Abstract
Objective
To describe the prevalence of multimorbidity involving 20 selected chronic conditions in a geographically defined US population, emphasizing age, sex, and ethnic differences.
Patients and Methods
Using the Rochester Epidemiology Project (REP) records-linkage system, we identified all residents of Olmsted County, MN on April 1, 2010, and we electronically extracted the International Classification of Diseases, ninth revision (ICD-9) codes associated with all healthcare visits made between April 1, 2005 and March 31, 2010 (5-year capture frame). Using these ICD-9 codes, we defined the 20 common chronic conditions recommended by the US Department of Health and Human Services. We counted only persons who received at least two codes for a given condition separated by more than 30 days, and calculated the age-, sex-, and ethnicity-specific prevalence of multimorbidity.
Results
Of the 138,858 study subjects, 52.4% were women, 38.9% had one or more conditions, 22.6% had two or more, and 4.9% had 5 or more conditions. The prevalence of multimorbidity (2 or more conditions) increased steeply with older age and reached 77.3% at ages 65 years and older. However, the absolute number of people affected by multimorbidity was higher in those younger than 65 years. Although the prevalence of multimorbidity was similar in men and women overall, the most common dyads and triads of conditions varied by sex. Compared to Whites, the prevalence of multimorbidity was slightly higher in Blacks and slightly lower in Asians.
Conclusion
Multimorbidity is common in the general population; it increases steeply with older age, has different patterns in men and women, and varies by ethnicity.
Introduction
Current population growth in the United States, increases in the older adult population, and changes in disease dynamics predict major increases in the prevalence of chronic diseases and combinations of chronic conditions (i.e., multimorbidity) and threaten both the public health and the financial health of our country. Medical, public health, and social programs have traditionally focused on single chronic diseases without considering the broader context of multiple risk factors and multimorbidity. Consequently, clinical practice guidelines focusing on a single disease may be inadequate when applied to persons with multimorbidity and may increase polypharmacy.1,2 The high prevalence of multiple chronic conditions necessitates the planning of preventive, treatment, and public health programs.2-11
In response to this health crisis, in 2010 the US Department of Health and Human Services (US-DHHS) developed a list of 20 conditions considered public health priorities for the nation and created a strategic framework for optimizing health and quality of life for individuals with multimorbidity.3,4 Despite national concerns, the United States has no comprehensive, clinical records-based data sets for all ages and for all regions of the nation in which to study multimorbidity.7 Therefore, important information may come from smaller populations for which a data collection infrastructure is in place. We used the records-linkage system maintained by the Rochester Epidemiology Project (REP) to study patterns of multimorbidity in a geographically defined US population with emphasis on its distribution by age, sex, and ethnicity.12 The characterization of multimorbidity patterns in a geographically defined population allows comparisons with other localized populations in the United States or worldwide to investigate geographic similarities or differences. In addition, our findings can be used to guide decisions for clinical practice or public health in the local community. Therefore, our study has important implications for a broad number of practitioners both locally and at the national and international level.
PATIENTS AND METHODS
Study population
The vast majority of medical care in Olmsted County, MN has been provided historically and is currently provided by a few health care institutions: Olmsted Medical Center and its affiliated hospital, Mayo Clinic and its two affiliated hospitals, Rochester Family Medicine Clinic, and a few smaller care facilities. The health care records from these institutions are linked together through the REP records-linkage system.12-14 Persons are considered residents of Olmsted County at the time of each health care visit based on their address (REP Census). The population counts obtained by the REP Census are similar to those obtained by the US Census, suggesting that virtually the entire population of the county is captured by the system.13,15 We used the REP Census to identify all individuals who resided in Olmsted County on April 1, 2010, but we excluded those individuals who had not given permission to use their medical records for research.13,16,17
Definition of 20 selected chronic conditions
The diagnostic indices of the REP were searched electronically to identify the International Classification of Diseases, ninth revision (ICD-9) codes associated with any health care visit from April 1, 2005 through March 31, 2010 (5-year capture frame). We then pooled the ICD-9 codes to define the 20 groups of chronic conditions proposed by the US DHHS.3,4,18 The list of the 20 conditions and the corresponding ICD-9 codes used in this study are provided in Supplemental Table 1.3,18
To decrease the risk of false positive diagnoses, only persons who received two codes for a given condition separated by more than 30 days within the 5-year capture frame were considered prevalent for a given condition. We defined multimorbidity as the presence of 2 or more of the 20 conditions in the 5 years before April 1, 2010 (the prevalence date). To explore more complex patterns of multimorbidity, we also counted the number of people with 5 or more of the 20 conditions within the same time frame. We used the term multimorbidity rather than its predecessor, comorbidity, because we did not consider any specific index condition (the 20 conditions were all treated equally).5
Statistical Analyses
The point prevalence of each chronic condition and of multimorbidity was measured using April 1, 2010 as the prevalence date and using a 5-year capture frame (the 5 years preceding the prevalence date).19 We also computed the age-, sex-, and ethnicity-specific prevalence of multimorbidity defined as combinations of 2 or more chronic conditions, or of 5 or more chronic conditions. For analyses stratified by ethnic group, we used the three most common groups in our local population, Whites, Blacks, and Asians (as defined by the US Census). In addition, for each age and sex group, we described the most common combinations of 2 of the 20 conditions (dyads) or of 3 of the 20 conditions (triads). Dyads and triads were considered independently; therefore, a person with 3 of the 20 conditions was considered to have 3 distinct dyads and 1 triad. For example, a person affected by the triad of hyperlipidemia, hypertension, and diabetes generated three distinct dyads: hyperlipidemia and hypertension, hypertension and diabetes, and hyperlipidemia and diabetes.
We developed a heat map to show the co-occurrence of each pair of the 18 most common conditions using absolute frequencies. The top-left triangle of the map refers to women and the lower-right triangle refers to men. Hotter colors (darker orange) correspond with a higher frequency of co-occurrence (higher prevalence of a dyad). We also developed a second heat map to show the ratios of observed versus expected frequencies of co-occurrence (accounting for age in single-year increments). These ratios can be interpreted as cross-sectional measures of association.19 Dyads that were observed more frequently than expected, assuming independence, are shown in shades of orange, and dyads that were observed less frequently than expected are shown in shades of purple (observed vs. expected ratio < 1.0). These heat maps were intended to explore patterns and to suggest hypotheses rather than to test statistical associations. Therefore, concerns about multiple comparisons do not apply.
Prevalence was directly standardized to the 2010 total US population by age and by sex when appropriate to make comparisons (2010 US Census). Because this study covered the target population completely, and no sampling was involved, statistical tests may not be appropriate, and confidence intervals were not included in the tables.20-22
RESULTS
Description of the Olmsted County Population
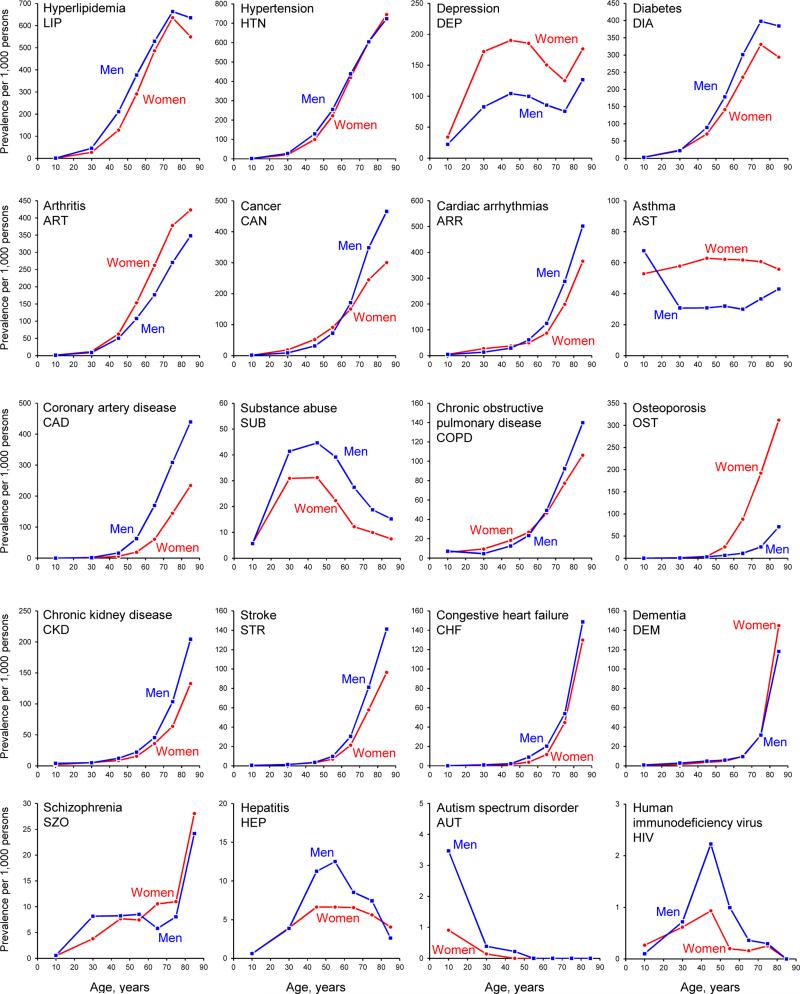
Overall, the REP infrastructure identified 142,992 Olmsted County, MN residents on April 1, 2010 compared with 144,248 individuals counted by the US Census on the same day.23 Of 142,992 residents, 138,858 provided Minnesota research authorization for medical record research (97.1%) and were included in our analyses. Figure 1 and Supplemental Table 2 show the age- and sex-specific prevalence of each of the 20 conditions considered separately. The graphs for each condition are presented in rows in descending order of frequency (by age- and sex-standardized prevalence).
Figure 1.
Age- and sex-specific prevalence (per 1,000 population) of the 20 chronic conditions considered separately. We used the same age groups as used in Tables 1 and 2 and in Supplemental Table 2; prevalence figures were plotted at the mid-point of each interval (e.g., at 10 years for 0-19 years). We used different scales for the y-axis to better show the age and sex patterns. Therefore, the magnitude of the differences cannot be compared across conditions (e.g., asthma vs. HIV). The 20 panels are presented by rows in decreasing order of frequency (by overall age- and sex-standardized prevalence).
Burden of multimorbidity by age, sex, and ethnicity
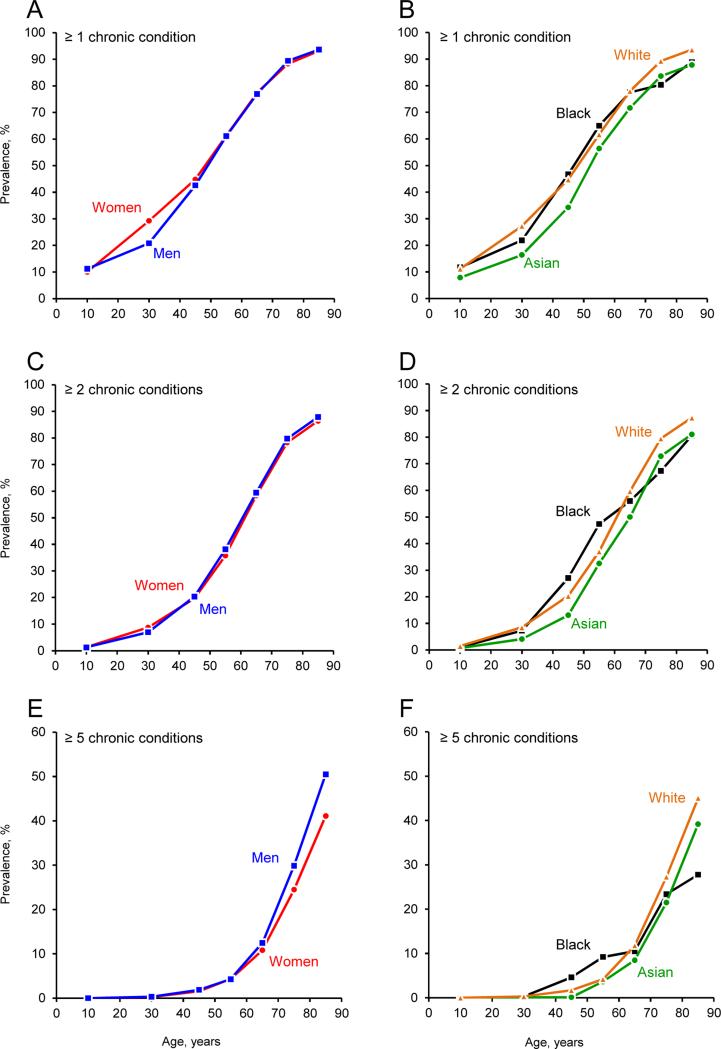
Table 1 shows the age- and sex-specific and the age-, sex-, and ethnicity-specific prevalence of 1 or more conditions, 2 or more conditions (multimorbidity), and 5 or more conditions. Multimorbidity increased steeply with older age and was similar in men and women (Figure 2; panel C). By contrast, the prevalence of people with 5 or more conditions was higher in men, especially at age 60 years or older (Figure 2, panel E). Even though the prevalence of multimorbidity increased steeply with older age, the absolute number of people with multimorbidity was larger for ages younger than 65 years (17,838) than at age 65 or older (13,606). This pattern was true for both men (8,436 vs. 5,961) and women (9,402 vs. 7,645).
Table 1.
Age-, sex-, and ethnicity-specific prevalence of multimorbidity in Olmsted County, MN (April 1, 2010)
| Men |
Women |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of chronic conditions |
Number of chronic conditions |
|||||||||
| Age (years) | Total N | None | ≥ 1 | ≥ 2a | ≥ 5b | Total N | None | ≥ 1 | ≥ 2a | ≥ 5b |
| All races | ||||||||||
| 0-19 | 19,316 | 17,158 (88.8) | 2,158 (11.2) | 244 (1.3) | 1 (<0.1) | 18,709 | 16,830 (90.0) | 1,879 (10.0) | 261 (1.4) | 1 (<0.1) |
| 20-39 | 18,028 | 14,273 (79.2) | 3,755 (20.8) | 1,258 (7.0) | 56 (0.3) | 21,051 | 14,893 (70.7) | 6,158 (29.3) | 1,839 (8.7) | 54 (0.3) |
| 40-49 | 8,978 | 5,155 (57.4) | 3,823 (42.6) | 1,829 (20.4) | 169 (1.9) | 9,650 | 5,325 (55.2) | 4,325 (44.8) | 1,902 (19.7) | 150 (1.6) |
| 50-59 | 9,036 | 3,517 (38.9) | 5,519 (61.1) | 3,445 (38.1) | 388 (4.3) | 9,944 | 3,859 (38.8) | 6,085 (61.2) | 3,557 (35.8) | 430 (4.3) |
| 60-69 | 5,506 | 1,269 (23.0) | 4,237 (77.0) | 3,271 (59.4) | 686 (12.5) | 6,248 | 1,411 (22.6) | 4,837 (77.4) | 3,646 (58.4) | 675 (10.8) |
| 70-79 | 3,359 | 356 (10.6) | 3,003 (89.4) | 2,678 (79.7) | 1,003 (29.9) | 3,921 | 457 (11.7) | 3,464 (88.3) | 3,069 (78.3) | 960 (24.5) |
| ≥ 80 | 1,903 | 121 (6.4) | 1,782 (93.6) | 1,672 (87.9) | 961 (50.5) | 3,209 | 222 (6.9) | 2,987 (93.1) | 2,773 (86.4) | 1,319 (41.1) |
| 0-64 | 58,419 | 40,916 (70.0) | 17,503 (30.0) | 8,436 (14.4) | 899 (1.5) | 62,838 | 41,798 (66.5) | 21,040 (33.5) | 9,402 (15.0) | 935 (1.5) |
| ≥ 65 | 7,707 | 933 (12.1) | 6,774 (87.9) | 5,961 (77.3) | 2,365 (30.7) | 9,894 | 1,199 (12.1) | 8,695 (87.9) | 7,645 (77.3) | 2,654 (26.8) |
| All ages | 66,126 | 41,849 (63.3) | 24,277 (36.7) | 14,397 (21.8) | 3,264 (4.9) | 72,732 | 42,997 (59.1) | 29,735 (40.9) | 17,047 (23.4) | 3,589 (4.9) |
| Standardizedc | ... | (61.6) | (38.4) | (23.4) | (5.6) | ... | (59.3) | (40.7) | (23.2) | (4.7) |
| Blacks | ||||||||||
| 0-19 | 1,535 | 1,356 (88.3) | 179 (11.7) | 18 (1.2) | 1 (0.1) | 1,487 | 1,312 (88.2) | 175 (11.8) | 14 (0.9) | 0 (0.0) |
| 20-39 | 1,133 | 920 (81.2) | 213 (18.8) | 73 (6.4) | 5 (0.4) | 1,201 | 903 (75.2) | 298 (24.8) | 97 (8.1) | 2 (0.2) |
| 40-49 | 384 | 211 (54.9) | 173 (45.1) | 98 (25.5) | 16 (4.2) | 351 | 181 (51.6) | 170 (48.4) | 101 (28.8) | 18 (5.1) |
| 50-59 | 262 | 104 (39.7) | 158 (60.3) | 115 (43.9) | 18 (6.9) | 226 | 67 (29.6) | 159 (70.4) | 116 (51.3) | 27 (11.9) |
| 60-69 | 87 | 24 (27.6) | 63 (72.4) | 44 (50.6) | 7 (8.0) | 113 | 21 (18.6) | 92 (81.4) | 68 (60.2) | 14 (12.4) |
| 70-79 | 48 | 9 (18.8) | 39 (81.3) | 35 (72.9) | 11 (22.9) | 59 | 12 (20.3) | 47 (79.7) | 37 (62.7) | 14 (23.7) |
| ≥ 80 | 14 | 0 (0.0) | 14 (100.0) | 12 (85.7) | 5 (35.7) | 22 | 4 (18.2) | 18 (81.8) | 17 (77.3) | 5 (22.7) |
| 0-64 | 3,358 | 2,606 (77.6) | 752 (22.4) | 325 (9.7) | 42 (1.3) | 3,326 | 2,474 (74.4) | 852 (25.6) | 367 (11.0) | 55 (1.7) |
| ≥ 65 | 105 | 18 (17.1) | 87 (82.9) | 70 (66.7) | 21 (20.0) | 133 | 26 (19.5) | 107 (80.5) | 83 (62.4) | 25 (18.8) |
| All ages | 3,463 | 2,624 (75.8) | 839 (24.2) | 395 (11.4) | 63 (1.8) | 3,459 | 2,500 (72.3) | 959 (27.7) | 450 (13.0) | 80 (2.3) |
| Standardizedc | ... | (62.4) | (37.6) | (23.4) | (5.0) | ... | (58.8) | (41.2) | (25.3) | (5.7) |
| Asians | ||||||||||
| 0-19 | 1,082 | 990 (91.5) | 92 (8.5) | 6 (0.6) | 0 (0.0) | 1,095 | 1,016 (92.8) | 79 (7.2) | 9 (0.8) | 0 (0.0) |
| 20-39 | 945 | 795 (84.1) | 150 (15.9) | 38 (4.0) | 0 (0.0) | 1,254 | 1,044 (83.3) | 210 (16.7) | 52 (4.1) | 2 (0.2) |
| 40-49 | 394 | 244 (61.9) | 150 (38.1) | 61 (15.5) | 0 (0.0) | 426 | 295 (69.2) | 131 (30.8) | 46 (10.8) | 1 (0.2) |
| 50-59 | 258 | 116 (45.0) | 142 (55.0) | 80 (31.0) | 2 (0.8) | 317 | 135 (42.6) | 182 (57.4) | 107 (33.8) | 19 (6.0) |
| 60-69 | 137 | 43 (31.4) | 94 (68.6) | 68 (49.6) | 19 (13.9) | 205 | 54 (26.3) | 151 (73.7) | 103 (50.2) | 10 (4.9) |
| 70-79 | 70 | 17 (24.3) | 53 (75.7) | 46 (65.7) | 14 (20.0) | 107 | 12 (11.2) | 95 (88.8) | 83 (77.6) | 24 (22.4) |
| ≥ 80 | 27 | 4 (14.8) | 23 (85.2) | 21 (77.8) | 11 (40.7) | 47 | 5 (10.6) | 42 (89.4) | 39 (83.0) | 18 (38.3) |
| 0-64 | 2,754 | 2,170 (78.8) | 584 (21.2) | 220 (8.0) | 13 (0.5) | 3,207 | 2,521 (78.6) | 686 (21.4) | 265 (8.3) | 25 (0.8) |
| ≥ 65 | 159 | 39 (24.5) | 120 (75.5) | 100 (62.9) | 33 (20.8) | 244 | 40 (16.4) | 204 (83.6) | 174 (71.3) | 49 (20.1) |
| All ages | 2,913 | 2,209 (75.8) | 704 (24.2) | 320 (11.0) | 46 (1.6) | 3,451 | 2,561 (74.2) | 890 (25.8) | 439 (12.7) | 74 (2.1) |
| Standardizedc | ... | (66.9) | (33.1) | (18.7) | (4.0) | ... | (66.4) | (33.6) | (19.4) | (4.0) |
| Whites | ||||||||||
| 0-19 | 14,781 | 13,054 (88.3) | 1,727 (11.7) | 203 (1.4) | 0 (0.0) | 14,302 | 12,797 (89.5) | 1,505 (10.5) | 223 (1.6) | 1 (<0.1) |
| 20-39 | 14,463 | 11,254 (77.8) | 3,209 (22.2) | 1,088 (7.5) | 48 (0.3) | 17,225 | 11,799 (68.5) | 5,426 (31.5) | 1,616 (9.4) | 46 (0.3) |
| 40-49 | 7,734 | 4,382 (56.7) | 3,352 (43.3) | 1,597 (20.6) | 145 (1.9) | 8,474 | 4,576 (54.0) | 3,898 (46.0) | 1,699 (20.0) | 128 (1.5) |
| 50-59 | 8,215 | 3,133 (38.1) | 5,082 (61.9) | 3,170 (38.6) | 359 (4.4) | 9,117 | 3,511 (38.5) | 5,606 (61.5) | 3,246 (35.6) | 367 (4.0) |
| 60-69 | 5,137 | 1,136 (22.1) | 4,001 (77.9) | 3,107 (60.5) | 649 (12.6) | 5,781 | 1,269 (22.0) | 4,512 (78.0) | 3,412 (59.0) | 638 (11.0) |
| 70-79 | 3,167 | 314 (9.9) | 2,853 (90.1) | 2,549 (80.5) | 963 (30.4) | 3,695 | 420 (11.4) | 3,275 (88.6) | 2,906 (78.6) | 909 (24.6) |
| ≥ 80 | 1,839 | 113 (6.1) | 1,726 (93.9) | 1,625 (88.4) | 943 (51.3) | 3,115 | 207 (6.6) | 2,908 (93.4) | 2,700 (86.7) | 1,289 (41.4) |
| 0-64 | 48,053 | 32,557 (67.8) | 15,496 (32.2) | 7,635 (15.9) | 817 (1.7) | 52,344 | 33,497 (64.0) | 18,847 (36.0) | 8,501 (16.2) | 826 (1.6) |
| ≥ 65 | 7,283 | 829 (11.4) | 6,454 (88.6) | 5,704 (78.3) | 2,290 (31.4) | 9,365 | 1,082 (11.6) | 8,283 (88.4) | 7,301 (78.0) | 2,552 (27.3) |
| All ages | 55,336 | 33,386 (60.3) | 21,950 (39.7) | 13,339 (24.1) | 3,107 (5.6) | 61,709 | 34,579 (56.0) | 27,130 (44.0) | 15,802 (25.6) | 3,378 (5.5) |
| Standardizedc | ... | (60.7) | (39.3) | (23.8) | (5.6) | ... | (58.3) | (41.7) | (23.6) | (4.7) |
Definition of multimorbidity is ≥ 2 of 20 conditions. In the total population of men and women combined, 31,444 people (22.6%) had multimorbidity. A total of 17,838 people had multimorbidity before age 65 years and 13,606 at age 65 years or older.
In the total population of men and women combined, 6,853 people (4.9%) had 5 or more conditions. A total of 1,834 people had 5 or more conditions before age 65 years and 5,019 at age 65 years or older.
Prevalence figures were directly standardized by age using the total US population with both sexes combined as standard (2010 Census). These standardized figures allow for direct comparisons across sex and ethnicity strata.
Figure 2.
Prevalence (per 100 population) of combinations of 1 or more, 2 or more (multimorbidity), or 5 or more of the 20 chronic conditions in men and women separately (panels A, C, and E), and stratified by ethnicity (panels B, D, and F). We used different scales for the y-axis in panels E and F to better show the differences.
The prevalence of multimorbidity through age 50-59 years was higher in Blacks than in Whites, and was lower in Asians than in Whites (Figure 2, panel D). Similarly, the prevalence of people with 5 or more conditions was higher in Blacks than in Whites and Asians through age 50-59 years, and was higher in Whites than in Blacks and Asians after age 60-69 years (Figure 2, panel F).
Most common dyads and triads by age and sex
Table 2 shows the most common dyads and triads of conditions by age and sex. The patterns of dyads and triads were different in men and women and varied with age. In the younger age groups (0-19, 20-39, and 40-49), dyads and triads including one mental condition (e.g., depression) were more common than in older age groups (50-59, 60-69, 70-79, and ≥ 80). Men experienced more dyads and triads including cancer than women. By contrast, women experienced more dyads or triads including arthritis. Dyads or triads including depression were more common in women than men in the age groups 50-59 and 60-69 years.
Table 2.
Most prevalent dyads and triads of chronic conditions in persons living in Olmsted County, MN (April 1, 2010)
| Dyad |
Triad |
|||||||
|---|---|---|---|---|---|---|---|---|
| Age (years) ranka | Men |
Women |
Men |
Women |
||||
| Combinationb | n (%)c | Combinationb | n (%)c | Combinationb | n (%)c | Combinationb | n (%)c | |
| 0 – 19 | ||||||||
| 1 | DEP - AST | 63 (0.3) | DEP - AST | 83 (0.4) | DEP - AST - SUB | 6 (<0.1) | DEP - AST - SUB | 13 (0.1) |
| 2 | DEP - SUB | 53 (0.3) | DEP - SUB | 74 (0.4) | ... | ... | ... | ... |
| 3 | AST - COPD | 44 (0.2) | AST - COPD | 30 (0.2) | ... | ... | ... | ... |
| 4 | ARR - AST | 14 (0.1) | DEP - ARR | 19 (0.1) | ... | ... | ... | ... |
| 5 | HTN - CKD | 12 (0.1) | AST - SUB | 18 (0.1) | ... | ... | ... | ... |
| 20 – 39 | ||||||||
| 1 | DEP - SUB | 429 (2.4) | DEP - SUB | 471 (2.2) | LIP - HTN - DIA | 66 (0.4) | DEP - AST - SUB | 86 (0.4) |
| 2 | LIP - HTN | 181 (1.0) | DEP - AST | 437 (2.1) | DEP - SUB - SZO | 48 (0.3) | LIP - DEP - DIA | 69 (0.3) |
| 3 | LIP - DIA | 178 (1.0) | LIP - DEP | 211 (1.0) | HTN - DEP - SUB | 47 (0.3) | DEP - ARR - SUB | 49 (0.2) |
| 4 | LIP - DEP | 137 (0.8) | DEP - ARR | 198 (0.9) | LIP - HTN - DEP | 40 (0.2) | DEP - ARR - AST | 48 (0.2) |
| 5 | HTN - DIA | 108 (0.6) | DEP - DIA | 159 (0.8) | LIP - DEP - DIA | 39 (0.2) | LIP - HTN - DEP | 42 (0.2) |
| 40 – 49 | ||||||||
| 1 | LIP - HTN | 620 (6.9) | LIP - DEP | 398 (4.1) | LIP - HTN - DIA | 285 (3.2) | LIP - HTN - DIA | 198 (2.1) |
| 2 | LIP - DIA | 570 (6.3) | LIP - HTN | 395 (4.1) | LIP - HTN - DEP | 129 (1.4) | LIP - DEP - DIA | 141 (1.5) |
| 3 | HTN - DIA | 356 (4.0) | LIP - DIA | 385 (4.0) | LIP - DEP - DIA | 128 (1.4) | LIP - HTN - DEP | 139 (1.4) |
| 4 | LIP - DEP | 315 (3.5) | HTN - DEP | 291 (3.0) | HTN - DEP - DIA | 84 (0.9) | HTN - DEP - DIA | 104 (1.1) |
| 5 | DEP - SUB | 237 (2.6) | HTN - DIA | 275 (2.8) | LIP - HTN - CAD | 79 (0.9) | LIP - DEP - ART | 72 (0.7) |
| 50 – 59 | ||||||||
| 1 | LIP - HTN | 1,555 (17.2) | LIP - HTN | 1,258 (12.7) | LIP - HTN - DIA | 743 (8.2) | LIP - HTN - DIA | 614 (6.2) |
| 2 | LIP - DIA | 1,235 (13.7) | LIP - DIA | 985 (9.9) | LIP - HTN - CAD | 330 (3.7) | LIP - HTN - ART | 348 (3.5) |
| 3 | HTN - DIA | 892 (9.9) | HTN - DIA | 787 (7.9) | LIP - HTN - ART | 272 (3.0) | LIP - HTN - DEP | 340 (3.4) |
| 4 | LIP - CAD | 535 (5.9) | LIP - DEP | 738 (7.4) | LIP - HTN - DEP | 243 (2.7) | LIP - DEP - DIA | 286 (2.9) |
| 5 | LIP - ART | 485 (5.4) | LIP - ART | 637 (6.4) | LIP - DIA - CAD | 232 (2.6) | LIP - DIA - ART | 256 (2.6) |
| 60 – 69 | ||||||||
| 1 | LIP - HTN | 1,804 (32.8) | LIP - HTN | 1,821 (29.1) | LIP - HTN - DIA | 993 (18.0) | LIP - HTN - DIA | 891 (14.3) |
| 2 | LIP - DIA | 1,337 (24.3) | LIP - DIA | 1,175 (18.8) | LIP - HTN - CAD | 628 (11.4) | LIP - HTN - ART | 669 (10.7) |
| 3 | HTN - DIA | 1,156 (21.0) | HTN - DIA | 1,058 (16.9) | LIP - DIA - CAD | 432 (7.8) | LIP - DIA - ART | 422 (6.8) |
| 4 | LIP - CAD | 856 (15.5) | LIP - ART | 1,000 (16.0) | LIP - HTN - ART | 430 (7.8) | HTN - DIA - ART | 387 (6.2) |
| 5 | HTN - CAD | 673 (12.2) | HTN - ART | 914 (14.6) | LIP - HTN - ARR | 398 (7.2) | LIP - HTN - DEP | 363 (5.8) |
| 6 | LIP - ART | 634 (11.5) | LIP - DEP | 577 (9.2) | HTN - DIA - CAD | 372 (6.8) | LIP - HTN - CAN | 334 (5.3) |
| 7 | LIP - CAN | 577 (10.5) | LIP - CAN | 552 (8.8) | LIP - HTN - CAN | 350 (6.4) | LIP - DEP - ART | 265 (4.2) |
| 8 | HTN - ART | 551 (10.0) | DIA - ART | 506 (8.1) | LIP - DIA - ART | 316 (5.7) | LIP - HTN - CAD | 256 (4.1) |
| 9 | LIP - ARR | 514 (9.3) | HTN - DEP | 481 (7.7) | HTN - DIA - ART | 292 (5.3) | LIP - HTN - ARR | 253 (4.0) |
| 10 | HTN - ARR | 487 (8.8) | HTN - CAN | 455 (7.3) | LIP - ARR - CAD | 286 (5.2) | LIP - DEP - DIA | 248 (4.0) |
| 70 – 79 | ||||||||
| 1 | LIP - HTN | 1,605 (47.8) | LIP - HTN | 1,823 (46.5) | LIP - HTN - DIA | 880 (26.2) | LIP - HTN - DIA | 895 (22.8) |
| 2 | LIP - DIA | 1,110 (33.0) | LIP - DIA | 1,068 (27.2) | LIP - HTN - CAD | 751 (22.4) | LIP - HTN - ART | 817 (20.8) |
| 3 | HTN - DIA | 1,039 (30.9) | HTN - ART | 1,058 (27.0) | LIP - HTN - ARR | 618 (18.4) | LIP - HTN - ARR | 498 (12.7) |
| 4 | LIP - CAD | 943 (28.1) | HTN - DIA | 1,050 (26.8) | LIP - HTN - CAN | 598 (17.8) | LIP - HTN - CAN | 489 (12.5) |
| 5 | LIP - CAN | 840 (25.0) | LIP - ART | 1,048 (26.7) | LIP - HTN - ART | 514 (15.3) | HTN - DIA - ART | 468 (11.9) |
| 6 | HTN - CAD | 816 (24.3) | LIP - CAN | 690 (17.6) | LIP - DIA - CAD | 474 (14.1) | LIP - DIA - ART | 462 (11.8) |
| 7 | LIP - ARR | 772 (23.0) | HTN - CAN | 627 (16.0) | LIP - ARR - CAD | 469 (14.0) | LIP - HTN - CAD | 449 (11.5) |
| 8 | HTN - CAN | 746 (22.2) | HTN - ARR | 610 (15.6) | HTN - ARR - CAD | 435 (13.0) | HTN - ART - ARR | 338 (8.6) |
| 9 | HTN - ARR | 733 (21.8) | LIP - ARR | 601 (15.3) | HTN - DIA - CAD | 428 (12.7) | LIP - HTN - OST | 321 (8.2) |
| 10 | LIP - ART | 697 (20.8) | DIA - ART | 561 (14.3) | LIP - DIA - ARR | 406 (12.1) | LIP - ART - ARR | 312 (8.0) |
| ≥ 80 | ||||||||
| 1 | LIP - HTN | 1,003 (52.7) | LIP - HTN | 1,509 (47.0) | LIP - HTN - CAD | 614 (32.3) | LIP - HTN - ART | 721 (22.5) |
| 2 | HTN - ARR | 798 (41.9) | HTN - ART | 1,107 (34.5) | LIP - HTN - ARR | 595 (31.3) | LIP - HTN - ARR | 682 (21.3) |
| 3 | LIP - CAD | 708 (37.2) | HTN - ARR | 1,006 (31.3) | LIP - HTN - CAN | 517 (27.2) | LIP - HTN - DIA | 663 (20.7) |
| 4 | HTN - CAD | 701 (36.8) | HTN - DIA | 846 (26.4) | LIP - HTN - DIA | 505 (26.5) | LIP - HTN - CAD | 576 (17.9) |
| 5 | HTN - CAN | 689 (36.2) | LIP - ART | 833 (26.0) | HTN - ARR - CAD | 494 (26.0) | HTN - ART - ARR | 529 (16.5) |
| 6 | LIP - ARR | 675 (35.5) | HTN - OST | 780 (24.3) | LIP - ARR - CAD | 487 (25.6) | LIP - HTN - CAN | 481 (15.0) |
| 7 | HTN - DIA | 631 (33.2) | HTN - CAN | 773 (24.1) | HTN - CAN - ARR | 434 (22.8) | LIP - HTN - OST | 460 (14.3) |
| 8 | LIP - CAN | 622 (32.7) | LIP - ARR | 748 (23.3) | LIP - HTN - ART | 389 (20.4) | HTN - DIA - ART | 432 (13.5) |
| 9 | ARR - CAD | 573 (30.1) | LIP - DIA | 715 (22.3) | LIP - CAN - ARR | 375 (19.7) | HTN - ARR - CAD | 423 (13.2) |
| 10 | LIP - DIA | 569 (29.9) | HTN - CAD | 671 (20.9) | LIP - CAN - CAD | 369 (19.4) | HTN - ART - CAN | 398 (12.4) |
| All ages | ||||||||
| 1 | LIP - HTN | 6,769 (10.2) | LIP - HTN | 6,912 (9.5) | LIP - HTN - DIA | 3,472 (5.3) | LIP - HTN - DIA | 3,304 (4.5) |
| 2 | LIP - DIA | 5,000 (7.6) | LIP - DIA | 4,485 (6.2) | LIP - HTN - CAD | 2,416 (3.7) | LIP - HTN - ART | 2,625 (3.6) |
| 3 | HTN - DIA | 4,182 (6.3) | HTN - DIA | 4,097 (5.6) | LIP - HTN - ARR | 1,912 (2.9) | LIP - HTN - ARR | 1,664 (2.3) |
| 4 | LIP - CAD | 3,194 (4.8) | HTN - ART | 3,811 (5.2) | LIP - HTN - ART | 1,671 (2.5) | LIP - DIA - ART | 1,567 (2.2) |
| 5 | HTN - CAD | 2,633 (4.0) | LIP - ART | 3,689 (5.1) | LIP - HTN - CAN | 1,632 (2.5) | HTN - DIA - ART | 1,567 (2.2) |
| 6 | LIP - ARR | 2,465 (3.7) | LIP - DEP | 2,616 (3.6) | LIP - DIA - CAD | 1,522 (2.3) | LIP - HTN - CAN | 1,479 (2.0) |
| 7 | LIP - CAN | 2,452 (3.7) | HTN - ARR | 2,350 (3.2) | LIP - ARR - CAD | 1,414 (2.1) | LIP - HTN - DEP | 1,456 (2.0) |
| 8 | LIP - ART | 2,446 (3.7) | HTN - DEP | 2,301 (3.2) | HTN - DIA - CAD | 1,338 (2.0) | LIP - HTN - CAD | 1,433 (2.0) |
| 9 | HTN - ARR | 2,444 (3.7) | LIP - CAN | 2,218 (3.0) | HTN - ARR - CAD | 1,304 (2.0) | HTN - ART - ARR | 1,146 (1.6) |
| 10 | HTN - ART | 2,202 (3.3) | HTN - CAN | 2,180 (3.0) | LIP - DIA - ARR | 1,198 (1.8) | LIP - DEP - DIA | 1,021 (1.4) |
Rank order from the most frequent to the least frequent dyad or triad. For the younger age groups (through age 59 years), we reported the 5 most frequent combinations; for the older age groups (60 years and older), we reported the 10 most frequent combinations.
Definition of acronyms in order of frequency: LIP = hyperlipidemia; HTN = hypertension; DEP = depression; DIA = diabetes; ART = arthritis; CAN = cancer; ARR = cardiac arrhythmias; AST = asthma; CAD = coronary artery disease; SUB = substance abuse disorders; COPD = chronic obstructive pulmonary disease; OST = osteoporosis; CKD = chronic kidney disease; STR = stroke; CHF = congestive heart failure; DEM = dementia; SZO = schizophrenia; HEP = hepatitis; AUT = autism spectrum disorder; and HIV = human immunodeficiency virus.
Prevalence figures based on less than 5 subjects are not shown (replaced by a “...”).
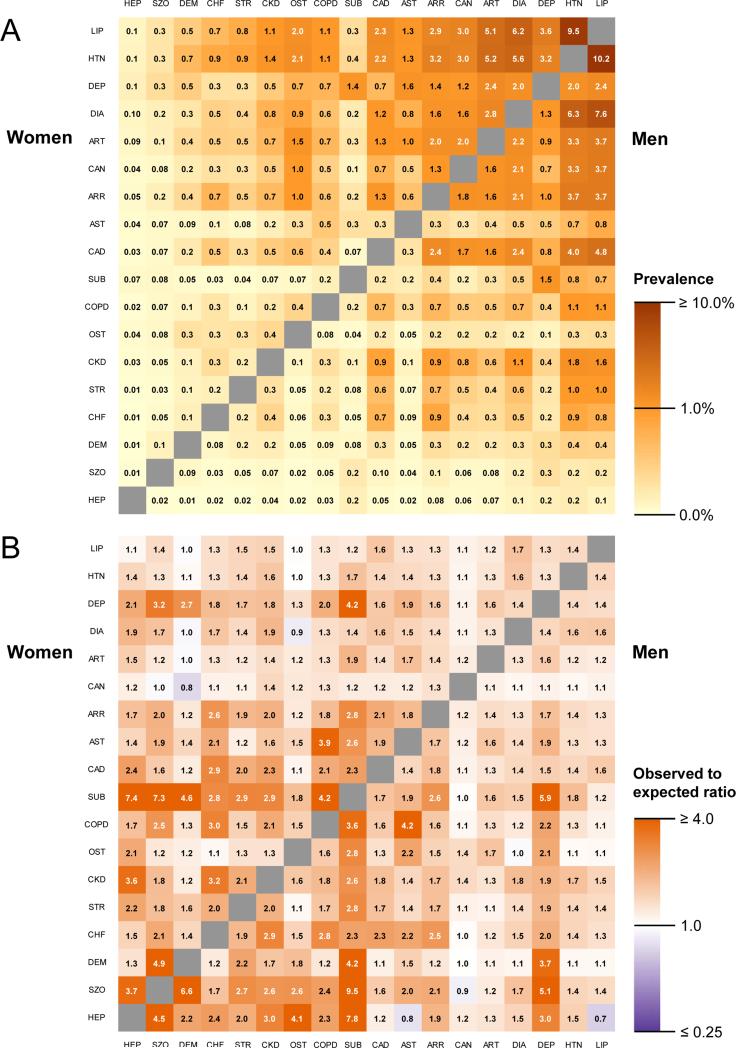
Figure 3, panel A shows a heat map of the frequency of co-occurrence of each pair of 18 conditions in men and women separately (dyads). Autism spectrum disorder and human immunodeficiency virus infection were excluded because they were uncommon in the overall population. Although the overall patterns of co-occurrence were similar in men and women, a visual inspection of the map reveals that women had more dyads including asthma, arthritis, dementia, osteoporosis, and depression (darker orange). Men had more dyads including coronary artery disease, cancer, and substance abuse disorders. These differences across sex were not tested statistically.
Figure 3.
Panel A, heat map of the burden of multimorbidity in terms of absolute frequency. The number in each square is the percent of co-occurrence in the overall population (all ages combined). The 18 conditions are listed on the X and Y axes of both panels in order of frequency. Panel B, heat map of the risk ratios obtained by dividing the observed frequency of each pair of 18 conditions by the frequency expected assuming independent probabilities. The ratios provide a cross-sectional measure of association. Autism spectrum disorder and human immunodeficiency virus infection were excluded in both panels because they were uncommon in the overall population. The color scale used for each panel is shown on the right. Values for men are shown in the lower right triangle, and values for women are shown in the upper left triangle. Definition of acronyms or abbreviations in order of frequency: LIP = hyperlipidemia; HTN = hypertension; DEP = depression; DIA = diabetes; ART = arthritis; CAN = cancer; ARR = cardiac arrhythmias; AST = asthma; CAD = coronary artery disease; SUB = substance abuse disorders; COPD = chronic obstructive pulmonary disease; OST = osteoporosis; CKD = chronic kidney disease; STR = stroke; CHF = congestive heart failure; DEM = dementia; SZO = schizophrenia; HEP = hepatitis.
Figure 3, panel B shows a heat map of a risk ratio obtained by dividing the observed frequency of co-occurrence of each pair of 18 conditions (shown in panel A) by the expected frequency of co-occurrence assuming independent probabilities (and accounting for age in single-year increments). For example, increased risk ratios (darker orange squares) were observed for substance abuse disorders (including drugs and alcohol but not smoking) in combination with schizophrenia, hepatitis, depression, dementia, stroke, osteoporosis, chronic obstructive pulmonary disease, and cardiac arrhythmias. Reduced risk ratios (purple squares) were observed for dementia and cancer and diabetes and osteoporosis in women, and for hepatitis and asthma, hepatitis and hyperlipidemia, and schizophrenia and cancer in men.
DISCUSSION
Discussion of principal findings
In our study, multimorbidity was common, increased steeply with older age, and was similar in men and women overall. However, more men than women had 5 or more conditions. Despite the traditional focus on multimorbidity in the older adult population,5,8-11 the absolute number of people affected by multimorbidity was higher in persons younger than 65 years than in persons 65 years or older. Multimorbidity was also higher in Blacks than in Whites, and in Whites than in Asians. The most common dyads and triads of conditions varied with age and were different in men and women. We developed a heat map for the co-occurrence of dyads using absolute frequencies and a heat map for the co-occurrence of dyads relative to the expected frequency. Our medical-records based findings provide a unique picture of multimorbidity in a geographically defined US population that emphasizes age, sex, and ethnic differences. Therefore, our findings have implications for clinical practice and for etiologic research both in the local community and at the national and international level.
Some of our findings deserve further comment and may suggest important directions for future research. First, although the prevalence of one or more, or of two or more conditions was similar in men and women, the prevalence of 5 or more conditions was higher in men older than age 60 years. This pattern may be explained by a higher risk to develop more complex combinations of multimorbidity in men than in women or by an improved survival in men with more complex multimorbidity. For example, for men living at home, the presence of a surviving spouse may improve care and thus increase their survival. By contrast, an older woman with 5 or more conditions is less likely to receive care from a surviving husband. Second, although the prevalence of multimorbidity increased with age, the absolute number of persons affected by multimorbidity was higher in persons younger than age 65 years. This pattern has several implications. From a clinical practice perspective, physicians involved in primary care need to consider the co-occurrence of conditions at all ages, not just in the geriatric population. In addition, multimorbidity among younger persons may be particularly important as a target for preventive interventions. Both the causes and the consequences of multimorbidity may be different depending on the age at which it develops. The timing of preventive interventions may be crucial.
Third, we observed some important ethnic differences. It remains unclear to which extent these differences are related to a different risk of developing multimorbidity, to a different probability of being diagnosed and coded in our system, or to a different survival after multimorbidity has developed. We plan to conduct further studies to address these unresolved questions. Fourth, although the overall prevalence of two or more conditions was similar in men and women, some combinations (dyads or triads) were more common in men and some in women. These dimorphic patterns may result from sex related differences such as genetic differences (e.g., XX vs. XY chromosomes), hormonal differences (e.g., effects of estrogen or testosterone), or reproductive differences (e.g., pregnancies or menopause). In addition, they may result from gender related differences in personality or behavior (subjective component of gender) or from differences due to social, cultural, and legal factors (societal component of gender). 24,25 The effects of sex and gender on multimorbidity are an important area for future research.
Some of the most common dyads or triads observed in the age groups 60-69, 70-79, or ≥ 80 years involved hyperlipidemia, hypertension, diabetes, and coronary artery disease. These combinations were expected given the high frequency of the individual conditions and have already been recognized in clinical practice. 26,27 Some of these conditions represent various elements of linked disease processes that are already managed synergistically, and there is less need for clinical transformation or changes in clinical guidelines.26,27 However, some other combinations of conditions are not yet widely recognized, and their recognition may prompt a transformation of our care delivery practices. Some of these combinations were different in men and women; for example, dyads and triads including arthritis and osteoporosis were more common in women and dyads and triads including cancer were more common in men.
The combinations of some less common conditions may be clinically important or may have research implications. For example, arrhythmia and osteoporosis occurred together in 0.2% of men and 1.0% of women (Figure 3, panel A). This co-occurrence may have a mechanistic explanation mediated by drug use (increased risk of atrial fibrillation in subjects treated with bisphosphonates, particularly with intravenous preparations).28 Recognition of this association may help in guiding approaches to modifing the treatment strategy for osteoporosis in some patients.
Our results for dyads and triads in the population younger than age 60 years are particularly interesting because clinical records-based data are limited for this segment of the US population.7 In the age groups 0-19, 20-39, 40-49, and 50-59 years, many of the most common dyads and triads included mental disorders. For example, the dyad of depression and substance abuse disorders in men had a prevalence of 0.3% at age 0-19, 2.4% at age 20-39, and 2.6% at age 40-49 years. The prevalence for women was 0.4% at age 0-19 and 2.2% at age 20-39 (Table 2). All of the 5 most common dyads and the 5 most common triads in the age group 20-39 years included depression in women but not in men. The triad including depression, substance abuse disorders, and asthma was the most common in men and women age 0-19 years. The second most common triad in men age 20-39 was depression, substance abuse disorders, and schizophrenia (0.3%). Other authors have emphasized that mental disorders are common in people younger than age 60 years who have other physical chronic conditions.29-32
Figure 3, panel A is useful to represent the burden of multimorbidity in terms of absolute frequency. Thus, the hotter squares (darker orange) indicate the dyads of conditions that community physicians or geriatricians encounter more frequently in practice. These patterns may inform medical practice and the delivery of care; however, they may be misleading if used to understand the mechanisms of developing multimorbidity. Two etiologically unrelated conditions will co-occur simply because they are common (joint probability of two independent events). These descriptive patterns in Olmsted County can be compared with the patterns observed in other localized populations in the United States or worldwide to investigate similarities or differences possibly related to environmental, genetic, socioeconomic, or cultural differences. In addition, these patterns can be used locally for health needs assessments (e.g., Olmsted County, Minnesota Community Health Needs Assessment: http://www.co.olmsted.mn.us/OCPHS/reports/Documents/Community%20Health%20Needs%20Assessment%202013.pdf), for surveillance (e.g., study of trends over time or assessment of the impact of community interventions), and for targeting preventive efforts and clinical services to the local community. Therefore, we envision that our findings will have an impact both locally and more generally at the national and international level.
The heat map of Figure 3, panel B shows the co-occurrence of conditions above and beyond what is expected simply by their frequency. This map shows hotter squares (orange) for pairs of conditions that co-occur more frequently than expected, and indicate diseases that may be causally related (e.g., hypertension and stroke) or that may share a common cause or pathogenetic mechanism (e.g., stroke and congestive heart failure). Even though our analyses were cross-sectional, and we did not explore which one of two conditions in a given dyad came first, our findings are useful for generating hypotheses. Some of the hot squares have been previously reported or are clinically predictable (e.g., the association of dementia with depression, of asthma with chronic obstructive pulmonary disease, or of substance abuse disorders with hepatitis or with chronic obstructive pulmonary disease). Some other hot squares are less predictable and may prompt the design of studies to test new hypotheses (e.g., the association of chronic kidney disease with hepatitis or with substance abuse disorders). Interestingly, cancer and dementia, and diabetes and osteoporosis occurred together less frequently than expected in women, and hepatitis and asthma, hepatitis and hyperlipidemia, and schizophrenia and cancer in men (purple squares). However, the analyses shown in Figure 3, panel B should not be interpreted as hypotheses testing and some of the findings may simply be due to chance.
Comparison with other studies
A large number of individual studies and reviews regarding multimorbidity have been published both in Europe and the United States.5,8-11 However, comparisons across studies remain problematic because there is limited consensus on the number and type of conditions to be considered, the source of diagnoses (interview vs. medical records), and the window of capture for chronic diseases (within 1 year, 2 years, 5 years, or lifelong before the prevalence date). We elected to compare our study with two other studies that were similarly based on medical records data (specifically, billing codes) and that used comparable definitions of multimorbidity.5,11
First, we compared our prevalence of multimorbidity for people aged 65 and older with the prevalence reported using national data from the Centers for Medicare and Medicaid Services (CMS).5 To improve comparability, we re-calculated our prevalence figures restricting the list to 15 conditions, restricting the window of capture of morbidities to 1 year (April 1, 2009 – March 31, 2010), and accepting all subjects who received at least one code for each specific condition as was done in the CMS study. We initially compared the prevalence of the conditions considered separately in Olmsted County to the CMS data. Supplemental Table 3 shows the results for 15 conditions. For some of the conditions, the prevalence in persons 65 or older was comparable (hypertension, hyperlipidemia, diabetes, arthritis, depression, chronic kidney disease, osteoporosis, chronic obstructive pulmonary disease, asthma, and stroke). For some conditions, our estimates were lower despite the use of similar codes (coronary artery disease and heart failure). The prevalence of dementia was lower in our population than in the CMS data even though the CMS study included only Alzheimer's disease and we also included other types of dementia. It remains unclear whether the lower prevalence of some conditions in Olmsted County may be caused by some residual methodological differences between the two studies, or it may be a genuine finding. It is conceivable that differences in socioeconomic factors, access to medical care, and local health promotion and preventive initiatives may explain part of these differences. For other conditions, the codes used in the two studies were different and the prevalence was not comparable (cardiac arrhythmias and cancer). These comparisons emphasize the importance of reaching consensus on the specific list of ICD-9 codes used to define each condition.3,5
Next, we compared the prevalence of multimorbidity. The findings in Olmsted County were similar to the findings from CMS despite the differences observed for some of the conditions considered separately. The prevalence of multimorbidity was 62.0% nationally and 62.4% in our study at ages 65-74 years, was 75.7% nationally and 74.6% in our study at ages 75-84 years, and was 81.5% nationally and 76.2% in our study at ages 85 years or older.5 The similar prevalence for older persons in our study and in the national study suggests that our findings for younger persons (< 65 years) may also be generalizable to the US population. Our findings may be particularly useful for this segment of the population, because clinical-records based data about multimorbidity in younger age groups are limited in the United States.7 In the absence of more general data at the national level, our findings may be used to guide decisions in clinical practice or public health.
Our findings were also comparable to those from a recent study in Scotland, UK. In the UK study, multimorbidity increased steeply with older age and was higher in women than in men overall.11,33-35 Despite some important differences in the number of conditions considered and in the capture frame (5 years in our study vs. a variable frame of 1 year, 5 years, or lifelong in the UK study), our findings were comparable to the UK findings. Both the UK study and our study showed that the absolute number of people with multimorbidity was greater in persons younger than 65 years than in persons 65 or older, although older people may be more likely to experience functional consequences from multimorbidity.36
Strengths and Limitations
Strengths of our study include access to medical record data (specifically, billing codes) on all conditions for an entire population, across age, sex, and ethnic groups regardless of insurance status, socioeconomic status, and care delivery setting. Because data were generated prospectively as part of routine medical care, patients were not involved in remembering or correctly reporting medical events or diagnoses. Medical records data are often difficult to obtain in the United States because there is no centralized health care surveillance system. In 2013, Wallace and Salive recognized that in the United States, there are no comprehensive, clinical records-based data sets for all ages and for all regions.7
One limitation of our study, which is shared with many other similar studies, is the limited validity of ICD-9 codes. Previous REP studies have shown that codes may be assigned in error, and manual review of the medical records is often needed to ascertain whether a person truly has the disease or condition of interest.37-41 We limited false positive diagnoses by requiring at least two diagnostic codes separated by more than 30 days for each condition. Another limitation was the cross-sectional nature of our analyses. Thus, we were unable to study the chronological directionality of dyads and triads of conditions. Our aims were descriptive and exploratory rather than hypothesis testing. Finally, our population included a lower percent of Black and Asians than other populations in the United States. 15
CONCLUSION
We described the prevalence of 20 chronic conditions across all age groups, in men and women separately, and across ethnic groups in the Olmsted County population. Multimorbidity is common in the general population; it increases steeply with age, has different patterns in men and women, and varies by ethnicity. Our findings have implications both for clinical practice and for etiologic research. On the one hand, our findings may inform the transition from single diagnosis-based guidelines to patient-based guidelines that also reflect differences in men and women.1,2,4 On the other hand, our findings may indicate areas in which to focus etiologic research on causes and consequences of chronic conditions.28
Supplementary Material
AKNOWLEDGMENTS
We thank Ms. Carol J. Greenlee for her assistance in typing and formatting the manuscript.
Financial Support: This study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Boyd was supported by the Paul Beeson Career Development Award Program (NIA K23 AG032910), the John A. Hartford Foundation, Atlantic Philanthropies, the Starr Foundation, and an anonymous donor.
Abbreviations and Acronyms
- ARR
cardiac arrhythmias
- ART
arthritis
- AST
asthma
- AUT
autism spectrum disorder
- CAD
coronary artery disease
- CAN
cancer
- CCC
Clinical Classification Codes
- CHF
congestive heart failure
- CKD
chronic kidney disease
- CMS
Centers for Medicare and Medicaid Services
- COPD
chronic obstructive pulmonary disease
- DEM
dementia
- DEP
depression
- DIA
diabetes
- HEP
hepatitis
- HIV
human immunodeficiency virus
- HTN
hypertension
- ICD-9
International Classification of Diseases, Ninth Revision
- LIP
hyperlipidemia
- OST
osteoporosis
- REP
Rochester Epidemiology Project
- STR
stroke
- SUB
substance abuse disorders
- SZO
schizophrenia
- US-DHHS
United States Department of Health and Human Services
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest/Financial Disclosures: The authors have no conflict of interest or financial disclosures to report.
REFERENCES
- 1.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716–724. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- 2.Hughes LD, McMurdo MET, Guthrie B. Guidelines for people not for diseases: the challenges of applying UK clinical guidelines to people with multimorbidity. Age Ageing. 2014;42(1):62–69. doi: 10.1093/ageing/afs100. [DOI] [PubMed] [Google Scholar]
- 3.Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis. 2013;10:E66. doi: 10.5888/pcd10.120239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services . Multiple Chronic Conditions - A Strategic Framework: Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions. Washington, D.C.: Dec, 2010. [Google Scholar]
- 5.Salive ME. Multimorbidity in Older Adults. Epidemiol Rev. 2013;35(1):75–83. doi: 10.1093/epirev/mxs009. [DOI] [PubMed] [Google Scholar]
- 6.Parekh AK, Goodman RA, Gordon C, Koh HK. Managing multiple chronic conditions: a strategic framework for improving health outcomes and quality of life. Public Health Rep. 2011;126(4):460–471. doi: 10.1177/003335491112600403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallace RB, Salive ME. The dimensions of multiple chronic conditions: where do we go from here? A commentary on the Special Issue of Preventing Chronic Disease. Prev Chronic Dis. 2013;10:E59. doi: 10.5888/pcd10.130104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic diseases--a systematic review on existing multimorbidity indices. J Geronotol A Biol Sci Med Sci. 2011;66(3):301–311. doi: 10.1093/gerona/glq208. [DOI] [PubMed] [Google Scholar]
- 9.Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–439. doi: 10.1016/j.arr.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Prados-Torres A, Calderon-Larranaga A, Hancco-Saavedra J, Poblador-Plou B, van den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67(3):254–266. doi: 10.1016/j.jclinepi.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 11.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 12.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., 3rd History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am J Epidemiol. 2011;173(9):1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41(6):1614–1624. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yawn BP, Yawn RA, Geier GR, Xia Z, Jacobsen SJ. The impact of requiring patient authorization for use of data in medical records research. J Fam Pract. 1998;47(5):361–365. [PubMed] [Google Scholar]
- 17.Jacobsen SJ, Xia Z, Campion ME, et al. Potential effect of authorization bias on medical record research. Mayo Clin Proc. 1999;74(4):330–338. doi: 10.4065/74.4.330. [DOI] [PubMed] [Google Scholar]
- 18.Cohen JW, Cohen SB, Banthin JS. The medical expenditure panel survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009;47(7 suppl 1):S44–50. doi: 10.1097/MLR.0b013e3181a23e3a. [DOI] [PubMed] [Google Scholar]
- 19.Porta MS, International Epidemiological Association . A Dictionary of Epidemiology. 5th ed. Oxford University Press; Oxford; New York: 2008. [Google Scholar]
- 20.Anderson DW, Mantel N. On epidemiologic surveys. Am J Epidemiol. 1983;118(5):613–619. doi: 10.1093/oxfordjournals.aje.a113671. [DOI] [PubMed] [Google Scholar]
- 21.Deming WE. Boundaries of Statistical Inference. In: Smith H, Johnson NL, editors. New Developments in Survey Sampling. Wiley-Interscience; New York: 1969. pp. 652–670. [Google Scholar]
- 22.Rocca WA, Cha RH, Waring SC, Kokmen E. Incidence of dementia and Alzheimer's disease: a reanalysis of data from Rochester, Minnesota, 1975-1984. Am J Epidemiol. 1998;148(1):51–62. doi: 10.1093/oxfordjournals.aje.a009560. [DOI] [PubMed] [Google Scholar]
- 23.US Census Bureau [June 16, 2014];US Decennial Census. 2010 http://www.census.gov/2010census/data/.
- 24.Rocca WA, Mielke MM, Vemuri P, Miller VM. Sex and gender differences in the causes of dementia: A narrative review. Maturitas. 2014 doi: 10.1016/j.maturitas.2014.05.008. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.IOM (Institute of Medicine) Women's Health Research: Progress, Pitfalls, and Promise. The National Academies Press; Washington, DC: 2010. [PubMed] [Google Scholar]
- 26.Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29(3):725–731. doi: 10.2337/diacare.29.03.06.dc05-2078. [DOI] [PubMed] [Google Scholar]
- 27.Pentakota SR, Rajan M, Fincke BG, et al. Does diabetes care differ by type of chronic comorbidity?: An evaluation of the Piette and Kerr framework. Diabetes Care. 2012;35(6):1285–1292. doi: 10.2337/dc11-1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharma A, Einstein AJ, Vallakati A, et al. Risk of atrial fibrillation with use of oral and intravenous bisphosphonates. Am J Card. 2014;113(11):1815–1821. doi: 10.1016/j.amjcard.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 29.Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry. 2007;29(5):409–416. doi: 10.1016/j.genhosppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 30.Goodell S, Druss BG, Reisinger Walker E. Foundation RWJ, editor. Mental disorders and medical comorbidity. The Synthesis Project, Policy Brief No 21. 2011 [PubMed] [Google Scholar]
- 31.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54(3):216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 32.Boyd C, Leff B, Weiss C, Wolff J, Hamblin A, Martin L. Clarifying multimorbidity to improve targeting and delivery of clinical services for medicaid populations. Center for Health Care Strategies, Inc; Dec, 2010. [Google Scholar]
- 33.Salisbury C. Multimorbidity: redesigning health care for people who use it. Lancet. 2012;380(9836):7–9. doi: 10.1016/S0140-6736(12)60482-6. [DOI] [PubMed] [Google Scholar]
- 34.Wang F, Xu S, Shen X, Guo X, Shen R. Epidemiology of multimorbidity. Lancet. 2012;380(9851):1382–1383. doi: 10.1016/S0140-6736(12)61794-2. [DOI] [PubMed] [Google Scholar]
- 35.Guthrie B, Watt G, Wyke S, Mercer SW. Epidemiology of multimorbidity. Author's reply. Lancet. 2012;380(9851):1383. doi: 10.1016/S0140-6736(12)61795-4. [DOI] [PubMed] [Google Scholar]
- 36.Komisar HL, Feder J. [June 16, 2014];Transforming Care for Medicare Beneficiaries with Chronic Conditions and Long-Term Care Needs: Coordinating Care Across All Services. http://cahpf.org/docuserfiles/georgetown_trnsfrming_care.pdf.
- 37.Leibson CL, Brown AW, Ransom JE, et al. Incidence of traumatic brain injury across the full disease spectrum: a population-based medical record review study. Epidemiology. 2011;22(6):836–844. doi: 10.1097/EDE.0b013e318231d535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leibson CL, Naessens JM, Brown RD, Jr., Whisnant JP. Accuracy of hospital discharge abstracts for identifying stroke. Stroke. 1994;25(12):2348–2355. doi: 10.1161/01.str.25.12.2348. [DOI] [PubMed] [Google Scholar]
- 39.Leibson CL, Needleman J, Buerhaus P, et al. Identifying in-hospital venous thromboembolism (VTE): a comparison of claims-based approaches with the Rochester Epidemiology Project VTE cohort. Med Care. 2008;46(2):127–132. doi: 10.1097/MLR.0b013e3181589b92. [DOI] [PubMed] [Google Scholar]
- 40.Roger VL, Killian J, Henkel M, et al. Coronary disease surveillance in Olmsted County objectives and methodology. J Clin Epidemiol. 2002;55(6):593–601. doi: 10.1016/s0895-4356(02)00390-6. [DOI] [PubMed] [Google Scholar]
- 41.Yawn BP, Wollan P, St Sauver J. Comparing shingles incidence and complication rates from medical record review and administrative database estimates: how close are they? Am J Epidemiol. 2011;174(9):1054–1061. doi: 10.1093/aje/kwr206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.