Summary
Objective
This paper analyzes evidence of the impact of patients’ adherence to pharmacological and non-pharmacological recommendations on the treatment costs of heart failure (HF) patients.
Methods
A systematic review was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Papers were searched using various combinations of the following keywords: ‘telemedicine’, ‘telemonitoring’, ‘telehealth’, ‘eHealth’, ‘remote monitoring’, ‘adherence’, ‘compliance’, ‘cost-effectiveness’, ‘cost-benefit’, ‘heart failure’, ‘healthcare costs’, ‘hospitalization’, and ‘drug costs’. We included only papers written in English or German, published between 1998 and 2014, and having one of our search terms in the title.
Results
Initially, 73 papers were selected. After a detailed review, these were narrowed done to 9 that reported an association between adherence and/or compliance and costs. However, none established a quantitative relationship between adherence and total healthcare costs.
Conclusion
A model-based cost-effectiveness analysis that appropriately considers adherence has not been carried out so far, but is needed to fully understand the potential economic benefits of telehealth.
Keywords: Telemedicine, mHealth, therapy adherence/compliance, cost-effectiveness, heart failure
Introduction
The Austrian federal government has defined, for the period 2013–2016, a large number of strategic objectives to improve the national healthcare system [1]. One of those objectives is the establishment and evaluation of telemedicine services. These are considered to significantly contribute to optimizing and strengthening the efficiency of healthcare processes. At the same time, within the scope of the eHealth action plan 2012–2020, the European Union has committed itself to enhancing efforts on data collection and benchmarking activities in healthcare, recommending that relevant national and international bodies include more specific eHealth indicators and assess the impact and economic value of eHealth implementation [2].
The World Health Organization (WHO), defines adherence as ‘the extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider’ [3]. It is important to distinguish between the terms ‘adherence’ and ‘compliance’. Adherence implies that the patient agrees with and actively implements the recommendations of the healthcare provider. In contrast, compliance implies that the patient is acting passively according to the provider’s orders. Poor patient adherence to pharmacological recommendations is one of the major causes of avoidable healthcare costs [4]. Since the number of patients with chronic diseases is growing constantly, the importance of patient adherence is simultaneously increasing.
To evaluate telemedicine services from an economic perspective, it is necessary to identify crucial economic factors affecting the adoption and acceptance of telemedicine among patients and healthcare providers. However, it is difficult to find appropriate methods for measuring these economic benefits. Thus, it is difficult to determine the added value of telemedicine services. The clinical advantages of telemedicine services for chronic heart failure (chronic HF) patients were proven for the first time in Austria in the MOBIle TELemonitoring in Heart Failure Patients (MOBITEL) clinical trial. It was found that the associated amount of effort needed to manually enter the collected data clearly influenced patient adherence. Several trial participants stopped collecting their data before the end of the trial for various reasons, including usability [5]. A second, large-scale, Austrian pilot study based on mHealth investigated diabetes patients’ adherence using two different telemedicine technologies (Web, and Applications or Apps). The results showed that the adherence rate was higher for patients using Apps than those using the Web [6]. These Austrian examples indicate that the use of appropriate monitoring technology affects patients’ adherence, and that adherence is strongly related to the acceptance of these services and their ability to reduce healthcare costs.
As Ramaekers et al. [7] have already shown, the improvement in treatment and quality of life of patients using telemedicine services is largely because of their adherence to pharmacological and non-pharmacological recommendations. Improving patients’ adherence is thus expected to have a major impact on disease progression and mortality, as well as improve patients’ quality of life. Improving adherence could reduce expensive hospitalizations, which would facilitate the propagation of telemedicine services and lower total healthcare costs.
Objectives
This study conducts a systematic review of the published literature to analyze the economic impact of chronic HF patients’ adherence to treatment recommendations and the cost-effectiveness of telemedicine services for this patient population. The focus was on the economic aspects of patients’ adherence as a basis for properly including adherence factors in subsequent economic modeling approaches.
Methods
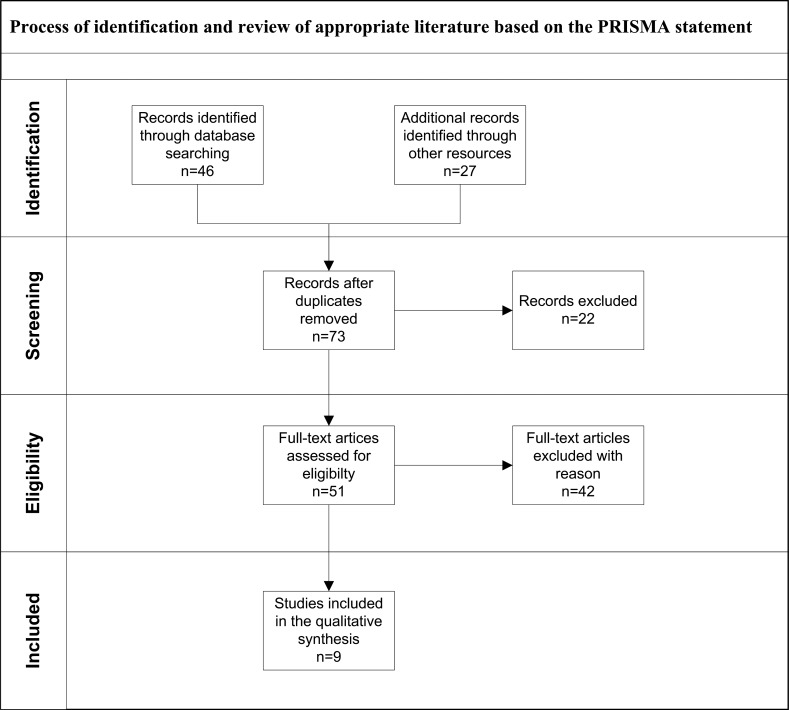
A multi-stage procedure was employed, following the recommendations specified in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (▶ Figure 1) [8]. In Stage 1, the three authors defined a set of keywords and corresponding technical terms: ‘telemedicine’, ‘telemonitoring’, ‘telehealth’, ‘eHealth’, ‘remote monitoring’, ‘adherence’, ‘compliance’, ‘cost-effectiveness’, ‘cost-benefit’, ‘heart failure’, ‘healthcare costs’, ‘hospitalization’, and ‘drug costs’. We used combinations of two or more (using the AND operation) of these terms to search PubMed [9] and Google Scholar [10] for appropriate research articles.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart of the systematic review.
We felt that it was necessary to include both ‘compliance’ and ‘adherence’ as keywords so that we could cover a wide spectrum of papers. We did not use medical subject headings (MeSH) because these terms were too coarse. We found 73 potential papers: 46 journal articles, 19 technical reports, 1 bachelor thesis, 3 master theses, and 4 PhD theses. We included only papers written in English or German, published between 1998 and 2014, and having one of our search terms in the title.
In Stage 2, we reviewed the abstracts of these 73 papers to determine their actual relevance. We excluded 22 articles for the following reasons: purely technical focus, lacking the characteristics of a research paper, or being out of scope.
In Stage 3, we conducted a full-text review of the 51 remaining papers. We examined the following:
Whether the papers analyzed adherence to pharmacological and non-pharmacological recommendations
Whether the papers reported the impact of adherence on the reduction of healthcare costs (the sum of medical procedure costs and drug costs)
Whether the papers specified the healthcare method (telemedicine versus standard care)
Only 9 articles met the above criteria and were included in the qualitative synthesis. They had been selected using the following groups of terms: ‘telemedicine, eHealth, adherence, heart failure’, ‘telemonitoring, cost-effectiveness, heart failure’, ‘adherence, telehealth, heart failure’, ‘compliance, telemonitoring, cost-effectiveness, heart failure’, and ‘hospitalization, adherence, healthcare costs’.
Results
▶ Table 1 provides an overview of the articles finally selected for review. The selected articles differed considerably in the sample size (n = 20–863) and duration of patients’ participation (3–41 months). The studies covered a wide geographical area, including countries from North America, Europe, and Asia.
Table 1.
Overview on the characteristics of the articles finally selected for review. The figures for Adherence / Compliance in the third column indicate how often these terms are present in the respective article.
| Author Year | Study/Journal | Type of disease (Sample Size)/Adherence/Compliance | Type of Study | Duration of patients’ participation in study | Country |
|---|---|---|---|---|---|
| Banka et al. 2013 [11] | Incremental Cost-Effectiveness of Guideline-Directed Medical Therapies for Heart Failure/JACC | HF with reduced ejection fraction (n.a)/10/0 | Standard healthcare Observational trial: cohort (follow-up) |
12–41 months | USA |
| Chen et al. 2013 [12] | Clinical Outcome and Cost-Effectiveness of a Synchronous Telehealth Service for Seniors and Non-seniors with Cardiovascular Diseases/JMIR | Cardio-vascular diseases (141)/2/2 | Telemedicine healthcare Quasi-Experimental (non-randomized controlled trial) | 6 months | TW |
| De Lusignan et al. 2001 [13] | Compliance and effectiveness of 1 year’s home telemonitoring. The report of a pilot study of patients with chronic heart failure/European Journal of Heart Failure | Chronic HF (20)/0/10 | Telemedicine vs. standard care RCT | 12 months | UK |
| Guzman-Clark et al. 2013 [14] | Predictors and Outcomes of Early Adherence to the Use of a Home Telehealth Device by Older Veterans with Heart Failure/Telemedicine and e-Health | HF (248)/84/1 | Telemedicine Retrospective cohort study | 3 months | USA |
| Heinen-Kammerer et al. 2003 [15] | Telemedizin in der Tertiärprävention: Wirtschaftlichkeits-Analyse des Telemedizin-Projektes Zertiva bei Herzinsuffizienz Patienten der Techniker Krankenkasse/Springer Berlin Heidelberg |
HF standard care (111)/0/0 HF telemonitoring (111)/0/0 |
Telemedicine vs. standard healthcare cost-effectiveness analysis based on TEN-HMS prospective, randomized study | 6 months | GE |
| Pandor et al. 2013 [16] | Home telemonitoring or structured telephone support programmes after recent discharge in patients with heart failure: systematic review and economic evaluation/ Health Technology Assessment | HF (n.a)/11/5 | Telemedicine vs. standard healthcare systematic review | 07/2010 –08/2012 | UK |
| Ramaekers et al. 2009 [7] | Adherence Among Telemonitored Patients with Heart Failure to Pharmacological and Nonpharmacological Recommendations/Telemedicine and e-Health | HF (101)/46/9 | Telemedicine vs. standard healthcare RCT | first 3 months | NL |
| Rohdeet al. 2013 [17] | Cost-effectiveness of heart failure therapies/Nature reviews cardiology | HF (n.a)/0/0 | Comparison of cost-effectiveness therapies | n.a | BR |
| Sokol et al. 2005 [18] | Impact of Medication Adherence on Hospitalization Risk and Healthcare Cost/Medical Care | Diabetes (3260) Hypertension (7981) Hypercholesterolemia (2981) Congestive HF (863)/82/4 | Standard healthcare Retrospective cohort study | 12 months | USA |
Each article’s priority in addressing adherence and compliance depended on its main focus. Articles with a high number of references to these terms (as shown in the column ‘Adherence/compliance’) usually discussed these issues more extensively in the text.
Banka et al. reported that full adherence to guideline-directed therapies can reduce healthcare costs for HF patients with reduced ejection fraction, using standard healthcare methods [11]. Financial support, such as co-payment for prescribed medications or providing financial incentives for patients, increases medical adherence and reduces the risk of hospitalization. However, only standard healthcare methods, not telemedicine, were used in this study.
Chen et al. [12] provided three different components of telemedicine services to patients with cardiovascular diseases: real-time transmission of biometric data, telephone exchanges between patients and healthcare teams, and 24-h analytical and decision-making support. They found that synchronous (real-time) telehealth services reduced the cost of the treatment of inpatients by reducing the duration and risk of hospitalization. However, they did not analyze the impact of patients’ adherence on the cost of telemedicine services.
De Lusignan et al. examined the effectiveness of telemedicine services for patients with chronic HF. Patients in their sample were randomly assigned to a telemedicine or standard care group. For both groups, the compliance rate for non-pharmacological recommendations (weight, pulse, and blood pressure [BP]) was between 75% and 90%. The telemedicine group had better compliance than the standard care group for collecting prescriptions for their cardiac medication, which has consequently led to an increase in medication costs. [13]. De Lusignan et al. focused on compliance to pharmacological recommendations and the associated medication costs only. They did not consider costs of medical procedures.
Guzman-Clark et al. analyzed predictors and outcomes of adherence of HF patients (in geriatrics, ambulatory/primary care, and home care services) using an asynchronous telemonitoring device. The results indicated a significantly higher mean adherence rate among HF patients using the telemedicine device in the ambulatory/primary care group. In the first 30 days of observation, comorbidity had a weak negative relationship with mean adherence. This study focused mainly on adherence related to the use of telemedicine devices and patients’ outcomes. The authors did not evaluate whether adherence could predict reduced treatment costs [14].
Heinen-Kammerer et al. examined the cost-effectiveness of telemonitoring services for patients with HF compared with standard healthcare methods. They concluded that telemonitoring services reduced treatment costs and re-hospitalization rates [15]. However, they did not examine the relevance of patients’ adherence to pharmacological and non-pharmacological recommendations.
In Pandor et al.’s systematic review, only 5 of the 21 included studies reported adherence (compliance) rates to the intervention. Adherence rates ranged between 55.1% and 84% for structured telephone support (STS) and between 81% and 98.5% for home telemonitoring (TM) [16]. These rates were related to only clinical effectiveness; Pandor et al. did not discuss how adherence influences treatment costs.
In a randomized controlled trial in which patients with HF received either standard care or telemonitoring, Ramaekers et al. found increased adherence and disease-specific knowledge among the telemedicine group. Both the telemedicine and standard care groups reported an average 89% adherence rate for appointments, taking prescribed medication, and smoking and alcohol restriction. They had medium adherence rates (70–75%) for daily weighing and sodium and fluid restriction, but low adherence rates (65%) for physical exercise [7]. This study focused on the impact of telemonitoring devices on disease-specific knowledge as well as adherence to non-pharmacological recommendations. It did not examine adherence to pharmacological recommendations and its effects on treatment costs.
Rohde et al. did not primarily focus on telehealth interventions. However, they present a detailed comparison of results of the published studies on the cost-effectiveness of HF therapies. Information about patients’ adherence and the related reduction in treatment costs was not available [17].
Sokol et al. confirmed that high levels of pharmacological adherence (80–100%) for diabetes, hypertension, and hypercholesterolemia treatments reduced hospitalization rates and consequently all-cause healthcare costs [18]. However, they did not find any significant cost reduction related to high levels of pharmacological adherence among patients with congestive HF. Further, their sample was limited to patients using standard healthcare methods, not telemedicine.
Our review has shown outcomes differed across research groups. Some of the findings regarding the impact of patients’ adherence to pharmacological recommendations on healthcare costs are partly contradictory (e.g., Sokol versus Banka). The reported cost reduction depended strongly on whether standard care method or telemedicine was used, as well as on the disease to be treated. Furthermore, because of the time frame within which these studies were carried out (from 1998 to 2014), it is necessary to consider technological developments during this period while interpreting these results, since these developments affect usability and other features of telemedicine services.
Discussion
The method used in this systematic review was based on the PRISMA statement. We used a structured process for the identification and review of relevant literature.
We found that using only a small number of individual reference terms to identify the appropriate literature was not effective. A combination of several groups of terms was necessary to increase success rate in the search process. The approach used to conduct the systematic review was deemed appropriate despite the small amount of literature found that dealt with adherence and telemedicine services. The potential problem of low inter-rater reliability in our analysis was not an issue, since only one person was involved in the final round of the review process.
An in-depth aggregation of results using a meta-analysis would require the definition of a common set of criteria (e.g. objective of the study, duration and type of treatment, technology used, type of disease and comorbidity, and demographics of the participants) that ideally would be shared by the studies to be included. In the small number of relevant articles reviewed in this study, each group of authors had defined its own set of criteria. No general statement can be made regarding the impact of adherence on healthcare costs for patients with HF.
A holistic assessment of all relevant economic costs and outcomes related to patient adherence is therefore still needed. There is currently no evidence that increased patient adherence to pharmacological and non-pharmacological recommendations, supported by using telemedicine services, has led to a reduction in treatment costs (e.g. medical procedures, emergency room admissions, hospitalization, and nursing costs) for HF patients. Economic evaluation of telemedicine services was not a primary objective of the reviewed research papers.
Conclusion
The present review indicates the absence of an explicit examination of how adherence to pharmacological and non-pharmacological recommendations affects total healthcare costs.
A model-based cost-effectiveness analysis, with an appropriate and standardized conceptualization of adherence, has not yet been done. Such an analysis is needed to further elucidate the impact of adherence on the cost-effectiveness of telemedicine services for patients with chronic HF.
Footnotes
Clinical Relevance Statement
In the future, clinicians will increasingly need to decide whether telehealth components should be included in the routine treatment of chronically ill patients. Telehealth services can significantly influence adherence and vice versa, but the cost-related benefits of adherence are yet unclear.
Conflict of Interest
The authors declare that they have no conflicts of interest in the research.
Human Subjects Protections
Human and/or animal subjects were not included in the project.
References
- 1.Bundesministerium für Gesundheit. Bundes-Zielsteuerungsvertrag. Nr. 986167_B-ZV_26062013 [Internet]. 2013Jun [zitiert 2013 Okt. 20]. Erreichbar unter: http://www.hauptverband.at/mediaDB/986167_B-ZV_26062013_Letztfassung_Unterschrieben.pdf. German [Google Scholar]
- 2.Brussels. European Commission. E-Health Action Plan 2012–2020: Innovative healthcare for the 21st century. 2012 Dec. Report Nr. COM (2012) 736 final [Google Scholar]
- 3.Sabate E.World Health Organization, Geneva (Switzerland). Adherence to long-term therapies: evidence for action. 2003. ISBN 9241545992 [PubMed] [Google Scholar]
- 4.O’Neill K.U.S. Surgeon general joins Baltimore launch of the National Script Your Future Campaign to highlight importance of taking medication as directed [Internet]. 2011November [cited 2014 Jan. 23]. Available from: http://scriptyourfuture.org/wp-content/themes/cons/m/release.pdf [Google Scholar]
- 5.AIT [Internet]. Vienna. Pressegespräch: Herzschwäche-bessere Prognose durch Telemedizin; 14March2013. [zitiert 2014 Jan. 05]. Erreichbar unter: http://www.ait.ac.at/news-events/single-view/?no_cache=1&tx_ttnews[tt_news]=1472. German [Google Scholar]
- 6.Schreier G, Eckmann H, Hayn D, Kreiner K, Kastner P, Lovell N.Web versus App – compliance of patients in a telehealth diabetes management programme using two different Technologies. J of Telemedicine and Telecare 2012; 18: 476–480 [DOI] [PubMed] [Google Scholar]
- 7.Ramaekers BL, Janssen-Boyne JJ, Gorgels AP, Vrijhoef HJ.Adherence among telemonitored patients with heart failure to pharmacological and nonpharmacological recommendations. Telemedicine and e-Health 2009; 15(6): 517–524 [DOI] [PubMed] [Google Scholar]
- 8.Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [Internet]. PRISMA Statement. [cited 2014 Jan. 10]. Available from: http://www.prisma-statement.org/ [Google Scholar]
- 9.PubMed Database [Internet]. National Centre for Biotechnology Information. Available from: http://www.ncbi.nlm.nih.gov/pubmed/ [Google Scholar]
- 10.Google Scholar [Internet]. Available from: http://scholar.google.com [Google Scholar]
- 11.Banka G, Heidenreich PA, Fonarow GC.Incremental cost-effectiveness of guideline-directed medical therapies for heart failure. JACC 2013; 20(10): 1–7 [DOI] [PubMed] [Google Scholar]
- 12.Chen YH, Lin YH, Hung CS, Huang CC, Yeih DF, Chuang PY, Ho YL, Chen MF.Clinical outcome and cost-effectiveness of a synchronous telehealth service for seniors and nonseniors with cardiovascular diseases: quasi-experimental study. JMIR 2013; 15(4): e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Lusignan S, Wells S, Johnson P, Meredith K, Leatham E.Compliance and effectiveness of 1 year’s home telemonitoring. The report of a pilot study of patients with chronic heart failure. Europ J of HF 2001; 3: 723–730 [DOI] [PubMed] [Google Scholar]
- 14.Guzman-Clark JR, van Servellen G, Chang B, Mentes J, Hahn TJ.Predictors and outcomes of early adherence to the use of a home telehealth device by older veterans with heart failure. Telemedicine and e-Health 2013; 19(3): 217–223 [DOI] [PubMed] [Google Scholar]
- 15.Heinen-Kammerer T, Kiencke P, Motzkat K, Neller S, Liecker B, Petereit F, Hecke T, Müller H, Rychlik R.Telemedizin in der Tertiärprävention: Wirtschaftlichkeitsanalyse des Telemedizin-Projektes Zertiva bei Herzinsuffizienz-Patienten der Techniker Krankenkasse. Springer Berlin Heidelberg; 2006. pp 531–549 German [Google Scholar]
- 16.Pandor A, Thokala P, Gomersall T, Baalbaki H, Stevens JW, Wang J, Wong R, Brennan A, Fitzgerald P.Home telemonitoring or structured telephone support programmes after recent discharge in patients with heart failure: systematic review and economic evaluation. HTA 2013; 17(32). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rohde LE, Bertoldi EG, Goldraich L, Polanczyk CA.Cost-effectiveness of heart failure therapies. Nature reviews/Cardiology 2013; 10(6): 338–354 [DOI] [PubMed] [Google Scholar]
- 18.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS.Impact of medication Aadherence on hospitalization risk and healthcare cost. Medical Care 2005; 43(6): 521–530 [DOI] [PubMed] [Google Scholar]
- 19.Dávalos ME, French MT, Burdick AE, Simmons SC.Economic evaluation of telemedicine: review of the literature and research guidelines for benefit – cost analysis. Telemedicine and e-Health 2009; 15(10): 933–948 [DOI] [PubMed] [Google Scholar]
- 20.Ploier M.E-Health und Telemedizin: Haftungsfragen. J Hyperton 2011; 15 (1). [Google Scholar]
- 21.Statistics Austria, Population forecasts [Internet], 2013. Oct. Report: results_overview_austria_029024. Available from: https://www.statistik.at/web_en/statistics/population/demographic_forecasts/popu lation_forecasts/index.html [Google Scholar]
- 22.Austrian federal ministry of health. Gesundheit Österreich GmbH, editor. Financing and expenditure, in: The Austrian healthcare system, Key facts 2010, June2010. p18–21 ISBN 978–3–902611–38–3 [Google Scholar]