Abstract
The importance of health policy and systems research and analysis (HPSR+A) is widely recognized. Universities are central to strengthening and sustaining the HPSR+A capacity as they teach the next generation of decision-makers and health professionals. However, little is known about the capacity of universities, specifically, to develop the field. In this article, we report results of capacity self- assessments by seven universities within five African countries, conducted through the Consortium for Health Policy and Systems Analysis in Africa (CHEPSAA).
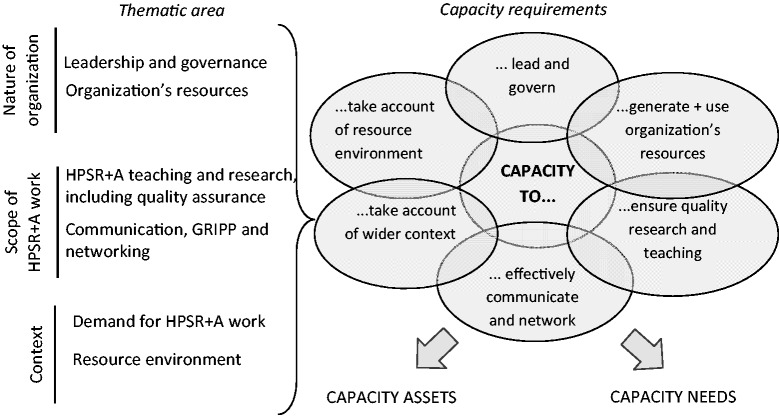
The capacity assessments focused on both capacity ‘assets’ and ‘needs’, and covered the wider context, as well as organizational and individual capacity levels. Six thematic areas of capacity were examined: leadership and governance, organizations’ resources, scope of HPSR+A teaching and research, communication, networking and getting research into policy and practice (GRIPP), demand for HPRS+A and resource environment. The self-assessments by each university used combinations of document reviews, semi-structured interviews and staff surveys, followed by comparative analysis. A framework approach, guided by the six thematic areas, was used to analyse data.
We found that HPSR+A is an international priority, and an existing activity in Africa, though still neglected field with challenges including its reliance on unpredictable international funding. All universities have capacity assets, such as ongoing HPSR+A teaching and research. There are, however, varying levels of assets (such as differences in staff numbers, group sizes and amount of HPSR+A teaching and research), which, combined with different capacity needs at all three levels (such as individual training, improvement in systems for quality assurance and fostering demand for HPSR+A work), can shape a future agenda for HPSR+A capacity strengthening.
Capacity assets and needs at different levels appear related. Possible integrated strategies for strengthening universities’ capacity include: refining HPSR+A vision, mainstreaming the subject into under- and post-graduate teaching, developing emerging leaders and aligning HPSR+A capacity strengthening within the wider organizational development.
Keywords: African universities, HPSR+A, capacity, assets and needs
KEY MESSAGES.
Health policy and systems research and analysis is an international priority, and an existing activity in Africa, though still a neglected field with numerous challenges including its reliance on unpredictable international funding.
African universities are central in strengthening African HPSR+A capacity because of their mandate to teach the next generation of policy-makers and health professionals. The universities themselves require capacity to teach, research and ensure the uptake of findings into policy and practice.
All seven CHEPSAA partners have existing capacity ‘assets’ to build upon. There are, however, varying levels of capacity assets, which, combined with different capacity needs, provide an agenda for capacity strengthening.
Possible strategies for strengthening universities’ capacity are refining HPSR+A vision, mainstreaming the subject into under/post-graduate teaching, developing emerging HPSR+A leaders and aligning HPSR+A capacity strengthening within wider organizational development.
Introduction
Health Policy and Systems Research (HPSR) is essential for health systems strengthening and achieving its goals such as improved health outcomes (WHO 2012). HPSR ‘… seeks to understand how societies organise themselves in achieving collective goals …’, is multi- and inter-disciplinary and covers international, national and local levels using a range of methodologies (Mills 2012; Sheikh et al. 2011; Gilson 2012; WHO 2012). The HPSR conducted in low- and middle-income countries is steadily growing (Gilson and Raphaely 2008) and includes increasing contributions from African universities. In addition to formal research, support for health system development typically includes routine analyses of, for example, National Health Accounts data or health statistics from the Health Information System—hence we use the term Health Policy and Systems Research and Analysis (HPSR+A), to represent the full range of research and analysis relevant to health systems.
The rising importance of HPSR+A reflects the need for adequate research and analytical capacity in a range of organizations including ministries of health, health policy analysis institutes, think tanks, academia and civil society (Green and Bennett 2007; Mayhew et al. 2008; Ranson and Bennett 2009; Greer 2010; Omaswa and Boufford 2010; Bennett et al. 2012b; Rispel and Doherty 2011).
Capacity, which can be defined as the ability of individuals or groups to perform tasks in a sustainable manner, is a complex concept involving different related elements—including structures and staff expertise—at individual, organizational and wider systems levels (Potter and Brough 2004; Green and Bennett 2007). Capacity to undertake health policy and systems research and teaching has been generally limited, particularly in developing countries (Gonzalez Block and Mills 2003; Adam et al. 2011; Decoster et al. 2011; Bennett et al. 2012a) and the need for HPSR+A capacity strengthening has been emphasized internationally (Green and Bennett 2007; WHO 2009; Sheikh et al. 2011).
Universities are central to strengthening and sustaining the HPSR+A capacity. They not only produce knowledge through research but are also mandated to teach the next generation of policy-makers, health professionals and researchers (Pariyo et al. 2011). Strengthening the capacity of African universities is arguably a more sustainable strategy for developing the field of HPSR+A in Africa, than relying on training in high-income countries, and may also address the challenge of individually contracted research consultancies (Wight 2008). At the same time, universities often find themselves struggling to balance academic objectives such as running degree-level training, with policy-relevant work such as regular engagement with decision-makers to ensure the uptake of HPSR+A research into policy and practice.
We found no frameworks for systematic assessments of universities’ capacity. As a result, capacity assessments often respond to the needs of individual projects and do not address wider organizational issues, fail to address the unique institutional opportunities and constraints that universities face, and focus on ‘capacity needs’ with less attention to existing strengths or ‘capacity assets’. While studies exist considering the capacity of ministries of health and independent entities (Briatte 2010; Greer 2010; Bennett et al. 2012b), work has only recently begun to explore the HPSR+A capacity of universities, typically within regional networks such as ASPHA (Association of Schools of Public Health in Africa). The existing work in Africa appears also to focus on research capacities (Simba 2012), and we found no assessments of universities’ capacity related to HPSR+A teaching and networking.
In this article, we report the results of capacity assessments of seven universities within five African countries in relation to HPSR+A conducted within the European Commission-funded Consortium for Health Policy and Systems Analysis in Africa (CHEPSAA). This collective, composed of 11 organizations in Africa and Europe, aims to strengthen African capacity to produce high-quality research, provide training, engage with policy networks and strengthen networking in the area of health policy and systems. We report findings from the comparative analysis of partner assessments and highlight key capacity issues for consideration by other universities and the field in general. While we report on findings from selected African universities, we envisage our results will have wider relevance to strengthening the field of HPSR+A more generally.
Methods
The CHEPSAA consortium comprises HPSR+A groups from 11 African and European universities. Capacity was not a criterion for membership in the project, though CHEPSAA partners represent groups with similar HPSR+A research and teaching interests and a history of previous partnerships.
CHEPSAA focuses particularly on three areas of capacity strengthening: staff and organizational development within partner institutions, HPSR+A course development, and networking and getting research into policy and practice (GRIPP) nationally and internationally. It is receiving financial support for a period of 4 years (2011–15) from the European Commission.
The purpose of the capacity assessments, conducted during the first project year, were partly to support planning of project activities, but even more importantly, to inform wider organizational development and networking in order to build the field of HPSR+A nationally, regionally and internationally.
In the assessments, we focused on both capacity ‘assets’ and capacity ‘needs’ within each African CHEPSAA partner institution. This is done, similar to existing literature (UNDP 2008), in recognition that all organizations are likely to have strengths though their application may be constrained (for example, staff expertise in publishing research may not be fully utilized due to high management workload).
The capacity assessments covered three related levels of capacity (wider context, organizational and individual), often referred to in the literature (LaFond and Brown 2003; Green and Bennett 2007; Bennett et al. 2010). A framework, covering these levels, was developed and guided the self-assessments by each university resulting in capacity assessment reports. A comparative analysis was then conducted on the basis of these reports.
The self-assessments by each university, and the subsequent comparative analysis, were driven by six thematic areas of capacity and our understanding of capacity requirements within each area. The development of these thematic areas was guided by the following three considerations. First, the understanding of capacity as a concept, which emphasizes the importance of effective leadership and governance within organizations’ roles and structures and identifies the resources as an important element of capacity (Potter and Brough 2004; Green and Bennett 2007). The second is the unique institutional specificity of universities, raising the significance of quality assurance for research and teaching. Last, the practice-oriented nature of HPSR+A work by universities, suggesting the importance of communication, networking and GRIPP (Bennett et al. 2011a; Sheikh et al. 2011). The identification of specific capacity requirements is driven by our understanding of key tasks and responsibilities within each thematic area.
As shown in Figure 1, the thematic areas reflect the three groups of issues (nature of organizations, scope of HPSR+A work and contextual issues), which guide the presentation of findings in this article.
Figure 1.
Conceptual framework for capacity assessments.
The assessments were conducted by the following CHEPSAA partners:
Ghana—Department of Health Policy, Planning and Management, School of Public Health, University of Ghana (SPH-UG).
Kenya—Tropical Institute of Community Health and Development, Great Lakes University of Kisumu (TICH-GLUK).
Nigeria—Health Policy Research Group and the Department of Health Administration and Management, College of Medicine, University of Nigeria Enugu-Campus (HPRG-COMUNEC).
Tanzania—Institute of Development Studies, University of Dar Es Salaam (IDS-UDSM).
South Africa—Health Policy and Systems Programme/Health Economics Unit, University of Cape Town (HPSP/HEU-UCT).
South Africa—School of Public Health, University of the Western Cape (SOPH-UWC).
South Africa—Centre for Health Policy, School of Public Health, University of Witwatersrand (CHP-WITS).
Partners used combinations of document reviews, semi-structured interviews and internal staff surveys in capacity self-assessments. A phased approach was used, with the context mapping proceeding first and informing the later assessment of organizational and individual capacity. Ethical approvals were obtained from respective ethical committees in each country.
A framework approach (Ritchie and Spencer 1994), guided by the above thematic areas and their capacity requirements, was used to analyse data for self-assessments and at the comparative level. The process for comparative analysis included development of a matrix of comparative findings, and its subsequent revision following partners’ comments at a consortium meeting to ensure validity of findings.
Findings
We now present the results of our comparative analysis. We start with an overview of the ‘nature of the partner organizations’ focusing on key issues related to leadership and governance and the organization’s resources. We then explore the ‘scope of HPSR+A work’ in each organization, including internal quality assurance mechanisms and communication and networking. Finally, we compare the ‘contextual issues’ influencing the capacity of universities to conduct HPSR+A, including demand for HPSR+A in each country.
Nature of organizations
In terms of organizational structures, all partner organizations are HPSR+A groups (academic programmes/units, schools, colleges, centres or institutes) nested within wider universities with access to central university managerial support for teaching and research, including management of finance and human resources. As shown in Table 1, the location of the group within respective university structures varied, which may also explain differences in their size and scope of HPSR+A teaching and research.
Table 1.
Overview of CHEPSAA partner organizations as of March 2012
| Country | Nigeria | Tanzania | Kenya | Ghana | South Africa |
||
|---|---|---|---|---|---|---|---|
| Partner | HPRG-COMUNEC | IDS-UDSM | TICH-GLUK | SPH-UG | CHP-WITS | SOPH-UWC | HPSP/HEU-UCT |
| Relation with University | Academic unit reports to College | Institute reports to University | Institute reports to University | School reports to University | Centre reports to School | School reports to Faculty | Academic programme/unit reports to School |
| Vision of HPSR+A group | Health research and teaching orientated | Importance of teaching and research health to development | Sustainable Health and development | HPSR+A implicit but recognized | Explicit focus on HPSR+A | Explicit focus includes HSPR+A | Explicit focus on HPSR+A |
| Financing arrangements | Teaching time funding subsidizes research | No subsidies between teaching and research | No subsidies between research, teaching and consultancies | No subsidies between teaching and research | Research grants subsidize teaching time | No subsidies between teaching and research | Research grants subsidize teaching time |
| No of HPSR+A academic staff | 7 | 4 | 10 | 35 | 9 | 13 | 12 |
| No HPSR+A academics with doctorate degrees | 3 | 3 | 2 | 25 | 4 | 4 | 9 |
| Ratio of senior (Prof. and Assoc. Prof.) vs junior HPSR+A academic staff | 3:4 | 3:1 | 4:6 | 22:13 | 5:4 | 4:9 | 3:9 |
| No of support/administration staff | 4 | 8 | 4 | 13 | 3 | 14 | 5 |
| Main issues on infrastructure | Unreliable electricity, IT and teaching space | Unreliable electricity, teaching aids/space | Unreliable electricity, IT and teaching space | Unreliable access to electricity, teaching aids/space | No significant infrastructural constraints were reported | ||
| HPSR+A within wider institution | Cross college research group | Taught units in existing course/research projects | Taught units in existing courses/research projects | Taught units in existing courses/research projects | HPSR+A research as core function | Whole school orientation | Programme within wider academic group |
| Group’s thematic focus/expertise | Health policy and financing | Health policy | Health Policy and Planning & Health systems | Human resources, Maternal Health | Financing, Human resources, Universal coverage, Health systems and policy | Human resources, Health policy and systems, Information system | Health policy and systems, Financing and economics, Governance |
| No of current HPSR+A research projects | 5 | 3 | 3 | 5 | 14 | 16 | 10 |
| Main HPSR+A teaching courses | MSc and PG diploma | MA in Dev-t Studies | MA in Community Health and Dev-t | MPH programme | MPH programme | MPH and PG diploma, short courses | MPH and PG diploma |
| No of core and elective modules focusing on HPSR+A | 9 | 1 | 2 | 8 | 4 | 20 | 7 |
With the exception of CHP-WITS and HPSP/HEU-UCT, which were set up primarily as research groups but are also expected to teach, all partners are regular university departments whose primary activity is teaching followed by research.
Leadership and governance
In relation to leadership and governance, we explored two issues: the existence and clarity of vision for HPSR+A and partners’ organizational structures and management approaches. The choice of these two issues is driven by recognition that the latter is likely to affect the ongoing HPSR+A activities, whereas the former can guide partners’ strategic direction.
Two clear capacity assets emerged from our analysis: a clear vision for HPSR+A as well as partners’ organizational structures and the resultant management approaches, as we set out next.
A clear vision for HPSR+A, outlining the direction of the CHEPSAA partner in the long term, was seen as important by all groups. A clear asset was that such a vision mostly existed within partner institutions, though was sometimes implicit and undocumented. Differences in the degree of explicitness of vision seemed to relate to two issues, which can provide opportunities for capacity strengthening. First, the relative position of the HPSR+A group within the wider university: the more autonomous units such as CHP-WITS and SOPH-UWC had documented visions for HPSR+A, possibly reflecting their degree of flexibility to determine own strategic direction. Secondly, the history of the partner: CHP-WITS was established to advance the field of Health Policy Research and Teaching and SOPH-UWC was set up to support district health system development; in both cases, the group’s vision has an explicit HPSR+A focus. On the other hand, the IDS-UDSM historically had no specific focus on health, rather focusing on broader sustainable development, leading to a less explicit focus on HPSR+A in their vision.
Two distinct approaches were found between partners’ organizational structures and management approaches. HPRG-COMUNEC and SPH-UG are situated within hierarchical university structures in which heads of groups are appointed for longer terms, similarly to most other CHEPSAA partners. A different approach was identified in SOPH-UWC where the Head of Department rotates every 3–5 years between senior academic staff and:
… succession plans are expected to be put in place two years in advance with respect to all rotating posts … to enable sufficient preparation time for both those incoming and incumbent. (Amde et al. 2012, p. 5)
Both these approaches can be considered as HPSR+A capacity assets within their own contexts. For example, one advantage of longer term appointments may be the potential consistency of management style, whereas the rotational approach may allow more room for fresh ideas and innovation.
Three assets can be identified in relation to management approaches. First, reported by all partners, was that management decisions are made collegially, typically by a committee comprising senior staff and, in case of HPRG-COMUNEC, requiring Board approvals at different levels. Clear job roles for academic staff, including management responsibilities, was reported as another asset in all CHEPSAA partners. A system of two-day annual retreats to identify strategic priority areas was reported in CHP-WITS and can be regarded as a third potential asset.
As for the capacity needs in relation to management approaches, two issues emerged from our analysis. The staff roles were sometimes less clear for support staff, for example in HPSP/HEU-UCT. Although all other CHEPSAA partners also appear to reflect upon their strategic direction, they did not identify any clear processes, representing another possible need for capacity strengthening.
Organizations’ resources
In the assessments we explored human, financial and infrastructure resources.
Three types of capacity assets were identified within different partner institutions. One asset, emphasized by all organizations, was the presence of champions, including internationally recognized experts in the field, for example in SPH-UG and HPSP/HEU-UCT. Although the degree of support varied between organizations, all partners had access to central university managerial support, such as management of finance and human resources, providing opportunities for HPSR+A groups to engage more with these structures to alleviate some managerial burden on individual academic units. Finally, a more developed infrastructure, such as availability of office and teaching space as well as equipment, was reported within South African universities as another capacity asset.
Multiple capacity needs were reported. All partners reflected on the shortage of dedicated resources for HPSR+A work, such as earmarked finance and staff time, though the degree varied. Resource constraints were reported less by South African universities.
In relation to human resources, staff shortages, particularly of senior and mid-career staff, were identified as a common concern across all partners: for example, at the time of assessment IDS-UDSM had only three HPSR+A academic staff:
The [current] age structure is such that majority of the staff, more than 50 percent, are either retirees or near retirement … By 2015 about 55 percent of staff will be retirees working on contract. (IDS 2012, p. 18)
Two factors appear to contribute to the paucity of HPSR+A staff. One is that as a new field there is a lack of established and funded posts for it and HPSR+A work therefore depends on unstable grants. The second is the lack of clear HPSR+A career paths within universities. These staff shortages, coupled with insecurity and high mobility of junior researchers in and out of this nascent discipline, means foreseeable challenges with succession planning in the longer term.
Availability of financial resources for HPSR+A was identified as another challenge though cost recovery for HPSR+A research and teaching varied across the universities. With the exception of HPSP/HEU-UCT and CHP-WITS, where research grant funding essentially cross-subsidizes some teaching time, most organizations have staff in university posts who teach HPSR+A. Research is, however, typically funded externally:
… almost all the [teaching] staff members … (90%) are on Ghana Government payroll. The remaining 10% receive their allowance/salary from specific project funds. However the situation with regards to core funding to … conduct research shows a reverse pattern. Grants from donors constituted over 90% of the total funds received for research activities … with government of Ghana (GOG) providing about 10% or less … (Agyepong et al. 2012, p. 16)
Funding for health policy and systems analysis (HPSA) teaching comes entirely from the government … HPSA research … [is funded] through external grants which is limited to the length of the project and is therefore not sustainable … (HPRG-COMUNEC 2012, p. 21)
Differences were found in infrastructure between South African and West and East African universities with the latter facing more challenges in relation to availability of office and teaching space, access to computer hardware and software and other teaching equipment.
In relation to finance, the distinction between capacity assets and needs was less clear cut. Both government and external grant funding sources appear important to ensure the sustainability of HPSR+A work in partner organizations. University funding for HPSR+A work, coming from government, is often seen as a more stable funding source to ensure continuity of HPSR+A work, particularly teaching. The research grants, although sometimes seen as unpredictable, do enable recruitment of additional staff and partially subsidize HPSR+A teaching in the two South African CHEPSAA partners.
Scope of HPSR+A work
In understanding the scope of HPSR+A work, we explored two thematic areas: (1) scope of research and teaching activities, including issues of quality assurance and (2) networking, communication and GRIPP. Both are set out next.
Scope of HPSR+A teaching and research
Mostly capacity assets were identified in relation to HPSR+A teaching and research, as we set out next. One clear asset was that all partners have ongoing HPSR+A research, including involvement in, or leadership of, international collaborative research such as CHEPSAA. The number of projects varied between 3 (IDS-UDSM) and 16 (SOPH-UWC). Research focused on health policy and systems issues, though individual partners also specialized thematically, such as in maternal health (SPH-UG), health financing (HPRG-COMUNEC, CHP-WITS, HPSP/HEU-UCT) or health information systems (SOPH-UWC). These differences we believe reflect the sizes of HPSR+A groups, their history, strategic vision, availability of resources, staff expertise and research interests, and balance between teaching and research.
All groups also teach HPSR+A at post-graduate level, typically as a module within a wider Masters programme (often, Public Health) or as short courses such as in the SOPH-UWC Winter School: a 3-week programme aimed to expose health workers to the key health policy and systems issues in the contexts of low- and middle-income countries.
Another asset in all partners was the existence of quality assurance mechanisms for both teaching and research. Approaches to ensuring ‘teaching’ quality appear similar across partners and typically included regular module reviews, using feedback from students and teachers. ‘Research’ quality assurance included combinations of ethics reviews, mentoring and coaching by senior colleagues and joint publications of study results. However, we also found two distinct approaches to research quality assurance within the CHEPSAA partners, ranging from the use of institutional research guidelines in TICH-GLUK to project-specific support in HPRG-COMUNEC; the latter is summarized by one respondent:
… there is always a quality assurance officer or two attached to every project in addition to monitoring and evaluation officers. We have supervisors who go to the field to supervise the field workers and the quality assurance officer supervises the supervisor and double checks all data coming in from the field. (Researcher, Nigeria)
On reflection, the project-based support is likely to be effective for targeted support, whereas effective institutional processes can be more sustainable in the long term.
In terms of capacity needs, there was less evidence of HPSR+A being taught within undergraduate programmes, suggesting that HPSR+A may not be seen as a core discipline for medical students. The fact that HPSR+A is embedded within wider programmes possibly reflects its interdisciplinary nature as well as its nascent position within the field of public health. However, as the HPSR+A field grows, one would expect the development of post-graduate programmes specialized on HPSR+A at both masters and doctoral levels.
Communication, GRIPP and networking
Existing networking experience was seen as a clear capacity asset of the CHEPSAA partners. As shown in Table 2, different partners, and CHEPSAA as a whole, are involved in multiple international HPSR+A research networks and/or similar consortia.
Table 2.
Selected international research partnerships involving CHEPSAA partners
| Network | CHEPSAAA partners involved |
|---|---|
| Consortium for Research on Equitable Health Systems (CREHS)—fosters collaborative research on how to strengthen health system policies and interventions in ways that preferentially benefit the poorest. | HPRG-COMUNEC, IDS-UDSM, TICH-GLUK, CHP-WITS, HPSP/HEU-UCT |
| Network on Equity in Health in South Africa (EQUINET)—supports research, advocacy and policy engagement around equity and health. | IDS-UDSM, CHP-WITS, SOPH-UWC, HPSP/HEU-UCT |
| International Network for the Demographic Evaluation of Populations and Their Health (INDEPTH)—developing District Health System Observatories for field training and student posting; ACT Consortium. | IDS-UDSM, HPRG-COMUNEC, SPH-UG, CHP-WITS, HPSP/HEU-UCT |
| Regional East African Community Health (REACH) Policy Initiative Project—knowledge brokering in East Africa. | TICH-GLUK |
| Social Aspects of HIV/AIDS Research Alliance (SAHARA)—specializing in HIV social research with strong linkages to policy making. | SPH-UG, CHP-WITS |
| Supporting the use of Research Evidence for Policy in African Health project (SURE)—supporting the use of research evidence for policy. | HPRG-COMUNEC, SPH-UG, |
| Resilient and Responsive Health Systems (RESYST)—aims to enhance the resilience and responsiveness of health systems to promote health and health equity and reduce poverty. | HPRG-COMUNEC, CHP-WITS, HPSP/HEU-UCT |
| Teasdale Corti—strengthening Nurses’ Capacity in HIV Policy development in Sub-Saharan Africa and the Caribbean. | TICH-GLUK |
Partners’ involvement in multiple international networks can facilitate their capacity strengthening through attracting funding for collaborative research and joint publications and can be seen as one capacity asset.
However, no formal national-level HPSR+A research networks were reported in the five countries, which represents one possible capacity need or an area for further development. Furthermore, although some partners do belong to the African Schools of Public Health Association, none of the CHEPSAA partners were part of formal HPSR+A teaching networks other than CHEPSAA.
Links with policy-makers, necessary for GRIPP, varied across partners. Well-established relations with policy-makers in HPSP/HEU-UCT (where researchers engaged in different decision fora over time) and SPH-UG (where the HPSR+A champions had joint appointments in both academia and services) were perceived as clear capacity assets.
However, in some partner groups, such as in IDS-UDSM, the interaction between researchers and policy-makers were perceived as generally weak and thus represent a capacity need. Most partners also identified a need to strengthen communication skills by researchers to ensure uptake of HPSR+A findings in policy and practice. At the same time, some researchers reflected that:
The government is not sincere about research, a lot of money is being spent on ‘what I call talk shops’ and not workshops because little or nothing is being implemented after such workshops and nothing is achieved yet a lot of money that could be given to fund genuine research is being spent without results. (Researcher, Nigeria)
There was also recognition that improving communications skills of individual researchers alone may not be sufficient to ensure the uptake of research into policy and practice. A culture of evidence-informed policies was seen as an important contextual determinant of evidence-informed policies.
Contextual issues
In relation to the contextual influences on partners’ capacity, we explored two issues: the demand for HPSR+A work and the nature of the resource environment for HPSR+A work.
Demand for HPSR+A work
One clear asset was a recognition that there is demand for teaching of HPSR+A in all five countries, reflected in the continuous uptake of HPSR+A modules within wider teaching programmes.
The demand for HPSR+A research by decision-makers, however, was perceived as limited by all partners thus highlighting one capacity need. The limited demand for HPSR+A research appears to be a reflection of three broad influences, which provide multiple entry points for future capacity strengthening of universities and building the field of HPSR+A. First, is the newness of the HPSR+A field and a greater reliance on clinical studies as compared with HPSR+A work for decision-making, possibly because of the clinical backgrounds of decision-makers. Secondly, all partners also felt that existing priority-setting mechanisms for health research largely favour clinical research leading to the dominance of clinical sciences within universities with HPSR+A units sometimes seen as ‘… a relatively “poor cousin” of clinical departments’ (Orgill and Gilson 2012, p. 4). Finally, the limited demand for HPSR+A work may reflect a lack of dedicated structures in support of HPSR+A work in each country: for example, no HPSR+A-specific Research Funding Councils were identified.
On a more positive note, all partners reflected that the demand for HPSR+A research is steadily increasing nationally and internationally. This is demonstrated by the growing number of projects implemented by partner institutions as well as increasing number of calls for HPSR+A research from international funders over the last several years.
Resource environment
In relation to the wider resource environment, all partners reflected that international funding is significant for HPSR+A research and can be regarded as one capacity asset.
However, in contrast, there is little government funding for research in the field. One researcher suggested that ‘… if the government is not willing to fund research into local priorities then it is inevitable that donor funding will direct research priorities’ (UCT staff, South Africa). The partners also stated that reliance on growing international funding can often drive and skew research priorities:
The big funders tend to dictate the research agenda. Some respondents felt that there was too much ‘top down’ and not enough ‘bottom up’ … Some respondents were also of the view that external funders’ demand for HPSA research has been extremely limited up to now. However, there was a sense that it would probably increase in the next few years because there is an increasing global effort to promote the field. (Nxumalo and Goudge 2012, p. 20)
Therefore, one clear capacity need is ensuring committed funding from national governments to support addressing local HPSR+A research priorities.
Next we discuss the key issues from the above findings in relation to future capacity strengthening and reflect on key study limitations.
Discussion
Our contention is that universities are central to strengthening the field of HPSR+A nationally and internationally because of their mandate to train future policy-makers, researchers, teachers and advocates. Our findings suggest that there is an urgent need to address the multiple capacity challenges of universities in relation to HPSR+A. At the same time, the contextual influences on capacity are well-recognized (Potter and Brough 2004; Green and Bennett 2007). We reinforce this by emphasizing the importance of effective research priority-setting mechanisms that recognize and value HPSR+A, leading to a more stable and responsive funding environment, and the potential uptake of HPSR+A evidence by decision-makers. It is obvious that universities alone are not in a position to affect these issues. Therefore, greater recognition and communication of different contextual influences to the relevant policy actors is likely to improve the success of capacity strengthening.
Many capacity assessments tend to focus on capacity needs (L'Hirondel 1998; Sidle et al. 2006; Green and Bennett 2007) with less explicit recognition of capacity assets in the assessments (UNDP, 2008). An important point from our findings is that all universities have capacity ‘assets’, such as ongoing HPSR+A teaching and research, which can often be neglected within capacity assessments. The varying levels of assets across CHEPSAA partners—such as staff, teaching courses and research projects—probably reflect the history of the HPSR+A groups and their positions within universities. Systematic identification and clear recognition of capacity assets can provide opportunities for sharing these assets within networks such as CHEPSAA, for example, through developing joint curricula and applying for collaborative research. Although we found evidence of networking by CHEPSAA partners internationally, sharing the assets within national research and teaching networks—for example, through delivery of joint teaching courses within national networks—was less evident and perhaps represents a focus for future capacity strengthening.
A clear recognition of capacity assets is essential especially where application of these assets are constrained and the assets thus need ‘unleashing’ within organizations (Development Assistance Committee 2006; UNDP 2006). For example, the presence of internationally recognized champions is one asset which is likely to help attract funding for HPSR+A projects such as CHEPSAA through ensuring the quality of grant applications. However, these champions can often be overburdened with routine administration and thus unable to regularly apply their expertise. An example of another asset is a clear vision for HPSR+A, which can be an important milestone for further development of the HPSR+A group within the wider institution. However, the application of this vision can be constrained by competing university priorities such as expansion of clinical research units and, therefore, the vision must align the development of HPSR+A with the wider organizational agenda.
Our findings, similar to the published literature (LaFond et al. 2002; Bennett et al. 2012a), suggest that capacity assets and needs at different levels are related. For example, degree of expertise of junior HPSR+A staff is likely to relate to existence, or lack, of HPSR+A-specific staff development opportunities within organizations and career paths for health policy and systems analysts within universities and governments. The recognition of these potential ‘chains’ is essential in sustaining future capacity strengthening initiatives. Future initiatives also need to explore different options for ‘joining up’ different assets within and across organizations: developing expertise of junior staff in grant proposal development through mentorship by senior staff and joint research proposal writing is one example. It is also important to recognize and, where appropriate, ensure the mutual reinforcement of different capacity strengthening strategies—for example, strengthened individual skills in teaching can potentially contribute to improved teaching quality assurance.
Looking more broadly, complementing existing literature (Bennett et al. 2011a; WHO 2012), our findings suggest that the field of HPSR+A is growing though still neglected. Experiences from other studies suggest that research priority setting that is nationally driven, interpretative and involving different policy actors can enhance the role of HPSR+A (Ranson and Bennett 2009); perceptions of policy-makers in relation to quality of evidence are important in uptake of evidence in policy and practice (Innvaer et al. 2002; Tomson et al. 2005; Burchett et al. 2012) and government motivation to use evidence can contribute to capacity strengthening of those who produce this evidence (Bennett et al. 2012b). We suggest that if building the field of HPSR+A is taken seriously by researchers, managers, policy-makers and health professionals, targeted efforts should be invested by each of these groups. More specifically, there is a need for better recognition of the value of HPSR+A in national research agendas, more commissioning of HPSR+A by governments and targeted international funding for capacity strengthening strategies. Ensuring and enhancing the mutual understanding between researchers and policy makers is essential for enhancing the recognition of value of HPSR+A and ensuring improved uptake of HPSR+A research in policy and practice.
The design of feasible and effective capacity strengthening strategies should ideally be informed by systematic capacity assessments, such as the one reported in this article. The specific strategies CHEPSAA will seek to implement in response to the capacity assessments reported here include: (1) developing/clarifying the vision for HPSR+A within individual groups and aligning it with the wider organization’s development; (2) mainstreaming HPSR+A into post-graduate and possibly under-graduate teaching through the development of short courses and modules on health policy and systems; (3) developing an emerging HPSR+A leaders’ programme for younger staff, covering essential competencies such as personal leadership principles, preparing grant proposals, managing research grants and effective communication of results; and (4) systematic organizational development through sharing partners’ experiences in mentoring, communication and researcher-policy engagement to support quality HPSR+A research and teaching.
More similarities, than differences, were found in relation to the HPSR+A capacity of the CHEPSAA partners. This homogeneity may reflect a combination of the three issues. Firstly, although capacity was not a criterion for CHEPSAA membership, the CHEPSAA consortium included groups with similar interests and history of partnerships within this nascent field. Secondly, the consistent use of the methodological framework, potentially contributed to the emphasis on, and the potential recognition of, similar capacity issues. Thirdly, similar contextual and organizational issues; for example, issues such as resource environment and historical developments may be different to, say, French-speaking HPSR+A groups with different development paths. The results from our relatively small-scale capacity assessments can provide the starting point for comparisons with results of future similar initiatives.
Before closing we acknowledge three potential limitations of our study. Firstly, our capacity assessments focused primarily on the HPSR+A groups, typically housed within Medical Faculties. However, some HPSR+A work is also likely to be conducted by other departments such as development studies or social policy groups. Further assessment of ‘cumulative’ capacity within the wider Universities may be appropriate as part of future studies. Secondly, the thematic areas covered in our assessments are specific to areas of CHEPSAA work and other projects may have different foci. Greater emphasis on conducting research or organizational development may be important to other universities and this would need to be considered in future capacity assessments. Thirdly, we focused specifically on CHEPSAA partner organizations rather than all HPSR+A groups within their settings, and acknowledge that other universities within the study countries are likely to have further capacity assets for the field to draw upon. Further studies may be appropriate to conduct comprehensive assessments of ‘collective’ national capacity, to inform better sharing of assets in capacity strengthening.
Conclusions
HPSR+A is an international priority and an existing activity in Africa, though still neglected field with numerous challenges, including its low priority in national health research and reliance on international funding for research.
Universities are central to strengthen HPSR+A capacity nationally and internationally, as they have a mandate to develop the next generation of policy-makers, health professionals and researchers. At the same time, universities themselves require adequate capacity to teach and to research, to communicate effectively research results and to influence policy and practice.
All African CHEPSAA partners discussed within this article have existing capacity ‘assets’ to build upon in capacity strengthening: all are actively engaged in research activities, teach health policy and systems to future generations of managers and researchers and support health systems development in their settings. However, there are varying levels of assets and clear needs for capacity strengthening.
Possible strategies for strengthening universities’ HPSR+A capacity include refining a clear vision for the field within the wider organizational agenda, mainstreaming the subject into under-graduate and post-graduate teaching, aligning HPSR+A capacity strengthening within wider organizational agenda and developing emerging leaders in the field of HPSR+A.
Acknowledgements
The authors would like to thank Uta Lehmann, Ermin Erasmus, Irene Agyepong, Stephen Okeyo, Jane Goudge, Peter Kamuzora, Goran Tomson and Don de Savigny for the useful comments in preparation of this article and leading their respective teams in contribution to methodology development and conduct of the capacity assessments.
Funding
The research leading to these results has received funding from the European Commission Seventh Framework Programme (FP7/2007–13) under Grant Agreement Number 265482.
Conflict of interest
None declared
References
- Adam T, Ahmad S, Bigdeli M, Ghaffar A, Røttingen J-A. Trends in health policy and systems research over the past decade: still too little capacity in low-income countries. PLoS One. 2011;6:e27263. doi: 10.1371/journal.pone.0027263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agyepong I, Aikins M, Esena R, Akweongo P, Aniah K. Assessment of Capacity Development Needs for Health Policy and Systems Analysis (HPSA) Research and Teaching in Ghana. Accra, Ghana: University of Ghana; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amde WK, Cailhol J, Lehmann U. Health Policy and Systems Research and Analysis: Capacity Needs Assessment of the School of Public Health, University of the Western Cape, South Africa. CHEPSAA report. Cape Town, South Africa: Consortium for Health Policy & Systems Analysis in Africa; 2012. [Google Scholar]
- Bennett S, Agyepong IA, Sheikh K, Hanson K, Ssengooba F, Gilson L. Building the field of health policy and systems research: an agenda for action. PLoS Medicine. 2011a;8:e1001081. doi: 10.1371/journal.pmed.1001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett S, Corluka A, Doherty J, et al. Approaches to developing the capacity of health policy analysis institutes: a comparative case study. Health Research Policy and Systems. 2012a;10 doi: 10.1186/1478-4505-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett S, Corluka A, Doherty J, et al. Influencing policy change: the experience of health think tanks in low- and middle-income countries. Health Policy Plan. 2012b;27:194–203. doi: 10.1093/heapol/czr035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett S, Paina L, Kim C, et al. What must be done to enhance capacity for Health Systems Research? 2010. Background paper for the global symposium on health systems research. 16–19 November 2010 Montreux, Switzerland. [Google Scholar]
- Briatte F. A case of weak architecture: the French Ministry of Health. Social Policy & Administration. 2010;44:155–71. [Google Scholar]
- Burchett HED, Lavis JN, Mayhew SH, Dobrow MJ. Perceptions of the usefulness and use of research conducted in other countries. Evidence & Policy: A Journal of Research, Debate and Practice. 2012;8:7–16. [Google Scholar]
- Decoster K, Appelmans A, Hill P. A Health Systems Research mapping exercise in 26 low- and middle-income countries: narratives from health systems researchers, policy brokers and policy-makers. 2011 Background paper commissioned by the Alliance for Health Policy and Systems Research to develop the WHO Health Systems Research Strategy. Alliance for Health Policy and Systems Research. [Google Scholar]
- Development Assistance Committee. The Challenge of Capacity Development: Working Towards Good Practice. 2006 Paris: Organisation for Economic Co-operation and Development. [Google Scholar]
- Gilson L, editor. Health Policy and Systems Research. A Methodology Reader. Geneva, Switzerland: Alliance for Health Policy and Systems Research, World Health Organization; 2012. [Google Scholar]
- Gilson L, Raphaely N. The terrain of health policy analysis in low and middle income countries: a review of published literature 1994-2007. Health Policy Plan. 2008;23:294–307. doi: 10.1093/heapol/czn019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez Block M, Mills A. Assessing capacity for health policy and systems research in low and middle income countries. Health Research Policy and Systems. 2003;1:1. doi: 10.1186/1478-4505-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green A, Bennett S, editors. Sound Choices: Enhancing Capacity for Evidence-Informed Health Policy. AHPSR Biennual Review. Geneva: WHO, Alliance for Health Policy and Systems Research; 2007. [Google Scholar]
- Greer SL. Standing up for health? Health departments in EU health policy formulation. Social Policy & Administration. 2010;44:208–24. [Google Scholar]
- HPRG-COMUNEC. Capacity Needs Assessment Report for CHEPSAA project. Enugu, Nigeria: University of Nigeria Enugu; 2012. [Google Scholar]
- IDS. Tanzania Needs Assessment Country Report. Dar Es Salaam: Tanzania, University of Dar Es Salaam; 2012. [Google Scholar]
- Innvaer S, Vist G, Trommald M, Oxman A. Health policy-makers' perceptions of their use of evidence: a systematic review. Journal of Health Services Research and Policy. 2002;7:239–44. doi: 10.1258/135581902320432778. [DOI] [PubMed] [Google Scholar]
- L'Hirondel A. An initial assessment of the needs of capacity in public health law. Global Health Law. 1998:53–57. [Google Scholar]
- LaFond A, Brown L. A Guide to Monitoring and Evaluation of Capacity-Building Interventions in the Health Sector in Developing Countries. 2003. Measure Evaluation Project. [Google Scholar]
- LaFond A, Brown L, Macintyre K. Mapping capacity in the health sector: a conceptual framework. International Journal of Health Planning and Management. 2002;17:3–22. doi: 10.1002/hpm.649. [DOI] [PubMed] [Google Scholar]
- Mayhew S, Doherty J, Pitayarangsarit S. Developing health systems research capacities through north-south partnership: an evaluation of collaboration with south Africa and Thailand. Health Research Policy and Systems. 2008;6:1–12. doi: 10.1186/1478-4505-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills A. Health policy and systems research: defining the terrain; identifying the methods. Health Policy Plan. 2012;27:1–7. doi: 10.1093/heapol/czr006. [DOI] [PubMed] [Google Scholar]
- Nxumalo N, Goudge J. Phase 2 Final Needs Assessment Report. Johannesburg, South Africa: University of Witwatersrand; 2012. [Google Scholar]
- Omaswa F, Boufford JI. Strong Ministries for Strong Health Systems. An Overview of the Study Report: Supporting Ministerial Health Leadership: A Strategy for Health Systems Strengthening. New York: The African Center for Global Health and Social Transformation (ACHEST) and The New York Academy of Medicine (NYAM); 2010. [Google Scholar]
- Orgill M, Gilson L. CHEPSAA Needs Assessment Report for the Health Policy and Systems Programme/Health Economics Unit, School of Public Health and Family Medicine, University of Cape Town. Cape Town, South Africa: University of Cape Town; 2012. [Google Scholar]
- Pariyo G, Serwadda D, Sewankambo N. A grander challenge: the case of Makerere University College of Health Sciences contributes to health outcomes in Africa. BMC International Health and Human Rights. 2011;11:52. doi: 10.1186/1472-698X-11-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter C, Brough R. Systemic capacity building: a hierarchy of needs. Health Policy Plan. 2004;19:336–45. doi: 10.1093/heapol/czh038. [DOI] [PubMed] [Google Scholar]
- Ranson M, Bennett S. Priority setting and health policy and systems research. Health Research Policy and Systems. 2009;7:27. doi: 10.1186/1478-4505-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rispel L, Doherty J. Research in support of health systems transformation in South Africa: the experience of the centre for health policy. Journal of Public Health Policy. 2011;32:S10–S29. doi: 10.1057/jphp.2011.33. [DOI] [PubMed] [Google Scholar]
- Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess R, editors. Analyzing Qualitative Data. New York: Routledge; 1994. [Google Scholar]
- Sheikh K, Gilson L, Agyepong IA, Hanson K, Ssengooba F, Bennett S. Building the field of health policy and systems research: framing the questions. PLoS Medicine. 2011;8:e1001073. doi: 10.1371/journal.pmed.1001073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidle JE, Were E, Wools-Kaloustian K, et al. A needs assessment to build international research ethics capacity. Journal of Empirical Research on Human Research Ethics. 2006;1:23–38. doi: 10.1525/jer.2006.1.2.23. [DOI] [PubMed] [Google Scholar]
- Simba D. Do universities in East and Central Africa have capacity for health systems research? Presentation at Second Global Symposium on Health Systems Research. 2012 31 October–3 November, Beijing, PR China. [Google Scholar]
- Tomson G, Paphassarang C, Jonsson K, Houamboun K, Akkhavong K, Wahlstrom R. Decision-makers and the usefulness of research evidence in policy implementation - a case study from Lao PDR. Social Science & Medicine. 2005;61:1291–9. doi: 10.1016/j.socscimed.2005.01.014. [DOI] [PubMed] [Google Scholar]
- UNDP. 2006 Capacity Development Practice Note. United Nations Development Programme. http://www.undp.org/cpr/iasc/content/docs/UNDP_Capacity_Development.pdf. [Google Scholar]
- UNDP. Capacity Assessment Practice Note. New York, USA: United Nations Development Programme; 2008. [Google Scholar]
- WHO. Scaling Up Research and Learning for Health Systems: Now is the Time. Report of a High Level Task Force, presented and endorsed at the Global Ministerial Forum on Research for Health 2008, Bamako, Mali. Geneva. Geneva: World Health Organization; 2009. [Google Scholar]
- WHO. Changing Mindsets - Strategy on Health Policy and Systems Research. Geneva: World Health Organization; 2012. [Google Scholar]
- Wight D. Most of our social scientists are not institution based … they are there for hire—Research consultancies and social science capacity for health research in East Africa. Social Science & Medicine. 2008;66:110–16. doi: 10.1016/j.socscimed.2007.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]