Abstract
Background
Readmissions are a common problem in cardiac surgery. The goal of this study was to examine the frequency, timing, and associated risk factors for readmission after cardiac surgery.
Methods
5,158 adult cardiac surgery patients (5,059 included in analysis) were prospectively enrolled in a 10center cohort study to assess risk factors for infection following cardiac surgery. Data were also collected on all-cause readmissions occurring within 65 days after surgery. Major outcomes included readmission rate stratified by procedure type, cause of readmission, length of readmission stay, and discharge disposition after readmission. Multivariable Cox regression was used to determine risk factors for time to first readmission.
Results
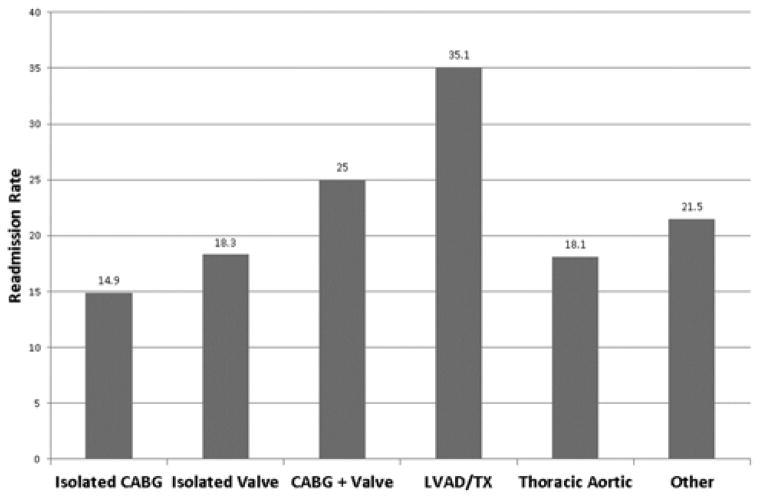
The overall rate of readmission was 18.7% (number of readmissions=945). When stratified by the most common procedure type, readmission rates were: isolated CABG (14.9%, n=248), isolated valve (18.3%, n=337), CABG + valve (25.0%, n=169). The three most common causes of first readmission within 30 days were: infection (17.1%, n=115), arrhythmia (17.1%, n=115), and volume overload (13.5%, n=91). More first readmissions occurred within 30 days (80.6%, n=672) than after 30 days (19.4%, n=162), and 50% of patients were readmitted within 22 days from index surgery. The median length of stay during the first readmission was 5 days. 15.8% (n=128) of readmitted patients were discharged to a location other than home. Baseline patient characteristics associated with readmission included: female gender, diabetes mellitus on medication, COPD, elevated creatinine, lower hemoglobin, and longer surgery time. In addition, the more complex surgical procedures were associated with increased risk of readmission compared to the CABG group.
Conclusions
Nearly 1 out of 5 patients who undergo cardiac surgery require readmission, an outcome with significant health and economic implications. Management practices to avert in-hospital infections, reduce post-operative arrhythmias, and avoid volume overload offer important targets for quality improvement.
Keywords: Hospital readmissions, length of stay, cardiac
INTRODUCTION
The continued rise in national healthcare expenditures has led to increasing focus on hospital readmission rates as a target for improving the overall quality and cost of healthcare delivery in the United States. A study by Jencks et al [1] demonstrated that in 2004, 20% of Medicare beneficiaries were readmitted within 30 days of hospital discharge at a cost of approximately $17.4 billion. Several analyses have demonstrated that the majority of readmissions are secondary to potentially preventable causes [2–3]. Recently, Dharmarajan and colleagues reported 30-day readmission rates for patients hospitalized with heart failure and acute myocardial infarction of 24.8% and 19.9%, respectively [4]. The Centers for Medicare and Medicaid Services Readmission Reduction Program was initiated on October 1, 2012, as part of the Affordable Care Act [5]. This new program administers penalties ranging from 0.01–1% of Medicare revenue for an excess 30-day readmission rate in the categories of heart failure, myocardial infarction, and pneumonia. Both the magnitude of the penalty and spectrum of conditions penalized are widely expected to increase and may include common cardiac surgical procedures. There is controversy, however, whether 30-day readmission measures are adequately data-driven and patient-focused [6].
Literature on readmissions after cardiac surgery is scant and studies examining readmissions in large surgical populations have demonstrated 30-day readmission rates ranging from 7 – 20 % [7–9]. In an analysis of all patients undergoing CABG surgery from 2005–2007 in New York State, Hannan et al. reported readmission rates ranging from 8.3 – 21.1%, with the most common causes of readmission being post-operative infection and heart failure [8]. Reducing readmission rates is a critical area for future quality improvement. Additional data are needed, however, to identify the etiologic spectrum and timing of readmissions to inform the development of targeted quality initiatives.
The goal of this study was to assess the frequency, timing, and risk factors associated with hospital readmissions for adult patients undergoing cardiac surgery. This investigation was part of a larger prospective cohort study that examined infectious complications after cardiac surgery within centers participating in the Cardiothoracic Surgical Trials Network (CTSN) [10].
PATIENTS AND METHODS
Study design and patients
The design and outcomes of the prospective observational cohort study, “Management Practices and the Risk of Infections following Cardiac Surgery”, have been previously reported [11]. Briefly, the study was conducted at 10 centers participating in the CTSN (funded by the National Institutes of Health and the Canadian Institutes of Health Research) in the United States and Canada. Inclusion criteria were any cardiac surgical intervention and age ≥ 18 years. Patients with active systemic infection, including endocarditis, at the time of surgery were excluded. The primary objective of the cohort study was to identify management practices associated with risk for infection.
The study sample size was not predetermined; rather enrollment continued until a minimum of 200 patients with a major infection were identified, which allowed for valid inferences from multivariable models. Data were transmitted from sites using a web-based electronic data capture system to a secure server at the Data Coordinating Center (DCC). The study sites and DCC received Institutional Review Board approval for the prospective cohort study. All patients provided written informed consent to participate in the study and to release their medical information during this time frame. From February 1 to September 30, 2010, 5,158 consecutive adult cardiac surgery patients were prospectively enrolled in the study. Patients were followed for 65 days after surgery and data on all-cause hospital readmission were collected during this time.
Endpoints
The primary end-point for the current analysis was the frequency and timing of all-cause readmissions within 65 days of the index cardiac surgical procedure, and patient and operative factors associated with readmission risk. Data on the timing and cause for readmission were collected as well as the length of readmission hospitalization and discharge disposition.
Data analysis
The dataset for the current study consisted of 5,059 patients who were discharged after index hospitalization. Patients were excluded if they died during the index hospitalization (n=52), had an index length of stay lasting more than 65 days after surgery (n=15) or if they had one readmission that lacked both readmission and discharge dates (n=32). For the purpose of this study, emergency room and rehabilitation visits were not considered as readmissions. Patients with missing readmission dates (but with known discharge dates, n=2) were included in the overall readmission statistics but were excluded from the time to event model. The time to event analysis models time from index surgical procedure to first readmission, while analyses characterizing the timing of first readmission (≤ 30 vs. > 30 days from discharge) uses time from index discharge to first readmission. We used Cox proportional hazards regression to model time from index surgical procedure to first readmission in relation to risk factors potentially related to readmission [12]. These models included a left truncation to account for patients who died during the index hospitalization and a competing risk to account for mortality after discharge. Predictors of interest included demographics, baseline laboratory values, comorbidities, and operative factors [Appendix]. Variables with a p value of 0.15 or less in the univariable analysis were considered in the multivariable model. A backward selection approach was used to identify significant risk factors at the 0.05 significance level. All analyses utilized SAS (SAS® v9.2; Cary, NC) and R2.15.2 statistical software [13].
RESULTS
Among the 5,059 patients who were discharged from the hospital within 65 days of surgery, mean age was 64±13 years, median body mass index (BMI) was 28 (Q1, Q3 [first and third quartiles] 25, 32) kg/m2, and 33% (n=1,654) were women (Table 1). Diabetes mellitus was present in 23% (n=1,144) of patients, 29% (n=1,455) had heart failure, and 14% (n=724) had at least mild COPD. Eighteen percent (n=930) of patients had undergone prior cardiac surgery. The most common procedures were isolated CABG (33%, n=1,661) and isolated valve surgery (36%, n=1,840). Median cardiopulmonary bypass time was 105 (Q1, Q3 78, 139) minutes.
Table 1.
Baseline Patient and Operative Characteristics
| Overall (N = 5059) | |
|---|---|
| Demographics | |
| Age, mean (SD) | 64.3 (13.2) |
| Male | 3405 (67.3%) |
| White | 4240 (83.9%) |
| BMI | 28.3 (25.1, 32.3) |
| Insurance | |
| Medicaid | 228 (4.5%) |
| Medicare | 1879 (37.2%) |
| Government (Other) | 617 (12.2%) |
| Private | 2067 (41.0%) |
| None/Self | 256 (5.1%) |
| Baseline Laboratories | |
| WBC, ×103/ml | 6.9 (5.7, 8.4) |
| Creatinine, mg/dL | 1.0 (0.8, 1.2) |
| Hemoglobin, g/dL | 13.4 (12.0, 14.6) |
| Cardiac morbidity | |
| Heart failure | 1455 (28.8%) |
| Ejection fraction | 55.0 (48.0, 60.0) |
| Previous cardiac surgery | 930 (18.4%) |
| Noncardiac morbidity | |
| Diabetesmellitusb | 1144 (22.6%) |
| COPD | |
| None | 4335 (85.7%) |
| Mild or moderate | 628 (12.4%) |
| Severe | 96 (1.9%) |
| Operative | |
| Surgery time, hours | 4.2 (3.3, 5.2) |
| Bypass time, minutesc | 105.0 (78.0, 139.0) |
| Surgery Type | |
| Elective | 3735 (73.8%) |
| Urgent | 1193 (23.6%) |
| Emergent | 131 (2.6%) |
| Procedure | |
| Isolated CABG | 1661 (32.8%) |
| Isolated valve | 1840 (36.4%) |
| CABG + valve | 675 (13.3%) |
| LVAD/TX | 111 (2.2%) |
| Thoracic aortic | 419 (8.3%) |
| Other | 353 (7.0%) |
Continuous variables are expressed as median (IQR) and categorical variables as count (%)
Insulin or oral medications
91.1% of patients had on-pump surgical procedures
Key: CABG, coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; LVADTX, left ventricular assist device or transplant surgery; SD, standard deviation
Incidence and cause of overall readmissions
Overall, 836 (16.5%) patients had one or more readmission for a total of 945 readmissions (total readmissions per index discharges = 18.7%). Of patients readmitted, 11.6% (n=97) experienced more than one readmission. When stratified by procedure type, overall readmission rates were as follows: isolated CABG (14.9%, n=248), isolated valve (18.3%, n=337), CABG + valve (25.0%, n=169), aortic surgery (18.1%, n=76), ventricular assist device or transplant (35.1%, n=39), and other (21.5%, n=76) (Figure 1). Infection accounted for 16% of the overall reasons for readmission. The five most common infections resulting in readmission were: superficial surgical site infection of the chest (24%, n=36), pneumonia (21.3%, n=32), deep surgical site infection of the chest (13.3%, n=20), superficial surgical site infection of the groin (10.7%, n=16), and bloodstream infection (6%, n=9).
Figure 1.
Overall readmission rates by procedure
Timing and etiology of first readmissions
Among patients with a known readmission date (n=834), 80.6% (n=672) were readmitted within 30 days following discharge. The causes for first readmission stratified by 30 days or beyond 30 days from hospital discharge are shown in Figure 2. Within 30 days, the three most common causes for first readmission included: infection (17.1%, n=115), arrhythmia (17.1%, n=115), and volume overload (13.5%, n=91). Beyond 30 days, the three most common causes of first readmission included: volume overload (13.6%, n=22), infection (13.0%, n=21), and chest pain (9.9%, n=16).
Figure 2.
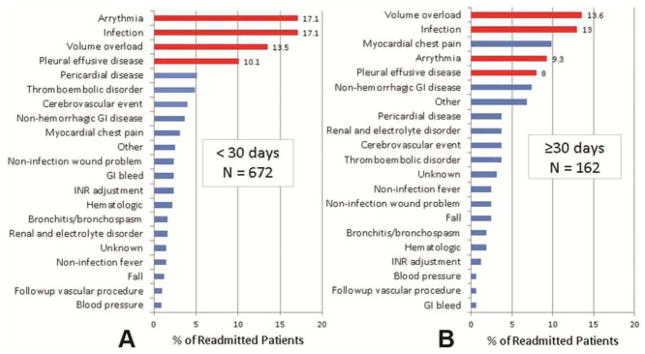
Indication for first readmission.
Red bars indicate the most common causes of readmission within 30 days of index discharge.
Predictors of first readmission
Table 2 presents the significant risk factors for readmission. They included female gender (HR 1.35; 95% CI 1.16, 1.57), diabetes mellitus on medication (HR 1.35; 95% CI 1.15, 1.59), COPD (HR 1.42; 95% CI 1.19, 1.68), and elevated creatinine (HR 1.10; 95% CI 1.05, 1.15). Higher hemoglobin levels were protective (HR 0.91; 95% CI 0.88, 0.95). Longer surgery time was associated with an increased risk of readmission (HR 1.15; 95% CI 1.10, 1.20). Compared to the CABG only group, LVAD/transplant patients were at the highest risk for readmission (HR 3.36; 95% CI 2.34, 4.84).
Table 2.
Risk factors associated with readmission
| Variable | HR (95% CI) | P Value |
|---|---|---|
| Female | 1.35 (1.16, 1.57) | <0.001 |
| Diabetes mellitus (yes/no) | 1.35 (1.15, 1.59) | <0.001 |
| COPD (yes/no) | 1.42 (1.19, 1.68) | <0.001 |
| Creatinine | 1.10 (1.05, 1.15) | <0.001 |
| Hemoglobin | 0.91 (0.88, 0.95) | <0.001 |
| Duration of surgery (hour) | 1.15 (1.10, 1.20) | <0.001 |
| Procedure (ref: CABG) | ||
| Valve | 1.33 (1.11, 1.60) | 0.002 |
| CABG + Valve | 1.52 (1.23, 1.88) | <0.001 |
| LVAD/TX | 3.36 (2.34, 4.84) | <0.001 |
| Thoracic aortic | 1.40 (1.06, 1.85) | 0.017 |
| Other | 1.41 (1.06, 1.89) | 0.019 |
Key: CI, confidence interval; COPD, chronic obstructive pulmonary disease; HR, hazard ratio; LVADTX, left ventricular assist device or transplant surgery
Length of stay and discharge disposition for first readmission
The median time from index surgical procedure to first readmission was 22 (Q1, Q3 14, 36) days. When stratified by procedure type, the median times for first readmissions were: isolated CABG (23 days), isolated valve (19 days), CABG + valve (23 days), aortic surgery (22 days), left ventricular assist device or transplant (42 days), and other (21 days). The median length of stay for the first readmission was 5 (Q1, Q3 3,9) days. Among patients admitted to the intensive care unit (ICU) during the first readmission (n=139), the median ICU length of stay was 2 (Q1, Q3 1,5) days. Almost all patients (84%) were discharged to home after the first readmission.
COMMENT
While advancements have been made over the past decade in improving outcomes following cardiac surgery, readmission rates remain high. In this large, multicenter, prospective cohort of adult cardiac surgery patients, the overall readmission rate was 18.7% with infection and arrhythmia being the two most common causes for first readmission within 30 days of discharge.
Timing of readmissions and public policy implications
The median time to first readmission from surgery was 22 days with 80.6% of first readmissions occurring within 30-days of discharge. The fact that the majority of readmissions occurred during the 30-day window from discharge is problematic for provider institutions given the recent CMS Readmission Reduction Initiative[5]. While readmission penalties currently do not apply to cardiac surgical procedures, many policy experts anticipate that there will be an expansion of penalties in the near future. Approximately 2,217 hospitals will be assessed penalties ranging from 0.01–1% of their Medicare revenue for the 2013 fiscal year for excess readmission ratios [14]. The total cost of penalties is now in the range of $280 million and the current 1% penalty cap is expected to increase [15]. While a 30 day time point for examining readmissions has often been criticized as clinically arbitrary, our analysis demonstrates that 30 day period captures the majority of readmissions.
Causes of readmissions
In our analysis, infections, arrhythmias, volume overload, and pleural effusions accounted for 58% of readmissions within 30 days of discharge and demonstrate areas where practice modifications may lead to quality improvement. Previous studies examining the New York State cardiac surgery registry have identified infections as the leading cause of readmission. Our study delineates the types of infection. Pneumonia, superficial sternotomy infections (chest), and deep sternotomy infections (chest) accounted for 58% of infection-related readmissions. These infections are potentially preventable complications that may be addressed through quality improvement initiatives. There has been a recent national focus on process of care measures and bundling strategies to prevent post-operative infections [16]. Of note, our prior analysis of post-operative infections identified pneumonia as the most frequent infection [11]. Respiratory bundling strategies to reduce pneumonia risk include: ventilator bundles, respiratory physiotherapy, and early ambulation [17]. Primary surgical site infections were the first and third most common source of infection-related readmission and similarly demonstrate the need for greater attention to processes of care. Relatively simple measures such as appropriate timing and dosing of antibiotics, attention to skin preparation, discontinuation of antibiotics after 24 hours, and hand washing have been demonstrated to reduce surgical site infections [18]. Unfortunately, previous studies have demonstrated that compliance with the aforementioned bundling strategies and process of care performance measures is poor [19]. With a growing focus on reducing readmissions, greater adoption of and attention to these strategies will be critical.
Arrhythmias, volume overload, and pleural effusions also served as common etiologies for readmission. Previous studies have demonstrated that a significant fraction of cardiac surgery patients experience postoperative atrial fibrillation and that such patients are susceptible to continuing arrhythmias after discharge [20]. There is wide variation in the management of post-operative atrial fibrillation, including the use of anti-arrhythmic medications and anticoagulants during and after hospitalization. Furthermore, patient compliance with post-operative anti-arrhythmic drug therapy is unknown. Post-operative atrial fibrillation is a common complication which, in our analysis, is also a common cause of readmission. Future, prospective studies directed at the peri-operative and post-discharge management of atrial fibrillation are necessary.
Readmissions for volume overload and pleural effusions identify the need for more careful attention to post-operative fluid management. Patients undergoing cardiac surgery are subject to wide fluctuations in fluid balance. Diurectics are commonly used to achieve a net negative fluid balance, but the degree to which patients are diuresed is often arbitrary and in response to pre-operative weight measurement and chest x-ray or physical exam findings demonstrating volume overload. Moreover, there are no specific guidelines for the dose and duration of diuretics upon discharge. Thus, greater attention to fluid balance in a more objective and consistent manner may allow for reductions in readmissions for volume overload and pleural effusions. This area also warrants further investigation in prospective studies.
Identifying patients at high risk for readmission
Several studies have focused on the use of explicit and well documented transition in care plans as means of reducing hospital readmissions. Given the high volume of cardiac surgery in the United States and the cost of such interventions, focusing readmission interventions on high-risk populations might make readmission reduction strategies more feasible across a broader range of hospitals. We demonstrate an association between complexity of the index surgical procedure and risk of readmission, with isolated CABG demonstrating the lowest readmission rate. There was a stepwise increase in readmission risk from isolated CABG, to isolated valve, to CABG with valve surgery. Patients undergoing placement of ventricular assist devices and heart transplantation, however, demonstrated the highest risk of readmission. Thus, patients undergoing more complex surgical procedures would appear to derive relatively greater benefit from readmission reduction programs.
When baseline characteristics were studied, female gender, treated diabetes mellitus, COPD, elevated creatinine, lower hemoglobin, and longer surgery correlated with increased risk of readmission. Several of the aforementioned risk factors observed in our analysis have been identified by other investigators and correlate with the most common etiologies for readmission [21]. Patients with diabetes mellitus have a higher risk of readmission for infections. Patients with COPD may also be at higher risk for developing pneumonia after surgery. Individuals with ventricular assist devices, prolonged surgery duration, and elevated serum creatinine are sensitive to fluid management and at higher risk for readmission for volume overload. Gender has been reported previously though its correlation with increased risk of readmission is less clearly understood [22]. These baseline factors as well as the influence of baseline hemoglobin on readmission risk require further exploration.
Resource utilization and future directions for readmission reduction initiatives
CMS currently estimates that avoidable hospital readmissions account for $17.4 billion of the $102.6 billion Medicare budget [23]. Cardiac surgery represents one of the most expensive procedural areas, with mean charge for CABG estimated at approximately $100,000 per case [24]. Hospital readmissions place strain on resource utilization with patients who are readmitted spending a median of 5 additional days in the hospital. Moreover, downstream financial costs must also be considered as our study demonstrated that nearly 20% of readmitted patients are discharged to a location other than home.
Future readmission reduction initiatives will be necessary given the need for quality improvement and the anticipated expansion of readmission penalties to cardiac surgery. Future studies will be needed to determine which readmission strategies are most effective for cardiac surgical patients. Given the fact that median time from surgery to first readmission in our study was 22 days, one simple solution might be for patients to return to the hospital earlier for their first scheduled post-operative visit, as is now commonly applied to patients after hospitalization for decompensated heart failure. In-patient educational initiatives focused on high risk patients is a second strategy that could reinforce medication compliance and early reporting of worrisome symptoms. Lastly, return visit educational programs or telephone outreach are additional, albeit more costly, programs for readmission reduction. Many of these strategies are already utilized in high volume surgical centers.
Limitations
There are several limitations to our analysis. First, data are representative of readmission rates at academic medical centers and do not include outcomes at non-academic centers. Second, in our analysis, we did not consider the impact of socioeconomic status as this information was not collected. In addition, complications that occurred during the index hospitalization may be risk factors for future readmissions. We did not collect non-infection related complications during the index hospitalization in this prospective study, and, therefore, did not include any complications (including infection) in the model. Lastly, since the primary purpose of the infections observational study was to capture infections within 65 days of cardiac surgery, the timing and numbers of readmissions were constrained by the index length of stay.
Conclusion and Implications
Overall readmissions after cardiac surgery remain relatively high with infections serving as a leading cause for readmission. Patient undergoing complex cardiac surgical procedures are at higher risk of readmission with additional risk factors including female gender, diabetes, COPD, elevated creatinine, lower hemoglobin, and longer surgery time. Our analysis not only demonstrates the timing and etiology of readmissions in a prospective cohort of patients but also identifies high risk groups of patients that may ultimately benefit from more focused readmission reduction strategies.
Acknowledgments
This research was supported by a cooperative agreement with the National Heart, Lung, and Blood Institute and the National Institute of Neurological Diseases and Stroke, National Institutes of Health, and by the Canadian Institutes of Health Research.
APPENDIX
Variables used in the analysis
Demographics
Age (y), gender, Caucasian, body mass index (kg/m2), insurance (Medicaid, Medicare, Other Government, Private, None/Self)
Baseline Laboratories
White cell count (×103/ml), creatinine (mg/dL), hemoglobin (g/dL)
Cardiac morbidity
Heart failure, ejection fraction, previous cardiac surgery, hypertension, baseline VAD, baseline intra-aortic balloon pump
Noncardiac morbidity
Diabetes mellitus, COPD, steroids use, hypercholesterolemia, peripheral vascular disease, cerebrovascular accident
Operative
Surgery time, surgery type (elective, urgent, emergent), cardiac procedure (CABG, Valve, CABG+Valve, LVAD/TX, Thoracic aortic, Other), incision type (full sternotomy vs. not full sternotomy), bypass use, circulatory arrest use, open sternum
Footnotes
This material was presented at the 49th annual meeting of the Society of Thoracic Surgeons, Los Angeles, CA United States, January 30, 2013
ClinicalTrials.gov Identifier: NCT01089712
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med. 2000;160:1074–81. doi: 10.1001/archinte.160.8.1074. [DOI] [PubMed] [Google Scholar]
- 3.Ashton CM, Del Junco DJ, Souchek S, Wray NP, Mansyur CL. The association between quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care. 1997;35:1044–1059. doi: 10.1097/00005650-199710000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–63. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CMS Readmission Reduction Program. [Accessed January 5, 2013];Government document. Available at http://www.gpo.gov/fdsys/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf.
- 6.Vaduganathan M, Bonow RO, Gheorghiade M. Thirty-day readmissions: the clock is ticking. JAMA. 2013;309:345–6. doi: 10.1001/jama.2012.205110. [DOI] [PubMed] [Google Scholar]
- 7.Stewart RD, Campos CT, Jennings B, Lollis SS, Levitsky S, Lahey SJ. Predictors of 30-day hospital readmission after coronary artery bypass. Ann ThoracSurg. 2000;70:169–74. doi: 10.1016/s0003-4975(00)01386-2. [DOI] [PubMed] [Google Scholar]
- 8.Hannan EL, Zhong Y, Lahey SJ, et al. 30-day readmissions after coronary artery bypass graft surgery in New York State. JACC CardiovascInterv. 2011;4:569–76. doi: 10.1016/j.jcin.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Hannan EL, Racz MJ, Walford G, et al. Predictors of readmission for complications of coronary artery bypass graft surgery. JAMA. 2003;290:773–80. doi: 10.1001/jama.290.6.773. [DOI] [PubMed] [Google Scholar]
- 10.Gardner TJ, O’Gara PT. The Cardiothoracic Surgery Network: randomized clinical trials in the operating room. J Thorac Cardiovasc Surg. 2010;139:830–4. doi: 10.1016/j.jtcvs.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Acker MA, Argenziano M, Puskas JD, et al. Infections After Cardiac Surgery: Initial Experience from the Cardiothoracic Surgical Trials Network. Circulation. 2011;124:A12247. [Google Scholar]
- 12.Geskus RB. Cause-Specific Cumulative Incidence Estimation and the Fine and Gray Model Under Both Left Truncation and Right Censoring. Biometrics. 2011;67:39–49. doi: 10.1111/j.1541-0420.2010.01420.x. [DOI] [PubMed] [Google Scholar]
- 13.Liesbeth CW, Fiocco M, Putter H. mstate: An R Package for the Analysis of Competing Risks and Multi-State Models. Journal of Statistical Software. 2011;38(7):1–30. URL http://www.jstatsoft.org/v38/i07/ [Google Scholar]
- 14.Clancy CM. New hospital readmission policy links financial and quality incentives. J Nurs Care Qual. 2013;28:1–4. doi: 10.1097/NCQ.0b013e3182725d82. [DOI] [PubMed] [Google Scholar]
- 15.Berenson RA, Paulus RA, Kalman NS. Medicare’s readmissions-reduction program--a positive alternative. N Engl J Med. 2012;366:1364–6. doi: 10.1056/NEJMp1201268. [DOI] [PubMed] [Google Scholar]
- 16.Curtis LT. Prevention of hospital-acquired infections: review of non-pharmacological interventions. J Hosp Infect. 2008;69:204–19. doi: 10.1016/j.jhin.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bonten MJ, Kollef MH, Hall JB. Risk factors for ventilator-associated pneumonia: from epidemiology to patient management. Clin Infect Dis. 2004 Apr 15;38(8):1141–9. doi: 10.1086/383039. [DOI] [PubMed] [Google Scholar]
- 18.Schweizer ML, Herwaldt LA. Surgical site infections and their prevention. Curr Opin Infect Dis. 2012;25:378–84. doi: 10.1097/QCO.0b013e32835532f7. [DOI] [PubMed] [Google Scholar]
- 19.Erasmus V, Daha TJ, Brug H, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31:283–94. doi: 10.1086/650451. [DOI] [PubMed] [Google Scholar]
- 20.Aranki SF, Shaw DP, Adams DH, et al. Predictors of atrial fibrillation after coronary artery surgery. Current trends and impact on hospital resources. Circulation. 1996;94:390–7. doi: 10.1161/01.cir.94.3.390. [DOI] [PubMed] [Google Scholar]
- 21.Price JD, Romeiser JL, Gnerre JM, Shroyer AL, Rosengart TK. Risk Analysis for Readmission after Coronary Artery Bypass Surgery: Developing a Strategy to Reduce Readmissions. J Am CollSurg. 2013;216:412–419. doi: 10.1016/j.jamcollsurg.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Edwards FH, Carey JS, Grover FL, Bero JW, Hartz RS. Impact of gender on coronary bypass operative mortality. Ann ThoracSurg. 1998;66:125–31. doi: 10.1016/s0003-4975(98)00358-0. [DOI] [PubMed] [Google Scholar]
- 23.The Congressional Research Service. Medicare hospital readmissions: issues, policy options and PPACA. Washington, D.C: [Accessed January 2, 2013]. Available at: http://www.ncsl.org/documents/health/Medicare_Hospital_Readmissions_and_PPACA.pdf. [Google Scholar]
- 24.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics - 2012 update: a report from the American Heart Association. Circulation. 2012;125:e2e, e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]