Abstract
The central aim of this study is to estimate prevalence, ages of onset, severity, and associated disability of anxiety disorders among African Americans, Caribbean Blacks, and non-Hispanic whites in the U.S. Results indicated that whites were at elevated risk for generalized anxiety disorder, panic disorder, and social anxiety compared to Caribbean Blacks and African Americans. Black respondents were more likely to meet criteria for PTSD. When African American and Caribbean Black respondents met criteria for an anxiety disorder, they experienced higher levels of overall mental illness severity and functional impairment compared to whites. White respondents were at greater risk to develop generalized anxiety, social anxiety, and panic disorders late in life. Risk of developing PTSD endured throughout the life course for blacks whereas whites rarely developed PTSD after young adulthood. These results can be used to inform targeted interventions to prevent or remediate anxiety disorders among these diverse groups.
Keywords: Race, Anxiety, Prevalence, Epidemiology, Ethnicity
1. Introduction
Panic disorder (PD), agoraphobia (AGO), social phobia (SAD), post-traumatic stress disorder (PTSD) and generalized anxiety disorder (GAD) are among the most prevalent psychiatric disorders in the United States (Kessler, Chiu, Demler, Merikangas, & Walters, 2005). The National Comorbidity Survey-Replication (NCS-R) finds that 28.8% of the general population meets criteria for at least one of these disorders. There is a limited amount of research available regarding the nature and prevalence of PD, AGO, SAD, PTSD, and GAD among various racial and ethnic subpopulations. Understanding race-ethnic differences among these disorders is especially important given recent national health care policy emphasis on racial disparities (U.S. Department of Health and Human Services, 2001). Knowledge of race-ethnic differences in terms of disorder prevalence, age at onset, gender, impairment, and other factors can inform targeted interventions to reduce health disparities among at risk groups (Breslau et al., 2005). As an example, early onset of certain anxiety disorders among a given race-ethnic group may provide support for the development of early detection/intervention efforts in settings where these youth are accessible (e.g., schools).
Previous studies have examined anxiety disorder rates among a range of ethnic groups in the U.S., including African Americans. Recently, Breslau and colleagues (Breslau et al., 2005), using the NCS-R sample, found that non-Hispanic whites had significantly greater rates of GAD compared to non-Hispanic blacks or Hispanics. Whites also had higher rates of PD compared to non-Hispanic blacks and elevated rates of SAD compared to Hispanic respondents. Lower rates of certain anxiety disorders (e.g., GAD) among blacks and Hispanics is somewhat surprising given elevated rates of unemployment, lower socioeconomic status, and other significant stressors (e.g., exposure to crime, racism) observed in these groups (Clark, Anderson, Clark, & Williams, 1999; Turner & Lloyd, 2004). These stressors could be expected to contribute to increased worry and tension which are key symptoms in certain anxiety disorders (e.g., GAD). The purpose of the present paper is to present a detailed examination of anxiety disorders among African Americans, blacks of Caribbean descent, and whites by investigating prevalence, severity, functional impairment, and socio-demographic correlates of anxiety disorders in these groups. Nearly all research addressing anxiety disorders among blacks to date has treated the black population as a homogeneous group (Jackson, Neighbors, Nesse, Trierweiler, & Torres, 2004; Jackson, Torres, et al., 2004; Williams & Harris-Reid, 1999). Blacks of Caribbean descent are the largest black ethnic subgroup in the United States (Jackson, Neighbors, et al., 2004; Jackson, Torres, et al., 2004; Williams, Lavizzo-Mourey, & Warren, 1994). The proportion of blacks of Caribbean descent in some large cities on the east coast (e.g. New York, Boston, Miami) is approximately one-quarter of the overall black population. Overall, Black Caribbeans currently outnumber Koreans and Cubans and are growing at a faster rate than both of these two groups (Logan & Deane, 2003). Notable differences exist between blacks of Caribbean descent and African Americans including distinctive languages, forms of social life, and even transnational migration experiences (Logan & Deane, 2003). Despite these important differences among blacks in the U.S., the co-categorization of blacks of Caribbean descent and African Americans into a single, heterogeneous racial group (“African Americans”), limits research examining differences in health status and social circumstances between these groups. Available literature suggests that important differences may exist between blacks of Caribbean descent and African Americans in rates of certain mental disorders and levels of emotional distress. Caribbean immigrants experience higher than expected rates of schizophrenia (Hemingway et al., 2001; Selten, Slaets, & Kahn, 1997) and mania (van Os et al., 1996). Additionally, foreign-born Caribbean Blacks report higher levels of overall psychological distress compared to African Americans born in the U.S. (Williams, 2000). Higher levels of overall psychological distress among Caribbean Blacks could lead one to predict higher rates of anxiety disorders among this group. However, similar rates of depression have been found among Caribbean Blacks compared to African Americans (Williams et al., 2007) suggesting that increased distress may not necessarily translate into higher rates of psychiatric illness.
In order to investigate race differences in the nature and prevalence of anxiety disorders this paper uses both the National Survey of American Life (NSAL) (Jackson, Neighbors, et al., 2004; Jackson, Torres, et al., 2004) and the National Comorbidity Survey-Replication (NCS-R) (Kessler et al., 2005) to obtain nationally representative estimates for African Americans, Caribbean Blacks, and non-Hispanic whites in the U.S. The NSAL (Jackson, Neighbors, et al., 2004; Jackson, Torres, et al., 2004) is the first nationally representative study of psychiatric disorders where comparisons between blacks of Caribbean descent and African Americans, can be made. The present paper also provides a detailed analysis of the onset of anxiety disorders which allows for a comprehensive understanding of when anxiety disorder risk is greatest among these groups. This onset-related information can help in the development of preventative and rehabilitative interventions that target high risk periods for these groups.
2. Method
2.1. Sample
The NSAL and the NCS-R were both based on multi-stage area probability samples and used sampling frames, sample selection, and professional interviewers from the Institute for Social Research at the University of Michigan (Heeringa et al., 2004).
The present study examines subgroups from the NCS-R and the NSAL together. Both the NSAL and the NCS-R are nationally representative household surveys of English-speaking, non-institutionalized adults aged 18 and over. Data were collected from 2001 to 2003. The NCS-R was administered in two parts: Part I included 9282 respondents and assessed core psychiatric diagnoses, and Part II included 5692 of the Part I respondents and assessed additional disorders, demographics, and risk factors (Kessler & Merikangas, 2004). The NCS-R response rate was 70.9%. The NCS-R sample included race/ethnicity proportions similar to the U.S. population. The NSAL sample included 3570 African Americans, 1621 blacks of Caribbean descent (Caribbean Blacks), and 891 non-Hispanic whites (Heeringa et al., 2004; Jackson, Neighbors, et al., 2004; Jackson, Torres, et al., 2004; Joe, Baser, Breeden, Neighbors, & Jackson, 2006). The overall response rate of the NSAL was 72.3% and response rates for the two black subgroups were 70.7% for African Americans and 77.7% for Caribbean Blacks. In the NSAL, the term “African American” refers to adults who self-identified as black but did not identify ancestral ties to the Caribbean. “Caribbean Black” refers to adults who self-identified as black and reported that they or at least one of their parents or grandparents descended from a Caribbean country.
Data from both the NSAL and NCS-R were weighted to adjust for disproportionate sampling probabilities, for non-response, and for sociodemographic differences between the samples and the 2000 U.S. Census population (Heeringa, Torres, Sweetman, & Baser, 2006; Heeringa et al., 2004; Kessler et al., 2004). An additional weight for the Part II NCS-R respondents adjusts for the oversampling of Part I respondents. The present paper examines the African American and Caribbean Black subsamples from the NSAL and the subsample of 6696 non-Hispanic white respondents from the NCS-R. The NSAL white respondents are not included in the present study because their interviews omitted important diagnostic sections investigated in this paper.
3. Measures
3.1. Psychiatric diagnosis assessment
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994) (DSM-IV) World Mental Health Composite International Diagnostic Interview (WMH-CIDI), was used to assess both 12-month and lifetime DSM-IV disorders (Kessler & Ustun, 2004).
The present study investigates five anxiety disorders: GAD, SAD, PTSD, PD, and AGO. Obsessive-compulsive disorder was not included in this study because the NSAL and NCS-R utilized different diagnostic methods for this disorder. Other diagnoses considered here include major depressive disorder, dysthymia, bipolar I and II, alcohol or drug abuse/dependence, anorexia, bulimia, and binge-eating disorder. The age of disorder onset was determined using a series of questions designed to enhance respondent recall (KnÄuper, Cannell, Schwarz, Bruce, & Kessler, 1999; Simon & VonKorff, 1995). If respondents could not remember their exact age when they first experienced the syndrome, follow-up questions attempted to elicit a plausible estimate of their age of onset (e.g., “Was it before you started school?” and “Was it before you were a teenager?”).
3.2. Severity of mental disorder and 30-day functioning
Cases with at least one 12-month disorder were divided into three severity categories. Those classified as serious met one or more of the following criteria: screened into the non-affective psychosis section and had been treated for psychosis; met criteria for bipolar I or II; had a serious suicide attempt in the past 12 months; had a score below 50 on the Global Assessment of Functioning scale (GAF) (American Psychiatric Association, 2000); had substance dependence with severe role impairment as defined by substance specific impairment questions; or scored between 7 and 10 on the Sheehan Disability Scale (Leon, Olfson, Portera, Farber, & Sheehan, 1997). Individuals classified as moderate had: suicidal ideation, gestures, or plan; a GAF score between 51 and 60; substance dependence without severe role impairment; or moderate role impairment in the presence of a mental disorder. All remaining cases were defined as mild.
The World Health Organization's Disability Assessment Schedule II (WHO-DAS-II) (Rehm et al., 1999) was used to assess 30-day functional impairment in 7 domains: days out of role, productivity (quality and quantity of daily activities at home and work), self-care (washing, dressing, etc.), mobility (standing, moving, etc.), cognition (concentration, memory, etc.), social (conversing, maintaining friendships, etc.), and family burden (respondent related health interference with the life and activities of friends and family). For days out of role, the outcome is number of days in the previous thirty that respondents were unable to carry out their normal activities. For the other domains, the impairment measure is the number of days (in the past thirty) that the respondents’ symptoms caused difficulty in functioning weighted by the level of difficulty.
3.3. Predictor variables
We investigated several sociodemographic variables to identify factors associated with the presence of 12-month anxiety disorders and to identify groups at elevated risk of anxiety disorders. Predictor variables included race/ethnicity, sex, age cohort, years of education, marital status, and income.
4. Statistical analysis
All analyses were weighted with a combined version of the NCS-R and NSAL. PTSD was assessed in Part II of the NCS-R interview, and the NCS-R Part II weight was applied to the analyses of PTSD. Standard errors, confidence intervals, and significance tests were properly adjusted for the complex sample designs of the NSAL and NCS-R.
Cross-tabulations were conducted using the PROC SURVEY-FREQ procedure of the SAS Version 9.1.3 software package (SAS Institute, 2005). The χ2 and corresponding p-values from these cross-tabulations are based on the Rao-Scott Chi-square test, a complex design-adjusted version of the Pearson Chi-square test (SAS Institute, 2005). Similarly, PROC SURVEYMEANS and PROC SURVEYREG were used to calculate mean scores and pairwise t-tests between race/ethnic groups, while multivariate logistic regressions were conducted using PROC SURVEYLOGISTIC. All SAS procedures used the Taylor-series linearization technique for calculating the complex-design based estimates of variance and standard error.
With respect to lifetime disorders and conditions, the NSAL and NCS-R data are heavily censored due to the wide range of respondent ages at interview. Due to this differential, lifetime prevalence estimates based on respondent status at age at interview are biased and tend to underestimate the lifetime disorder risk. Survival analysis methods were used to address this censoring problem.
Instead of lifetime prevalence, we focus on cumulative lifetime probability, or projected risk, of developing disorders by specific ages. Cumulative lifetime probability curves and hazard curves for each disorder were estimated across the three race/ethnicities from the corresponding Kaplan–Meier survival curves (Kaplan & Meier, 1958). The cumulative curves were used to compare the cumulative projected risk of developing a given disorder by a given age across each race/ethnic group. The hazard curves represent the non-cumulative, immediate risk of developing a given disorder at different ages over the lifespan; as such, they were used to characterize typical disorder onset ages and to investigate differences in age of onset patterns across the three race/ethnic groups. Log-rank χ2 statistics were used to test for statistically significant differences in onset ages across the groups. In addition, separate cumulative lifetime probability curves were estimated using only respondents who developed the focal anxiety disorder to derive the median and the 25th and 75th percentile onset ages.
Multivariate Cox proportional hazards regression was used to assess sociodemographic risk factors of developing the disorders (Cox, 1972; Hosmer & Lemeshow, 2000). The education and marital status variables were coded as time-varying predictors in order to determine their values at the time of disorder onset, rather than at the time of interview, allowing more accurate assessment of their associations with disorder onset. Education was coded as time-varying by assuming a uniform, chronological education history for each respondent in which 12 years of education corresponds to being a student to age 18, 16 years of education corresponds to being a student to age 22, and other years of education correspond to ages consistent with this scheme. Using this method, the time-varying education status of each year of each respondent's life was categorized as either “student” or as having 0–11, 12, 13–15, or 16 or more terminal years of education. Marital status was coded as time-varying by categorizing the marital status of each year of each respondent's life as either never, currently, or previously married.
All survival-based analyses were conducted in R, an open-source statistical programming language and environment (R Development Core Team, 2006), using the “survey” package (Lumley, 2004) to adjust standard errors and significance tests for the effects of the weighting, stratification, and clustering of the surveys’ sample designs. The categorical factors in the Cox proportional hazards models were tested for overall statistical significance with Wald χ2 tests using the complex design-adjusted variance–covariance matrix of the coefficients.
5. Results
5.1. 12-Month prevalence of anxiety disorders
The overall 12-month prevalence (SE) was 2.30% (0.16) for GAD, 6.34% (0.27) for SAD, 3.50% (0.20) for PTSD, 2.51% (0.15) for PD, and 0.91% (0.09) for AGO. Statistically significant overall differences in the 12-month prevalences across the three race/ ethnicity groups were found for both GAD and SAD. African Americans and Caribbean Blacks had similar 12-month rates of both GAD and SAD whereas rates for whites were considerably higher (Table 1).
Table 1.
12-month prevalence of anxiety disorders by sociodemographic characteristics, stratified by race/ethnicity.
| GAD |
Social anxiety disorder |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total; n = 11710; % (SE) | AA; n = 3430; % (SE) | CB; n = 1584; % (SE) | W; n = 6696; % (SE) | Total; n = 11712 | AA; n = 3431; % (SE) | CB; n = 1585; % (SE) | W; n = 6696; % (SE) | |||
| Overall | 2.30 (0.16) | 1.37 (0.23) | 1.40 (0.61) | 2.71 (0.20) | 6.34 (0.27) | 4.55 (0.43) | 4.68 (1.21) | 7.11 (0.36) | ||
| Gender | ||||||||||
| Male | 1.70 (0.24) | 0.79 (0.33) | 1.54 (1.17) | 2.04 (0.30) | 5.62 (0.42) | 3.42 (0.54) | 5.07 (1.98) | 6.44 (0.54) | ||
| Female | 2.84 (0.22) | 1.83 (0.25) | 1.26 (0.57) | 3.33 (0.31) | 6.99 (0.40) | 5.44 (0.60) | 4.28 (0.84) | 7.75 (0.55) | ||
| Age cohort | ||||||||||
| 18-29 | 1.81 (0.27) | 0.77 (0.33) | 1.67 (0.94) | 2.32 (0.36) | 7.70 (0.68) | 5.06 (0.93) | 4.27 (1.15) | 9.14 (1.04) | ||
| 30-44 | 2.91 (0.29) | 1.74 (0.51) | 0.58 (0.23) | 3.59 (0.35) | 7.58 (0.56) | 4.25 (0.65) | 7.97 (3.03) | 9.24 (0.80) | ||
| 45-59 | 2.97 (0.33) | 2.13 (0.51) | 3.45 (2.91) | 3.25 (0.41) | 6.65 (0.58) | 5.73 (0.90) | 2.43 (0.92) | 7.06 (0.73) | ||
| >60 | 1.15 (0.25) | 0.34 (0.24) | NA | 1.38 (0.31) | 2.85 (0.33) | 2.66 (0.82) | 0.53 (0.34) | 2.94 (0.36) | ||
| Marital status | ||||||||||
| Married/partner | 1.96 (0.23) | 0.88 (0.35) | 2.07 (1.22) | 2.26 (0.27) | 5.24 (0.31) | 3.18 (0.68) | 4.24 (1.75) | 5.86 (0.36) | ||
| Previously married | 3.47 (0.38) | 2.21 (0.47) | 0.46 (0.31) | 4.23 (0.57) | 7.35 (0.58) | 4.93 (0.63) | 1.44 (0.49) | 8.80 (0.88) | ||
| Never married | 2.02 (0.25) | 1.31 (0.37) | 0.91 (0.40) | 2.50 (0.34) | 7.91 (0.61) | 6.03 (0.89) | 7.33 (2.39) | 9.10 (0.91) | ||
| Education | ||||||||||
| 0-11 years | 1.87 (0.38) | 0.90 (0.30) | 2.85 (2.72) | 2.54 (0.63) | 8.26 (0.53) | 6.52 (0.71) | 7.13 (3.38) | 9.60 (0.79) | ||
| 12 years | 2.13 (0.28) | 1.06 (0.32) | 0.91 (0.44) | 2.68 (0.39) | 6.06 (0.44) | 4.00 (0.65) | 3.42 (1.01) | 7.12 (0.62) | ||
| 13-15 years | 2.49 (0.25) | 1.67 (0.44) | 1.14 (0.96) | 2.80 (0.30) | 6.22 (0.65) | 3.23 (0.79) | 5.98 (3.37) | 7.24 (0.86) | ||
| >16 years | 2.40 (0.35) | 1.52 (0.60) | 0.72 (0.35) | 2.63 (0.41) | 5.43 (0.58) | 4.09 (0.99) | 2.50 (1.25) | 5.79 (0.67) | ||
| Region | ||||||||||
| Northeast | 2.44 (0.24) | 1.87 (0.65) | 1.97 (0.93) | 2.65 (0.23) | 5.78 (0.54) | 4.93 (1.38) | 3.72 (0.63) | 6.22 (0.68) | ||
| Midwest | 2.43 (0.30) | 2.28 (0.80) | NA | 2.48 (0.32) | 6.87 ( 0.57) | 5.91 (1.23) | 22.22 (15.44) | 7.06 (0.65) | ||
| South | 2.34 (0.30) | 1.12 (0.26) | 1.04 (0.89) | 3.19 (0.43) | 5.80 (0.45) | 3.97 (0.55) | 5.25 (3.21) | 7.06 (0.67) | ||
| West | 1.87 (0.23) | 0.33 (0.34) | NA | 2.22 (0.31) | 7.61 (0.74) | 4.87 (1.49) | 1.99 (2.25) | 8.26 (0.89) | ||
| Poverty | ||||||||||
| Poverty line or below | 2.15 (0.37) | 1.59 (0.48) | 1.73 (1.51) | 3.17 (0.59) | 8.16 (0.77) | 5.22 (0.66) | 3.30 (1.59) | 13.72 (1.93) | ||
| >1 to 3 times poverty line | 2.38 (0.31) | 1.65 (0.41) | 2.19 (1.45) | 3.15 (0.47) | 6.29 (0.48) | 5.30 (0.78) | 7.34 (3.02) | 7.23 (0.60) | ||
| >3 to 6 times poverty line | 2.13 (0.27) | 0.99 (0.39) | 0.80 (0.24) | 2.71 (0.34) | 5.74 (0.45) | 3.14 (0.75) | 2.77 (1.00) | 7.06 (0.60) | ||
| >6 times poverty line | 1.86 (0.29) | 0.28 (0.28) | NA | 2.20 (0.34) | 4.89 (0.53) | 2.63 (1.33) | 2.40 (1.04) | 5.36 (0.58) | ||
| PTSD |
Panic disorder |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total; n = 11710; % (SE) | AA; n = 3430; % (SE) | CB; n = 1584; % (SE) | W; n = 6696; % (SE) | Total; n = 11712 | AA; n = 3431; % (SE) | CB; n = 1585; % (SE) | W; n = 6696; % (SE) | |||
| Overall | 3.66 (0.23) | 3.80 (0.36) | 5.16 (1.69) | 3.49 (0.30) | 2.51 (0.15) | 2.31 (0.29) | 2.70 (1.66) | 2.59 (0.18) | ||
| Gender | ||||||||||
| Male | 2.21 (0.25) | 2.37 (0.51) | 7.01 (2.72) | 1.86 (0.22) | 1.60 (0.19) | 1.40 (0.37) | 4.04 (3.18) | 1.59 (0.19) | ||
| Female | 4.90 (0.33) | 4.91 (0.48) | 3.26 (0.94) | 4.97 (0.47) | 3.33 (0.24) | 3.04 (0.41) | 1.33 (0.37) | 3.51 (0.30) | ||
| Age cohort | ||||||||||
| 18-29 | 4.78 (0.55) | 5.56 (1.01) | 10.30 (5.83) | 3.70 (0.47) | 2.32 (0.35) | 2.07 (0.54) | 4.38 (2.50) | 2.34 (0.45) | ||
| 30-44 | 3.55 (0.44) | 3.15 (0.71) | 4.11 (2.49) | 3.85 (0.55) | 3.31 (0.37) | 2.31 (0.51) | 2.88 (2.47) | 3.84 (0.48) | ||
| 45-59 | 4.71 (0.51) | 4.04 (0.97) | 2.47 (1.31) | 5.16 (0.60) | 3.06 (0.38) | 3.56 (0.77) | 1.64 (0.70) | 2.92 (0.45) | ||
| >60+ | 1.31 (0.30) | 2.11 (0.81) | 0.16 (0.16) | 1.0 (0.25) | 0.91 (0.17) | 0.87 (0.37) | NA | 0.94 (0.20) | ||
| Marital status | ||||||||||
| Married/partner | 2.96 (0.26) | 3.35 (0.57) | 4.47 (2.63) | 2.73 (0.27) | 1.87 (0.16) | 1.78 (0.32) | 0.62 (0.28) | 1.92 (0.19) | ||
| Previously married | 5.24 (0.52) | 4.46 (0.67) | 1.69 (0.98) 6 | .06 (0.81) | 4.00 (0.45) | 3.28 (0.65) | 0.58 (0.32) | 4.49 (0.60) | ||
| Never married | 3.60 (0.39) | 3.83 (0.60) | 8.36 (3.62) | 2.96 (0.46) | 2.61 (0.38) | 2.23 (0.47) | 7.30 (5.14) | 2.63 (0.50) | ||
| Education | ||||||||||
| 0-11 years | 4.63 (0.55) | 4.73 (0.81) | 5.28 (3.51) | 4.45 (0.74) | 3.37 (0.46) | 3.33 (0.56) | 8.80 (7.19) | 3.13 (0.61) | ||
| 12 years | 3.56 (0.37) | 4.03 (0.62) | 5.29 (2.08) | 3.11 (0.47) | 2.14 (0.22) | 2.07 (0.43) | 1.51 (0.71) | 2.18 (0.26) | ||
| 13-15 years | 3.66 (0.41) | 3.87 (0.77) | 3.64 (1.55) | 3.55 (0.50) | 2.65 (0.30) | 1.27 (0.42) | 1.14 (0.43) | 3.16 (0.38) | ||
| >16 years | 2.98 (0.52) | 1.45 (0.44) | 6.74 (5.46) | 3.36 (0.65) | 2.30 (0.28) | 3.11 (0.97) | 0.42 (0.22) | 2.17 (0.27) | ||
| Region | ||||||||||
| Northeast | 4.08 (0.49) | 5.41 (0.96) | 2.33 (0.69) | 3.63 (0.70) | 3.03 (0.38) | 2.50 (0.89) | 1.38 (0.39) | 3.34 (0.45) | ||
| Midwest | 3.75 (0.56) | 5.11 (1.23) | 27.01 (11.62) | 3.00 (0.55) | 2.24 (0.32) | 2.61 (1.00) | 22.22 (15.44) | 2.05 (0.29) | ||
| South | 3.37 (0.29) | 3.21 (0.40) | 5.13 (2.53) | 3.49 (0.41) | 2.67 (0.23) | 2.29 (0.31) | 0.70 (0.54) | 2.98 (0.33) | ||
| West | 3.76 (0.71) | 2.18 (0.43) | 11.57 (10.58) | 4.05 (0.86) | 1.86 (0.28) | 1.62 (0.51) | 7.56 (5.12) | 1.80 (0.30) | ||
| Poverty | ||||||||||
| Poverty line or below | 6.29 (0.68) | 6.33 (0.89) | 3.84 (1.91) | 6.44 (1.13) | 4.38 (0.52) | 4.03 (0.50) | 6.36 (5.19) | 4.79 (1.08) | ||
| >1 to 3 times poverty line | 3.80 (0.39) | 3.32 (0.51) | 5.96 (2.12) | 4.13 (0.61) | 2.81 (0.29) | 2.08 (0.37) | 3.45 (1.99) | 3.51 (0.42) | ||
| >3 to 6 times poverty line | 2.88 (0.31) | 2.77 (0.50) | 2.54 (1.32) | 2.93 (0.40) | 1.69 (0.22) | 0.74 (0.34) | 0.36 (0.23) | 2.18 (0.29) | ||
| >6 times poverty line | 2.61 (0.46) | 1.85 (1.01) | 9.02 (7.88) | 2.56 (0.47) | 1.88 (0.35) | 3.56 (1.64) | 0.86 (0.70) | 1.61 (0.29) | ||
| Agoraphobia w/o panic |
|||||
|---|---|---|---|---|---|
| Total; n =11711; % (SE) | AA; n = 3431; % (SE) | CB; n = 1584; % (SE) | W; n = 6696; % (SE) | ||
| Overall | 0.91 (0.09) | 1.09 (0.18) | 0.60 (0.26) | 0.85 (0.11) | |
| Gender | |||||
| Male | 0.75 (0.15) | 0.64 (0.27) | 0.18 (0.18) | 0.81 (0.18) | |
| Female | 1.05 (0.14) | 1.45 (0.24) | 1.03 (0.47) | 0.88 (0.16) | |
| Age cohort | |||||
| 18-29 | 1.04 (0.21) | 1.06 (0.28) | 0.90 (0.40) | 1.04 (0.29) | |
| 30-44 | 0.86 (0.18) | 0.84 (0.33) | 0.72 (0.58) | 0.87 (0.23) | |
| 45-59 | 1.36 (0.23) | 2.09 (0.46) | 0.15 (0.15) | 1.13 (0.28) | |
| >60 | 0.30 (0.12) | 0.23 (0.17) | 0.29 (0.29) | 0.32 (0.15) | |
| Marital status | |||||
| Married/partner | 0.67 (0.13) | 0.98 (0.29) | 0.73 (0.46) | 0.57 (0.15) | |
| Previously married | 1.18 (0.21) | 1.37 (0.31) | 0.31 (0.25) | 1.10 (0.28) | |
| Never married | 1.22 (0.28) | 1.01 (0.30) | 0.56 (0.24) | 1.38 (0.42) | |
| Education | |||||
| 0-11 years | 2.05 (0.35) | 2.29 (0.56) | 0.14 (0.14) | 1.96 (0.46) | |
| 12 years | 0.92 (0.21) | 1.21 (0.34) | 1.10 (0.76) | 0.78 (0.28) | |
| 13-15 years | 0.59 (0.14) | 0.26 (0.25) | 0.37 (0.25) | 0.71 (0.17) | |
| >16 years | 0.46 (0.14) | 0.10 (0.10) | 0.42 (0.36) | 0.54 (0.18) | |
| Region | |||||
| Northeast | 0.97 (0.17) | 1.23 (0.31) | 1.02 (0.44) | 0.88 (0.23) | |
| Midwest | 0.88 (0.19) | 1.31 (0.38) | NA | 0.77 (0.22) | |
| South | 1.02 (0.14) | 1.08 (0.26) | 0.11 (0.03) | 1.01 (0.17) | |
| West | 0.60 (0.26) | 0.55 (0.59) | NA | 0.63 (0.29) | |
| Poverty | |||||
| Poverty line or below | 2.06 (0.34) | 2.29 (0.47) | 2.21 (1.37) | 1.66 (0.46) | |
| >1 to 3 times poverty line | 1.19 (0.21) | 0.92 (0.24) | 0.40 (0.25) | 1.53 (0.36) | |
| >3 to 6 times poverty line | 0.46 (0.13) | 0.47 (0.28) | 0.21 (0.17) | 0.46 (0.14) | |
| >6 times poverty line | 0.36 (0.14) | 0.37 (0.39) | 0.10 (0.11) | 0.36 (0.16) | |
Abbreviations: GAD, generalized anxiety disorder; PTSD, post-traumatic stress disorder; AA, African American; CB, Caribbean Black; W, White; SE, standard error; NA, not available. Cells containing NA did not have sufficient numbers of respondents to calculate the required quantities. All estimates are weighted to be nationally representative of the given population and subpopulations in the coterminous 48 states of the U.S. Standard errors and Chi-square statistics are adjusted for the sampling stratification, clustering, and weighting of the data. Within a given row, Chi-squared values index the associations between race/ethnicity and the focal anxiety disorder among respondents meeting the given row's sociodemographic characteristic.
5.2. Sociodemographic correlates of 12-month anxiety disorders
Controlling for all sociodemographic factors in logistic regression models (Table 2), whites had elevated odds of all 12-month anxiety disorders except PTSD. Overall, females had increased odds of 12-month GAD, SAD, PTSD, and PD. Conversely, PTSD was significantly more prevalent among Caribbean Black males compared to Caribbean Black females. Respondents below age 60 were more likely to meet criteria for all 12-month anxiety disorders compared to those aged 60 or older. Respondents who were separated, divorced, or widowed at the time of their interviews, compared to those who were married or cohabitating, had increased odds of all of the 12-month anxiety disorders except for AGO. Additionally, respondents who had never been married were more likely to meet criteria for 12-month SAD than were their married counterparts. Having eleven or fewer years of education was associated with elevated odds of both SAD and AGO. Being at or below the poverty line was associated with increased odds of all 12-month anxiety disorders except for GAD. Finally, respondents living between 1 and 3 times the poverty line had elevated odds of SAD and AGO.
Table 2.
Sociodemographic correlates of 12-month DSM-IV/WMH-CIDI anxiety disorders.
| OR (95% CI) |
|||||
|---|---|---|---|---|---|
| GAD | Social phobia | PTSD | Panic disorder | Agoraphobia w/o PD | |
| Race/ethnicity | |||||
| African American | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Caribbean Black | 1.2 (0.5-3.2) | 1.2 (0.6-2.1) | 1.6 (0.8-3.4) | 1.4 (0.4-5.1) | 0.7 (0.2-1.8) |
| NCS-R White | 2.9 (2.1-4.1)* | 2.4 (1.8-3.2)* | 1.2 (0.96-1.6) | 1.8 (1.2-2.5)* | 1.5 (1.01-2.3)* |
| Sex | |||||
| Male | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Female | 1.7 (1.2-2.3)* | 1.3 (1.02-1.6)* | 2.1 (1.6-2.6)* | 1.8 (1.4-2.4)* | 1.3 (0.8-2.2) |
| Cohort | |||||
| 18-29 | 2.2 (1.2-3.8)* | 3.3 (2.3-4.9)* | 6.8 (3.8-12.2)* | 4.1 (2.4-6.8)* | 5.5 (1.9-16.6)* |
| 30-44 | 3.7 (2.3-6.1)* | 3.9 (2.8-5.6)* | 4.3 (2.3-7.9)* | 6.1 (3.7-10.0)* | 5.8 (2.3-15.7)* |
| 45-59 | 3.4 (2.1-5.6)* | 3.3 (2.3-4.7)* | 5.1 (2.9-8.8)* | 5.4 (3.3-8.6)* | 9.5 (4.2-21.5)* |
| >60 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Marital status | |||||
| Married | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Never married | 1.3 (0.8-1.9) | 1.4 (1.1-1.8)* | 0.7 (0.5-1.0) | 1.2 (0.8-1.7) | 1.2 (0.5-3.1) |
| Previously married | 2.0 (1.5-2.7)* | 1.6 (1.3-2.0)* | 1.8 (1.4-2.4)* | 2.0 (1.4-2.9)* | 1.3 (0.7-2.5) |
| Education | |||||
| 0-11 years | 0.9 (0.5-1.5) | 1.8 (1.3-2.4)* | 1.4 (0.9-2.2) | 1.4 (0.9-2.1) | 3.6 (1.7-8.0)* |
| 12 years | 0.9 (0.6-1.3) | 1.1 (0.8-1.4) | 1.1 (0.8-1.6) | 0.8 (0.6-1.1) | 1.7 (0.8-3.7) |
| 13-15 years | 1.0 (0.7-1.6) | 1.1 (0.8-1.4) | 1.0 (0.7-1.5) | 0.9 (0.7-1.3) | 1.0 (0.5-2.1) |
| >16 years | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Poverty | |||||
| Poverty line or below | 1.6 (0.9-2.7) | 1.7 (1.1-2.6)* | 1.9 (1.2-3.0)* | 2.3 (1.3-3.8)* | 3.9 (1.5-10.4)* |
| >1 to 3 times poverty line | 1.6 (0.98-2.5) | 1.4 (1.02-1.9)* | 1.3 (0.8-2.0) | 1.6 (0.99-2.6) | 3.0 (1.04-8.4)* |
| >3 to 6 times poverty line | 1.2 (0.8-1.7) | 1.2 (0.9-1.6) | 1.0 (0.7-1.4) | 0.9 (0.6-1.5) | 1.2 (0.5-3.1) |
| >6 times poverty line | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
Abbreviations: OR, odds ratio; CI, confidence interval; GAD, generalized anxiety disorder; PTSD, post-traumatic stress disorder; PD, panic disorder. Each column represents the results of a single, multivariate logistic regression model with the 12-month anxiety disorder as the outcome and all of the sociodemographic factors as covariates. Results observed for a given variable are net of the effects of the other variables in the models. All model estimates are weighted to be nationally representative of the given population and subpopulations in the coterminous 48 states of the U.S. Confidence intervals are adjusted for the sampling stratification, clustering, and weighting of the data. Chi-square values were obtained from design-based variance-covariance matrices to adjust for the stratification, clustering, and weighting of the data.
Indicates an odds ratio significantly different from 1.0, p < 0.05.
5.3. Severity of mental illness and 30-day functional impairment
There were significant associations between race/ethnicity and severity of mental illness for all of the anxiety disorders except AGO (Table 3). For each disorder, Caribbean Blacks had the highest proportion of cases in the severe category compared to the other two groups.
Table 3.
Severity of mental illness by race/ethnicity among respondents with 12-month anxiety disorders.
| Severity of mental illness, % (SE) |
||||
|---|---|---|---|---|
| Mild | Moderate | Severe | ||
| GAD | ||||
| African American | 24.5 (1.6) | 59.4 (5.0) | 16.1 (5.4) | |
| Caribbean Black | 30.4 (25.9) | 17.1 (7.0) | 52.5 (29.3) | |
| non-Hispanic White | 55.9 (3.6) | 32.9 (3.5) | 11.2 (2.1) | |
| Social phobia | ||||
| African American | 23.8 (3.7) | 51.5 (4.4) | 24.7 (4.3) | |
| Caribbean Black | 43.5 (20.2) | 23.0 (8.9) | 33.5 (18.0) | |
| non-Hispanic White | 37.4 (2.6) | 44.8 (3.0) | 17.8 (2.0) | |
| PTSD | ||||
| African American | 29.8 (3.5) | 45.4 (4.6) | 24.8 (4.5) | |
| Caribbean Black | 8.4 (5.5) | 21.7 (5.7) | 69.9 (8.4) | |
| non-Hispanic White | 37.6 (4.7) | 41.3 (4.1) | 21.1 (3.0) | |
| Panic disorder | ||||
| African American | 22.4 (4.7) | 51.8 (3.5) | 25.7 (5.0) | |
| Caribbean Black | 44.42 (6.6) | 12.1 (7.7) | 43.5 (2.5) | |
| non-Hispanic White | 33.8 (2.6) | 44.0 (3.2) | 22.2 (2.8) | |
| Agoraphobia w/o PD | ||||
| African American | 37.2 (6.1) | 36.4 (6.1) | 26.4 (4.2) | |
| Caribbean Black | 17.7 (4.9) | 31.0 (5.0) | 51.3 (7.9) | |
| non-Hispanic White | 34.2 (8.8) | 37.0 (5.6) | 28.8 (6.9) | |
Abbreviations: SE, standard error; GAD, generalized anxiety disorder; PTSD, post-traumatic stress disorder; PD, panic disorder. All estimates are weighted to be nationally representative of the given population and subpopulations in the coterminous 48 states of the U.S. Standard errors and Chi-square statistics are adjusted for the sampling stratification, clustering, and weighting of the data. Percentages within a given row sum to 100% and reflect the within-race/ethnicity distributions of mental illness severity among respondents with the focal 12-month anxiety disorder. Chi-square values index the association between race/ethnicity and severity of mental illness among respondents with the given 12-month anxiety disorder.
Generally, whites with an anxiety disorder reported the lowest levels of 30-day functional impairment on the 7 domains of the WHO-DAS-II (Table 4). In particular, the “Out of Role” domain means for whites were significantly lower than those for African Americans for all five anxiety disorders. Similarly, among respondents with GAD or PD, whites had significantly lower impairment means compared to African Americans in all but one WHO-DAS-II domain.
Table 4.
Thirty-day compariso ns of functional impairment using the WHO-DAS-II functional impairment domains in respondents with 12-month anxiety disorders, by race/ethnicity. The values are given as mean score (SE).
| Out of role | Productivity | Self-care | Mobility | Cognition | Social | Family burden | |
|---|---|---|---|---|---|---|---|
| GAD | |||||||
| African American | 10.09 (1.64) | 9.46 (1.56) | 1.54 (0.46) | 5.10 (0.48) | 2.69 (0.56) | 1.60 (0.28) | 8.54 (1.46) |
| Caribbean Black | 9.19 (1.77) | 9.98 (3.53) | 0.46 (0.39) | 2.84 (1.95) | 4.96 (3.48) | 0.38 (0.28)a | 14.33 (1.75)a |
| non-Hispanic White | 2.89 (o.48)a,b | 4.11 (0.57)a | 0.62 (0.21) | 3.06 (0.40)a | 0.89 (0.15)a | 0.57 (0.14)a | 2.52 (0.42)a,b |
| F(2, 256), p-value | 16.4, p < 0.001 | 9.5, p < 0.001 | 2.0, p = 0.14 | 2.3, p = 0.11 | 10.7, p < 0.001 | 4.6, p = 0. 01 | 21.0, p < 0.001 |
| Social anxiety disorder | |||||||
| African American | 7.04 (0.94) | 7.97 (0.91) | 0.85 (0.27) | 3.89 (0.54) | 2.35 (0.40) | 1.61 (0.35) | 5.79 (0.83) |
| Caribbean Black | 7.12 (5.40) | 7.15 (5.22) | 3.11 (2.64) | 4.88 (3.95) | 4.82 (2.77) | 3.60 (2.56) | 6.52 (3.94) |
| non-Hispanic White | 3.81 (0.40)a | 4.78 (0.42)a | 0.46 (0.11) | 2.90 (0.24) | 1.32 (0.18)a | 0.97 (0.14) | 3.59 (0.40)a |
| F(2, 694), p-value | 8.7, p < 0.001 | 8.6, p < 0.001 | 8.6, p < 0.001 | 2.1, p = 0.12 | 10.2, p < 0.001 | 6.4, p< 0. 01 | 6.3, p< 0.01 |
| PTSD | |||||||
| African American | 7.75 (0.91) | 8.02 (0.96) | 0.78 (0.22) | 3.85 (0.78) | 1.87 (0.49) | 1.34 (0.31) | 5.01 (0.95) |
| Caribbean Black | 14.69 (4.14) | 10.71 (5.41) | 2.96 (2.57) | 4.73 (3.88) | 3. 51 (3.20) | 2.94 (2.55) | 6.36 (3.80) |
| non-Hispanic White | 4.35 (0.80)a,b | 6.09 (0.81) | 1.09 (0.26) | 4.40 (0.68) | 1.69 (0.26) | 1.28 (0.21) | 4.26 (0.64) |
| F(2, 391), p-value | 10.3, p < 0.001 | 3.0, p = 0. 05 | 2.8, p = 0.06 | 0.3, p = 0.73 | 1.5, p = 0.23 | 1.7, p = 0. 19 | 0.8, p = 0.44 |
| Panic disorder | |||||||
| African American | 9.44 (1.16) | 10.44 (1.15) | 1.12 (0.23) | 4.47 (0.57) | 3.12 (0.42) | 2.12 (0.39) | 6.32 (0.96) |
| Caribbean Black | 10.43 (3.27) | 10.76 (3.28) | 4.80 (1.94) | 7.62 (2.69) | 6. 25 (2.32) | 5.24 (1.69) | 7.98 (2.45) |
| non-Hispanic White | 4.34 (0.75)a | 6.09 (0.66)a | 0.39 (0.11)a,b | 3.79 (0.76) | 1.71 (0.34)a | 1.24 (0.21)a,b | 3.30 (0.58)a |
| F(2, 294), p-value | 8.4, p < 0.001 | 6.2, p < 0. 01 | 14.9, p < 0.001 | 1.4, p = 0.26 | 6.2, p < 0.01 | 5.6, p< 0. 01 | 5.4, p< 0.01 |
| Agoraphobia w/o PD | |||||||
| African American | 11.41 (1.00) | 10.11 (0.85) | 0.70 (0.04) | 5.36 (1.08) | 2. 22 (0.25) | 1.26 (0.21) | 7.08 (0.48) |
| Caribbean Black | 3.98 (0.82)a | 4.21 (0.80)a | 2.47 (0.39)a | 3.55 (0.13) | 0.83 (0.13)a | 0.90 (0.31) | 4.77 (2.74) |
| non-Hispanic White | 6.66 (1.49)a | 8.25 (1.43) | 1.45 (0.61) | 3.32 (0.81) | 2.13 (0.56)b | 2.64 (0.71)b | 5.22 (1.53) |
| F(2, 106), p-value | 2.6, p = 0.08 | 0.6, p = 0. 53 | 0.6, p = 0.53 | 1.15, p = 0.32 | 0.1, p = 0.90 | 1.2, p = 0. 29 | 0.7, p = 0.50 |
Abbreviations: WHO-DAS-II, World Health Organization Disability Assessment Schedule II; SE, standard error; GAD, generalized anxiety disorder; PTSD, post-traumatic stress disorder; PD, panic disorder. All estimates are weighted to be nationally representative of the given population and subpopulations in the coterminous 48 states of the U.S. Standard errors and F statistics are adjusted for the sampling stratification, clustering, and weighting of the data. Out of role is the number of days of the 30 days preceding the time of interview that respondents reported being completely unable to carry out their normal daily activities. The other six domains indicate the number of days during the same time period in which the respondents' symptoms made carrying out their normal daily domain-specific activities difficult, weighted by the reported degree of that difficulty.
Indicates a significant follow-up t-test (p < 0.05) for the difference between the given mean and the corresponding mean for African Americans.
Indicates a significant follow-up t-test (p < 0.05) for the difference between the given mean and the corresponding mean for Caribbean Blacks.
5.4. Cumulative projected lifetime risk and age of onset
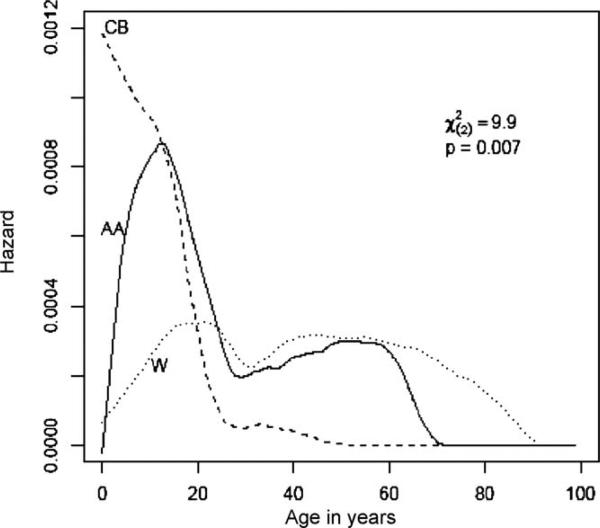
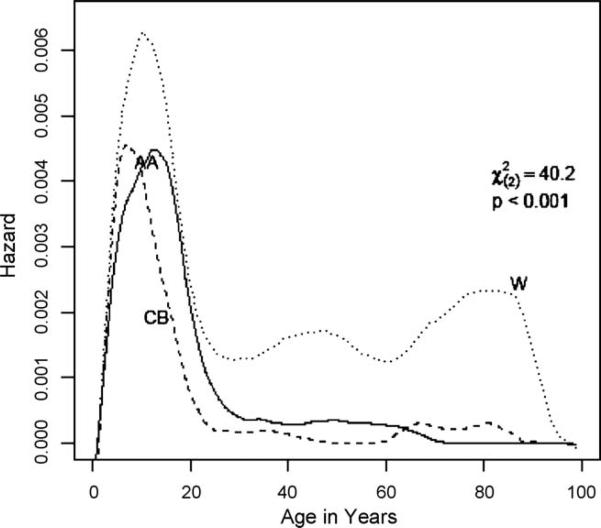
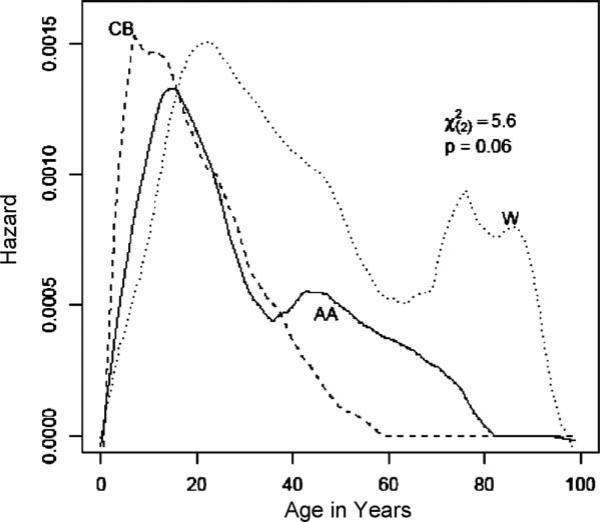
There were statistically significant (p < 0.01) differences across the three race/ethnicity groups in the patterns of risk across the lifespan for all disorders except for PD, for which only a marginally significant (p = 0.06) difference was found (Figs. 1–5). At any given age, non-Hispanic whites had higher cumulative and immediate risk of developing GAD and SAD compared to African Americans and Caribbean Blacks (Table 5 and Figs. 1 and 2). For all three race/ethnic groups, risk for GAD was initially elevated in the late teens and early twenties before declining at subsequent ages (Fig. 1). All three groups were at their greatest risk of developing SAD before age 20 (Fig. 2), with the risk for African Americans and Caribbean Blacks largely confined to this age range. Whites also experienced a sharp drop in risk after age 20, but remained somewhat at risk of developing SAD throughout the rest of the lifespan. The pattern of risk across the three groups observed for GAD and SAD was reversed for PTSD, with African Americans and Caribbean Blacks having both higher cumulative and immediate risk across the lifespan compared to whites (Table 5 and Fig. 3). African Americans were at greatest risk of developing PTSD at any age before approximately age 60 when Caribbean Blacks experienced resurgence in PTSD (Fig. 3). PTSD onset risk was similar across groups and highest in the late teens to early twenties. The three groups experienced their greatest immediate risk for PD at different ages: pre- to early-teenage years for Caribbean Blacks; mid- to late-teens for African Americans, and mid-twenties for whites (Fig. 4). After approximately age 20, the immediate risk was highest among whites and remained so throughout the rest of the lifespan. Both African Americans and Caribbean Blacks were at their greatest risk of developing AGO earlier in life than were whites. Risk of AGO for whites peaked around age 20, and after a small decrease in the thirties, remained relatively constant in later life. This is in contrast to Caribbean Blacks, whose risk for developing AGO was largely confined to before age 20 and was virtually non-existent after age 40.
Fig.1.
Age of onset of GAD by race/ethnicity. These hazard functions describe how the risk of first onset of GAD (Generalized Anxiety Disorder) changes across the lifespan for the three race/ethnic groups.
Fig. 5.
Age of onset of agoraphobia by race/ethnicity.
Table 5.
Projected cumulative lifetime risk at select ages in years, lifetime prevalence, and age of onset quartiles for anxiety disorders, by race/ethnicity.
| Projected lifetime risk at selected ages in years, % (SE)a |
Overall lifetime prevalence, % (SE) | Quartiles of ages of onsetb |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 10 | 20 | 30 | 40 | 50 | 60 | 70 | 25th %-tile | 50th %-tile (median) | 75th %-tile | ||
| GAD | |||||||||||
| African American | 0.25 (0.10) | .63 (0.24) | 2.39 (0.30) | 3.11 (0.36) | 4.42 (0.50) | 4.62 (0.54) | 4.62 (0.54) | 3.26 (0.36) | 14 | 21 | 35 |
| Caribbean Black | 0.07 (0.19) | .62 (0.88) | 2.31 (1.07) | 2.76 (1.22) | 3.41 (1.59) | 3.41 (1.59) | 3.41 (1.59) | 2.67 (0.82) | 12 | 19 | 23 |
| non-Hispanic White | 0.48 (0.08) | .82 (0.16) | 3.63 (0.24) | 5.29 (0.30) | 6.74 (0.36) | 8.15 (0.44) | 8.78 (0.50) | 5.90 (0.32) | 19 | 27 | 40 |
| Social anxiety disorder | |||||||||||
| African American | 2.92 (0.32) | .66 (0.48) | 7.32 (0.50) | 7.59 (0.52) | 7.75 (0.53) | 8.37 (0.62) | 8.37 (0.62) | 7.58 (0.52) | 7 | 12 | 16 |
| Caribbean Black | 3.68 (l.3l) | .74 (1.61) | 5.89 (1.64) | 6.10 (1.69) | 6.10 (1.69) | 6.10 (1.69) | 6.10 (1.69) | 6.00 (1.20) | 6 | 9 | 13 |
| non-Hispanic White | 4.31 (0.25) | .76 (0.34) | 9.98 (0.37) | 11.32 (0.40) | 12.89 (0.44) | 13.98 (0.49) | 15.10 (0.57) | 12.39 (0.45) | 8 | 13 | 25 |
| PTSD | |||||||||||
| African American | 1.65 (0.24) | .04 (0.42) | 7.18 (0.51) | 9.03 (0.60) | 11.25 (0.74) | 12.08 (0.82) | 12.56 (0.90) | 9.10 (0.54) | 12 | 19 | 31 |
| Caribbean Black | 2.13 (1.00) | .80 (1.33) | 7.29 (1.90) | 9.28 (2.26) | 10.18 (2.47) | 10.18 (2.47) | 13.84 (5.76) | 8.42 (1.80) | 10 | 23 | 26 |
| non-Hispanic White | 1.45 (0.19) | .07 (0.31) | 5.85 (0.37) | 6.54 (0.40) | 7.43 (0.45) | 8.04 (0.49) | 8.39 (0.53) | 6.84 (0.54) | 12 | 18 | 27 |
| Panic disorder | |||||||||||
| African American | 0.62 (0.15) | .22 (0.28) | 2.97 (0.33) | 3.36 (0.37) | 4.02 (0.45) | 4.37 (0.51) | 4.86 (0.66) | 3.45 (0.33) | 12 | 17 | 25 |
| Caribbean Black | 1.69 (0.89) | .08 (1.20) | 3.92 (1.37) | 4.41 (1.52) | 4.54 (1.57) | 4.61 (1.61) | 4.61 (1.61) | 4.12 (1.61) | 7 | 15 | 21 |
| non-Hispanic White | 0.40 (0.08) | .81 (0.16) | 3.45 (0.23) | 4.61 (0.28) | 5.44 (0.31) | 6.09 (0.36) | 6.61 (0.42) | 4.81 (0.23) | 18 | 25 | 35 |
| Agoraphobia w/o PD | |||||||||||
| African American | 0.40 (0.08) | .81 (0.16) | 3.45 (0.23) | 4.61 (0.28) | 5.44 (0.31) | 6.09 (0.36) | 6.61 (0.42) | 2.08 (0.32) | 9 | 13 | 18 |
| Caribbean Black | 1.37 (0.81) | .04 (0.98) | 2.07 (0.99) | 2.15 (1.02) | 2.15 (1.02) | 2.15 (1.02) | 2.15 (1.02) | 2.11 (0.94) | 4 | 8 | 12 |
| non-Hispanic White | 0.17 (0.05) | .52 (0.09) | 0.85 (0.11) | 1.00 (0.13) | 1.49 (0.17) | 1.64 (0.19) | 2.09 (0.28) | 1.31 (0.14) | 15 | 24 | 45 |
Abbreviations: SE, standard error; GAD, generalized anxiety disorder; PTSD, post-traumatic stress disorder; PD, panic disorder. All estimates are weighted to be nationally representative of the given population and subpopulations in the coterminous 48 states of the U.S.
Percentages represent the probability of an individual from a given race/ethnic group developing the focal disorder by the ages indicated in the column headings. Estimates were derived from Kaplan-Meier curves containing respondents who developed the focal disorder by their age at interview as well as those who did not.
Age of onset percentiles represent the ages by which 25%, 50%, and 75% of respondents developed the focal disorder. Estimates were derived from Kaplan-Meier curves containing only those respondents who developed the focal disorder by their age at interview.
Fig. 2.
Age of onset of SAD by race/ethnicity. These hazard functions describe how the risk of first onset of SAD (Social Anxiety Disorder) changes across the lifespan for the three race/ethnic groups.
Fig. 3.
Age of onset of PTSD by race/ethnicity. These hazard functions describe how the risk of first onset of PTSD (Post-Traumatic Stress Disorder) changes across the lifespan for the three race/ethnic groups.
Fig. 4.
Age of onset of panic disorder by race/ethnicity. These hazard functions describe how the risk of first onset of PD (Panic Disorder) changes across the lifespan for the three race/ethnic groups.
Caribbean Blacks had the earliest median age of onset for all disorders except PTSD and had the youngest 75th percentile onset ages for all disorders. In contrast, with the exception of PTSD, whites remained at risk of developing anxiety disorders for a wider age range than the other two groups. This difference was quite dramatic for SAD and AGO with whites’ 75th percentile ages of onset being 25 and 45, respectively, whereas the highest of the other two groups was in the teenage years. These race/ethnic differences aside, the 75th percentiles of the age of onset distributions tended to be youngest for SAD for all three groups and for AGO for African Americans and Caribbean Blacks. GAD had the oldest onset ages at the 75th percentile.
5.5. Sociodemographic and psychiatric risk factors
Race/ethnicity was a statistically significant predictor overall for all five anxiety disorders (Table 6). Specifically, whites were at increased risk of developing GAD, SAD, and PD and decreased risk of developing PTSD and AGO compared to African Americans. Females were more at risk than males of developing all five disorders. Age cohort was a strong predictor of disorder onset across all five disorders, although less strong for AGO, with younger cohorts being more likely to develop the disorders than those aged 60 or older. Marital status at age of disorder onset was predictive for the development of all disorders except AGO. Specifically, being “never married” was a risk factor for developing SAD, but was a protective factor for PTSD and PD compared to being “currently married.” In addition, compared to being “currently married”, being “previously married” was associated with increased risk of subsequently developing GAD, SAD and PTSD. Education was significantly associated with only AGO, with a trend for increased risk among those with less than 16 years of education.
Table 6.
Multivariate risk factors for lifetime onset of DSM-IV/WMH-CIDI anxiety disorders.
| HR (95% CI) |
|||||
|---|---|---|---|---|---|
| GAD | SAD | PTSD | Panic Disorder | Agoraphobia w/o PD | |
| Race/ethnicity | |||||
| African American | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Caribbean Black | 0.8 (0.3-1.8) | 0.8 (0.5-1.3) | 1.0 (0.6-1.8) | 1.3 (0.6-3.2) | 1. 1 (0.4-2.7) |
| NCS-R White | 1.6 (1.2-2.1)* | 1.5 (1.3-1.8)* | 0.7 (0.6-0.9) | 1.4 (1.1-1.7)* | 0.5 (0.3-0.8) |
| Sex | |||||
| Male | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Female | 1.5 (1.1-2.0)* | 1.3 (1.1-1.5)* | 2.7 (2.3-3.2)* | 1.8 (1.4-2.2)* | 1.8 (1.2-2.6)* |
| Cohort | |||||
| 18-29 | 2.8 (1.9-4.2)* | 1.7 (1.4-2.2)* | 4.3 (3.0-6.2)* | 4.2 (2.5-7.0)* | 2.4 (1.0-5.6)* |
| 30-44 | 2.2 (1.6-3. )* | 2.0 (1.6-2.6)* | 3.1 (2.2-4.5)* | 3.9 (2.4-6.2)* | 2.7 (1.3-5.5)* |
| 45-59 | 2.1 (1.4-3.1)* | 2.0 (1.7-2.4)* | 2.8 (1.9-4.0)* | 3.0 (1.8-4.8)* | 2.6 (1.3-5.2)* |
| >60 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Marital statusa | |||||
| Married | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Never married | 0.8 (0.6-1.1) | 1.8 (1.2-2.8)* | 0.6 (0.5-0.9)* | 0.6 (0.5-0.9)* | 0.5 (0.2-1.4) |
| Previously married | 1.7 (1.3-2.3)* | 2.3 (1.2-4.4)* | 1.5 (1.1-1.9)* | 0.8 (0.6-1.1) | 1.1 (0.6-2.2) |
| Educationa | |||||
| Student | 1.2 (0.6-2.4) | 1.3 (0.6-2.5) | 0.9 (0.5-1.5) | 0.9 (0.5-1.6) | 3.6 (0.7-17.4) |
| 0-11 years | 1.0 (0.7-1.5) | 1.6 (0.9-3.1) | 1.3 (0.9-1.9) | 0.9 (0.6-1.5) | 5. 0 (1.6-15.5)* |
| 12 years | 0.8 (0.5-1.1) | 1.6 (0.8-3.2) | 1.0 (0.7-1.4) | 0.8 (0.6-1.2) | 1. 6 (0.4-6.3) |
| 13-15 years | 1.3 (0.9-1.8) | 1.1 (0.6-2.4) | 1.0 (0.7-1.4) | 1.0 (0.6-1.4) | 3.1 (1.3-7.7)* |
| >16 years | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Prior/concurrent onset of | |||||
| Any mood disordera | 4.1 (2.9-5.8)* | 5.6 (4.4-7.2)* | 6.3 (5.0-8.0)* | 4.6 (3.6-5.8)* | 3.8 (2.2-6.4)* |
| Any substance disordera | 1.3 (0.96-1.8) | 1.6 (0.99-2.6) | 2.6 (2.0-3.3)* | 1.6 (1.1-2.4)* | 1.5 (0.8-2.6) |
| Any eating disordera | 1.1 (0.6-1.9) | 2.2 (1.1-4.0)* | 1.4 (0.9-2.2) | 1.6 (1.03-2.4)* | 2.0 (0.9-4.0) |
Abbreviations: WMH-CIDI, World Mental Health version of the Composite International Diagnostic Interview; HR, hazard ratio; CI, confidence interval; GAD, generalized anxiety disorder; SAD, social anxiety disorder; PTSD, post-traumatic stress disorder; PD, panic disorder. Each column represents the results of a single, multivariate Cox proportional hazards regression model with the onset age of the focal anxiety disorder as the outcome and all of the sociodemographic factors as covariates. Results observed for a given variable are net of the effects of the other variables in the models. All model estimates are weighted to be nationally representative of the given population and subpopulations in the coterminous 48 states of the U.S. Confidence intervals are adjusted for the sampling stratification, clustering, and weighting of the data. Chi-square values were obtained from design-based variance-covariance matrices to adjust for the stratification, clustering, and weighting of the data.
Variables are coded in the models as time-varying such that associations reflect the status of respondents at the age of anxiety disorder onset and not necessarily their status at the time of their interview.
Indicates a hazard ratio significantly different from 1.0, p < 0.05.
All five of the anxiety disorders were strongly associated with the prior or concurrent onset of mood disorder. That is, individuals who had developed a mood disorder at a given age were significantly more likely to develop an anxiety disorder at that same age or later. The strongest association was found for PTSD. The weakest association was found for AGO. The prior/ concurrent onset of a substance disorder significantly elevated the risk of developing PTSD (HR = 2.6, 95% CI: 2.0–3.3) and PD (HR = 1.6, 95% CI: 1.1–2.4). Additionally, prior/concurrent substance disorder elevated the risks for GAD and SAD at a marginally statistically significant level (p < 0.10). Finally, prior/ concurrent onset of an eating disorder raised the risk of developing SAD and PD.
6. Discussion
The results of this study indicate that anxiety disorders are common and impairing conditions for African Americans, Caribbean Blacks, and whites in the U.S. Most anxiety disorders (GAD, PD, SAD) were more prevalent among whites compared to African Americans and Caribbean Blacks. These divergent rates are similar to a recent study reporting higher rates of GAD and SAD among whites (Breslau et al., 2006). Elevated rates of PD among whites in this study mirrors a similar elevated rate found in the Epidemiologic Catchment Area Survey (Eaton, Dryman, & Weissman, 1991). Increased risk for most anxiety disorders among whites remains somewhat counterintuitive given increased social and economic stressors experienced by blacks (Clark et al., 1999; Turner & Lloyd, 2004). One potential explanation for these reduced rates may be that harsh social circumstances experienced by many blacks results in particularly high levels of resilience in the face of stress (Neal-Barnett & Smith, 1997; Neal & Turner, 1991). It is also possible that higher levels of religiosity among blacks may buffer the impact of anxiety-evoking stressors which may provide some protection from certain disorders (Taylor, Chatters, & Jackson, 2007; Taylor, Chatters, Jayakody, & Levin, 1996; Taylor, Chatters, & Levin, 2004).
Elevated risk for most anxiety disorders among whites may also relate in part to mood disorder risk. Major depression and other mood disorders are more prevalent among whites (Breslau et al., 2005) and the present study indicates that persons who meet criteria for depression are at greater risk to experience a subsequent or concurrent anxiety disorder. Thus, it is possible that some of the increased risk of anxiety disorders among whites may occur secondarily to a primary depressive disorder. A similar argument can be made that pre-existing substance abuse disorders also contribute to elevated rates of certain anxiety disorders among whites since whites are at increased substance use disorder risk over blacks (Breslau et al., 2005). Overall, it is likely that preexisting mood and substance disorders account for some portion of the increased risk for most anxiety disorders among whites.
In contrast to the lower rates of most anxiety disorders found among African Americans and Caribbean Blacks, PTSD was more prevalent among African Americans and Caribbean Blacks. This elevated rate likely relates at least in part to increased exposure to high-trauma (e.g., crime) environments (Alim, Charney, & Mellman, 2006a; Alim, Graves, & Mellman, 2006b; Breslau, Davis, & Andreski, 1995; Carter, Sbrocco, & Carter, 1996; Schwartz, Bradley, & Sexton, 2005). Further, blacks are also more likely to experience race-related stressors and oppression that can lead to increased feelings of victimization (Alim, Graves, et al., 2006; Schwartz et al., 2005) which may also increase the risk for PTSD. Finally, Breslau and colleagues (Breslau, Chilcoat, & Kessler, 1999) found that previous exposure to a violent assault led to an increased risk for PTSD from a subsequent trauma, and that this risk persisted over time. Since black children are more likely to live in areas where their risk for being a victim or a witness of violent assault is higher (Margolin & Gordis, 2000) they may have increased risk for PTSD (Boney-McCoy & Finkelhor, 1995).
Importance of comparative prevalence rates notwithstanding, levels of mental illness severity and disability were generally greater among African Americans and Caribbean Blacks compared to whites. Caribbean Black respondents with anxiety disorders were particularly likely to experience severe mental illness compared to the other race/ethnic groups. Similarly, African Americans and Caribbean Blacks with anxiety disorders reported greater levels of functional impairment compared to whites. Overall, although black participants were generally less likely to suffer from an anxiety disorder compared to whites, blacks who do meet criteria are often highly impaired.
There were several other important socio-demographic correlates and risk factors that influenced the rates of anxiety disorders in this study. As expected, being female increased risk for all anxiety disorders among African Americans and whites, especially GAD, PTSD, and PD. Several scholars have identified both psychosocial (Silverman & Carter, 2006) and biological (Altemus, 2006) processes related to high anxiety disorder risk among females. However, the relationship between gender and anxiety disorders for Black Caribbeans is contrary to the findings of African Americans and whites and contrary to previous research. Among black Caribbeans, men had significantly higher rates of PTSD than women. In fact, black Caribbean men had the highest rates of PTSD of the six gender and race groups studied. This finding is consistent with higher suicide attempt (Joe et al., 2006) and major depression (Williams et al., 2007) risk among black Caribbean men compared to women. Additionally, non-significant, yet higher than expected rates of GAD, SAD, and PD were observed among Caribbean Black men relative to Caribbean Black females. Although there are many possible reasons for these findings, recent research suggests that Caribbean women have an easier adjustment to immigration (Foner, 2005). In fact, Caribbean Black women may experience increased power and autonomy from improved employment opportunities in the US (Butterfield, 2004; Foner, 1998, 2005) which may be stressful for Caribbean Black men given the patriarchal nature of Caribbean households (Chevannes, 2001).
Similarly, previously married persons also experienced increased risk for anxiety disorders, especially SAD. Higher risk of SAD among respondents while not married or cohabitating likely relates to problems securing a partner in addition to anxiety resulting from terminated relationships. Finally, lowered educational achievement, higher rates of poverty, or both were observed among persons with 12-month SAD, PTSD, PD, and AGO. Again, these economic and educational hardships likely both contribute to and result from anxiety disorders (Jayakody, Danziger, & Kessler, 1998).
Our extensive examination of ages of onset among the three race/ethnic groups in this study yielded several interesting findings that help to account for the high rates of SAD, GAD, and PD among whites and high rates of PTSD among African Americans and Caribbean Blacks. For most anxiety disorders, whites, African Americans, and Caribbean Blacks experience greatest risk to develop a disorder in their teens or twenties. However, for many anxiety disorders (GAD, SAD, PD), whites carry substantially greater risk to experience the onset of a new anxiety disorder after age sixty. It is not possible to clearly determine precisely why whites are at extended risk to develop these conditions but differential rates of workforce participation (Green, 2005) and late-life migration patterns (Watkins, 1989) may play important risk and protective roles for older persons. White American men are substantially more likely to remain in the workforce beyond age sixty (Green, 2005) which may expose them to greater work stress, including age-related discrimination (Noonan, 2005), which may increase risk for new anxiety disorders later in life. It is important to note that lower work force participation among older blacks is substantially influenced by reduced workforce participation opportunities as opposed to a greater preference for retirement (Flippen & Tienda, 2000; McNamara & Williamson, 2004). Whites also far exceed blacks in the rate of late-life relocation to different parts of the country (Newbold, 1996; Watkins, 1989). Although these transitions can be positive for some individuals, others may find establishing interpersonal relationships, navigating new surroundings, and living far from family members quite challenging (Castle, 2001), which also may increase risk for late-life anxiety disorders. In contrast to reduced late-life risk for most anxiety disorders among blacks, late-life PTSD risk was high among African Americans and Caribbean Blacks. This finding likely relates to increased exposure to high-trauma environments late in life and other socio-cultural factors as described above.
One of the most interesting findings related to age of disorder onset is the greater risk of early onset for all anxiety disorders among Caribbean Blacks. One partial explanation for this finding may relate to the relatively common practice of “child fostering” (Waters, 1999). This rearing style involves youth living in the Caribbean with a grandparent until adolescence followed by immigration to the U.S. to live with the youth's biological parents (Waters, 1999). The combination of immigration to a new country coupled with being raised by parents that the youth may not know well is often quite stressful and may elevate risk for anxiety disorders among these youth. A second possible contributor to early onset anxiety disorders among Caribbean Blacks may relate to high levels of academic/vocational achievement stress experienced by many children of immigrant parents (Waters, 1999). Parents raised in the Caribbean often expect high levels of academic/vocational achievement for their children, but racial discrimination and poor schools in many areas populated by Caribbean Blacks can contribute to a large gap between parent expectations and youth achievement (Waters, 1999). This tension may contribute to the increased anxiety disorder risk observed among Caribbean Black youth. Clearly, more study is needed to further delineate the reasons for early onset anxiety disorders in this group.
The present study has limitations. First, although this is the largest study of whites, Caribbean Blacks, and African Americans with anxiety disorders conducted to date, the limited number of African Americans and Caribbean Blacks meeting criteria for certain anxiety disorders limits statistical power when attempting to estimate interactions between race/ethnicity and the socio-demographic correlates of and risk factors for the anxiety disorders. Second, the cross-sectional nature of this study does not allow for ongoing assessment of temporal relationships between disorders or precise investigation of causative factors over time. Third, although the NCS-R and NSAL have screening sections for psychotic disorders, they do not fully assess non-affective psychotic disorders.
Overall, the present report provides the most comprehensive information about anxiety disorders among African Americans, Caribbean Blacks, and whites in the U.S. It is clear that anxiety disorders are significant public health problems in the white and black communities in the U.S. Differences in anxiety disorder risk and disorder onset ages can be used to inform targeted interventions to prevent or remediate anxiety disorders among these diverse groups. Future research is needed to further delineate differences in the heterogeneous white and black populations with respect to anxiety disorder prevalence, symptom profiles, comorbidity, impairment, service utilization, and responses to treatment.
Acknowledgements
We appreciate the assistance provided in all aspects of the NSAL study by the Program for Research on Black Americans faculty and research staff including Jamie Abelson, M.S.W., Phyllis Stillman, BA, Julie Sweetman, MS, and Myriam Torres, MS. Special thanks to Dr. Ronald C. Kessler for development in the NCS-R of the diagnostic algorithms used in this study and for permission to use the non-Hispanic white NCS-R sample for this study.Funding/support: The NSAL is supported by the National Institute of Mental Health (NIMH; U01-MH57716) with supplemental support from the OBSSR Office of Behavioral and Social Science Research at the National Institutes of Health (NIH) and the University of Michigan.
References
- Alim TN, Charney DS, Mellman TA. An overview of post-traumatic stress disorder in African Americans. Journal of Clinical Psychology. 2006a;62:801–813. doi: 10.1002/jclp.20280. [DOI] [PubMed] [Google Scholar]
- Alim TN, Graves E, Mellman TA. Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. Journal of the National Medical Association. 2006b;98:1630–1636. [PMC free article] [PubMed] [Google Scholar]
- Altemus M. Sex differences in depression and anxiety disorders: Potential biological determinants. Hormones and Behavior. 2006;50:534–538. doi: 10.1016/j.yhbeh.2006.06.031. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Boney-McCoy S, Finkelhor D. Psychosocial sequalae of violent victimization in a national youth sample. Journal of Consulting and Clinical Psychololgy. 1995;63:726–736. doi: 10.1037//0022-006x.63.5.726. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P. Risk factors of PTSD-related traumatic events: A prospective analysis. American Journal of Psychiatry. 1995;152:529–535. doi: 10.1176/ajp.152.4.529. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC. Previous exposure to trauma and PTSD effects of subsequent trauma: Results from the Detroit Area Survey of Trauma. American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Kendler K, Su M, Williams D, Kessler RC. Specifying race-ethnic difference in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2005;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Aguilar S, Kendler KS, Su M, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2006;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butterfield S. Challenging American conceptions of rare and ethnicity: Second generation West Indian immigrants. International Journal of Sociology and Social Policy. 2004;24:75–102. [Google Scholar]
- Carter MM, Sbrocco T, Carter C. African Americans and anxiety disorders research: Development of a testable theoretical framework. Psychotherapy. 1996;33:449–463. [Google Scholar]
- Castle NG. Relocation of the elderly. Medical Care Research and Review. 2001;58:291–333. doi: 10.1177/107755870105800302. [DOI] [PubMed] [Google Scholar]
- Chevannes B. Learning to be a man: Culture, socialization and gender identity in five Caribbean communities. University of the West-Indies Press; Kingston, Jamica: 2001. [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychyosocial model. American Psychologist. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Cox DR. Regression models and life-tables. Journal of the Royal Statistical Society. Series B (Methodological) 1972;34:187–220. [Google Scholar]
- Eaton WW, Dryman A, Weissman MM. Panic and phobia. In: Robins LN, Regier DA, editors. Psychiatric disorders in America. Free Press; New York: 1991. [Google Scholar]
- Flippen C, Tienda M. Pathways to retirement: Patterns of labor force participation and labor market exit among the pre-retirement population. Journal of Gerontology. 2000;55B:S14–S27. doi: 10.1093/geronb/55.1.s14. [DOI] [PubMed] [Google Scholar]
- Foner N. Benefits and burdens: Immigrant women and work in New York City. Gender Issues. 1998;16:5–24. [Google Scholar]
- Foner N. In a new land: A comparative view of immigration. New York University Press; New York: 2005. [Google Scholar]
- Green CA. Race, ethnicity, and social security retirement age in the U.S. Feminist Economics. 2005;11:117–143. [Google Scholar]
- Heeringa SG, Torres M, Sweetman JS, Baser R. Sample design, weighting, and variance estimation for the 2001–2003 National Survey of American Life (NSAL) Adult Sample (technical report) Survey Research Center of the Institute for Social Research at the University of Michigan; Ann Arbor, MI: 2006. [Google Scholar]
- Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES). International Journal of Methods in Psychiatric Research. 2004;13:221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemingway H, Whitty CJM, Shipley M, Stansfeld MS, Brunner E, Fuhrer R, et al. Psychosocial risk factors for coronary disease in white South Asian and Afro-Caribbean civil servants: The Whitehall II study. Ethnicity and Disease. 2001;11:391–400. [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied survival analysis: Regression modeling of time to event data. John Wiley & Sons Inc; New York: 2000. [Google Scholar]
- Jackson JS, Neighbors HW, Nesse RM, Trierweiler SJ, Torres M. Methodological innovations in the National Survey of American Life. International Journal of Methods of Psychiatric Research. 2004a;13:289–298. doi: 10.1002/mpr.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, et al. The National Survey of American Life: A study of racial, ethnic and cultural influences on mental disorders and mental health. International Journal of Methods in Psychiatric Research. 2004b;13:196–207. doi: 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayakody R, Danziger S, Kessler RC. Early-onset psychiatric disorders and male socioeconomic status. Social Science Research. 1998;27:371–387. [Google Scholar]
- Joe S, Baser RE, Breeden G, Neighbors HW, Jackson JS. Prevalence of and risk factors for lifetime suicide attempts among Blacks in the United States. JAMA. 2006;296(17):2112–2123. doi: 10.1001/jama.296.17.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan EL, Meier P. Nonparametric estimation form incomplete observations. Journal of The American Statistical Association. 1958;53:457–481. [Google Scholar]
- Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, et al. The US National Comorbidity Survey Replication (NCS-R): Design and field procedures. International Journal of Methods in Psychiatric Research. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): Background and aims. Intenational Journal of Methods in Psychiatric Research. 2004;13:60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KnÄuper B, Cannell CF, Schwarz N, Bruce ML, Kessler RC. Improving accuracy of major depression age-of-onset reports in the US National Comorbidity Survey. International Journal of Methods in Psychiatric Research. 1999;8:39–48. [Google Scholar]
- Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. International Journal of Psychiatry Medicine. 1997;27:93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- Logan JR, Deane G. Black diversity in metropolitan America. The Mumford Center for Comparative Urban and Regional Research; Albany, NY: 2003. [Google Scholar]
- Lumley T. Analysis of complex survey samples. Journal of Statistical Software. 2004;9 [Google Scholar]
- Margolin G, Gordis EB. The effects of family and community violence on children. Annual Review of Psychology. 2000;51:445–479. doi: 10.1146/annurev.psych.51.1.445. [DOI] [PubMed] [Google Scholar]
- McNamara TK, Williamson JB. Race, gender, and the retirement decisions of people ages 60–80: Prospects for age integration in employment. International Journal of Aging and Human Development. 2004;59:255–286. doi: 10.2190/GE24-03MX-U34P-AMNH. [DOI] [PubMed] [Google Scholar]
- Neal-Barnett AM, Smith SJ. African Americans. In: Friedman S, editor. Cultural issues in the treatment of anxiety. Guilford Press; New York: 1997. pp. 154–174. [Google Scholar]
- Neal AM, Turner SM. Anxiety disorders research with African Americans: Current status. Psychological Bulletin. 1991;109:400–410. doi: 10.1037/0033-2909.109.3.400. [DOI] [PubMed] [Google Scholar]
- Newbold KB. Determinants of elderly interstate migration in the United States. Research on Aging. 1996;18:451–476. [Google Scholar]
- Noonan AE. At this point now: Older workers’ reflections on their current employment experiences. International Journal of Aging and Human Development. 2005;61:211–241. doi: 10.2190/38CX-C90V-0K37-VLJA. [DOI] [PubMed] [Google Scholar]
- Rehm J, Ustun B, Saxena S, Nelson CB, Chatterji S, Ivis F, et al. On the development and psychometric testing of the WHO screening instrument to assess disablement in the general population. International Journal of Methods of Psychiatric Research. 1999;8:110–123. [Google Scholar]
- SAS Institute . SAS/STAT user's guide, version 9.1. SAS Institute Inc; Cary, NC: 2005. [Google Scholar]
- Schwartz AC, Bradley RL, Sexton M. Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatric Services. 2005;56:212–215. doi: 10.1176/appi.ps.56.2.212. [DOI] [PubMed] [Google Scholar]
- Selten JP, Slaets JP, Kahn RS. Schizophrenia in Surinamese and Dutch Antillean immigrants to The Netherlands: Evidence of an increased incidence. Psychological Medicine. 1997;27:807–811. doi: 10.1017/s0033291797005199. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services Mental health: Culture, race, and ethnicity—A supplement to mental health: A report of the surgeon general—executive summary. 2001 Retrieved from: www.surgeongeneral.gov/library/mentalhealth/cre/ [PubMed]
- Silverman WK, Carter R. Anxiety disturbance in girls and women. In: Worell J, Goodheart CD, editors. Handbook of girls’ and womens’ psychological health: Gender and well-being across the lifespan. Oxford University Press; New York: 2006. [Google Scholar]
- Simon GE, VonKorff M. Recall of psychiatric history in cross-sectional surveys: Implications for epidemiologic research. Epidemiologic Reviews. 1995;17(1):221. doi: 10.1093/oxfordjournals.epirev.a036180. [DOI] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Jackson JS. Religious and spiritual Involvement among older African Americans, black Caribbeans and whites: Findings from the National Survey of American Life. Journal of Gerontology: Social Sciences. 2007;62B:S238–S250. doi: 10.1093/geronb/62.4.s238. [DOI] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Jayakody RT, Levin JS. Black and white differences in religious participation: A multi-sample comparison. Journal for the Scientific Study of Religion. 1996;35:403–410. [Google Scholar]
- Taylor RJ, Chatters LM, Levin JS. Religion in the lives of African Americans: Social psychological and health perspectives. Sage; Newbury Park: 2004. [Google Scholar]
- R Development Core Team . R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2006. [Google Scholar]
- Turner RJ, Lloyd DA. Stress burden and the lifetime incidence of psychiatric disorder in young adults: Racial and ethnic contrasts. Archives of General Psychiatry. 2004;41:481–488. doi: 10.1001/archpsyc.61.5.481. [DOI] [PubMed] [Google Scholar]
- van Os J, Takei N, Castle DJ, Wessely S, Der G, Macdonald AM, et al. The incidence of mania: Time trends in relation to gender and ethnicity. Social Psychiatry and Psychiatric Epidemiology. 1996;31:129–136. doi: 10.1007/BF00785759. [DOI] [PubMed] [Google Scholar]
- Waters MC. Black identities: West Indian immigrant dreams and American realities. Russell Sage Foundation; New York: 1999. [Google Scholar]
- Watkins JF. Gender and race differentials in elderly migration. Research on Aging. 1989;11:33–52. doi: 10.1177/0164027589111002. [DOI] [PubMed] [Google Scholar]
- Williams DR. Race, stress and mental health: Findings from the Commonwealth Minority Health Survey. In: Hogue C, Hargraves M, Scott-Collins K, editors. Minority health in America: Findings and policy implication from the Commonwealth Fund Minority Health Survey. Johns Hopkins University Press; Baltimore, MD: 2000. pp. 209–243. [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and non-Hispanic Whites: Results from the National Survey of American Life. Archives of General Psychiatry. 2007;64:307–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Williams DR, Harris-Reid M. Race and mental health: Emerging patterns and promising approaches. In: Horwitz AV, Scheid TL, editors. A handbook for the study of mental health: Social contexts, theories and systems. Cambridge University Press; New York, NY: 1999. pp. 295–314. [Google Scholar]
- Williams DR, Lavizzo-Mourey R, Warren RC. The concept of race and health status in America. Public Health Reports. 1994;109:26–41. [PMC free article] [PubMed] [Google Scholar]