Abstract
BACKGROUND:
Compared with other parents, mothers of children with autism spectrum disorder or other neurodevelopmental disabilities experience more stress, illness, and psychiatric problems. Although the cumulative stress and disease burden of these mothers is exceptionally high, and associated with poorer outcomes in children, policies and practices primarily serve the identified child with disabilities.
METHODS:
A total of 243 mothers of children with disabilities were consented and randomized into either Mindfulness-Based Stress Reduction (mindfulness practice) or Positive Adult Development (positive psychology practice). Well-trained, supervised peer mentors led 6 weeks of group treatments in 1.5-hour weekly sessions, assessing mothers 6 times before, during, and up to 6 months after treatment. Mothers had children with autism (65%) or other disabilities (35%). At baseline, 85% of this community sample had significantly elevated stress, 48% were clinically depressed, and 41% had anxiety disorders.
RESULTS:
Using slopes-as-outcomes, mixed random effects models, both treatments led to significant reductions in stress, depression, and anxiety, and improved sleep and life satisfaction, with large effects in depression and anxiety. Mothers in Mindfulness-Based Stress Reduction versus Positive Adult Development had greater improvements in anxiety, depression, sleep, and well-being. Mothers of children with autism spectrum disorder improved less in anxiety, but did not otherwise differ from their counterparts.
CONCLUSIONS:
Future studies are warranted on how trained mentors and professionals can address the unmet mental health needs of mothers of children with developmental disabilities. Doing so improves maternal well-being and furthers their long-term caregiving of children with complex developmental, physical, and behavioral needs.
Keywords: autism spectrum disorders, developmental disabilities, maternal stress and mental health, mindfulness based stress reduction, positive psychology
What’s Known on This Subject:
Mothers of children with neurodevelopmental disabilities often experience poor health, high stress, anxiety, and depression. Highly stressed parents are less effective in their parenting roles, risking their children's developmental progress.
What This Study Adds:
Evidence-based interventions in mindfulness and positive psychology significantly reduce distress in mothers of children with disabilities. Well-trained peer-mentors are effective interventionists. Adult-oriented services are needed for these mothers to improve their mental health and sustain their caregiving over the long-term.
Compared with mothers of typically developing children, mothers of children with neurodevelopmental disabilities experience more stress, psychiatric problems, and poorer health.1 Higher levels of stress in these parents are predicted by economic hardship,2 insufficient supports,3,4 and such child problems as aggression, self-injury, and social or communicative deficits.5,6 Although the positive aspects of raising children with disabilities are increasingly recognized,7 studies in this population consistently find maternal susceptibility to depressive and anxiety disorders or symptoms,8,9 insomnia, poor sleep quality,10 and stress chronicity marked by blunted diurnal cortisol trajectories,11,12 reduced immune functioning,13 and accelerated telomere shortening.14 Because neurodevelopmental disorders are prevalent, comprising the top 5 chronic medical conditions affecting US children,15 the cumulative disease burden of these parents is alarmingly high, adding to the growing costs to society of autism spectrum disorders (ASD) or other developmental disabilities.16
Highly stressed parents are less able to implement interventions for their children with disabilities, and their children make less developmental progress.17 Even so, services for families of children with disabilities primarily focus on the child’s needs. Thus, parents may be taught strategies to facilitate their children’s cognitive, linguistic, physical, or social development or to manage their difficult behaviors.18 Parent interventions also include anticipatory guidance about the child’s disability, advocacy training, involvement in disability-specific organizations, and respite care or “short breaks” from round-the-clock caregiving.19
Although parent training can lead to modest collateral benefits on maternal stress,20 and disability organizations provide support and advice, these programs were not developed to treat parental mental health. Similarly, respite care provides parents a welcomed reprieve,19 but does not teach them how to cope with stress once the break is over.
This study instead treated parental distress directly, with business as usual for children. Although treating parents is much less common than child-oriented interventions, cognitive-behavioral therapies can effectively reduce distress in mothers of children with developmental disabilities or chronic health problems.20 Individual psychotherapies, however, rely on professionals, which may prove costly, and do not necessarily reach at-risk mothers who are stressed but do not seek formal clinical care. This study thus used peer-mentors (well-trained mothers of offspring with disabilities) to lead group interventions in community settings, thereby taking advantage of naturally occurring parent-to-parent rapport.
Parents were randomly assigned to either Mindfulness-Based Stress Reduction (MBSR), which has demonstrated efficacy across both clinical and healthy populations,21,22 or Positive Adult Development (PAD), which incorporated evidence-based interventions from positive psychology.23,24 These interventions were selected because they were conducive to group formats led by trained mentors, and controlled studies find that they effectively enhance well-being and reduce anxiety, depression, and sleep problems in other clinical populations.25 Further, mindfulness practice has been piloted in other parent groups,26 and concepts in positive psychology, such as maximizing virtues, abilities, and optimism, resonate with the disability community.7
This study’s first aim tested whether it would be beneficial to treat parents in groups led by peer-mentors by using adult-oriented curricula. In the second aim, we tested our expectation that even though both interventions would be effective, MBSR would confer some advantages over PAD. MBSR has a larger literature supporting its efficacy, and even beginners show robust neural changes linked to mindfulness practice.27 Third, because mothers of children with autism (versus with other disabilities) often report more stress, illness, and psychiatric symptoms,8,28 we determined if mothers of children with ASD responded differently to treatment.
Methods
Identifying and Enrolling Participants. Parents of any age were recruited as long as they were the primary caregivers of offspring with developmental disabilities. Eligibility criteria also included willingness to be randomized into groups, and no previous training in mindfulness or positive psychology practices. Current or past psychiatric problems were not used as eligibility criteria. The study was advertised via Web sites and announcements to local and state disability organizations. To maximize enrollment, treatment sessions were offered during the day or evening in an accessible community setting, with optional, on-site child care for offspring with disabilities or siblings. Parents who used child care services (42.1%) did not differ from other participants at baseline or treatment response.
As shown in Table 1, mothers averaged 40 years of age, and most were married (73%) and white (70%). Similar numbers of participants had either high or low annual incomes, with 38% falling below the US median income level. Offspring with disabilities averaged 10 years of age, 65% had ASD, and 35% had other developmental disabilities.
TABLE 1.
Participant Demographic Features and Baseline Outcome Measures
| Demographic features | |
| Age, mean (SD), range | 40.87 (8.92), 23–76 y |
| Married % | 73 |
| Number in household, mean (SD), range | 4.07 (1.34), 2–9 |
| Employed outside home, % | 47.5 |
| Race, % | |
| White | 69.6 |
| African American | 14.7 |
| Hispanic | 9.2 |
| Asian, other | 6.5 |
| Education, % | |
| High school degree | 29.9 |
| 2 or 4 y college | 44.7 |
| Professional | 25.4 |
| Annual income $, % | |
| <15 000–29 000 | 18.3 |
| 30 000–49 000 | 19.3 |
| 50 000–59 000 | 20.2 |
| 70 000–99 000 | 23.4 |
| >100 000 | 18.8 |
| Child features | |
| Age, mean (SD), range | 10.85 (7.53) 2–54 y |
| Male, % | 72.3 |
| ASD, % | 64.9 |
| Autistic disorder | 36.1 |
| PDD-NOS | 14.4 |
| Asperger disorder | 14.4 |
| Other developmental disabilities, % | 35.1 |
| Genetic syndromes | 9.1 |
| Developmental disabilities | 20.0 |
| Psychiatric disorders | 6.0 |
| Baseline outcome measures | |
| BDI, mean (SD) | 19.99 (10.86) |
| BDI clinically significant, % (score ≥ 20) | 47.3 |
| BAI, mean (SD) | 13.41 (9.56) |
| BAI clinically significant, % (score ≥ 16) | 35.7 |
| Insomnia Inventory, mean (SD) | 12.33 (6.43) |
| PSI-Parent Distress, mean (SD) | 36.80 (8.51) |
| PSI-Dysfunctional Interactions, mean (SD) | 30.91 (8.17) |
| PSI-Difficult Child, mean (SD) | 40.79 (9.53) |
| PSI-clinically significant total scores, % | 86.5 |
| Life Satisfaction Scale, mean (SD) | 17.59 (6.66) |
| Psychological Well-Being, mean (SD) | 73.66 (12.73) |
PDD-NOS, pervasive developmental disorders-not otherwise specified.
Randomization. All participants provided written, informed consent using institutional review board–approved procedures. After completing baseline measures, they were randomly assigned via a computer program to either the MBSR or PAD 6-week group intervention. Parents who attended as couples (n = 50) were yoked and randomized together into a treatment arm. No significant differences in baseline characteristics or treatment responses were found between mothers who attended singly or with their spouses. Fathers’ treatment responses are analyzed separately later.
Outcome Assessments. Outcomes were assessed in 6 waves at baseline, midtreatment, at the end of treatment, and posttreatment at 1, 3, and 6 months. Mothers were thus enrolled in the study for 8 months between March 2010 and December 2012.
Outcomes were standardized measures often in clinical or developmental disabilities research. The primary outcome, the Parenting Stress Index-Short Form (PSI),29 contains 3 domains: Parental Distress, Dysfunctional Parent-Child Interactions, and Difficult Child. Although we report all 3, the PSI Parental Distress domain was most pertinent, as we did not treat children or expect dramatic changes in child problems. Secondary outcomes included the Beck Depression Inventory (BDI),30 Beck Anxiety Inventory (BAI),31 Insomnia Severity Index,32 Ryff Scales of Psychological Well-Being (short form total score),33 and the Life Satisfaction Scale.34 For each outcome, higher scores indexed more of the measured construct.
Mentor Training, Supervision, and Treatment Fidelity. Four well-trained, supervised peer-mentors, all mothers of children with disabilities, led the group interventions, 2 per treatment arm. Mentors received 4 months of training on the intervention curriculum, role of a mentor, and research ethics. Mentors enrolled in either MBSR classes or online positive psychology training, completed directed readings, and engaged in regular mindfulness or positive psychology practices. A social worker provided instruction on mentorship, including lessons on professional boundaries, confidentiality, and identifying participants in need of professional services. Mentors received institutional review board certification by taking online and university classes on the responsible conduct of research and data integrity.
Subsequent to training, a social worker or psychologist observed mentors during treatment sessions and met with them weekly for supervision. Clinical supervisors also ensured high treatment fidelity based on well-accepted criteria: preparing meeting rooms and materials, establishing group guidelines, adhering to weekly lessons and content, ensuring participant understanding of materials, reviewing homework, and properly collecting data.35
Treatment Groups. Peer-mentors co-led weekly groups, which never exceeded 15 participants. MBSR taught specific breathing, meditation, and movement techniques, including paying attention to the breath; deep belly breathing; the relaxation response; self-observation without self-evaluation; Qigong (gentle movements); and the sitting, body scan, and loving-kindness meditations.22,25 PAD emphasized ways to temper such emotions as guilt, conflict, worry, and pessimism by identifying and recruiting character strengths and virtues, by using strengths in new ways, and by exercises involving gratitude, forgiveness, grace, and optimism.23,24 All participants were encouraged to practice specific exercises at home and share these experiences at group meetings. The MBSR and PAD curricula will soon be available at the Vanderbilt Center for Technology Transfer and Commercialization Web site (www.vanderbilt.edu/cttc/).
Statistical Power. We conducted a longitudinal power analysis36 on a hypothetical outcome, assuming an n of 100 per group and traditional standards (power = 80%, 2-sided tests, α < 0.05). This yielded a minimum detectable effect size (ES) of d = 0.33 at the last wave, or power to detect small- to medium-sized differences in time slopes. Our minimum ES is in the range of treatment effects reported in recent meta-analyses of positive psychology37 (ES = 0.31) and mindfulness38 (ES = 0.51) interventions.
Statistical Analyses. For each outcome, we used a common approach for longitudinal data: a slope-as-outcome, mixed random-effects model.36,39 Multiwave longitudinal modeling takes advantage of all available observations; thus, incomplete cases are not dropped or are missing values imputed. Assuming that the untestable theory of missing at random holds, this strategy yields findings that are not biased.36,39
Mothers had up to 6 unique wave-time observations, with average wave-times for the sample of 0.00, 0.73, 1.32, 2.64, 4.49, and 7.71 months. The first 3 points measured outcomes before, during, and after treatment, and the last 3 points, during follow-up. We used 2, piecewise slopes that represented 2 study epochs: changes during treatment, and changes during follow-up. As clinical trials often use a single-slope model, we tested the 2-slope against the traditional 1-slope model by using maximum likelihood and Bayesian χ2 analyses. For all outcomes, the 2-slope model was a significantly better, more accurate fit (χ2 (1) > 32.00, P < .001).
The analytic model was simple, focused only on answering the 3 study aims. Given the high number of possible covariates (eg, maternal age, SES), we used the strength of existing literature8,28 to select just 1 important covariate, child ASD versus non-ASD, to model on intercept and slope parameters. Effect sizes were calculated by using Cohen’s d formula40 (M1 − M2/SDpooled), corrected for dependence among means. All outcomes were standardized to a mean of 0 and SD of 1, allowing further magnitude of change comparisons across measures.
Results
Enrollment
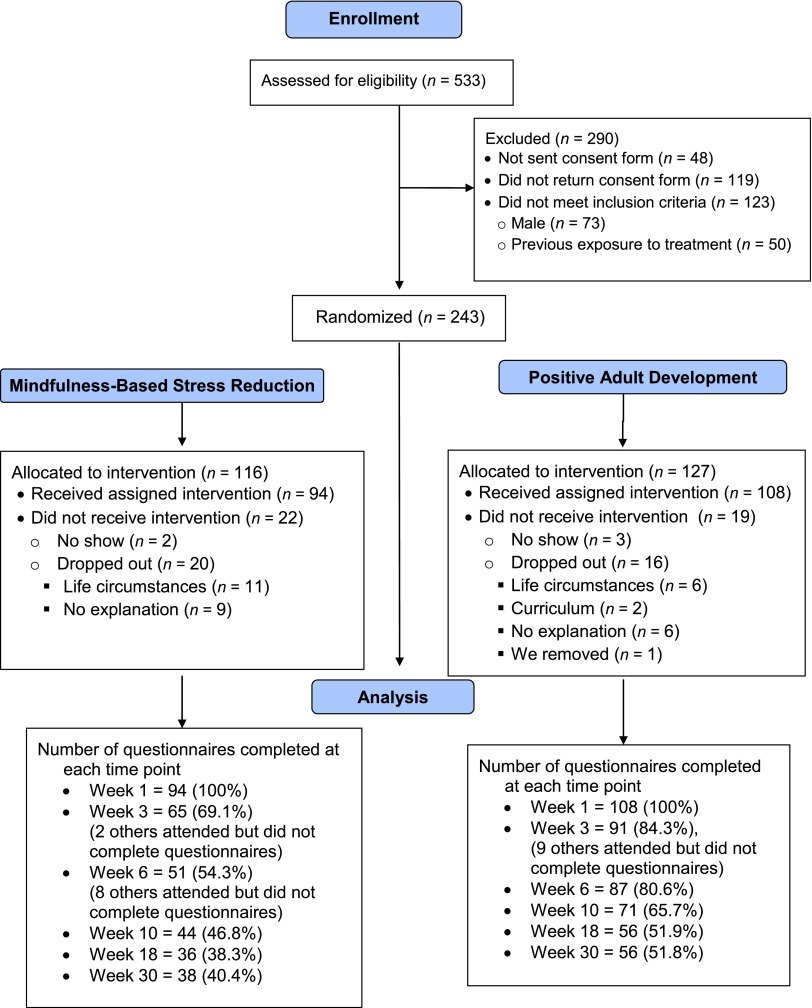
Figure 1 shows that of the 533 assessed for eligibility, 167 did not complete consent procedures, and 123 were not deemed eligible for the study (ie, children did not have developmental disabilities, fathers, already exposed to treatment). This left 243 women who were randomized into MBSR or PAD; no baseline differences were found in mothers or children across treatments. Once enrolled, most women completed treatment (n = 202); no adverse events were reported. Reasons for dropping out (n = 41) were primarily attributed to life circumstances (eg, family crises, unexpected events). The t tests revealed no significant demographic or baseline differences between those who dropped out versus completed treatment. Follow-up 2×2 ANOVAs (MBSR versus PAD by dropouts versus completers) revealed no significant main or interaction effects in baseline assessments or demographics, indicating no apparent differential dropout biases.41
FIGURE 1.
Participant enrollment.
Baseline Characteristics
Table 1 summarizes mean baseline scores on outcome measures. Even though a positive psychiatric history was not an eligibility criterion, 47% had clinically elevated depression scores on the BDI; 36% exceeded anxiety clinical cut-points on the BAI, and most, 87%, had clinically elevated stress scores on the PSI. These elevations are consistent with participants’ descriptions of their previous diagnoses of depressive (48.0%) or anxiety (40.6%) disorders, and use of psychotropic medications (58.0%). Mean Insomnia Severity scores indicated subthreshold insomnia, and mean Life Satisfaction scores were slightly below average.
Aim 1
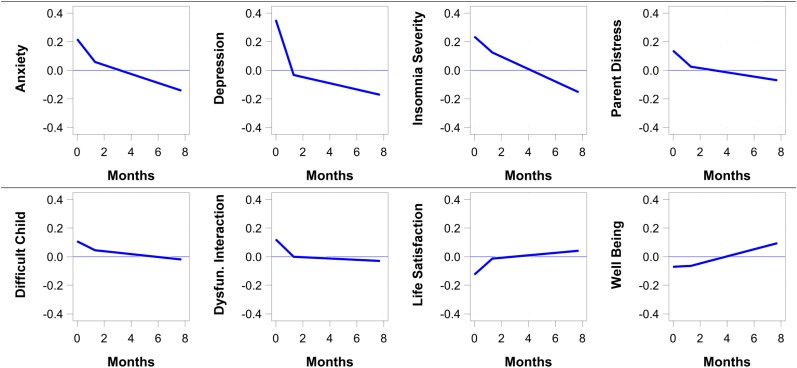
To determine if maternal distress improved during treatment or follow-up for the sample as a whole, 8 unconditional regression models were analyzed that included only the within-persons time variables. Results are presented in Table 2 and Fig 2. Mothers showed significant improvements during treatment in primary outcomes of parental distress and dysfunctional parent-child interactions as well as in 4 secondary outcomes of anxiety, depression, insomnia severity, and life satisfaction.
TABLE 2.
Estimates and SEs from “Unconditional” Models With Only Between-Persons Variables
| Anxiety | Depression | Insomnia Severity Total | Parent Distress | Difficult Child | Dysfunctional Parent-Child Interactions | Life Satisfaction | Psychological Well-Being Total | |
|---|---|---|---|---|---|---|---|---|
| Time 1 Intercept | 0.22** (0.07) | 0.35** (0.07) | 0.24** (0.07) | 0.14* (0.07) | 0.11 (0.07) | 0.12 (0.07) | –0.13 (0.07) | –0.07 (0.07) |
| Treatment slope | –0.12** (0.03) | –0.29** (0.03) | –0.08** (0.03) | –0.08* (0.03) | –0.05 (0.03) | –0.09** (0.03) | 0.08** (0.03) | 0.01 (0.03) |
| Follow-up slope | –0.03* (0.01) | –0.02* (0.01) | –0.04** (0.01) | –0.01 (0.01) | –0.01 (0.01) | –0.00 (0.01) | 0.01 (0.01) | 0.02* (0.01) |
P < .05. **P < .01.
FIGURE 2.
Plot of unconditional model score plots showing treatment and follow-up slopes for the whole sample. Note: For Anxiety, Depression, Insomnia Severity, Parent Distress, Difficult Child, and Dysfunctional Parent-Child Interaction, higher scores indicate worse functioning. For Life Satisfaction and Psychological Well-Being, higher scores indicate better functioning.
Overall, participants continued to improve or maintain gains during follow-up; no outcomes significantly worsened. From baseline through the end of the 6-month follow-up period improvements of large magnitudes were found in anxiety (Cohen’s d = 0.81) and depression (d = 0.98), medium effects in insomnia (d = 0.67) and personal distress (d = 0.49), and smaller effects in life satisfaction (d = −0.43) and dysfunctional parent-child interactions (d = 0.29). Psychological well-being, which did not change during intervention, began to improve during follow-up (d = −0.38).
Aims 2 and 3
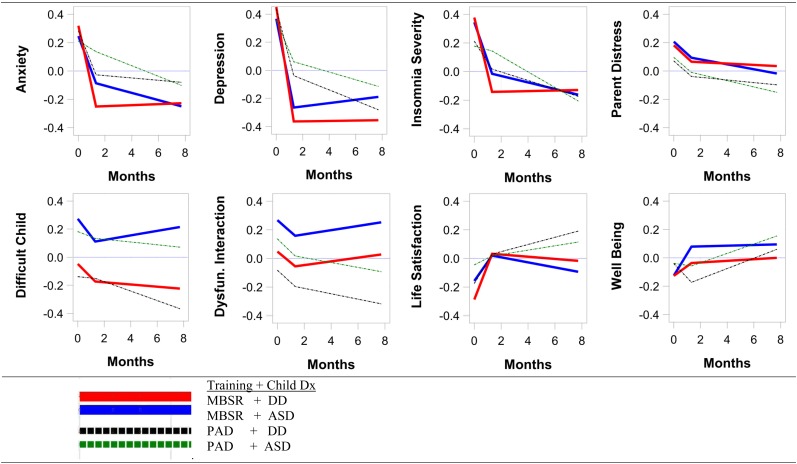
To test if treatment or follow-up responses depended on the type of treatment or child’s disability, between-person’s variables of treatment type (MBSR versus PAD) and child’s disability (ASD versus other disabilities) were entered into the regression models. Results are shown in Table 3 and Fig 3. With randomization, no baseline differences were found between treatment groups (intercept findings; Table 3). Mothers of children with ASD scored higher than other mothers on just 1 variable, the PSI’s Difficult Child domain.
TABLE 3.
Estimates and SEs From “Conditional” Models That Include Treatment Condition and Type of Disability
| Anxiety | Depression | Insomnia Severity | Parental Distress | Difficult Child | Dysfunctional Parent-Child Interaction | Life Satisfaction | Psychological Well-Being | |
|---|---|---|---|---|---|---|---|---|
| Time 1 Intercept | 0.28* (0.14) | 0.44** (0.13) | 0.21 (0.13) | 0.07 (0.13) | –0.14 (0.13) | –0.08 (0.13) | –0.18 (0.13) | –0.04 (0.13) |
| MBSR (vs PAD) | 0.03 (0.14) | 0.01 (0.13) | 0.17 (0.14) | 0.11 (0.14) | 0.09 (0.14) | 0.13 (0.14) | –0.11(0.14) | –0.08 (0.14) |
| ASD (vs DD) | –0.07 (0.15) | –0.08 (0.14) | –0.03 (0.15) | 0.02 (0.15) | 0.32* (0.14) | 0.22 (0.15) | 0.13 (0.14) | 0.00 (0.14) |
| Treatment slope | –0.24** (0.08) | –0.36** (0.08) | –0.15 (0.08) | –0.08 (0.08) | –0.01 (0.07) | –0.09 (0.08) | 0.16* (0.07) | –0.10 (0.07) |
| MBSR (vs PAD) | –0.20* (0.08) | –0.26** (0.08) | –0.25** (0.08) | –0.01 (0.08) | –0.08 (0.07) | 0.01 (0.08) | 0.09 (0.07) | 0.17* (0.07) |
| ASD (vs DD) | 0.18* (0.08) | 0.14 (0.08) | 0.12 (0.08) | 0.00 (0.09) | –0.03 (0.08) | –0.00 (0.09) | –0.11 (0.08) | 0.08 (0.07) |
| Follow-up slope | –0.01 (0.02) | –0.04* (0.02) | –0.03 (0.02) | –0.01 (0.02) | –0.03* (0.01) | –0.02 (0.02) | 0.03 (0.01) | 0.04 (0.02) |
| MBSR (vs PAD) | 0.01 (0.02) | 0.04* (0.02) | 0.03 (0.02) | 0.00 (0.02) | 0.03 (0.02) | 0.03 (0.02) | –0.03* (0.02) | –0.03 (0.02) |
| ASD (vs DD) | –0.03 (0.03) | 0.01 (0.02) | –0.02 (0.02) | –0.01 (0.02) | 0.02 (0.02) | 0.00 (0.02) | –0.01 (0.02) | –0.00 (0.02) |
DD, other developmental disabilities. *P < .05. **P < .01.
FIGURE 3.
Model score plots showing treatment and posttreatment slopes for treatment condition (MBSR versus PAD) and type of disability (ASD versus other developmental disabilities [DD]).
Figure 3 shows that both groups declined in primary stress outcomes, but participants in MBSR versus PAD showed greater improvements during treatment in anxiety (d’s = 0.88 vs 0.44), depression (d’s = 1.03 vs 0.58), and insomnia (ds = 1.10 vs 0.26). Only 1 treatment difference emerged between disability groups: mothers of children with ASD improved less in anxiety. Still, from baseline to 6-month follow-up, these mothers showed a large, gradual attenuation of anxiety (d = 0.94).
Change at follow-up was generally similar for those in MBSR versus PAD, and for mothers of children with or without ASD. However, relative to mothers in MBSR, those in PAD experienced more improvement in depression and life satisfaction during follow-up.
Discussion
Chronic stress impairs health, well-being, and the ability to learn and retain information.42 But even given the enormous public health cost of stress, we have yet to fully appreciate how chronic stress affects the health and mental health of mothers of children with neurodevelopmental disabilities, as well as their child-rearing practices. Instead of the usual child-oriented interventions, this study treated parent distress by using adult-oriented, evidence-based strategies.
Mothers in both the MBSR and PAD treatments showed less personal stress and dysfunctional parent-child interactions on the primary outcome, as well as less anxiety and depression, and improved sleep and life satisfaction. Depression, anxiety, and life satisfaction continued to improve during follow-up and improvements in other areas were sustained up to 6 months after treatment. Effect sizes were medium to large for depression and anxiety in both treatments from baseline to 6-month follow-up. Such improvements across groups are likely due to a confluence of shared treatment factors: a group setting with other parents, peer-mentors who could readily understand participants’ experiences, and programs that jettisoned traditional parent training and instead met parental needs to be less stressed and more engaged in their own adult development.
Although no differential treatment effects were found in primary stress indices, mothers enrolled in MBSR (versus PAD) showed significantly greater improvements, with larger effect sizes, in depression, anxiety, sleep, and life satisfaction. Such advantages in MBSR may be associated with the immediacy of physiologic relaxation responses incurred in mindfulness practice, including strengthened attention to bodily sensations, and less reliance on rumination or other automatic emotions.21,27 The PAD interventions, however, were more cognitively oriented, with exercises that require more time and reflection (eg, identifying and engaging character strengths, practicing kindness and gratitude).24 Indeed, mothers in PAD versus MBSR reported improved life satisfaction and reduced depression during the longer follow-up period. Both treatments were advantageous, however, and new work aims to integrate features of mindfulness and positive psychology interventions.43
In contrast to previous literature, mothers of children with ASD versus other disabilities did not report more distressful affect. However, no such group differences are also seen when child variables are well controlled,44 or when mothers are grouped by a stress biomarker instead of their child’s diagnosis.12 Response to treatment also was similar across diagnostic groups, although mothers of children with ASD showed less immediate improvements in anxiety. This dampened response may relate to the broader autism phenotype, or presumptive genetic vulnerability to mild social, anxiety, or cognitive symptoms in first-degree relatives of individuals with ASD.45 These mothers may thus warrant more intensive or longer anxiety treatments.
Taking advantage of parent-to-parent rapport, we found that well-trained, supervised peer-mentors are effective interventionists. This approach meets urgent calls to improve global mental health by training nonspecialists to address unmet mental health needs.46,47 These same calls also highlight needs to integrate mental health screening or services into primary health care settings. Although pediatricians are uniquely well positioned to screen mothers of patients with disabilities, multiple challenges remain in doing so.48–50
A limitation of this study is that we did not use an untreated control group, and thus cannot conclude that either intervention was associated with better maternal outcomes than no treatment. However, untreated mothers of offspring with disabilities do not necessarily become less depressed over time; indeed by early old age they experience more health and mental health problems than they did in middle-age, and at higher rates than control parents.51 Further, meta-analyses of studies from the 1980s onward show no hints of decreased maternal mental health vulnerabilities over the years.8,28 Given this historical context, we used a comparative effectiveness design that applies interventions already proven to be effective in controlled studies to real-world settings and high-risk groups.
A second limitation is that we did not test effects of maternal improvements on child functioning. It is well known, however, that maternal depression has detrimental effects on children, and that child outcomes improve when maternal depression is well-treated.52 We found modest improvements in dysfunctional parent-child interactions primarily during treatment. Improved maternal mental health may thus set the stage for better child functioning, but these mothers may benefit even further with additional help in parenting strategies.
Other limitations also deserve mention, including that outcome measures relied on self-reports. One could argue, however, that maternal self-perceptions are exactly what treatment aimed to change. Even so, future studies need to include biomarkers of stress and confirmation of medical or psychiatric conditions. Parents in our study may not represent the population of all parents of children with developmental disabilities, but they were more diverse in age, race, and income than those typically included in MBSR or positive psychology interventions.21,41 Given the number of study outcomes, significant findings with smaller effect sizes could be due to chance and thus need to be replicated in future work. A final limitation, inherent in “real-world” effectiveness studies, is dropout owing to life circumstances, and in our case to caregiving demands, and dwindling questionnaire compliance during follow-up. These factors also pose challenges to follow-up beyond 6 months. However, we ensured that the study was adequately powered, dropouts versus completers did not significantly differ, and that differential attrition biases did not occur.
Conclusions
With advances in pediatric care, more children with neurodevelopmental disabilities are living well into adulthood, and most continue to reside with their aging parents.53 Even so, glaring knowledge gaps exist on the compromised health and mental health of the lifelong parent caregivers of young or adult children with developmental disabilities. This study helps bring these mothers into the research limelight and justifies future efforts to promote their well-being and long-term caregiving abilities.
Supplementary Material
Acknowledgments
The authors are grateful to the outstanding peer-mentors who skillfully led the treatment groups: Roxanne Carreon, Karen Pilkerton, Janet Shouse, and Lisa Price. We thank Jimmy Pilkerton for his assistance with MBSR, and our superb clinical supervisors, Carol Rabideau, LCMSW, and Michelle Foote Pearce, DMin, RN. We also thank Lynette Henderson, PhD, for her excellent contributions to the PAD curriculum; Gordan Peerman, DMin, and Kathy Wood, MEd, for their thoughtful contributions to the MBSR curriculum; Elizabeth Roof, MS, for her skills in launching this study; Roy Elam, MD, for his enthusiastic support of this work; and Robert Hodapp, PhD, for comments on an earlier manuscript draft. Finally, a very special thanks goes to the families who graciously participated in this research.
Glossary
- ASD
autism spectrum disorders
- BAI
Beck Anxiety Inventory
- BDI
Beck Depression Inventory
- ES
effect size
- MBSR
Mindfulness-Based Stress Reduction
- PAD
Positive Adult Development
- PSI
Parenting Stress Index-Short Form
Footnotes
Dr Dykens developed the study rationale, aims, and design, led and supervised the implementation of the study, and drafted and revised the final manuscript; Dr Fisher managed data entry and quality, conducted preliminary descriptive statistics, completed Figure 1’s Consolidated Standards of Reporting Trials flow diagram, and critically reviewed the final manuscript; Dr Taylor assisted with data analyses and interpretation, drafted the results section, constructed and revised Tables 2 and 3, and critically reviewed the final manuscript; Dr Lambert conducted data analyses by using slopes as outcomes, drafted the power analysis and statistical approach sections, created and revised Figures 2 and 3, and reviewed the final manuscript; Dr Miodrag assisted with data interpretation, provided background literature on maternal stress and mindfulness practice, conducted preliminary analyses in mothers of children with autism, and reviewed the final manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01110343).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Institutes of Health’s (NIH) National Center for Complementary and Alternative Medicine grant 5RC1AT005612 to the first author, and used core research services provided by NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development grant P30HD015052 to the Vanderbilt Kennedy Center, and NIH’s National Center for Advancing Translational Sciences award UL1TR000445 to Vanderbilt University. Dr Taylor's participation was supported by K01MH92598, National Institute of Mental Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Dr Taylor has participated in grant review panels and given presentations for Autism Speaks. The other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Miodrag N, Hodapp RM. Chronic stress and health among parents of children with intellectual and developmental disabilities. Curr Opin Psychiatry. 2010;23(5):407–411 [DOI] [PubMed] [Google Scholar]
- 2.Parish SL, Rose RA, Weiss-Grinstein M, Richman EL, Andrews ME. Material hardship in US families raising children with disabilities. Exceptional Children. 2008;75:71–92 [Google Scholar]
- 3.Hassall R, Rose J, McDonald J. Parenting stress in mothers of children with an intellectual disability: The effects of parent cognition in relation to child characteristics and family support. J Intellect Disabil Res. 2005;496(pt 6):405–418 [DOI] [PubMed] [Google Scholar]
- 4.Anderson LL, Larson SA, Wuorio A. 2010 FINDS National Survey Technical Report Part 1: Family Caregiver Survey. Minneapolis, MN: University of Minnesota; 2011 [Google Scholar]
- 5.Dykens EM. Psychopathology in children with intellectual disability. J Child Psychol Psychiatry. 2000;41(4):407–417 [PubMed] [Google Scholar]
- 6.Neece CL, Green SA, Baker BL. Parenting stress and child behavior problems: a transactional relationship across time. Am J Intellect Dev Disabil. 2012;117(1):48–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dykens EM. Toward a positive psychology of mental retardation. Am J Orthopsychiatry. 2006;76(2):185–193 [DOI] [PubMed] [Google Scholar]
- 8.Singer GHS. Meta-analysis of comparative studies of depression in mothers of children with and without children with developmental disabilities. Am J Ment Retard. 2006;111(3):155–169 [DOI] [PubMed]
- 9.Taylor JL, Warren ZE. Maternal depressive symptoms following autism spectrum diagnosis. J Autism Dev Disord. 2012;42(7):1411–1418 [DOI] [PubMed] [Google Scholar]
- 10.Gallagher S, Phillips AC, Carroll D. Parental stress is associated with poor sleep quality in parents caring for children with developmental disabilities. J Pediatr Psychol. 2010;35(7):728–737 [DOI] [PubMed] [Google Scholar]
- 11.Seltzer MM, Greenberg JS, Hong J, et al. Maternal cortisol levels and behavior problems in adolescents and adults with ASD. J Autism Dev Disord. 2010;40(4):457–469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dykens EM, Lambert W. Trajectories of diurnal cortisol in mothers of children with autism and other developmental disabilities: relations to health and mental health. J Autism Dev Disord. 2013;43(10):2426–2434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gallagher S, Phillips AC, Drayson MT, Carroll D. Parental caregivers of children with developmental disabilities mount a poor antibody response to pneumococcal vaccination. Brain Behav Immun. 2009;23(3):338–346 [DOI] [PubMed] [Google Scholar]
- 14.Epel ES, Blackburn EH, Lin J, et al. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci U S A. 2004;101(49):17312–17315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halfon N, Houtrow A, Larson K, Newacheck PW. The changing landscape of disability in childhood. Future Child. 2012;22(1):13–42 [DOI] [PubMed] [Google Scholar]
- 16.Ganz ML. The lifetime distribution of the incremental societal costs of autism. Arch Pediatr Adolesc Med. 2007;161(4):343–349 [DOI] [PubMed] [Google Scholar]
- 17.Osborne LA, McHugh L, Saunders J, Reed P. Parenting stress reduces the effectiveness of early teaching interventions for autistic spectrum disorders. J Autism Dev Disord. 2008;38(6):1092–1103 [DOI] [PubMed] [Google Scholar]
- 18.Matson JL, Mahan S, LoVullo SV. Parent training: a review of methods for children with developmental disabilities. Res Dev Disabil. 2009;30(5):961–968 [DOI] [PubMed] [Google Scholar]
- 19.Robertson J, Hatton C, Wells E, et al. The impacts of short break provision on families with a disabled child: an international literature review. Health Soc Care Community. 2011;19(4):337–371 [DOI] [PubMed] [Google Scholar]
- 20.Singer GHS, Ethridge BL, Aldana SL. Primary and secondary effects of parenting stress and stress management interventions for parents of children with developmental disabilities: a meta-analysis. Ment Retard Dev Disabil Res Rev. 2007;13:357–369 [DOI] [PubMed] [Google Scholar]
- 21.Baer RA. Mindfulness training as a clinical intervention: A concept and empirical review. Clin Psychol Sci Prac. 2003;10:125–143 [Google Scholar]
- 22.Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300(11):1350–1352 [DOI] [PubMed] [Google Scholar]
- 23.Seligman MEP, Steen TA, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. Am Psychol. 2005;60(5):410–421 [DOI] [PubMed] [Google Scholar]
- 24.Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol. 2009;65(5):467–487 [DOI] [PubMed] [Google Scholar]
- 25.Brown KW, Ryan RM, Creswell JD. Mindfulness: theoretical foundation and evidence for its salutary effects. Psychol Inq. 2007;18(4):211–237 [Google Scholar]
- 26.Duncan LG, Coatsworth JD, Greenberg MT. A model of mindful parenting: implications for parent-child relationships and prevention research. Clin Child Fam Psychol Rev. 2009;12(3):255–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang Y-Y, Posner MI. Special issue on mindfulness neuroscience. Soc Cogn Affect Neurosci. 2013;8(1):1–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hayes SA, Watson SL. The impact of parenting stress: a meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J Autism Dev Disord. 2013;43(3):629–642 [DOI] [PubMed] [Google Scholar]
- 29.Abidin R. Parent Stress Index Professional Manual. 3rd ed. Odessa, TX: Psychological Assessment Resources; 1995 [Google Scholar]
- 30.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996 [Google Scholar]
- 31.Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. San Antonio, TX: Psychological Corporation; 1990 [Google Scholar]
- 32.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307 [DOI] [PubMed] [Google Scholar]
- 33.Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719–727 [DOI] [PubMed] [Google Scholar]
- 34.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess. 1985;49(1):71–75 [DOI] [PubMed] [Google Scholar]
- 35.Bellg AJ, Borrelli B, Resnick B, et al. Treatment Fidelity Workgroup of the NIH Behavior Change Consortium . Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–451 [DOI] [PubMed] [Google Scholar]
- 36.Diggle PJ, Heagerty P, Liang K-Y, Zeger SL. Analysis of Longitudinal Data. 2nd ed. Oxford, UK: Oxford University Press; 2002 [Google Scholar]
- 37.Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health. 2013;13:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol. 2010;78(2):169–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 40.Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159 [DOI] [PubMed] [Google Scholar]
- 41.Bell ML, Kenward MG, Fairclough DL, Horton NJ. Differential dropout and bias in randomised controlled trials: when it matters and when it may not. BMJ. 2013;346:e8668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Juster R-P, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35(1):2–16 [DOI] [PubMed] [Google Scholar]
- 43.Cohn MA, Fredrickson BL. In search of durable positive psychology interventions: predictors and consequences of long-term positive behavior change. J Posit Psychol. 2010;5(5):355–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Griffith GM, Hastings RP, Nash S, Hill C. Using matched groups to explore child behavior problems and maternal well-being in children with Down syndrome and autism. J Autism Dev Disord. 2010;40(5):610–619 [DOI] [PubMed] [Google Scholar]
- 45.Piven J. The broad autism phenotype: a complementary strategy for molecular genetic studies of autism. Am J Med Genet. 2001;105(1):34–35 [PubMed] [Google Scholar]
- 46.Kazdin AE, Rabbit SM. Novel models for delivering mental health services and reducing the burden of mental illness. Clin Psychol Sci. 2013;1:170–191 [Google Scholar]
- 47.Collins PY, Patel V, Joestl SS, et al. Scientific Advisory Board and the Executive Committee of the Grand Challenges on Global Mental Health . Grand challenges in global mental health. Nature. 2011;475(7354):27–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Olson AL, Dietrich AJ, Prazar G, Hurley J. Brief maternal depression screening at well-child visits. Pediatrics. 2006;118(1):207–216 [DOI] [PubMed] [Google Scholar]
- 49.Heneghan AM, Silver EJ, Bauman LJ, Stein REK. Do pediatricians recognize mothers with depressive symptoms? Pediatrics. 2000;106(6):1367–1373 [DOI] [PubMed] [Google Scholar]
- 50.Heneghan AM, Mercer M, DeLeone NL. Will mothers discuss parenting stress and depressive symptoms with their child’s pediatrician? Pediatrics. 2004;113(3 pt 1):460–467 [DOI] [PubMed] [Google Scholar]
- 51.Seltzer MM, Floyd F, Song J, Greenberg J, Hong J. Midlife and aging parents of adults with intellectual and developmental disabilities: impacts of lifelong parenting. Am J Intellect Dev Disabil. 2011;116(6):479–499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wickramaratne P, Gameroff M, Pilowsky DJ, et al. Children of depressed mothers 1 year after remission of maternal depression: Findings from the STA R*D-Child Study. Am J Psychiatry. 2011;168:593–602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Braddock D, Hemp R, Rozzolo MC, Haffer L, Tanis ES, Wu J. The State of the States in Developmental Disabilities. Boulder, CO: Coleman Institute for Cognitive Disabilities; 2011 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.