Abstract
Pulmonary and systemic organ injury produced by oxidative stress including lipid peroxidation is a fundamental tenet of ischemia-reperfusion injury, inflammatory response to cardiac surgery, and cardiopulmonary bypass (CPB) but is not routinely measured in a surgically relevant time frame. To initiate a paradigm shift toward noninvasive and real-time monitoring of endogenous lipid peroxidation, we have explored pulmonary excretion and dynamism of exhaled breath ethylene during cardiac surgery to test the hypothesis that surgical technique and ischemia-reperfusion triggers lipid peroxidation. We have employed laser photoacoustic spectroscopy to measure real-time trace concentrations of ethylene from the patient breath and from the CPB machine. Patients undergoing aortic or mitral valve surgery-requiring CPB (n = 15) or off-pump coronary artery bypass surgery (OPCAB) (n = 7) were studied. Skin and tissue incision by diathermy caused striking (>30-fold) increases in exhaled ethylene resulting in elevated levels until CPB. Gaseous ethylene in the CPB circuit was raised upon the establishment of CPB (>10-fold) and decreased over time. Reperfusion of myocardium and lungs did not appear to enhance ethylene levels significantly. During OPCAB surgery, we have observed increased ethylene in 16 of 30 documented reperfusion events associated with coronary and aortic anastomoses. Therefore, novel real-time monitoring of endogenous lipid peroxidation in the intraoperative setting provides unparalleled detail of endogenous and surgery-triggered production of ethylene. Diathermy and unprotected regional myocardial ischemia and reperfusion are the most significant contributors to increased ethylene.
Keywords: cardiopulmonary bypass, oxidative stress, ischemia-reperfusion injury, off-pump coronary artery bypass grafting
contemporary cardiac surgery provides symptom relief from heart disease and improves patient prognosis. However, the operation remains associated with significant myocardial, pulmonary, and systemic adverse outcomes (18, 25). Aortic cross-clamping and extracorporeal circulation and associated oxidative stress and pulmonary and systemic inflammatory response are considered major contributors.
Although the role of oxidative stress is clearly defined in animal models of ischemia-reperfusion injury and extracorporeal circulation, the nature, degree, and significance of oxidative stress in the setting of human cardiac surgery remain more controversial (3, 6, 10, 15). Liquid-phase biomarkers of oxidative stress have provided inconclusive evidence (1, 6, 7, 16, 20). Parallel to these biomarker studies, pulmonary excretion and analysis of volatile organic compounds in exhaled breath have also been considered. Interestingly, exhaled breath hydrocarbons have emerged as gaseous footprints of in vivo lipid peroxidation, but studies have been limited to discrete sampling and offline analysis in a specialized laboratory setting with results unavailable in a surgically relevant time frame (2, 19, 23, 26).
There is extensive biochemical evidence linking production of ethylene to lipid peroxidation. Lieberman and Hochstein (13) found that peroxidation of lipids was coupled to the generation of ethylene in rat liver microsomes in the presence of cuprous ions, providing an original model for the biogenesis of ethylene in animal cells. These milestone observations were confirmed in different isolated preparations (9, 4) and extended to animal models of endogenous or induced lipid peroxidation (12, 24, 27). Treating animals with established lipid peroxidation-inducing agents such as CCl4, δ-aminolevulinic acid, or Ni(II) caused a significant time-dependent and long-lasting production of ethylene, which was measureable in the breath of mice and rats. Sagai and Ichinose (24) investigated age-related lipid peroxidation and found breath hydrocarbons as sensitive indexes of peroxidation associated with aging with substantial increase in exhaled ethylene in aged compared with young animals. To explore the human relevance of these models, we have conducted unique preclinical studies and demonstrated increased ethylene release associated with lipid peroxidation in healthy volunteers during UV irradiation (17, 11). In these experiments, 21 male volunteers were exposed to UV light from a commercial solarium for 15 min. Individual data suggested that ethylene rises within 2 min of exposure, with ethylene exhalation increasing to 17.2 ± 7.3 pmol·kg−1·min−1 from pre-UV exposure levels of 1.39 ± 0.38 pmol·kg−1·min−1. These responses were eliminated by shielding the subjects from solarium by a UV protective Lexan barrier. On the basis of such substantial evidence, we have proposed utilizing real-time laser photoacoustic detection of ethylene (8) to monitor in vivo oxidative stress associated with cardiac surgery.
To investigate the feasibility of continuous assessment of lipid peroxidation by expired ethylene in the clinical setting of cardiac surgery, we have studied patients undergoing the most common surgical valvular and coronary artery bypass grafting procedures. There is tremendous scientific debate regarding the impact of cardiopulmonary bypass, myocardial and pulmonary ischemia, and reperfusion on myocardial, pulmonary, and systemic lipid peroxidation. Furthermore, there are contradictory studies regarding the effect of electrocautery and sternotomy on gaseous footprints of lipid peroxidation. In our study, we addressed these issues by conducting two related studies: one focusing on cardiopulmonary bypass and the other on beating heart surgery.
METHODS
Patients
For the first series, 15 patients requiring aortic and mitral valve repair/replacement utilizing extracorporeal circulation were studied to evaluate the impact of 1) diathermy and sternotomy, 2) cardiopulmonary bypass (CPB), 3) cardioplegia-protected global myocardial ischemia-reperfusion injury associated with aortic cross-clamping, 4) separation from CPB and pulmonary reperfusion, and 5) post-CPB period. In the second series, the influence of regional and unprotected myocardial ischemia-reperfusion was investigated in seven patients undergoing beating heart off-pump coronary artery bypass grafting (OPCAB). The Regional Ethics Committee approved this study as part of the Harefield BIOSTRESS program. All patients provided written, informed consent.
Specific anesthetic considerations included total intravenous anesthesia (before, during, and after CPB), application of stable ventilation parameters throughout the study, and preparation of the anesthetic machines to avoid trace contamination with inhalational agents, which caused spectral interference with ethylene detection. Surgical conduct was according to routine practice. Standard CPB management included membrane oxygenators, arterial line filters, systemic hypothermia down to 32°C, and nonpulsatile flow of 2.4 l·min−1·m−2, with a mean arterial pressure greater than 50 mmHg. The myocardium was protected by use of intermittent antegrade cold blood cardioplegia (4:1 blood to crystalloid ratio). Combined anterograde and retrograde cardioplegia was employed selectively, according to clinical need.
Measurement of Exhaled Ethylene
The ethylene detector.
We used the ETD-300 ethylene detector (by Sensor Sense, Nijmegen, The Netherlands), which is based on laser photoacoustic spectroscopy principle and uses a CO2 laser emitting light in the 10-μm region, where ethylene presents the strongest absorption. Currently, ETD-300 is able of measuring ethylene online in the 300 pptv (pptv = parts per trillion by volume, 1:1012) range within a 5-s time scale offering wide dynamic range, operational simplicity, and relative portability.
The gas sampling system.
The gas sampling system ensured uninterrupted gas flow from the patient or CPB machine to the ethylene detector. A small portion of the exhaled gas flow was continuously sampled at a constant flow rate of 4 l/h with a mass flow controller (Brooks Instrument, Ede, The Netherlands) from the anesthesia/CPB machine by using a diaphragm pump (Knf, type NMP830KTDC, Germany) through a Teflon PTFA sampling line of 1/16-in. diameter and ∼4 m long (Polyfluor Plastics, Oosterhout, The Netherlands). The gas flow was passed through a CO2 scrubber containing 42 g of soda lime and a water trap with 40 g CaCl2 after the pump and prior entering the ethylene detector.
Real-time ethylene measurement.
While the patient was anesthetized in the anesthetic induction room, the sampling line was connected to the expiratory limb of ventilation circuit in the operating room to monitor baseline ethylene levels present in the ventilation circuit at a ventilation setting mimicking the predicted ventilation strategy for the given patient. The sampling line was positioned distal to the bacterial filter in the expiratory limb of the ventilation circuit with a clinically approved tube attachment.
Following transfer of the patient to the operating room, ventilation commenced with this setting, allowing determination of the patient baseline ethylene concentrations. Particular attention was given to commencement of surgery and the temporal relationship of diathermy application for skin incision and subsequent sternotomy. For the prebypass period, the sampling gas line remained connected to the ventilation circuit to monitor the real-time production of ethylene. Following heparin administration, the sampling line was transferred to the exhaust of the oxygenator part of the cardiopulmonary bypass machine. Gaseous ethylene was then continuously measured during the recirculating priming phase, upon commencement of cardiotomy suction and establishment of full cardiopulmonary bypass. Special consideration was given to measuring ethylene concentration at the time of the release of aortic cross-clamp and myocardial reperfusion. After rewarming and commencement of mechanical ventilation, the sampling line was returned to the ventilation circuit with an aim to compare exhaled ethylene just prior to and after separation of cardiopulmonary bypass. In addition, ethylene was constantly monitored in the postbypass period.
Data Analysis
The main advantage of the real-time analysis is that changes in measured concentrations can be directly linked to clinical events and management changes. Thus we have made serious efforts to liaise with clinical staff to document surgical events, anesthetic measures and perfusion procedures and to identify their impact and relationship with dynamic ethylene changes. To demonstrate these relationships, we have presented a series of representative traces obtained at specific phases of surgery or in response to particular clinical events.
Because there are no similar real-time breath analysis studies on the field, it is important to compare our experiments with previous studies that used offline analysis at discrete and predetermined sampling time points. To do this, we have averaged our real-time ethylene data for 3 min at different time points during surgery. These data would be equivalent to ethylene concentrations in a breath sample collected in bags over a similar time period.
The distribution of quantitative data was checked by the Shapiro-Wilk or Kolmogorov-Smirnow test. Normally distributed data are presented as means ± SD. Data exhibiting nonnormal distribution are presented as a median and lower and upper quartile. Qualitative data are presented as percentage of whole analyzed group. Repeated-measures analysis of variance or variance on ranks was used to compare experimental groups with appropriate post hoc tests. Value of P < 0.05 was considered statistically significant. The analysis was performed with the SigmaPlot version 12.0 statistical software package (Systat Software 2011–12).
RESULTS
Clinical Summary
Patient demographics and clinical outcomes of the two patient populations are summarized in Table 1. Both groups included mainly elderly patients. All patients survived in the OPCAB group whereas one patient died after valve surgery. Patients in both groups required a few hours of postoperative mechanical ventilation and stayed in the intensive care unit for a few days. Vasoactive and inotrope requirement was higher in the valve patients and both groups exhibited systemic inflammatory response as evidenced by laboratory measures of white cell blood counts and C-reactive protein levels.
Table 1.
Patient demographics and outcomes
| Patient Variable | CPB | OPCAB |
|---|---|---|
| Age, yr | 74.8 ± 6.7 | 73.3 ± 6.6 |
| Sex, % male | 66% | 100% |
| Body mass index | 27.8 ± 3.7 | 27.0 ± 3.1 |
| Surgery time, min | 286 ± 90 | 209 ± 25 |
| CPB time, min | 82 (74;106) | |
| AXC time, min | 62 (43;69) | |
| Clinical outcomes | ||
| Survival | 14/15 | 7/7 |
| Duration of mechanical ventilation, h | 9 (4;72) | 5 (3;5) |
| Intensive care unit stay, days | 3 (2;10) | 4 (2;4) |
| Inotrope requirement, μg·kg−1·72 h−1 | ||
| Epinephrine | 0.0 (0.0;16.4) | 0.0 (0.0;0.0) |
| Norepinephrine | 130 (0.0;599) | 3.5 (0.0;16.2) |
| Milrinone | 242 (63;393) | 0.0 (0.0;0.0) |
| SIRS response | ||
| Peak white blood cell count, 109/l | 15.2 ± 4.8 | 11.6 ± 3.6 |
| Peak CRP, mg/l | 184 ± 112 | 179 ± 73 |
CPB, cardiopulmonary bypass; OPCAB, off-pump coronary artery bypass grafting; SIRS, systemic inflammatory response; CRP, C-reactive protein.
Exhaled Ethylene During Valve Surgery and CPB
Figure 1A shows a representative example of continuous monitoring of ethylene produced spanning the entire duration of cardiac surgery. This experiment clearly demonstrates dynamic changes in expired ethylene concentrations at specific phases of surgery and the unique release of ethylene from the exhaust of CPB circuit. Figure 1B summarizes averaged breath ethylene data of all valve surgery patients at various stages of surgery.
Fig. 1.
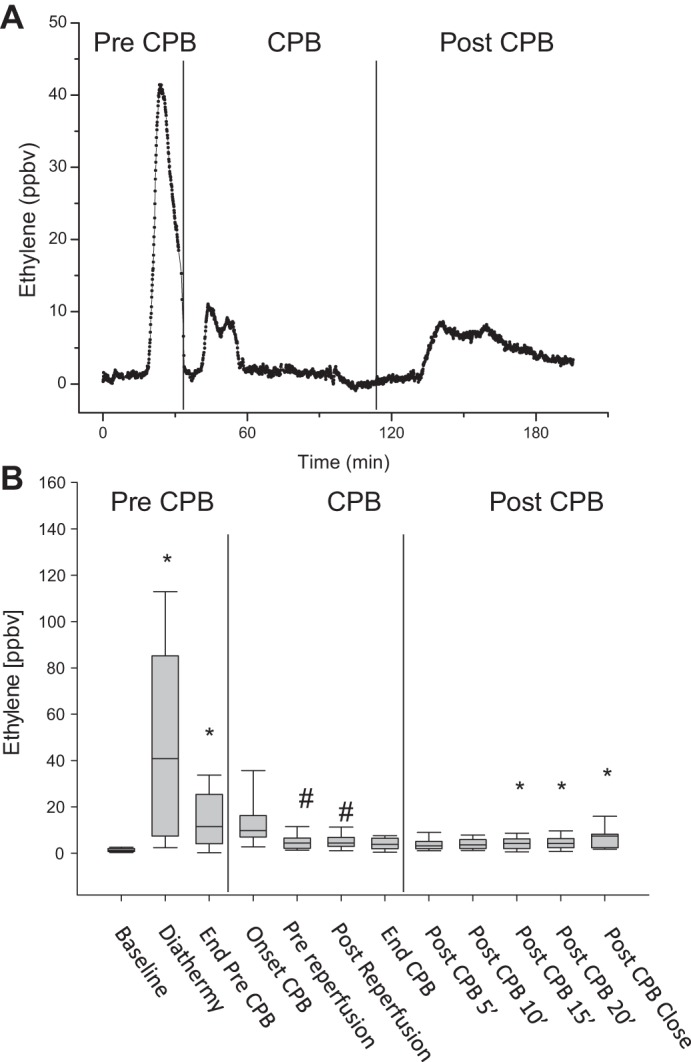
Intraoperative real-time monitoring of ethylene measured in patients undergoing cardiac surgery with cardiopulmonary bypass (CPB). Sampling line was positioned in the expiratory limb of the ventilator circuit prior to and at the end of CPB and following CPB and to the exhaust of the oxygenator of CPB machine during CPB. Box plots represent 3–5 min ethylene averages. *P < 0.05 compared with patient baseline for ventilated groups. #P < 0.05 among CPB groups.
Sternotomy and prebypass period.
Valvular surgery patients exhibited 1.200 (0.7; 2.0) parts per billion by volume (ppbv) baseline levels of ethylene prior to commencement of surgery. Surgical skin and tissue incision using diathermy resulted in striking, robust, and persistent increases in ethylene [peak concentrations of 40.8 (7.4; 85.2) (1:109), Figs. 1 and 2A]. The concentrations of breath ethylene remained higher compared with baseline levels for the remaining of the prebypass period [11.5 (4.1; 25.4) ppbv at the end of the pre-CPB period representing an area under curve (AUC) of 7.7 ± 1.6 ppbv × s for the entire pre-CPB episode].
Fig. 2.
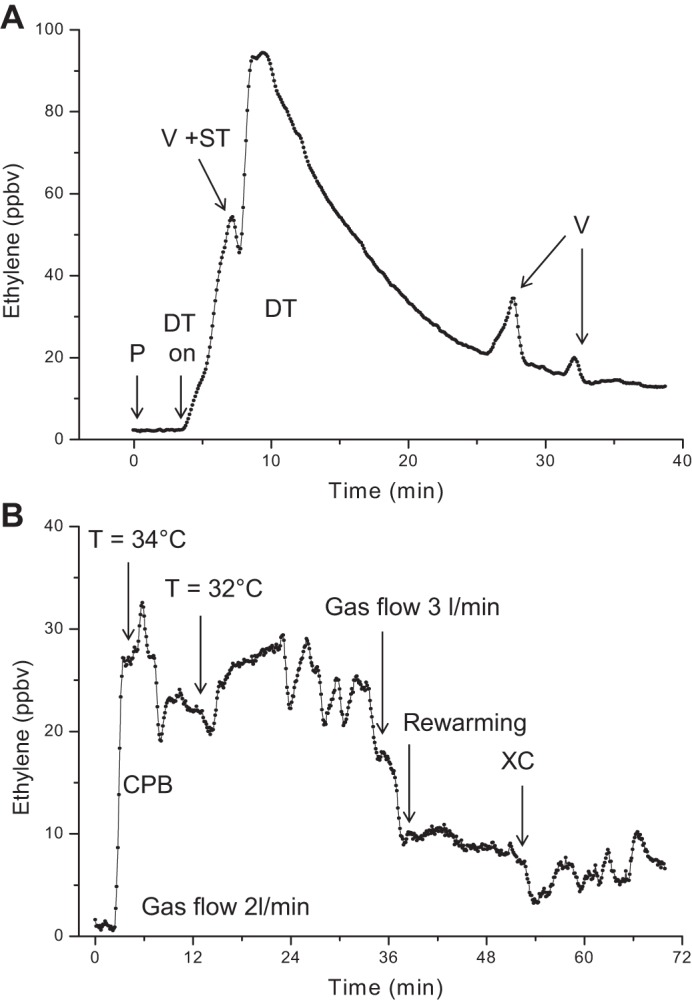
Impact of sternotomy (A) and cardiopulmonary bypass (B) on gaseous ethylene. A: typical example of real-time monitoring of ethylene following initial diathermy (DT) for skin incision and sternotomy (ST). P, patient baseline; V, ventilation hold. B: example of real-time monitoring of ethylene at onset of CPB showing influence of changing fresh gas flow, temperature (T), rewarming, and aortic cross-clamp release (XC).
Bypass period.
Compared with the recirculating priming phase (in the absence of blood return), there was an immediate rise in ethylene upon return of the cardiotomy suction blood to the CPB circuit following full heparinization. In addition, there was a significant rise in ethylene upon achievement of full CPB [9.75 (7.0; 16.3) vs. 0.7 (0.5; 1) ppbv; Figs. 1 and 2B]. Average ethylene concentrations were significantly less at later time points during CPB such as prior to removal of aortic cross-clamp and at the end of rewarming period. We noted significant changes in measured ethylene release in response to various changes in perfusion management such as changes in sweep gas flow (Fig. 2B) or application of hemofiltration (not shown).
We have also observed characteristic biphasic ethylene responses (consisting of an initial decrease followed by return to baseline) associated with the deairing protocol (filling the heart and commencement of ventilation) and release of aortic cross-clamp (Fig. 2B). Compared with the immediate predeairing period (5 min average), ethylene concentrations were similar after release of the aortic cross-clamp [4.4 (2.1; 6.55) vs. 4.4 (2.9; 6.85) ppbv, respectively, Fig. 1B].
Postbypass period.
The process of separation from CPB, rapidly changing hemodynamics, protamine administration, and occasional breath holding resulted in dynamically changing expired ethylene levels during the initial postbypass period. Average concentrations of ethylene in the first 5 min after CPB were not different from the preceding period just prior to separation from CPB [3.2 (1.9; 5.1) ppbv vs. 3.85 (1.975; 6.50) ppbv]. Subsequently, ethylene levels remained largely unchanged apart from chest closure, where repeated application of diathermy for hemostasis was associated with higher breath ethylene [7.4 (2.3; 8.2) ppbv, Fig. 1B].
Exhaled Ethylene During OPCAB
Increases in the concentrations of ethylene as a result of skin incision and sternotomy during OPCAB surgery was similar to valvular surgery (Fig. 3). Notably, there was more prolonged application of diathermy during the preparatory phase of surgery (prior to grafting) resulting in more prolonged increases in ethylene (AUC of 14.6 ± 0.7 ppbv × s) in this period. We have noted 22 reperfusion events associated with clamping and release of main coronary arteries during distal anastomoses. In addition we have documented eight reperfusion events following proximal aortic anastomoses. Fourteen of these events produced no change in breath ethylene concentrations. Sixteen reperfusion events were associated with typical increases in ethylene release; however, the magnitude of these increases appeared smaller than the effect of diathermy. Four of these increases may have been confounded by concomitant surgical and anesthetic factors such as breath holding or major manipulation of heart and hemodynamic changes (Fig. 3). Summary data are presented in Fig. 4 showing the effect of diathermy, significantly higher than baseline levels of ethylene at the end of harvesting the graft conduits and at the time of heparin administration and during the distal anastomoses. Exhaled ethylene remained high throughout surgery although later time points did not show statistical significance by multiple pairwise comparisons.
Fig. 3.
Example of real-time monitoring of ethylene during off-pump coronary artery bypass surgery (OPCAB) grafting showing the reperfusion events associated with completing of distal and proximal aortic anastomoses. LAD, left anterior descending, PDA, posterior descending; CFX, circumflex coronary artery; ASC, aortic side clamp; OM, obtuse marginal.
Fig. 4.
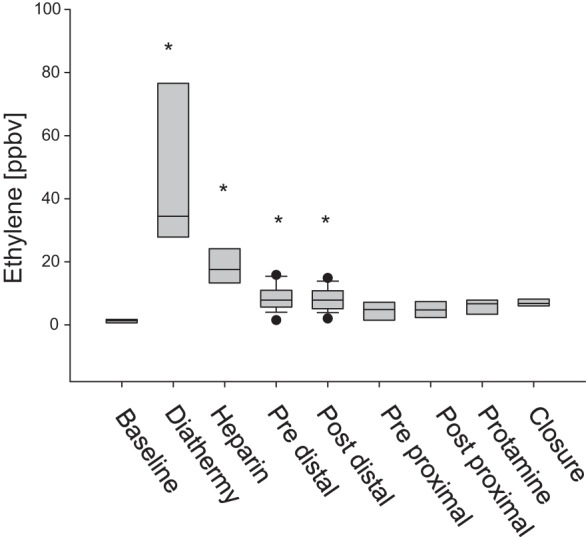
Summary data of real-time monitoring of ethylene during OPCAB grafting showing the major clinical and reperfusion events associated with completing of distal anastomoses and proximal aortic anastomoses. Box plots represent 3–5 min ethylene averages. *P < 0.05 compared with patient baseline.
DISCUSSION
Here we present the results of the first real-time assessment of lipid peroxidation in cardiac surgery and perioperative medicine utilizing pulmonary excretion and accumulation of ethylene in exhaled breath. Such application represents the true translation of several decades of substantive basic research on ethylene and lipid peroxidation to biochemical and molecular monitoring of inflammation at the bedside at the point of patient care. The ability of monitoring ethylene at trace gas levels noninvasively, in real time, and in the real-world clinical environment without significant sample preparation and processing has provided us with unprecedented resolution of the dynamism of lipid peroxidation during the entire course of surgery. This novel information has major implications for the central debate regarding the status of oxidative stress in cardiac surgery and for the innovation of breath analysis to perioperative medicine and beyond.
Several authors have found significant rise of lipid peroxidation products such as malondialdehyde-conjugated dienes, and thiobarbituric acid reactive substances in the venous coronary sinus blood following myocardial reperfusion in the setting of cardiac surgery (1, 10, 15, 20). Yet there are significant inconsistencies in the literature regarding the timing, magnitude, and significance of such changes. Furthermore, recent investigation found no increase in lipid peroxidation products in the coronary effluent or myocardial homogenates or subcellular fractions following aortic cross-clamp and reperfusion and no detectable alterations in myocardial ultrastructures (6, 7, 16).
On the basis of short-chain hydrocarbon production during decomposition of omega fatty acids, the pulmonary excretion of volatile gases ethane and pentane have been considered noninvasive exhaled breath biomarkers of total body and myocardial lipid peroxidation. The milestone study of Andreoni et al. (2) and subsequent studies (14, 19, 26) utilized discrete breath collections and laboratory analysis and provided insights into these breath biomarkers. However, there are significant inherent limitations of such methodology and significant controversy remains regarding the triggers, timing, and relevance of ethane kinetics.
Our measurements evidently demonstrate the feasibility of continuous measurement of exhaled ethylene in mechanically ventilated patients throughout surgery and in the exhaust of the cardiopulmonary bypass circuit. The ethylene monitor can be located adjacent to the operating room. Moreover, sampling and analysis can be performed with only minor modification of the ventilation circuit. However, total intravenous anesthesia had to be employed to avoid spectral interference from volatile anesthetic agents.
Our data clearly demonstrate substantial increases in ethylene release at critical early stages of surgery and persistently elevated levels for most part of the intraoperative period. The experiments provide conclusive evidence pertinent to the debate on the substantial contribution of electrocautery to overall lipid peroxidation (2, 19, 26). Firstly, our experiments reveal previously unrecognized details and magnitude of early hydrocarbon release associated with diathermy and skin incision. In our experiments, this significant rise in ethylene clearly followed the application of diathermy and preceded events associated with sternotomy such as breath holding and splitting the sternum with the surgical saw. Secondly, although we typically observed a washout curve, ethylene levels did not return to baseline levels, suggesting the possibility of longer-term impact of diathermy and sustained ethylene release from cauterized tissue. Thirdly, lesser applications of diathermy prior to chest closure also produced smaller but significant increases in breath ethylene, thereby potentially contributing to overall oxidative stress burden. Finally, such effect of diathermy was also pronounced in OPCAB procedures. Indeed the prolonged application of diathermy to prepare the vascular conduits resulted in greater releases of ethylene (doubling the ethylene AUC) in the period prior to revascularization. There is evidence that OPCAB is not free from surgical inflammation and such contribution of diathermy should be taken into consideration when interpreting fluid phase biomarkers of lipid peroxidation and oxidative stress in beating heart surgery (22, 21).
The contribution of extracorporeal circulation to oxidative stress is less conclusive. We observed increased ethylene release by the oxygenator of the CPB circuit at the beginning of CPB (compared with background levels during priming), which is consistent with washout of ethylene from the blood compartment. This may relate to earlier diathermy applications, but we cannot rule out potential triggers associated with commencement of bypass such as temporary activation of blood elements, partial lung ischemia, and systemic effects of nonpulsatile blood flow. Nevertheless, steady-state levels of ethylene decreased to baseline rather than increased with progression of CPB, suggesting that these mechanisms were not the major source of lipid peroxidation during surgery.
Our ethylene data should be considered as part of the wider inflammatory response to CPB. Similar to others, we have demonstrated increased neutrophil activation during CPB; therefore, neutrophil-derived oxidants could contribute to overall lipid peroxidation. Analysis of proinflammatory cytokine response demonstrated small increases in some proinflammatory cytokines (IL-8, IL-6, IL-1) and parallel large increases in the appropriate anti-inflammatory cytokines indicating cytokine balance in the plasma compartment (unpublished observations). Beyond ethylene, we have also investigated other redox gases including exhaled nitric oxide (NO) and carbon monoxide (CO) release in patients undergoing cardiac surgery. There was no evidence for increased NO and CO in our routine patient populations.
These results may indicate that current conduct of CPB results in lesser inflammatory and oxidative stress response in routine and low-risk patients. We have to realize that perfusion technologies have undergone tremendous developments and now are extensively utilized for days and weeks to facilitate organ recovery during extracorporeal mechanical support and membrane oxygenation. Perfusion technologies are also being recognized as some of the most revolutionary progresses in current practice of cardiothoracic transplantation such as during ex vivo perfusion and short-term recovery and reconditioning of injured hearts and lungs.
In addition to events during CPB, separation from CPB was not associated with significant immediate increases in breath ethylene suggesting that pulmonary reperfusion and restoration of systemic pulsatile flow was not associated with increased oxidative stress. However, at later stages exhaled ethylene remained significantly higher than baseline measurements and ongoing pulmonary and systemic inflammation may have contributed to such responses.
Global myocardial ischemia-reperfusion during valvular procedures was not associated with increased ethylene release, suggesting that there was effective protection against lipid peroxidation-mediated damage. Although the measurements reveal exceptional details of ethylene production during reperfusion that may be confounded by deairing events and temporary reduction of perfusion flow during release of aortic cross-clamp, average ethylene prior to and after reperfusion did not change. Blood cardioplegia, moderate degree of hypothermia, and antioxidant effects of propofol may have contributed to lack of lipid peroxidation in our patients (5, 7, 15).
Ethylene responses to regional myocardial ischemia during OPCAB were variable, and we have identified three prototype responses. In ∼50% of reperfusion events, restoration of native coronary flow or full bypass grafting was associated with no changes in ethylene release. However, the remaining reperfusion events produced a detectable rise in exhaled ethylene. In a few cases we cannot rule out confounding factors associated with necessary management of the anastomoses (stopping ventilation, major manipulation of the heart, short burst of diathermy), but in the rest of the events we conclude a true reperfusion-related increase in ethylene. Our real-time analysis indicates that these reperfusion events occur on the downslope of the diathermy-induced ethylene release and that the contribution of reperfusion to measured concentrations of ethylene is variable (3–44%).
The determinants of lipid peroxidation and ethylene release during OPCAB surgery remain to be established, but collateral circulation, antioxidant treatment, hemodynamic management of heart displacement, and coronary occlusion may play a role.
In conclusion, our original studies suggest that sensitive, totally noninvasive, and real-time analysis of lipid peroxidation using breath ethylene is feasible in the clinical and perioperative setting. This innovative approach has irrefutably demonstrated the significant contribution of diathermy to overall oxidative stress and identified increased ethylene associated with regional myocardial ischemia on an individual basis. Clearly, our observations challenge the oxidative stress concept of injury associated with aortic cross-clamping and CPB. They also highlight complexities of breath analysis in the perioperative environment and strongly support the application of real-time methods as frontiers of breath biomarker research in the dynamic surgical setting.
Future Directions
These pilot studies in low-risk cardiac surgical patients pave the way for future studies to study oxidative stress in higher risk populations and in those individuals who develop postoperative complications. This technology could advance the field by correlating ethylene levels with broader measures of inflammation in both preclinical and clinical settings and with organ dysfunction or outcomes in future large-scale clinical trials. We need to better understand mechanisms of release of ethylene, and single organ contributions should be evaluated by use of ex vivo human lung or heart perfusions. Studies should also further address physiological and physical determinants of exhaled ethylene such as the influence of cardiac output, ventilation, and temperature. Once these aspects are established, real-time monitoring of ethylene may have the potential of becoming the “capnography” of perioperative inflammation and oxidative stress. Ultimately such monitoring could enable testing pharmacological interventions or changing surgical practices in reducing lipid peroxidation and surgical complications. Our innovative method may also offer novel opportunities in molecular monitoring for other fields of pulmonary and circulation research and medicine.
GRANTS
These studies were supported by the National Institute of Health Research, The Royal Brompton and Harefield NHS Foundation Trust Biomedical Research Unit; the EU-FP6-Infrastructures-5, FP6-026183, Life Science Trace Gas facility; the GO-EFRO Ultragas 2009-010034, Ultra sensitive gas analysis systems for medical diagnostic and quality monitoring of horticultural products; and Erasmus Programme Mobility 2011/2012 for staff training.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author (s).
AUTHOR CONTRIBUTIONS
S.M.C., S.t.L.H., M.D., F.J.H., T.H.R., and N.M. conception and design of research; S.M.C., R.K., T.H.R., and N.M. performed experiments; S.M.C., R.K., T.H.R., and N.M. analyzed data; S.M.C., S.t.L.H., T.H.R., and N.M. interpreted results of experiments; S.M.C. and N.M. prepared figures; S.M.C. and N.M. drafted manuscript; S.M.C., R.K., M.D., T.H.R., and N.M. edited and revised manuscript; S.M.C., R.K., S.t.L.H., M.D., F.J.H., T.H.R., and N.M. approved final version of manuscript.
ACKNOWLEDGMENTS
We are grateful for Harefield Hospital Theatres perfusionists and nurses for valuable collaboration, help, and discussions during these studies.
Collaborators of the Harefield BIOSTRESS study include Mohamed Amrani, Toufan Bahrami, Fabio De Robertis, Jullien Gaer, Shahzad Raja, and Andre R. Simon from the Department of Surgery, Royal Brompton and Harefield NHS Foundation Trust, Harefield, UK; Uta Bellin, John Farrimond, Isabelle Fonteyne, Andrew Gaunt, Donna Hall, Paul Harris, Sundeep Kaul, Lakshmi Kuppurao, Nicholas Lees, Simon Mattison, Grainne McDermott, Ian McGovern, Jerry Mitchell, Royston David, Anne Sigel, Christopher Walker, and Gavin Wright from the Department of Anaesthesia, Royal Brompton and Harefield NHS Foundation Trust, Harefield, UK; Paula Rogers from the Department of Cardiology, Royal Brompton and Harefield NHS Foundation Trust, Harefield, UK; and Rosalba Romano and Rosada Davey from the Section of Anaesthesia, Pain Medicine and Intensive Care, Department of Surgery and Cancer, Faculty of Medicine, Imperial College London, London, UK.
REFERENCES
- 1.Akila, D'souza B, Vishwanath P, D'souza V. Oxidative injury and antioxidants in coronary artery bypass graft surgery: off-pump CABG significantly reduces oxidative stress. Clin Chim Acta 375: 147–152, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Andreoni KA, Kazui M, Cameron DE, Nyhan D, Sehnert SS, Rohde CA, Bulkley GB, Risby TH. Ethane: a marker of lipid peroxidation during cardiopulmonary bypass in humans. Free Radic Biol Med 26: 439–445, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Bell RM, Yellon DM. There is more to life than revascularization: therapeutic targeting of myocardial ischemia/reperfusion injury. Cardiovasc Ther 29: e67–e79, 2011 [DOI] [PubMed] [Google Scholar]
- 4.Bousquet JF, Thimann KV. Lipid peroxidation forms ethylene from 1-aminocyclopropane-1-carboxylic acid and may operate in leaf senescence. Proc Natl Acad Sci USA 81: 1724–1727, 1984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown RH, Wagner EM, Cope KA, Risby TH. Propofol and in vivo oxidative stress: effects of preservative. J Breath Res 3: 016003, 2009 [DOI] [PubMed] [Google Scholar]
- 6.Chambers DJ. Oxidative stress injury during cardiac surgery: how important is it? Cardiovasc Res 73: 626–628, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Clermont G, Vergely C, Jazayeri S, Lahet J, Goudeau J, Lecour S, David M, Rochette L, Girard C. Systemic free radical activation is a major event involved in myocardial oxidative stress related to cardiopulmonary bypass. Anesthesiology 96: 80–87, 2002 [DOI] [PubMed] [Google Scholar]
- 8.Cristescu SM, Persijn ST, Hekkert STL, Harren FJM. Laser-based systems for trace gas detection in life sciences. Appl Phys B 92: 343–349, 2008 [Google Scholar]
- 9.Dumelin EE, Tappel AL. Hydrocarbon gases produced during in vitro peroxidation of polyunsaturated fatty acids and decomposition of preformed hydroperoxides. Lipids 12: 894–900, 1997 [DOI] [PubMed] [Google Scholar]
- 10.Ferrari R, Alfieri O, Curello S, Ceconi C, Cargnoni A, Marzollo P, Pardini A, Caradonna E, Visioli O. Occurrence of oxidative stress during reperfusion of the human heart. Circulation 81: 201–211, 1990 [DOI] [PubMed] [Google Scholar]
- 11.Harren FJM, Berkelmans R, Kuiper K, te Lintel Hekkert S, Scheepers P, Hollander P, Dekhuijzen R, Parker DH. On-line laser photoacoustic detection of ethene in exhaled air as biomarker of ultraviolet radiation damage of the human skin. Appl Phys Lett 74: 1761–1763, 1999 [Google Scholar]
- 12.Knight JA, Hopfer SM, Reid MC, Wong SH, Sunderman FW., Jr. Ethene (ethylene) and ethane exhalation in Ni[II]-treated rats, using an improved rebreathing apparatus. Ann Clin Lab Sci 16: 386–394, 1986 [PubMed] [Google Scholar]
- 13.Lieberman M, Hochstein P. Ethylene formation in rat liver microsomes. Science 152: 213–214, 1966 [DOI] [PubMed] [Google Scholar]
- 14.Mendis S, Sobotka PA, Leja FL, Euler DE. Breath pentane and plasma lipid peroxides in ischemic heart disease. Free Radic Biol Med 19: 679–684, 1995 [DOI] [PubMed] [Google Scholar]
- 15.Mezzetti A, Calafiore AM, Lapenna D, Deslauriers R, Tian G, Salerno TA, Verna AM, Bosco G, Pierdomenico SD, Caccurullo F. Intermittent antegrade warm cardioplegia reduces oxidative stress and improves metabolism of the ischemic-reperfused human myocardium. J Thorac Cardiovasc Surg 109: 787–795, 1995 [DOI] [PubMed] [Google Scholar]
- 16.Milei J, Forcada P, Fraga CG, Grana DR, Iannelli G, Chiariello M, Tritto I, Ambrosio G. Relationship between oxidative stress, lipid peroxidation, and ultrastructural damage in patients with coronary artery disease undergoing cardioplegic arrest/reperfusion. Cardiovasc Res 73: 710–719, 2007 [DOI] [PubMed] [Google Scholar]
- 17.Moeskops BW, Steeghs MM, van Swam K, Cristescu SM, Scheepers PT, Harren FJM. Real-time trace gas sensing of ethylene, propanal and acetaldehyde from human skin in vivo. Physiol Meas 27: 1187–1196, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Nalysnyk L, Fahrbach K, Reynolds MW, Zhao SZ, Ross S. Adverse events in coronary artery bypass graft (CABG) trials: a systematic review and analysis. Heart 89: 767–772, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pabst F, Miekisch W, Fuchs P, Kischkel S, Schubert JK. Monitoring of oxidative and metabolic stress during cardiac surgery by means of breath biomarkers: an observational study. J Cardiothorac Surg 2: 37, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pantke U, Volk T, Schmutzler M, Kox WJ, Sitte N, Grune T. Oxidized proteins as a marker of oxidative stress during coronary heart surgery. Free Radic Biol Med 27: 1080–1086, 1999 [DOI] [PubMed] [Google Scholar]
- 21.Raja SG, Berg GA. Impact of off-pump coronary artery bypass surgery on systemic inflammation: current best available evidence. J Card Surg 22: 445–455, 2007 [DOI] [PubMed] [Google Scholar]
- 22.Rasmussen BS, Laugesen H, Sollid J, Gronlund J, Rees SE, Toft E, Gjedsted J, Dethlefsen C, Tonnesen E. Oxygenation and release of inflammatory mediators after off-pump compared with after on-pump coronary artery bypass surgery. Acta Anaesthesiol Scand 51: 1202–1210, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Risby TH, Sehnert SS. Clinical application of breath biomarkers of oxidative stress status. Free Radic Biol Med 27: 1182–1192, 1999 [DOI] [PubMed] [Google Scholar]
- 24.Sagai M, Ichinose T. Age-related changes in lipid peroxidation as measured by ethane, ethylene, butane and pentane in respired gases of rats. Life Sci 27: 731–738, 1980 [DOI] [PubMed] [Google Scholar]
- 25.Selim M. Perioperative stroke. N Engl J Med 356: 706–713, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Stenseth R, Nilsen T, Haaverstad R, Vitale N, Dale O. Frequent sampling allows detection of short and rapid surges of exhaled ethane during cardiac surgery. Perfusion 22: 391–396, 2007 [DOI] [PubMed] [Google Scholar]
- 27.Stolik S, Ramon-Gallegos E, Pacheco M, Tomas SA, Cruz-Orea A, Pérez-Zapata AJ, Gaebler R, Sánchez-Sinencio F. Photoacoustic measurement of ethylene as a real time biomarker of lipid peroxidation processes in mice. Anal Sci 17: s365–s367, 2001 [Google Scholar]



