Abstract
Background
Mutations in the LMNA gene encoding A-type nuclear lamins can cause dilated cardiomyopathy with or without skeletal muscular dystrophy. Previous studies have shown abnormally increased extracellular signal-regulated kinase 1/2 activity in hearts of LmnaH222P/H222P mice, a small animal model. Inhibition of this abnormal signaling activity with a mitogen-activated protein kinase kinase 1/2 (MEK1/2) inhibitor has beneficial effects on heart function and survival in these mice. However, such treatment has not been examined relative to any standard of care intervention for dilated cardiomyopathy or heart failure. We therefore examined the effects of an angiotensin II converting enzyme (ACE) inhibitor on left ventricular function in LmnaH222P/H222P mice and assessed if adding a MEK1/2 inhibitor would provide added benefit.
Methods
Male LmnaH222P/H222P mice were treated with the ACE inhibitor benazepril, the MEK1/2 inhibitor selumetinib or both. Transthoracic echocardiography was used to measure left ventricular diameters and fractional shortening was calculated.
Results
Treatment of LmnaH222P/H222P mice with either benazepril or selumetinib started at 8 weeks of age, before the onset of detectable left ventricular dysfunction, lead to statistically significantly increased fractional shortening compared to placebo at 16 weeks of age. There was a trend towards a great value for fractional shortening in the selumetinib-treated mice. When treatment was started at 16 weeks of age, after the onset of left ventricular dysfunction, the addition of selumetinib treatment to benazepril lead to a statistically significant increase in left ventricular fractional shortening at 20 weeks of age.
Conclusions
Both ACE inhibition and MEK1/2 inhibition have beneficial effects on left ventricular function in LmnaH222P/H222P mice and both drugs together have a synergistic benefit when initiated after the onset of left ventricular dysfunction. These results provide further preclinical rationale for a clinical trial of a MEK1/2 inhibitor in addition to standard of care in patients with dilated cardiomyopathy caused by LMNA mutations.
Keywords: lamin, cardiomyopathy, nuclear envelope, mitogen-activated protein kinase
1. Introduction
Mutations in the lamin A/C gene (LMNA) were first shown to cause Emery-Dreifuss muscular dystrophy, which is characterized by a prominent dilated cardiomyopathy [1]. Subsequent genetic studies showed that LMNA mutations could similarly cause an isolated dilated cardiomyopathy and other muscular dystrophy phenotypes with dilated cardiomyopathy [2-5]. Indeed, mutations in LMNA may be responsible for approximately 7.5% of inherited cases of dilated cardiomyopathy [6,7].
Cardiomyopathy caused by LMNA mutations is almost always progressive, often leading to premature death or heart transplantation [6,8-12]. The conduction system is usually affected early, manifesting as sick sinus syndrome, atrioventricular block or bundle branch blocks, often requiring implantation of a permanent pacemaker. Malignant ventricular arrhythmias are also common and can be an earliest clinical manifestation. Heart failure occurs in approximately 10% of patients by age 30 years and 65% by age 50 years. By an age of 60 years, 55% of patients with cardiomyopathy and LMNA mutation die of cardiovascular death or undergo heart transplantation compared to 11% of patients with idiopathic cardiomyopathy without LMNA mutation.
Given the high prevalence of malignant ventricular arrhythmias in patients with LMNA mutations, some authors have recommended placement of an intracardiac cardioverter defibrillator at the time of pacemaker insertion, even if the degree of systolic dysfunction does not meet the generally accepted criteria for primary prophylaxis [13]. Otherwise, clinical management generally follows standard of care recommended for all patients with heart failure. Standard medical therapy eventually includes blocking the activity of angiotensin II, either by using angiotensin II converting enzyme (ACE) inhibitors or angiotensin receptor blockers [11]. Despite standard medical therapy with drugs such as ACE inhibitors, heart failure almost always progresses.
We previously discovered abnormally elevated mitogen-activated protein kinase activities in hearts of LmnaH222P/H222P mice, which develop cardiomyopathy recapitulating that caused by LMNA mutations in humans [14]. This abnormal hyperactivation of mitogen-activated protein kinase signaling occurs in hearts of LmnaH222P/H222P mice prior to the onset of any clinically detectable disease, suggesting that it is a primary factor in pathogenesis [14,15]. Inhibitions of the extracellular signal-regulated kinase 1/2 (ERK1/2), Jun N-terminal kinase and p38α branches of this signaling pathway all have some beneficial effects in LmnaH222P/H222P mice [16-19]. In particular, treatment with selumetinib, an inhibitor of mitogen-activated protein kinase kinase 1/2 (MEK1/2), the enzyme that activates ERK1/2, improves left ventricular ejection fraction (fractional shortening), decreases cardiac fibrosis and prolongs survival in these mice [20]. However, MEK1/2 inhibition has not been compared to any standard heart failure drugs, which would be a necessary step in potentially translating this novel therapy to human subjects. Furthermore, in human patients MEK1/2 inhibition would potentially be added to other standard heart failure therapies. We therefore compared early treatment with the MEK1/2 inhibitor selumetinib to treatment with the ACE inhibitor benazepril in LmnaH222P/H222P mice and examined the combination of these two drugs after the development of cardiac dysfunction.
2. Material and Methods
2.1. Mice
LmnaH222P/H222P mice were bred and genotyped as previously described [21]. Mice were fed chow and housed in a disease-free barrier facility with 12h/12h light/dark cycles. The Institutional Animal Care and Use Committee at Columbia University Medical Center approved the use of animals and the study protocol.
2.2. Treatment protocol
Selumetinib (Selleck Chemicals) and benazepril (Sigma-Aldrich) were dissolved in DMSO (Sigma-Aldrich). The placebo control consisted of the same volume of DMSO. Selumetinib was administered at a dose of 1.0 mg/kg/day at benazepril at a dose of 10 mg/kg/day by intraperitoneal injection using a 27 5/8-gauge syringe.
2.3. Transthoracic echocardiography
Mice were anesthetized with 1.5% isoflurane inhalation and placed on a heating pad (37°C). Echocardiography was performed by independent cardiologists using a Vevo 770 ultrasound with a 30 MHz transducer applied to the chest wall (VisualSonics). Cardiac ventricular dimensions were measured in 2D mode and M-mode 3 times for the number of animals indicated.
2.4. Statistical analysis
Values were compared using two-way ANOVA (Tukey post hoc correction) or Student t-test with Welch's correction. Statistical analyses were performed using Prism (GraphPad Software).
3. Results
3.1. Comparison of MEK1/2 inhibition to ACE inhibition in LmnaH222P/H222P mice
We initiated treatment of male LmnaH222P/H222P mice with either 1.0 mg/kg/day of the MEK1/2 inhibitor selumetinib, 10 mg/kg/day of the ACE inhibitor benazepril or vehicle placebo (dimethylsulfoxide, DMSO) at 8 weeks of age and continued until the mice were 16 weeks. At 8 weeks of age, these mice are asymptomatic with normal heart function but by 16 weeks they have left ventricular dilatation and decreased fractional shortening [21]. We performed transthoracic echocardiography on mice in the three groups at 16 weeks of age and measured heart rate, left ventricular end diastolic diameter and left ventricular end systolic diameter and calculated fractional shortening (Table 1).
Table 1.
Echocardiographic results at 16 weeks of age for LmnaHH222P/HH222P mice treated with placebo (DMSO), benazepril or selumetinib (n = 7 mice per group); values are means ± standard errors of means
| Drug | HR (/min) | LVEDD (mm) | LVESD (mm) | FS (%) |
|---|---|---|---|---|
| DMSO | 498 ± 7 | 4.0 ± 0.2 | 3.3 ± 0.4 | 19.0 ± 5.9 |
| benazepril | 497 ± 9 | 3.9 ± 0.2 | 2.9 ± 0.1 | 25.8 ± 2.4* |
| selumetinib | 501 ± 9 | 3.7 ± 0.2 | 2.8 ± 0.1* | 30.7 ± 5.3** |
HR, heart rate; LVEDD, left ventricular end diastolic diameter; LVESD, left ventricular end systolic diameter; FS, left ventricular fractional shortening.
P<0.05
P<0.005 compared to DMSO.
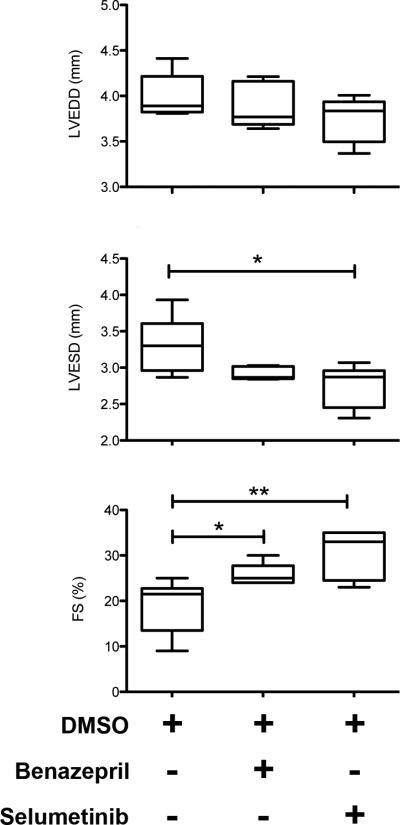
Mice treated with benazepril had no significant differences in left ventricular end diastolic or end systolic diameters compared to placebo-treated mice (Fig. 1). Benazepril treatment did however lead to statistically significant improvement in left ventricular fractional shortening. In contrast, statistically significantly smaller left ventricular end systolic diameter was observed in mice treated with selumetinib compared to those treated with placebo; they also had a significantly increased left ventricular fractional shortening (Fig. 1). There was a trend toward a greater improvement in fractional shortening with selumetinib compared to benazepril; however, the difference was not significant (P = 0.08).
Fig. 1.
Box-and-whisker plots showing mean left ventricular end diastolic diameter (LVEDD), left ventricular end systolic diameter (LVESD) and left ventricular fractional shortening (FS) in 16-week old male LmnaH222P/H222P mice treated with DMSO (n = 7), benazepril (n = 7) or selumetinib (n = 7). Values are shown as 25th to 75th percentiles of the ranked set of data values. The line in the middle is the median. Whiskers (Tukey method) extend down to the minimum value and up to the maximum value. *P<0.05, **P<0.005.
3.2. Combined MEK1/2 inhibition and ACE inhibition in LmnaH222P/H222P mice
At 16 weeks, male LmnaH222P/H222P mice have significantly increased left ventricular end diastolic and end systolic diameters compared to wild type mice [16,18,21]. They also have depressed cardiac contractility, with fractional shortening decreased by 10% to 40% compared to wild type mice. Given that ACE inhibitors are a current treatment initiated in almost all human patients with heart failure, we assessed the potential benefit of adding the MEK1/2 inhibitor selumetinib to benazepril in LmnaH222P/H222P mice after heart dysfunction occurred at 16 weeks of age. We initiated treatment of male LmnaH222P/H222P mice with either 10 mg/kg/day of benazepril alone or 1.0 mg/kg/day of selumetinib plus 10 mg/kg/day of benazepril at 16 weeks of age and continued it until the mice were 20 weeks. We performed transthoracic echocardiography on mice in both groups at 20 weeks of age and measured heart rate, left ventricular end diastolic diameter and left ventricular end systolic diameter and calculated fractional shortening (Table 2).
Table 2.
Echocardiography results at 20 weeks of age for LmnaHH222P/H222P mice treated with benazepril (n=9) or benzapril plus selumetinib (n=5); values are means ± standard errors of means
| Drug(s) | HR (/min) | LVEDD (mm) | LVESD (mm) | FS (%) |
|---|---|---|---|---|
| benazepril | 497 ± 9 | 4.3 ± 0.2 | 3.7 ± 0.3 | 12.5 ± 2.9 |
| benazepril + selumetinib | 501 ± 9 | 4.1 ± 0.3 | 3.4 ± 0.3 | 16.0 ± 2.2* |
HR, heart rate; LVEDD, left ventricular end diastolic diameter; LVESD, left ventricular end systolic diameter; FS, left ventricular factional shortening.
P<0.05
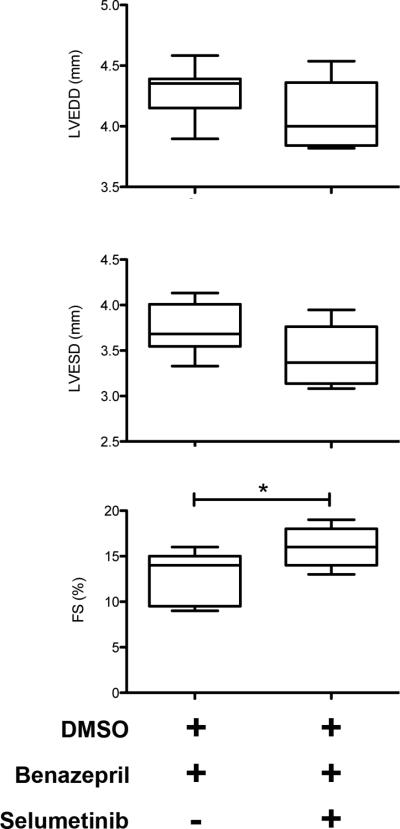
Treatment of LmnaH222P/H222P mice with both selumetinib and benazepril compared to benazepril alone lead to a trend towards smaller left ventricular end diastolic and end systolic diameters in LmnaH222P/H222P mice at 20 weeks of age (Fig. 2). However, the differences did not reach statistical significance. Combined treatment gave a statistically significant improvement in left ventricular fractional shortening compared to benazepril alone (Fig. 2). Hence, ACE inhibition and MEK1/2 inhibition had a synergistic effect on left ventricular function in LmnaH222P/H222P mice.
Fig. 2.
Box-and-whisker plots showing mean left ventricular end diastolic diameter (LVEDD), left ventricular end systolic diameter (LVESD) and left ventricular fractional shortening (FS) in 20-week old male LmnaH222P/H222P mice treated with benazepril (n = 9) or benazepril plus selumetinib (n = 5). Values are shown as 25th to 75th percentiles of the ranked set of data values. The line in the middle is plotted as the median. Whiskers (Tukey method) extend down to the minimum value and up to the maximum value. *P<0.05.
4. Discussion
Inhibition of angiotensin II activity is a well-established approach to the treatment of patients with severe chronic heart failure [22]. While mostly studied in acquired dilated cardiomyopathy, ACE inhibition is generally implicated in patients with primary genetic cardiomyopathy as well [23,24]. There are no published reports on the efficacy of ACE inhibitors in patients with dilated cardiomyopathy caused by LMNA mutation. However, an ACE inhibitor plus a beta-blocker may be beneficial in patients with Duchenne muscular dystrophy, who also have a primary genetic cardiomyopathy [25,26]. Hence, the effects of inhibiting the renin-angiotensin-aldosterone axis may have beneficial in all or most forms of cardiomyopathy and heart failure. Cardiac dysfunction and heart failure, especially in patients with primary genetic cardiomypathies, progress despite such treatment. Hence, standard therapies such as ACE inhibition should ideally be combined with specific therapies targeted at primary pathogenic mechanisms that may be operative in cardiomyopathies of different genetic etiologies.
We have shown that hearts of LmnaH222P/H222P mice have abnormally elevated ERK1/2 activity prior to the onset of clinical disease [14,15]. Pharmacological blockade of ERK1/2 activity in these mice has beneficial effects including improved left ventricular fractional shortening, decreased cardiac fibrosis and prolonged survival [16,18,20]. Our current results show that blocking either ERK1/2 activity with a MEK1/2 inhibitor or angiotensin II activity with an ACE inhibitor has beneficial effects on left ventricular fractional shortening when started before the onset of significant heart dysfunction. Perhaps more significantly, we show that adding a MEK1/2 inhibitor to an ACE inhibitor after the onset of left ventricular dysfunction in LmnaH222P/H222P mice has significantly enhanced beneficial effects on left ventricular fractional shortening compared to an ACE inhibitor alone. While human patients may be on other medications such as beta-blockers and spironolactone, our results in model mice show that addition of a MEK1/2 inhibitor has beneficial effects beyond at least one standard of care intervention for cardiomyopathy caused by LMNA mutation. These preclinical results also provide further rationale for a clinical trial of a MEK1/2 inhibitor in such patients.
Both ACE and MEK1/2 inhibition are beneficial on cardiac function in Lmna cardiomyopathy.
MEK1/2 inhibitor has beneficial effects beyond ACE inhibition for Lmna cardiomyopathy.
These results provide further preclinical rationale for a clinical trial of a MEK1/2 inhibitor.
Acknowledgments
Funding
This research was supported by grants from the Los Angeles Thoracic and Cardiovascular Foundation and the United States National Institutes of Health (grant number R01AR048997).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
Drs Muchir and Worman are inventors on a pending United States patent application on methods for treating and/or preventing cardiomyopathies by ERK and JNK inhibition filed by the Trustees of Columbia University in the City of New York.
References
- 1.Bonne G, Di Barletta MR, Varnous S, et al. Mutations in the gene encoding lamin A/C cause autosomal dominant Emery-Dreifuss muscular dystrophy. Nat. Genet. 1999;21:285–288. doi: 10.1038/6799. [DOI] [PubMed] [Google Scholar]
- 2.Fatkin D, MacRae C, Sasaki T, et al. Missense mutations in the rod domain of the lamin A/C gene as causes of dilated cardiomyopathy and conduction-system disease. N. Engl. J. Med. 1999;341:1715–1724. doi: 10.1056/NEJM199912023412302. [DOI] [PubMed] [Google Scholar]
- 3.Muchir A, Bonne G, van der Kooi AJ, et al. Identification of mutations in the gene encoding lamins A/C in autosomal dominant limb girdle muscular dystrophy with atrioventricular conduction disturbances (LGMD1B) Hum. Mol. Genet. 2000;9:1453–1459. doi: 10.1093/hmg/9.9.1453. [DOI] [PubMed] [Google Scholar]
- 4.Brodsky GL, Muntoni F, Miocic S, et al. Lamin A/C gene mutation associated with dilated cardiomyopathy with variable skeletal muscle involvement. Circulation. 2000;101:473–476. doi: 10.1161/01.cir.101.5.473. [DOI] [PubMed] [Google Scholar]
- 5.Bonne G, Mercuri E, Muchir A, et al. Clinical and molecular genetic spectrum of autosomal dominant Emery-Dreifuss muscular dystrophy due to mutations of the lamin A/C gene. Ann. Neurol. 2000;48:170–180. [PubMed] [Google Scholar]
- 6.Taylor MR, Fain PR, Sinagra G, et al. Natural history of dilated cardiomyopathy due to lamin A/C gene mutations. J. Am. Coll. Cardiol. 2003;41:771–780. doi: 10.1016/s0735-1097(02)02954-6. [DOI] [PubMed] [Google Scholar]
- 7.Parks SB, Kushner JD, Nauman D, et al. Lamin A/C mutation analysis in a cohort of 324 unrelated patients with idiopathic or familial dilated cardiomyopathy. Am. Heart J. 2008;156:16161–9. doi: 10.1016/j.ahj.2008.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arbustini E, Pilotto A, Repetto A, et al. Autosomal dominant dilated cardiomyopathy with atrioventricular block: a lamin A/C defect-related disease. J. Am. Coll. Cardiol. 2002;39:981–990. doi: 10.1016/s0735-1097(02)01724-2. [DOI] [PubMed] [Google Scholar]
- 9.van Berlo JH, de Voogt WG, van der Kooi AJ, et al. Meta-analysis of clinical characteristics of 299 carriers of LMNA gene mutations: do lamin A/C mutations portend a high risk of sudden death? J. Mol. Med. 2005;83:79–83. doi: 10.1007/s00109-004-0589-1. [DOI] [PubMed] [Google Scholar]
- 10.Pasotti M, Klersy C, Pilotto A, et al. Long-term outcome and risk stratification in dilated cardiolaminopathies. J. Am. Coll. Cardiol. 2008;52:1250–1260. doi: 10.1016/j.jacc.2008.06.044. [DOI] [PubMed] [Google Scholar]
- 11.Lu JT, Muchir A, Nagy PL, et al. LMNA cardiomyopathy: cell biology and genetics meet clinical medicine. Dis. Model. Mech. 2011;4:562–568. doi: 10.1242/dmm.006346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Rijsingen IA, Arbustini E, Elliott PM, et al. Risk factors for malignant ventricular arrhythmias in lamin a/c mutation carriers a European cohort study. J. Am. Coll. Cardiol. 2013;59:493–500. doi: 10.1016/j.jacc.2011.08.078. [DOI] [PubMed] [Google Scholar]
- 13.Meune C, Van Berlo JH, Anselme F, et al. Primary prevention of sudden death in patients with lamin A/C gene mutations. N. Engl. J. Med. 2006;354:209–210. doi: 10.1056/NEJMc052632. [DOI] [PubMed] [Google Scholar]
- 14.Muchir A, Pavlidis P, Decostre V, et al. Activation of MAPK pathway links LMNA mutations to cardiomyopathy in Emery-Dreifuss muscular dystrophy. J. Clin. Invest. 2007;117:1282–1293. doi: 10.1172/JCI29042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choi JC, Muchir A, Wu W, et al. Temsirolimus activates autophagy and ameliorates cardiomyopathy caused by lamin A/C gene mutation. Sci. Transl. Med. 2012;4:144ra102. doi: 10.1126/scitranslmed.3003875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muchir A, Shan J, Bonne G, et al. Inhibition of extracellular signal-regulate kinase signaling to prevent cardiomyopathy caused by mutation in the gene encoding A-type lamins. Hum. Mol. Genet. 2009;18:241–247. doi: 10.1093/hmg/ddn343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu W, Shan J, Bonne G, et al. Pharmacological inhibition of c-Jun N-terminal kinase signaling prevents cardiomyopathy caused by mutation in LMNA gene. Biochim. Biophys. Acta. 2010;1802:632–638. doi: 10.1016/j.bbadis.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu W, Muchir A, Shan J, et al. Mitogen activated protein kinase inhibitors improve heart function and prevent fibrosis in cardiomyopathy caused by lamin A/C gene mutation. Circulation. 2011;123:53–61. doi: 10.1161/CIRCULATIONAHA.110.970673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muchir A, Wu W, Choi JC, et al. Abnormal p38α mitogen-activated protein kinase signaling in dilated cardiomyopathy caused by lamin A/C gene mutation. Hum. Mol. Genet. 2012;21:4325–4333. doi: 10.1093/hmg/dds265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muchir A, Reilly SA, Wu W, et al. Treatment with selumetinib preserves cardiac function and improves survival in cardiomyopathy caused by mutation in the lamin A/C gene. Cardiovasc. Res. 2012;93:311–319. doi: 10.1093/cvr/cvr301. [DOI] [PubMed] [Google Scholar]
- 21.Arimura T, Helbling-Leclerc A, Massart C, et al. Mouse model carrying H222P-Lmna mutation develops muscular dystrophy and dilated cardiomyopathy similar to human striated muscle laminopathies. Hum. Mol. Genet. 2005;14:155–169. doi: 10.1093/hmg/ddi017. [DOI] [PubMed] [Google Scholar]
- 22.Packer M. Vasodilator and inotropic therapy for severe chronic heart failure: passion and skepticism. J. Am. Coll. Cardiol. 1983;2:841–852. doi: 10.1016/s0735-1097(83)80230-7. [DOI] [PubMed] [Google Scholar]
- 23.Taylor MR, Carniel E, Mestroni L. Cardiomyopathy, familial dilated. Orphanet J. Rare Dis. 2006;1:27. doi: 10.1186/1750-1172-1-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2012;14:803–869. doi: 10.1093/eurjhf/hfs105. [DOI] [PubMed] [Google Scholar]
- 25.Ogata H, Ishikawa Y, Ishikawa Y, et al. Beneficial effects of beta-blockers and angiotensin-converting enzyme inhibitors in Duchenne muscular dystrophy. J. Cardiol. 2009;53:72–78. doi: 10.1016/j.jjcc.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 26.Viollet L, Thrush PT, Flanigan KM, et al. Effects of angiotensin-converting enzyme inhibitors and/or beta blockers on the cardiomyopathy in Duchenne muscular dystrophy. Am. J. Cardiol. 2012;110:98–102. doi: 10.1016/j.amjcard.2012.02.064. [DOI] [PubMed] [Google Scholar]