Supplemental digital content is available in the text.
Key Words: SEDENTARY, PHYSICAL ACTIVITY, ACCELEROMETRY, BIOMARKERS, CARDIOMETABOLIC
ABSTRACT
Purpose
The detrimental effects of sedentary time on health may act by replacing time spent in physical activities. The aim of this study was to examine cross-sectional associations between objectively assessed sedentary and physical activity domains and cardiometabolic risk factors using a novel isotemporal substitution paradigm.
Methods
Participants were 445 healthy men and women (mean age, 66 ± 6 yr), without history or objective signs of cardiovascular disease, drawn from the Whitehall II epidemiological cohort. Physical activity was objectively measured using accelerometers (ActiGraph GT3X) worn around the waist during waking hours for 4–7 consecutive days. We examined the effects of replacing sedentary time with light activity or moderate-to-vigorous physical activity (MVPA) on a range of risk factors (HDL cholesterol, triglycerides, HbA1c, and body mass index) using an isotemporal substitution paradigm.
Results
In partition models, where the time in each of the intensity categories was held constant, only MVPA remained associated with risk factors. In isotemporal substitution models that held total (wear) time constant, replacing 10-min sedentary time with an equal amount of MVPA was associated with favorable effects in all risk factors, including HbA1c (B = −0.023; 95% confidence interval (CI), −0.043 to −0.002), BMI (B = −0.39; 95% CI, −0.54 to −0.24), HDL cholesterol (B = 0.037; 95% CI, 0.021–0.054), and triglycerides (B = −0.035; 95% CI, −0.061 to −0.009).
Conclusions
The associations between sedentary behavior and cardiometabolic risk may be dependent on the types of activities that are displaced by sedentary time.
Sedentary behavior, when self-reported, has been consistently associated with risk of cardiovascular disease (CVD) in population cohort studies (6,8,21,27). In general population studies, there is some cross-sectional evidence to suggest detrimental linear associations between objectively assessed sedentary time and various cardiometabolic risk factors (7,15–18), although the literature remains equivocal (11,23,25,28). The discrepancy in findings is possibly due to the use of different motion sensors that use various methods to define sedentary activity and also varying statistical approaches to analyze data. For example, various studies have considered sedentary bouts and breaks from sitting as predictors of metabolic health (1,7,26) whereas others have considered total sedentary time as a continuous variable (7,11,15–18,23,25,28). The detrimental effects of sedentary time may act by replacing time spent in physical activities, although few studies have explored this hypothesis. Further work is therefore required in the field of sedentary behavior to better understand time reallocation of different activities. Understanding time reallocation effects is crucial to better inform interventions that aim to reduce sedentary behaviors. Given the barriers to physical activity, it would be desirable if individuals could gain benefits from incorporating relatively light levels of activity into their lifestyles, which might be accomplished by simply displacing sedentary time with movement.
Recently, the isotemporal substitution model, which was originally developed from nutritional epidemiology, has been applied to physical activity research (24). This paradigm is designed to simultaneously model the specific activity being performed and the specific activity being displaced in an equal time exchange fashion. The technique is particularly suited to data collected objectively from movement sensors because these devices capture all activities over a finite period of wear and their output can cover the entire intensity spectrum of physical activity.
We have previously reported associations between objectively assessed sedentary time and body mass index (BMI) (12), although these associations were not independent of moderate-to-vigorous physical activity (MVPA). Thus, the aim of this study was to use the isotemporal substitution method to explore associations with a wider range of cardiometabolic risk markers when replacing sedentary time with light activity or MVPA in a sample of older adults.
RESEARCH DESIGN AND METHODS
Participants.
A sample of participants was drawn from the Whitehall II epidemiological cohort, as previously described (12), to conduct a cross-sectional study. The criteria for entry into the study included no history or objective signs of CHD and no previous diagnosis or treatment for hypertension, inflammatory diseases, or allergies. This information was confirmed by a telephone interview and verified from clinical data collected from the previous seven phases of the main Whitehall II study. Volunteers were of white European origin, age 56–79 yr. Selection was stratified by grade of employment (current or most recent) to include participants from higher and lower socioeconomic status. Participants were prohibited from using any antihistamine or anti-inflammatory medication 7 d before testing and were rescheduled if they reported colds or other infections on the day of testing. Participants gave a full informed consent to participate in the study, and ethical approval was obtained from the University College London Hospitals committee on the ethics of human research.
Physical activity assessment.
Participants wore an accelerometer (ActiGraph GT3X; ActiGraph Corp., Pensacola, FL) mounted at the hip, which records movement on the vertical and horizontal axes, during waking hours for seven consecutive days. Participants removed the device for sleeping and water-based activities. The accelerometer provides a measure of the frequency, intensity, and duration of physical activity and allows classification of activity levels as sedentary, light, moderate, and vigorous. The raw accelerometry data were processed using a specialist software (MAHUffe, Cambridge, United Kingdom) to produce a series of standardized variables. All participants included in the present analysis recorded a minimum wear time of 10 h·d−1 for 4–7 d (62 participants (18% of sample) wore the ActiGraph for 4–6 d, and the remainder, for the full 7 d). The first and last days of data were excluded from the analysis, and nonwear time was defined as intervals of at least 60 consecutive minutes of 0 cpm. We used cutoff points previously used in studies among older adults (14) to calculate daily times in each activity intensity band, as follows: sedentary (<1.5 METs), 0–199 cpm; light (1.5–3 METs), 200–1998 cpm; MVPA (>3 METs), ≥1999 cpm. All physical activity variables were converted to time (min) per valid day.
Clinical variables.
Participants attended a clinic visit before being fitted with an ActiGraph. Height and weight were recorded in light clothing for the calculation of BMI. Fasting blood samples were taken for analysis of total and HDL cholesterol (HDL-C) and triglycerides, which were measured within 72 h in a serum stored at 4°C using enzymatic calorimetric methods. Glucose homeostasis was assessed from glycated hemoglobin (HbA1c) concentration assayed using boronate affinity chromatography, a combination of boronate affinity and liquid chromatography.
Covariates.
Participants reported current smoking levels and statin use, and civil service work grade was recorded as a marker of socioeconomic status.
Statistical analysis.
All analyses were cross-sectional. Linear regression was used to examine associations between 10-min time units of sedentary activity, light activity, and MVPA and metabolic risk factors. We chose to use 10-min blocks because this is the minimum bout of time in which activities should be accrued to meet the current physical activity guidelines. Models were adjusted for age, sex, smoking, statin use, and employment grade. We ran three types of models. 1) The first are single-factor models that represent the association of each intensity category (sedentary and light activity and MVPA) with cardiometabolic risk factors without mutual adjustment for other categories of activity. 2) Partition models represent the estimated effects of time spent in each intensity category, holding the time in each of the other categories constant but without holding total time constant. Thus, all activity categories were entered simultaneously into the model without adjustment for total wear time. 3) Coefficients for the isotemporal substitution models represent the estimated effects of substituting a specified intensity category for the category dropped while holding total (wear) time constant. Thus, in isotemporal substitution models that examined the effect of replacing sedentary time with MVPA, the model included light activity, MVPA, total wear time, and other covariates whereas a model examining the effect of replacing MVPA with sedentary time included sedentary time, light activity, total wear time, and other covariates. These methods are described in detail elsewhere (2,24). Isotemporal substitution models assume linear relations between dependent and independent variables that were established before running any models. All analyses were conducted using SPSS version 21.
RESULTS
The analyses contained 445 participants (female, 49.6%; mean age, 66 ± 6 yr; range, 57–79 yr). The characteristics of the sample have been described elsewhere (12). Overall, the sample was in good health, with normal levels of HDL-C (1.73 ± 0.49 mmol·L−1), triglycerides (1.38 ± 0.70 mmol·L−1), glycated hemoglobin (5.70% ± 0.54%), and BMI (25.9 ± 4.1 kg·m−2). Only 5.4% were current smokers, and 22.0% was medicated with statins. Participants wore the ActiGraph for 889 ± 68 min·d−1 on average, and 72.3%, 23.5%, and 4.2% of wear time were spent in sedentary and light activity and MVPA categories, respectively. There were low-to-moderate correlations between the different activity categories (see Table, Supplemental Digital Content 1, http://links.lww.com/MSS/A383, Pearson correlations between different activity categories).
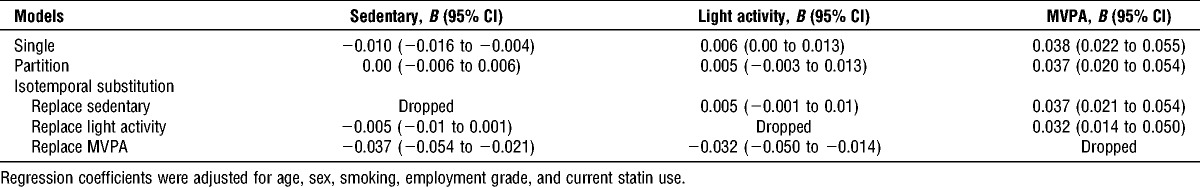
Tables 1–4 present coefficients for the various models. In single models, sedentary activity was adversely associated with BMI and HDL-C; light activity was favorably associated with HDL-C; whereas MVPA was favorably associated with all risk factors. In the partition models, where the time in each of the intensity categories was held constant, only MVPA remained favorably associated with all cardiometabolic risk factors. Lastly, in isotemporal substitution models that held total time constant, replacing sedentary time with MVPA was associated with favorable effects in all metabolic risk factors, including HbA1c (B = −0.023; 95% confidence interval (CI), −0.043 to −0.002), BMI (B = −0.39; 95% CI, −0.54 to −0.24), HDL-C (B = 0.037; 95% CI, 0.021–0.054), and triglycerides (B = −0.035; 95% CI, −0.061 to −0.009). Replacing light activity with MVPA was also associated with favorable effects in all metabolic risk factors, including HbA1c (B = −0.024; 95% CI, −0.047 to −0.001), BMI (B = −0.39; 95% CI, −0.55 to −0.22), HDL-C (B = 0.032; 95% CI, 0.014–0.050), and triglycerides (B = −0.031; 95% CI, −0.060 to −0.002).
TABLE 1.
Single, partition, and isotemporal substitution models examining the relation between 10-min changes in time spent in sedentary, light, and moderate- to vigorous-intensity activity and glycated hemoglobin (n = 445).
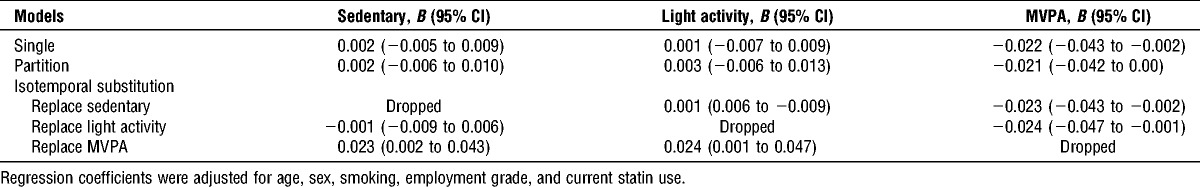
TABLE 4.
Single, partition, and isotemporal substitution models examining the relation between 10-min changes in time spent in sedentary, light, and moderate- to vigorous-intensity activity and triglycerides (n = 445).
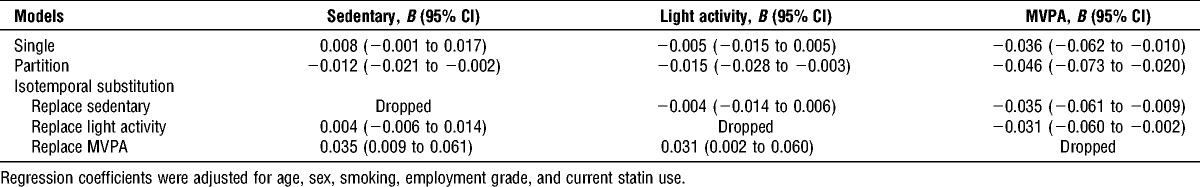
TABLE 2.
Single, partition, and isotemporal substitution models examining the relation between 10-min changes in time spent in sedentary, light, and moderate- to vigorous-intensity activity and BMI (n = 445).
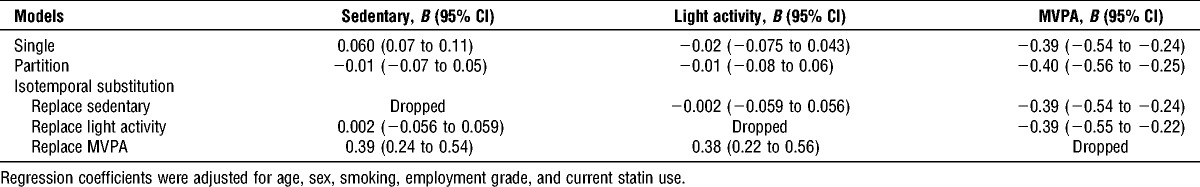
TABLE 3.
Single, partition, and isotemporal substitution models examining the relation between 10-min changes in time spent in sedentary, light, and moderate- to vigorous-intensity activity and HDL-C (n = 445).
DISCUSSION
The evidence linking sedentary behavior with CVD remains equivocal, which might be explained by numerous factors. The first is the use of different motion sensors that use different methods to define sedentary activity and introduce various degrees of measurement error. Second, various statistical approaches have been used to analyze the data and few have considered time reallocation effects. We have previously shown that objectively assessed sedentary time was not associated with a range of risk factors after adjusting for MVPA (12,28), although the present findings suggest that the association of sedentary and active time with cardiometabolic risk can be better conceptualized by using the isotemporal substitution model. The substitution model controls for the confounding effect of total discretionary time (wear time), so that the observed associations between different activities and metabolic risk factors are independent of one another and also of total discretionary time.
Our results demonstrate that replacing sedentary time with an equal amount of MVPA was associated with a more favorable cardiometabolic profile. The conceptualization of sedentary behavior as an “independent” risk factor for cardiometabolic outcomes has been questioned because limited plausible biological mechanisms have been identified to date (20). Most epidemiological data (5,6,21,27) demonstrate that MVPA modifies the association between sedentary behavior and CVD, albeit they are deemed statistically independent of one another. That is, the absolute risk of CVD is lower in physically active participants that record high amounts of sedentary time compared with that in their inactive counterparts. Thus, the effects of sedentary behavior may be largely driven through displacing time in other activities that require movement.
Some studies have demonstrated associations between light-intensity activity and metabolic risk factors (3,4,13,18), which has generated the hypothesis that short breaks in sedentary time may have beneficial effects. Nevertheless, associations between interruptions of sedentary time and metabolic outcomes seem to be substantially weaker than those with sedentary time (7). We did not demonstrate beneficial effects of replacing sedentary time with light-intensity activity, nor was there any substantial evidence to suggest any effects of light activity in single models. In contrast, replacing sedentary time of 30 min·d−1 with equal amounts of light physical activity was associated with better physical health in a sample of older adults (3). Some recent experimental work has also suggested that replacing sitting with periods of light activity and standing has favorable effects on glucose and insulin sensitivity (9,10). Taken together, these discrepancies might be partly explained by the fact that our sample contained healthy participants with low-risk factors and no history of major diseases. Thus, the effects of breaking up sedentary time with light activity may be more beneficial among inactive samples with substantial disease burden.
Methodological limitations of differentiating between sitting, standing, and light activity may also be relevant. For example, the ActiGraph used in this study quantifies time spent in different intensities of activity by summing time above and below specified count thresholds. This method works reasonably well for identifying moderate-to-vigorous levels of activity but is less accurate for distinguishing sedentary and light activities (19), which might have partly explained why we observed limited effects of substituting sedentary time for light activity. Indeed, among older adults, there may be propensity for greater time in the lower end of the light intensity spectrum (<1000 cpm) but time in the upper band (1000–1999 cpm) may have important health benefits that are masked. Nevertheless, some evidence exist suggesting that activity >1000 cpm may indeed be above 3 METs for some individuals (22); thus, using a cutoff of 2000 cpm would in fact have produced a conservative estimate for moderate-intensity activity in the present study. Methods that use postural allocation may be more reliable to distinguish sitting from standing and other forms of lighter activity from higher ends of the intensity spectrum. Participants removed the device for sleeping and water-based activities; thus, we cannot account for the effects of activities undertaken during nonwear time. Nevertheless, a recent study using the isotemporal substitution model demonstrated that the effects of substituting sedentary time with MVPA on metabolic risk markers were similar across different sleep duration categories (2). The cross-sectional design of our study limits the ability to make causal inferences, and reallocation of time does not reflect a true temporal substitution.
In summary, our results demonstrate that replacing sedentary time with an equal amount of MVPA was associated with a more favorable cardiometabolic risk profile. The association of sedentary behavior with health outcomes may be dependent on the types of activities that are displaced by sedentary time. Thus, interventions that are designed to reduce sedentary behavior should be mindful of the types of activities that one might use to substitute sitting time with.
Supplementary Material
Acknowledgments
This study was funded by the British Heart Foundation (RE/10/005/28296). The funding agency had no role in the study design, collection, analysis and interpretation of data, writing of the report, or in the decision to submit the article for publication.
The authors’ contributions were as follows: M. H. had full access to the data and takes responsibility for the integrity and accuracy of the results. All authors contributed to the concept and design of study, drafting, and critical revision of the manuscript. All authors have approved the final version to be published.
None of the authors report any conflict of interest.
The results of the present study do not constitute endorsement by the American College of Sports Medicine.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.acsm-msse.org).
REFERENCES
- 1. Bankoski A, Harris TB, McClain JJ, et al. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care. 2011; 34 (2): 497– 503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Buman MP, Winkler EA, Kurka JM, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2014; 179; 323– 34 [DOI] [PubMed] [Google Scholar]
- 3. Buman MP, Hekler EB, Haskell WL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010; 172: 1155– 65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Camhi SM, Sisson SB, Johnson WD, Katzmarzyk PT, Tudor-Locke C. Accelerometer-determined moderate intensity lifestyle activity and cardiometabolic health. Prev Med. 2011; 52: 358– 60 [DOI] [PubMed] [Google Scholar]
- 5. Chau JY, Grunseit AC, Chey T, et al. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One. 2013; 8 (11): e80000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chomistek AK, Manson JE, Stefanick ML, et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: results from the Women’s Health Initiative. J Am Coll Cardiol. 2013; 61 (23): 2346– 54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cooper AR, Sebire S, Montgomery AA, et al. Sedentary time, breaks in sedentary time and metabolic variables in people with newly diagnosed type 2 diabetes. Diabetologia. 2012; 55: 589– 99 [DOI] [PubMed] [Google Scholar]
- 8. Dunstan DW, Barr EL, Healy GN, et al. Television viewing time and mortality: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Circulation. 2010; 121 (3): 384– 91 [DOI] [PubMed] [Google Scholar]
- 9. Dunstan DW, Kingwell BA, Larsen R, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012; 35: 976– 83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Duvivier BM, Schaper NC, Bremers MA, et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS One. 2013; 8: e55542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ekelund U, Brage S, Griffin SJ, Wareham NJ; ProActive UK Research Group. Objectively measured moderate- and vigorous-intensity physical activity but not sedentary time predicts insulin resistance in high-risk individuals. Diabetes Care. 2009; 32: 1081– 6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hamer M, Venuraju SM, Urbanova L, Lahiri A, Steptoe A. Physical activity, sedentary time, and pericardial fat in healthy older adults. Obesity (Silver Spring). 2012; 20: 2113– 7 [DOI] [PubMed] [Google Scholar]
- 13. Hamer M, Bostock S, Hackett R, Steptoe A. Objectively assessed sedentary time and type 2 diabetes mellitus: a case-control study. Diabetologia. 2013; 56: 2761– 2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Harris TJ, Owen CG, Victor CR, Adams R, Cook DG. What factors are associated with physical activity in older people, assessed objectively by accelerometry? Br J Sports Med. 2009; 43: 442– 50 [DOI] [PubMed] [Google Scholar]
- 15. Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2009; 31: 369– 71 [DOI] [PubMed] [Google Scholar]
- 16. Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011; 32: 590– 7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Henson J, Yates T, Biddle SJ, et al. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013; 56: 1012– 20 [DOI] [PubMed] [Google Scholar]
- 18. Kim J, Tanabe K, Yokoyama N, Zempo H, Kuno S. Objectively measured light-intensity lifestyle activity and sedentary time are independently associated with metabolic syndrome: a cross-sectional study of Japanese adults. Int J Behav Nutr Phys Act. 2013; 10: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc. 2011; 43 (8): 1561– 7 [DOI] [PubMed] [Google Scholar]
- 20. Latouche C, Jowett JB, Carey AL, et al. Effects of breaking up prolonged sitting on skeletal muscle gene expression. J Appl Physiol (1985). 2013; 114: 453– 60 [DOI] [PubMed] [Google Scholar]
- 21. Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012; 95 (2): 437– 45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Matthews CE, Keadle SK, Sampson J, et al. Validation of a previous-day recall measure of active and sedentary behaviors. Med Sci Sports Exerc. 2013; 45 (8): 1629– 38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McGuire KA, Ross R. Sedentary behavior is not associated with cardiometabolic risk in adults with abdominal obesity. PLoS One. 2011; 6: e20503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009; 170: 519– 27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scheers T, Philippaerts R, Lefevre J. SenseWear-determined physical activity and sedentary behavior and metabolic syndrome. Med Sci Sports Exerc. 2013; 45 (3): 481– 9 [DOI] [PubMed] [Google Scholar]
- 26. Shiroma EJ, Freedson PS, Trost SG, Lee IM. Patterns of accelerometer-assessed sedentary behavior in older women. JAMA. 2013; 310 (23): 2562– 3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Stamatakis E, Hamer M, Dunstan DW. Screen-based entertainment time, all-cause mortality, and cardiovascular events: population-based study with ongoing mortality and hospital events follow-up. J Am Coll Cardiol. 2011; 57 (3): 292– 9 [DOI] [PubMed] [Google Scholar]
- 28. Stamatakis E, Davis M, Stathi A, Hamer M. Associations between multiple indicators of objectively-measured and self-reported sedentary behaviour and cardiometabolic risk in older adults. Prev Med. 2012; 54: 82– 7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


