The Patient Protection and Affordable Care Act (ACA) established coverage requirements for clinical preventive services for most types of public and private health insurance.1 Combined with significant insurance expansions, these provisions could improve access to a wide range of preventive health services for children and adults. This policy change is important for public health professionals who provide clinical preventive services, as well as for efforts to achieve greater access to preventive services through community-based prevention efforts. However, because of variations in the requirements established under the ACA, as well as ongoing challenges in implementation, advances in access and coverage will be fully realized only through sustained engagement and action on the part of the public health community.
In this installment of Law and the Public's Health, we explain the ACA's preventive services provisions and how they apply across various forms of health insurance. We then discuss ongoing barriers to coverage and conclude with ways public health stakeholders can maximize the impact of the new requirements.
THE ACA PREVENTIVE SERVICES PROVISIONS
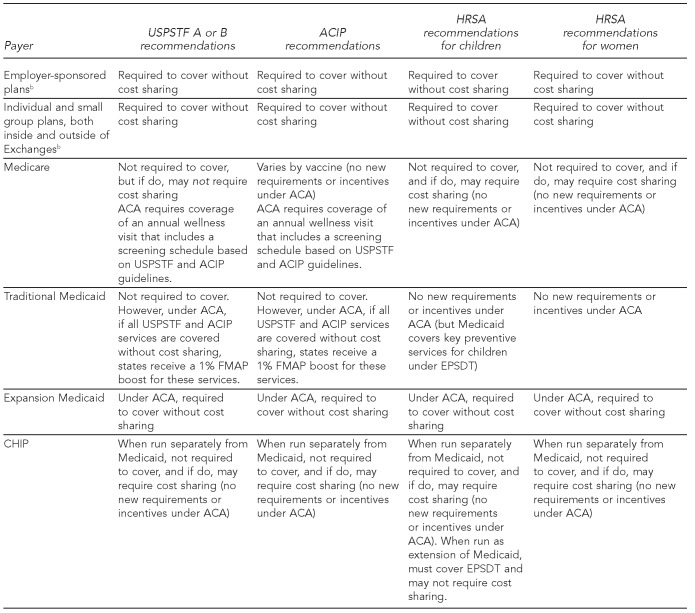
The ACA's preventive services provisions build upon a single definition of preventive services coverage.2 At the same time, this definition varies in its application to the principal forms of health insurance that exist in the wake of the ACA: private coverage obtained through employer-sponsored health plans or purchased in the individual market, Medicare, Medicaid for both traditional beneficiary populations and those made newly eligible by the ACA's adult eligibility expansion, and the Children's Health Insurance Program (CHIP).
The ACA's definition of preventive services
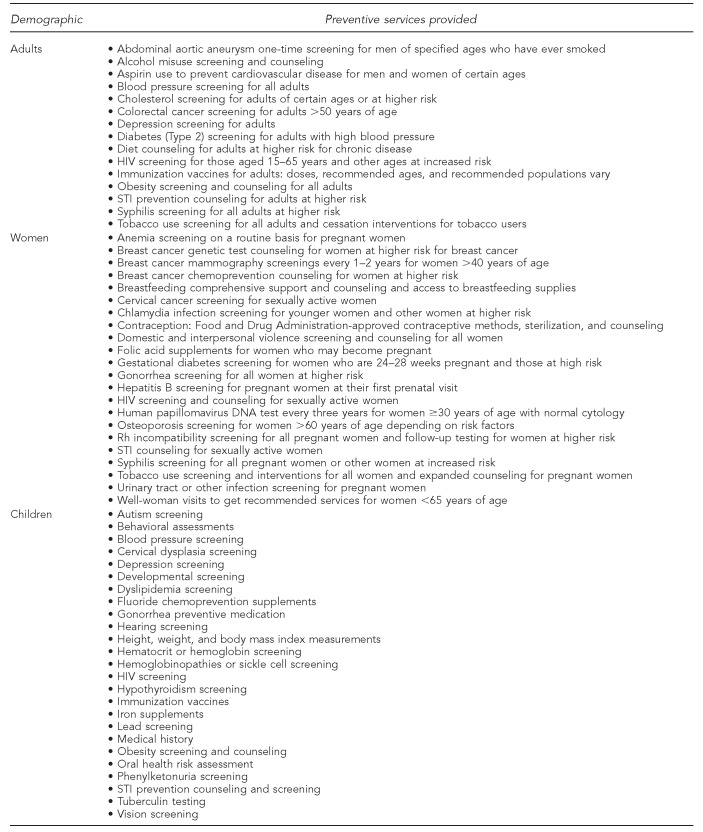
The starting point in understanding this complex interaction between the ACA's preventive services coverage standard and various forms of health insurance is the ACA's definition of covered preventive services. This definition2 encompasses the following range of screening and treatment procedures, all of which must be covered without cost sharing (e.g., deductibles, coinsurance, and copayments):
U.S. Preventive Services Task Force (USPSTF) items or services with a grade of “A” or “B”;
Immunizations recommended by the Centers for Disease Control and Prevention's Advisory Committee on Immunization Practices (ACIP);
Evidence-informed preventive care and screening guidelines for infants, children, and adolescents recommended by the Health Resources and Services Administration (HRSA) (reflected in the “Bright Futures” recommendations developed by HRSA in cooperation with the American Academy of Pediatrics);3 and
Additional preventive care and screening services for women recommended by HRSA (based on a set of recommendations made by an Institute of Medicine panel and adopted by HRSA in 2011).4,5
We refer to these services as “§2713 services” because they are codified at §2713 of the Public Health Service Act (Figure 1).2
Figure 1.
Summary chart of §2713a preventive services
aPHSA §2713, added by Pub. L. No. 111-148 §1001 (2010).
HIV = human immunodeficiency virus
STI = sexually transmitted infection
Private health insurance coverage
Employer-sponsored health plans.
More than half of all working-age Americans are covered through employer-sponsored plans.6 The ACA applies the §2713 preventive services coverage standard to employer-sponsored plans—whether self-insured and, thus, exempt from state insurance regulation, or fully insured and subject to state insurance laws—that are governed by the Employee Retirement Income Security Act.7 The only exception is for employer plans that are covered by the ACA's grandfathering provisions and, thus, are exempt from many of the Act's regulatory reforms.8 Plans lose their grandfathering status over time when they make changes to cost sharing or benefits. As of 2013, about 36% of insured employees were covered through grandfathered plans, down from 56% in 2011.9
Private health insurance plans purchased in the individual market, whether through the Exchange or in the non-Exchange market.
The §2713 coverage standard also applies to private health insurance plans purchased in the individual market, whether through state Exchanges or in the non-Exchange market. As with employer plans, the ACA provides an exemption for grandfathered plans.
In the case of both employer-sponsored and individually purchased private insurance, federal regulations10 and guidelines clarify several aspects of this private coverage obligation:
Cost sharing for associated office visit: When an enrollee receives a covered preventive service, a plan may not impose cost sharing for the visit unless either (1) the provider bills the service and visit separately or (2) the preventive service was not the primary purpose of the visit.10 The guidance is not clear on who determines what constitutes the primary purpose of a visit.
Well-woman visit: A well-woman visit is a preventive service because it is included in the HRSA guidelines.5 Therefore, plans cannot require cost sharing for the visit itself or for any §2713 services provided during the visit, even if the visit and services are billed separately.
Treatment that results from a covered preventive service: Plans may impose cost sharing for treatment that is needed subsequent to a §2713 service (e.g., treatment for chlamydia that is detected in a covered screening).10
In-network vs. out-of-network providers: In general, plans that use a provider network (virtually all plans) are not required to cover out-of-network preventive services.10 However, if no in-network provider is available to deliver a §2713 service (e.g., if no network provider can insert a long-acting reversible contraceptive), a plan must cover the service out of network without cost sharing.11
Frequency, method, treatment, or setting: If the authoritative body (e.g., USPSTF, ACIP, or HRSA) does not specify the “frequency, method, treatment, or setting” for a service, a plan may use “reasonable medical management techniques” and “the relevant evidence base” to apply coverage limitations.10 The guidelines appear to presume insurer discretion to make a reasonableness determination.
Contraceptives: The women's services category includes the full range of U.S. Food and Drug Administration (FDA)-approved contraceptives.12 Regulations apply this coverage requirement while exempting houses of worship and creating accommodations for certain religiously affiliated nonprofit organizations.13 As of summer 2014, cases challenging the legality of the accommodation for religiously affiliated nonprofits—including Little Sisters of the Poor Home for the Aged v. Sebelius and Notre Dame v. Sebelius—were making their way through the lower courts.14,15 In June 2014, the Supreme Court decided that closely held for-profit corporations also cannot be required to provide comprehensive contraceptive coverage in violation of the religious beliefs of their owners.16
ACA preventive services in Medicare
Medicare contains a patchwork of preventive services coverage requirements. Although the ACA makes some changes, it does not significantly alter this patchwork.
The Medicare Improvements for Patients and Providers Act of 2008 authorizes the Centers for Medicare & Medicaid Services (CMS), which administers Medicare, to extend coverage to USPSTF-recommended services that are “reasonable and necessary” and “appropriate” for Medicare beneficiaries.17 The ACA retained this authority in CMS while further specifying that coverage of USPSTF-recommended services must be without cost sharing.18 At the same time, the ACA did not alter Medicare coverage requirements for vaccines: some vaccines are covered without cost sharing under Medicare Part B, while others are covered only through Part D and subject to Part D cost-sharing requirements.19
The ACA does not specifically require Medicare to cover the HRSA-recommended children's or women's preventive services, although both groups are found among the Medicare beneficiary population (in the case of children, those with end-stage renal disease). For women, current Medicare screening benefits offer some, but not complete, overlap.20 FDA-approved contraceptives that require a prescription presumably would be covered as a Part D service, but only for beneficiaries who purchase Part D.
Medicare also covers a one-time “Welcome to Medicare” visit that includes certain preventive screenings.21 The ACA added an “annual wellness visit” that includes establishment of a personalized screening schedule based on USPSTF and ACIP recommendations.22 Both the initial and annual visits are covered without cost sharing.23
ACA preventive services in Medicaid
Pre-ACA.
Medicaid's early and periodic screening, diagnostic, and treatment (EPSDT) benefit includes a full array of preventive services, generally without cost sharing, for all mandatory and most optional groups of infants, children, and adolescents younger than 21 years of age.24,25 In addition, all Medicaid beneficiaries of childbearing age are entitled to relatively comprehensive family planning services. But for other adult preventive services, coverage is optional for the program's traditional eligibility groups (i.e., pregnant women, caretaker relatives, and adults who receive Supplemental Security Income benefits). Studies suggest considerable variation across states.26,27
ACA changes.
The ACA changes this picture to a certain degree, while still leaving the potential for gaps.
Newly eligible adults and children: Newly eligible adults (i.e., all other nonelderly adults with family incomes ≤138% of the federal poverty level) are entitled to the same benefits extended to individuals who purchase insurance coverage in the individual and small group markets. Thus, their coverage includes all §2713 preventive benefits without cost sharing.28 In states that opt to extend eligibility to these adults, their coverage will include the full range of preventive benefits. The ACA also preserves EPSDT services for all children and adolescents up to 21 years of age.29
Adults eligible under traditional categories: Coverage of preventive services for “traditional” adults remains a state option.30 However, under the ACA, states that cover all USPSTF- and ACIP-recommended services and immunizations without cost sharing will receive a 1% increase in the Federal Medical Assistance Percentage (FMAP) for those services.31
ACA preventive services in CHIP
CHIP serves uninsured low- and moderate-income children up to 19 years of age who live in families with incomes that are too high for Medicaid.32 In states that run their CHIP programs as an extension of Medicaid (only seven states; Washington, DC; and five territories),32 CHIP must include EPSDT, generally without cost sharing. However, in most states, CHIP is run, at least in part, as a separate program, whose coverage rules are not as comprehensive as EPSDT.33 The ACA does not change these rules (Figure 2).
Figure 2.
Summary of required §2713a preventive services, by payer
aPHSA §2713, added by Pub. L. No. 111-148 §1001 (2010).
bExcluding grandfathered plans
USPSTF = U.S. Preventive Services Task Force
ACIP = Advisory Committee on Immunization Practices
HRSA = Health Resources and Services Administration
ACA = Affordable Care Act
FMAP = Federal Medical Assistance Percentage
EPSDT = early and periodic screening, diagnostic, and treatment
CHIP = Children's Health Insurance Program
ONGOING CHALLENGES
The new preventive services requirements have the potential to greatly improve health, but major challenges remain. An overarching problem is that, by statute, the preventive services requirement is limited to services endorsed by USPSTF, ACIP, or HRSA. Services with rapidly evolving evidence bases may not be reviewed and recommended in a timely manner, delaying their inclusion as part of the preventive coverage mandate. Other significant concerns vary by coverage type.
Operationalizing and enforcing the benefit in private employer-based, individual, and small group plans
For people with private coverage, the law on preventive services coverage is simple, but the details are not. For example, the exemption of grandfathered plans means that many people will continue to go without comprehensive preventive services coverage. Furthermore, rules for coverage and billing are complicated and could result in unexpected cost sharing, such as for office visits billed separately or for treatment resulting from a covered screening.
Oversight and enforcement are also a matter of concern. Like much of the ACA, enforcement of §2713 falls largely to state insurance commissioners. If a state informs the Secretary of the U.S. Department of Health and Human Services that it does not intend to enforce the law—as Alabama, Missouri, Oklahoma, Texas, and Wisconsin had as of January 201434—enforcement is a direct federal responsibility. It is unclear what, if any, systems states have in place to monitor if plans are meeting the preventive services requirements. Nor is the federal enforcement mechanism clear. Even if individuals are aware of the preventive services to which they are entitled, they may not know how to seek redress if their plans attempt to inappropriately restrict coverage.
Finally, the Supreme Court's decision on contraceptive coverage offered by “closely held” for-profit corporations may threaten access to comprehensive contraceptive coverage for women who work for any closely held for-profit corporation that decides to oppose coverage on religious grounds, and could open the door for analogous denials of other covered benefits by other for-profit corporations, even those that are not “closely held.”
Optimizing prevention in Medicare
In Medicare, preventive services coverage continues to have a number of weaknesses. One weakness is that coverage of USPSTF-recommended services remains at CMS's discretion; although CMS has added coverage for a number of USPSTF-recommended services, such as screening and counseling for sexually transmitted infections and intensive behavioral therapy for obesity,35,36 future additions could be subject to political or economic shifts in the prioritization of prevention.
Coverage of vaccines in Medicare remains problematic post-ACA, with only some vaccines (e.g., influenza, pneumococcal, and hepatitis B) routinely covered without cost sharing under Part B. Other vaccines are covered under the Part D drug benefit, but cost sharing can apply and may be considerable; for example, cost sharing under Part D for the shingles vaccine averaged $57 in 2009.19 Furthermore, not all Medicare beneficiaries have Part D coverage: in 2013, of 52 million Medicare beneficiaries, only 35.7 million had Part D coverage, and only some of the remainder had other sources of drug coverage (e.g., retiree plans), leaving an estimated 10% without coverage for most vaccines and other drugs.37
Another concern is that Medicare appears to be opting to cover certain preventive services only for limited providers in limited settings. For a number of preventive services added in recent years, such as the sexually transmitted infection screening and obesity services referenced previously, CMS has decided that Medicare will only reimburse primary care providers in primary care settings, despite broader underlying USPSTF recommendations that support other providers, other settings, or both.38,39 This trend seems to put in place an unnecessary barrier to preventive services.
Promoting the coverage of preventive services in Medicaid
ACA's preventive services provisions result in uneven coverage across Medicaid populations. In states that expand Medicaid, the newly eligible will have access to §2713 services without cost sharing. However, for low-income adults eligible prior to the expansion—including pregnant women and people with disabilities—states can decide which adult preventive services to cover and whether to require cost sharing.
CMS is working to encourage states to cover all USPSTF- and ACIP-recommended services for all Medicaid enrollees by promoting the 1% FMAP boost and highlighting other flexibilities.40 However, broad uptake has not yet occurred. The fact that nearly half the states have failed to expand their Medicaid programs further hinders access to preventive services for low-income people.41
For children in Medicaid, the EPSDT program theoretically includes all appropriate and medically necessary preventive services with little or no cost sharing and is broad enough to cover all §2713 services. However, in practice, many states do not routinely promote, or monitor uptake of, preventive services under EPSDT.42,43 In addition, as noted previously, CHIP programs operated separately from Medicaid are not required to cover EPSDT or §2713 services.
THE ROLE OF PUBLIC HEALTH
Despite these challenges, the ACA represents major progress for coverage of clinical preventive services, progress that public health professionals can help maximize through several key activities. First, the public health community should promote patient awareness of the preventive services available to them, especially vulnerable populations (e.g., the newly insured), who may lack an established source of medical care and advice. Second, public health stakeholders should work with providers to ensure that they understand the requirements and are promoting the use of appropriate preventive services among their patient populations. Third, state and local health departments are well situated to track the implementation of the preventive services requirements, and should develop ways to monitor progress and identify any unforeseen barriers that arise. Finally, public health officials and partners should educate policy makers on the importance of expanding access to preventive services, and encourage state Medicaid plans to include coverage of §2713 services without cost sharing for all enrollees. These activities will help ensure that ACA's preventive services provisions translate into meaningful uptake and improved health for all Americans.
REFERENCES
- 1. Pub. L. No. 111-148 (2010)
- 2. PHSA §2713, added by Pub. L. No. 111-148 §1001 (2010)
- 3.Bright Futures, American Academy of Pediatrics. Recommendations for preventive pediatric health care [cited 2014 Jun 24] Available from: URL: http://brightfutures.aap.org/clinical_practice.html.
- 4.Institute of Medicine. Washington: National Academies Press; 2011. Jul, Clinical preventive services for women: closing the gaps. [Google Scholar]
- 5.Health Resources and Services Administration (US) Women's preventive services guidelines [cited 2014 Jun 24] Available from: URL: http://www.hrsa.gov/womensguidelines.
- 6.Robert Wood Johnson Foundation. Number of Americans obtaining health insurance through an employer declines steadily since 2000. Princeton (NJ): RWJF; 2013. Apr 11, Also available from: URL: http://www.rwjf.org/en/about-rwjf/newsroom/newsroom-content/2013/04/number-of-americans-obtaining-health-insurance-through-an-employ.html [cited 2014 Jun 24] [Google Scholar]
- 7. Pub. L. No. 111-148 §1563(e) (2010)
- 8. Pub. L. No. 111-148 §1251 (2010)
- 9.Henry J Kaiser Family Foundation. 2013 employer health benefits survey. 2013. [cited 2014 Jun 24]. Available from: URL: http://kff.org/private-insurance/report/2013-employer-health-benefits.
- 10.Department of the Treasury, Department of Labor, Department of Health and Human Services (US) Interim final rules for group health plans and health insurance issuers relating to coverage of preventive services under the Patient Protection and Affordable Care Act. Fed Reg. 2010;75:41726–60. Also available from: URL: https://webapps.dol.gov/FederalRegister/HtmlDisplay.aspx?DocId=24044&AgencyId=8&DocumentType=2 [cited 2014 Jun 24] [PubMed] [Google Scholar]
- 11.Department of Labor (US) FAQs about Affordable Care Act implementation part XII. 2013. Feb 20, [cited 2014 Jun 24]. Available from: URL: http://www.dol.gov/ebsa/faqs/faq-aca12.html.
- 12.Department of Health and Human Services (US) Coverage of certain preventive services under the Affordable Care Act; final rules. Fed Reg. 2014;78:39870–99. Also available from: URL: http://www.gpo.gov/fdsys/pkg/FR-2013-07-02/pdf/2013-15866.pdf [cited 2014 Jul 1] [Google Scholar]
- 13. Conestoga Wood Specialties Corp. v. Sebelius, 724 F. 3d 377 (3rd. Cir. 2013)
- 14. Little Sisters of the Poor Home for the Aged v. Sebelius. D.C. No. 1:13-CV-02611-WJM-BNB (2013)
- 15. University of Notre Dame v. Sebelius. 743 F. 3d 547 (2014)
- 16. Burwell v. Hobby Lobby Stores, Inc. 573 U.S. (2014)
- 17. 42 USC §1395x(ddd)(1)
- 18. Pub. L. No. 111-148, §4104 (2010)
- 19.Government Accountability Office (US) Medicare: many factors, including administrative challenges, affect access to Part D vaccinations. 2011 [cited 2014 Jun 24] Available from: URL: http://www.gao.gov/products/GAO-12-61.
- 20.Centers for Medicare & Medicaid Services (US) Your Medicare coverage: preventive and screening services [cited 2014 Jun 24] Available from: URL: https://www.medicare.gov/coverage/preventive-and-screening-services.html.
- 21.Centers for Medicare & Medicaid Services (US) Your “Welcome to Medicare” preventive visit [cited 2014 Jun 24] Available from: URL: http://www.medicare.gov/people-like-me/new-to-medicare/welcome-to-medicare-visit.html.
- 22. Pub. L. No. 111-148, §4103 (2010)
- 23.Centers for Medicare & Medicaid Services (US) Your Medicare coverage: preventive visit and yearly wellness exams [cited 2014 Jun 24] Available from: URL: http://www.medicare.gov/coverage/preventive-visit-and-yearly-wellness-exams.html.
- 24. 42 U.S.C. §1396d(a)(4)(B)
- 25. 42 U.S.C. §1396d(r)(5)
- 26.Wilensky SE, Gray EA. Existing Medicaid beneficiaries left off the Affordable Care Act's prevention bandwagon. Health Aff (Millwood) 2013;32:1188–95. doi: 10.1377/hlthaff.2013.0224. [DOI] [PubMed] [Google Scholar]
- 27.Kaiser Commission on Medicaid and the Uninsured. Coverage of preventive services for adults in Medicaid. 2012. [cited 2014 Jun 24]. Available from: URL: http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8359.pdf.
- 28. Pub. L. No. 111-148 §2001 (2010)
- 29.Department of Health and Human Services (US) Medicaid and Children's Health Insurance Programs: essential health benefits in alternative benefit plans, eligibility notices, fair hearing and appeal processes, and premiums and cost sharing; exchanges: eligibility and enrollment. Fed Reg. 2013;78:42159. [PubMed] [Google Scholar]
- 30. 42 C.F.R. §440.225.
- 31. Pub. L. No. 111-148 §4106 (2010)
- 32.Centers for Medicare & Medicaid Services (US) Children's Health Insurance Program (CHIP) [cited 2014 May 7] Available from: URL: http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Childrens-Health-Insurance-Program-CHIP/Childrens-Health-Insurance-Program-CHIP.html.
- 33.Centers for Medicare & Medicaid Services (US) CHIP cost sharing [cited 2014 May 7] Available from: URL: http://medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Childrens-Health-Insurance-Program-CHIP/CHIP-Cost-Sharing.html.
- 34.Centers for Medicare & Medicaid Services (US) The Center for Consumer Information & Insurance Oversight: compliance [cited 2014 Jun 24] Available from: URL: http://www.cms.gov/CCIIO/Programs-and-Initiatives/Health-Insurance-Market-Reforms/compliance.html.
- 35.Centers for Medicare & Medicaid Services (US) Screening for sexually transmitted infections (STIs) and high intensity behavioral counseling (HIBC) to prevent STIs. 2012. May 23, [cited 2014 Jun 24]. Available from: URL: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM7610.pdf.
- 36.Centers for Medicare & Medicaid Services (US) Intensive behavioral therapy (IBT) for obesity. 2014. [cited 2014 Jun 24]. Available from: URL: http://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/icn907800.pdf.
- 37.Henry J Kaiser Family Foundation. The Medicare prescription drug benefit fact sheet. 2013. [cited 2014 Jun 24]. Available from: URL: http://kff.org/medicare/fact-sheet/the-medicare-prescription-drug-benefit-fact-sheet.
- 38.Centers for Medicare & Medicaid Services (US) National coverage determination (NCD) for screening for sexually transmitted infections (STIs) and high-intensity behavioral counseling (HIBC) to prevent STIs (210.10) 2011. [cited 2014 Jun 24]. Available from: URL: http://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=352&ncdver=1&bc=AAAAgAAAAAAAAA%3d%3d&#Top.
- 39.Centers for Medicare & Medicaid Services (US) National coverage determination (NCD) for intensive behavioral therapy for obesity (210.12) 2011. [cited 2014 Jun 24]. Available from: URL: http://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=353&ncdver=1&CoverageSelection=Both&ArticleType=All&PolicyType=Final&s=All&KeyWord=obesity&KeyWordLookUp=Title&KeyWordSearchType=And&bc=gAAAABAAAAAAAA%3d%3d&. [PubMed]
- 40.Centers for Medicare & Medicaid Services (US), Center for Medicaid and CHIP Services. Letter re: Affordable Care Act Section 4106 (preventive services) 2013. Feb 1, [cited 2014 Jun 24]. Available from: URL: http://www.medicaid.gov/Federal-Policy-Guidance/downloads/SMD-13-002.pdf.
- 41.Henry J. Kaiser Family Foundation. Status of state action on the Medicaid Expansion decision, 2014 [cited 2014 Jun 24] Available from: URL: http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act.
- 42.Government Accountability Office (US) Medicaid preventive services: concerted efforts needed to ensure beneficiaries receive services. Report to the Chairman, Committee on Finance, U.S. Senate; GAO-09-578. August 2009 [cited 2014 Jun 24]. Available from: URL: http://www.gao.gov/new.items/d09578.pdf. [Google Scholar]
- 43.Rosenbaum S, Wilensky S, Allen K. EPSDT at forty: modernizing a pediatric health policy to reflect a changing health care system. Hamilton (NJ): Center for Health Care Strategies, Inc.; 2008. [Google Scholar]