Abstract
The present studies examined the toxic interaction between the non-coxib celecoxib derivative OSU-03012 and phosphodiesterase 5 (PDE5) inhibitors, and to determine the roles of endoplasmic reticulum stress response regulators in cell survival. PDE5 inhibitors interacted in a greater than additive fashion with OSU-03012 to kill parental glioma and stem-like glioma cells. Knock down of the endoplasmic reticulum stress response proteins IRE1 or XBP1 enhanced the lethality of OSU-03012, and of [OSU-03012 + PDE5 inhibitor] treatment. Pan-caspase and caspase 9 inhibition did not alter OSU-03012 lethality but did abolish enhanced killing in the absence of IRE1 or XBP1. Expression of the mitochondrial protective protein BCL-XL or the caspase 8 inhibitor c-FLIP-s, or knock down of death receptor CD95 or the death receptor – caspase 8 linker protein FADD, suppressed killing by [OSU-03012 + PDE5 inhibitor] treatment. CD95 activation was blocked by the nitric oxide synthase inhibitor L-NAME. Knock down of the autophagy regulatory proteins Beclin1 or ATG5 protected cells from OSU-03012 and of [OSU-03012 + PDE5 inhibitor] toxicity. Knock down of IRE1 enhanced OSU-03012/[OSU-03012 + PDE5 inhibitor] –induced JNK activation and inhibition of JNK suppressed the elevated killing caused by IRE1 knock down. Knock down of CD95 blunted JNK activation. Collectively our data demonstrates that PDE5 inhibitors recruit death receptor signaling to enhance OSU-03012 toxicity in GBM cells.
Introduction
OSU-03012, a derivative of the drug Celecoxib, lacks COX2 inhibitory activity (1,2). COX2 is over-expressed in several tumor types and drugs that inhibit COX2 i.e. Celecoxib have been shown to cause tumor cell specific increases in cell death, and that are also associated with a lower rate of growth (3–6). Prolonged treatment with COX2 inhibitors can reduce the incidence of developing cancer, which, in addition, argues that COX2 inhibitors have cancer preventative effects (7,8). Expression levels of COX2 do not simplistically correlate with tumor cell sensitivity to COX2 inhibitors (9,10). Thus, COX2 inhibitors must have additional cellular targets to explain their anti-tumor biological actions.
Compared to the parent Celecoxib, OSU-03012 has a similar level of bio-availability in pre-clinical animal models and has an order of magnitude greater efficacy at killing tumor cells (11–13). Based on encouraging pre-clinical data OSU-03012 is currently undergoing Phase I evaluation in patients with solid and liquid tumors. Studies from the initial Phase I trial noted that the “C max after single dose was dose-proportional but high PK variability was observed, likely due to inadequate disintegration and dissolution of the formulation in the stomach (14).” The C max of OSU-03012 in plasma after 1 day at the MTD of 800 mg BID was ~1 μM. After 28 days of treatment the C max was ~2 μM. Thus, even considering the problems associated with OSU-03012 drug absorption in patients, our use of OSU-03012 in prior studies and in the present manuscript of 1.0–2.0 μM of the drug in vitro is clinically relevant.
Initially, the tumoricidal effects of OSU-03012 in transformed cells were argued to be via inhibition of the enzyme PDK-1, within the PI3K pathway (1). And, in the low micro-Molar range, it has been shown that OSU-03012 can lower AKT phosphorylation. In our previous studies, inhibition of either ERK1/2 or phosphatidyl-inositol 3 kinase signaling enhanced the toxicity of OSU-03012 (11–13,15). However, our data has also argued that OSU-03012 toxicity, and in addition its radiosensitizing effects, could not simplistically be attributed only to suppression of AKT signaling (12,13,15). Specifically, our prior studies have argued that OSU-03012 killed tumor cells through mechanisms which involved endoplasmic reticulum (ER) stress signaling through activation of PKR-like endoplasmic reticulum kinase (PERK), down-regulation of the HSP70 family chaperone BiP/GRP78, and a caspase-independent form of cell death (11–13,15).
ER stress signaling is mediated by three proximal sensors, PERK, the IRE1 (inositol-requiring protein 1α)/XBP1 (X-box binding protein 1) system and ATF6 (activating transcription factor 6). Previously we demonstrated that knock down of PERK suppressed OSU-03012 toxicity however this effect appeared to be only partially eiF2α dependent (12,13). IRE1 is the oldest and most conserved branch of the unfolded protein response (UPR)/ER stress response in metazoans (16). IRE1 contains both a kinase domain and an endoribonuclease activity. Dimerization and autophosphorylation of IRE1 results in activation of the endonuclease activity, causing alternative splicing of XBP1 mRNA and expression of the active XBP1 transcription factor (17). It has also been noted that IRE1 can have a more relaxed specificity for mRNA substrates, with evolutionary similarity to the actions of RNase L, and that in an XBP1 –independent fashion reduces mRNA levels (18,19). This form of IRE1 biology was called regulated IRE1-dependent degradation (or RIDD) (18,19). In theory, signaling by PERK and by RIDD should mediate the survival of stressed cells, by reducing protein levels. But, alternatively, RIDD could also possibly facilitate death of ER stressed cells (20). The IRE1-like endonuclease RNase L is a highly active interferon –inducible RNase and the level to which RNase L is expressed regulates survival/death decisions in ER stressed cells (21). Thus low amounts of IRE1 activity could promote survival, with higher levels of activity promoting cell death.
Tumors of the brain are notoriously difficult to control. Untreated adult glioblastoma (GBM) patients have a mean survival of several months that is only prolonged up to 12–16 months by aggressive therapeutic intervention. New therapeutic approaches that could translate to the clinic for this malignancy are urgently required. In two recently published studies we demonstrated that phosphodiesterase 5 (PDE5) inhibitors enhanced the toxicity of standard of care chemotherapies in bladder and pediatric CNS tumors (22, 23). In the present studies, we determined whether PDE5 inhibitors interacted with OSU-03012 to kill glioma cells and we defined the molecular mechanisms by which ER stress effector pathways regulated OSU-03012 toxicity.
Materials and Methods
Materials
Phospho-/total- antibodies were purchased from Cell Signaling Technologies (Danvers, MA) and Santa Cruz Biotech. (Santa Cruz, CA). The Anti-CD95 antibody [DX3] (ab25638) was from Abcam (Cambridge, MA). All drugs, including OSU-03012, were purchased from Selleckchem (Houston, TX) (Figure 1A). Commercially available validated short hairpin RNA molecules to knock down RNA/protein levels were from Qiagen (Valencia, CA). At least two different validated siRNA molecules were independently used to confirm the effects observed were not due to non-specific effects. Antibody reagents, other kinase inhibitors, caspase inhibitors cell culture reagents, and non-commercial recombinant adenoviruses have been previously described. Previously characterized semi-established GBM5/GBM6/GBM12/GBM14 glioblastoma cells were supplied by Dr. C.D. James (University of California, San Francisco) and Dr. J.N. Sarkaria (Mayo Clinic, Rochester MN) and were not further characterized by ourselves (24). The primary human GBM isolates (patient 1; patient 2; patient 3) were obtained/isolated from disgarded tumor tissue after standard of care surgery. Patients had previously given informed consent under an IRB protocol to the use of tumor tissue. Tumor samples were made anonymous of all patient identifiers by the VCU TDAAC prior to hand-over to the Dent laboratory.
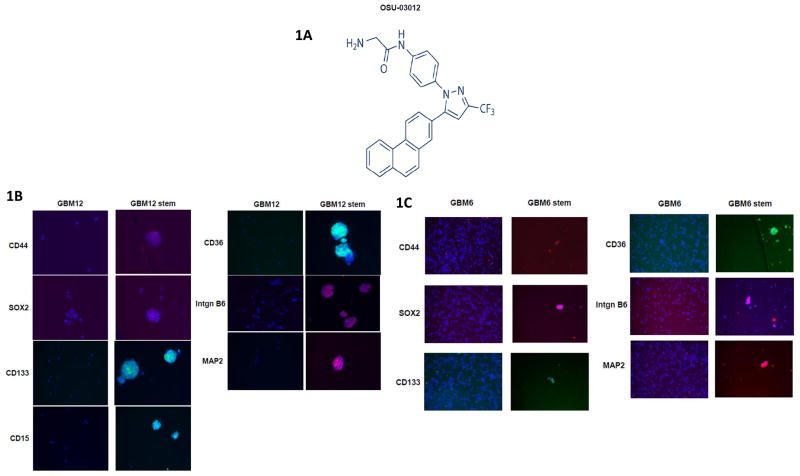
Figure 1. OSU-03012 and characterization of stem-like glioma cells.<.
br>(A) The chemical structure of OSU-03012. (B) and (C) Parental GBM6/12 cells were cultured in StemCell Technologies NeuroCult NS-A Basal Medium supplemented with 20 μg/ml bFGF, 20 μg/ml EGF and 2 mM heparin. CD133+ glioma cells from this population were isolated by fluorescence-activated cell sorting analysis. Cells grew as neurospheres and were characterized for stem cell markers: CD36; integrin α6; CD133; Nestin; CD15; SOX2; CD44; MAP-2; GFAP (n = 3).
Methods
Cell culture and in vitro exposure of cells to drugs
All fully established cancer lines were cultured at 37 °C (5% (v/v CO2) in vitro using RPMI supplemented with 10% (v/v) fetal calf serum and 10% (v/v) Non-essential amino acids. All primary human GBM cells were cultured at 37 °C (5% (v/v) CO2) in vitro using RPMI supplemented with 2% (v/v) fetal calf serum and 10% (v/v) Non-essential amino acids at 37 °C (5% (v/v CO2). GBM5/6/12/14 stem cells were cultured in StemCell Technologies NeuroCult NS-A Basal Medium supplemented with 20 μg/ml bFGF, 20 μg/ml EGF and 2 mM heparin. CD133+ glioma cells from this population were isolated by fluorescence-activated cell sorting analysis. Cells e.g. GBM12, grew as neurospheres and were characterized for multiple stem cell markers, including CD44, SOX2, CD133, CD15, CD36, Integrin B6 and MAP2 (Figure 1B). Neurosphere GBM cells had an approximate 10-fold greater tumorigenicity in vivo than parental wild type GBM cells (data not shown). For short-term cell killing assays and immunoblotting, cells were plated at a density of 3 × 103 per cm2 and 24h after plating were treated with various drugs, as indicated. In vitro small molecule inhibitor treatments were from a 100 mM stock solution of each drug and the maximal concentration of Vehicle (DMSO) in media was 0.02% (v/v). Cells were not cultured in growth factor free media during any study.
Cell treatments, SDS-PAGE and Western blot analysis
Cells were treated with various drug concentrations, as indicated in the Figure legends. Samples were isolated at the indicated times and SDS PAGE and immunoblotting was performed as described in refs 11–13,15. Blots were observed by using an Odyssey IR imaging system (LI-COR Biosciences, Lincoln, NE).
Recombinant adenoviral vectors; infection in vitro
We generated and purchased previously noted recombinant adenoviruses as per refs 11–13,15. Cells were infected with these adenoviruses at an approximate m.o.i. as indicated in the Figure/Legend (usually an moi of 50). Cells were incubated for 24 h to ensure adequate expression of transduced gene products prior to drug exposures.
Detection of cell death by Trypan Blue assay
Cells were harvested by trypsinization with Trypsin/EDTA for ~10 min at 37 °C. Harvested cells were combined with the culture media containing unattached cells and the mixture centrifuged (800 rpm, 5 min). Cell pellets were resuspended in PBS and mixed with trypan blue agent. Viability was determined microscopically using a hemocytometer (11–13,15). Five hundred cells from randomly chosen fields were counted and the number of dead cells was counted and expressed as a percentage of the total number of cells counted. Cell killing was confirmed using the Sceptor instrument (Millipore, Billerica MA) which measured tumor cell size/sub G1 DNA as an indication of tumor cell viability.
Soft agar colony formation assay
Free floating GBM5/6/12/14 stem cells were triturated to form single cells and were plated into soft agar in sextuplicate using established procedures (500–1000 cells per 60 mm dish) (25). Cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Twenty four h after drug treatment the plates were washed with drug free media and the cover media was replaced with drug free media. Colonies were permitted to form over the following 20 days, after which they were stained and colonies counted.
Colony formation assay
Tumor cells plated as single cells (250–4,000 cells/well) in sextuplicate were treated with OSU-03012 (OSU 0.5–2.0 nM) and/or sildenafil (SIL, 0.5–2.0 μM) at a fixed concentration ratio for 24h, after which the media was removed and replaced with drug free media. Colonies were permitted to form for the following 10–14 days. Colonies were fixed, stained and counted (> 50 cells per colony).
Assessment of autophagy
Cells were transfected with a plasmid to express a green fluorescent protein (GFP) and red fluorescent protein (RFP) tagged form of LC3 (ATG8). For analysis of cells transfected with the GFP-RFP-LC3 construct, the GFP/RFP -positive vesicularized cells were examined under the X40 objective of a Zeiss Axiovert fluorescent microscope.
Plasmid transfection
Plasmids
Cells were plated as described above and 24 h after plating, transfected. Plasmids (0.5 μg) expressing a specific mRNA or appropriate vector control plasmid DNA was diluted in 50 μl serum-free and antibiotic-free medium (1 portion for each sample). Concurrently, 2 μl Lipofectamine 2000 (Invitrogen), was diluted into 50 μl of serum-free and antibiotic-free medium. Diluted DNA was added to the diluted Lipofectamine 2000 for each sample and incubated at room temperature for 30 min. This mixture was added to each well/dish of cells containing 200 μl serum-free and antibiotic-free medium for a total volume of 300 μl and the cells were incubated for 4h at 37°C. An equal volume of 2X medium was then added to each well. Cells were incubated for 48h, then treated with drugs. To assess transfection efficiency of plasmids we used a plasmid to express GFP and defined the percentage of cells being infected as the percentage of GFP+ cells. For all cell lines the infection efficiency was > 70%.
siRNA
Cells were plated in 60 mm dishes from a fresh culture growing in log phase as described above, and 24h after plating transfected. Prior to transfection, the medium was aspirated and 1 ml serum-free medium was added to each plate. For transfection, 10 nM of the annealed siRNA, the positive sense control doubled stranded siRNA targeting GAPDH or the negative control (a “scrambled” sequence with no significant homology to any known gene sequences from mouse, rat or human cell lines) were used (predominantly Qiagen, Valencia, CA; occasional alternate siRNA molecules were purchased from Ambion, Inc., Austin, Texas). At least two different validated siRNA molecules were independently used to confirm the effects observed were not due to non-specific effects. Ten nM siRNA (scrambled or experimental) was diluted in serum-free media. Four μl Hiperfect (Qiagen) was added to this mixture and the solution was mixed by pipetting up and down several times. This solution was incubated at room temp for 10 min, then added drop-wise to each dish. The medium in each dish was swirled gently to mix, then incubated at 37 °C for 2h. One ml of 10% (v/v) serum-containing medium was added to each plate, and cells were incubated at 37 °C for 24–48h before re-plating (50 × 103 cells each) onto 12-well plates. Cells were allowed to attach overnight, then treated with drugs (0–48h). Trypan blue exclusion assays and SDS PAGE/immunoblotting analyses were then performed at the indicated time points.
Data analysis
Comparison of the effects between various in vitro drug treatments was performed after analysis of variance using the Student’s t test. Differences with a p value of <0.05 were considered statistically significant. Experiments shown are the means of multiple individual points from multiple studies (± S.E.M.). Median dose-effect isobologram colony-formation analyses to determine synergism of drug interaction were performed according to the methods of Chou and Talalay using the CalcuSyn program for Windows (Biosoft, Cambridge, UK). Cells were treated with agents at an escalating fixed concentration drug dose. A combination index of <1.00 indicates synergy of interaction between the two drugs; a combination index of 1.00 indicates an additive interaction; a combination index (CI) value of >1.00 indicates antagonism of action between the agents.
Results
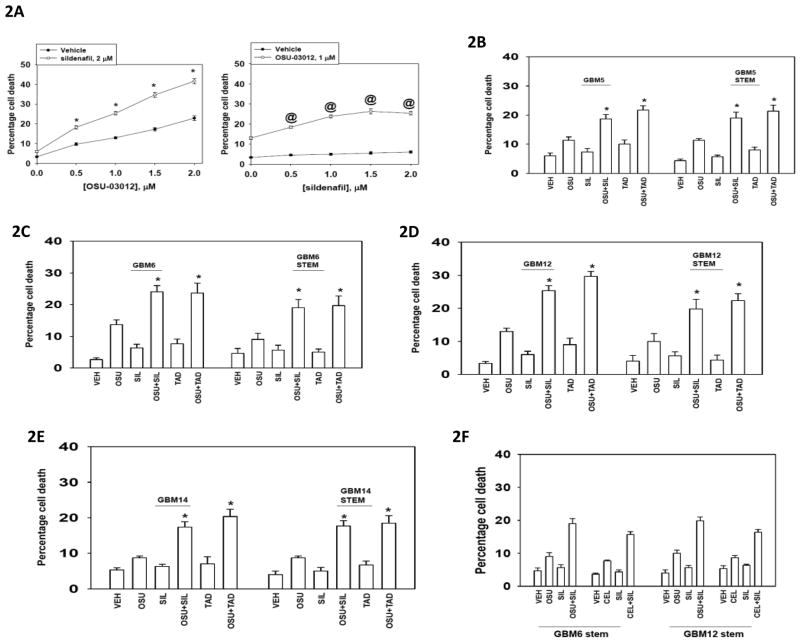
Initial studies examined the interaction between OSU-03012 and the PDE5 inhibitors sildenafil (Viagra) and tadalafil (Cialis) in parental glioma cells and glioma cells selected for stem-ness growing without attachment in serum free media containing growth factors. In a dose-dependent fashion OSU-03012 interacted with sildenafil to kill glioma cells (Figure 2A). OSU-03012 interacted with PDE5 inhibitors in an apparent greater than additive fashion to kill both parental and stem-like glioma cells (Figures 2B–2E). This was confirmed using median dose effect colony formation assays (Table 1). Very similar data to that generated with OSU-03012 were obtained using the FDA approved parent drug celecoxib at clinically relevant concentrations (Figure 2F, unpublished data).
Figure 2. OSU-03012 and sildenafil/tadalafil interact to kill multiple GBM cell isolates.
(A) GBM12 cells were treated with vehicle (VEH, DMSO), OSU-03012 (0–2 μM), sildenafil (0–2 μM) or the drugs in combination, as shown in the Figure. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than OSU treatment alone; @ p < 0.05 greater than sildenafil treatment alone. (B)–(E) GBM5, GBM6, GBM12 and GBM14 cells as well as selected stem cell-like neurosphere variants of these cells were treated with vehicle (VEH, DMSO), OSU-03012 (1 μM), sildenafil (2 μM), tadalafil (1 μM) or the drugs in combination, as shown in the Figure. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than OSU treatment alone. (F) GBM6-stem and GBM12-stem cells were treated with vehicle (VEH, DMSO), OSU-03012 (1 μM), sildenafil (2 μM), celecoxib (5 μM) or the drugs in combination, as shown in the Figure. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM).
Table 1. OSU-03012 and sildenafil synergize to kill glioblastoma cells.
GBM6 and GBM12 cells (250–1500 cells/well) were plated in sextuplicate and allowed to attach for 12h. Cells were treated with OSU-03012 (OSU, 0.5–2.0 μM); sildenafil (SIL, 0.5–2.0 μM); or the drugs combined for 24h. Media was removed, plates washed, and cells cultured for the next 10–14 days in media lacking drugs. After ~10 days media was removed, plates washed, and cells fixed and stained. The number of colonies per plate (> 50 cells per colony) was counted, plating efficiencies determined, and the relative changes in colony formation entered into the Calcusyn for Windows program to determine synergy (n = 3). A CI (combination index) of less than 0.70 indicates a strong level of synergy.
| GBM6 | GBM12 | ||||
|---|---|---|---|---|---|
| OSU μM | SIL μM | CI | OSU μM | SIL μM | CI |
| 0.50 | 0.50 | 0.63 | 0.50 | 0.50 | 0.69 |
| 1.00 | 1.00 | 0.58 | 1.00 | 1.00 | 0.63 |
| 1.50 | 1.50 | 0.49 | 1.50 | 1.50 | 0.56 |
| 2.00 | 2.00 | 0.44 | 2.00 | 2.00 | 0.49 |
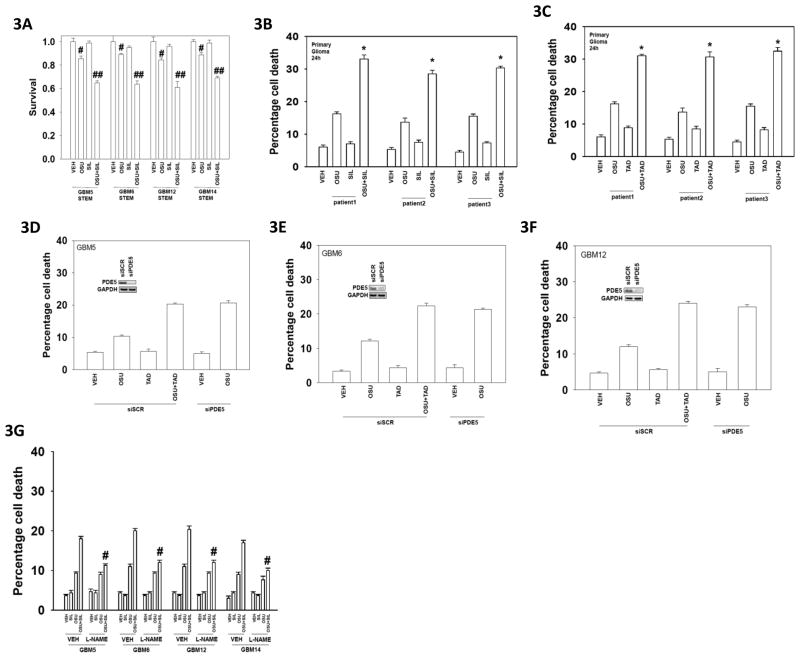
Of note was that the amount of killing caused by the drug combination differed little comparing parental and stem-like cell populations. Similar drug interaction data were obtained using stem-like cells in colony formation assays (Figure 3A). Glioma cells freshly isolated from patient tumors also exhibited a greater than additive killing effect when treated with OSU-03012 and PDE5 inhibitors (Figures 3B and 3C). We next determined whether PDE5 represented a key target for PDE5 inhibitors in our drug combination studies. Knock down of PDE5 in GBM cells enhanced OSU-03012 lethality to a similar extent as did tadalafil (Figures 3D–3F). Multiple PDE5 siRNA molecules gave similar effects, as we have observed before (22,23). In the tonic regulation vascular smooth muscle relaxation, PDE5 inhibitors are thought to act through increasing levels of cyclic GMP resulting in increased levels of nitric oxide (NO) (26, and references therein). Incubation of GBM cells with the NO synthase inhibitor L-NG-Nitroarginine Methyl Ester (L-NAME) suppressed cell killing by the OSU-03012 and sildenafil drug combination (Figure 3G).
Figure 3. OSU-03012 and sildenafil interact to kill multiple GBM cell isolates.
(A) Free floating GBM5/6/12/14 neurosphere stem cells were triturated to form single cells and were plated into soft agar in sextuplicate (500–1000 cells/dish). Cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Twenty four h after drug treatment the cover media was replaced with drug free media. Colonies were permitted to form over the following 20 days, after which they were stained and colonies counted (n = 3 +/− SEM). # p < 0.05 less than vehicle control; ## p < 0.05 less than value in OSU-03012 treated. (B) and (C) Freshly isolated GBM tumor cells (patients 1–3) were treated with vehicle (VEH, DMSO), OSU-03012 (1 μM), sildenafil (2 μM), tadalafil (1 μM) or the drugs in combination. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than OSU treatment alone. (D), (E), (F) GBM5/6/12 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA to knock down expression of PDE5. Thirty six h after transfection cells were treated with vehicle (VEH, DMSO), OSU-03012 (1 μM), sildenafil (2 μM), tadalafil (1 μM) or the drugs in combination, as indicated in the Figure. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than corresponding value in siSCR treatment. (G) GBM5/6/12 cells were pre-treated with vehicle (PBS) or L-NAME (1 μM). Cells were then treated with vehicle (VEH, DMSO), OSU-03012 (1 μM), sildenafil (2 μM), or the drugs in combination. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) # p < 0.05 less than OSU+SIL treatment in the absence of L-NAME.
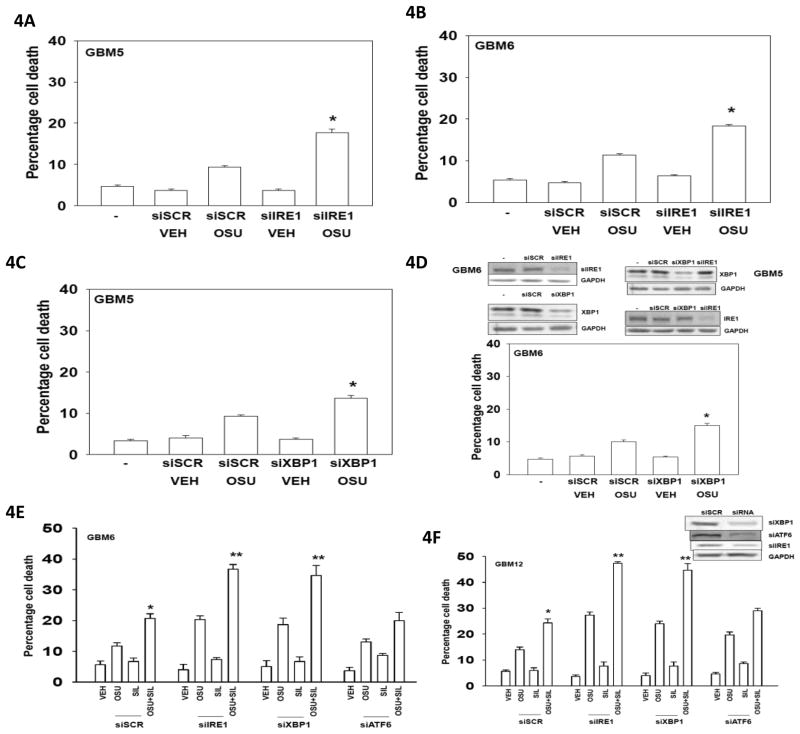
In several prior studies we demonstrated that ER stress signaling by PKR-like endoplasmic reticulum kinase (PERK) played a major role in mediating the toxic actions of OSU-03012 (12,13,15). Our present studies focused on the defining the role of the IRE1/XBP1 arm of the ER stress response in OSU-03012/OSU-03012 + sildenafil biology in GBM cells. We found that knock down of the IRE1/XBP1 arm of ER stress signaling pathway enhanced OSU-03012 toxicity (Figures 4A–4D). Knock down of IRE1/XBP1 signaling also enhanced [OSU-03012 + sildenafil] toxicity (Figures 4E and 4F).
Figure 4. IRE1/XBP1 signaling is protective against OSU-03012 and (OSU-03012 + sildenafil) toxicity.<.
br>(A) and (B) GBM5 and GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA to knock down expression of IRE1. Thirty six h after transfection cells were treated with vehicle (VEH, DMSO) or OSU-03012 (1.0 μM). Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than corresponding value in siSCR treatment. (C) and (D) GBM5 and GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA to knock down expression of XBP1. Thirty six h after transfection cells were treated with vehicle (VEH, DMSO) or OSU-03012 (1.0 μM). Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than corresponding value in siSCR treatment. (E) and (F) GBM6 and GBM12 cells were transfected with either a scrambled siRNA (siSCR) or with siRNA molecules to knock down expression of IRE1, XBP1 or ATF6. Thirty six h after transfection cells were treated with vehicle (VEH, DMSO), OSU-03012 (1 μM), sildenafil (2 μM) or the drugs in combination. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than OSU treatment alone; ** p < 0.05 greater than corresponding value in siSCR cells.
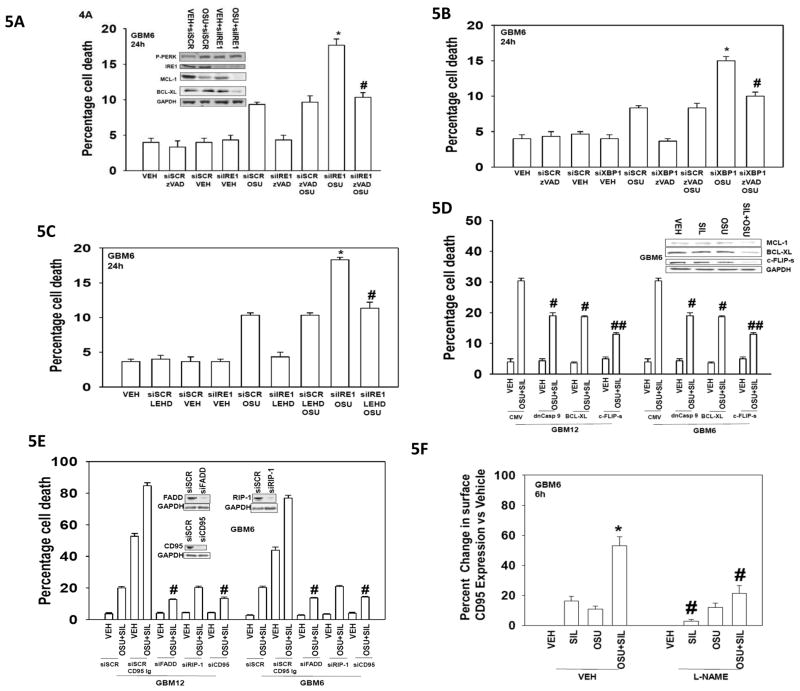
Previously we demonstrated that pan-inhibition of caspases using the agent zVAD did not reduce OSU-03012 toxicity, and similar findings were made herein (Figures 5A and 5B). However, the ability of IRE1/XBP1 knock down to enhance OSU-03012 lethality was abolished by use of the pan-caspase inhibitor zVAD. Of note was that the caspase 9 inhibitor LEHD, but not the caspase 8 inhibitor IETD, protected cells (Figure 4C, data not shown). This would argue that knock down of IRE1 is facilitating activation of the intrinsic apoptosis pathway. Unlike treatment with OSU-03012 alone, inhibition of caspase 8 by over-expression of c-FLIP-s reduced [OSU-03012 + sildenafil] lethality (Figure 5D). As caspase 8 inhibition was protective against [OSU-03012 + sildenafil] lethality we next determined whether death receptor signaling played a role in drug combination lethality; knock down of CD95 or of Fas associated death domain protein (FADD) suppressed [OSU-03012 + sildenafil] lethality (Figure 5E). An agonistic anti-CD95 antibody was more effective at killing than [OSU-03012 + sildenafil] treatment and enhanced [OSU-03012 + sildenafil] lethality. Incubation of GBM cells with the NO synthase inhibitor L-NAME suppressed CD95 activation by the OSU-03012 and sildenafil drug combination (Figure 5F).
Figure 5. Knock down of IRE1 enhances OSU-03012 and (OSU-03012 + sildenafil) toxicity through caspase dependent pathways.<.
br>(A) GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA to knock down expression of IRE1. Thirty six h after transfection cells were pre-treated with the pan-caspase inhibitor zVAD (50 μM) then treated with vehicle (VEH, DMSO) or OSU-03012 (1.0 μM). Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than corresponding value in siSCR treatment; # p < 0.05 less than (siIRE1 + OSU-03012) value. Inset blots: GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA to knock down expression of IRE1. Thirty six h after transfection cells were treated with vehicle (VEH, DMSO) or OSU-03012 (1.0 μM). Six h after treatment cells were lysed and immunoblotting performed to determine the expression of MCL-1 and BCL-XL and the phosphorylation of PERK. (B) GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA to knock down expression of XBP1. Thirty six h after transfection cells were pre-treated with the pan-caspase inhibitor zVAD (50 μM) then treated with vehicle (VEH, DMSO) or OSU-03012 (1.0 μM). Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than corresponding value in siSCR treatment; # p < 0.05 less than (siXBP1 + OSU-03012) value. (C) GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA to knock down expression of IRE1. Thirty six h after transfection cells were pre-treated with the caspase 9 inhibitor LEHD (50 μM) then treated with vehicle (VEH, DMSO) or OSU-03012 (1.0 μM). Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) * p < 0.05 greater than corresponding value in siSCR treatment; # p < 0.05 less than (siIRE1 + OSU-03012) value. (D) GBM6 and GBM12 cells were infected at 50 m.o.i. with either an empty vector adenovirus (CMV) or viruses to express dominant negative caspase 9, BCL-XL or the caspase 8 inhibitor c-FLIP-s. Twenty four h after infection cells were treated with vehicle (DMSO) or with OSU-03012 (1.0 μM) and sildenafil (2 μM) combined. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) # p < 0.05 less than corresponding value in CMV infected cells; ## p < 0.05 less than value in BCL-XL infected cells. Inset Panel: Cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Six h after treatment cells were lysed and immunoblotting performed to determine the expression of MCL-1, BCL-XL and c-FLIP-s. (E) GBM6 and GBM12 cells were transfected with either a scrambled siRNA (siSCR) or with siRNA molecules to knock down expression of CD95, FADD or RIP-1. Thirty six h after transfection cells were treated with vehicle (DMSO) or with OSU-03012 (1.0 μM) and sildenafil (2 μM) combined. As a positive control one set of siSCR transfected cells were treated with an agonistic azide free anti-CD95 antibody (2 μg) (the use of a control IgG was also performed but is not shown for clarity). Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM) # p < 0.05 less than corresponding value in siSCR transfected cells. (F) GBM6 cells in 96 well plates were pre-treated with vehicle or L-NAME (1 μM). Cells were then treated with OSU-03012 (OSU 1.0 μM) and/or sildenafil (SIL, 2.0 μM). Six h after treatment cells were fixed to the plate and immunohistochemistry performed to determine the plasma membrane levels of CD95. The intensity of CD95 immunostaining was determined using a Hermes Wiscan instrument with associated Wisoft data analysis package (n = 3 +/− SEM). * p < 0.05 value greater than celecoxib treatment alone; # p < 0.05 less than corresponding value in vehicle treated cells.
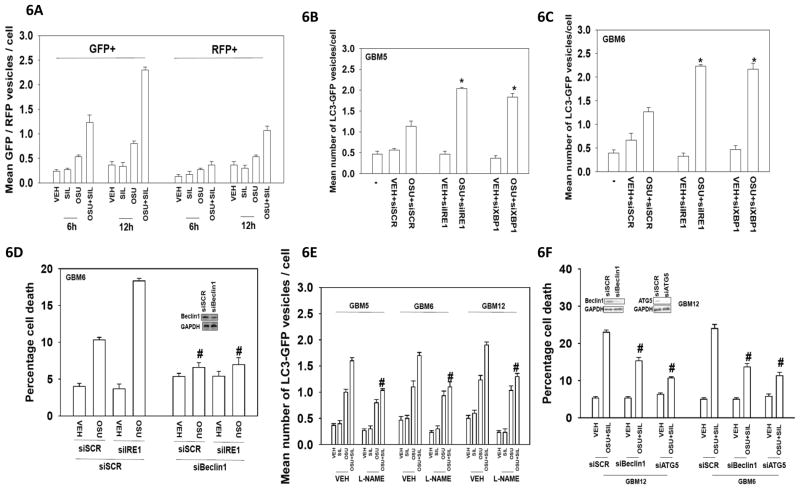
Prior studies from our laboratory have shown that increased PERK-dependent autophagy was causal in OSU-03012 toxicity as a single agent (12,13,15). Hence we next determined the induction of autophagy after knock down of IRE1 and after exposure of GBM cells to OSU-03012 and sildenafil. OSU-03012 and sildenafil interacted in a greater than additive fashion to induce autophagy, and in a time dependent fashion increased numbers of GFP+ vesicles (early autophagy, autophagosomes) followed by increased numbers of RFP+ vesicles (late autophagy, autolysosomes) were observed (Figure 6A). Knock down of IRE1 or of XBP1 enhanced the numbers of OSU-03012 -induced GFP+ vesciles (Figures 6B and 6C). Although cell killing following IRE1/XBP1 knock down was inhibited by the pan-caspase inhibitor zVAD (see data in Figure 5), we also found that knock down of Beclin1 suppressed the enhancement of autophagy and of cell killing caused by IRE1 knock down (Figure 6D). Inhibition of NOS enzymes/NO generation using L-NAME suppressed OSU-03012 and sildenafil –induced GFP+ vesicle formation (Figure 6E). Knock down of the autophagy regulatory proteins Beclin1 or of ATG5 suppressed OSU-03012 and sildenafil toxicity arguing autophagy was a toxic event (Figure 6F).
Figure 6. The regulation of autophagy by OSU-03012 and sildenafil.<.
br>(A) GBM6 cells were transfected with a plasmid to express LC3-GFP-RFP. Twenty four h after transfection cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Cells were microscopically examined 6h and 12h after drug exposure for the numbers of GFP+ and RFP+ intense staining vesicles (n = 3 +/− SEM). (B) and (C) GBM5 and GBM6 cells were transfected with a plasmid to express LC3-GFP and either a scrambled siRNA (siSCR) or with siRNA molecules to knock down expression of IRE1 or XBP1. Thirty six h after transfection cells were treated with vehicle (DMSO) or OSU-03012 (1.0 μM). Cells were microscopically examined 6h after drug exposure for the numbers of GFP+ intense staining vesicles (n = 3 +/− SEM). * p < 0.05 greater than corresponding value in siSCR transfected cells. (D) GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with siRNA molecules to knock down expression of IRE1 and/or Beclin1, as indicated. Thirty six h after transfection cells were treated with vehicle (DMSO) or OSU-03012 (1.0 μM). Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM). # p < 0.05 less than corresponding value in siSCR transfected cells. (E) GBM6 cells were transfected with a plasmid to express LC3-GFP-RFP. Twenty four h after transfection cells were pre-treated with vehicle (PBS) or L-NAME (1 μM). Cells were then treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Cells were microscopically examined 12h after drug exposure for the numbers of GFP+ and RFP+ intense staining vesicles (n = 3 +/− SEM). # p < 0.05 less than OSU+SIL treatment in the absence of L-NAME. (F) GBM6 and GBM12 cells were transfected with either a scrambled siRNA (siSCR) or with siRNA molecules to knock down expression of Beclin1 or ATG5. Thirty six h after transfection cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM). # p < 0.05 less than corresponding value in siSCR transfected cells.
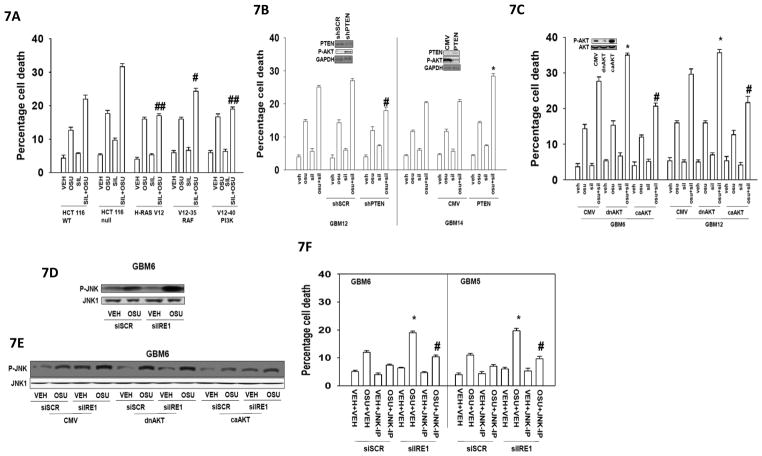
We next defined the roles of signaling pathways in the survival/killing of cells treated with OSU-03012 and sildenafil. Initially we made use of HCT116 colon cancer cells expressing in wild type cells mutant active K-RAS D13 or mutant forms of H-RAS V12 that specifically activated RAF-1 or PI3K (Figure 7A) (27). Expression of H-RAS V12 protected cells from OSU-03012 and sildenafil toxicity to a greater extent than did expression of K-RAS D13. The protective effect of H-RAS V12 was lost in cells expressing a mutant H-RAS V12 protein that specifically activated RAF-1 but not a H-RAS V12 protein that specifically activated PI3K (Figure 7A). In glioma cells expression of phosphatase and tensin homolog (PTEN) or knock down of PTEN enhanced or suppressed OSU-03012 and sildenafil toxicity, respectively (Figure 7B). In glioma cells expression of dominant negative AKT or expression of activated AKT enhanced or suppressed OSU-03012 and sildenafil toxicity, respectively (Figure 7C).
Figure 7. The roles of signal transduction pathways in the regulation of OSU-03012 and sildenafil toxicity.<.
br>(A) HCT116 colon cancer cells (Wild type cells expressing K-RAS D13; null cells with K-RAS D13 deleted; null cells expressing H-RAS V12; null cells expressing H-RAS V12–35 that activates RAF-1; null cells expressing H-RAS V12–40 that activates PI3K) were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM). # p < 0.05 less than corresponding value in wild type cells; ## p < 0.05 less than corresponding value in V12–35 cells. (B) GBM12 cells (wild type PTEN) were transfected with a plasmid to express a scrambled shRNA (shSCR) or a plasmid to express an shRNA to knock down expression of PTEN. GBM14 cells (PTEN null) were transfected with an empty vector plasmid (CMV) or a plasmid to express PTEN. Thirty six h after transfection cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM). # p < 0.05 less than corresponding value in shSCR transfected cells; * p < 0.05 greater than corresponding value in CMV transfected cells. (C) GBM6 and GBM12 cells were infected at 50 m.o.i. with an empty vector adenovirus (CMV) or adenoviruses to express dominant negative AKT (dnAKT) or to express activated AKT (caAKT). Twenty four h after infection cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM). # p < 0.05 less than corresponding value in CMV infected cells; * p < 0.05 greater than corresponding value in CMV cells. (D) GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA molecule to knock down expression of IRE1. Thirty six h after transfection cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Six h after drug treatment cells were isolated and immunoblotting performed to detect the levels of total JNK1 and phospho-JNK1. (E) GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA molecule to knock down expression of IRE1. In parallel cells were transfected with either an empty vector plasmid (CMV) or plasmids to express dominant negative AKT (dnAKT) or activated AKT (caAKT). Thirty six h after transfection cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Six h after drug treatment cells were isolated and immunoblotting performed to detect the levels of total JNK1 and phospho-JNK1. (F) GBM5 and GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA molecule to knock down expression of IRE1. Thirty six h after transfection cells were pre-treated with vehicle (DMSO) or with the JNK-inhibitory peptide (JNK-IP, 10 μM). Cells were then treated with vehicle (DMSO) or OSU-03012 (1.0 μM). Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM). # p < 0.05 less than corresponding value in siSCR cells; * p < 0.05 greater than corresponding value in siSCR cells.
IRE1 has been proposed to regulate the JNK pathway, with IRE1 signaling promoting activation of the pathway. Thus we next investigated the role of JNK signaling in our system with respect to IRE1 function, as well as OSU-03012 and sildenafil treatment. To our great surprise, knock down of IRE1 enhanced OSU-03012 –induced JNK activation (Figure 7D). Expression of dominant negative AKT enhanced OSU-03012 –induced JNK activation but did not further enhance JNK activation in IRE1 knock down cells whereas expression of activated AKT suppressed JNK activation under all conditions (Figure 7E). Inhibition of JNK signaling suppressed the enhancement of OSU-03012 toxicity by IRE1 knock down (Figure 7F).
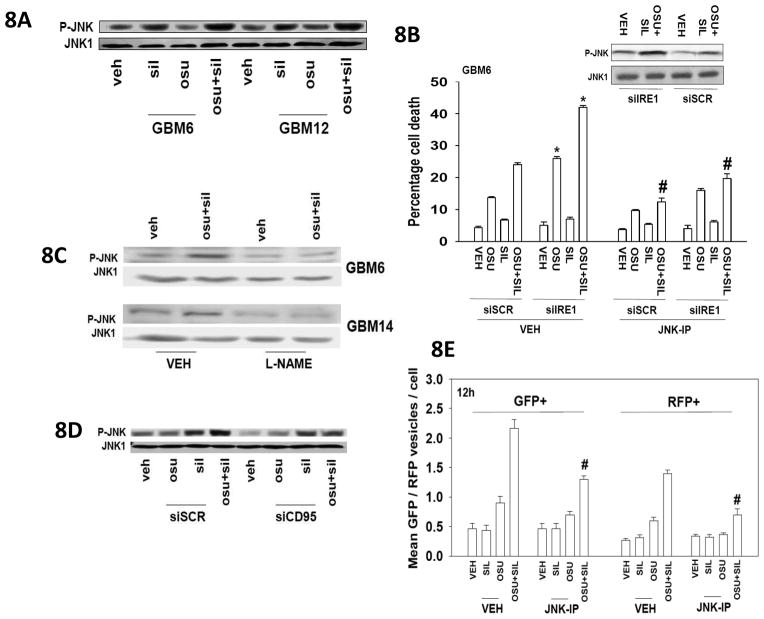
Additional studies then defined the role of JNK signaling with respect to OSU-03012 and sildenafil treatment. Sildenafil enhanced OSU-03012 –induced JNK activation (Figure 8A). Inhibition of JNK signaling suppressed the enhancement of OSU-03012 toxicity in combination with sildenafil (Figure 8B). Inhibition of NOS enzymes using L-NAME suppressed the activation of JNK caused by combined exposure to OSU-03012 and sildenafil (Figure 8C). In Figure 5 we noted that knock down of CD95 or FADD protected cells from OSU-03012 and sildenafil toxicity. Knock down of CD95 expression blocked the enhanced activation of JNK in OSU-03012 and sildenafil treated cells (Figure 8D). In Figure 6 we noted that sildenafil and OSU-03012 interacted to elevate the levels of autophagy; a toxic form of autophagy. Inhibition of JNK suppressed the induction of autophagy by OSU-03012 and sildenafil as judged by reduced levels of GFP+ and RFP+ vesicles (Figure 8E).
Figure 8. The roles of the JNK pathway in the regulation of OSU-03012 and sildenafil toxicity.<.
br>(A) GBM6 and GBM12 cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Six h after drug treatment cells were isolated and immunoblotting performed to detect the levels of total JNK1 and phospho-JNK1. (B) GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA molecule to knock down expression of IRE1. Thirty six h after transfection cells were pre-treated with vehicle (DMSO) or with the JNK-inhibitory peptide (JNK-IP, 10 μM). Cells were then treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs in combination. Twenty four h after drug treatment cells were isolated and viability determined by trypan blue exclusion assay (n = 3 +/− SEM). # p < 0.05 less than corresponding value in siSCR cells; * p < 0.05 greater than corresponding value in siSCR cells. (C) GBM6 and GBM14 cells were pre-treated with vehicle (PBS) or with L-NAME (1 μM). Cells were then treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Six h after drug treatment cells were isolated and immunoblotting performed to detect the levels of total JNK1 and phospho-JNK1. (D) GBM6 cells were transfected with either a scrambled siRNA (siSCR) or with an siRNA molecule to knock down expression of the death receptor CD95. Thirty six h after transfection cells were treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs in combination. Six h after drug treatment cells were isolated and immunoblotting performed to detect the levels of total JNK1 and phospho-JNK1. (E) GBM6 cells were transfected with a plasmid to express LC3-GFP-RFP. Twenty four h after transfection cells were pre-treated with vehicle (DMSO) or with the JNK-inhibitory peptide (JNK-IP, 10 μM). Cells were then treated with vehicle (DMSO), OSU-03012 (1.0 μM), sildenafil (2 μM) or the drugs combined. Cells were microscopically examined 12h after drug exposure for the numbers of GFP+ and RFP+ intense staining vesicles (n = 3 +/− SEM). # p < 0.05 less than corresponding value in VEH cells lacking the JNK-IP.
Discussion
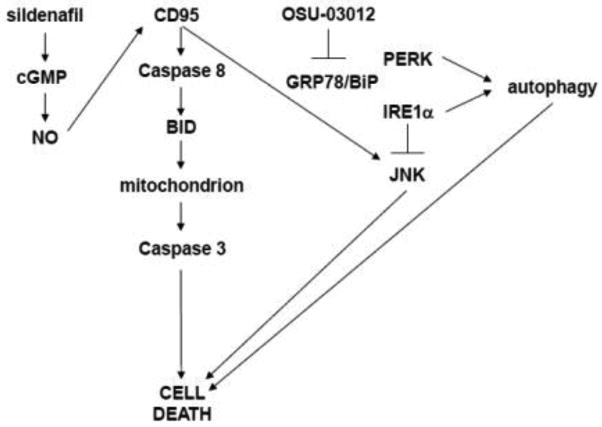
The present studies were initiated to determine whether PDE5 inhibitors interacted with OSU-03012 to kill tumor cells. In multiple primary human GBM cell types, as well as in freshly isolated human GBM cells, sildenafil enhanced OSU-03012 lethality. Furthermore, in primary human GBM cell types selected for CD133+ and stem cell-like growth as neurospheres in serum free media, tumor cell killing was as effective as that observed in parental cells. Furthermore, the parent compound of OSU-03012, celecoxib, also interacted with PDE5 inhibitors to kill GBM cells (and mammary carcinoma cells, unpublished observations). As discussed below, our data argue for a complex series of signaling events that regulate drug combination toxicity (Figure 9).
Figure 9. Putative signaling pathways modulated by OSU-03012 and sildenafil treatment.
OSU-03012 causes an ER stress response associated with reduced GRP78/BiP expression which leads to the activation of PERK and IRE1 signaling.
Our prior studies have linked OSU-03012 –induced ER stress signaling by PERK as being causal in the toxicity of the drug (12,13,15). The present studies demonstrated that the IRE1/XBP-1 arm of the ER stress response was protective against OSU-03012, and that the ATF6 arm appeared not to significantly alter the response. Knock down of IRE1/XBP-1 also enhanced OSU-03012 and sildenafil combination toxicity. We have previously shown that OSU-03012 as a single agent enhances cell death through a caspase-indpendent mechanism, however, the enhanced levels of killing caused by IRE1/XBP-1 knock down was caspase dependent. Inhibition of caspase 9, but not caspase 8, blunted enhanced killing by IRE1/XBP-1 knock down which correlated with reduced BCL-XL and MCL-1 expression. Thus IRE1/XBP-1 knock down was facilitating activation of the intrinsic apoptosis pathway. In contrast to data with OSU-03012 and IRE1/XBP-1 knock down, enhanced cell killing by the combination of OSU-03012 and sildenafil was blocked by inhibition of caspase 8 or knock down of CD95/FADD demonstrating that the extrinsic pathway was being induced by the drug combination.
Studies by others have shown that ER stress via IRE1 can signal to activate the JNK pathway, thus it was to our considerable surprise that loss of IRE1 function facilitated OSU-03012 -induced activation of the JNK pathway by OSU-03012 and this enhancement in JNK signaling was causal in cell death (29,30). We noted that IRE1 knock down was enhancing basal levels of PERK phosphorylation and it is possible that our JNK activation was due to this compensatory signaling effect. Expression of an activated form of AKT suppressed drug/knockdown –induced JNK activation and maintained tumor cell viability. Using point mutants of H-RAS V12 that activate specific downstream signaling pathways as well as manipulation of PTEN function and AKT activity we determined that signaling by the AKT pathway also protected against OSU-03012 and sildenafil drug combination toxicity. In this instance drug combination –induced JNK pathway activation was dependent on the drug combination causing CD95 activation.
In prior studies we demonstrated that OSU-03012 toxicity was dependent on increased levels of autophagy. Knock down of IRE1 enhanced OSU-03012 –induced LC3-GFP+ and LC3-RFP+ vesicle formation and, although enhanced killing by drug/knock down was inhibited by the pan-caspase inhibitor zVAD and the caspase 9 inhibitor LEHD, knock down of Beclin1 protected cells under these conditions. These findings argue for a link between autophagy and the mitochondrial apoptosis pathway, that ourselves and others have previously explored (31,32). As we know from prior studies that OSU-03012 induces autophagy and causes cathepsin B –dependent cleavage of BID, our findings suggest the induction of autophagy is a primary event that facilitates mitochondrial dysfunction thereby promoting activation of the intrinsic pathway.
Sildenafil was developed as an inhibitor of PDE5 with cardio-protective effects, and serendipitously became an approved thereapeutic for erectile dysfunction (33). PDE5 expression is not confined to the corpus cavernosum in the human penis and is expressed in the wider vasculature, myocardium and tumor cells (34,35). PDE5 catalyzes the degradation of cyclic GMP; i.e. thus PDE5 inhibitors increase cGMP levels (36). Nitric oxide (NO) induces smooth muscle relaxation via the actions of cGMP (37). NO at nanomolar levels binds tightly to a heme group in NO-guanylyl cyclase (GC), also known as soluble guanylyl cyclase, and causes a ~150-fold activation of the enzyme (38). Activation of NO-GC elevates cGMP levels, which initiate the cGMP signaling pathway, in part through activation of cGMP dependent protein kinase (PKG) (39). It is known in non-tumor cells that cGMP/PKG, through its stimulatory actions upon the ERK, p38 MAPK, JNK and NFκB pathways can increase the expression of inducible nitric oxide synthase (iNOS) (40–42). In our present studies we noted that sildenafil treatment increased iNOS levels (unpublished observations). Thus increased levels of NO activate GC and increase cGMP levels, that activates signaling pathways which increase iNOS levels; and increased iNOS levels lead to further increases in cellular NO. Elevation of cGMP or overexpression of constitutively active PKG can result in phosphorylation and activation of the JNK pathway and promote apoptosis (43–47). This is similar to our findings where sildenafil and OSU-03012 interacted to cause toxic JNK activation. High concentrations of sildenafil and vardenafil induce caspase-dependent apoptosis of B-chronic lymphocytic leukemia cells but not in normal B cells, suggesting a tumor selective toxicity of PDE5 inhibitors (48). PDE5 inhibitors enhance tumor/vasculature permeability and efficacy of chemotherapy in a rat brain tumor model (49). When transiently expressed in HT29 colon cancer cells, constitutively activated mutants of PKG beta, inhibit colony formation and induce apoptosis (50). In PC12 cells cGMP signaling, via activation of the AKT pathway prevents apoptosis (51). Others have argued that cGMP and NO kills cells through activation of the CD95/FAS-L pathway (52). These latter findings are similar to the data in the present manuscript where OSU-03012 and sildenafil interacted to kill through CD95 activation.
The precise mechanisms by which the PDE5 inhibitor/OSU-03012 drug combination activates the death receptor CD95 is at present open to conjecture. Incubation with L-NAME blocked CD95 activation and suppressed cell killing. High levels of NO can nitrosylate the activating tyrosine residues in CD95, thereby inhibiting ligand independent CD95 activation (53). Earlier manuscipts have argued in hematopoietic cells that NO, in a cyclic GMP independent fashion, can inhibit CD95 –induced apoptosis (54,55). Others however have argued that NO can up-regulate expression of CD95 that promotes apoptosis (56,57). Another possible regulatory step in the CD95 activation process that may be impacted by the PDE5 inhibitor/OSU-03012 drug combination is the generation of ceramide. Fumonisin B1 blocked CD95 activation. Prior studies by our group have shown ceramide generation can play a key role in CD95 activation, particularly through de novo ceramide synthase enzymes (58). Nitric oxide has been noted to reduce the generation of ceramide in response to tumor necrosis factor alpha (59). However inhibition of ceramide synthase enzymes has also been shown to blunt NO –induced cardio-myocyte cell killing (60). The ability of PDE5 inhibitors and OSU-03012 to interact in a toxic fashion could also possibly be dose- and schedule-dependent, though prior studies using sildenafil at higher concentrations still argued for sildenafil as a potentiator of chemotherapy toxicity (22,23). Clearly, much additional experimentation will be required to fully understand how the PDE5 inhibitor/OSU-03012 drug combination activates the extrinsic/CD95 pathway. OSU-03012 is presently undergoing Phase I clinical testing. The C max of the drug was ~2 μM at the MTD of 800 mg BID, though the C max was variable due to poor adsorption from the stomach (14). The drug is presently being re-formulated for additional Phase I clinical studies. Our data in the present manuscript demonstrated that the parent drug, celecoxib, also interacted with PDE5 inhibitors to kill GBM cells. Furthermore, in a separate series of studies combining celecoxib with sildenafil we were able to demonstrate a strong anti-tumor action in vivo using both HER2+ and triple negative mammary carcinoma cells (ubpublished observations). Although some of the recently developed anti-cancer drugs have strong single agent effects due to their targeting oncogene addicted cells, many drugs will have more modest single agent effects and as such will need to be rationally combined with other agents to achieve a better therapeutic index. Our studies combining OSU-03012 and sildenafil being a case in point. Based on our data in both GBM and mammary carcinoma cells combining celecoxib and sildenafil, a Phase I trial will open in 2015 combining these agents for the therapy of solid tumor malignancies.
Acknowledgments
Support to P. Dent for the present study was funded from PHS grants from the National Institutes of Health [R01-CA141704, R01-CA150214, R01-DK52825]. Thanks to PJ and JS for assistance during this project. PD is the holder of the Universal Inc. Chair in Signal Transduction Research.
Abbreviations
- ERK
extracellular regulated kinase
- MEK
mitogen activated extracellular regulated kinase
- EGF
epidermal growth factor
- OSU
OSU-03012
- PARP
poly ADP ribosyl polymerase
- PI3K
phosphatidyl inositol 3 kinase
- −/−
null/gene deleted
- ERK
extracellular regulated kinase
- MAPK
mitogen activated protein kinase
- MEK
mitogen activated extracellular regulated kinase
- PTEN
Phosphatase and tensin homolog
- R
receptor
- JNK
c-Jun NH2-terminal kinase
- dn
dominant negative
- COX
cyclooxygenase
- P
phospho-
- ca
constitutively active
- WT
wild type
- PERK
PKR like endoplasmic reticulum kinase
- HSP
heat shock protein
Footnotes
The authors have no conflicts of interest to report.
References
- 1.Zhu J, Huang JW, Tseng PH, Yang YT, Fowble JW, Shiau CW, et al. From the cyclooxygenase-2 inhibitor celecoxib to a novel class of 3-phosphoinositide-dependent protein kinase-1 inhibitors. Cancer Res. 2004;64:4309–4318. doi: 10.1158/0008-5472.CAN-03-4063. [DOI] [PubMed] [Google Scholar]
- 2.Johnson AJ, Smith LL, Zhu J, Heerema NA, Jefferson S, Mone A, et al. A novel celecoxib derivative, OSU-03012, induces cytotoxicity in primary CLL cells and transformed B-cell lymphoma cell line via a caspase-and Bcl-2-independent mechanism. Blood. 2005;105:2504–2509. doi: 10.1182/blood-2004-05-1957. [DOI] [PubMed] [Google Scholar]
- 3.Koehne CH, Dubois RN. COX-2 inhibition and colorectal cancer. Semin Oncol. 2004;31:12–21. doi: 10.1053/j.seminoncol.2004.03.041. [DOI] [PubMed] [Google Scholar]
- 4.Cui W, Yu CH, Hu KQ. In vitro and in vivo effects and mechanisms of celecoxib-induced growth inhibition of human hepatocellular carcinoma cells. Clin Cancer Res. 2005;11:8213–8221. doi: 10.1158/1078-0432.CCR-05-1044. [DOI] [PubMed] [Google Scholar]
- 5.Kang SG, Kim JS, Park K, Kim JS, Groves MD, Nam DH. Combination celecoxib and temozolomide in C6 rat glioma orthotopic model. Oncol Rep. 2006;15:7–13. [PubMed] [Google Scholar]
- 6.Klenke FM, Gebhard MM, Ewerbeck V, Abdollahi A, Huber PE, Sckell A. The selective Cox-2 inhibitor celecoxib suppresses angiogenesis and growth of secondary bone tumors: an intravital microscopy study in mice. BMC Cancer. 2006;12:6–9. doi: 10.1186/1471-2407-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kashfi K, Rigas B. Is COX-2 a ‘collateral’ target in cancer prevention? Biochem Soc Trans. 2005;33:724–727. doi: 10.1042/BST0330724. [DOI] [PubMed] [Google Scholar]
- 8.Narayanan BA, Narayanan NK, Pittman B, Reddy BS. Adenocarcina of the mouse prostate growth inhibition by celecoxib: downregulation of transcription factors involved in COX-2 inhibition. Prostate. 2006;66:257–265. doi: 10.1002/pros.20331. [DOI] [PubMed] [Google Scholar]
- 9.Patel MI, Subbaramaiah K, Du B, Chang M, Newman RA, Cordon-Cardo C, Thaler HT, Dannenberg AJ. Celecoxib inhibits prostate cancer growth: evidence of a cyclooxygenase-2-independent mechanism. Clin Cancer Res. 2005;11:1999–2007. doi: 10.1158/1078-0432.CCR-04-1877. [DOI] [PubMed] [Google Scholar]
- 10.Kulp SK, Yang YT, Hung CC, Chen KF, Lai JP, Tseng PH, Fowble JW, Ward PJ, Chen CS. 3-Phosphoinositide-dependent protein kinase-1/Akt signaling represents a major cyclooxygenase-2-independent target for celecoxib in prostate cancer cells. Cancer Res. 2004;64:1444–1451. doi: 10.1158/0008-5472.can-03-2396. [DOI] [PubMed] [Google Scholar]
- 11.Yacoub A, Park MA, Hanna D, Hong Y, Mitchell C, Pandya AP, Harada H, Powis G, Chen CS, Koumenis C, Grant S, Dent P. OSU-03012 promotes caspase-independent but PERK-, cathepsin B-, BID-, and AIF-dependent killing of transformed cells. Mol Pharmacol. 2006;70:589–603. doi: 10.1124/mol.106.025007. [DOI] [PubMed] [Google Scholar]
- 12.Park MA, Yacoub A, Rahmani M, Zhang G, Hart L, Hagan MP, Calderwood SK, Sherman MY, Koumenis C, Spiegel S, Chen CS, Graf M, Curiel DT, Fisher PB, Grant S, Dent P. OSU-03012 stimulates PKR-like endoplasmic reticulum-dependent increases in 70-kDa heat shock protein expression, attenuating its lethal actions in transformed cells. Mol Pharmacol. 2008;73:1168–84. doi: 10.1124/mol.107.042697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Booth L, Cazanave SC, Hamed HA, Yacoub A, Ogretmen B, Chen CS, Grant S, Dent P. OSU-03012 suppresses GRP78/BiP expression that causes PERK-dependent increases in tumor cell killing. Cancer Biol Ther. 2012;13:224–36. doi: 10.4161/cbt.13.4.18877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mateo J, De Bono SJ, Ramanathan RK, Lustberg MB, Zivi A, Basset D, Ng M, Young AM, Garrett M, Decordova S, Raynaud FI, Yap TA, Zukiwski AA, Proniuk S, Shapiro CL. A first-in-human phase I trial of AR-12, a PDK-1 inhibitor, in patients with advanced solid tumors. J Clin Oncol. 2013;31(suppl):abstr 2608. http://meetinglibrary.asco.org/content/115148-132. [Google Scholar]
- 15.Booth L, Cruickshanks N, Ridder T, Chen CS, Grant S, Dent P. OSU-03012 interacts with lapatinib to kill brain cancer cells. Cancer Biol Ther. 2012;13:1501–11. doi: 10.4161/cbt.22275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Y, Brandizzi F. IRE1: ER stress sensor and cell fate executor. Trends Cell Biol. 2013;23:547–55. doi: 10.1016/j.tcb.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pavitt GD, Ron D. New insights into translational regulation in the endoplasmic reticulum unfolded protein response. Cold Spring Harb Perspect Biol. 2012 Jun 1;4(6) doi: 10.1101/cshperspect.a012278. pii: a012278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hollien J, Weissman JS. Decay of endoplasmic reticulum-localized mRNAs during the unfolded protein response. Science. 2006;313:104–7. doi: 10.1126/science.1129631. [DOI] [PubMed] [Google Scholar]
- 19.Hollien J, Lin JH, Li H, Stevens N, Walter P, Weissman JS. Regulated Ire1-dependent decay of messenger RNAs in mammalian cells. J Cell Biol. 2009;186:323–31. doi: 10.1083/jcb.200903014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sano R, Reed JC. ER stress-induced cell death mechanisms. Biochim Biophys Acta. 2013;1833:3460–70. doi: 10.1016/j.bbamcr.2013.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bork P, Sander C. A hybrid protein kinase-RNase in an interferon-induced pathway? FEBS Lett. 1993;334:149–52. doi: 10.1016/0014-5793(93)81701-z. [DOI] [PubMed] [Google Scholar]
- 22.Booth L, Roberts JL, Cruickshanks N, Conley A, Durrant DE, Das A, Fisher PB, Kukreja RC, Grant S, Poklepovic A, Dent P. Phosphodiesterase 5 inhibitors enhance chemotherapy killing in gastrointestinal/genitourinary cancer cells. Mol Pharmacol. 2014;85:408–19. doi: 10.1124/mol.113.090043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Booth L, Roberts JL, Conley A, Cruickshanks N, Ridder T, Grant S, Poklepovic A, Dent P. HDAC inhibitors enhance the lethality of low dose salinomycin in parental and stem-like GBM cells. Cancer Biol Ther. 2014;15:305–16. doi: 10.4161/cbt.27309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giannini C, Sarkaria JN, Saito A, Uhm JH, Galanis E, Carlson BL, Schroeder MA, James CD. Patient tumor EGFR and PDGFRA gene amplifications retained in an invasive intracranial xenograft model of glioblastoma multiforme. Neuro Oncol. 2005;7:164–76. doi: 10.1215/S1152851704000821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cruickshanks N, Hamed HA, Booth L, Tavallai S, Syed J, Sajithlal GB, Grant S, Poklepovic A, Dent P. Histone deacetylase inhibitors restore toxic BH3 domain protein expression in anoikis-resistant mammary and brain cancer stem cells, thereby enhancing the response to anti-ERBB1/ERBB2 therapy. Cancer Biol Ther. 2013;14:982–96. doi: 10.4161/cbt.26234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Das A, Durrant D, Mitchell C, Mayton E, Hoke NN, Salloum FN, Park MA, Qureshi I, Lee R, Dent P, Kukreja RC. Sildenafil increases chemotherapeutic efficacy of doxorubicin in prostate cancer and ameliorates cardiac dysfunction. Proc Natl Acad Sci U S A. 2010;107:18202–7. doi: 10.1073/pnas.1006965107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carón RW, Yacoub A, Li M, Zhu X, Mitchell C, Hong Y, Hawkins W, Sasazuki T, Shirasawa S, Kozikowski AP, Dennis PA, Hagan MP, Grant S, Dent P. Activated forms of H-RAS and K-RAS differentially regulate membrane association of PI3K, PDK-1, and AKT and the effect of therapeutic kinase inhibitors on cell survival. Mol Cancer Ther. 2005;4:257–70. [PubMed] [Google Scholar]
- 28.Booth L, Cazanave SC, Hamed HA, Yacoub A, Ogretmen B, Chen CS, Grant S, Dent P. OSU-03012 suppresses GRP78/BiP expression that causes PERK-dependent increases in tumor cell killing. Cancer Biol Ther. 2012;13:224–36. doi: 10.4161/cbt.13.4.18877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kato H, Katoh R, Kitamura M. Dual regulation of cadmium-induced apoptosis by mTORC1 through selective induction of IRE1 branches in unfolded protein response. PLoS One. 2013;8:e64344. doi: 10.1371/journal.pone.0064344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kato H, Nakajima S, Saito Y, Takahashi S, Katoh R, Kitamura M. mTORC1 serves ER stress-triggered apoptosis via selective activation of the IRE1-JNK pathway. Cell Death Differ. 2012;19:310–20. doi: 10.1038/cdd.2011.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang Y, Hamed HA, Cruickshanks N, Fisher PB, Grant S, Dent P. Obatoclax and lapatinib interact to induce toxic autophagy through NOXA. Mol Pharmacol. 2012;81:527–40. doi: 10.1124/mol.111.076851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sentelle RD, Senkal CE, Jiang W, Ponnusamy S, Gencer S, Selvam SP, Ramshesh VK, Peterson YK, Lemasters JJ, Szulc ZM, Bielawski J, Ogretmen B. Ceramide targets autophagosomes to mitochondria and induces lethal mitophagy. Nat Chem Biol. 2012;8:831–8. doi: 10.1038/nchembio.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zusman RM, Morales A, Glasser DB, Osterloh IH. Overall cardiovascular profile of sildenafil citrate. Am J Cardiol. 1999;83:35C–44C. doi: 10.1016/s0002-9149(99)00046-6. [DOI] [PubMed] [Google Scholar]
- 34.Shan X, Quaile MP, Monk JK, French B, Cappola TP, Margulies KB. Differential expression of PDE5 in failing and nonfailing human myocardium. Circ Heart Fail. 2012;5:79–86. doi: 10.1161/CIRCHEARTFAILURE.111.961706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karami-Tehrani F, Moeinifard M, Aghaei M, Atri M. Evaluation of PDE5 and PDE9 Expression in Benign and Malignant Breast Tumors. Arch Med Res. 2012;43:470–5. doi: 10.1016/j.arcmed.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 36.Zhang X, Yan G, Ji J, Wu J, Sun X, Shen J, Jiang H, Wang H. PDE5 inhibitor promotes melanin synthesis through the PKG pathway in B16 melanoma cells. J Cell Biochem. 2012;113:2738–43. doi: 10.1002/jcb.24147. [DOI] [PubMed] [Google Scholar]
- 37.Kato M, Blanton R, Wang GR, Judson TJ, Abe Y, Myoishi M, Karas RH, Mendelsohn ME. Direct Binding and Regulation of RhoA by Cyclic GMP-dependent Protein Kinase Iα. J Biol Chem. 2012;287:41342–51. doi: 10.1074/jbc.M112.421040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Potter LR. Guanylyl cyclase structure, function and regulation. Cell Signal. 2011;23:1921–6. doi: 10.1016/j.cellsig.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Friebe A, Koesling D. The function of NO-sensitive guanylyl cyclase: what we can learn from genetic mouse models. Nitric Oxide. 2009;21:149–56. doi: 10.1016/j.niox.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 40.Komalavilas P, Shah PK, Jo H, Lincoln TM. Activation of mitogen-activated protein kinase pathways by cyclic GMP and cyclic GMP-dependent protein kinase in contractile vascular smooth muscle cells. J Biol Chem. 1999;274:34301–9. doi: 10.1074/jbc.274.48.34301. [DOI] [PubMed] [Google Scholar]
- 41.Das A, Xi L, Kukreja RC. Protein kinase G-dependent cardioprotective mechanism of phosphodiesterase-5 inhibition involves phosphorylation of ERK and GSK3beta. J Biol Chem. 2008;283:29572–85. doi: 10.1074/jbc.M801547200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Choi CY, Park KR, Lee JH, Jeon YJ, Liu KH, Oh S, Kim DE, Yea SS. Isoeugenol suppression of inducible nitric oxide synthase expression is mediated by down-regulation of NF-kappaB, ERK1/2, and p38 kinase. Eur J Pharmacol. 2007;576:151–9. doi: 10.1016/j.ejphar.2007.07.034. [DOI] [PubMed] [Google Scholar]
- 43.Thompson WJ, Piazza GA, Li H, Liu L, Fetter J, Zhu B, Sperl G, Ahnen D, Pamukcu R. Exisulind induction of apoptosis involves guanosine 3′,5′-cyclic monophosphate phosphodiesterase inhibition, protein kinase G activation, and attenuated beta-catenin. Cancer Res. 2000;60:3338–42. [PubMed] [Google Scholar]
- 44.Deguchi A, Thompson WJ, Weinstein IB. Activation of protein kinase G is sufficient to induce apoptosis and inhibit cell migration in colon cancer cells. Cancer Res. 2004;64:3966–73. doi: 10.1158/0008-5472.CAN-03-3740. [DOI] [PubMed] [Google Scholar]
- 45.Zhu B, Strada S, Stevens T. Cyclic GMP-specific phosphodiesterase 5 regulates growth and apoptosis in pulmonary endothelial cells. Am J Physiol Lung Cell Mol Physiol. 2005;289:L196–206. doi: 10.1152/ajplung.00433.2004. [DOI] [PubMed] [Google Scholar]
- 46.Zhu B, Zhang L, Alexeyev M, Alvarez DF, Strada SJ, Stevens T. Type 5 phosphodiesterase expression is a critical determinant of the endothelial cell angiogenic phenotype. Am J Physiol Lung Cell Mol Physiol. 2009;296:L220–8. doi: 10.1152/ajplung.90474.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhu B, Strada SJ. The novel functions of cGMP-specific phosphodiesterase 5 and its inhibitors in carcinoma cells and pulmonary/cardiovascular vessels. Curr Top Med Chem. 2007;7:437–54. doi: 10.2174/156802607779941198. [DOI] [PubMed] [Google Scholar]
- 48.Sarfati M, Mateo V, Baudet S, Rubio M, Fernandez C, Davi F, Binet JL, Delic J, Merle-Beral H. Sildenafil and vardenafil, types 5 and 6 phosphodiesterase inhibitors, induce caspase-dependent apoptosis of B-chronic lymphocytic leukemia cells. Blood. 2003;101:265–9. doi: 10.1182/blood-2002-01-0075. [DOI] [PubMed] [Google Scholar]
- 49.Black KL, Yin D, Ong JM, Hu J, Konda BM, Wang X, Ko MK, Bayan JA, Sacapano MR, Espinoza A, Irvin DK, Shu Y. PDE5 inhibitors enhance tumor permeability and efficacy of chemotherapy in a rat brain tumor model. Brain Res. 2008;1230:290–302. doi: 10.1016/j.brainres.2008.06.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhu B, Vemavarapu L, Thompson WJ, Strada SJ. Suppression of cyclic GMP-specific phosphodiesterase 5 promotes apoptosis and inhibits growth in HT29 cells. J Cell Biochem. 2005;94:336–50. doi: 10.1002/jcb.20286. [DOI] [PubMed] [Google Scholar]
- 51.Ha KS, Kim KM, Kwon YG, Bai SK, Nam WD, Yoo YM, Kim PK, Chung HT, Billiar TR, Kim YM. Nitric oxide prevents 6-hydroxydopamine-induced apoptosis in PC12 cells through cGMP-dependent PI3 kinase/Akt activation. FASEB J. 2003;17:1036–47. doi: 10.1096/fj.02-0738com. [DOI] [PubMed] [Google Scholar]
- 52.Hayden MA, Lange PA, Nakayama DK. Nitric oxide and cyclic guanosine monophosphate stimulate apoptosis via activation of the Fas-FasL pathway. J Surg Res. 2001;101:183–9. doi: 10.1006/jsre.2001.6257. [DOI] [PubMed] [Google Scholar]
- 53.Reinehr R, Görg B, Höngen A, Häussinger D. CD95-tyrosine nitration inhibits hyperosmotic and CD95 ligand-induced CD95 activation in rat hepatocytes. J Biol Chem. 2004;279:10364–73. doi: 10.1074/jbc.M311997200. [DOI] [PubMed] [Google Scholar]
- 54.Mannick JB, Miao XQ, Stamler JS. Nitric oxide inhibits Fas-induced apoptosis. J Biol Chem. 1997;272:24125–8. doi: 10.1074/jbc.272.39.24125. [DOI] [PubMed] [Google Scholar]
- 55.Dimmeler S, Haendeler J, Sause A, Zeiher AM. Nitric oxide inhibits APO-1/Fas-mediated cell death. Cell Growth Differ. 1998;9:415–22. [PubMed] [Google Scholar]
- 56.Fukuo K, Hata S, Suhara T, Nakahashi T, Shinto Y, Tsujimoto Y, Morimoto S, Ogihara T. Nitric oxide induces upregulation of Fas and apoptosis in vascular smooth muscle. Hypertension. 1996;27:823–6. doi: 10.1161/01.hyp.27.3.823. [DOI] [PubMed] [Google Scholar]
- 57.Hayden MA, Lange PA, Nakayama DK. Nitric oxide and cyclic guanosine monophosphate stimulate apoptosis via activation of the Fas-FasL pathway. J Surg Res. 2001;101:183–9. doi: 10.1006/jsre.2001.6257. [DOI] [PubMed] [Google Scholar]
- 58.Park MA, Mitchell C, Zhang G, Yacoub A, Allegood J, Häussinger D, Reinehr R, Larner A, Spiegel S, Fisher PB, Voelkel-Johnson C, Ogretmen B, Grant S, Dent P. Vorinostat and sorafenib increase CD95 activation in gastrointestinal tumor cells through a Ca(2+)-de novo ceramide-PP2A-reactive oxygen species-dependent signaling pathway. Cancer Res. 2010;70:6313–24. doi: 10.1158/0008-5472.CAN-10-0999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.De Nadai C, Sestili P, Cantoni O, Lièvremont JP, Sciorati C, Barsacchi R, Moncada S, Meldolesi J, Clementi E. Nitric oxide inhibits tumor necrosis factor-alpha-induced apoptosis by reducing the generation of ceramide. Proc Natl Acad Sci U S A. 2000;97:5480–5. doi: 10.1073/pnas.070062397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rabkin SW. Fumonisin blunts nitric oxide-induced and nitroprusside-induced cardiomyocyte death. Nitric Oxide. 2002;7:229–35. doi: 10.1016/s1089-8603(02)00115-5. [DOI] [PubMed] [Google Scholar]