Supplemental digital content is available in the text.
Key Words: age-related macular degeneration, early age-related macular degeneration, drusen, pigmentary abnormalities, polypoidal choroidal vasculopathy, Asian
ABSTRACT
Purpose
To investigate the relationship between the early signs of age-related macular degeneration (AMD) and the risk of developing exudative AMD (typical AMD or polypoidal choroidal vasculopathy [PCV]) in the fellow eye of Japanese patients with unilateral exudative AMD, focusing particularly on eyes with only pigmentary abnormality.
Methods
This study is a retrospective observational consecutive case series. We retrospectively reviewed the medical charts of patients who revisited the AMD clinic from 2010 to 2011 and confirmed 129 cases with unilateral exudative AMD at their first visit (baseline). The non-affected eyes at baseline (the second eye) were categorized by the presence of early signs of AMD. The incidence of exudative AMD (typical AMD or PCV) in the fellow eye was confirmed by fluorescein and indocyanine green angiography.
Results
Of the 129 patients, 14 (10.9%) developed exudative AMD in the fellow eye (median follow-up, 3.2 years; n = 7 typical AMD and n = 7 PCV). Eyes with both pigmentary abnormalities and large drusen were more likely to develop typical AMD (age- and sex-adjusted odds ratio = 9.46, 95% confidence interval = 1.05 to 85.0), whereas pigmentary abnormalities without large drusen were associated with PCV (age- and sex-adjusted odds ratio = 15.9, 95% confidence interval = 1.8 to 140.5).
Conclusions
There was a difference in the association between early signs of AMD and incident development of either typical AMD or PCV. Further research is warranted to determine whether pigmentary abnormalities alone may be an important risk factor for PCV in Asians.
Age-related macular degeneration (AMD) is a leading cause of vision loss worldwide as well as in Japan. The features of AMD have been reported to be different between Asian and white populations. In Asian populations, polypoidal choroidal vasculopathy (PCV) is more common and may be present in as much as 50% of eyes with exudative AMD.1–3 In contrast, white eyes with exudative AMD mostly have typical AMD, and the frequency of PCV is less than 10%.4–6 In Asian populations, the prevalence of AMD in females is lower, and the proportion of exudative AMD is greater compared to that in white populations.7,8
Drusen and retinal pigmentary abnormalities within the macula are well-recognized early signs of AMD.9,10 In white populations, pigmentary abnormalities have been considered as retinal pigment epithelial (RPE) changes related to AMD only if those areas are associated with drusen.11 The Beaver Dam Study12 defined early age-related maculopathy as the presence of soft indistinct or reticular drusen or by the presence of any drusen type except hard indistinct, with pigmentary abnormalities in the macular area. Ferris et al.13 recently proposed a clinical classification system for AMD, which does not include pigmentary abnormalities alone as an early sign of AMD. Pigmentary abnormalities have been considered an early sign of AMD only when coexisting with drusen in studies based on white populations.9,10,12,14
A study showed that eyes that developed PCV had pigmentary atrophy without drusen just before the emergence of exudative changes.15 Another cross-sectional study in an Asian population showed that the prevalence of soft drusen in the fellow eyes of exudative AMD is lower in eyes with PCV than in eyes with typical AMD.1,2 These results suggest that pigmentary abnormalities without drusen may be more important risk factors than drusen for PCV in Asians. However, the association between such early signs and the risk of progression to exudative AMD in Asians has not been widely studied.
The aim of this observational case series was to examine the associations between early signs of AMD and the risk of developing typical AMD or PCV in the fellow eye of patients with unilateral exudative AMD in an Asian population, focusing particularly on eyes with only pigmentary abnormalities.
METHODS
This study followed the tenets of the Declaration of Helsinki and was approved by the ethics committee at Keio University School of Medicine. Informed consent was obtained from subjects after explaining the nature and possible consequences of the study.
Study Participants
This is a retrospective observational consecutive case series based on a detailed medical chart review. We recruited patients 50 years and older, with a definitive diagnosis of exudative AMD at least one eye, who presented at the Medical Retina (AMD) Clinic of the Department of Ophthalmology, Keio University Hospital (Tokyo, Japan), from January 2010 to January 2011. Of these, we enrolled patients who had unilateral exudative AMD at their first visit (baseline) with follow-up periods longer than 12 months. Diagnosis was made by the agreement of two masked retinal specialists, from fundus photographs, fluorescein angiography (FA), and/or indocyanine green angiography (ICGA). When the two retinal specialists did not agree, the diagnosis was made after further discussion with a third retinal specialist. Patients with choroidal neovascularization (CNV) other than AMD, such as myopic retinopathy, angioid streaks, or histoplasmosis, were excluded from this analysis.
Assessment of Early Signs of AMD in the Fellow Eye
The non-affected eyes at baseline (the fellow eye at risk) were categorized into four groups based on the presence of large drusen (≥125 μm)13,16 and/or pigmentary abnormalities in the fellow eye: 1) no early signs of AMD (group N), 2) large drusen alone (group D), 3) pigmentary abnormalities alone (group P), and 4) both large drusen and pigmentary abnormalities (group D + P) (Fig. 1).
FIGURE 1.
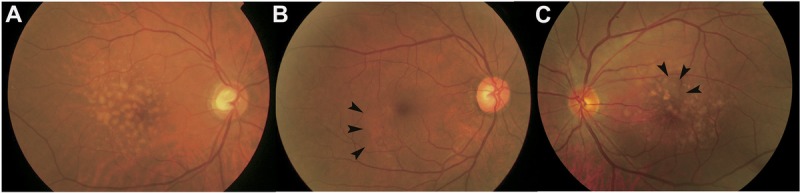
Categories based on the early signs of age-related macular degeneration. A, Large drusen alone (group D). B, Pigmentary abnormalities alone (group P) (pigmentary abnormalities indicated by arrowheads). C, Both large drusen and pigmentary abnormalities (group D + P) (pigmentary abnormalities indicated by arrowheads).
Drusen were classified based on size. The maximal lesion size within the macula was estimated using grading circles (within 1500 μm of foveal center), and drusen larger than 125 μm were considered to be large drusen.13,16 Retinal pigmentary abnormalities were defined as having either decreased or increased pigmentation within the macula.11,13,16
Assessment of Incident Exudative AMD in the Fellow Eye
The patients were followed up regularly at 1- to 6-month intervals or whenever the patients had new visual symptoms. At every visit, patients underwent best-corrected visual acuity test, binocular ophthalmoscopy, slit-lamp biomicroscopy with noncontact lenses, and/or OCT. The incidence of exudative AMD in the fellow eye was defined when CNV or exudative changes related to CNV (such as RPE detachment, retinal detachment, retinal hemorrhage, subretinal hemorrhage, or hard exudates) were observed. Differential diagnosis of typical AMD or PCV was made by the agreement of two masked retinal specialists, from FA, ICGA (TRX 50DX; Topcon Medical Systems, Tokyo, Japan), and/or OCT-C7 (Nidek, Gamagori, Japan) findings. When the two retinal specialists did not agree, the diagnosis was made after further discussion with a third retinal specialist.
Typical AMD was defined when the patients had serous or hemorrhagic exudative change, or both, and consistent CNV depicted on FA and ICGA.17,18 Polypoidal choroidal vasculopathy was defined according to the criteria of the Japanese study group of PCV.19 In brief, PCV is defined as having at least one of the criteria as follows: elevated orange-red lesions (excluding pigment epithelial detachment, choroidal hemangioma, and subretinal blood) observed by fundus examination or characteristic polypoidal lesions on ICGA.
Statistical Analysis
Statistical analysis was performed with SPSS software version 19.0 (SPSS, Inc., Chicago, IL). The χ2 test was used to compare categorical data with adjusted residual values. Analysis of variance with post hoc Tukey test was used for continuous variables. Using multivariate logistic regression models, the odds ratios (ORs) and their 95% confidence intervals (CIs) for the cumulative incidence of AMD were estimated between persons with and without early signs of AMD, adjusting for age and sex.
RESULTS
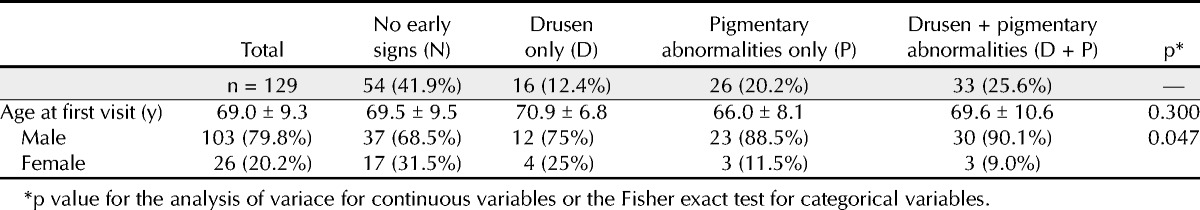
We identified 132 patients 50 years and older with unilateral CNV at their first visit (baseline). Of these, 1 patient with geographic atrophy, 1 patient with retinal angiomatous proliferation, and 1 patient who lacked a good-quality fundus photograph for clinical assessment were excluded. As a result, 129 Japanese patients with unilateral exudative AMD at baseline were included in the current analysis. Table 1 shows the baseline characteristics of the patients in this study; 103 were men (79.8%) and 26 were women, with a mean age of 69.3 years. There was no significant difference in age among the groups, but the difference in sex configuration was significant (p = 0.047).
TABLE 1.
Baseline characteristics of patients with unilateral exudative AMD
Of the 129 patients with unilateral exudative AMD at baseline, 14 (10.9%) developed exudative AMD in the second eye during the follow-up period (median ± quartile deviation, 38 ± 20.5 months). Of these 14 patients, 7 developed typical AMD and 7 developed PCV (Table 2). Development of typical AMD in fellow eyes occurred in 1 (1.9%) of 54 patients with no early signs of AMD (group N), in 1 (6.3%) of 16 patients with drusen only (group D), in 5 (15.2%) of 33 patients with drusen and pigmentary abnormalities (group D + P), and in none of 26 patients with pigmentary abnormalities only (group P). On the other hand, development of PCV in fellow eyes occurred in 1 (1.9%) of 54 patients in group N, in 6 (23.1%) of 26 patients in group P, and in none of patients in groups D and D + P. After adjusting for age and sex, patients in group D + P were more likely to develop typical AMD than patients in group N (OR = 9.46, 95% CI = 1.05 to 85.0, p = 0.04; Table 2) (see Figure 2, Supplemental Digital Content 1, which demonstrates a case of typical AMD development from group D + P, available at http://links.lww.com/OPX/A181). Patients in group P were more likely to develop any exudative AMD in the fellow eye (OR = 7.80, 95% CI = 1.45 to 41.9, p = 0.02). This association was mainly driven by the association between group P and PCV (OR = 15.9, 95% CI = 1.80 to 140.5, p = 0.01; Table 2) (see Figure 3, Supplemental Digital Content 2, which demonstrates a case of PCV development from group P, available at http://links.lww.com/OPX/A182).
TABLE 2.
Cumulative incidence of AMD in the fellow eye and age- and sex-adjusted odds ratio

We also analyzed the participants in concordance with a recently proposed classification by Ferris et al.13 Two (6.5%) of 31 patients with no signs of AMD and 5 (7.8%) of 64 patients with intermediate AMD developed typical AMD; on the other hand, 4 (12.9%) of 31 patients with no signs of AMD and 3 (4.7%) of 64 patients with intermediate AMD developed PCV. Regarding the cumulative incidence of AMD by pigmentary abnormalities and drusen size, 3 (27.3%) of 11 patients having pigmentary abnormalities with none or small drusen (<63 μm), 3 (12.5%) of 11 patients having pigmentary abnormalities with medium drusen (≥63 to <125 μm), and 6 (17.6%) of 34 patients having pigmentary abnormalities with large drusen (≥125 μm) developed late AMD.
DISCUSSION
In this study of patients with unilateral exudative AMD at baseline, as previously reported, fellow eyes with signs of both drusen and pigmentary abnormalities were more likely to develop typical AMD. Furthermore, we found that fellow eyes with pigmentary abnormalities alone were more likely to develop PCV. This result suggests that pigmentary abnormalities without drusen may be more important risk factors than drusen for PCV in Asians.
It is well recognized that eyes with both drusen and pigmentary abnormalities have an increased risk of developing exudative AMD compared to eyes with drusen alone in white population.20,21 In the Age-Related Eye Disease Study,20 the presence of large drusen and any pigmentary abnormalities were regarded as the major risk factors for advanced AMD; each factor was summed across both eyes, yielding a five-step scale (from no factor to four factors). The 5-year risk of advanced AMD was found to increase as 0.5%, 3%, 12%, 25%, and 50% for persons with zero, one, two, three, and four risk factors, respectively. Our finding of an association between eyes with both large drusen and pigmentary abnormalities and typical AMD is consistent with the previous consensus.
We found fellow eyes with pigmentary abnormalities alone without drusen more likely to develop PCV in our sample. Polypoidal choroidal vasculopathy often follows a “remitting-relapsing” course, presenting with chronic, multiple, recurrent serosanguineous detachments of the RPE and neurosensory retina.22 Signs of subretinal fibrosis, pigment epithelial hyperplasia, and atrophic degeneration may remain after the spontaneous resolution of the acute serosanguineous phase.23 Another study reported that abnormal choroidal vascular networks in a proposed origin of PCV lesions were present before the clinical manifestation of PCV lesions in more than half the eyes,15 which showed high vascular hyperpermeability.24 We speculate that the pigmentary abnormalities preceding the development of PCV could be the result of chronic changes caused by repeated mild serosanguineous detachments induced by the abnormal choroidal vascular network. If this were the case, pigmentary abnormalities without drusen could be a risk factor for future clinical presentation of exudative maculopathy secondary to PCV.
In white people, pigmentary abnormalities are considered RPE changes related to AMD only if those areas are associated with drusen11; thus, they were considered an early sign of AMD only when coexisting with drusen,9,10,14 and pigmentary abnormalities alone had not been considered to be a risk factor. Recently, Ferris et al.13 proposed a new clinical classification system for AMD. Regarding their report, persons with no visible drusen, small drusen (<63 μm), or pigmentary abnormalities should be considered to have no signs of AMD. Persons with medium drusen (≥63 to <125 μm) but without pigmentary abnormalities should be considered to have early AMD. Persons with large drusen (≥125 μm) or with pigmentary abnormalities associated with at least medium drusen should be considered to have intermediate AMD. They reported that 5-year risks of progressing to late AMD were estimated to increase approximately 100-fold, ranging from a 0.5% 5-year risk for normal aging changes to a 50% risk for the highest intermediate AMD risk group. In concordance with a recently proposed classification by Ferris et al.,13 a greater proportion of patients with intermediate AMD developed typical AMD compared to persons with no signs of AMD; on the other hand, a greater proportion of patients with no signs of AMD still developed PCV and it was more than that in the intermediate group. This discrepancy probably arises because eyes with pigmentary abnormalities alone (i.e., without drusen) are considered to have no sign of AMD in the classifications. Ferris et al. also described the relative importance of hyperpigmentary or hypopigmentary abnormalities in the absence of drusen as a significant risk factor for AMD, although they concluded that eyes having pigmentary abnormalities with no or small drusen (<63 μm) were not an important risk of progression to late AMD because none of the 64 patients having that in one eye progressed to AMD over 5 years. For reference, 3 (27.3%) of 11 eyes having pigmentary abnormalities with no or small drusen progressed to late AMD in our sample. These results cannot be directly compared. However, it was not a low rate, and there may be a possibility that Asians might have a different risk from white population. The current classification of AMD, defining that pigmentary abnormalities are considered as early signs of AMD only when they are coexisted with drusen, may be applicable when subtypes of exudative AMD is mostly typical AMD. We consider that a classification that incorporates pigmentary abnormalities alone as precursors to PCV may be needed where prevalence of PCV is relatively high such as in Asian populations.
There are several limitations in our study. First, this is a retrospective study, capturing occurrence of AMD in consecutive cases with unilateral AMD. A well-designed prospective study is anticipated. Second, there were only a small number of patients who developed exudative AMD in the fellow eye in this study. We adopted a study design in which we examined fellow eye involvement of exudative AMD to determine the associations of early signs of AMD and incident exudative AMD within a relatively short follow-up period. Our findings should therefore be confirmed and validated in prospective cohort studies with a larger sample size involving detailed assessments for early signs of AMD.
In conclusion, in our series of patients, eyes with both pigmentary abnormalities and large drusen were more likely to develop typical AMD, whereas pigmentary abnormalities without large drusen were associated with PCV. Further studies are warranted to confirm whether pigmentary abnormalities alone are a risk for PCV. Such studies may be able to guide the clinician to the relative risks of AMD subtypes in Asian populations.
Yoko Ozawa
Department of Ophthalmology
Keio University School of Medicine
35 Shinanomachi Shinjuku-ku
Tokyo 160-8582
Japan
e-mail: ozawa@a5.keio.jp
ACKNOWLEDGMENTS
The authors declare no financial support or conflicting relationship.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.optvissci.com).
SUPPLEMENTAL DIGITAL CONTENT
Supplemental Digital Content 1 (Figure 2), which demonstrates a case of typical AMD development from group D+P, available at http://links.lww.com/OPX/A181). Supplemental Digital Content 2 (Figure 3), which demonstrates a case of PCV development from group P, available at http://links.lww.com/OPX/A182.
REFERENCES
- 1. Maruko I, Iida T, Saito M, Nagayama D, Saito K. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol 2007; 144: 15– 22 [DOI] [PubMed] [Google Scholar]
- 2. Mori K, Horie-Inoue K, Gehlbach PL, Takita H, Kabasawa S, Kawasaki I, Ohkubo T, Kurihara S, Iizuka H, Miyashita Y, Katayama S, Awata T, Yoneya S, Inoue S. Phenotype and genotype characteristics of age-related macular degeneration in a Japanese population. Ophthalmology 2010; 117: 928– 38 [DOI] [PubMed] [Google Scholar]
- 3. Wen F, Chen C, Wu D, Li H. Polypoidal choroidal vasculopathy in elderly Chinese patients. Graefes Arch Clin Exp Ophthalmol 2004; 242: 625– 9 [DOI] [PubMed] [Google Scholar]
- 4. Yannuzzi LA, Wong DW, Sforzolini BS, Goldbaum M, Tang KC, Spaide RF, Freund KB, Slakter JS, Guyer DR, Sorenson JA, Fisher Y, Maberley D, Orlock DA. Polypoidal choroidal vasculopathy and neovascularized age-related macular degeneration. Arch Ophthalmol 1999; 117: 1503– 10 [DOI] [PubMed] [Google Scholar]
- 5. Ladas ID, Rouvas AA, Moschos MM, Synodinos EE, Karagiannis DA, Koutsandrea CN. Polypoidal choroidal vasculopathy and exudative age-related macular degeneration in Greek population. Eye (Lond) 2004; 18: 455– 9 [DOI] [PubMed] [Google Scholar]
- 6. Lafaut BA, Leys AM, Snyers B, Rasquin F, De Laey JJ. Polypoidal choroidal vasculopathy in Caucasians. Graefes Arch Clin Exp Ophthalmol 2000; 238: 752– 9 [DOI] [PubMed] [Google Scholar]
- 7. Kawasaki R, Yasuda M, Song SJ, Chen SJ, Jonas JB, Wang JJ, Mitchell P, Wong TY. The prevalence of age-related macular degeneration in Asians: a systematic review and meta-analysis. Ophthalmology 2010; 117: 921– 7 [DOI] [PubMed] [Google Scholar]
- 8. Yasuda M, Kiyohara Y, Hata Y, Arakawa S, Yonemoto K, Doi Y, Iida M, Ishibashi T. Nine-year incidence and risk factors for age-related macular degeneration in a defined Japanese population the Hisayama study. Ophthalmology 2009; 116: 2135– 40 [DOI] [PubMed] [Google Scholar]
- 9. Klein R, Klein BE, Tomany SC, Meuer SM, Huang GH. Ten-year incidence and progression of age-related maculopathy: The Beaver Dam Eye Study. Ophthalmology 2002; 109: 1767– 79 [DOI] [PubMed] [Google Scholar]
- 10. Wang JJ, Foran S, Smith W, Mitchell P. Risk of age-related macular degeneration in eyes with macular drusen or hyperpigmentation: the Blue Mountains Eye Study cohort. Arch Ophthalmol 2003; 121: 658– 63 [DOI] [PubMed] [Google Scholar]
- 11. Klein R, Davis MD, Magli YL, Segal P, Klein BE, Hubbard L. The Wisconsin age-related maculopathy grading system. Ophthalmology 1991; 98: 1128– 34 [DOI] [PubMed] [Google Scholar]
- 12. Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology 1992; 99: 933– 43 [DOI] [PubMed] [Google Scholar]
- 13. Ferris FL, 3rd, Wilkinson CP, Bird A, Chakravarthy U, Chew E, Csaky K, Sadda SR. Clinical classification of age-related macular degeneration. Ophthalmology 2013; 120: 844– 51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mitchell P, Smith W, Attebo K, Wang JJ. Prevalence of age-related maculopathy in Australia. The Blue Mountains Eye Study. Ophthalmology 1995; 102: 1450– 60 [DOI] [PubMed] [Google Scholar]
- 15. Ueta T, Iriyama A, Francis J, Takahashi H, Adachi T, Obata R, Inoue Y, Tamaki Y, Yanagi Y. Development of typical age-related macular degeneration and polypoidal choroidal vasculopathy in fellow eyes of Japanese patients with exudative age-related macular degeneration. Am J Ophthalmol 2008; 146: 96– 101 [DOI] [PubMed] [Google Scholar]
- 16.Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol 2001; 119: 1417– 36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Barbazetto I, Burdan A, Bressler NM, Bressler SB, Haynes L, Kapetanios AD, Lukas J, Olsen K, Potter M, Reaves A, Rosenfeld P, Schachat AP, Strong HA, Wenkstern A. Photodynamic therapy of subfoveal choroidal neovascularization with verteporfin: fluorescein angiographic guidelines for evaluation and treatment—TAP and VIP report no. 2. Arch Ophthalmol 2003; 121: 1253– 68 [DOI] [PubMed] [Google Scholar]
- 18.Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials—TAP report. Arch Ophthalmol 1999; 117: 1329– 45 [PubMed] [Google Scholar]
- 19.Japanese Study Group of Polypoidal Choroidal Vasculopathy. [Criteria for diagnosis of polypoidal choroidal vasculopathy.]. Nihon Ganka Gakkai Zasshi 2005; 109: 417– 27 [PubMed] [Google Scholar]
- 20. Ferris FL, Davis MD, Clemons TE, Lee LY, Chew EY, Lindblad AS, Milton RC, Bressler SB, Klein R. A simplified severity scale for age-related macular degeneration: AREDS Report No. 18. Arch Ophthalmol 2005; 123: 1570– 4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Macular Photocoagulation Study Group. Risk factors for choroidal neovascularization in the second eye of patients with juxtafoveal or subfoveal choroidal neovascularization secondary to age-related macular degeneration. Arch Ophthalmol 1997; 115: 741– 7 [DOI] [PubMed] [Google Scholar]
- 22. Ciardella AP, Donsoff IM, Huang SJ, Costa DL, Yannuzzi LA. Polypoidal choroidal vasculopathy. Surv Ophthalmol 2004; 49: 25– 37 [DOI] [PubMed] [Google Scholar]
- 23. Sho K, Takahashi K, Yamada H, Wada M, Nagai Y, Otsuji T, Nishikawa M, Mitsuma Y, Yamazaki Y, Matsumura M, Uyama M. Polypoidal choroidal vasculopathy: incidence, demographic features, and clinical characteristics. Arch Ophthalmol 2003; 121: 1392– 6 [DOI] [PubMed] [Google Scholar]
- 24. Sasahara M, Tsujikawa A, Musashi K, Gotoh N, Otani A, Mandai M, Yoshimura N. Polypoidal choroidal vasculopathy with choroidal vascular hyperpermeability. Am J Ophthalmol 2006; 142: 601– 7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


