Abstract
Vitamin D is an essential steroid hormone, with well-established effects on mineral metabolism, skeletal health, and recently established effects on the cardiovascular and immune systems. Vitamin D deficiency is highly prevalent and evidence is mounting that it contributes to the morbidity and mortality of multiple chronic diseases, including systemic lupus erythematosus (SLE). Patients with SLE avoid the sun because of photosensitive rashes and potential for disease flare, so adequate oral supplementation is critical. This review will describe the prevalence of vitamin D deficiency in patients with SLE, identify risk factors for deficiency, describe the consequences of deficiency, and review current vitamin D recommendations for patients with rheumatic diseases.
Vitamin D is an essential steroid hormone with well-established effects on mineral metabolism, skeletal health, and more recently established profound effects on cardiovascular and immune system health.1 Lifestyle factors have led to an increased prevalence of vitamin D deficiency, while improved availability and reliability of 25-hydroxyvitamin D (25(OH)D) testing have led to better awareness of widespread deficiency. It recently has become apparent that vitamin D deficiency contributes to the morbidity and mortality of multiple chronic diseases. Because patients with systemic lupus erythematosus (SLE) are told to avoid the sun, a common trigger of disease flares, vitamin D deficiency is even more prevalent in SLE patients than in the general population.2,3
This review will describe the prevalence of vitamin D deficiency in patients with SLE, identify risk factors for deficiency, describe the consequences of deficiency, and review current vitamin D recommendations for patients with SLE and other rheumatic diseases.
Prevalence of Vitamin D Deficiency
Vitamin D Deficiency is Common and Starts Early
Vitamin D deficiency is a global health problem and is being detected at all ages, including newborns, with widespread deficiency during pregnancy.4 Out of 100 infants born in South Carolina, 46% had fetal cord blood 25(OH)D under 11 ng/ml, which are levels associated with the development of rickets.4 In Michigan, 50% of mothers and 65% of their newborn infants were severely deficient at a 25(OH)D level less than 12 ng/ml.5
Despite growing awareness of vitamin D deficiency and an exponential rise in the frequency of testing in laboratories across the United States, in at least some populations, deficiency remains a growing problem. Insufficient levels of 25(OH)D, defined as less than 30 ng/mL, have risen from approximately 40% from 1988–1994 to approximately 70% during 2001–2004 among Caucasians, with an increase in insufficient levels from 88% to 97% among African Americans during the same periods of time.6 This data from the National Health and Nutrition Examination Survey finds nearly all African Americans and most Mexican-Americans (90%) have vitamin D insufficiency.6
Vitamin D Deficiency in Patients with Lupus
It is notable that the same ethnic disparities seen in the prevalence of vitamin D deficiency are seen in the prevalence of SLE, with African Americans and Hispanics having a disproportionately higher risk for developing SLE and having the most severe disease manifestations. Several methods have been used to examine potential links between vitamin D status and SLE, including case-control, cohort, and retrospective observational studies. The best measure of vitamin D availability is serum level of 25(OH)D, since dietary intake alone is not an adequate surrogate marker of vitamin D status.7
In one study comparing 123 recently diagnosed cases with SLE and 240 age- and sex-matched healthy controls, a trend toward lower 25(OH)D levels in cases compared to controls was noted, which was statistically significant in Caucasians.8 Levels of 25(OH)D were significantly lower among African Americans, compared to Caucasians (mean 15.9 vs 31.3 ng/ml, respectively). Overall, 67% of the subjects were vitamin D insufficient, with deficiency significantly more likely in patients with renal disease or photosensitivity, or both, adjusting for race, season, age, and smoking.8
Multiple studies since have confirmed that the majority of patients with SLE have insufficient levels of 25(OH)D, even if taking vitamin D supplementation,9 although the average supplement dose remains only 400 IU to 800 IU daily. One report found anti-vitamin D antibodies in 4% of patients with SLE, possibly contributing to vitamin D clearance10; however, this remains to be confirmed in other SLE populations.
Risk Factors for Deficiency
Traditional Risk Factors
The major source of vitamin D is sun exposure. Under the influence of ultraviolet B (UVB) radiation, 7-dehydroxy-cholesterol in the skin is photoconverted to previtamin D3 (cholecalciferol). Time of day, season, latitude, altitude, clothing, sunscreen use, pigmentation, and age are all factors that influence the effectiveness of this photoconvertion by UVB. Those with darker skin pigmentation who are living at latitudes more distant from the equator are especially prone to vitamin D deficiency, due to the ability of melanin to protect from harmful UV radiation, often at the expense of vitamin D synthesis if UVB exposure is not adequate to compensate.11 This explains, in part, the alarmingly high prevalence of vitamin D deficiency seen among African Americans and Hispanic Americans.
Emerging Risk Factors
More attention is being given now to medications, such as corticosteroids, that accelerate the catabolism of 25(OH)D and 1,25(OH)2D (the active form of vitamin D). Patients taking corticosteroids often require higher daily doses of vitamin D to maintain adequate levels, as do patients with malabsorption. Additionally, with the obesity epidemic hitting many parts of the world and adipose tissue serving as a “sink hole” for vitamin D, it is important to include vitamin D deficiency as one of the risks associated with obesity.12
Consequences of Deficiency for Patients with SLE
Vitamin D in Fracture Prevention
Patients with SLE have a higher risk for osteoporosis and fragility fractures, compared to age-matched controls.13 Vitamin D deficiency is one of several osteoporosis risk factors common among patients with SLE, including high disease activity, renal disease, corticosteroid use, and premature ovarian failure from cytotoxic medications such as cyclophosphamide.14 Since most patients with SLE have multiple disease-associated and traditional osteoporosis risk factors, bone mineral density loss tends to run a rapid course, making vitamin D status even more important.
Two recent meta-analyses of randomized controlled trials, eight for falls (N = 2426) and 12 for non-vertebral fractures (N = 42,279), showed that higher-dose vitamin D intake reduced fall risk by 19% and fracture risk by 15% to 29%.15 Despite the evidence, a recent study found that even among community-based patients with SLE and risk factors for fracture, such as corticosteroid use, osteoporosis prophylaxis was suboptimal, with only 56% to 58% taking calcium and vitamin D.16
Cardiovascular Disease Risk with Low Vitamin D
Patients with SLE are at a much higher risk of cardiovascular disease at a much earlier age. In addition to its musculoskeletal effects, vitamin D plays a cardioprotective role. The Framingham Offspring Study (N = 1739) found that 25(OH)D levels lower than 15 ng/ml increased the risk of a first cardiovascular event by 62% in hypertensive patients (p = 0.01).17
In a cross-sectional study of 181 females with SLE, Wu and colleagues18 found lower 25(OH)D levels to be associated with several cardiovascular risk factors in the univariate model. Once adjustments were made for other known cardiovascular risk factors, this association was no longer seen; however, it may be that the study was underpowered to account for the strong correlation between 25(OH)D level and obesity.
In contrast to previous studies, Freedman and colleagues found a positive correlation between a one-time measurement of 25(OH)D and carotid and aortic calcification among 340 African Americans with type 2 diabetes.19 Limitations include the cross-section design, low mean 25(OH)D among all the participants, plus only 4% of participants were taking calcium or vitamin D. At this point, these limited findings should not diminish the importance of addressing vitamin D deficiency in all populations, including African Americans. Attention to vitamin D status is especially important in light of numerous studies showing improved cardiovascular disease (CVD) end points with higher 25(OH)D levels, including one recent randomized trial of African Americans showing significantly improved arterial stiffness with vitamin D repletion using a 2000 IU daily dose.20
Malignancy and Overall Mortality
Among the general population, having a 25(OH)D level lower than 20 ng/ml is associated with an increased risk of dying from breast, colon, ovarian, and prostate cancer.1 Administration of 1100 IU of vitamin D daily over 4 years was shown in a randomized controlled trial in 1179 postmenopausal females to significantly reduce all-cancer risk.21 Impressively, a meta-analysis of 18 randomized controlled trials showed that participants randomized to vitamin D supplementation experienced fewer deaths compared to those randomized to placebo.22
Immune System Effects of Vitamin D Deficiency
In the 1980s, researchers observed high expression of a vitamin D receptor (VDR) in lymphocytes and macrophages, sparking interest in a potential role of vitamin D in immunity.23 T lymphocytes, B lymphocytes, and dendritic cells each express VDR and produce the enzymes 1α-hydroxylase and 24-hydroxylase; therefore, making them capable of producing the active form of vitamin D, 1,25(OH)2D, locally in a paracrine manner.24 Several hundred vitamin D-regulated genes have been identified, including many involved with the innate and adaptive immune system.
Immunologic effects of 1,25(OH)2D include decreasing Th1 CD4+ T cells and cytokines, increasing regulatory T cells, downregulating T-cell driven IgG production, inhibiting the differentiation of dendritic cells, and preventing the proliferation of activated B cells.25–28 The overall effect of 1,25(OH)2D is enhancement of protective innate immune responses, while maintaining self-tolerance by dampening over-zealous adaptive immune responses.
Studies of cord blood have found vitamin D-dependent differences in cytokine profiles, even at birth, with low levels of 25(OH)D correlating significantly with low levels of the anti-inflammatory cytokine IL-10.29 The long-term effects of vitamin D deficiency in utero and in early childhood, during critical periods of immune system development, are being investigated.
Influence on Lupus Disease Activity
Although studies of 25(OH)D levels and disease activity in SLE have not had consistent results, the two largest studies to date both show a significant correlation between higher disease activity and lower 25(OH)D.27,30 Data from 165 patients with SLE from three centers showed significantly higher disease activity among patients with severe vitamin D deficiency [25(OH)D equal or less than 10 ng/ml], compared to those with less severe deficiency (p = 0.026).27 Among 378 patients with SLE from several European and Israeli cohorts, serum 25(OH)D was found to be inversely related to disease activity (p = 0.018).30 Improving vitamin D status among patients with SLE may benefit other common manifestations as well, such as fatigue31 and cognitive dysfunction.32
Current Recommendations for Patients with Lupus
Unlike other vitamins, currently very little of our daily vitamin D comes from food. Many experts are recommending increased vitamin D fortification of common foods to help counteract widespread deficiency. But for now, oral vitamin D supplementation is needed for most, if not all, patients with SLE. As our knowledge expands, we may find out that higher thresholds are needed for optimal health; however, at this time, the minimally adequate level of 25(OH)D is 30 ng/ ml. In many labs, the 25(OH)D assay is still quite expensive (ranging from $100 to $200 per test). So, it seems reasonable to test once at baseline and then at 3 months following a change in vitamin D dosing, but no more frequent testing than that is necessary.
A phase I study of daily oral vitamin D3 showed that doses up to 4000 IU/day for 3 months was safe and well-tolerated among African American patients with SLE. We now await results of an ongoing multi-center randomized controlled trial of daily vitamin D3 that is comparing up to 800 IU daily with 2000 IU or 4000 IU daily for reducing interferon-alpha expression among patients with SLE (http://clinicaltrials.gov/ct2/show/NCT00710021).
Until prospective trial results are available, many experts would recommend correcting vitamin D deficiency with 50,000 IU capsule of vitamin D2 weekly for 8 weeks, followed by either 50,000 IU of vitamin D2 every 2 to 4 weeks or by 1000 IU to 2000 IU of vitamin D3 daily.1 The dose required to achieve and maintain adequate levels of 25(OH)D depends on the starting level, with roughly 100 IU of additional daily oral vitamin D3 required to raise the serum 25(OH)D level by 1 ng/ml.33 Keep in mind that it takes approximately 3 months to achieve a steady state once supplementation is started, so rechecking a 25(OH)D should not be done any sooner than 3 months.34 Individual responses may vary and known risk factors for deficiency should be taken into account.
Conclusions
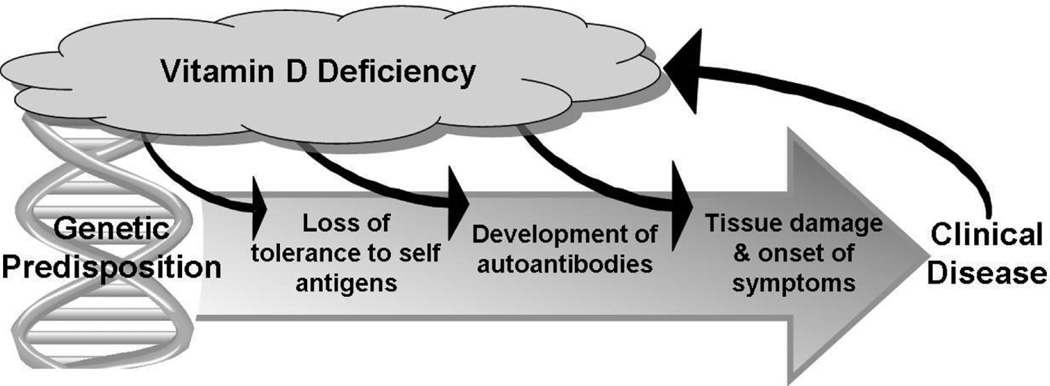
It is well established that many people have inadequate levels of 25(OH)D, particularly patients with SLE, who have additional risk factors for deficiency inherent to SLE. Evidence is accumulating that vitamin D plays a key role in the pathogenesis and progression of autoimmunity (Fig. 1). We hold out hope that something as safe, inexpensive, and widely available as vitamin D turns out to be effective as a disease-suppressing intervention for patients with SLE. In addition to the potential benefit of vitamin D replacement on SLE activity, patients will also avoid the excess morbidity and mortality associated with vitamin D deficiency. Continued research will help us better understand the role of vitamin D as immunomodulatory and determine the ideal range of serum 25(OH)D for musculoskeletal, cardiovascular, and immune health.
Figure 1.
Proposed mechanism for the influence of vitamin D deficiency on the development and progression of SLE. Left untreated, the cycle of vitamin D deficiency will continue due to the sun avoidance and photosensitivity associated with having SLE.
Acknowledgment
This work has been supported in part by a grant from the National Institutes of Health (Kamen NIH 1K23AR052364-01A2).
Footnotes
Disclosure Statement
The author has no financial or proprietary interest in the subject matter or materials discussed in the manuscript, including, but not limited to, employment, consultancies, stock ownership, honoraria, and paid expert testimony.
References
- 1.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 2.Kamen DL, Aranow C. The link between vitamin D deficiency and systemic lupus erythematosus. Curr Rheumatol Rep. 2008;10(4):273–280. doi: 10.1007/s11926-008-0044-3. [DOI] [PubMed] [Google Scholar]
- 3.Damanhouri LH. Vitamin D deficiency in Saudi patients with systemic lupus erythematosus. Saudi Med J. 2009;30(10):1291–1295. [PubMed] [Google Scholar]
- 4.Basile LA, Taylor SN, Wagner CL, et al. Neonatal vitamin D status at birth at latitude 32 degrees 72’: evidence of deficiency. J Perinatol. 2007;27(9):568–571. doi: 10.1038/sj.jp.7211796. [DOI] [PubMed] [Google Scholar]
- 5.Lee JM, Smith JR, Philipp BL, et al. Vitamin D deficiency in a healthy group of mothers and newborn infants. Clin Pediatr (Phila) 2007;46(1):42–44. doi: 10.1177/0009922806289311. [DOI] [PubMed] [Google Scholar]
- 6.Ginde AA, Liu MC Camargo CA Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med. 2009;169(6):626–632. doi: 10.1001/archinternmed.2008.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cutolo M, Otsa K, Paolino S, et al. Vitamin D involvement in rheumatoid arthritis and systemic lupus erythaematosus. Ann Rheum Dis. 2009;68(3):446–447. doi: 10.1136/ard.2008.093476. [DOI] [PubMed] [Google Scholar]
- 8.Kamen DL, Cooper GS, Bouali H, et al. Vitamin D deficiency in systemic lupus erythematosus. Autoimmun Rev. 2006;5(2):114–117. doi: 10.1016/j.autrev.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 9.Toloza SM, Cole DE, Gladman DD, et al. Vitamin D insufficiency in a large female SLE cohort. Lupus. 2010;19(1):13–19. doi: 10.1177/0961203309345775. [DOI] [PubMed] [Google Scholar]
- 10.Carvalho JF, Blank M, Kiss E, et al. Anti-vitamin D, vitamin D in SLE: preliminary results. Ann N Y Acad Sci. 2007;1109:550–557. doi: 10.1196/annals.1398.061. [DOI] [PubMed] [Google Scholar]
- 11.Shoenfeld N, Amital H Shoenfeld Y. The effect of melanism and vitamin D synthesis on the incidence of autoimmune disease. Nat Clin Pract Rheumatol. 2009;5(2):99–105. doi: 10.1038/ncprheum0989. [DOI] [PubMed] [Google Scholar]
- 12.Looker AC. Do body fat and exercise modulate vitamin D status? Nutr Rev. 2007;65(8 Pt 2):S124–S126. doi: 10.1301/nr.2007.aug.s124-s126. [DOI] [PubMed] [Google Scholar]
- 13.Rhew EY, Lee C, Eksarko P, et al. Homocysteine, bone mineral density, and fracture risk over 2 years of followup in women with and without systemic lupus erythematosus. J Rheumatol. 2008;35(2):230–236. [PubMed] [Google Scholar]
- 14.Becker A, Fischer R, Scherbaum WA, Schneider M. Osteoporosis screening in systemic lupus erythematosus: impact of disease duration and organ damage. Lupus. 2001;10(11):809–814. doi: 10.1177/096120330101001108. [DOI] [PubMed] [Google Scholar]
- 15.Bischoff-Ferrari HA, Shao A, Dawson-Hughes B, et al. Benefit-risk assessment of vitamin D supplementation. Osteoporos Int. 2010;21(7):1121–1132. doi: 10.1007/s00198-009-1119-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmajuk G, Yelin E, Chakravarty E, et al. Osteoporosis screening, prevention, and treatment in systemic lupus erythematosus: application of the systemic lupus erythematosus quality indicators. Arthritis Care Res (Hoboken) 2010;62(7):993–1001. doi: 10.1002/acr.20150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang TJ, Pencina MJ, Booth SL, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117(4):503–511. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu PW, Rhew EY, Dyer AR, et al. 25-hydroxyvitamin D and cardiovascular risk factors in women with systemic lupus erythematosus. Arthritis Rheum. 2009;61(10):1387–1395. doi: 10.1002/art.24785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freedman BI, Wagenknecht LE, Hairston KG, et al. Vitamin d, adiposity, and calcified atherosclerotic plaque in african-americans. J Clin Endocrinol Metab. 2010;95(3):1076–1083. doi: 10.1210/jc.2009-1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.London GM, Guerin AP, Verbeke FH, et al. Mineral metabolism and arterial functions in end-stage renal disease: potential role of 25-hydroxyvitamin D deficiency. J Am Soc Nephrol. 2007;18(2):613–620. doi: 10.1681/ASN.2006060573. [DOI] [PubMed] [Google Scholar]
- 21.Lappe JM, Travers-Gustafson D, Davies KM, et al. Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr. 2007;85(6):1586–1591. doi: 10.1093/ajcn/85.6.1586. [DOI] [PubMed] [Google Scholar]
- 22.Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007;167(16):1730–1737. doi: 10.1001/archinte.167.16.1730. [DOI] [PubMed] [Google Scholar]
- 23.Deluca HF, Cantorna MT. Vitamin D: its role and uses in immunology. FASEB J. 2001;15(14):2579–2585. doi: 10.1096/fj.01-0433rev. [DOI] [PubMed] [Google Scholar]
- 24.Kamen DL, Tangpricha V. Vitamin D and molecular actions on the immune system: modulation of innate and autoimmunity. J Mol Med. 2010;88(5):441–450. doi: 10.1007/s00109-010-0590-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arnson Y, Amital H, Shoenfeld Y. Vitamin D and autoimmunity: new aetiological and therapeutic considerations. Ann Rheum Dis. 2007;66(9):1137–1142. doi: 10.1136/ard.2007.069831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen S, Sims GP, Chen XX, et al. Modulatory effects of 1,25-dihydroxyvitamin D3 on human B cell differentiation. J Immunol. 2007;179(3):1634–1647. doi: 10.4049/jimmunol.179.3.1634. [DOI] [PubMed] [Google Scholar]
- 27.Ben-Zvi I, Aranow C, Mackay M, et al. The impact of vitamin D on dendritic cell function in patients with systemic lupus erythematosus. PLoS One. 2010;5(2):e9193. doi: 10.1371/journal.pone.0009193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Linker-Israeli M, Elstner E, Klinenberg JR, et al. Vitamin D(3) and its synthetic analogs inhibit the spontaneous in vitro immunoglobulin production by SLE-derived PBMC. Clin Immunol. 2001;99(1):82–93. doi: 10.1006/clim.2000.4998. [DOI] [PubMed] [Google Scholar]
- 29.Zittermann A, Dembinski J, Stehle P. Low vitamin D status is associated with low cord blood levels of the immunosuppressive cytokine interleukin-10. Pediatr Allergy Immunol. 2004;15(3):242–246. doi: 10.1111/j.1399-3038.2004.00140.x. [DOI] [PubMed] [Google Scholar]
- 30.Amital H, Szekanecz Z, Szucs G, et al. Serum concentrations of 25-OH vitamin D in patients with systemic lupus erythematosus (SLE) are inversely related to disease activity: is it time to routinely supplement patients with SLE with vitamin D? Ann Rheum Dis. 2010;69(6):1155–1157. doi: 10.1136/ard.2009.120329. [DOI] [PubMed] [Google Scholar]
- 31.Ruiz-Irastorza G, Gordo S, Olivares N, et al. Changes in vitamin D levels in patients with systemic lupus erythematosus: Effects on fatigue, disease activity, and damage. Arthritis Care Res (Hoboken) 2010;62(8):1160–1165. doi: 10.1002/acr.20186. [DOI] [PubMed] [Google Scholar]
- 32.Przybelski RJ, Binkley NC. Is vitamin D important for preserving cognition? A positive correlation of serum 25-hydroxyvitamin D concentration with cognitive function. Arch Biochem Biophys. 2007;460(2):202–205. doi: 10.1016/j.abb.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 33.Heaney RP. Vitamin D in health and disease. Clin J Am Soc Nephrol. 2008;3(5):1535–1541. doi: 10.2215/CJN.01160308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hollis BW, Wagner CL. Assessment of dietary vitamin D requirements during pregnancy and lactation. Am J Clin Nutr. 2004;79(5):717–726. doi: 10.1093/ajcn/79.5.717. [DOI] [PubMed] [Google Scholar]