00012-x. [DOI] [PubMed] [Google Scholar]
- Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, Rivera-Rodriguez AJ. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56:1669–1686. doi: 10.1080/00140139.2013.838643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horbar JD, Rogowski J, Plsek PE, Delmore P, Edwards WH, Hocker J, Kantak AD, Lewallen P, Lewis W, Lewit E, McCarroll CJ, Mujsce D, Payne NR, Shiono P, Soll RF, Leahy K, Carpenter JH. Collaborative quality improvement for neonatal intensive care. Pediatrics. 2001;107:14–22. doi: 10.1542/peds.107.1.14. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press; Washington, DC: 2001. [Google Scholar]
- Johnson BH, Abraham M, Conway J, Simmons L, Edgman-Levitan S, Sodomka P, Schlucter J, Ford D. Partnering with Patients and Families to Design a Patient- and Family-Centered Health Care System: Recommendations and Promising Practices. Institute for Family-Centered Care; Bethesda, MD: 2008. [Google Scholar]
- Katzenbach JR, Smith DK. The Wisdom of Teams: Creating the High-Performance Organization. Harvard Business School Press; Boston, MA: 1994. [Google Scholar]
- Kelly MM, Xie A, Carayon P, Dubenske LL, Ehlenbach ML, Cox ED. Strategies for improving family engagement during family-centered rounds. Journal of Hospital Medicine. 2013;8:201–207. doi: 10.1002/jhm.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozlowski SWJ, Ilgen DR. Enhancing the Effectiveness of Work Groups and Teams. Psychological Science in the Public Interest. 2006;7:77–124. doi: 10.1111/j.1529-1006.2006.00030.x. [DOI] [PubMed] [Google Scholar]
- Kyng M. Users and computers: a contextual approach to design of computer artifacts. Scandinavian Journal of Information Systems. 1998;10:7–43. [Google Scholar]
- Li Y, Carayon P, Xie A, Kelly MM, Cartmill R, Wetterneck TB, Cox ED. Work system challenges to implementing a family-centered rounds checklist. 2013 International Symposium on Human Factors and Ergonomics in Health Care: Advancing the Cause; Baltimore, MD. 2013. [Google Scholar]
- Manias E, Claydon-Platt K, McColl GJ, Bucknall TK, Brand CA. Managing complex medication regimens: Perspectives of consumers with osteoarthritis and healthcare professionals. The Annals of Pharmacotherapy. 2007;41:764–771. doi: 10.1345/aph.1H623. [DOI] [PubMed] [Google Scholar]
- Mattessich PW, Monsey BR. A Review of Research Literature on Factors Influencing Successful Collaboration. Amherst H. Wilder Found; St. Paul, MN: 1992. Collaboration: What Makes It Work. [Google Scholar]
- Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. British Medical Journal. 2000;320:50–52. doi: 10.1136/bmj.320.7226.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal VS, Sigrest T, Ottolini MC, Rauch D, Lin H, Kit B, Landrigan CP, Flores G. Family-centered rounds on pediatric wards: A PRIS network survey of US and Canadian hospitalists. Pediatrics. 2010;126:37–43. doi: 10.1542/peds.2009-2364. [DOI] [PubMed] [Google Scholar]
- Moustakas C. Phenomenological Research Methods. Sage Publications; Thousand Oaks, CA: 1994. [Google Scholar]
- Patel H, Pettitt M, Wilson JR. Factors of collaborative working: A framework for a collaboration model. Applied Ergonomics. 2012;43:1–26. doi: 10.1016/j.apergo.2011.04.009. [DOI] [PubMed] [Google Scholar]
- Reid PR, Compton WD, Grossman JH, Fanjiang G. A New Engineering/Health Care Partnership. The National Academies Press; Washington, D.C: 2005. Building a Better Delivery System. [PubMed] [Google Scholar]
- Salas E, Stagl KC, Burke CS, Goodwin GF. Fostering team effectiveness in organizations: toward an integrative theoretical framework. Nebraska Symposium on Motivation. 2007;52:185–243. [PubMed] [Google Scholar]
- Schwarz N, Sudman S. Autobiographical Memory and the Validity of Retrospective Reports. Springer-Verlag; New York: 1994. [Google Scholar]
- Singleton RJ, Straits BC, Straits MM, McAllister RJ. Approaches to Social Research. Oxford University Press; New York, NY: 1988. [Google Scholar]
- Sisterhen LL, Blaszak RT, Woods MB, Smith CE. Defining family-centered rounds. Teaching and Learning in Medicine. 2007;19:319–322. doi: 10.1080/10401330701366812. [DOI] [PubMed] [Google Scholar]
- Smith MJ, Carayon-Sainfort P. A balance theory of job design for stress reduction. International Journal of Industrial Ergonomics. 1989;4:67–79. [Google Scholar]
- Thomson AM, Perry JL. Collaboration processes: inside the black box. Public Administration Review. 2006;66:20–32. [Google Scholar]
- Tregunno D, Ross Baker G, Barnsley J, Murray M. Competing values of emergency department performance: Balancing multiple stakeholder perspectives. Health Services Research. 2004;39:771–791. doi: 10.1111/j.1475-6773.2004.00257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Manen M. Researching Lived Experience. State University of New York Press; New York: 1990. [Google Scholar]
- Wetterneck TB, Hundt AS, Carayon P. FMEA team performance in health care: A qualitative analysis of team member perceptions. Journal of Patient Safety. 2009;5:102–108. doi: 10.1097/PTS.0b013e3181a852be. [DOI] [PubMed] [Google Scholar]
- Wilson JR, Haines HM. Participatory ergonomics. In: Salvendy G, editor. Handbook of Human Factors and Ergonomics. John Wiley & Sons; New York: 1997. pp. 490–513. [Google Scholar]
- Xie A, Carayon P, Kelly MM, Li Y, Cartmill R, DuBenske LL, Brown RL, Cox ED. Managing different perspectives in the redesign of family-centered rounds in a pediatric hospital. Proceedings of the Human Factors and Ergonomics Society 56th Annual Meeting; Santa Monica, CA: The Human Factors and Ergonomics Society; 2012. pp. 1733–1737. [Google Scholar]
- Yin RK. Case Study Research: Design and Methods. 2. Sage Publications; Thousand Oaks, CA: 1994. [Google Scholar]


