Summary
Objective
The amount of clinical information that anesthesia providers encounter creates an environment for information overload and medical error. In an effort to create more efficient OR and PACU EMR viewer platforms, we aimed to better understand the intraoperative and post-anesthesia clinical information needs among anesthesia providers.
Materials and Methods
A web-based survey to evaluate 75 clinical data items was created and distributed to all anesthesia providers at our institution. Participants were asked to rate the importance of each data item in helping them make routine clinical decisions in the OR and PACU settings.
Results
There were 107 survey responses with distribution throughout all clinical roles. 84% of the data items fell within the top 2 proportional quarters in the OR setting compared to only 65% in the PACU. Thirty of the 75 items (40%) received an absolutely necessary rating by more than half of the respondents for the OR setting as opposed to only 19 of the 75 items (25%) in the PACU. Only 1 item was rated by more than 20% of respondents as not needed in the OR compared to 20 data items (27%) in the PACU.
Conclusion
Anesthesia providers demonstrate a larger need for EMR data to help guide clinical decision making in the OR as compared to the PACU. When creating EMR platforms for these settings it is important to understand and include data items providers deem the most clinically useful. Minimizing the less relevant data items helps prevent information overload and reduces the risk for medical error.
Keywords: Anesthesia, electronic medical record, health information technology
1. Background
The combination of continuous monitoring and the ability of the electronic medical record (EMR) to store large amounts of data creates a potential for information overload when caring for critically ill patients [1]. This has been demonstrated in the operating room (OR) setting where omissions and inconsistencies relating to large amounts of data often occur [2]. The potential dangers underlying information overload relate to the inability of practitioners to discern pertinent from irrelevant information [3] and the accumulation of errors of cognition and performance associated with data corruption [4, 5].
A possible way to combat the risks of information overload center on the development and implementation of advanced health information technologies (HITs). The Institute of Medicine and the United States Department of Health and Human Services have both advocated for the enhanced creation and use of efficient EMRs [6]. Recently, the HIT for Economic and Clinical Health (HITECH) Act was enacted which has allocated federal funds to aid in this endeavor. Efforts to specifically improve perioperative HITs have been rewarded with improved efficiency and positive financial outcomes [7, 8]. Although it has not been systematically demonstrated, improvement in perioperative electronic medical record (EMR) interfaces is a potential way to improve patient safety as well [9].
Anesthesia providers face specific and unique challenges when dealing with large amounts of data, much of which is continuous in nature. To combat these challenges significant effort has been made towards improving the intraoperative display and presentation of data [10-14]. In addition, the creation and increased use of Anesthesia Information Management Systems (AIMS) has been shown to improve many aspects of health care delivery [15-17]. However, most AIMS are not connected with main hospital EMRs and lack data for continuity of care [18-20]. Practitioners often must use multiple software packages and query many information sources to have access to the necessary data. Such systems limit the transparency and integration of data and create multiple avenues for error [21]. As a result, the ability to create perioperative EMR interfaces with enhanced capacities to survey and aggregate data is of upmost importance [22].
The development of a novel EMR viewer platform, Ambient Warning and Response Evaluation (AWARE), at our institution resulted in improved performance and decreased errors of cognition in the ICU setting when compared to the standard EMR system [4]. The creation of this specific platform was based on expert panel input and data utilization models designed to assess the specific information needs of the unit [23, 24]. This design methodology is in contrast to the vendor-generated platforms most commonly used in hospital EMRs [25].
2. Objectives
While recognizing that information needs vary depending upon the specific task at hand (e.g. intraoperative monitoring has a distinct workflow with particular information requirements when compared to pre-operative evaluation) the primary objective of this study was to establish base information needs of perioperative clinicians in the intraoperative and post-anesthesia care settings. Integration of these elements into the workflow was not addressed or an objective of this study. To our knowledge, this is the first study that attempts to elucidate the exact clinical information needs of anesthesia practitioners. In the present study we address this gap in knowledge by using a modified Delphi process utilizing a survey to determine what data anesthesia providers find useful in clinical decision making for inclusion into future EMR viewer platforms.
3. Methods
3.1 Study Design
A web-based survey was conducted at Mayo Clinic, Rochester, MN, an academic tertiary health care center, equipped with a comprehensive EMR [26]. The Mayo Clinic has 112 ORs and 120 post-anesthesia care unit (PACU) beds distributed throughout its Rochester campus. The survey was conducted among anesthesia providers of varying clinical roles. The Institutional Review Board waived the requirement for written consent for the study.
3.2 Study Subjects
The survey was distributed to all anesthesia providers among 4 distinct clinical role designations: attending physicians (AP), certified registered nurse anesthetists (CRNA), physicians-in-training (PT) consisting of current anesthesia residents and fellows, and student registered nurse anesthetists (SRNA). There were a total of 518 possible survey participants with the number of providers in each role as follows: AP – 133, CRNA – 259, PT – 54, SRNA – 72.
3.3 Data Collection
3.3.1 Instruments
An expert panel, consisting of anesthesia APs, reviewed our current EMR and AIMS and identified 75 data elements considered important to clinical users in the OR and PACU setting. All data items are included in our current AIMS and EMR and would have been familiar to the respondent. Items were separated into the following categories for survey display: demographics (4 items), pre-operative clinical information (18 items), intraoperative physiologic information (13 items), intraoperative medication information (13 items), intraoperative lab information (7 items), clinical care (8 items), and practice management (12 items). Pre-operative clinical information items were selected as being intended for use in intraoperative management. Using a 7-point Likert scale (ranging from not needed to absolutely necessary) subjects were asked to rate each of the 75 data items as follows: “On a scale…indicate how important it is to have this information available to you on a screen, in the OR and/or PACU settings, as you go about your routine tasks.” A free-text box was included at the end of the survey allowing participants to identify clinical data points not included in the survey and to provide additional comments as desired.
3.3.2 Procedures
The survey was created using the LimeSurvey (www.limesurvey.org) web-based stand-alone tool installed inside the Mayo Clinic firewall and distributed to the study participants via email. In keeping with Delphi methodology the identity of participants and survey results were not recorded.
3.4 Data Analyses
Survey responses were collected and tabulated by Microsoft Excel 2010. In order to ensure consistency of results with similar studies performed at our institution the 7-point Likert scale was coded from 0 to 6. The mean was calculated for each data item with items then ranked in descending order for generation of proportional quarters. The percentage of participants ranking each individual data item as not needed (0 score) or absolutely necessary (6 score) was also determined. Each data item was analyzed individually to determine if there was any statistically significant inter-role rating variability. These analyses were done for both the OR and PACU setting independently.
Responses were further analyzed by determining each respondent’s cumulative mean for all data items as well as the percentage of items rated as absolutely necessary with analyses once again stratified according to clinical role. This data was also compared between the OR and PACU setting as well.
3.5 Statistics
The Kruskal-Wallis test was used to compare cumulative means and percentage of items rated as absolutely necessary among the 4 provider groups. If this test generated a p-value < 0.05 then a Tukey-Kramer test was used for pairwise comparisons. A Bland-Altman plot was used to assess the agreement of means between the OR and PACU setting for each provider. All descriptive statistics were performed in JMP (v 9.0.1, SAS Institute, Cary, NC); p < 0.05 was considered statistically significant. TABLEAU® software (Seattle, WA) was used for data visualization.
4. Results
Five-hundred and eighteen survey requests were distributed with 137 responses obtained, giving a response rate of 26%. Of the 137 surveys returned, 25 incomplete surveys were discarded with 5 others being excluded due to respondents either ranking all items as absolutely necessary (1 SRNA and 1 unknown role) or giving low scores for every data item (2 AP and 1 PT). The 107 surveys used for data analyses were distributed among the 4 clinical roles as follows: AP – 48 (response rate – 36%), CRNA – 35 (14%), PT – 17 (32%), SRNA – 7 (10%).
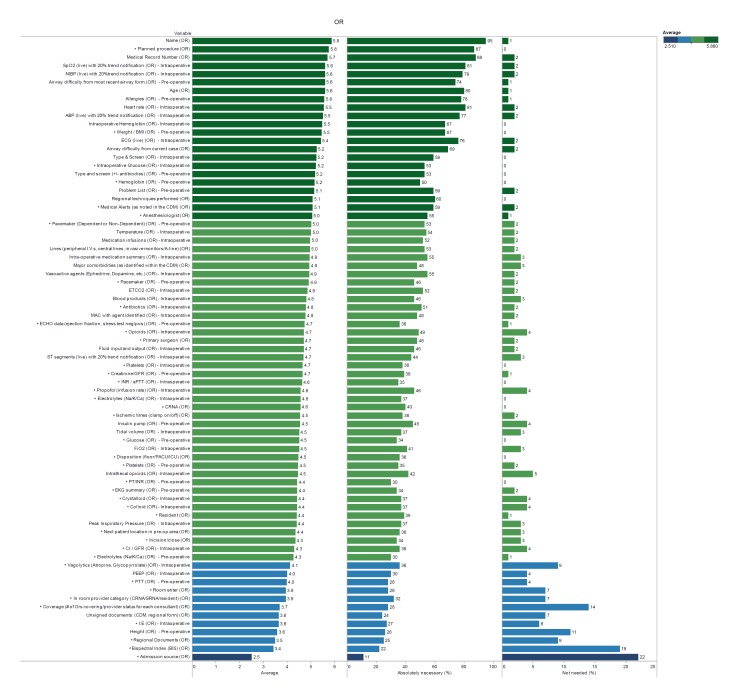
▶ Figure 1 shows each of the 75 data items listed by descending mean for the OR setting. The top 5 data items with the highest mean for the OR were name, planned procedure, medical record number, SpO2, and NIBP. The median data item rating was 4.7 (maximum 6) with 84% of the data items falling within the top 2 proportional quarters. All 4 demographic items (name, planned procedure, medical record, and age) were among the top 10 highest rated items. Seven of the 10 lowest rated items were either from the clinical care (bispectral index and regional documents) or practice management (admission source, unsigned documents, coverage, in room provider category, and room enter) domains.
Fig. 1.
Data categories in descending order of the mean as rated by anesthesia providers to the perceived importance of each in caring for patients in the OR setting. Proportional quarters are demonstrated by shading of the graph bars. Also shown are the percentages of respondents that rated each data category absolutely necessary and not needed. Data items that demonstrated statistically significant inter-role rating variability are marked with an asterisk (*).
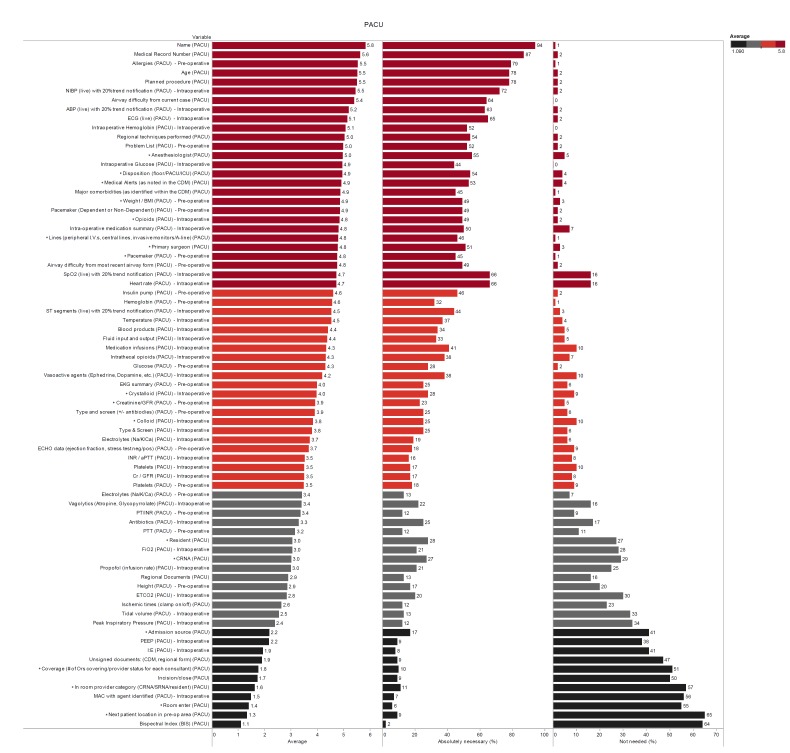
Similarly, ▶ Figure 2 displays the mean rankings of data items as rated for the PACU setting. The top 5 rated items for the PACU were name, medical record number, allergies, age, and planned procedure, four of which were from the demographic domain. As well, 7 of the 10 lowest rated items were either from the clinical care or practice management domains. The median PACU data item rating was 4.0 with only 65% of data items in the top 2 proportional quarters.
Fig. 2.
Data categories in descending order of the mean as rated by anesthesia providers to the perceived importance of each in caring for patients in the PACU setting. Proportional quarters are demonstrated by shading of the graph bars. Also shown are the percentages of respondents that rated each data category absolutely necessary and not needed. Data items that demonstrated statistically significant inter-role rating variability are marked with an asterisk (*).
Also displayed in ▶ Figure 1 and ▶ Figure 2 is the percentage of respondents that rated each item as absolutely necessary or not needed. Name received the highest percentage of responders rating it as an absolutely necessary data item in both the OR (95%) and PACU (94%) setting. Thirty of the 75 items (40%) received an absolutely necessary rating by more than 50% of respondents for the OR setting as opposed to only 19 of the 75 items (25%) in the PACU. Only 1 item (admission source) was rated by more than 20% of respondents as not needed in the OR compared to 20 data items (27%) in the PACU.
▶ Figure 1 and ▶ Figure 2 also identify specific data items that demonstrated statistically significant inter-role rating variability. There were 40 and 18 items that had inter-role variability in the OR and PACU settings respectively. Of the 40 items in the OR setting 23 (58%) were contained in the pre-operative clinical information and practice management domains. Only 1 of the 13 intraoperative physiological information data items (I:E) demonstrated inter-role rating variation. In the PACU setting variation existed for 10 of the 12 practice management data items. In the OR setting only 6 (15%) of the inter-role rating variations involved providers with similar training backgrounds (AP versus PT or CRNA versus SRNA) with 3 (17%) such variations occurring in the PACU setting.
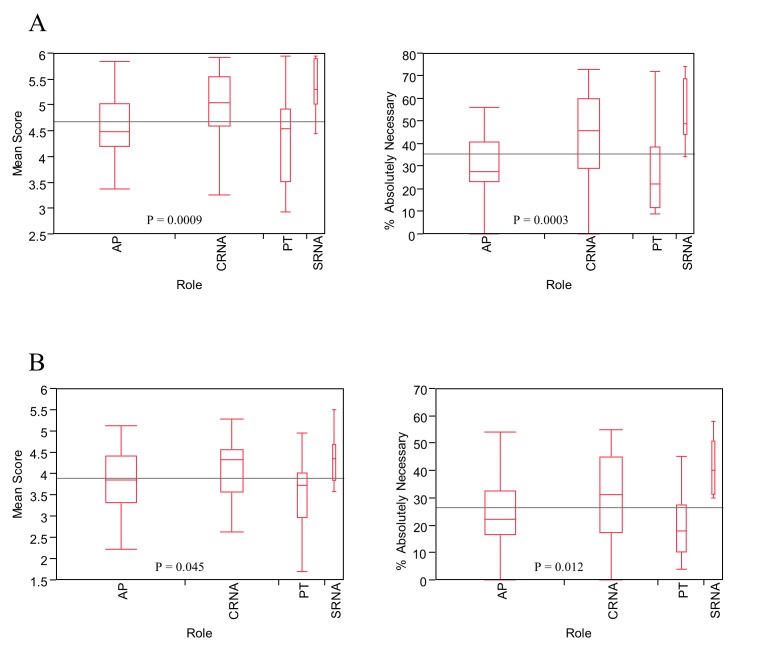
When overall rating means were stratified by clinical role there was a statistically significant difference in respondent’s combined mean for all data items as well as the percentage of items rated as absolutely necessary (▶ Figure 3). This significant difference was found in both the OR and PACU settings. The Tukey-Kramer test demonstrated statistically significant differences between CRNAs and PTs in both settings and SRNAs and PTs in the OR only. SRNAs and APs also differed significantly in the OR setting.
Fig. 3.
Variance in the overall mean score and percentage of items rated as absolutely necessary when stratified by clinical role in the OR (A) and PACU (B) setting. Data are displayed in box-whisker graphs (median, interquartile range, total range) with the lighter horizontal line showing the grand mean. The reported p values indicate the results of Kruskal-Wallis rank sums test.
Bland-Altman analyses (not shown) indicated that providers had overall higher means when rating data items in the OR setting compared to the PACU with a mean difference of 0.79 (95% CI: 0.69–0.89).
Analysis of free-text items did not reveal any information not already included in the survey or part of the study team’s objectives.
5. Discussion
We conducted a survey among anesthesia providers to assess the perioperative clinical information needs in an effort to create a more effective EMR viewer for the OR and PACU settings. To our knowledge this is the first study attempting to assess these specific needs in a systematic way. Our survey had a high absolute response number with participants distributed among 4 distinct clinical roles. The data demonstrates that anesthesia providers have more clinical information needs in the OR setting compared to the PACU, a finding that aligns with what one would expect clinically. This is evidenced by the fact that providers gave nearly 1 point higher overall mean for OR data items when compared to the PACU. In addition, the percentage of data items rated as absolutely necessary was almost double in the OR setting when compared to the PACU with a larger number of PACU items being rated as not needed.
Data items that ranked consistently high in both settings were demographic information such as name, age, planned procedure, and medical record number. Given the prevalence of surgical safety checklists in the study institution it is not surprising that demographic information was rated as being highly valuable in the operating room setting. The importance of these simple data items seem to agree with respondents from another study suggesting that uncertainty of patient identity is one of the leading causes of near misses in the OR [27]. Real-time physiological data, such as SpO2 and heart rate, were consistently rated as more important in the OR setting with items such as airway difficulty and allergies topping the PACU list.
In further analyses, there were statistically significant rating variations in both clinical settings when comparing between physicians (APs and PTs) and nurse anesthetists (CRNA and SRNA). Cumulative mean rating scores of APs and PTs tended to track together while both nurse anesthetists’ roles shared similar opinions regarding the importance of individual clinical data items. When comparing ratings for specific data items there were very few significant variations when comparing within the physician (AP versus PT) and nurse anesthetist (CRNA versus SRNA) roles respectively. These findings may highlight to whom anesthesia trainees and learners look to for modeling of clinical habits and perceptions. For example, in one study anesthesia residents, when compared to CRNAs, rated the quality and quantity of faculty guidance from attending anesthesiologists much more favorably [28]. Similarly, SRNA students gave much more positive ratings for clinical learning helpfulness to CRNA preceptors than to anesthesiologist preceptors or residents [29, 30].
The understanding of the clinical information needs of anesthesia providers is crucial to the creation of integrated EMR systems that help improve perioperative data flow and communication. Information accumulation and dispersion is a key component to patient safety in the perioperative setting [31]. As a result, much research has been dedicated to the improvement of communication and information transfer among the various clinical roles [32]. One study demonstrated that communication failures occur in approximately one-third of team exchanges with 35% of these failures being attributed to missing or inaccurate information [33]. In addition, there are also discrepancies in the perceived importance of different types of information between provider roles [34], a finding consistent with our results. For example, the practice management domain items demonstrated significant inter-role rating variation as APs rated these items much higher than respondents from the other roles, a finding expected secondary to differing role responsibilities.
Wong et al conducted mixed-method interviews among thirty-three OR team-members (surgeons, anesthesiologists, and nurses) to determine the importance and quality of information sources available [34]. When rating the importance of information sources there was a broad distribution with anesthesiologists receiving the highest quality rating. Those interviewed suggested that the creation of novel “IT system(s) to function as a central information repository” as a way to improve communication and information transfer.
In addition to intra-OR information communication, there is evidence of information corruption when transitioning to PACU care. Anwari surveyed PACU nurses regarding their impression of the quality of handovers received from the anesthesiologist caring for the patient in the OR. Among data items that were often not passed along included premedication details (missed 63% of the time) and intraoperative analgesia used (36%) [35]. By tailoring EMR interfaces to meet the needs of both the OR and PACU we equip anesthesiologists, already viewed as a reliable information source, with the tools necessary to combat information corruption and improve perioperative communication and ultimately patient safety.
This survey is the first step in a process of creating and adapting an EMR viewer that involves a design allowing for end-users to influence its final product. A methodical process such as this is important in creating an environment where the implementation of new technology is well accepted and tailored to the needs of the users [36]. Including anesthesia stake holders in the content of EMR systems is vital for improving acceptance following implementation [37]. Combining our survey results with the concepts of data transparency and integration [21] can optimize the customization of our systems-based EMR viewer (AWARE) for use at our institution with replication of similar systems in various perioperative settings.
Limitations in our study include the fact this survey was conducted at a single institution. Local biases and training practices may limit our finding’s generalizability to other institutions; however, the tailoring of needs to local preferences should be the focus of such processes. Nevertheless, duplication of our findings at other institutions may enhance validation and wide spread generalization of results. Despite the geographic generalizability limitations, the fact that our survey was distributed and completed by a wide variety of providers spread throughout multiple roles adds robustness and enhances local application.
It may also be questioned why we included CRNA and SRNA providers in the rating of PACU data items. Most academic institutions currently have PACUs that are staffed by registered nurses and PTs, with APs acting as supervisors with little, if any, CRNA/SRNA involvement. However, as nurse anesthetist’s roles increase and they are given more autonomy, their involvement in the care continuum of surgical patients will also evolve and increase [38]. For example, in the United States there are 16 states (including the authors’) that allow CRNAs to practice independently without medical supervision [39]. As a result, including CRNAs and SRNAs in the evaluation of PACU items seemed appropriate and important.
Another limitation of our study is the inability to determine how each survey participant determined importance of the data items. For example, it is possible that some may have determined importance based on the frequency of use while others may have put emphasis on data items that, if neglected, could lead to the most detrimental consequences. As a result, there were times when items were rated as not needed by some while at the same time being rated absolutely necessary by others. However, by allowing each respondent to determine their own interpretation of importance we were able to combine individual responses to generate population-based observations to help guide EMR platform development.
Analysis of pre-operative evaluations and management was not included as a priority of this survey. It would be important for future studies to focus on addressing the specific needs of providers during this important perioperative domain.
6. Conclusion
When surveyed, anesthesia providers demonstrated a larger need for OR data compared to the PACU to help guide clinical decision making. When creating EMR platforms for these settings it is important to understand and include data items providers deem the most clinically useful. Minimization of the less relevant data items can help prevent information overload and reduce the risk for medical errors. Future development of novel OR and PACU EMR interfaces should incorporate such concepts as described in this study.
Footnotes
Clinical Relevance Statement
It is imperative to configure EMR platforms that cater to the exact needs of anesthesia providers in the perioperative setting. To our knowledge, this is the first study that attempts to elucidate the exact perioperative clinical information needs and address this gap in knowledge. Practitioners and consumers can use this knowledge in helping them guide creation of perioperative specific EMR platforms for this unique clinical setting.
Conflict of Interest
Mayo Clinic and authors (VH, BWP) hold the patent application on AWARE technology referenced in this paper. AWARE is licensed to Ambient Clinical Analytics Inc. The results of the survey will inform modifications to AWARE for the OR and PACU clinical settings.
Financial Disclosure
None.
Funding Source
This publication was supported by Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Protection of Human and Animal Subjects
The study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects, and was reviewed by the Mayo Clinic Institutional Review Board.
References
- 1.Manor-Shulman O, Beyene J, Frndova H, Parshuram CS.Quantifying the volume of documented clinical information in critical illness. J Crit Care 2008; 23(2): 245–250 [DOI] [PubMed] [Google Scholar]
- 2.Driscoll WD, Columbia MA, Peterfreund RA.An observational study of anesthesia record completeness using an anesthesia information management system. Anesth Analg 2007; 104(6): 1454–1461 [DOI] [PubMed] [Google Scholar]
- 3.Potter AK, Johnson DP.Extracting the pertinent from the irrelevant. Minn Med 1994; 77(4): 58. [PubMed] [Google Scholar]
- 4.Ahmed A, Chandra S, Herasevich V, Gajic O, Pickering BW.The effect of two different electronic health record user interfaces on intensive care provider task load, errors of cognition, and performance. Crit Care Med 2011; 39(7): 1626–1634 [DOI] [PubMed] [Google Scholar]
- 5.Pickering BW, Hurley K, Marsh B.Identification of patient information corruption in the intensive care unit: using a scoring tool to direct quality improvements in handover. Crit Care Med 2009; 37(11): 2905–2912 [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine CoQoHCiA. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 1999 [Google Scholar]
- 7.Randa K.Using IT to drive operational efficiency in the OR. Healthc Financ Manage 2010; 64(12): 90–92, 94 [PubMed] [Google Scholar]
- 8.Foglia RP, Alder AC, Ruiz G.Improving perioperative performance: the use of operations management and the electronic health record. J Pediatr Surg 2013; 48(1): 95–98 [DOI] [PubMed] [Google Scholar]
- 9.Ellner SJ, Joyner PW.Information technologies and patient safety. Surg Clin North Am 2012; 92(1): 79–87 [DOI] [PubMed] [Google Scholar]
- 10.Blike GT, Surgenor SD, Whalen K.A graphical object display improves anesthesiologists’ performance on a simulated diagnostic task. J Clin Monit Comput 1999; 15(1): 37–44 [DOI] [PubMed] [Google Scholar]
- 11.Blike GT, Surgenor SD, Whalen K, Jensen J.Specific elements of a new hemodynamics display improves the performance of anesthesiologists. J Clin Monit Comput 2000; 16(7): 485–491 [DOI] [PubMed] [Google Scholar]
- 12.Charabati S, Bracco D, Mathieu PA, Hemmerling TM.Comparison of four different display designs of a novel anaesthetic monitoring system, the ’integrated monitor of anaesthesia (IMA)’. Br J Anaesth 2009; 103(5): 670–677 [DOI] [PubMed] [Google Scholar]
- 13.Wachter SB, Johnson K, Albert R, Syroid N, Drews F, Westenskow D.The evaluation of a pulmonary display to detect adverse respiratory events using high resolution human simulator. J Am Med Inform Assoc 2006; 13(6): 635–642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wachter SB, Markewitz B, Rose R, Westenskow D.Evaluation of a pulmonary graphical display in the medical intensive care unit: an observational study. J Biomed Inform 2005; 38(3): 239–243 [DOI] [PubMed] [Google Scholar]
- 15.Ehrenfeld JM, Rehman MA.Anesthesia information management systems: a review of functionality and installation considerations. J Clin Monit Comput 2011; 25(1): 71–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stol IS, Ehrenfeld JM, Epstein RH.Technology diffusion of anesthesia information management systems into academic anesthesia departments in the United States. Anesth Analg 2014; 118(3): 644–650 [DOI] [PubMed] [Google Scholar]
- 17.Spring SF, Sandberg WS, Anupama S, Walsh JL, Driscoll WD, Raines DE.Automated documentation error detection and notification improves anesthesia billing performance. Anesthesiology 2007; 106(1): 157–163 [DOI] [PubMed] [Google Scholar]
- 18.Egger Halbeis CB, Epstein RH, Macario A, Pearl RG, Grunwald Z.Adoption of anesthesia information management systems by academic departments in the United States. Anesth Analg 2008; 107(4): 1323–1329 [DOI] [PubMed] [Google Scholar]
- 19.Trentman TL, Mueller JT, Ruskin KJ, Noble BN, Doyle CA.Adoption of anesthesia information management systems by US anesthesiologists. J Clin Monit Comput 2011; 25(2): 129–135 [DOI] [PubMed] [Google Scholar]
- 20.Jamoom E, Beatty P, Bercovitz A, Woodwell D, Palso K, Rechtsteiner E.Physician adoption of electronic health record systems: United States, 2011. NCHS Data Brief 2012; 98: 1–8 [PubMed] [Google Scholar]
- 21.Rothman B, Sandberg WS, St Jacques P.Using information technology to improve quality in the OR. Anesthesiol Clin 2011March; 29(1): 29–55 [DOI] [PubMed] [Google Scholar]
- 22.Stabile M, Cooper L.Review article: the evolving role of information technology in perioperative patient safety. Can J Anaesth 201; 60(2): 119–126 [DOI] [PubMed] [Google Scholar]
- 23.Pickering BW, Gajic O, Ahmed A, Herasevich V, Keegan MT.Data utilization for medical decision making at the time of patient admission to ICU. Crit Care Med 2013; 41(6): 1502–1510 [DOI] [PubMed] [Google Scholar]
- 24.Pickering BW, Herasevich V, Ahmed A, Gajic O.Novel Representation of Clinical Information in the ICU: Developing User Interfaces which Reduce Information Overload. Appl Clin Inform 2010; 1(2): 116–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frassica JJ.CIS: where are we going and what should we demand from industry? J Crit Care 2004; 19(4): 226–233 [DOI] [PubMed] [Google Scholar]
- 26.Carpenter PC.The electronic medical record: perspective from Mayo Clinic. Int J Biomed Comput 1994; 34(1–4): 159–171 [DOI] [PubMed] [Google Scholar]
- 27.Haugen AS, Murugesh S, Haaverstad R, Eide GE, Softeland E.A survey of surgical team members’ perceptions of near misses and attitudes towards Time Out protocols. BMC Surg 2013; 13: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dexter F, Logvinov II, Brull SJ.Anesthesiology residents’ and nurse anesthetists’ perceptions of effective clinical faculty supervision by anesthesiologists. Anesth Analg 2013; 116(6): 1352–1355 [DOI] [PubMed] [Google Scholar]
- 29.Elisha S, Rutledge DN.Clinical education experiences: perceptions of student registered nurse anesthetists. AANA J 2011; 79(4 Suppl.): S35–S42 [PubMed] [Google Scholar]
- 30.Meno KM, Keaveny BM, O’Donnell JM.Mentoring in the operating room: a student perspective. AANA J 2003; 71(5): 337–341 [PubMed] [Google Scholar]
- 31.Mills P, Neily J, Dunn E.Teamwork and communication in surgical teams: implications for patient safety. J Am Coll Surg 2008; 206(1): 107–112 [DOI] [PubMed] [Google Scholar]
- 32.Nagpal K, Vats A, Lamb B, Ashrafian H, Sevdalis N, Vincent C, Moorthy K.Information transfer and communication in surgery: a systematic review. Ann Surg 2010; 252(2): 225–239 [DOI] [PubMed] [Google Scholar]
- 33.Lingard L, Espin S, Whyte S, Regehr G, Baker GR, Reznick R, Bohnen J, Orser B, Doran D, Grober E.Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care 2004; 13(5): 330–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wong HW, Forrest D, Healey A, Shirafkan H, Hanna GB, Vincent CA, Sevdalis N.Information needs in operating room teams: what is right, what is wrong, and what is needed? Surg Endosc 2011; 25(6): 1913–1920 [DOI] [PubMed] [Google Scholar]
- 35.Anwari JS.Quality of handover to the postanaesthesia care unit nurse. Anaesthesia 2002; 57(5): 488–493 [DOI] [PubMed] [Google Scholar]
- 36.Rikli J, Huizinga B, Schafer D, Atwater A, Coker K, Sikora C.Implementation of an electronic documentation system using microsystem and quality improvement concepts. Adv Neonatal Care 2009; 9(2): 53–60 [DOI] [PubMed] [Google Scholar]
- 37.Gocsik T.Last man standing? Advice for engaging anesthesia clinicians when implementing an EMR in anesthesiology services. Healthc Inform 2012; 29(10): 32, 7 [PubMed] [Google Scholar]
- 38.Schreiber R, MacDonald M.A closer look at the „supervision“ and „direction“ of certified registered nurse anesthetists. Can Nurse 2008; 104(3): 28–33 [PubMed] [Google Scholar]
- 39.Matsusaki T, Sakai T.The role of Certified Registered Nurse Anesthetists in the United States. J Anesth 2011; 25(5): 734–740 [DOI] [PubMed] [Google Scholar]