Abstract
Yersinia pestis biovar Microtus is considered to be a virulent to larger mammals, including guinea pigs, rabbits and humans. It may be used as live attenuated plague vaccine candidates in terms of its low virulence. However, the Microtus strain’s protection against plague has yet to be demonstrated in larger mammals. In this study, we evaluated the protective efficacy of the Microtus strain 201 as a live attenuated plague vaccine candidate. Our results show that this strain is highly attenuated by subcutaneous route, elicits an F1-specific antibody titer similar to the EV and provides a protective efficacy similar to the EV against bubonic plague in Chinese-origin rhesus macaques. The Microtus strain 201 could induce elevated secretion of both Th1-associated cytokines (IFN-γ, IL-2 and TNF-α) and Th2-associated cytokines (IL-4, IL-5, and IL-6), as well as chemokines MCP-1 and IL-8. However, the protected animals developed skin ulcer at challenge site with different severity in most of the immunized and some of the EV-immunized monkeys. Generally, the Microtus strain 201 represented a good plague vaccine candidate based on its ability to generate strong humoral and cell-mediated immune responses as well as its good protection against high dose of subcutaneous virulent Y. pestis challenge.
Keywords: Yersinia pestis, plague, live attenuated vaccine, Rhesus macaques, protection
Introduction
Plague is a zoonotic disease caused by Gram-negative bacterium Yersinia pestis, which is usually transmitted to humans from infected rodents via the bite of an infected flea.1Historically, plague was a lethal infectious disease afflicting human populations, leading to millions of deaths. Plague has been classified as a re-emerging infectious disease recently by the World Health Organization2 and has attracted a considerable attention because of its potential misuse as an agent of biological warfare or bioterrorism.3 Although Y. pestis is the sole cause of plague, the disease may present clinically 3 main forms, including the bubonic, septicemic and pneumonic plagues. Patients with bubonic plague can develop secondary pneumonic or septic infection. Pneumonic plague can then be spread from person to person via respiratory droplets generated from the sneezing and coughing of patients.4Without timely and proper treatment, mortality is very high for plague.1
Currently, there is not an ideal plague vaccine for human use. Y. pestis killed whole cell vaccines only have a short protection against bubonic plague and are needed for frequent boosting to maintain immunity.5,6 Live attenuated vaccine EV provides the theoretical advantage of simultaneously priming immunity against many antigens, and is able to elicit both humoral response and cell-mediated immunity,7,8 and is effective against bubonic and pneumonic plague in humans, but it shows side effects of varying severity and has not been used in the Western world.5,9,10 Other types of live attenuated plague vaccines to induce protective immunity include the introduction of Y. pestis antigens in live attenuated Salmonella and Y. pseudotuberculosis etc. These live attenuated vectored vaccines could induce humoral, mucosal and cellular immunity, and be developed for mass vaccination against pneumonic plague via oral route.11-13However, these live attenuated vectored vaccines express a limited number of Y. pestis antigens. Recent studies are being focused on the development of acellular vaccines (subunit vaccines and DNA vaccines) containing F1 and LcrV antigens.14 Subunit vaccines based on F1 and/or LcrV are efficacious against both bubonic and pneumonic plagues in some experimental animals and had obvious advantages over killed whole cell vaccines in terms of safety and/or efficacy.15-18 However, mice vaccinated with F1 antigen alone fail to provide protection against the F1-negative Y. pestis infection.19 Thus, an F1+LcrV subunit vaccine is preferred.20 In addition, subunit vaccines based on F1 and LcrV antigens failed to fully protect African green monkeys, and the adequate evidence about whether or not they will protect humans has yet to be demonstrated.21,22 Our previous study23 and several reports7,24,25 have indicated that subunit vaccines in alhydrogel elicit robust humoral immunity, and their potential to prime effective cellular immunity has yet to be demonstrated. Several studies suggest that antibodies alone may not provide optimal protection against plague, and that vaccines harnessing both humoral and cellular defense mechanisms should provide superior defense.22,26 The DNA vaccines based on Y. pestis F1 and LcrV genes alone or in combination are efficacious against both bubonic and pneumonic plague.15,16,18 However, DNA vaccines usually elicit lower and slower immune responses than conventional vaccines, and gene gun immunization that delivers DNA-coated particles into the dermis of the skin needs to be used for improving immune responses.15,27 Taken together, the future studies of new plague vaccines should be focused on developing the subunit vaccines priming cell-mediated immune responses, DNA vaccines eliciting highly effective and quicker immune responses, the vectored vaccines expressing more protective antigens of Y. pestis in live attenuated Salmonella and Y. pseudotuberculosis etc or live attenuated Y. pestis vaccines with both highly attenuated property and protective efficacy in both animals and humans.
The major challenge in developing live attenuated Y. pestis vaccines is to reduce their virulence while maintaining their immunogenicity. A proper balance between attenuation and immunogenicity is required for developing an ideal live attenuated Y. pestis vaccine. To reduce the potential of reversion to virulence, several live attenuated mutants have been constructed based on conditionally virulent Y. pestis Pgm- strains.28-32 Constructing double-mutant strains based on Y. pestis Pgm- strains has an advantage over developing single mutants from virulent strains in terms of safety. Y. pestis biovar Microtus strains are thought to be avirulent to larger mammals, such as guinea pigs, rabbits and humans,33 which may be used as a parental strain to develop attenuated vaccines for humans because these strains have all known protective antigens.34 However, the Microtus strains’ protective efficacy against plague has yet to be demonstrated in larger mammals. In this study, we investigated the possibility of using Microtus strain 201 as a live attenuated plague vaccine candidate. Our results show that the Microtus strain 201 is highly attenuated in Chinese-origin rhesus macaque model of infection and provides effective protection against subcutaneous Y. pestis infection in this model.
Results
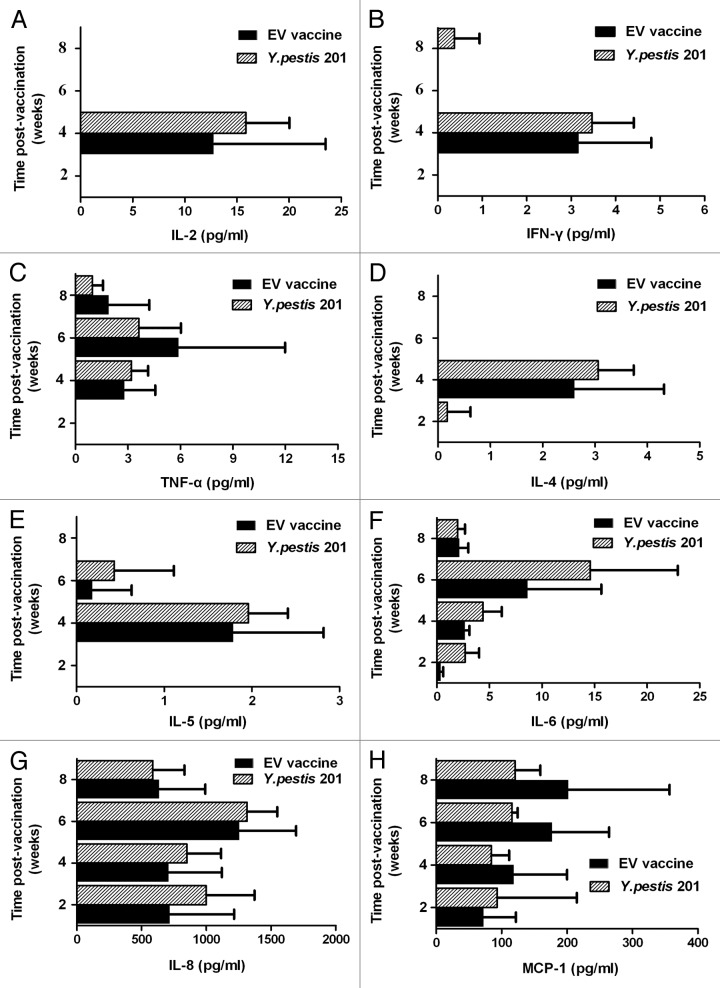
Antibody responses to F1 and V antigens
The titers of F1- or V-specific antibody in all immunized animals were determined on week 2, 4, 6, and 8 after primary immunization. The geometric mean of antibody titers and the standard error of the mean from each group of the animals were calculated from the data obtained by ELISA. The antibody response to F1 in 2 immunized groups of animals was shown in Figure 1. The statistical analysis showed that there was no significant anti-F1 IgG titer difference between the immunized animals with the EV and those with the Y. pestis 201 (P > 0.05). In contrast, anti-V IgG was undetectable in both groups of animals (data not shown). These results indicated that the Y. pestis 201 elicited a humoral immune response similar to the live attenuated vaccine EV.
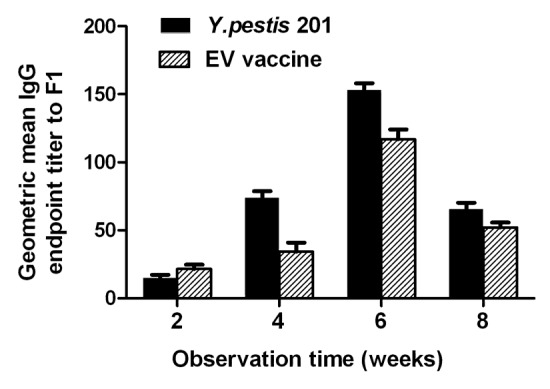
Figure 1. Development of IgG titers to F1 in Chinese-origin rhesus macaques immunized with the Y. pestis strain 201 and the EV vaccine on week 2, 4, 6, and 8 post immunization.
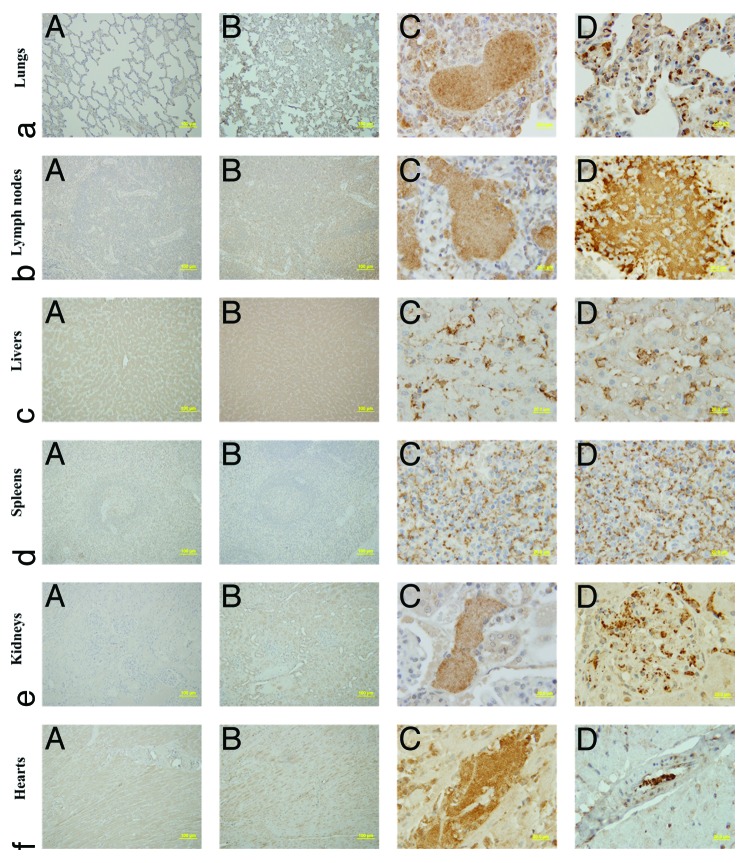
The Y. pestis 201 induces cytokine or chemokine production
To assess immune correlates contributing to the significant protection observed in the immunized animals with the Y. pestis 201, the release of cytokines and chemokines IFN-γ, TNF-α, IL-2, IL-4, IL-5, IL-6, IL-8, MCP-1, and RANTES was measured by Cytometric Bead Array between the 2- and 8-week (w) point of immunization (POI). Elevated levels of six cytokines IL-2 (Fig. 2A), IFN-γ (Fig. 2B), TNF-α (Fig. 2C), IL-4 (Fig. 2D), IL-5 (Fig. 2E), and IL-6 (Fig. 2F), and 2 chemokines IL-8 (Fig. 2G) and MCP-1 (Fig. 2H) were found in sera from the animals immunized with the Y. pestis 201 or the EV. In contrast, there was no elevated level of the chemokine RANTES in sera from the animals immunized with the Y. pestis 201 or the EV. ANOVA analysis showed that there was no significant IL-2, IFN-γ, TNF-α, IL-4, IL-5, IL-6, IL-8, or MCP-1 difference between the Y. pestis 201 and the EV groups (P > 0.05). The levels of IL-2, IFN-γ, IL-4, and IL-5 were elevated by the Y. pestis 201 or the EV immunization at 4-w POI, and reduced rapidly. Compared with above cytokines, significantly high level of IL-6, TNF-α, IL-8, and MCP-1 production was induced at early POI by the Y. pestis 201 or the EV, and maintained for a longer time.
Figure 2. Production of cytokines IFN-γ, TNF-α, IL-2, IL-4, IL-5, and IL-6 and chemokines IL-8, MCP-1 and RANTES in Chinese-origin rhesus macaques immunized with the Y. pestis strain 201 and the EV on week 2, 4, 6, and 8 post immunization. Cytokine or chemokine production was calculated by subtracting the cytokine or chemokine concentration in control animals from the concentration measured in the Y. pesti 201- or the EV-immunized animals.
Protective efficacy
Three groups of the immunized animals with a single dose of the Y. pestis 201, the EV or PBS were challenged with 1.74 × 109 CFU of virulent Y. pestis strain 141 by the subcutaneous route on week 9 post primary immunization, and followed by observation for 21 d. All (6/6) of the animals survived the challenge in the group vaccinated with the EV, and 83.3% (5/6) protection was observed in the group immunized with the Y. pestis 201 during the 21-d’s post-challenge observation. In contrast, 3 control animals all succumbed to a same dose of Y. pestis 141 challenge within 2–3 d. Log-rank (Mantel-Cox) Test analysis showed no survival difference between the Y. pestis 201 and the EV groups (P > 0.05).
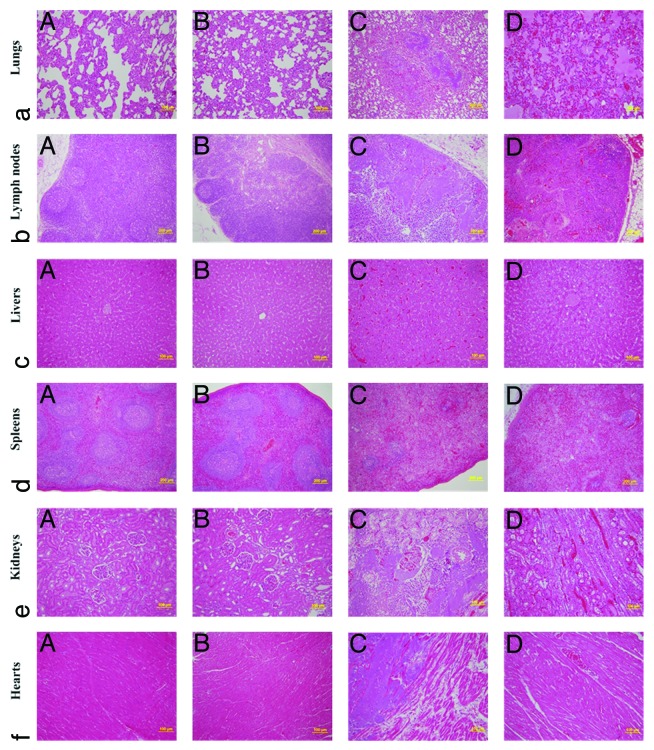
Localization of Y. pestis within organs
Microbiological examination showed that Y. pestis were isolated from lymph nodes, hearts, livers, spleens, and lungs of the dead animals, including one from the Y. pestis 201 group and control animals. The survivors were euthanized humanely and autopsied for microbiological analysis on day 21 post challenge. No Y. pestis were isolated from lymph nodes, hearts, livers, spleens, and lungs of these animals. These results indicate that the death of animals was caused by the systemic infection of Y. pestis, and Y. pestis have been eliminated from the survival animals.
The F1 antigen of Y. pestis was identified by immunohistochemistry staining in the formalin-fixed paraffin-embedded lungs, lymph node, liver, spleen, kidney, and heart tissues. Bacteria could be visualized as those expressing the F1 antigen (brown and yellow stain). Numerous bacteria were observed in the tissues of the control animals (Fig. 3D, a–f) and one dead animal from the Y. pestis 201 group (Fig. 3C, a–f), no bacteria were found in the tissues of the animals immunized with the EV or survivors immunized with 201 strain (Fig. 3A, a-f and B, a–f).
Figure 3. The F1 antigen of Y. pestis was identified by Immunohistochemitry staining. Bacteria were visualized as those expressing F1 antigen (brown and yellow stain). Numerous bacteria were observed in the tissues of lungs (a), lymph node (b), liver (c), spleen (d), kidney (e), and heart (f) of one dead animal of the Y. pestis 201 group (C) and control animals (D).
Clinical signs and histopathology
After immunization with the Y. pestis 201, no systemic symptoms were observed, but there was a red and swollen induration at the inoculation site in the immunized animals. After challenge with Y. pestis 141, all animals, including vaccinated and control animals, were observed to assess clinical manifestations during the 21-d’s post-challenge observation. Different degrees of pustules or skin ulcerations were observed at the site of the injection in majority of the immunized animals with the Y. pestis 201 or the EV 5∼8 d after challenge with Y. pestis 141, no other side effects were observed and all the vaccinated animals are in good spirits. By contrast, only a little red swelling was observed at the injection sites of the control animals because of their rapid death, but the control animals had lethargy after challenge with Y. pestis 141. Photographs taken from some animals immunized with the Y. pestis 201 (Fig. 4A and B) and the EV (Fig. 4C and D) exhibited skin ulcerations at the injection sites after challenge with Y. pestis 141. An animal with severe ulcer has an open sore in the skin that looks like a crater (Fig. 4C), whereas another animal with severe skin ulcer has extensive ulcerate at the injection sites (Fig. 4B). There was no difference between the animals immunized with the EV and those vaccinated with the 201 strain in the light of degree of skin ulcer and mental state. These results indicated that although the Y. pestis 201 or the EV could markedly elevate the survival rate, they failed to protect the immunized animals from skin lesion caused by Y. pestis infection.
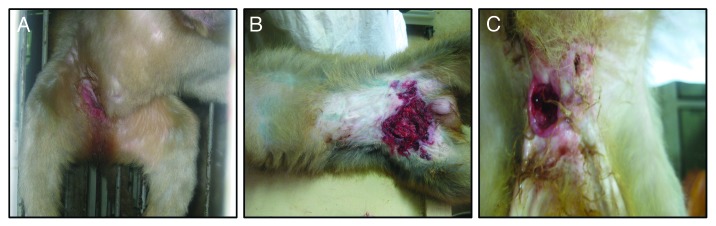
Figure 4. Skin ulcerations at the site of the injection in the immunized animals after challenge with Y. pestis 141. (A) Photo taken from the animal of the Y. pestis 201 group 8 d after challenge with virulent Y. pestis 141. (B) Photo taken from the animal of the Y. pestis 201 group 8 d after challenge with virulent Y. pestis 141. (C) Photo taken from the animals of the EV group 8 d after challenge with virulent Y. pestis 141.
The samples of heart, liver, spleen, lungs, kidneys and lymphoid nodes from the animals immunized with the Y. pestis 201, the EV and PBS were collected after challenge with Y. pestis 141 and fixed in 10% neutral buffered formalin. The tissues were trimmed, paraffin embedded, sectioned and stained with hematoxylin and eosin (H and E). The slides prepared from these organs were observed under light microscope for pathological changes. No changes in histopathology were found in all examined tissues from all survivors after challenge with Y. pestis 141 (Fig. 5A, a–f and B, a–f), whereas the control animals (Fig. 5D, a–f) and one dead animal from the Y. pestis 201 group (Fig. 5C, a–f) showed evident alterations in these tissues. Disappearance of recognizable lung tissue architecture and formulation of inflammatory cell focus mainly composed of lymphocytes were observed in the lung tissues of one dead animal from the Y. pestis 201 group (Fig. 5C, a), whereas edema, congestion and inflammatory cell infiltration were found in the lung tissues of the control animals (Fig. 5D, a). Lymph node tissues showed architectural deterioration and low numbers of lymphocytes in both one dead animal from the Y. pestis 201 group and the control animals, respectively (Fig. 5C, b and D, b). Slight congestion within sinus hepaticus and hepatic cell degeneration were observed in both one dead animal from the Y. pestis 201 group and the control animals, respectively (Fig. 5C, c and D, c). The spleen tissues of one dead animal from the Y. pestis 201 group and the control animals showed reduced amount of white pulp, acinuslienalis and lymphocytes (Fig. 5C, d and D, d). Interstitial lymphocyte infiltration and vascular engorgement were observed in both one dead animal from the Y. pestis 201 group and the control animals, respectively (Fig. 5C, e and D, e). Segmentation of cardiac muscle fibers and vascular engorgement were found in heart tissues of 1 dead animal from the Y. pestis 201 group and the control animals, respectively (Fig. 5C, f and D, f).
Figure 5. Histopathology of the tissues from the immunized animals and the control animals. Tissue sections were stained with hematoxylin and eosin for pathological examination after infection with Y. pestis. (A) Tissue sections from the animals immunized with the EV and then infected with virulent Y. pestis strain 141. (B) Tissue sections from the animal immunized with the Y. pestis 201 and then infected with virulent Y. pestis strain 141. (C) Tissue sections from one dead animal of the Y. pestis 201 group after challenge with virulent Y. pestis strain 141. (D) Tissue sections from the control animals after infection with virulent Y. pestis strain 141.
Discussion
Historically, live attenuated strains were the most effective type of plague vaccines, which were usually obtained from virulent isolates by continuous multiple passages on routine growth media at a temperature of 26–28 °C. Pigmentation (Pgm)-deficient strains of Y. pestis arise spontaneously during in vitro passage, which results in the attenuation of Y. pestis usually owing to deletion of a 102-kb region of the chromosome that encodes proteins related to iron utilization.35 The EV strain, a spontaneous Pgm mutant, was derived from the EV strain isolated by Girard and Robic from a human case of bubonic plague in Madagascar in 1926,36 and known as the most immunogenic derivative used for animals and humans. However, it can cause fatal plague in some non-human primates,37 and retains virulence when administered by the intranasal (i.n.) and intravenous (i.v.) routes.26,37,38 Recently, a case of lethal septicemic plague caused by an attenuated Pgm- mutant of Y. pestis UC91309 was reported in an U. S. laboratory, because the victim had hereditary hemochromatosis with abnormally high levels of iron deposition in liver tissue and antemortem serum samples.39Pgm-deficient vaccines are highly virulent to people with hemochromatosis, which ensures excess iron supply for vaccine strains with attenuated iron uptake. It is important to explore novel rationally attenuated Y. pestis strains with distinct functional roles as vaccine candidates for use against plague.
Y. pestis biovar Microtus strains have been proved to be avirulent to guinea pigs, rabbits and humans,33 but their virulence and protection in nonhuman primates has not been determined. In this study, although the LD50 of the Y. pestis strain 201 was not determined in Chinese-origin rhesus macaques, its virulence for Chinese-origin rhesus macaques was estimated to be more than 1010 CFU because all animals survived after immunization with 1.4 × 1010 CFU of the Y. pestis strain 201 by subcutaneous route. When the animals immunized with the Y. pestis 201 were challenged with high level of virulent Y. pestis strain 141 by the subcutaneous route, the Y. pestis 201 provided an effective protective efficacy similar to the EV. This is the first report that shows the biovar Microtus Y. pestis 201 strain is avirulent in Chinese-origin rhesus macaques. More importantly, this study first demonstrates the biovar Microtus Y. pestis 201 strain is able to provide effective protection against bubonic plague. When the immunized animals with the Y. pestis 201 or the EV were challenged with virulent Y. pestis 141, different degrees of pustules or skin ulcerations were observed at the site of the injection in majority of the animals 5∼8 d after infection. These results indicated that although the Y. pestis 201 or the EV could markedly elevate the survival rate, they failed to protect the immunized animals from skin lesion caused by high dose of virulent Y. pestis.
Although antibody level induced in vaccinated primates and rodents does not correlate with protective efficacy, it has long been recognized that humoral immunity plays an important role in protection against plague.21,40 Furthermore, it is suggested that vaccines effectively prime both humoral and cellular immunity could provide superior defense against pneumonic plague.7,8,41,42 To assess the nature of the immunological response caused by the Y. pestis 201, F1- or V-specific antibody titers representing humoral immune response, and Th1- or Th2-associated cytokines were determined in sera of the immunized animals. We observed that the Y. pestis 201 elicited a humoral immune response similar to the EV. However, both strains elicited higher anti-F1 IgG titer and undetectable anti-V IgG in both groups of animals. LcrV is a multifunctional protein secreted by the type III system, which both forms the translocation pore at the tip of the surface-exposed needle and provides protective immunity to Y. pestis infections.43-47 Although V-antigen is a surface-exposed protein, it is only localized at the tip of the needle and is not secreted as much as F1-antigen. This may explain why only a small amount of antibody to V-antigen is produced in animals immunized with the EV and the Y. pestis strain 201. Therefore, we suggested that V-antigen might not play an important role in humoral immunity when animals were immunized with live attenuated vaccines or KWC vaccines, compared with F1-antigen. Several previous studies have demonstrated that IFN-γ and TNF-α contribute to protection against a lethal systemic Y. pestis challenge, and that cytokine-mediated Th1-type cellular immunity is very important to overcome the immunosuppression induced by Y. pestis infection.7,31,48,49 In this study, we observed that the Y. pestis 201 or the EV induced not only the increase of IFN-γ and TNF-α production but also that of IL-2 secretion, revealing that the Y. pestis 201 or the EV could induce cytokine-mediated Th1-type cellular immune response in Chinese-origin rhesus macaque model. Moreover, the secretion of IL-4, IL-5, or IL-6 was significantly elevated in the immunized groups after immunization with the Y. pestis 201 or the EV. These results indicated that the Y. pestis 201 or the EV elicited a mixture of Th1 and Th2 responses, which could be particularly important in plague vaccines, because Th1 response is important for the clearance of intracellular pathogens, and Th2 response plays a role in the clearance of extracellular pathogens.50-52
Chemokines released from a variety of cells constitute a superfamily of small peptides that play a crucial role in trafficking and recruiting effector leukocytes to primary sites of immune responses and inflammations.53 In addition, chemokines were also found to mediate Th1 or Th2 type immune responses. The present study was undertaken to measure concentrations of the chemokine RANTES, IL-8, and MCP-1 in sera from the animals immunized with the Y. pestis 201 or the EV. Elevated levels of two chemokines IL-8, a mediator of Th1 type cellular immune responses,54 and MCP-1 predominantly chemotactic for Th2 cells,55 were observed in sera from the animals immunized with the Y. pestis 201 or the EV. These observations revealed that the protection provided by these 2 live attenuated vaccines was at least attributed to both the chemoattraction of IL-8 and MCP-1, and the modulation of Th1/Th2 balance. However, no elevated level of RANTES, a regulator for both Th1 and Th2 cell types,56 was observed in the two groups of immunized animals. This result seems to be consistent with a previous report, in which no elevated levels of MCP-1, MIP-1α, RANTES, MIP-1β, and IL-8 were found in sera of Indonesian-origin cynomolgus macaques within 96 h after aerosol infection with Y. pestis CO92, but the elevated concentration of MCP-1, MIP-1α or IL-8 was observed in some lung tissue 72 h after aerosol infection with Y. pestis CO92.57 No elevated levels of MCP-1 and IL-8 were observed in sera of the animals infected with Y. pestis CO92, which may be attributed to short-term of observation. However, in some lung tissue, the elevated concentration of MCP-1 and IL-8, not RANTES was observed, indicating that MCP-1 and IL-8 secreted earlier than RANTES or Y. pestis CO92 does not induce elevated level of RANTES in Indonesian-origin cynomolgus macaques.
To evaluate histopathologically the protective efficacy of the Y. pestis 201 and the EV, the heart, liver, spleen, lung, kidney, and lymph node tissues from the survivors, one dead animal of the Y. pestis 201 group and control animals were examined under microscopy. The survival animals did not display histopathological lesions in all the examined tissues, whereas the control animals and one dead animal of the Y. pestis 201 group showed different degrees of pathological alterations in the heart, liver, spleen, lung, kidney and lymph node tissues. Immunohistochemical staining and postmortem analysis also showed bacteria in all the examined organs of the control animals and one dead animal of the Y. pestis 201 group, whereas no bacteria were observed in the survival animals. However, in our previous study, when Chinese-origin rhesus macaques were challenged subcutaneously with 6 × 106 CFU of Y. pestis 141, no evident changes were observed in the heart tissues.58 Evidence from the present and previous studies suggests that high-dose challenge can cause histopathological lesions in heart tissues. In the present study, the tissues were only examined at 21 d after the challenge. The possibility of histopathological lesion and bacterial presence at earlier stages of infection should not be excluded. Postmortem analysis, immunohistochemical staining and histopathological examination demonstrated that the Y. pestis 201 and the EV can effectively protect Chinese-origin rhesus macaques from pathological changes in the examined organs and eliminate Y. pestis. The control animals died from the lesions of many organs caused specifically by Y. pestis infection. However, after challenge with Y. pestis 141, the majority of the vaccinated animals were shown different degrees of pustules or skin ulcerations at the site of the injection. The Y. pestis 201 or the EV seems to not protect the immunized animals from skin lesion caused by Y. pestis infection, but the lesions were healed within an observation of period of 21 d. This result perhaps precisely demonstrated the potential of the Y. pestis 201 or the EV.
The current study first demonstrates that the biovarMicrotus Y. pestis 201 strain is avirulent in non-human primates and able to provide effective protection against bubonic plague. The Microtus strain 201 represented a good plague vaccine candidate based on its ability to generate strong humoral and cell-mediated immune responses as well as its good protection against high dose of subcutaneous virulent Y. pestis challenge. However, its potential to provide effective protection against pneumonic plague has yet to be demonstrated. Pneumonic plague is the most dangerous and rapidly transmissible form of the disease,59 which can be spread from person-to-person via respiratory droplets generated from sneezing and coughing of the patients. Without timely and proper treatment, mortality is very high for pneumonic plague.1 It is imperative to develop a vaccine that can provide effective protection against pneumonic plague. It is suggested that vaccines effectively prime both humoral and cellular immunity could provide superior defense against pneumonic plague.7,8,41,42 The current study showed that immunization with the Y. pestis strain 201 could induce both cytokine-mediated Th1-type cellular immune response and Th2-type humoral immune response. Therefore, we speculate that the Y. pestis strain 201 might have the potential to provide effective protection against pneumonic plague. In the following studies, we will investigate whether the Y. pestis strain 201 can provide effective protection against pneumonic plague. In addition, we will further evaluate the virulence of the Y. pestis strain 201 by comparing with EV strain.
Materials and Methods
Bacterial strains and animals
The Y. pestis strain 201 was isolated from Microtusbrandti in Inner Mongolia, China and has LD50 of 3 CFU for BALB⁄c mice by the subcutaneous route, while the LD50 in the i.v.-infected mice was 1.9 CFU.60 Its major phenotypes are F1+ (able to produce fraction 1 capsule), LcrV+ (presence of V antigen), Pst+ (able to produce pesticin), and Pgm+ (pigmentation on Congo-red media). The genome contents of strain 201 were identical to Y. pestis strain 91001 according to our previous DNA microarray based comparative genomic analysis. Both strain 201 and strain 91001 belong to a newly established Y. pestis biovar, microtus,61 which is supposed to be avirulent to humans but highly lethal to mice.33 The live attenuated strain EV was obtained from the Lanzhou Institute of Biological Products (LIBP).
Chinese-origin rhesus macaques (2-y-old) were obtained from Laboratory Animal Research Center, Academy of Military Medical Science (licensed from the Ministry of Health in General Logistics Department of Chinese People’s Liberation Army, permit no. SCXK-2007-004). All protocols were approved by Committee of the Welfare and Ethics of Laboratory Animals, Beijing Institute of Microbiology and Epidemiology. Each animal was kept in a vertical dimension of stainless steel wire bottom cage, which has a perch and adequate vertical space to keep the whole body, including its tail, above the cage floor. All single-caged animals were raised in the same room with windows where they are social housing and see the outside world through windows. All animals were raised in an air-conditioned laboratory with an ambient temperature of 21–25 °C and a relative humidity of 40%–60%. Each animal was provided with gnawing sticks, a restricted diet of approximately 150 g of standard monkey keeping diet per day, and water was available ad libitum during the entire course of this study. Fresh fruit was given once daily to each of the animals who received their fresh fruit in the puzzle feeder. To alleviate the suffering of rhesus macaques, a minimum number of animals were used to ensure statistical significance. All moribund animals after the challenge with Y. pestis were euthanized by using pentobarbital sodium anesthesia. All animal experiments were conducted strictly in compliance with the Regulations of Good Laboratory Practice for nonclinical laboratory studies of drug issued by the National Scientific and Technologic Committee of People’s Republic of China.
Animal immunizations
Fifteen Chinese-origin rhesus macaques were randomly divided into 3 groups, including 2 experimental groups and 1 control group. Each one of 2 experimental groups contained 6 animals, and the PBS-immunized control group had 3 animals. Two experimental groups of animals were subcutaneously injected in the groin area with the Y. pestis 201 (1.4 × 1010 CFU) and the EV (1.57 × 1010 CFU), respectively. Each animal of the control group was subcutaneously given the same volume of PBS only.
Antigen-specific antibody assays
Blood samples were collected from the forelimb veins of the immunized animals on week 2, 4, 6, or 8 after primary immunization. Sera were assayed for the presence of F1- or V-specific IgG by a modified ELISA.62The titers of specific antibodies were estimated as the maximum dilution of serum giving an OD reading 0.2 units over background. Background values were obtained from serum samples collected from the PBS-immunized animals. Antibody endpoint titers per immunization group are presented as the geometric mean endpoint titers to F1 and V antigens.
Measurement of cytokines and chemokines
Sera were collected from the two experimental groups of animals on week 2, 4, 6, and 8 after primary immunization and from the control group of animals. The levels of cytokines and chemokines IFN-γ, TNF-α, IL-2, IL-4, IL-5, IL-6, IL-8, MCP-1, and RANTES were measured by Cytometric Bead Array (CBA) according to the manufacturer’s protocol (BD Biosciences). Data were analyzed by using FCAP Array 0.1 and BD Cytometric Bead Array 1.4 software assay. Cytokine production was calculated by subtracting the cytokine or chemokine concentration in control animals from the concentration measured in the Y. pesti 201- or the EV-immunized animals. The results are presented as the means of assays performed in each group at different time points.
Challenge with Y. pestis
Both immunized and naïve Chinese-origin rhesus macaques were challenged with the virulent Y. pestis 141 strain, which was isolated from Marmotahimalayana in Qinghai-Tibet plateau and has a median lethal dose (MLD) of 5.6 CFU for BALB/c mice, 17.8 CFU for guinea pigs and New Zealand White rabbits by the subcutaneous route. All the immunized Chinese-origin rhesus macaques were challenged with 1.74 × 109 CFU by the subcutaneous route in another side of groin area on week 9 after the primary immunization, and then, closely observed for 21 d. All the survival animals were euthanized humanely for a post-mortem examination. Hearts, livers, spleens, lungs and lymph nodes of the challenged animals were removed to confirm if Y. pestis was presented in these organs.
Histopathology
Tissues collected from dead animals were placed into 10% neutral buffered formalin, dehydrated through a serial alcohol gradient (70%, 80%, 90%, 95%, and 100%), cleared with xylene, infiltrated with wax, and then embedded in paraffin.63The surviving animals at Day 21 after the challenge were humanely euthanized by intraperitoneal injection of barbital sodium. As stated above, their tissues were removed and fixed in 10% neutral buffered formalin for paraffin block preparation. Tissue sections were stained with hematoxylin and eosin (HE) for histopathological examination.
Immunohistochemistry (IHC)
IHC staining was performed following the user’s manual of the PV-9000 Kit (ZSGB-Bio).64 Briefly, after the paraffin-embedded tissue sections were deparaffinized and rehydrated, the sections were subjected to antigen exposure in citrate buffer solution (0.1 M, pH 6.0) by microwaving at 95 °C for 20 min, and incubated with 3% H2O2 in methanol for 10 min to block endogenous peroxidase activity. The sections were incubated for 12 h with the purified rabbit anti-F1 antigen of Y. pestis polyclonal antibody at 4 °C, whereas the control spleen tissues were incubated in PBS. The sections were incubated with Polymer Helper for 20 min at 37 °C, and then with polyperoxidaseantirabbitIgG (ZSGB-Bio) for 10–20 min at 37 °C. The slides were stained with 3, 3′-diaminobenzidinetetrahydrochloride (DAB). Finally, the sections were rinsed, counterstained, dehydrated, cleaned, mounted, and examined under light microscopy.65
Statistical analysis
The differences of antibody titer, cytokines and chemokines between the Y. pestis 201 and the EV groups were compared by analysis of variance (ANOVA) with SARS 8.0 software. Survival difference between the Y. pestis 201 and the EV groups was analyzed by Log-rank (Mantel-Cox) Test. Probability values of <0.05 were taken as significant.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgment
Financial support for this study came from the National Natural Science Foundation of China (contract no. 81171529) and the National High Technology Research and Development Program of China (863 program) (contract no. 2012AA02A403).
References
- 1.Perry RD, Fetherston JD. Yersinia pestis--etiologic agent of plague. Clin Microbiol Rev. 1997;10:35–66. doi: 10.1128/cmr.10.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williamson ED. Plague vaccine research and development. J Appl Microbiol . 2001;91:606–8. doi: 10.1046/j.1365-2672.2001.01497.x. [DOI] [PubMed] [Google Scholar]
- 3.Riedel S. Plague: from natural disease to bioterrorism Proc (BaylUniv Med Cent) . 2005;18:116–24. doi: 10.1080/08998280.2005.11928049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang H, Cui Y, Wang Z, Wang X, Guo Z, Yan Y, Li C, Cui B, Xiao X, Yang Y, et al. A dog-associated primary pneumonic plague in Qinghai Province, China. Clin Infect Dis . 2011;52:185–90. doi: 10.1093/cid/ciq107. [DOI] [PubMed] [Google Scholar]
- 5.Russell P, Eley SM, Hibbs SE, Manchee RJ, Stagg AJ, Titball RW. A comparison of Plague vaccine, USP and EV76 vaccine induced protection against Yersinia pestis in a murine model. Vaccine. 1995;13:1551–6. doi: 10.1016/0264-410X(95)00090-N. [DOI] [PubMed] [Google Scholar]
- 6.Titball RW, Williamson ED. Yersinia pestis (plague) vaccines. Expert OpinBiolTher. 2004;4:965–73. doi: 10.1517/14712598.4.6.965. [DOI] [PubMed] [Google Scholar]
- 7.Parent MA, Berggren KN, Kummer LW, Wilhelm LB, Szaba FM, Mullarky IK, Smiley ST. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect Immun. 2005;73:7304–10. doi: 10.1128/IAI.73.11.7304-7310.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Philipovskiy AV, Smiley ST. Vaccination with live Yersinia pestis primes CD4 and CD8 T cells that synergistically protect against lethal pulmonary Y. pestis infection. Infect Immun. 2007;75:878–85. doi: 10.1128/IAI.01529-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morton M, Garmory HS, Perkins SD, O’Dowd AM, Griffin KF, Turner AK, Bennett AM, Titball RW. A Salmonella entericaserovarTyphi vaccine expressing Yersinia pestis F1 antigen on its surface provides protection against plague in mice. Vaccine. 2004;22:2524–32. doi: 10.1016/j.vaccine.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 10.Williamson ED, Eley SM, Griffin KF, Green M, Russell P, Leary SE, Oyston PC, Easterbrook T, Reddin KM, Robinson A, et al. A new improved sub-unit vaccine for plague: the basis of protection. FEMS Immunol Med Microbiol. 1995;12:223–30. doi: 10.1111/j.1574-695X.1995.tb00196.x. [DOI] [PubMed] [Google Scholar]
- 11.Rosenzweig JA, Chopra AK. The future of plague vaccines: hopes raised by a surrogate, live-attenuated recombinant vaccine candidate. Expert Rev Vaccines. 2012;11:659–61. doi: 10.1586/erv.12.34. [DOI] [PubMed] [Google Scholar]
- 12.Derbise A, CerdàMarín A, Ave P, Blisnick T, Huerre M, Carniel E, Demeure CE. An encapsulated Yersinia pseudotuberculosis is a highly efficient vaccine against pneumonic plague. PLoSNegl Trop Dis. 2012;6:e1528. doi: 10.1371/journal.pntd.0001528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sizemore DR, Warner EA, Lawrence JA, Thomas LJ, Roland KL, Killeen KP. Construction and screening of attenuated ΔphoP/Q Salmonella typhimurium vectored plague vaccine candidates. Hum VaccinImmunother. 2012;8:371–83. doi: 10.4161/hv.18670. [DOI] [PubMed] [Google Scholar]
- 14.Mizel SB, Graff AH, Sriranganathan N, Ervin S, Lees CJ, Lively MO, Hantgan RR, Thomas MJ, Wood J, Bell B. Flagellin-F1-V fusion protein is an effective plague vaccine in mice and two species of nonhuman primates. Clin Vaccine Immunol. 2009;16:21–8. doi: 10.1128/CVI.00333-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garmory HS, Freeman D, Brown KA, Titball RW. Protection against plague afforded by immunisation with DNA vaccines optimised for expression of the Yersinia pestis V antigen. Vaccine. 2004;22:947–57. doi: 10.1016/j.vaccine.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 16.Grosfeld H, Cohen S, Bino T, Flashner Y, Ber R, Mamroud E, Kronman C, Shafferman A, Velan B. Effective protective immunity to Yersinia pestis infection conferred by DNA vaccine coding for derivatives of the F1 capsular antigen. Infect Immun. 2003;71:374–83. doi: 10.1128/IAI.71.1.374-383.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leary SE, Griffin KF, Garmory HS, Williamson ED, Titball RW. Expression of an F1/V fusion protein in attenuated Salmonella typhimurium and protection of mice against plague. MicrobPathog. 1997;23:167–79. doi: 10.1006/mpat.1997.0141. [DOI] [PubMed] [Google Scholar]
- 18.Wang S, Heilman D, Liu F, Giehl T, Joshi S, Huang X, Chou TH, Goguen J, Lu S. A DNA vaccine producing LcrV antigen in oligomers is effective in protecting mice from lethal mucosal challenge of plague. Vaccine. 2004;22:3348–57. doi: 10.1016/j.vaccine.2004.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friedlander AM, Welkos SL, Worsham PL, Andrews GP, Heath DG, Anderson GW, Jr., Pitt ML, Estep J, Davis K. Relationship between virulence and immunity as revealed in recent studies of the F1 capsule of Yersinia pestis. Clin Infect Dis. 1995;21(Suppl 2):S178–81. doi: 10.1093/clinids/21.Supplement_2.S178. [DOI] [PubMed] [Google Scholar]
- 20.Heath DG, Anderson GW, Jr., Mauro JM, Welkos SL, Andrews GP, Adamovicz J, Friedlander AM. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine. 1998;16:1131–7. doi: 10.1016/S0264-410X(98)80110-2. [DOI] [PubMed] [Google Scholar]
- 21.Bashaw J, Norris S, Weeks S, Trevino S, Adamovicz JJ, Welkos S. Development of in vitro correlate assays of immunity to infection with Yersinia pestis. Clin Vaccine Immunol. 2007;14:605–16. doi: 10.1128/CVI.00398-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smiley ST. Current challenges in the development of vaccines for pneumonic plague. Expert Rev Vaccines. 2008;7:209–21. doi: 10.1586/14760584.7.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Qi Z, Zhou L, Zhang Q, Ren L, Dai R, Wu B, Wang T, Zhu Z, Yang Y, Cui B, et al. Comparison of mouse, guinea pig and rabbit models for evaluation of plague subunit vaccine F1+rV270. Vaccine. 2010;28:1655–60. doi: 10.1016/j.vaccine.2009.02.078. [DOI] [PubMed] [Google Scholar]
- 24.Do Y, Park CG, Kang YS, Park SH, Lynch RM, Lee H, Powell BS, Steinman RM. Broad T cell immunity to the LcrV virulence protein is induced by targeted delivery to DEC-205/CD205-positive mouse dendritic cells. Eur J Immunol. 2008;38:20–9. doi: 10.1002/eji.200737799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williamson ED, Eley SM, Stagg AJ, Green M, Russell P, Titball RW. A sub-unit vaccine elicits IgG in serum, spleen cell cultures and bronchial washings and protects immunized animals against pneumonic plague. Vaccine. 1997;15:1079–84. doi: 10.1016/S0264-410X(96)00303-9. [DOI] [PubMed] [Google Scholar]
- 26.Smiley ST. Immune defense against pneumonic plague. Immunol Rev. 2008;225:256–71. doi: 10.1111/j.1600-065X.2008.00674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bennett AM, Phillpotts RJ, Perkins SD, Jacobs SC, Williamson ED. Gene gun mediated vaccination is superior to manual delivery for immunisation with DNA vaccines expressing protective antigens from Yersinia pestis or Venezuelan Equine Encephalitis virus. Vaccine. 1999;18:588–96. doi: 10.1016/S0264-410X(99)00317-5. [DOI] [PubMed] [Google Scholar]
- 28.Anisimov AP, Shaikhutdinova RZ, Pan’kina LN, Feodorova VA, Savostina EP, Bystrova OV, Lindner B, Mokrievich AN, Bakhteeva IV, Titareva GM, et al. Effect of deletion of the lpxM gene on virulence and vaccine potential of Yersinia pestis in mice. J Med Microbiol. 2007;56:443–53. doi: 10.1099/jmm.0.46880-0. [DOI] [PubMed] [Google Scholar]
- 29.Feodorova VA, Pan’kina LN, Savostina EP, Sayapina LV, Motin VL, Dentovskaya SV, Shaikhutdinova RZ, Ivanov SA, Lindner B, Kondakova AN, et al. A Yersinia pestislpxM-mutant live vaccine induces enhanced immunity against bubonic plague in mice and guinea pigs. Vaccine. 2007;25:7620–8. doi: 10.1016/j.vaccine.2007.08.055. [DOI] [PubMed] [Google Scholar]
- 30.Okan NA, Mena P, Benach JL, Bliska JB, Karzai AW. The smpB-ssrA mutant of Yersinia pestis functions as a live attenuated vaccine to protect mice against pulmonary plague infection. Infect Immun. 2010;78:1284–93. doi: 10.1128/IAI.00976-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szaba FM, Kummer LW, Wilhelm LB, Lin JS, Parent MA, Montminy-Paquette SW, Lien E, Johnson LL, Smiley ST. D27-pLpxL, an avirulent strain of Yersinia pestis, primes T cells that protect against pneumonic plague. Infect Immun. 2009;77:4295–304. doi: 10.1128/IAI.00273-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Welkos S, Pitt ML, Martinez M, Friedlander A, Vogel P, Tammariello R. Determination of the virulence of the pigmentation-deficient and pigmentation-/plasminogen activator-deficient strains of Yersinia pestis in non-human primate and mouse models of pneumonic plague. Vaccine. 2002;20:2206–14. doi: 10.1016/S0264-410X(02)00119-6. [DOI] [PubMed] [Google Scholar]
- 33.Fan Z, Ruo Y, Wang S, Jin L, Zhou X, Liu J, Zhang Y, Li F. Microtusbrandti plague in the XilinGol Grassland was inoffensive to humans. Chin J Control Endem Dis. 1995;10:56–7. [Google Scholar]
- 34.Song Y, Tong Z, Wang J, Wang L, Guo Z, Han Y, Zhang J, Pei D, Zhou D, Qin H, et al. Complete genome sequence of Yersinia pestis strain 91001, an isolate avirulent to humans. DNA Res. 2004;11:179–97. doi: 10.1093/dnares/11.3.179. [DOI] [PubMed] [Google Scholar]
- 35.Fetherston JD, Schuetze P, Perry RD. Loss of the pigmentation phenotype in Yersinia pestis is due to the spontaneous deletion of 102 kb of chromosomal DNA which is flanked by a repetitive element. MolMicrobiol. 1992;6:2693–704. doi: 10.1111/j.1365-2958.1992.tb01446.x. [DOI] [PubMed] [Google Scholar]
- 36.Girard G. [IMMUNITY IN PLAGUE. ACQUISITIONS SUPPLIED BY 30 YEARS OF WORK ON THE “PASTEURELLA PESTIS EV” (GIRARD AND ROBIC) STRAIN] Biol Med (Paris) 1963;52:631–731. [PubMed] [Google Scholar]
- 37.Meyer KF, Smith G, Foster L, Brookman M, Sung M. Live, attenuated Yersinia pestis vaccine: virulent in nonhuman primates, harmless to guinea pigs. J Infect Dis. 1974;129(Suppl):S85–12. doi: 10.1093/infdis/129.Supplement_1.S85. [DOI] [PubMed] [Google Scholar]
- 38.Une T, Brubaker RR. In vivo comparison of avirulentVwa- and Pgm- or Pstr phenotypes of yersiniae. Infect Immun. 1984;43:895–900. doi: 10.1128/iai.43.3.895-900.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frank KM, Schneewind O, Shieh W-J. Investigation of a researcher’s death due to septicemic plague. N Engl J Med. 2011;364:2563–4. doi: 10.1056/NEJMc1010939. [DOI] [PubMed] [Google Scholar]
- 40.Green M, Rogers D, Russell P, Stagg AJ, Bell DL, Eley SM, Titball RW, Williamson ED. The SCID/Beige mouse as a model to investigate protection against Yersinia pestis. FEMS Immunol Med Microbiol. 1999;23:107–13. doi: 10.1111/j.1574-695X.1999.tb01229.x. [DOI] [PubMed] [Google Scholar]
- 41.Lee-Lewis H, Anderson DM. Absence of inflammation and pneumonia during infection with nonpigmentedYersinia pestis reveals a new role for the pgm locus in pathogenesis. Infect Immun. 2010;78:220–30. doi: 10.1128/IAI.00559-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fetherston JD, Kirillina O, Bobrov AG, Paulley JT, Perry RD. The yersiniabactin transport system is critical for the pathogenesis of bubonic and pneumonic plague. Infect Immun. 2010;78:2045–52. doi: 10.1128/IAI.01236-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fields KA, Nilles ML, Cowan C, Straley SC. Virulence role of V antigen of Yersinia pestis at the bacterial surface. Infect Immun. 1999;67:5395–408. doi: 10.1128/iai.67.10.5395-5408.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nilles ML, Williams AW, Skrzypek E, Straley SC. Yersinia pestisLcrV forms a stable complex with LcrG and may have a secretion-related regulatory role in the low-Ca2+ response. J Bacteriol. 1997;179:1307–16. doi: 10.1128/jb.179.4.1307-1316.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fields KA, Straley SC. LcrV of Yersinia pestis enters infected eukaryotic cells by a virulence plasmid-independent mechanism. Infect Immun. 1999;67:4801–13. doi: 10.1128/iai.67.9.4801-4813.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cowan C, Philipovskiy AV, Wulff-Strobel CR, Ye Z, Straley SC. Anti-LcrV antibody inhibits delivery of Yops by Yersinia pestis KIM5 by directly promoting phagocytosis. Infect Immun. 2005;73:6127–37. doi: 10.1128/IAI.73.9.6127-6137.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nilles ML, Fields KA, Straley SC. The V antigen of Yersinia pestis regulates Yopvectorial targeting as well as Yop secretion through effects on YopB and LcrG. J Bacteriol. 1998;180:3410–20. doi: 10.1128/jb.180.13.3410-3420.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nakajima R, Brubaker RR. Association between virulence of Yersinia pestis and suppression of gamma interferon and tumor necrosis factor alpha. Infect Immun. 1993;61:23–31. doi: 10.1128/iai.61.1.23-31.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parent MA, Wilhelm LB, Kummer LW, Szaba FM, Mullarky IK, Smiley ST. Gamma interferon, tumor necrosis factor alpha, and nitric oxide synthase 2, key elements of cellular immunity, perform critical protective functions during humoral defense against lethal pulmonary Yersinia pestis infection. Infect Immun. 2006;74:3381–6. doi: 10.1128/IAI.00185-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.O’Garra A. Cytokines induce the development of functionally heterogeneous T helper cell subsets. Immunity. 1998;8:275–83. doi: 10.1016/S1074-7613(00)80533-6. [DOI] [PubMed] [Google Scholar]
- 51.Sher A, Coffman RL. Regulation of immunity to parasites by T cells and T cell-derived cytokines. Annu Rev Immunol. 1992;10:385–409. doi: 10.1146/annurev.iy.10.040192.002125. [DOI] [PubMed] [Google Scholar]
- 52.Abbas AK, Murphy KM, Sher A. Functional diversity of helper T lymphocytes. Nature. 1996;383:787–93. doi: 10.1038/383787a0. [DOI] [PubMed] [Google Scholar]
- 53.Baggiolini M. Chemokines and leukocyte traffic. Nature. 1998;392:565–8. doi: 10.1038/33340. [DOI] [PubMed] [Google Scholar]
- 54.Sin J, Kim JJ, Pachuk C, Satishchandran C, Weiner DB. DNA vaccines encoding interleukin-8 and RANTES enhance antigen-specific Th1-type CD4(+) T-cell-mediated protective immunity against herpes simplex virus type 2 in vivo. J Virol. 2000;74:11173–80. doi: 10.1128/JVI.74.23.11173-11180.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nakajima H, Kobayashi M, Pollard RB, Suzuki F. Monocyte chemoattractant protein-1 enhances HSV-induced encephalomyelitis by stimulating Th2 responses. J LeukocBiol. 2001;70:374–80. [PubMed] [Google Scholar]
- 56.Lit LC, Wong C-K, Tam L-S, Li EK-M, Lam CW-K. Raised plasma concentration and ex vivo production of inflammatory chemokines in patients with systemic lupus erythematosus. Ann Rheum Dis. 2006;65:209–15. doi: 10.1136/ard.2005.038315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Koster F, Perlin DS, Park S, Brasel T, Gigliotti A, Barr E, Myers L, Layton RC, Sherwood R, Lyons CR. Milestones in progression of primary pneumonic plague in cynomolgus macaques. Infect Immun. 2010;78:2946–55. doi: 10.1128/IAI.01296-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tian G, Qiu Y, Qi Z, Wu X, Zhang Q, Bi Y, Yang Y, Li Y, Yang X, Xin Y, et al. Histopathological observation of immunized rhesus macaques with plague vaccines after subcutaneous infection of Yersinia pestis. PLoS One. 2011;6:e19260. doi: 10.1371/journal.pone.0019260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Feodorova VA, Corbel MJ. Prospects for new plague vaccines. Expert Rev Vaccines. 2009;8:1721–38. doi: 10.1586/erv.09.129. [DOI] [PubMed] [Google Scholar]
- 60.Yang F, Ke Y, Tan Y, Bi Y, Shi Q, Yang H, Qiu J, Wang X, Guo Z, Ling H, et al. Cell membrane is impaired, accompanied by enhanced type III secretion system expression in Yersinia pestis deficient in RovA regulator. PLoS One. 2010;5:e12840. doi: 10.1371/journal.pone.0012840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhou D, Tong Z, Song Y, Han Y, Pei D, Pang X, Zhai J, Li M, Cui B, Qi Z, et al. Genetics of metabolic variations between Yersinia pestisbiovars and the proposal of a new biovar, microtus. J Bacteriol. 2004;186:5147–52. doi: 10.1128/JB.186.15.5147-5152.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rasoamanana B, Leroy F, Boisier P, Rasolomaharo M, Buchy P, Carniel E, Chanteau S. Field evaluation of an immunoglobulin G anti-F1 enzyme-linked immunosorbent assay for serodiagnosis of human plague in Madagascar. ClinDiagn Lab Immunol. 1997;4:587–91. doi: 10.1128/cdli.4.5.587-591.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rohr LR, Layfield LJ, Wallin D, Hardy D. A comparison of routine and rapid microwave tissue processing in a surgical pathology laboratory.Quality of histologic sections and advantages of microwave processing. Am J ClinPathol. 2001;115:703–8. doi: 10.1309/15FB-FLD1-408X-JQA3. [DOI] [PubMed] [Google Scholar]
- 64.Chen Z, Zhuo F-L, Zhang S-J, Tian Y, Tian S, Zhang J-Z. Modulation of tropoelastin and fibrillin-1 by infrared radiation in human skin in vivo. PhotodermatolPhotoimmunolPhotomed. 2009;25:310–6. doi: 10.1111/j.1600-0781.2009.00465.x. [DOI] [PubMed] [Google Scholar]
- 65.Chen S, Cheng A, Wang M, Zhu D, Luo Q, Liu F, Chen X. Immunohistochemical detection and localization of new type gosling viral enteritis virus in paraformaldehyde-fixed paraffin-embedded tissue. Vet ImmunolImmunopathol. 2009;130:226–35. doi: 10.1016/j.vetimm.2009.02.011. [DOI] [PubMed] [Google Scholar]