Abstract
Background
Women undergoing surgery for ovarian cancer are severely ill and are high users of health services. Contributing to these increased utilization rates are the multiple modalities used to treat ovarian cancer, and the complications and side effects from those treatments.
Objective
To evaluate the effectiveness of an intervention provided by advanced practice nurses and a psychiatric consultation-liaison nurse on patients' self-report of health care utilization compared to an attention control intervention in women undergoing surgery for a suspected diagnosis of ovarian cancer.
Method
A two-group, experimental, longitudinal design was used to compare women who were assigned randomly to the intervention group or to an attention control group at baseline within 48 hours after surgery and 1, 3, and 6 months after surgery. Healthcare utilization was measured as the number of self-reported inpatient admissions and outpatient visits, including emergency room visits, oncology outpatient visits, and primary care visits. Nurse interventions consisted of 16 contacts: symptom management, counseling, education, direct nursing care, coordination of resources, and referrals. The attention control interventions consisted of 9 contacts that included instructions on use of a symptom management toolkit and strategies on how to manage symptoms.
Results
There were no differences in hospitalizations and oncology outpatient visits between the two groups. The main finding of this study was a significant difference in the number of primary care visits between the two groups. Women in the attention control group went to their primary care providers more often than the intervention group. The women who reported more visits also reported more depressive symptoms. In addition, a trend was found in the number of emergency room visits between the two groups. The intervention group visited the emergency room more often because the nurse instructed patients to go when they recognized symptoms that needed urgent care after hours.
Discussion
Women in the intervention group appropriately used the emergency room to manage their problems after hours, whereas more women in the attention control group reported significantly more primary care visits. These findings highlight the need for health care providers representing various disciplines to coordinate services across specialties, especially for women who have depressive symptoms.
Keywords: ovarian cancer, advanced practice nurse, health care utilization, coordination of care, primary care, clinical home
Women with ovarian cancer have high utilization rates of health services (Yabroff et al., 2007). Contributing to the high rates are the multiple modalities used to treat ovarian cancer, and the complications and side effects from those treatments. Ovarian cancer is treated usually with aggressive surgery, followed shortly thereafter by chemotherapy (Hennessy, Coleman, & Markman, 2009). Postoperatively, common complications, side-effects of chemotherapies, and psychological distress from the diagnosis (Hodgkinson et al., 2007; McCorkle, Benoliel, Donaldson, et al., 1989; Norton et al., 2004) can prompt women with ovarian cancer to rely more heavily on healthcare services, thus increasing costs.
When national healthcare survey and discharge data were used to estimate health service use by women 45 years and older with cardiovascular disease, osteoporosis, breast cancer, or gynecological cancers, the resource use reported for those with ovarian cancer was substantial. Women with a primary diagnosis of ovarian cancer had almost 5 million physician office outpatient visits, over 160,000 hospital outpatient visits, and over 15,000 emergency department visits annually in 1995 (Hoerger et al., 1999).
Yabroff et al. (2007) used Surveillance, Epidemiology, and End Results (SEER) data to identify 763,527 patients over age 65 years with various cancers. Using Medicare claims data, frequency of health service use was calculated for these patients. Among this large group of patients with cancer, those with ovarian cancer (n = 16,968) had the highest mean number of physician visits (23.9 visits) and the highest estimated net patient time associated with medical care (368.1 hours) during the initial phase of care (the first 12 months). Research has focused on the improvement of survival and health outcomes of patients with ovarian cancer after they received the standard therapy, which involves aggressive cytoreductive surgery followed by platinum and paclitaxel chemotherapy (Collinson & Jayson, 2009; Hennessy et al., 2009).
A number of factors have been reported to influence health care utilization: race and socioeconomic status (Earle, Neumann, Gelber, Weinstein, & Weeks, 2002); age, increasing comorbidity, not being married, and type of surgery (Farjah et al., 2009); chemotherapy and postsurgical complications (Dy, Sharkey, Herbert, Haddad, & Wu, 2006); type of treatment, tumor type, stage, comorbidity, time since diagnosis, and quality of life (Jones & Doebbeling, 2007; Mols, Helfenrath, Vingerhoets, Coebergh, & van de Poll-Franse, 2007); education, socioeconomic status, gender, health insurance, and self-rated health status (Sadetsky et al., 2005; Shankar et al., 2007); and worse physical functioning, late-stage disease, and three or more comorbid conditions, (Kurtz, Kurtz, Given, & Given, 2005).
As a result, there is increasing interest in the potential for interventions in cancer care to reduce health services utilization while maintaining health outcomes and lowering costs. McCorkle, Benoliel, Donaldson, et al. (1989) and McCorkle et al. (1994, 2000) have demonstrated positive outcomes (decreased symptom distress, improved functional status and mental health, and longer survival) associated with a home care nursing intervention delivered by advanced practice nurses (APNs) following discharge after cancer surgery. They studied hospitalization admissions as an outcome, but the results were nonsignificant (McCorkle, Benoliel, & Georgiadou, 1989). Similarly, Bakitas et al. (2009) found nonsignificant health care utilization (reduced days in the hospital, the intensive care unit, emergency department visits) when comparing participants receiving usual oncology care to those receiving an intervention by APNs addressing physical, psychological, and care coordination.
Conversely, a study conducted by Naylor et al. (2004) with heart failure patients demonstrated that a comprehensive APN discharge intervention significantly reduced healthcare utilization, measured by readmission rates, hospital days per patient, and healthcare costs, compared to a control group. However, no additional studies were found measuring the effects of the APN role on healthcare utilization in oncology patients following hospitalization, except one nurse-directed symptom control randomized clinical trial with 222 patients undergoing chemotherapy as outpatients. Patients in the treatment group who received standardized protocols to manage their symptoms reported fewer emergency room visits than patients in the control group. The intervention was also effective in reducing the number of hospital visits for a subgroup of patients who had high symptom severity at enrollment (Kurtz, Kurtz, Given, & Given, 2006). Findings from previous studies on the effects of nursing care on health care utilization in cancer care have been limited, and additional research is warranted.
The purpose of this study was to evaluate the effectiveness of an intervention provided by APNs in conjunction with a psychiatric consultation-liaison nurse (PCLN) on patients' self-report of healthcare utilization compared to an attention control intervention for similar patients. The hypothesis was: By 6 months postsurgery for suspected ovarian cancer, women randomized to a specialized nursing intervention group would have reduced healthcare utilization compared to women in the attention control group. The impact of the interventions on healthcare utilization was evaluated, controlling for personal and clinical characteristics (age, education, comorbid conditions, physical functioning, uncertainty, depressive symptoms, symptom distress, and stage of diagnosis).
The conceptual framework used in this investigation was based on the classic work of Donabedian (1966), who identified the structure, process, and outcome as essential components of the measurement of quality in health care. Mitchell and Shortell (1997) redesigned this model, incorporating patient characteristics to accommodate for differences in case mix and severity of illness. The expanded model reflects the dynamic relationships among four components: the healthcare system, patients, interventions, and outcomes, with nursing interventions constantly working within the constraints of the system and in relation to patient characteristics to produce health outcomes (Mitchell, Ferketich, & Jennings, 1998). Patient factors are suggested to influence the nature, course, and symptom presentation of health problems, which then affect the interventions chosen by clinicians (Sidani & Braden, 1998). In turn, chosen interventions vary according to the type, complexity, and dose of the intervention; consequently affecting outcomes, including healthcare utilization.
Method
Design
A two-group, experimental, longitudinal design was used to compare women who were assigned randomly to the intervention group (n = 67) or to an attention control group (n = 70) at baseline within 48 hours after surgery and 1, 3, and 6 months after surgery. These time intervals were selected to represent critical transitions in recovery along the illness trajectory, including the first 100 days of the existential plight triggered by the diagnosis (Weisman & Worden, 1976).
Inclusion Criteria
From December 2003 to June 2006, recruitment took place at an urban teaching hospital associated with a comprehensive cancer center. Inclusion criteria were: (a) a suspected primary diagnosis of ovarian cancer following abdominal surgery; (b) prognosis of at least 6 months; (c) discharged from hospital with an order to initiate chemotherapy; (d) 21 years of age or older; and (e) living within the State of Connecticut. All subjects received their initial care on inpatient surgical units at an academic medical center in the Northeast.
Recruitment
The study was approved by the Institutional Review Boards at Yale University School of Nursing and the participating hospital. At daily gynecological oncology rounds, a staff nurse identified patients who met inclusion criteria and subsequently approached patients about their willingness to learn more about the study. The Project Director then met with eligible patients in the hospital to obtain consent and administer baseline questionnaires. Once baseline data were completed, the sealed envelope technique was used to randomize patients into the intervention or attention control group. Block randomization was done by the statistician using random tables in groups of six, and only the Project Director had knowledge of the sequence within a specific block. The intervention staff for both groups was blinded to group assignment, as well as the research assistants who interviewed patients to complete their self-report questionnaires.
Specialized Nursing Intervention
The specialized nursing intervention was designed to target specific problems within each phase of the illness trajectory. The intervention consisted of 18 contacts by an oncology APN during the first 6 months after hospital discharge. These contacts occurred in patients' homes or by telephone: two contacts per week the first 30 days and one contact every other week through 180 days. Initial contacts over the first month were more intensive to prevent and monitor postoperative complications. Subsequent contacts were bimonthly to ensure stabilization. The APN's primary objective was to assist patients in developing and maintaining self-management skills, facilitate their active participation in decisions affecting their treatment, and monitor and manage their physical and psychological health. The APN's activities included symptom management, counseling, education, direct nursing care, coordination of resources, and referrals (Hughes, Hodgson, Muller, Robinson, & McCorkle, 2000). Intervention strategies were tailored to each patient's needs and personal priorities, and were determined jointly by the APN and patient.
Screening for emotional distress was completed at baseline using the Distress Thermometer for the entire sample (Roth et al., 1998). Women in the intervention group who scored four or greater on the scale, indicating significant distress, received an evaluation by the psychiatric consultation liaison nurse (PCLN). Based on the PCLN evaluation, the APN developed a collaborative plan of care targeting the patient's specific emotional needs. Women in the attention control group who indicated emotional distress received usual care from the medical social worker assigned to the gynecological service.
All patients in the study, regardless of randomization assignment, received the Symptom Management Toolkit, a health education manual with information about intervention strategies to address 16 symptoms commonly experienced postsurgically or with chemotherapy. The Toolkit contains descriptions for each symptom and includes etiology, strategies for management, and advice about when to call the oncologist (Given, Given, & Espinosa, 2003).
Attention Control Intervention
The attention control intervention consisted of 9 contacts by a research assistant during the 6 months. The research assistant's objective was to instruct patients on use of the Toolkit and facilitate proposed strategies. Patients whose concerns extended beyond the purview of the Toolkit were encouraged to call their oncologists.
The research assistant's initial contact took place in the patient's home. Subsequent contacts were via telephone; weekly the first month followed by monthly calls through the remaining 5 months (Table 1).
Table 1. Schedule of Contacts for Intervention and Attention Control Groups.
| Group | Interventionist Qualifications | Number of subjects | Number of contacts | Nature of contacts | Intervention Components |
|---|---|---|---|---|---|
| Specialized Nursing Intervention Program (SNIP) plus | Advanced Practice Nurse in Oncology (APN) | 59 | 18 Total 2 per Week month 1 2 per Month months 2-6 | 8 home visits 7 telephone calls 3 clinic visits |
|
| Psychiatric Consultation Liaison Nurse (PCLN) with APN in oncology | Advanced Practice Nurse in Mental Health Nursing | 30 of 59 | 1 to 2 additional contacts | 1 clinic visit/home visit for evaluation telephone follow-up |
|
| Attention Control | Research Assistant with BS and MS degrees | 62 | 8 Total 1 per Week month 1 1 per Month months 2-6 | Contact 1: home visit Contacts 2-8: telephone calls |
|
Variables and Measurements
Healthcare utilization data
Health care utilization was measured as the number of inpatient admissions and outpatient visits, including emergency room visits, oncology outpatient visits, and primary care visits as reported by the patients at each of their intervention contacts. A medical record review to document healthcare utilization was done following the patients' 6-month enrollment in the study, but not all subjects received follow-up care at the cancer center. In addition, the documentation of outpatient visits was incomplete. A 95% agreement was obtained between the self-report data and the medical record review for hospitalizations and emergency room visits on the 123 participants treated at the cancer center. Therefore, only self-report data was used to include the additional 22 participants treated at network affiliate hospitals.
Covariates
Patient demographic and clinical information was self-reported and collected at baseline using an investigator-developed form. Four standardized scales with valid and reliable psychometric properties were used to measure quality of life outcomes: depressive symptoms, uncertainty, symptom distress, and physical and mental health.
Depressive symptoms were measured using the 20-item Center for Epidemiological Studies-Depression Scale (CES-D). The total score ranges from 0 to 60, with a score of 16 or more indicating impairment. Original reporting of Cronbach's alpha for the reliability of the CES-D ranged from 0.84 to 0.90 (Radloff, 1977).
Uncertainty was measured using the five items of the unpredictability subscale of the Mishel Uncertainty in Illness Scale. Mishel defines uncertainty as “the person's inability to determine the meaning of illness-related events” and unpredictability is the “lack of contingency between illness and treatment cues and illness outcomes” (Mishel, 1981, p. 259). Unpredictability scores range from 5 to 25, with higher scores indicating more uncertainty with respect to unpredictability. The scale has been found to be reliable and stable across multiple populations (Mishel, 1981).
Symptom distress was measured using the Symptom Distress Scale, which contains 13 symptoms commonly experienced by patients with cancer. Total symptom distress is obtained as the unweighted sum of the 13 items, a value that can range from 13 to 65. Both internal consistency and test-retest reliability estimates indicated the scale was reliable (McCorkle & Young, 1978).
Physical and mental health was measured using the Short-Form Health Survey (SF-12), which consists of 12 items representing physical and mental health. Higher scores represent better health status. Test-retest reliability of the physical and mental subscales have been reported as .89 and .76, respectively (Ware, Kosinski, Turner-Bowker, & Gandek, 2007).
Power Analysis
Because the clinical trial was not designed to focus on healthcare utilization outcomes in cancer patients, the sample size was not determined for this analysis. Due to a lack of studies testing the APN intervention effect on the healthcare utilization from previous studies, the power analysis for this study could not be conducted. Alternatively, the estimated healthcare utilization and effect sizes between the APN intervention and control groups are provided from the regression models in the result section.
Data Analysis
Differences in healthcare utilization between the APN intervention and control groups were examined using regression models with count data. In descriptive analysis, the proportions of zero (no utilization) and the average number of utilization instances were compared by intervention group and the stage of cancer. Healthcare utilization could occur through two phases of decision-making process (Gerdtham, 1997). The first phase represents whether patients have urgent problems to be hospitalized or visit emergency rooms, or whether they decide to visit an oncologist or primary physician. Only a small proportion of patients may have serious or urgent physical problems within 6 months after surgery. The second phase explains how many times those problems reoccur or patients decide to visit physicians repeatedly. The Poisson and negative binomial hurdle models are used to estimate the amount of healthcare utilization with two regression parts incorporating these two portions (Carmeron & Trivedi, 1998). The hurdle models were developed for comparing four types of healthcare utilization using PROC NLMIXED, SAS version 9.1.
The APN intervention group reported higher emotional distress at baseline using the Distress Thermometer than the attention control group. Therefore, in the multivariate analysis using the hurdle model, the effects of the intervention and other covariates on healthcare utilization were tested after controlling for the Distress Thermometer score at baseline. Using the likelihood function, the Akaike Information Criterion (AIC), and the Bayesian Information Criterion (BIC), either the Poisson or negative binomial hurdle model was selected for the final model. To hold the .05 level of significance for these multiple tests, p-values were compared with .0125 (= .05/4) using the Bonferroni correction. Therefore, the probability of falsely concluding significant intervention effects on any of four types of utilization is .05 if the true intervention effects on all outcomes were not significant.
Results
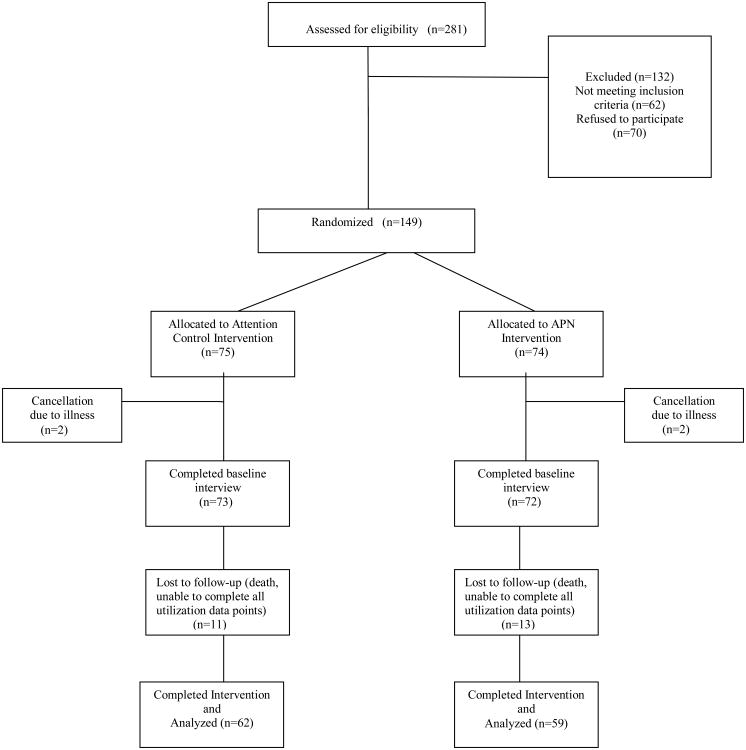
A total of 281 women were identified as eligible to participate in the study. Sixty-two were lost to follow-up, primarily because they were not scheduled for chemotherapy, or they were scheduled for treatment at another center. Of the remaining 219 women, 149 enrolled (68%). The main reasons for refusal to consent included unwillingness to take on one more thing (n = 18), not interested (n = 15), family refused (n = 14), patient too ill (n = 12), involved in another study (n = 6), requiring extra nursing care (n = 4), and fear of research (n = 1). Four enrolled subjects were excluded due to lack of complete data at baseline; the final sample consisted of 145 women (Figure 1). Among those 145 women, there were 121 women who had complete information at Wave 2, Wave 3, and Wave 4. Therefore the sample size for this analysis was 121 women with three waves of follow-up data (363 observations); 62 were from the attention control group and 59 from the intervention group.1
Figure 1. Consort Flow Diagram: Numbers of Subjects Screened and Recruited and Completed Trial.
Patient characteristics in intervention and attention control groups were similar (Table 2). The recurrent patients were about 25%. Fifty-eight percent had a primary diagnosis of ovarian cancer; 32% of the patients were diagnosed at an early stage. The average cost of medical expenditures the month before surgery was about $9,500. The mean comorbidity index was 2.9 diseases (Satariano, Ragheb, & Depuis, 1989).
Table 2. Personal Characteristics and Health Outcomes Between Intervention and Control Groups.
| APN Intervention n = 59 | Attention Control n = 62 | |
|---|---|---|
| Demographics | ||
|
| ||
| Mean (SD) | Mean (SD) | |
| Age | 60.2 (9.8) | 62.4 (12.7) |
| EDT | 5.6 (2.7) | 5.0 (2.7) |
| Race | n (%) | n (%) |
| White | 53 (89.8%) | 57 (91.9%) |
| Non-White | 6 (10.2%) | 5 (7.1%) |
| Marital Status | ||
| Never married | 6 (10.2%) | 8 (12.9%) |
| Married or with partner | 30 (50.8%) | 38 (61.3%) |
| Divorced | 18 (30.5%) | 9 (14.5%) |
| Widowed | 5 (8.5%) | 7 (11.3%) |
| Education | ||
| High school or less | 13 (22.4%) | 23 (37.1%) |
| College | 29 (50.0%) | 28 (45.2%) |
| Graduate School | 16 (27.6%) | 11 (17.7%) |
| Employment Status | ||
| Employed | 23 (39.6%) | 31 (50.0%) |
| Not working | 14 (24.1%) | 8 (12.9%) |
| Retired | 21 (36.2%) | 23 (37.1%) |
| Cancer Stage | ||
| Early | 21 (35.6%) | 18 (29.5%) |
| Late | 38 (64.4%) | 43 (70.5%) |
| Comorbidities | ||
| 0 | 8 (13.6%) | 9 (14.5%) |
| 1-2 | 16 (27.1%) | 16 (25.8%) |
| >2 | 35 (59.3%) | 37 (59.7%) |
| Income ($) | ||
| 0-29,999 | 12 (23.1%) | 11 (20.0%) |
| 30,000-59,999 | 14 (26.9%) | 15 (27.3%) |
| 60,000-and above | 16 (50.0%) | 29 (52.7%) |
| Family History of Cancer | 45 (76.3%) | 46 (74.2%) |
|
| ||
| Health Outcomes | ||
|
| ||
| M (SD) | M (SD) | |
| SF12** | 0.37 (0.20) | 0.45 (0.18) |
| Symptom Distress (SDS) ** | 1.26 (0.52) | 1.06 (0.52) |
| Depression (CES-D)** | 18.66 (7.57) | 14.62 (8.15) |
| Uncertainty (MUIS)** | 2.04 (0.69) | 1.68 (0.70) |
| Stay at hospital | 6.72 (5.07) | 6.55 (4.85) |
Notes. There is significant difference in each health outcome between APN intervention and control groups based on t-test. APN = advanced practice nurse; EDT = emotional distress thermometer; SDS = Symptom Distress Scale; CES-D = Center for Epidemiological Studies-Depression Scale; MUIS = Mishel Uncertainty in Illness Scale
Differences in individual characteristics and the baseline quality of life scales between the two groups were examined using t-tests. Patients who were assigned to the APN intervention were more likely to have less physical function, more symptom distress, more depressive symptoms, and more uncertainty at baseline compared to those assigned to the attention control group. Other individual characteristics were not significantly different between the groups.
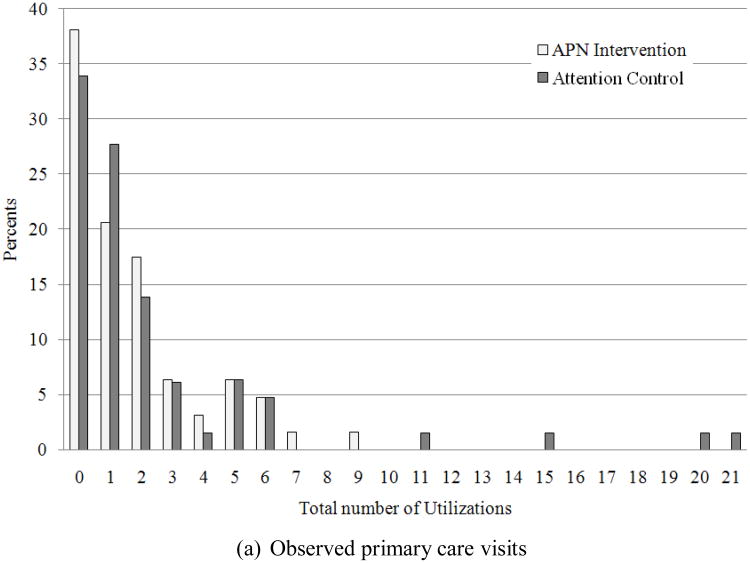
The proportion of no hospitalizations and outpatient visits and the average number of these health care utilization instances by the intervention and the cancer stage are shown in Table 3. Among individuals who reported at least one visit, patients receiving the APN intervention (2.75±2.03) tended to have fewer primary care visits compared to those in the attention control group (3.59±4.66). Within a month after hospital discharge, no significant difference in healthcare utilization was seen between the groups. Patients with late-stage cancer reported more hospitalizations. Greater average hospitalizations were observed in patients with late-stage cancer compared to those with early-stage cancer.
Table 3. Distribution of Health Care Utilization by Group and Stage of Cancer.
| Hospitalization | Emergency Room Visit | Oncology Outpatient Visit | Primary Care Visit | |||||
|---|---|---|---|---|---|---|---|---|
| None | More than one hospitalization | None | More than one visit | None | More than one visit | None | More than one visit | |
| M (SD) | M (SD) | M (SD) | M (SD) | |||||
| Intervention Group | ||||||||
| APN | 64.4% | 2.43 (2.09) | 78.0% | 1.85 (1.14) | 0.0% | 9.19 (5.74) | 32.2% | 2.75 (2.03) |
| Attention Control | 61.3% | 1.62 (0.71) | 75.8% | 1.40 (0.74) | 3.2% | 8.27 (4.49) | 29.0% | 3.59 (4.66) |
| Stage of Cancer | ||||||||
| Early Stage | 84.6% | 1.17 (0.41) | 76.9% | 1.50 (1.04) | 0.0% | 7.87 (6.10) | 28.2% | 3.57 (4.58) |
| Late Stage | 51.8% | 2.13 (2.13) | 77.8% | 1.67 (0.71) | 2.5% | 9.13 (4.62) | 32.1% | 3.02 (3.15) |
The effects of an APN intervention on four types of healthcare utilization were examined using the hurdle model after controlling for baseline distress thermometer scores and other covariates (Table 4). The regression of nonzero counts includes the covariate coefficients to estimate the mean amount of healthcare utilization, whereas the regression of zero counts represents the coefficients to estimate the probability of no utilization. Because there was no inflation of zero counts in oncology outpatient visits, a general negative binomial model without the regression of zero counts was used for oncology visits. Patients who received the APN intervention reported fewer primary care visits (beta = −0.59±0.16, p = .0003). The intervention effect was significant for primary care visits at the .05 level of significance using the Bonferroni correction.
Table 4. Effects of Intervention and Personal Characteristics on Health Care Utilization.
| Hospitalization | Emergency room visit | Oncology outpatient visit | Primary care visit | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Beta | SE | p | Beta | SE | p | Beta | SE | p | Beta | SE | p | |
| Regression of non-zero counts | ||||||||||||
| APN Intervention vs. Attention Control | 0.28 | 0.36 | .4319 | 1.02 | 0.59 | .0852 | 0.07 | 0.11 | .5359 | -0.59 | 0.16 | .0003 |
| Baseline Distress Thermometer | -0.09 | 0.07 | .2135 | -0.22 | 0.19 | .2500 | 0.02 | 0.02 | .4163 | -0.09 | 0.03 | .0071 |
| Comorbidity | 0.05 | 0.09 | .5494 | 0.34 | 0.19 | .0714 | 0.01 | 0.03 | .6027 | 0.03 | 0.04 | .5073 |
| SF12 | 1.18 | 1.43 | .4123 | -0.71 | 2.39 | .7682 | -0.25 | 0.38 | .5101 | -2.71 | 0.58 | <.0001 |
| Symptom Distress | 0.87 | 0.56 | .1243 | - | - | - | -0.07 | 0.14 | .2447 | -0.29 | 0.19 | .1216 |
| Depression | 0.00 | 0.03 | .8680 | -0.01 | 0.04 | .8597 | -0.01 | 0.01 | .4365 | 0.05 | 0.01 | <.0001 |
| Uncertainty | -0.05 | 0.31 | .8719 | 0.27 | 0.46 | .5525 | 0.27 | 0.10 | .0066 | -0.50 | 0.12 | .0001 |
| Stay at hospital | 0.05 | 0.05 | .2668 | 0.14 | 0.17 | .4125 | -0.01 | 0.01 | .6233 | -0.05 | 0.02 | .0108 |
| Stage of cancer (Late vs. Early) | 1.68 | 1.01 | .0982 | -0.46 | 0.70 | .5100 | 0.10 | 0.12 | .4144 | -0.02 | 0.15 | .8857 |
| Age | -0.03 | 0.01 | .0422 | -0.06 | 0.03 | .0506 | -0.00 | 0.01 | .6606 | -0.00 | 0.01 | .5875 |
|
| ||||||||||||
| Regression of zero counts | ||||||||||||
| APN Intervention vs. Attention Control | 0.11 | 0.45 | .8101 | 0.40 | 0.49 | .4194 | - | - | - | -0.03 | 0.46 | .9434 |
| Baseline Distress Thermometer | 0.02 | 0.09 | .7937 | 0.03 | 0.10 | .7848 | - | - | - | -0.05 | 0.09 | .6249 |
| Comorbidity | -0.14 | 0.11 | .2237 | -0.20 | 0.12 | .0996 | - | - | - | -0.12 | 0.12 | .3145 |
| SF12 | -0.24 | 1.56 | .8780 | -1.33 | 1.58 | .4019 | - | - | - | -4.21 | 1.71 | .0154 |
| Symptom Distress | 0.53 | 0.59 | .3643 | - | - | - | - | - | - | -1.41 | 0.65 | .0319 |
| Depression | -0.03 | 0.04 | .4554 | -0.01 | 0.04 | .8905 | - | - | - | -0.01 | 0.04 | .7707 |
| Uncertainty | -0.07 | 0.38 | .8602 | -0.97 | 0.46 | .0364 | - | - | - | 0.11 | 0.40 | .7731 |
| Stay at hospital | 0.11 | 0.06 | .0645 | 0.03 | 0.06 | .5468 | - | - | - | 0.07 | 0.05 | .1493 |
| Stage of cancer (Late vs. Early) | 1.91 | 0.55 | .0007 | -0.01 | 0.52 | .9900 | - | - | - | 0.16 | 0.50 | .7539 |
| Age | 0.02 | 0.02 | .4615 | 0.04 | 0.02 | .1029 | - | - | - | -0.02 | 0.02 | .4554 |
Notes. *** The p-values were evaluated with the Bonferroni correction (.05/4=.0124).
*** The negative binomial distribution was used for oncology outpatient visit, because zero was not inflated (i.e., most patients has more than one oncology outpatient visit).
Patients who had early-stage cancer were more likely to have a problem that required hospitalization (beta = 1.91±0.55, p = .0007). Older patients were associated with fewer number of hospitalizations than younger patients (beta = -0.03, SE = 0.01, p = .0422). There were no other significant covariates associated with emergency room visits. Women with greater uncertainty reported more oncology outpatient visits. Women with high emotional distress, better physical function, and more uncertainty tended not to use their primary care physicians, but women with greater depressive symptoms had significantly more visits to their primary care providers at the .05 level.
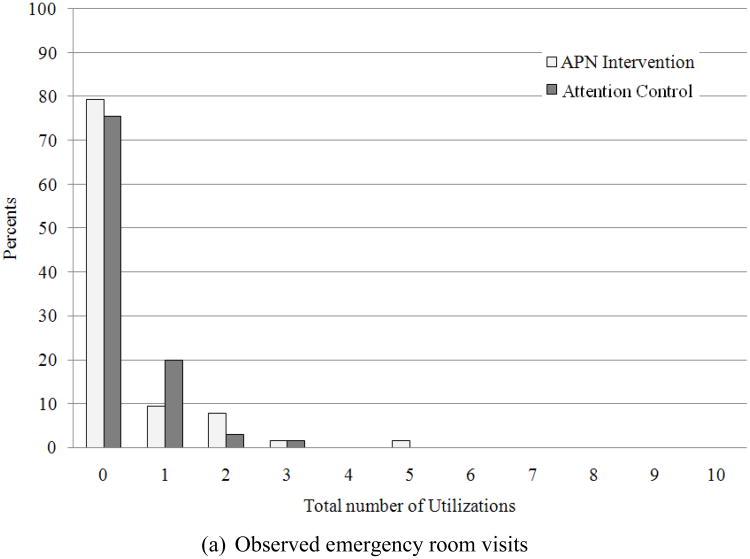
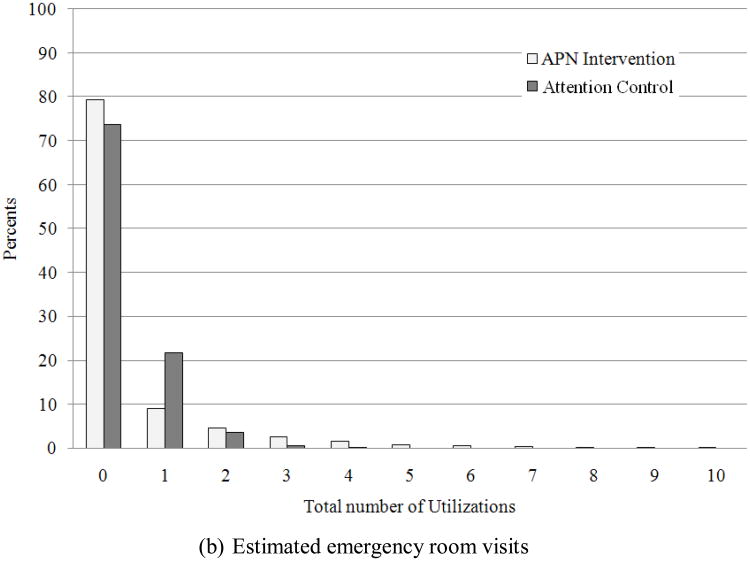
Using the estimated mean number of healthcare utilization from the models, effect sizes were estimated in four types of healthcare utilization. These effect sizes were adjusted for differences in baseline health outcomes between the intervention groups. Fairly small effect sizes were estimated in hospitalizations (effect size = 0.01) and oncology outpatient visits (effect size = 0.07). However, a relatively large effect size of 0.36 was estimated in emergency room and primary care visits. The estimated emergency visits effect size is larger in the APN intervention (APN = 0.38 vs. Attention control = 0.28), whereas primary care visits was estimated more frequently in the attention control group (APN = 1.58 vs. Control = 2.45).
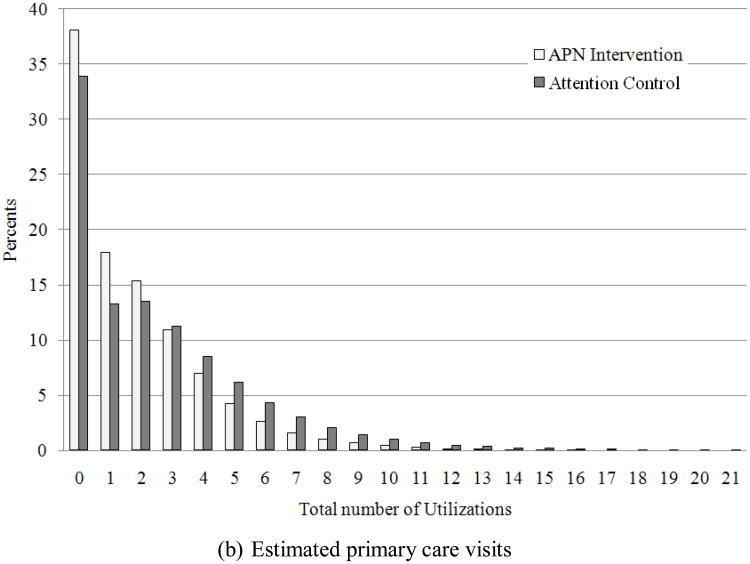
Observed distributions of healthcare utilization (emergency room visits and primary care visits) and estimated distribution from the hurdle models are shown in Figures 2 and 3. The estimated distributions from the hurdle model show a fairly good fit for the observed utilization. That is, the hurdle models successfully represent the large number of no utilization, which cannot be fitted using general regression models.
Figure 2. Observed (a) and Estimated (b) Distribution of Emergency Room Visits by Intervention.
Figure 3. Observed (a) and Estimated (b) Distribution of Primary Care Visits by Intervention.
Discussion
A 6-month intervention provided by oncology APNs was tested to see if it would produce lower healthcare utilization by women treated for ovarian cancer after surgery compared to women who received a symptom management educational intervention only. Almost 63% of women in both groups were not hospitalized and over 76% were not admitted to the emergency room over the 6 months after surgery. However, for the subsample of women who used healthcare services, there were no differences in hospitalizations between the two groups. In addition, there were no differences in oncology outpatients visits between the two groups. These two findings were expected because the women were managed by a single group of gynecological surgeons who also monitored the women for their chemotherapy treatments. The protocols were well-established and most of the hospitalizations and oncology outpatient visits were scheduled for treatment and were not urgent visits. The practice of gynecological oncology surgeons treating women with chemotherapy is standard in this specialization and may have been an important factor in the significant reduction of depressive symptoms and improved mental health in both groups. Results of the quality of life outcomes are reported elsewhere (McCorkle et al., 2009).
In the subsample of high users, there was a trend (p = .0852) in the number of emergency room visits between the two groups; the intervention group visited more often. This trend towards more emergency room visits was not surprising given that the intervention provided by the APNs included instructing patients to go there when they reported experiencing symptoms needing urgent medical care after hours. The APNs recognized symptoms related to wound infections, bleeding, and bowel obstructions that could not be managed at home. This subsample of women who went to the emergency room were younger, were receiving aggressive chemotherapy, and had greater numbers of comorbidities requiring close surveillance.
The main finding of this study was a significant difference in the number of primary care visits between the two groups. Women in the attention control group went to their primary care providers more often than the intervention group. The women in the attention control group who required more visits reported more depressive symptoms and better physical health than the APN intervention group. Since the number of women with emotional distress and comorbid conditions were equal at baseline across the two groups, it seems reasonable that the interventions provided by the APNs in conjunction with the PCLN assisted those women with depressive symptoms, whereas the attention control group sought additional help through their primary care providers. This is an important finding since neither group had additional hospitalizations.
The findings underscore that the most effective cancer care requires a practice home for each patient. This home can be housed within medical oncology or primary care, depending on the circumstances (e.g. geographical variations, insurance). The home requires that one practice team holds itself accountable to patients to guide and support patients along the cancer-care continuum. Primary care providers are key in the management of patients for their ongoing health maintenance, but they may think they do not have adequate information to answer cancer patients' questions. Oncology providers can serve as the practice home, if patients are referred to oncology upon suspicion or confirmation of a diagnosis. Ideally, through coordination of care with primary care physicians, oncology providers can ensure that patients' general preventative needs are met and comorbid conditions, including mental health conditions, are well-managed (McCorkle et al., in press).
There are a number of important limitations to be considered when interpreting the findings. These results are based on women undergoing surgery and chemotherapy for ovarian cancer and may not be applicable to people with other cancers. Also, the sample was recruited from one comprehensive cancer center at an academic facility in the Northeast, and treatments may vary by geographical regions and community settings. Data were limited to self-report questionnaires and need to be validated with other approaches. The healthcare utilization variables measured were also self-report accounts by the women and measured at varied times by both groups. These data, instead of medical record review data, are reported because not all subjects received ongoing care at the same institution and access to their medical records was not obtained for the full sample; therefore, the self-report data were more complete. Finally, the number of subjects who reported healthcare utilization was small; additional research is needed with a larger sample.
The current findings advance the understanding of healthcare services used by women while they are receiving chemotherapy for ovarian cancer. These findings highlight the need for healthcare providers representing various disciplines to coordinate services across specialties, especially for women who have high emotional distress or depressive symptoms, and who are younger. The significance of the findings regarding the presence of depressive symptoms in women who were high users of healthcare services is important for all physicians and other healthcare providers caring for women receiving cancer treatment. The transition of patients from hospital to outpatient care and from surgical services to medical oncology is a time of high uncertainty and needs to be recognized as a priority in ensuring quality care (Institute of Medicine, 2008).
Yancik, Ganz, Varricchio, and Conley (2001) have noted that little is known about the effect of comorbid conditions on cancer and cancer treatment. They have advocated for the development of systems to identify and monitor comorbid conditions at the time of diagnosis and over time. This will become even more apparent as people continue to live longer with the increased likelihood of developing cancer alongside age-related comorbid conditions, including mental health conditions. Aziz (2006) expands this recommendation to survivorship in that quality care includes systems to manage, treat, and prevent comorbidities. Multidisciplinary partnerships should begin at diagnosis, continue during treatment and throughout follow-up, and not be limited to survivorship care at the completion of treatment. Effective symptom management and recognition by clinicians of the patient's prediagnostic comorbid conditions are critical factors to be considered in the management of these women. In this study, APNs provided the essential monitoring of patients' emotional distress along with physical and psychosocial interventions to ensure recovery after surgery and during chemotherapy treatment.
Certainly the use of APNs to monitor and manage patient symptoms during cancer treatment may increase the appropriate use of emergency room services because patients were encouraged to seek the urgent care they needed. Such interventions may decrease the use of primary care services, because more everyday concerns are met by APNs in oncology outpatient settings. As a result, such interventions may save healthcare dollars in hospitalizations and increase spending in other areas. The evidence signals the need for additional research to test the effects of various models of care that can bridge between two worlds – the fragmented, poorly coordinated healthcare system and the complex biopsychosocial needs of cancer patients and their families during cancer treatment (Cheung, Neville, Cameron, Cooke, & Earle, 2009).
The committee for the IOM report (2008) developed a model for effective delivery of psychosocial services that includes coordination among specialties. Key aspects of the model were: (a) identifying physical and psychosocial health needs, (b) linking patients and families to services they need, (c) supporting patients and families as they manage the illness, (d) coordinating psychosocial and biomedical care, and (e) following up on the delivery of care to determine effectiveness, and making modifications as needed. The findings underscore the committee's recommendations, but the challenge is to identify strategies for implementing models of care for facilitating patients' coordination and management across specialties that address the whole patient and then determining how to make them cost-effective.
Acknowledgments
Funding was received from The National Institutes of Health, National Institute for Nursing Research, 1R01NR07778, R. McCorkle, PI.
Footnotes
To examine the potential bias due to the lost to follow up, a weighted analysis was performed (weight is generated based on the differences of the characteristics between the follow up and the lost 1to follow up samples). No substantial differences were found between the weighted and unweighted analysis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ruth McCorkle, The Florence S. Wald Professor of Nursing, School of Nursing, Yale University. New Haven, Connecticut.
Sangchoon Jeon, School of Nursing, Yale University, New Haven, Connecticut.
Elizabeth Ercolano, School of Nursing, Yale University, New Haven, Connecticut.
Peter Schwartz, School of Medicine, Yale University, New Haven, Connecticut.
References
- Aziz N. Late effects of cancer treatment and follow-up care needs among cancer survivors. Invited commentary and foreword. The American Journal of Nursing. 2006;106(Supplement 3):3. [Google Scholar]
- Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, Seville J, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The Project ENABLE II randomized clinical trial. JAMA. 2009;302(7):741–749. doi: 10.1001/jama.2009.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmeron AC, Trivedi PK. Regression analysis of count data. Cambridge, England: Cambridge University Press; 1998. Econometric Society Monograph No. 30. [Google Scholar]
- Cheung WY, Neville BA, Cameron DB, Cook EF, Earle CC. Comparisons of patient and physician expectations for cancer survivorship care. Journal of Clinical Oncology. 2009;27(15):2489–2495. doi: 10.1200/JCO.2008.20.3232. [DOI] [PubMed] [Google Scholar]
- Collinson F, Jayson G. New therapeutic agents in ovarian cancer. Current Opinion in Obstetrics & Gynecology. 2009;21(1):44–53. doi: 10.1097/GCO.0b013e32831ffe71. [DOI] [PubMed] [Google Scholar]
- Donabedian A. Evaluating the quality of medical care. The Milbank Memorial Fund Quarterly. 1966;44(3) 1:166–206. [PubMed] [Google Scholar]
- Dy SM, Sharkey P, Herbert R, Haddad K, Wu AW. Comorbid illnesses and health care utilization among Medicare beneficiaries with lung cancer. Critical Reviews in Oncology/Hematology. 2006;59(3):218–225. doi: 10.1016/j.critrevonc.2006.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earle CC, Neumann PJ, Gelber RD, Weinstein MC, Weeks JC. Impact of referral patterns on the use of chemotherapy for lung cancer. Journal of Clinical Oncology. 2002;20(7):1786–1792. doi: 10.1200/JCO.2002.07.142. [DOI] [PubMed] [Google Scholar]
- Farjah F, Wood DE, Varghese TK, Massarweh NN, Symons RG, Flum DR. Health care utilization among surgically treated Medicare beneficiaries with lung cancer. The Annals of Thoracic Surgery. 2009;88(6):1749–1756. doi: 10.1016/j.athoracsur.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Given BA, Given CW, Espinosa C. Symptom management toolkit. Lansing, MI: Family Care Research Program, Michigan State University; 2003. [Google Scholar]
- Gerdtham UG. Equity in health care utilization: Further tests based on hurdle models and Swedish micro data. Health Economics. 1997;6(3):303–319. doi: 10.1002/(sici)1099-1050(199705)6:3<303::aid-hec270>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Hennessy BT, Coleman RL, Markman M. Ovarian cancer. Lancet. 2009;374(9698):1371–1382. doi: 10.1016/S0140-6736(09)61338-6. [DOI] [PubMed] [Google Scholar]
- Hodgkinson K, Butow P, Fuchs A, Hunt GE, Stenlake A, Hobbs KM, et al. Long-term survival from gynecologic cancer: Psychosocial outcomes, supportive care needs and positive outcomes. Gynecologic Oncology. 2007;104(2):381–389. doi: 10.1016/j.ygyno.2006.08.036. [DOI] [PubMed] [Google Scholar]
- Hoerger TJ, Downs KE, Lakshmanan MC, Lindrooth RC, Plouffe L, Jr, Wendling B, et al. Healthcare use among U.S. women aged 45 and older: Total costs and costs for selected postmenopausal health risks. Journal of Women's Health & Gender-Based Medicine. 1999;8(8):1077–1089. doi: 10.1089/jwh.1.1999.8.1077. [DOI] [PubMed] [Google Scholar]
- Hughes LC, Hodgson NA, Muller P, Robinson LA, McCorkle R. Information needs of elderly postsurgical cancer patients during the transition from hospital to home. Journal of Nursing Scholarship. 2000;32(1):25–30. doi: 10.1111/j.1547-5069.2000.00025.x. [DOI] [PubMed] [Google Scholar]
- Cancer care for the whole patient: Meeting psychosocial needs. Institute of Medicine; Washington, DC: National Academy of Science; 2008. [PubMed] [Google Scholar]
- Jones LE, Doebbeling CC. Beyond the traditional prognostic indicators: The impact of primary care utilization on cancer survival. Journal of Clinical Oncology. 2007;25(36):5793–5799. doi: 10.1200/JCO.2007.13.6127. [DOI] [PubMed] [Google Scholar]
- Kurtz ME, Kurtz JC, Given CW, Given BA. Utilization of services among elderly cancer patients: Relationship to age, symptoms, physical functioning, cormorbidity, and survival status. Ethnicity & Disease. 2005;15(2 Supplement 2):S17–S22. [PubMed] [Google Scholar]
- Kurtz ME, Kurtz JC, Given CW, Given B. Effects of a symptom control intervention on utilization of health care services among cancer patients. Medical Science Monitor. 2006;12(7):CR319–CR324. [PubMed] [Google Scholar]
- McCorkle R, Benoliel JQ, Donaldson G, Georgiadou F, Moinpour C, Goodell B. A randomized clinical trial of home nursing care of lung cancer patients. Cancer. 1989;64(6):1375–1382. doi: 10.1002/1097-0142(19890915)64:6<1375::aid-cncr2820640634>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- McCorkle R, Benoliel JQ, Georgiadou F. The effects of home care on patients & symptoms, hospitalizations, and complications. In: Funk SG, Tornquist EM, Champagne MT, Copp LA, Wiese RA, editors. Key aspects of comfort: Management of pain, fatigue and nausea. New York, NY: Springer; 1989. [Google Scholar]
- McCorkle R, Dowd M, Ercolano E, Schulman-Green D, Williams AL, Siefert ML, et al. Effects of a nursing intervention on quality of life outcomes in post-surgical women with gynecological cancers. Psycho-Oncology. 2009;18(1):1365–1375. doi: 10.1002/pon.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCorkle R, Ercolano E, Lazenby M, Schulman-Green D, Schilling L, Korig K, et al. Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA: A Journal for Clinicians. doi: 10.3322/caac.20093. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCorkle R, Jepson C, Malone D, Lusk E, Braitman L, Buhler-Wilkerson E, et al. The impact of posthospital home care on patients with cancer. Research in Nursing & Health. 1994;17(4):243–251. doi: 10.1002/nur.4770170403. [DOI] [PubMed] [Google Scholar]
- McCorkle R, Strumpf NE, Nuamah IF, Adler DC, Cooley ME, Jepson C, et al. A specialized home care intervention improves survival among older post-surgical cancer patients. Journal of the American Geriatrics Society. 2000;48(12):1707–1713. doi: 10.1111/j.1532-5415.2000.tb03886.x. [DOI] [PubMed] [Google Scholar]
- McCorkle R, Young K. Development of a symptom distress scale. Cancer Nursing. 1978;1(5):373–378. [PubMed] [Google Scholar]
- Mitchell PH, Fertetich S, Jennings BM. Quality health outcomes model. American Academy of Nursing Expert Panel on Quality Health Care. Image: The Journal of Nursing Scholarship. 1998;30(1):43–46. doi: 10.1111/j.1547-5069.1998.tb01234.x. [DOI] [PubMed] [Google Scholar]
- Mitchell PH, Shortell SM. Adverse outcomes and variations in organization of care delivery. Medical Care. 1997;35(11 Supplement):NS19–NS32. doi: 10.1097/00005650-199711001-00003. [DOI] [PubMed] [Google Scholar]
- Mishel MH. The measurement of uncertainty in illness. Nursing Research. 1981;30(5):258–263. [PubMed] [Google Scholar]
- Mols F, Helfenrath KA, Vingerhoets AJ, Coebergh JW, van de Poll-Franse LV. Increased health care utilization among long-term cancer survivors compared to the average Dutch population: A population-based study. International Journal of Cancer. 2007;121(4):871–877. doi: 10.1002/ijc.22739. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Brooten DA, Campbell RL, Maislin G, MaCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatrics Society. 2004;52(5):675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- Norton TR, Manne SL, Rubin S, Carlson J, Hernandez E, Edelson MI, et al. Prevalence and predictors of psychological distress among women with ovarian cancer. Journal of Clinical Oncology. 2004;22(5):919–926. doi: 10.1200/JCO.2004.07.028. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D: Scale A self-report depression scale for researching the general population. Application of Psychological Measures. 1977;1:385–401. [Google Scholar]
- Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC. Rapid screening for psychologic distress in men with prostate carcinoma: A pilot study. Cancer. 1998;82(10):1904–1908. doi: 10.1002/(sici)1097-0142(19980515)82:10<1904::aid-cncr13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Sadetsky N, Lubeck D, Latini DM, Pasta DJ, Kawakami J, DuChane J, et al. Demographics, insurance coverage, and utilization of medical services in newly diagnosed prostate cancer: Data from caPSURE. Managed Care Interface. 2005;18(2):25–30. [PubMed] [Google Scholar]
- Shankar SM, Carter A, Sun CL, Francisco L, Baker KS, Gurney JG, et al. Health care utilization by adult long-term survivors of hematopoietic cell transplant: Report from the Bone Marrow Transplant Survivor Study. Cancer Epidemiology, Biomarkers & Prevention. 2007;16(4):834–839. doi: 10.1158/1055-9965.EPI-06-0714. [DOI] [PubMed] [Google Scholar]
- Satariano WA, Ragheb NE, Depuis MH. Comorbidity in older women with breast cancer: An epidemiologic approach. In: Yancik R, Yates J, editors. Cancer in the elderly: Approaches to early detection and treatment. New York, NY: Springer; 1989. [Google Scholar]
- Sidani S, Braden C. Evaluating nursing interventions: A theory-driven approach. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Ware JE, Kosinski M, Turner-Bowker DM, Gandek MS. User's manual for SFv2 Health survey(With a supplement documenting Sf-12 Health survey) Boston, MA: Quality Metric Incorporated and Health Assessment Lab; 2007. [Google Scholar]
- Weisman AD, Worden JW. The existential plight in cancer: Significance of the first 100 days. International Journal of Psychiatry in Medicine. 1976;7(1):1–15. doi: 10.2190/uq2g-ugv1-3ppc-6387. [DOI] [PubMed] [Google Scholar]
- Yabroff KR, Davis WW, Lamont EB, Fahey A, Topor M, Brown ML, et al. Patient time costs associated with cancer care. Journal of the National Cancer Institute. 2007;99(1):14–23. doi: 10.1093/jnci/djk001. [DOI] [PubMed] [Google Scholar]
- Yancik R, Ganz PA, Varricchio CG, Conley B. Perspectives on comorbidity and cancer in older patients: Approaches to expand the knowledge base. Journal of Clinical Oncology. 2001;19(4):1147–1151. doi: 10.1200/JCO.2001.19.4.1147. [DOI] [PubMed] [Google Scholar]