Abstract
In a retrospective analysis of childhood thyroid nodules, 18% were radiographic incidentalomas and 41% were discovered by a clinician's palpation; 40% were discovered by patients' families. The latter group had the largest nodules and highest rates of thyroid cancer metastasis, suggesting opportunities for earlier detection through annual well-child visits.
Keywords: Thyroid Cancer, Thyroid Nodule, Incidentaloma, Ultrasound
Thyroid cancer, the most common endocrine malignancy, usually presents as a thyroid nodule and its outcome is improved by early diagnosis and treatment. Although most thyroid nodules are benign, the cancer risk of a thyroid nodule is greater in children than in adults1, and rates of thyroid cancer metastasis and extrathyroidal extension are much higher in children.2, 3 Understanding how childhood thyroid nodules are detected could help develop recommendations to improve rates of early diagnosis.
Methods
We retrospectively reviewed the medical records of all patients up to 18 years of age evaluated in our thyroid clinic between July 1997 and March 2011 who proved to have one or more thyroid nodule ≥1 cm at ultrasound. Data recorded included age, sex, nodule size, and the findings of operative pathology. Indications for biopsy and thyroid surgery have been previously described1 and, throughout the course of this study, adhered to current consensus guidelines of the American Thyroid Association.4
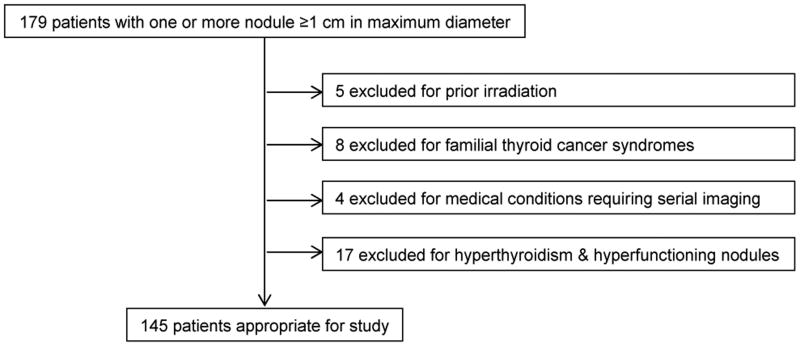
To focus on sporadic thyroid nodules, we excluded five children with a history of prior neck irradiation and eight others with familial thyroid cancer syndromes. To avoid radiographic detection bias, we also excluded four individuals with medical conditions requiring serial imaging (one with cystic fibrosis and three childhood cancer survivors). Finally, seventeen children with hyperfunctioning nodules were excluded with the reasoning that their coexisting hyperthyroidism may have confounded or delayed the diagnosis of their nodules.
The remaining 145 patients were considered appropriate for study (Figure). The method of nodule discovery was determined in most (n =120) through medical record review, which was facilitated by our thyroid clinic's standardized nursing intake form that includes the open-ended question of “who found the thyroid nodule”. The remaining families were invited to participate in a prospective telephone survey to ask who found the thyroid nodule, and this was completed in 21 cases. In total, data were available in 97% (141 of 145) of potential study subjects.
Patient features were entered into the REDCap data capture tool5 and potential associations with the method of nodule detection examined by post-hoc comparison by Sidak-adjusted critical p-value (continuous variables) or cell-specific chi-squared statistic (categories). P values <0.05 were considered significant. Research was approved by our institutional review boards.
Results
Methods of Nodule Discovery
Eighteen percent (26 of 141) of the study population had nodules discovered as radiographic incidentalomas. The most common indication for these studies was neck trauma (n = 8), followed by neck/arm pain (n =6), lymphadenopathy (n = 5), autoimmune thyroiditis (n = 3; imaging requested to quantify diffuse thyromegaly), headache (n = 2), pneumonia (n = 1), and scoliosis (n = 1).
Twenty seven percent (38 of 141) of the children in this series were discovered to have nodules by physical examinations performed at well-child visits and another 14% (20 of 141) were detected by clinician palpation at sick visits (n = 12) or subspecialty consultations (n = 8). All sick visits were scheduled for the complaint of upper respiratory infection, and thus included palpation of the anterior neck and cervical lymph nodes. Similarly, subspecialty consultations were in clinics (endocrinology, allergy, gynecology, or anesthesiology) that standardly perform neck palpation.
Forty percent (57 of 141) of families stated that the thyroid nodule was first noted by the patient (n = 29), parent (n = 20), other family members (n =6), or acquaintances (n = 2; one neighbor and one patient's schoolmate).
Associations between Method of Nodule Discovery and Other Patient Features
After grouping patients by method of nodule discovery, we compared patient features across groups (Table). No significant difference in age of presentation (p = 0.78) or number of nodules per patient (p = 0.48) was found. However, compared with the other groups, those with radiographic incidentalomas had the lowest female:male (1.9:1; p = 0.009) and the lowest cancer rate (4%; p = 0.02). In contrast, nodules self-discovered by families had the highest female:male ratio (13.2:1), a much higher cancer prevalence (25%), and the highest rates of thyroid cancer metastasis (64%). Median dominant nodule size varied significantly across all four groups (p <0.0001), with radiographically detected nodules being the smallest (1.4 cm) and self-discovered nodules being the largest (2.8 cm).
Table 1. Associations between Method of Nodule Discovery and Patient Features.
| Patient Features | Median (range) or N (%) | P† | |||
|---|---|---|---|---|---|
| Radiographic incidentaloma | Palpated at sick/consult visit | Palpated at well exam | Discovered by family | ||
| Patients | 26 (18%) | 20 (14%) | 38 (27%) | 57 (40%) | |
| Age, yr | 15.8 (11.1–18.9) | 15.6 (6.6–18.9) | 15.3 (5.4–18.9) | 15.2 (5.5–18.9) | 0.78 |
| Females:males | 17:9 (65:35%)* | 16:4 (80:20%) | 32:6 (84:16%) | 53:4 (93:7%)** | 0.009 |
| Nodules ≥1 cm | 1 (1–2) | 1 (1–6) | 1 (1–3) | 1 (1–10) | 0.48 |
| Dominant nodule diameter, mm | 14 (10–46)* | 21 (10–54) | 25 (12–42) | 28 (11–64)** | <0.0001 |
| Thyroid cancer | 1 (4%)* | 6 (30%) | 13 (34%) | 14 (25%) | 0.02 |
| Metastasis‡ | 0 (0%) | 2 (33%) | 7 (54%) | 9 (64%) | 0.69 |
Significantly lower or
significantly higher than in other groups, according to post-hoc comparison by Sidak-adjusted critical p-value (continuous variables) or cell-specific chi-squared statistic (categories).
Testing for equal distribution in all groups, including 4 patients with unknown method of discovery (data not shown), by Kruskal-Wallis test (continuous variables), or Fisher exact test (dichotomous features).
Among patients with thyroid cancer. All patients with “Metastasis” had lymph node metastases and, in addition, one child in the “Discovered by family” group also had diffuse pulmonary metastases.
Discussion
Our study indicates that, although many pediatric nodules are recognized by a clinician's exam, the majority are discovered either as radiographic incidentalomas or by the patient's family. In addition, we observed significant associations between the method of nodule discovery, cancer prevalence, and nodule size.
Radiographically detected nodules were the smallest and many were not palpable. The smallest nodules detected by palpation were those discovered at sick or consultation visits that required focused examination of the neck, followed by those recognized at routine well-child visits, and finally those discovered by the patients' families themselves. Although this retrospective analysis could not control for variables such the nodules' firmness or rates of growth, one interpretation of this pattern is that an opportunity exists to promote earlier detection of childhood thyroid cancers by encouraging compliance with annual well-child visits and the routine inclusion of thyroid palpation in pediatric primary care.
For palpable abnormalities concerning for thyroid nodules, measuring serum TSH prior to subspecialty referral is useful to expedite imaging triage (radioiodine scintigraphy if TSH is suppressed; vs. neck ultrasonography and possible biopsy if TSH is normal or high) to address cancer risk 1. Discrete nodules warrant evaluation even in children with the preexisting diagnosis of autoimmune thyroiditis, as the cancer risk of nodules in this subgroup is similar to that of nodules in the general pediatric population1.
Even though the prognosis of most children with thyroid cancer is favorable2, 3, early detection improves outcome4 and may avoid the obligate risks of aggressive treatments required to treat advanced stages of disease. In this context, it is worth noting that nodules that were self-discovered by families represented 41% of the cancers diagnosed in this cohort and that, within this group, 64% had lymph node metastases and 7% had pulmonary spread. Although an appropriate index of suspicion for thyroid neoplasia is important for all primary care providers, the relative rarity of thyroid nodules in children presents a special challenge to pediatricians as it decreases their opportunity to diagnose thyroid pathology and to become familiar with associated physical examination findings.2, 6, 7 This challenge can be overcome by training in thyroid palpation technique and by repetition through annual well-child appointments.
Figure. Study Population.
Acknowledgments
We are indebted to the patients and families evaluated in this series and to Christian Botte, MD (supported by the Harvard Catalyst | The Harvard Clinical and Translational Science Center [National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health 8UL1TR000170-05, and financial contributions from Harvard University and its affiliated academic health care centers), for his expertise and assistance in REDCap database design.
Supported by a donation from the Murray Family and the National Institutes of Health (DK076099 and DK007699).
Footnotes
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gupta A, Ly S, Castroneves LA, Frates MC, Benson CB, Feldman HA, et al. A standardized assessment of thyroid nodules in children confirms higher cancer prevalence than in adults. The Journal of clinical endocrinology and metabolism. 2013;98:3238–45. doi: 10.1210/jc.2013-1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waguespack SG, Francis G. Initial management and follow-up of differentiated thyroid cancer in children. J Natl Compr Canc Netw. 2010;8:1289–300. doi: 10.6004/jnccn.2010.0095. [DOI] [PubMed] [Google Scholar]
- 3.Hung W, Sarlis NJ. Current controversies in the management of pediatric patients with well-differentiated nonmedullary thyroid cancer: a review. Thyroid. 2002;12:683–702. doi: 10.1089/105072502760258668. [DOI] [PubMed] [Google Scholar]
- 4.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 5.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rallison ML, Dobyns BM, Keating FR, Jr, Rall JE, Tyler FH. Thyroid nodularity in children. Jama. 1975;233:1069–72. [PubMed] [Google Scholar]
- 7.Hogan AR, Zhuge Y, Perez EA, Koniaris LG, Lew JI, Sola JE. Pediatric thyroid carcinoma: incidence and outcomes in 1753 patients. The Journal of surgical research. 2009;156:167–72. doi: 10.1016/j.jss.2009.03.098. [DOI] [PubMed] [Google Scholar]