Abstract
Bronchodilators are a central therapy for symptom relief in respiratory diseases such as chronic obstructive pulmonary disease (COPD) and asthma, with inhaled β2-adrenoceptor agonists and anticholinergics being the primary treatments available. The present studies evaluated the in vivo pharmacology of (R)-6-[[3-[[4-[5-[[2-Hydroxy-2-(8-hydroxy-2-oxo-1,2-dihydroquinolin-5-yl)ethyl]amino]pent-1-ynyl]phenyl]carbamoyl]phenyl]sulfonyl]-4-[(3-methoxyphenyl)amino]-8-methylquinoline-3-carboxamide (GS-5759), a novel bifunctional compound with both phosphodiesterase 4 (PDE4) inhibitor and long-acting β2-adrenoceptor agonist (LABA) activity, which has been optimized for inhalation delivery. GS-5759 dose-dependently inhibited pulmonary neutrophilia in a lipopolysaccharide (LPS) aerosol challenge model of inflammation in rats with an ED50 ≤ 10 μg/kg. GS-5759 was also a potent bronchodilator with an ED50 of 0.09 μg/kg in guinea pigs and 3.4 μg/kg in dogs after methylcholine (MCh) and ragweed challenges respectively. In cynomolgus monkeys, GS-5759 was dosed as a fine-particle dry powder and was efficacious in the same dose range in both MCh and LPS challenge models, with an ED50 = 70 μg/kg for bronchodilation and ED50 = 4.9 μg/kg for inhibition of LPS-induced pulmonary neutrophilia. In models to determine therapeutic index (T.I.), efficacy for bronchodilation was evaluated against increased heart rate and GS-5759 had a T.I. of 700 in guinea pigs and >31 in dogs. In a ferret model of emesis, no emesis was seen at doses several orders of magnitude greater than the ED50 observed in the rat LPS inflammation model. GS-5759 is a bifunctional molecule developed for the treatment of COPD, which has both bronchodilator and anti-inflammatory activity and has the potential for combination as a triple therapy with a second compound, within a single inhalation device.
Keywords: Animal model, anti-inflammatory, β2-adrenoceptor agonist, bronchodilator, COPD, phoshphodiestersae 4
Introduction
Inhaled bronchodilators are the cornerstone for symptom relief in chronic obstructive pulmonary disease (COPD) with β2-adrenoceptor agonists and muscarinic receptor antagonists the primary therapies prescribed (Cazzola et al. 2012a). Recently the oral phosphodiesterase 4 (PDE4) inhibitor roflumilast (Daxas®; Daliresp™) has been registered for the treatment of moderate to severe COPD for patients with associated chronic bronchitis and at risk of exacerbations. Oral PDE4 inhibitors are dose-limited, however, due to low tolerability and adverse events such as nausea and emesis (Spina 2008). The relatively narrow window for efficacy over tolerability may limit the effectiveness of this class of compound and topical inhalation may provide an alternative approach to increase the therapeutic window but to date, no inhaled PDE4 inhibitors have reached late-stage clinical trials.
Bifunctional or dual selective molecules that contain two pharmacophores that can engage separate mechanisms which are covalently linked is an approach to increase the number of therapeutic targets that can be engaged from a single inhalation device. Novel bifunctional molecules containing both a β2 agonist and a muscarinic antagonist moiety have been developed and several have entered into late-stage clinical trials (Cazzola et al. 2012b). Such molecules can have several potential advantages, one of these being that the greater molecular weight achieved through covalently linking two molecules can aid in lung retention and reduce systemic exposure to improve the therapeutic window (Robinson et al. 2011). A single molecule also provides the advantage of matched pharmacokinetics, simplified formulation and clinical development, compared to two distinct chemical entities in combination (Matera et al. 2011). Additionally, a single chemical entity that interacts with two distinct mechanisms which are delivered in an optimal ratio within the lung microenvironment provides the greatest opportunity for local additive or synergistic activity (Phillips and Salmon 2012).
β2-adrenoceptors are present in many tissues and organs throughout the body playing a central role in pathophysiology and their impaired function during ageing has been implicated in diseases such as diabetes (Santulli et al. 2012; Santulli and Iaccarino 2013). β2-adrenoceptor agonists signal via Gs proteins, which by coupling to adenylyl cyclase, increases intracellular cyclic adenosine monophosphate (cAMP) production. Inhibition of PDE4, the enzyme responsible for hydrolyzing cAMP, also leads to elevated cellular levels. Engagement of both mechanisms simultaneously has been shown to have superior anti-inflammatory and antifibrotic effects in monocytes, fibroblasts, and in epithelial cells (Seldon et al. 2005; Tannheimer et al. 2012a,b; Moodley et al. 2013). A bifunctional compound with β2-adrenoceptor agonist and PDE4 inhibitor activity optimized for inhaled use may provide additive or synergistic activity and maximize local lung efficacy while maintaining a high therapeutic margin.
(R)-6-[[3-[[4-[5-[[2-Hydroxy-2-(8-hydroxy-2-oxo-1,2-dihydroquinolin-5-yl)ethyl]amino]pent-1-ynyl]phenyl]carbamoyl]phenyl]sulfonyl]-4-[(3-methoxyphenyl)amino]-8-methylquinoline-3-carboxamide (GS-5759) is a bifunctional compound with two pharmacophores covalently linked, and has both β2-adrenoceptor agonist and PDE4 inhibitor activity and the in vitro pharmacological profile of this molecule has been described (Tannheimer et al. 2014). These studies demonstrated that GS-5759 had low nanomolar potency at β2-adrenoceptors and at PDE4 isoenzymes. GS-5759 is a full and potent β2-adrenoceptor agonist (EC50 < 10 nmol/L) in guinea pig tissue strips with slow dissociation kinetics. It also has anti-inflammatory activity in human peripheral blood monocytes and neutrophils with high potency (IC50’s < 10 nmol/L), an activity which was contributed to by engagement of both mechanisms. In the present studies, we provide data demonstrating the bronchodilator activity for GS-5759 following bronchoconstriction challenges in three preclinical animal species and dose-dependent anti-inflammatory activity in two rodent models of COPD. Additionally, when GS-5759 was delivered topically as a formulated dry powder in nonhuman primates it demonstrated dose-dependent bronchodilator and anti-inflammatory activity. The potential of GS-5759 to cause cardiovascular changes and its tolerability related to PDE4 inhibitor side effects was also investigated.
Materials and Methods
Compound preparation and dosing
The test compounds GS-5759, 6-(3-(dimethylcarbamoyl)phenylsulfonyl)-4-(3-methoxyphenylamino)-8-methylquinoline-3-carboxamide (GSK256066), and indacaterol were synthesized by Gilead chemists. Roflumilast was purchased from Kemprotec Limited (Middlesbrough, UK). For the studies employing mice, rats, ferrets or guinea pigs, GS-5759 was prepared and dosed as a fine-particle suspension to anaesthetized animals intratracheally (IT) by bolus delivery directly into the lungs in a phosphate-buffered saline (PBS) or saline vehicle. Typical particle size distributions were 50% of the material <4 μm and 90% of the material <12 μm. For studies in dogs and monkeys, a micronized dry powder formulation was insufflated into the lungs of anaesthetized animals via a cuffed endotracheal tube. Typical particle size distributions were 50% of the material <3 μm and 90% of the material <11 μm.
Animals
Male Lewis rats and C3H/HeN mice were obtained from Charles River (Hollister, CA) and had access to 5053 Rodent Chow (PMI Nutrition International, Brentwood, MO) and water ad libitum. Rats were housed on a 12-h lights-on, lights-off cycle and acclimated to their housing facilities for a minimum of 5 days prior to use. Studies were performed at an off-site vivarium in Seattle, Washington with approval from a local Institutional Animal Care and Use Committee. Male Dunkin–Hartley guinea pigs (500–700 g), free of guinea pig pathogens, were obtained from Jackson Laboratories (Wilmington, MA). Neutered and descented male ferrets were obtained from Triple F Farms (∼12 weeks old, Sayre, PA). Cynomolgus monkeys were obtained from the Lovelace Respiratory Research Institute (LRRI) breeding colony (Albuquerque, NM). Beagles were either purchased from Covance (male naïve for safety studies, Chandler, AZ) or born and maintained in the LRRI colony and housed in kennel buildings with access to indoor and outdoor runs. All procedures were conducted under protocols approved by the Institutional Animal Care and Use Committee at LRRI, which is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International.
Acetylcholine-induced bronchoconstriction in conscious guinea pigs
Male Dunkin–Hartley guinea pigs (500–700 g, n = 6) were anaesthetized with isoflurane and IT dosed with GS-5759 (6.2–124 μg/kg) or indacaterol (30 μg/kg). Animals were allowed to recover and changes in lung function (expressed as area under the curve (AUC) of PenH for 20 min) to acetylcholine (ACh) aerosol challenge (4 mg/mL for 1 min) was assessed in Buxco chambers (Wilmington, NC). The endpoint PenH was calculated as a ratio of peak expiratory pressure over peak inspiratory peak multiplied by the pause. ACh challenges were performed at 24 h before compound treatment and 4, 8, and 24 h post compound treatment.
Inhaled lipopolysaccharide-induced pulmonary neutrophilia in lewis rats
Male Lewis rats (320–400 g) were pretreated orally or IT (under 3–4% isoflurane anaesthesia) with the appropriate dose of test compound or vehicle alone (PO vehicle: 0.5% methylcellulose in water [Sigma-Aldrich, St. Louis, MO]; intratracheal vehicle: 0.5% Tween-20 in PBS) at a dose volume of 10 mL/kg for oral delivery or 0.5 mL/kg for intratracheal delivery. Formulations for intratracheal dosing studies were administered as fine-particle suspensions. Two hours following intratracheal pretreatments or 1 h following oral pretreatments, rats were exposed to an aerosolized lipopolysaccharide (LPS) solution (1.0 mg/mL) from Escherichia coli, serotype 026:B6 (Sigma-Aldrich) at a rate of 3.0 L/min for 20 min using a segmented rat exposure chamber (Braintree Scientific, Inc., Braintree, MA). Following LPS exposure, rats were euthanized 2 h post-LPS exposure for cytokine analysis or 4 h post-LPS for cell and pulmonary neutrophil differentiation by pentobarbital overdose (390 mg, i.p.). Bronchoalveolar lavage (BAL) fluid was collected through a 14-gauge blunt needle inserted into the exposed trachea using five, 5-mL washes of PBS. For cytokine studies (n = 6 per group), BAL fluid was collected 2 h post-LPS exposure, centrifuged and supernatants were collected and frozen on dry ice. Rat tumour necrosis factor-α (TNF-α), chemokine (C C motif) ligand 2 (CCL2), chemokine (C C motif) ligand 3 (CCL3), and interleukin-1α (IL-1α) concentrations in undiluted BAL fluid supernatants were measured by Procarta cytokine multiplex kit (Affymetrix/Panomics, Santa Clara, CA), run according to the manufacturer’s protocol. Concentration of cytokines (pg/mL) was calculated from a standard curve and results reported as mean ± SEM. For dose–response studies (n = 5–18) per group, BAL fluid was collected 4 h post-LPS exposure, centrifuged, resuspended in 3 mL of PBS and total cell counts were performed on a Countess Cell Counter (Invitrogen, Carlsbad, CA) with differential cell counts performed after May–Grunwald (Sigma-Aldrich) and Giemsa (Richard Allen Scientific, Kalamazoo, MI) staining. Percentage and differential cell counts were determined following microscopic counting of a minimum 300 cells per sample.
Cigarette smoke-exposed C3H/HeN mice
C3H/HeN female mice (n = 6–8) were lightly anaesthetized with isoflurane and IT dosed with compounds either once or twice daily, except for ciclesonide which was dosed orally. Each day, 1 h after compound dosing, mice were exposed (whole body exposure) to cigarette smoke for 6 h per day over 3 weeks (5 day, 5 day, 4 day), (mean exposure of 100 mg (first 5 days) and 250 mg (last 9 days) of total particulate matter/m3) to smoke generated from Kentucky 2R4F research cigarettes (Kentucky Tobacco Research and Development Center, University of Kentucky, Lexington, KY). Twenty four hours following the final exposure, BAL were performed and the total and individual cell numbers counted in the lavage fluid.
Non-human primate lung resistance and pulmonary neutrophil infiltration models
For lung resistance studies, cynomolgus monkeys (n = 6) were anaesthetized and then intubated with an endotracheal tube and micronized powders of GS-5759 (7–133 μg/kg) or indacaterol (27 or 66 μg/kg) were insufflated into the lungs. Two hours later animals were challenged with increasing methylcholine (MCh) aerosol challenges until lung resistance increased up to 150% (PC150) of the baseline value. The amount of protection achieved by the compounds was assessed for each animal compared to its own PC150 value attained 1 week previously when they had received vehicle only. These PC150 data were transformed for each compound dose to a percentage inhibition of MCh-induced bronchoconstriction compared to vehicle treatment. For the pulmonary neutrophilia model, cynomolgus monkeys were anaesthetized and then intubated with an endotracheal tube and micronized powders of GS-5759 (2–700 μg/kg) or GSK256066 (4.3 or 43 μg/kg) were insufflated into the lungs. Two hours later animals were again anaesthetized and exposed to an aerosol of LPS (1.0 mg/mL) through a face mask for 15 min. Twenty-four hours post-LPS, BAL were performed and the number of total and individual cells counted in the lavage fluid. Neutrophils are the primary inflammatory cell recruited in the model and these cells were used as the primary readout.
Simultaneous measurement of lung resistance and heart rate in anaesthetized guinea pigs
Male Dunkin–Hartley guinea pigs (500–700 g, n = 3–6) were anaesthetized with ketamine and xylazine. The trachea was then cannulated and attached to a ventilator and then the left common carotid artery monitored for heart rate and the right jugular vein cannulated for intravenous ACh challenge. ACh challenges (7.5–250 μg/mL/kg) were performed to establish a dose response for lung resistance (RL) and baseline heart rate (beats/min) was monitored. Guinea pigs were then IT dosed with GS-5759 (0.02–62.1 μg/kg) or indacaterol (0.01–10 μg/kg) and heart rate was monitored throughout the rest of the experiment. Two hours after dosing, a second ACh challenge was performed and airway resistance measured and compared to predosing baseline measurements.
Measurement of pulmonary resistance and heart rate in beagle dogs
Male beagle dogs (2.5–4 years, n = 4), sensitized to ragweed (RW) allergen early in life, were used for this efficacy study (Redman et al. 2001; Barrett et al. 2003). These dogs have increased RW-specific IgE and IgG with increased airways hyperresponsiveness to inhaled RW and MCh and lung eosinophilia. For the total pulmonary resistance studies, sensitized dogs were anaesthetized, intubated with a cuffed endotracheal tube, and micronized powders of GS-5759 (1.4–18.2 μg/kg) or indacaterol (0.3–10.6 μg/kg) were insufflated into the lung. Inhibition of bronchoconstriction was compared to vehicle treatment done about 2 weeks prior to first treatment. The dogs were challenged with a previously determined dose of RW that led to an immediate bronchoconstriction (∼300–400% increase in pulmonary resistance). One hour post dosing, animals received an aerosol RW allergen challenge to the lungs and changes in pulmonary resistance (RL) were monitored for the next 30 min. In parallel studies to monitor heart rate effects, a separate group of naïve dogs (10.1–12.4 kg) were implanted with telemeters (TL11M2-D70-PCT; Data Sciences International, Minneapolis, MN) that allowed for continuous monitoring of heart-rate (vehicle n = 4, compound treated n = 3–4) and anaesthetized with isoflurane and dosed as above (without allergen challenge) with GS-5759 (10, 50 and 103 μg/kg) and indacaterol (3 and 10 μg/kg), and heart rate and blood pressure monitored for 200 min post dosing.
Ferret emesis model
Ferrets (sex unknown, n = 4) were dosed orally with roflumilast (0.1–10 mg/kg) or IT with GS-5759 (300–3000 μg/kg), and were monitored for 3 h post dosing and the number of emetic events within that time counted.
Statistical analysis
Data are presented as the arithmetic mean ± SEM for the raw data or as the mean ± SEM of the percentage of the vehicle response or where each animal acted as its own control. Statistical analysis was performed for each study using one-way analysis of variance (ANOVA) employing Bonferroni correction for normally distributed data or Dunnett’s correction for nonparametric data to evaluate for specific differences between individual groups. For dog heart rate and blood pressure studies, two-way ANOVA matched by column, Bonferroni post test to compare all columns was performed.
A value of P > 0.05 was considered statistically significant (GraphPad Prism, San Diego, CA).
Results
GS-5759 was made by covalently linking the pharmacophores of an inhaled β2-adrenoceptor agonist (Rossi and Polese 2013), with the pharmacophore of an inhaled PDE4 inhibitor (Singh et al. 2010). Due to the similarity of their pharmacophores, indacaterol and GSK256066 were used as comparator molecules in our studies in a molar dose-matched fashion as well as with the oral PDE4 inhibitor roflumilast.
Potency and duration of bronchoprotection against ACh-induced bronchoconstriction in conscious guinea pigs
When administered IT, GS-5759 (6.2, 62 or 124 μg/kg) demonstrated a dose- and time-dependent protection against ACh-induced bronchoconstriction. At the highest dose GS-5759 (124 μg/kg) inhibited bronchoconstriction by 77 ± 5% (P < 0.01) at 4 h post dosing, 60 ± 21% (P < 0.01) at 8 h and 36 ± 25% at 24 h. When dosed at equimolar 70 nmol/kg doses, both GS-5759 and indacaterol (30 μg/kg) had similar dose- and time-dependent bronchoprotection profiles. At 4 h post dosing GS-5759 had 62 ± 17% (P < 0.01) bronchoprotection compared to 55 ± 27% (P < 0.05) for indacaterol, at 8 h 49 ± 23% (P < 0.05) compared to 52 ± 15% (P < 0.05) and at 24 h post dosing 24 ± 27% compared to 14 ± 13% for indacaterol (Fig. 1).
Figure 1.
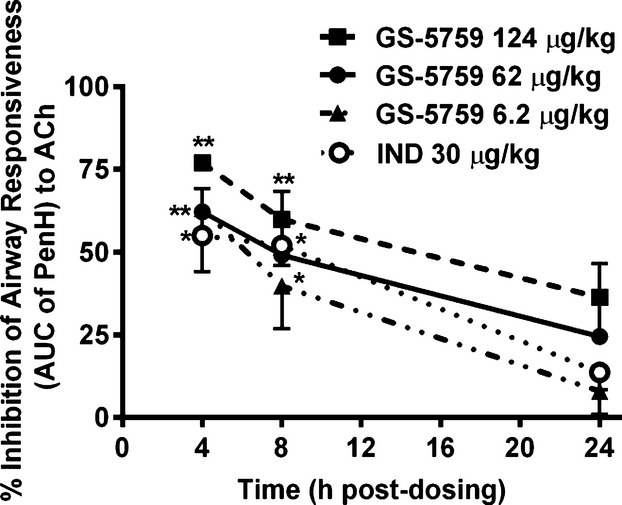
Dose- and time-dependent bronchoprotection against ACh-induced bronchoconstriction by GS-5759 in Dunkin–Hartley guinea pigs. ACh challenges were performed at 24 h before compound treatment and 4, 8, and 24 h post compound treatment. Data represent the mean ± SEM of the percentage inhibition of bronchoconstriction as measured by PenH compared to a precompound dosing level elicited by the same dose of ACh, with each animal acting as its own control (n = 6 animals per dose-group), *P < 0.05, **P < 0.01 compared to vehicle treatment. IND, indacaterol.
Anti-inflammatory activity of GS-5759 in an LPS-induced pulmonary neutrophilia model in lewis rats
In vivo anti-inflammatory activity was assessed in an LPS aerosol-induced pulmonary inflammation model in Lewis rats. Neutrophils in BAL fluid were evaluated 4 h post-LPS exposure with typically 8–10 × 106 cells counted compared to 2–5 × 104 cells in saline exposed control animals. GS-5759 demonstrated a dose-dependent inhibition of neutrophils counted in BAL fluid with an ED50 ≤ 10 μg/kg (10 nmol/kg) and maximum inhibition of 85 ± 2.7% (P < 0.001) at 300 μg/kg (311 nmol/kg). In comparison, the inhaled PDE4 inhibitor GSK256066 dose-dependently inhibited neutrophilia with an ED50 = 55 μg/kg (106 nmol/kg) and maximum inhibition of 79 ± 7.5% (P < 0.001) at 300 μg/kg (578 nmol/kg). Oral administration of roflumilast also demonstrated a dose-dependent inhibition of BAL neutrophilia with an ED50 = 1000 μg/kg (2480 nmol/kg) and maximum inhibition of 73 ± 10% (P < 0.05) at 10,000 μg/kg (24,802 nmol/kg). Indacaterol had a modest effect on LPS-induced neutrophilia attaining 48 ± 11% inhibition at 100 μg/kg (Fig. 2A).
Figure 2.
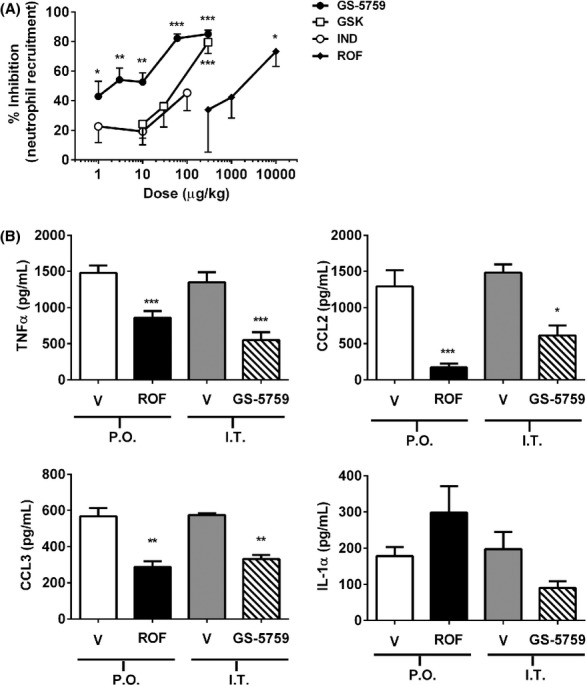
Dose-related inhibition of neutrophil recruitment and proinflammatory cytokine production by GS-5759 in the BAL of LPS-exposed Lewis rats. (A) Data represent the mean ± SEM of the percent maximum inhibition of neutrophils in BAL fluid compared to vehicle-treated animals 4 h post-LPS aerosol exposure for n = 5–18 animals per group. (B) Data represent the mean ± SEM of proinflammatory cytokines in BAL fluid 2 h post-LPS aerosol exposure for n = 6 animals per group. Open bars represent oral vehicle, black bars represent roflumilast (10 mg/kg, oral), shaded bars represent intratracheal vehicle and hatched bars represent GS-5759 (300 μg/kg, IT). *P < 0.05, **P < 0.01, ***P < 0.001 compared to vehicle-treated animals dosed via the same route of administration. GSK is GSK256066, IND, indacaterol; ROF, roflumilast.
In separate experiments, proinflammatory cytokines were measured in BAL fluid at 2 h post-LPS exposure. Robust levels of IL-1α (197 ± 47 pg/mL), TNF-α (1348 ± 139 pg/mL), CCL2 (1483 ± 114 pg/mL) and CCL3 (574 ± 10 pg/mL) were induced following LPS exposure compared to saline exposed animals (85 ± 24 pg/mL in all groups). GS-5759 (300 μg/kg) inhibited TNF-α by 55 ± 12% (P < 0.001) and the neutrophil chemokines CCL2 and CCL3 by 56 ± 11% (P < 0.05) and 42 ± 2% (P < 0.01) respectively. In comparison, roflumilast (10 mg/kg, oral) inhibited TNF-α by 42 ± 2% (P < 0.001), CCL2 by 84 ± 5% (P < 0.001), and CCL3 by 49 ± 5% (P < 0.01). Neither compound markedly inhibited IL-1α (Fig. 2B).
Effect of GS-5759 in a cigarette smoke-induced model of pulmonary inflammation in mice
The activity of GS-5759 was assessed in an 18 days cigarette smoke-induced pulmonary inflammation model in C3H/HeN mice. Cigarette smoke exposure induced pulmonary neutrophilia in vehicle-treated mice with a mean of 15.8 × 104 ± 2.8 cells/mL compared to 0.34 × 104 ± 0.20 cells/mL in vehicle-treated and air-exposed control mice (P < 0.001) (Fig. 3). GS-5759 (0.3 or 1.0 mg/kg, q.d.) had little effect on pulmonary neutrophilia but dosed at 3.3 mg/kg, b.i.d. caused a 62 ± 6% inhibition compared to vehicle-treated and smoke-exposed mice (P < 0.05). GSK256066 (0.57 mg/kg) and indacaterol (0.43 mg/kg) dosed once daily had no effect on pulmonary neutrophilia, and when they were dosed in combination (molar-matched to GS-5759 1.0 mg/kg) they elicited a 40 ± 8% inhibition which did not attain statistical significance. The glucocorticosteroid ciclesonide (1.0 mg/kg) dosed q.d. orally, also had no effect on pulmonary neutrophilia.
Figure 3.
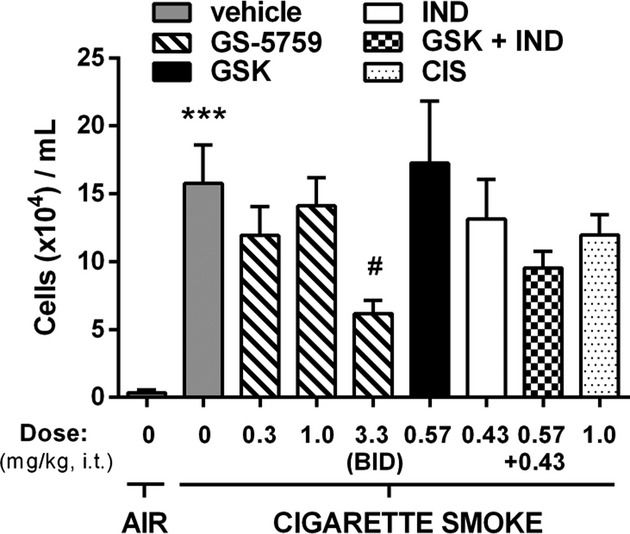
Dose-related inhibition of neutrophil recruitment by GS-5759 in the BAL of cigarette smoke-exposed C3H/HeN mice. Data represent the mean ± SEM neutrophil numbers in the BAL fluid following cigarette smoke exposure of mice over 18 days (n = 6–8). GSK, GSK256066; IND, indacaterol; CIS, ciclesonide. ***P < 0.001 compared to vehicle-treated and air-exposed mice, #P < 0.05 compared to vehicle-treated and smoke-exposed mice.
Evaluation of bronchodilator and anti-inflammatory potency of GS-5759 in cynomolgus monkeys
Studies were conducted to evaluate the effect of GS-5759 (micronized dry powder formulation) on MCh-induced lung resistance and LPS-induced neutrophilia in cynomolgus monkeys. Effects on bronchoconstriction were evaluated as PC150 (concentration of MCh required to cause a 150% increase in lung resistance) compared to baseline levels, and the mean concentration required to achieve PC150 following vehicle treatment was 103 ± 30 mg/mL. GS-5759 (7–133 μg/kg) inhibited MCh-induced lung resistance in a dose-dependent manner reaching a maximum plateau of inhibition at doses of 70 μg/kg (66 ± 5%, P < 0.05) and 133 μg/kg (65 ± 10%, P < 0.05). Indacaterol dosed with molar-matched equivalents to GS-5759 (70 and 133 μg/kg) caused 53 ± 9% (27 μg/kg) and 55 ± 10% (66 μg/kg) protection respectively (Fig. 4A). In the inflammation model, LPS exposure was employed with BAL 24 h post challenge. LPS caused an increase in neutrophils recovered in BAL fluid of 2.0 × 106 ± 0.63 cells/mL compared to 1.4 × 103 ± 1.0 cells/mL in saline exposed monkeys (P < 0.001). GS-5759 demonstrated a dose-related inhibition of pulmonary neutrophilia measured in BAL fluid with an ED50 of 4.9 μg/kg (5.0 nmol/kg) and a maximal 81% ± 16 (P < 0.05) inhibition at the 700 μg/kg dose. At doses of 70 and 7 μg/kg GS-5759 inhibited BAL neutrophilia by 64 ± 10% (P < 0.05) and 46 ± 15%, respectively, and at the same molar-matched doses, GSK256066 inhibited neutrophils by 50 ± 14% (43 μg/kg) and 42 ± 14% (4.3 μg/kg) respectively (Fig. 4B). The data suggest that the bronchoprotection and anti-inflammatory activity for GS-5759 effects are observed within the same dose range (7–70 μg/kg) but with the ED50 for anti-inflammatory activity lower than that for bronchodilation (Fig. 4C).
Figure 4.
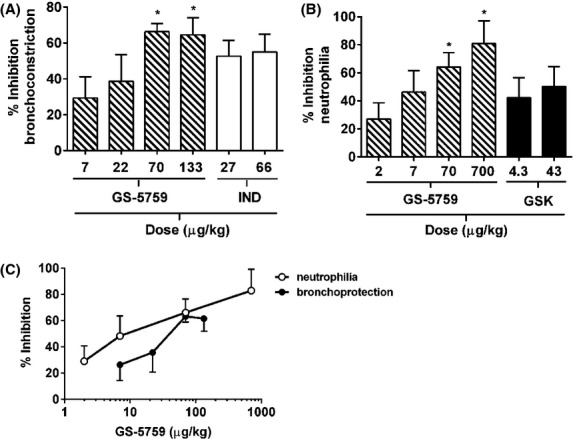
Dose-related inhibition of MCh-induced lung resistance and LPS-induced pulmonary neutrophilia by GS-5759 in cynomolgus monkeys. (A) Data represent the mean ± SEM of the percent maximum inhibition of MCh-induced lung resistance compared to vehicle treatment of the same animals 7 days previously. GS-5759 at 70 and 133 μg/kg is the molar equivalent of indacaterol at 27 and 66 μg/kg. (B) Data represent the mean ± SEM of the percent maximum inhibition of neutrophils in BAL fluid compared to vehicle-treated animals 24 h post-LPS aerosol exposure. GS-5759 at 7 and 70 μg/kg is the molar equivalent of GSK256066 at 4.3 and 43 μg/kg. n = 6 animals per group for both studies. IND, indacaterol; GSK, GSK256066. *P < 0.05 compared to vehicle-treated animals. (C) Comparison of the dose responses of GS-5759 demonstrating overlapping pharmacologies with respect to bronchoprotection and inhibition of pulmonary neutrophilia.
Effect of GS-5759 on bronchoconstriction and heart rate in guinea pigs
Dose–response curves for β2-adrenoceptor-induced bronchoprotection compared to β1-adrenoceptor-induced tachycardia were measured simultaneously in anaesthetized guinea pigs (pigs). Both GS-5759 and indacaterol demonstrated a dose-dependent inhibition of ACh-induced bronchoconstriction with ED50 values of 0.1 nmol/kg (0.088 μg/kg) and 0.35 nmol/kg (0.15 μg/kg) respectively (Fig. 5A). GS-5759 increased heart rate in a dose-dependent manner with a maximal increase of 9.8 ± 1.7% at 70 nmol/kg (62 μg/kg). In comparison indacaterol also increased heart rate dose-dependently with a maximal increase of 21.9 ± 2.4% at 23.3 nmol/kg (10 μg/kg) (Fig. 5B). A therapeutic index (T.I.) for both compounds could be determined by comparing the dose required to induce a 10% increase in heart rate to that which elicited 50% bronchoprotection. For GS-5759, a 10% increase in heart rate was achieved at a dose of 70 nmol/kg and the ED50 for bronchoprotection was 0.1 nmol/kg establishing a T.I. of 700. In comparison indacaterol had a T.I of 0.2 (0.07–0.35 nmol/kg).
Figure 5.
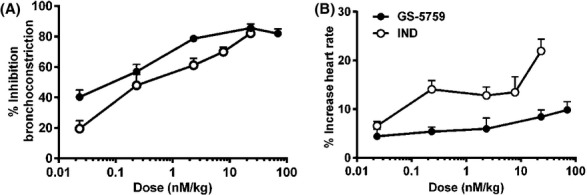
Dose-related effects of GS-5759 and indacaterol on ACh-induced bronchoconstriction and heart rate in anaesthetized Dunkin–Hartley guinea pigs. Guinea pigs were IT dosed with GS-5759 (0.02–62 μg/kg) or indacaterol (IND) (0.01–10 μg/kg) and heart rate was monitored throughout the experiment. Two hours after dosing, a second ACh challenge was performed and airway resistance measured compared to predosing measurements. Data represent the mean ± SEM of the percentage inhibition of bronchoconstriction as measured by RL (A) and percentage increase in heart rate (B) compared to each animals predosing level, n = 3–6 animals per dose group.
Effect of GS-5759 on pulmonary resistance and heart rate in beagle dogs
Dose–response effects on RW allergen-induced pulmonary resistance (β2-adrenoceptor-mediated) in sensitized dogs were compared to β1-adrenoceptor-induced tachycardia in separate groups of dogs. Both GS-5759 (1.4–18.2 μg/kg) and indacaterol (0.3–10.6 μg/kg) demonstrated a dose-related protection against antigen-induced pulmonary resistance with ED50 values of 3.4 μg/kg (3.5 nmol/kg) and 0.5 μg/kg (1.3 nmol/kg) respectively (Fig. 6A). In studies to evaluate the effects on heart rate and blood pressure, indacaterol caused a dose-related increase in heart rate in dogs, with a 10 μg/kg (26 nmol/kg) dose inducing a significant increase in heart rate compared to vehicle-treated dogs from 50 to 200 min post dosing and in mean blood pressure between 45 and 110 min. Dosing of GS-5759 (10, 50 and 103 μg/kg) did not induce a significant increase in heart rate or mean blood pressure at any dose compared to vehicle-treated dogs (Fig. 6B–C). Therapeutic indices could be established by comparing the dose that caused a significant increase in heart rate to the ED50 for bronchoprotection, these values were >31 (>107/3.4 nmol/kg) for GS-5759 and 20 (26/1.3 nmol/kg) for indacaterol.
Figure 6.
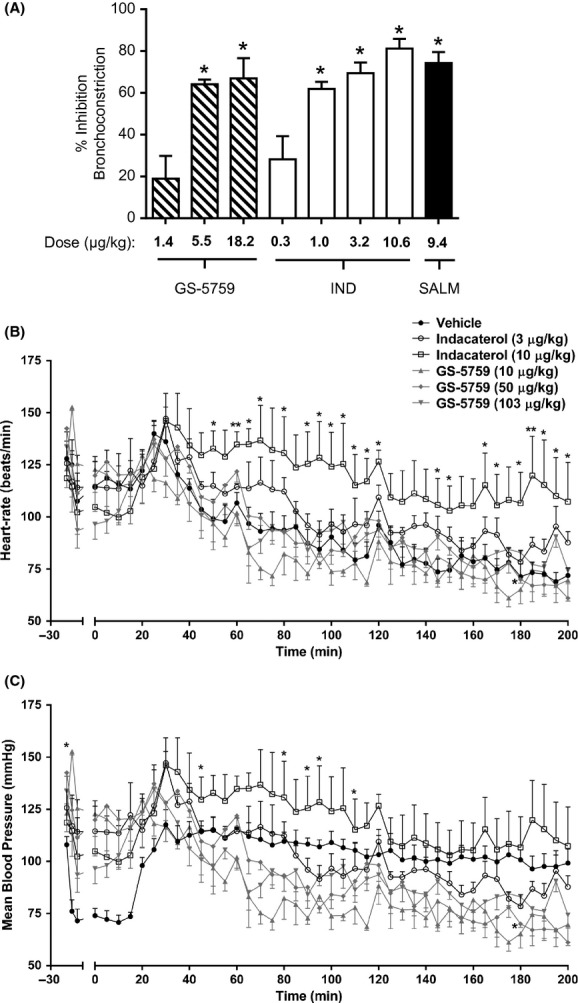
Dose-related effects on ragweed-induced pulmonary resistance and heart rate and blood pressure by GS-5759 and indacaterol in beagle dogs. (A) Data represent the mean ± SEM of the percent inhibition of ragweed antigen-induced bronchoconstriction in sensitized dogs compared to vehicle treatment of the same animals 7–14 days previously, n = 4 animals per group. GS-5759 at 18.2 μg/kg is the molar equivalent to indacaterol (IND) at 10.6 μg/kg and salmeterol (SALM) at 9.4 μg/kg. GS-5759 at 1.4 and 5.5 μg/kg is the molar equivalent to indacaterol at 1.0 and 3.2 μg/kg. (B, C) Data represent the mean ± SEM for heart beats per minute (B) and mean blood pressure (C) in beagle dogs following treatment with vehicle, GS-5759 or indacaterol (vehicle-treated dogs n = 8, GS-5759 or indacaterol-treated dogs n = 3–4), *P < 0.05, **P < 0.01 compared to vehicle treatment.
Emetic potential of GS-5759 in ferrets
Studies were conducted to evaluate the emetic potential of GS-5759 in ferrets, a documented side effect of PDE4 inhibitors both clinically and preclinically. Animals dosed with vehicle, either orally or IT, did not have emesis. GS-5759 (0.3–3.0 mg/kg) did not induce emesis at any dose tested, whereas roflumilast (0.1–10 mg/kg) caused a dose-dependent induction of emesis. The no effect dose of roflumilast for emesis was 0.1 mg/kg and the greatest response observed was at the maximum dose tested of 10 mg/kg with a total of 6.4 ± 1 vomits (P < 0.001) per ferret in 3 h (Fig. 7).
Figure 7.
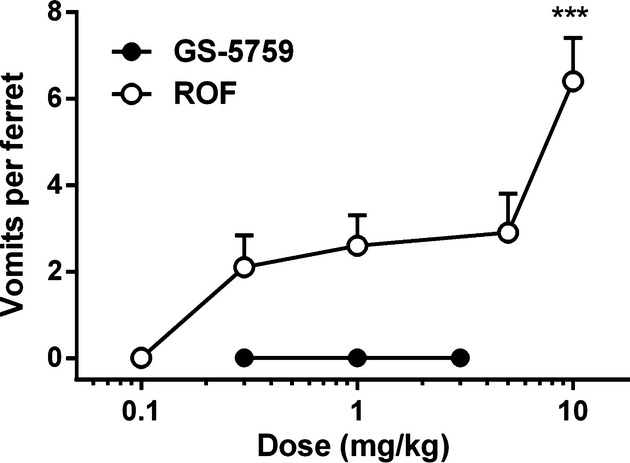
Dose-related effects of GS-5759 and roflumilast on emesis in conscious ferrets. Ferrets were dosed orally with roflumilast (ROF) or intratracheally with GS-5759, and were monitored for 3 h post dosing and the number of emetic events within that time counted. Data represent the mean ± SEM of the number of emetic events per animal following treatment (n = 4 animals per group), ***P < 0.001 compared to vehicle-treated animals.
Discussion
These studies characterize the in vivo pharmacology of GS-5759 as a bronchodilator and as an anti-inflammatory agent in preclinical animal species. GS-5759 demonstrated a dose-related bronchodilation in guinea pigs, dogs, and cynomolgus monkeys. In the guinea pig, the dose relationship was assessed in conscious animals using the enhanced pause (PenH), a methodology which has been debated in recent years as to its validity as an appropriate measurement for airway resistance (Lomask 2006). For this reason our studies also included experiments using direct measurement of airway resistance in anaesthetized guinea pigs, as well as the airway resistance studies in dogs and monkeys. GS-5759 also demonstrated dose-related anti-inflammatory activity in LPS-induced lung neutrophilia models in rats and cynomolgus monkeys, and inhibition of cigarette smoke-induced neutrophilia in mice.
In the rat LPS model of pulmonary neutrophilia GS-5759 appeared to be more potent than GSK256066, and this may have been due to the contribution of the β2-adrenoceptor agonist component of the molecule providing further anti-inflammatory activity, which appeared to be additive to the PDE4 inhibitory effect. Indacaterol alone demonstrated only modest anti-inflammatory effects in the model. Both GS-5759 and GSK256066 inhibited pulmonary neutrophilia to a similar level to that observed for the oral PDE4 inhibitor roflumilast. These data, along with the fact that at the highest doses of GS-5759 and roflumilast used in the studies showed significant inhibition of TNF-α, CCL2 and CCL3, suggests that similar levels of anti-inflammatory pulmonary efficacy can be achieved, whether dosed topically to the lungs or systemically by oral dosing in the LPS model.
GS-5759 also demonstrated anti-inflammatory activity in a cigarette smoke-induced model of pulmonary neutrophilia. As cigarette smoke exposure is a common risk factor for development of COPD, this challenge model may be relevant to the key pathways underlying the inflammatory processes relevant in the disease (Nikota and Stämpfli 2012). PDE4 inhibitors have previously been reported to be efficacious in acute models of cigarette smoke exposure in rodents. Cigarette smoke exposure of the C3H/HeN strain causes a robust inflammatory response to inhaled cigarette smoke exposure with lung cell increases relevant to human COPD (Xu et al. 2007, 2008). The model utilized in this study used a protocol of 14 exposure days of cigarette smoke in a total of 18 days, and such a model may be considered subchronic. Both GS-5759 and GSK256066 failed to inhibit neutrophilia at doses which were efficacious in the rat LPS-induced neutrophilia model, however, GS-5759 was efficacious at a higher dose. It remains, therefore, unclear whether higher doses of PDE4 inhibitor are required to elicit an effect in the model or whether there is something unique with the bifunctional nature of GS-5759. A combination of GSK256066 and indacaterol did not elicit an inhibitory response, although a dose match of GS-5759 was also not active. The more subchronic exposure protocol used in these studies may explain the ineffectiveness of PDE4 inhibition alone to demonstrate activity in the model compared to other more acute exposure models.
An important consideration during the preclinical development of GS-5759 was to have an appropriately balanced pharmacology at the two targets such that bronchodilatory and anti-inflammatory activity could be achieved within the same dose range. Experiments were designed to look at bronchodilator and anti-inflammatory activity in two separate models in the cynomolgus monkey, where a micronized dry powder formulation could be administered to the lungs using the same delivery methodology and over the same dose range. The results from these experiments indicated that GS-5759 was effective as both a bronchodilator following MCh challenge, and as an anti-inflammatory in an LPS-induced neutrophilia model. The maximal response of GS-5759 in both models appeared to plateau around the same dose, however, the ED50 for anti-inflammatory activity was lower than that for the bronchodilator effect. This suggests that maximum anti-inflammatory activity can be achieved within the dose–response window for bronchodilation and this may have important implications to the effectiveness of this compound, as it is likely that the clinical dose will be dictated by the bronchodilator dose response (Wang et al. 2012).
A further component of our studies was to evaluate the therapeutic margins of GS-5759 with respect to the known on-target biological side effects for long-acting β2-adrenoceptor agonist (LABAs) and PDE4 inhibitors, namely tachycardia and nausea/emesis respectively. We utilized several preclinical models to address this issue. For the β2-adrenoceptor agonist component, anaesthetized guinea pigs were used and simultaneous bronchodilation and heart rate monitoring was performed. GS-5759 and indacaterol had similar molar-matched dose-related effects on bronchodilation, but significantly higher doses of GS-5759 were required to increase heart rate compared to indacaterol, resulting in a higher T.I. for GS-5759. Similar experiments were performed in beagle dogs dosing the compounds as topically delivered micronized dry powders. Both compounds had comparable molar-matched dose responses for bronchodilation, but GS-5759 had a superior window for effects on heart rate and blood pressure at doses up to 25-fold above the dose required to elicit a 50% maximal bronchodilation. Indacaterol did elicit a significant and sustained tachycardia at a dose 20-fold above the dose which elicited 50% bronchodilation. These data, from both the guinea pig and dog models, indicate that GS-5759 has a therapeutic window no worse, and probably superior to, that of indacaterol. GS-5759 has a similar affinity for human β1-adrenoceptor compared to indacaterol as determined in functional cellular assays with receptors expressed in 293 cells (Tannheimer et al. 2014). A likely explanation for this is the molecular size and physical-chemical properties of GS-5759, which may lead to long tissue retention times and slow transit from the lungs into the systemic circulation. Additionally, GS-5759 has high plasma protein binding and fast clearance in pre-clinical species (data not shown), and these characteristics may also contribute to very low free fraction of compound being available systemically to induce cardiac side effects.
To look at the PDE4 inhibitor-specific side effects, we utilized a model of emesis in the ferret which has been established as an appropriate model to evaluate the emetic potential of PDE4 inhibitor (Kobayashi et al. 2011; Nials et al. 2011). The oral PDE4 inhibitor roflumilast was used as a positive control, which demonstrated a dose-related increase in emesis similar to previous literature reports (Davis et al. 2009). The dose responses for emesis and efficacy in the rat LPS model overlapped, supporting what has been reported clinically for roflumilast as having a very narrow therapeutic window (Giembycz 2008). GS-5759 did not induce emesis at any dose tested suggesting it also has a wide therapeutic window, presumably achieved by its high lung to systemic exposures following topical dosing.
These studies have described the pharmacology of GS-5759, a bifunctional molecule with both β2-adrenoceptor agonist and PDE4 inhibitor activity, which has been optimized for topical lung delivery. These mechanisms both act via modulation and elevation of cAMP levels, with the potential to act in concert for additive or synergistic activity. The rat LPS studies suggest that GS-5759 has additive anti-inflammatory activity. The PDE4 inhibitor roflumilast is used clinically in COPD but is dose limited due to side effects and may not achieve the maximum potential efficacy for this mechanism in the lungs (Giembycz and Newton 2011). Delivery of a PDE4 inhibitor by inhalation may increase the therapeutic margin and efficacy, but to date an inhaled PDE4 inhibitor has not proceeded to registration trials. The inhaled PDE4 inhibitor UK-500,001 did complete a phase II proof of concept trial in COPD but did not meet its primary forced expiratory volume in 1 sec (FEV1) end-point (Vestbo et al. 2009). The reason for this failure is not clear, but the combination of a β2-adrenoceptor agonist and PDE4 inhibitor that both elevate cellular cAMP levels and prevent its breakdown has the potential to provide an alternative, and potentially superior, way to target this mechanism over PDE4 inhibition alone. The opportunity to have both a bronchodilator agent and an anti-inflammatory agent within a single molecule delivered by a simple inhalation device is attractive for the treatment of COPD, particularly as GS-5759 is targeting two precedented clinical mechanisms. There would also be the opportunity for combining GS-5759 with an anticholinergic or glucocorticosteroid to target three precedented mechanisms in COPD, delivered by a single inhalation device.
Acknowledgments
We thank Mark A. Giembycz and Robert Newton from the University of Calgary who provided critical discussions around the interpretation of the data described.
Glossary
- ACh
acetylcholine
- ANOVA
analysis of variance
- AUC
area under the curve
- BAL
bronchoalveolar lavage
- CCL2
chemokine (C C motif) ligand 2
- CCL3
chemokine (C C motif) ligand 3
- COPD
chronic obstructive pulmonary disease
- FEV1
forced expiratory volume in 1 sec
- GOLD
global initiative for chronic obstructive lung disease
- GS-5759
(R)-6-[[3-[[4-[5-[[2-Hydroxy-2-(8-hydroxy-2-oxo-1,2-dihydroquinolin-5-yl)ethyl]amino]pent-1-ynyl]phenyl]carbamoyl]phenyl]sulfonyl]-4-[(3-methoxyphenyl)amino]-8-methylquinoline-3-carboxamide
- GSK256066
6-(3-(dimethylcarbamoyl)phenylsulfonyl)-4-(3-methoxyphenylamino)-8-methylquinoline-3-carboxamide
- IL-1α
interleukin-1α
- IT
intratracheally
- LABA
long-acting β2-adrenoceptor agonist
- LPS
lipopolysaccharide
- LRRI
Lovelace Respiratory Research Institute
- MCh
methylcholine
- PDE4
phosphodiesterase 4
- RW
ragweed
- T.I.
therapeutic index
- TNF-α
tumour necrosis factor-α
Disclosure
None declared.
References
- Barrett EG, Rudolph K, Bowen LE, Muggenburg BA, Bice DE. Effect of inhaled ultrafine carbon particles on the allergic airway response in ragweed-sensitized dogs. Inhalation Toxicol. 2003;15:151–165. doi: 10.1080/08958370304474. [DOI] [PubMed] [Google Scholar]
- Cazzola M, Page CP, Calzetta L, Matera MG. Pharmacology and therapeutics of bronchodilators. Pharmacol Rev. 2012a;64:450–504. doi: 10.1124/pr.111.004580. [DOI] [PubMed] [Google Scholar]
- Cazzola M, Rogliani P, Segreti A, Matera MG. An update on bronchodilators in Phase I and II clinical trials. Expert Opin Investig Drugs. 2012b;21:1489–14501. doi: 10.1517/13543784.2012.710602. [DOI] [PubMed] [Google Scholar]
- Davis T, Peterson JJ, Kou JP, Capper-Spudich EA, Ball D, Nials AT, et al. The identification of a novel phosphodiesterase 4 inhibitor, 1-ethyl-5-{5-[(4-methyl-1-piperazinyl)methyl]-1,3,4-oxadiazol-2-yl}-N-(tetrahydro-2H-pyran-4-yl)-1H-pyrazolo[3,4-b]pyridin-4-amine (EPPA-1), with improved therapeutic index using pica feeding in rats as a measure of emetogenicity. J Pharmacol Exp Ther. 2009;330:922–931. doi: 10.1124/jpet.109.152454. [DOI] [PubMed] [Google Scholar]
- Giembycz MA. Can the anti-inflammatory potential of PDE4 inhibitors be realized: guarded optimism or wishful thinking? Br J Pharmacol. 2008;155:288–290. doi: 10.1038/bjp.2008.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giembycz MA, Newton R. Harnessing the clinical efficacy of phosphodiesterase 4 inhibitors in inflammatory lung diseases: dual-selective phosphodiesterase inhibitors and novel combination therapies. Handb Exp Pharmacol. 2011:415–446. doi: 10.1007/978-3-642-17969-3_18. [DOI] [PubMed] [Google Scholar]
- Kobayashi M, Kubo S, Iwata M, Ohtsu Y, Takahashi K, Shimizu Y. ASP3258, an orally active potent phosphodiesterase 4 inhibitor with low emetic activity. Int Immunopharmacol. 2011;11:732–739. doi: 10.1016/j.intimp.2011.01.023. [DOI] [PubMed] [Google Scholar]
- Lomask M. Further exploration of the Penh parameter. Exp Toxicol Pathol. 2006;57(Suppl. 2):13–20. doi: 10.1016/j.etp.2006.02.014. [DOI] [PubMed] [Google Scholar]
- Matera MG, Page CP, Cazzola M. Novel bronchodilators for the treatment of chronic obstructive pulmonary disease. Trends Pharmacol Sci. 2011;32:495–506. doi: 10.1016/j.tips.2011.04.003. [DOI] [PubMed] [Google Scholar]
- Moodley T, Wilson SM, Joshi T, Rider CF, Sharma P, Yan D, et al. Phosphodiesterase 4 inhibitors augment the ability of formoterol to enhance glucocorticoid-dependent gene transcription in human airway epithelial cells: a novel mechanism for the clinical efficacy of roflumilast in severe chronic obstructive pulmonary disease. Mol Pharmacol. 2013;83:894–906. doi: 10.1124/mol.112.083493. [DOI] [PubMed] [Google Scholar]
- Nials AT, Tralau-Stewart CJ, Gascoigne MH, Ball DI, Ranshaw LE, Knowles RG. In vivo characterization of GSK256066, a high-affinity inhaled phosphodiesterase 4 inhibitor. J Pharmacol Exp Ther. 2011;337:137–144. doi: 10.1124/jpet.110.173641. [DOI] [PubMed] [Google Scholar]
- Nikota JK, Stämpfli MR. Cigarette smoke-induced inflammation and respiratory host defense: insights from animal models. Pulm Pharmacol Ther. 2012;25:257–262. doi: 10.1016/j.pupt.2012.05.005. [DOI] [PubMed] [Google Scholar]
- Phillips G, Salmon M. Bifunctional compounds for the treatment of COPD. Annu Rep Med Chem. 2012;47:209–221. [Google Scholar]
- Redman TK, Rudolph K, Barr EB, Bowen LE, Muggenburg BA, Bice DE. Pulmonary immunity to ragweed in a Beagle dog model of allergic asthma. Exp Lung Res. 2001;27:433–451. doi: 10.1080/019021401300317143. [DOI] [PubMed] [Google Scholar]
- Robinson C, Zhang J, Garrod DR, Newton GK, Jenkins K, Perrior TR. Future inhaled drugs by virtual innovation: allergen delivery inhibitors. Future Med Chem. 2011;3:1567–1570. doi: 10.4155/fmc.11.107. [DOI] [PubMed] [Google Scholar]
- Rossi A, Polese G. Indacaterol: a comprehensive review. Int J Chronic Obstruct Pulmon Dis. 2013;8:353–363. doi: 10.2147/COPD.S21625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santulli G, Iaccarino G. Pinpointing beta adrenergic receptor in ageing pathophysiology: victim or executioner? Evidence from crime scenes. Immun Ageing. 2013;10:10. doi: 10.1186/1742-4933-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santulli G, Lombardi A, Sorriento D, Anastasio A, Del Giudice C, Formisano P, et al. Age-related impairment in insulin release: the essential role of beta(2)-adrenergic receptor. Diabetes. 2012;61:692–701. doi: 10.2337/db11-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seldon PM, Meja KK, Giembycz MA. Rolipram, salbutamol and prostaglandin E2 suppress TNFalpha release from human monocytes by activating Type II cAMP-dependent protein kinase. Pulm Pharmacol Ther. 2005;18:277–284. doi: 10.1016/j.pupt.2004.12.012. [DOI] [PubMed] [Google Scholar]
- Singh D, Petavy F, Macdonald AJ, Lazaar AL, O’Connor BJ. The inhaled phosphodiesterase 4 inhibitor GSK256066 reduces allergen challenge responses in asthma. Respir Res. 2010;11:26. doi: 10.1186/1465-9921-11-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spina D. PDE4 inhibitors: current status. Br J Pharmacol. 2008;155:308–315. doi: 10.1038/bjp.2008.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tannheimer SL, Sorensen EA, Haran AC, Mansfield CN, Wright CD, Salmon M. Additive anti-inflammatory effects of beta 2 adrenoceptor agonists or glucocorticosteroid with roflumilast in human peripheral blood mononuclear cells. Pulm Pharmacol Ther. 2012a;25:178–184. doi: 10.1016/j.pupt.2012.01.003. [DOI] [PubMed] [Google Scholar]
- Tannheimer SL, Wright CD, Salmon M. Combination of roflumilast with a beta-2 adrenergic receptor agonist inhibits proinflammatory and profibrotic mediator release from human lung fibroblasts. Respir Res. 2012b;13:28. doi: 10.1186/1465-9921-13-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tannheimer SL, Sorensen EA, Cui Z-H, Kim M, Patel L, Baker WR, et al. The in vitro pharmacology of GS-5759, a novel bifunctional phosphodiesterase 4 inhibitor and long acting β2-adrenoceptor agonist. J Pharmacol Exp Ther. 2014;349:1–9. doi: 10.1124/jpet.113.210997. [DOI] [PubMed] [Google Scholar]
- Vestbo J, Tan L, Atkinson G, Ward J. A controlled trial of 6-weeks’ treatment with a novel inhaled phosphodiesterase type-4 inhibitor in COPD. Eur Respir J. 2009;33:1039–1044. doi: 10.1183/09031936.00068908. [DOI] [PubMed] [Google Scholar]
- Wang Y, Lee JY, Michele T, Chowdhury BA, Gobburu JV. Limitations of model based dose selection for indacaterol in patients with chronic obstructive pulmonary disease. Int J Clin Pharmacol Ther. 2012;50:622–630. doi: 10.5414/CP201758. [DOI] [PubMed] [Google Scholar]
- Xu J, Xu F, Wang R, Seagrave J, Lin Y, March TH. Cigarette smoke-induced hypercapnic emphysema in C3H mice is associated with increases of macrophage metalloelastase and substance P in the lungs. Exp Lung Res. 2007;33:197–215. doi: 10.1080/01902140701459514. [DOI] [PubMed] [Google Scholar]
- Xu J, Xu F, Barrett E. Metalloelastase in lungs and alveolar macrophages is modulated by extracellular substance P in mice. Am J Physiol Lung Cell Mol Physiol. 2008;295:L162–L170. doi: 10.1152/ajplung.00282.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]


