Abstract
Objectives
Studies have shown that differences among individuals and social groups in accessing and using information on health and specific threats have an impact on their knowledge and behaviors. These differences, characterized as communication inequalities, may hamper the strength of a society's response to a public health emergency. Such inequalities not only make vulnerable populations subject to a disproportionate burden of adversity, but also compromise the public health system's efforts to prevent and respond to pandemic influenza outbreaks. We investigated the effect of socioeconomic status (SES) and health communication behaviors (including barriers) on people's knowledge and misconceptions about pandemic influenza A(H1N1) (pH1N1) and adoption of prevention behaviors.
Methods
The data for this study came from a survey of 1,569 respondents drawn from a nationally representative sample of American adults during pH1N1. We conducted logistic regression analyses when appropriate.
Results
We found that (1) SES has a significant association with barriers to information access and processing, levels of pH1N1-related knowledge, and misconceptions; (2) levels of pH1N1-related knowledge are associated positively with the adoption of recommended prevention measures and negatively with the adoption of incorrect protective behaviors; and (3) people with higher SES, higher news exposure, and higher levels of pH1N1-related knowledge, as well as those who actively seek information, are less likely than their counterparts to adopt incorrect prevention behaviors.
Conclusion
Strategic public health communication efforts in public health preparedness and during emergencies should take into account potential communication inequalities and develop campaigns that reach across different social groups.
2009–2010 pandemic influenza A(H1N1) (pH1N1), a highly transmittable form of virus that initially appeared deadly, was seen to perfectly fit the disease profile of a lethal pandemic influenza anticipated to affect human health on a scale similar to the 1918 flu. As such, it attracted global attention and caused worldwide fear. During the early stages, when little was known about the disease severity or transmission mode, the novel pH1N1 virus received extensive coverage in the media and raised public concerns. One month after the first case, the World Health Organization (WHO) raised the influenza pandemic alert level to “Phase 5” on April 29, 2009, and only six weeks later to “Phase 6,” the highest level. As of June 10, 2009, 27,737 confirmed cases of pH1N1 infection were reported in 74 countries.1,2 Faced with a pandemic with possible high mortality, public officials identified mass media channels such as television, radio, and newspaper to promote public awareness, increase public knowledge, and cue the public to adopt protective behaviors. Studies have shown that routine exposure and strategic use of mass media can effectively provide public health information.3–6 However, all individuals and social groups do not have the same access to this information.7,8 Communication inequalities, defined as the differences in exposure to public health communication messages and capacity to access, process, and act upon the information received, are influenced by social determinants3,9–14 and may result in disparities in health-related knowledge, behavior choices, and, ultimately, health outcomes.10,12,15–23
pH1N1 offered an opportunity to assess the influence of communication inequalities on people's knowledge about a public health threat and their subsequent compliance to recommended behaviors during a public health emergency. Level of knowledge was positively associated with socioeconomic status (SES) and was a strong predictor of adopting prevention practices.6,14,16–24 Researchers also found that adopting prevention measures was strongly associated with sociodemographic factors and health communication behaviors, such as information seeking, news exposure, and perceived trust in the information sources.6,15–23,25,26 During the course of pH1N1, public health communication campaigns about social distancing and hand hygiene were effective, prompting the public to curtail hand-shaking and hugging at social gatherings and adopt regular hand washing or use of hand sanitizers.27–39 Yet, misconceptions also tend to arise in times of uncertainty, plausibly leading to adopting ineffective practices and jeopardizing efforts to contain the disease. pH1N1 was originally referred to by health officials and the WHO as “swine flu,” causing worldwide confusion regarding the danger posed by pigs39–42 and influencing incorrect prevention measures such as avoiding pork43,44 despite repeated efforts to counter the inaccurate information.
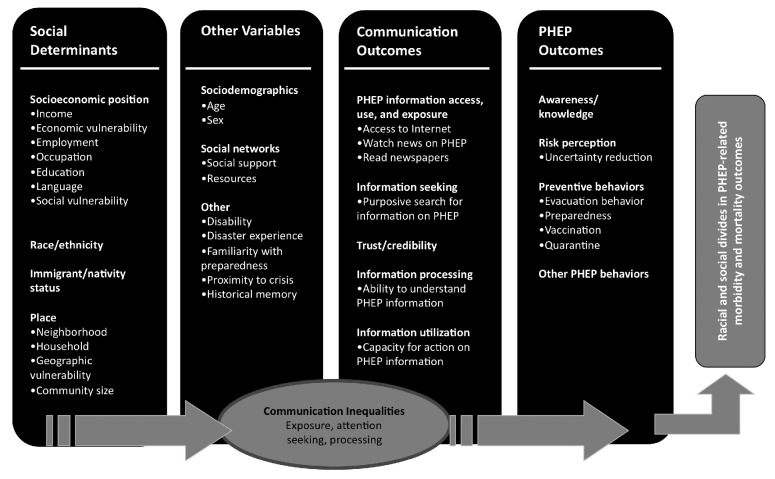
Nevertheless, few studies have investigated the role communication inequalities play in people's knowledge and misconceptions about a perceived threat and in subsequent behavioral compliances. According to the structural influence model (SIM) of communication in public health,8 health communication behaviors can be a pathway linking individual and social determinants (e.g., race/ethnicity and SES) with health outcomes (Figure). SIM posits that public communications can influence health by raising awareness, providing information, and reinforcing knowledge and behaviors; however, communication inequalities can affect people's attention to, processing of, and acting upon health information and the consequential behavioral outcomes, thereby exacerbating disparities among social groups.4,7,11,24,45,46 We used SIM to guide the investigation on the role of communication inequalities in public health emergencies.
Figure.
Structural influence model of communication inequalitiesa
aJung M, Lin L, Viswanath K. Associations between health communication behaviors, neighborhood social capital, vaccine knowledge, and parents' H1N1 vaccination of their children. Vaccine 2013;31:4860-6.
PHEP = public health emergency preparedness
METHODS
Survey instrument
We constructed a survey instrument from December 2009 through January 2010 to investigate the U.S. population's levels of pH1N1-related knowledge, communication, and preparedness behaviors. Prior to developing the survey, we conducted five focus groups with participants from diverse racial/ethnic and socioeconomic backgrounds in Massachusetts. We conducted cognitive testing with potential participants before finalizing the survey.
Sample
The data for this study came from a survey of 1,569 respondents drawn from a nationally representative sample of U.S. adults aged 18 years and older, collected from late February to early March 2010. Respondents participated in Knowledge Networks' KnowledgePanel® and were recruited using a dual sampling frame, a combination of random-digit-dial and address-based sampling, allowing for sampling of individuals with no telephone landlines. Households were provided with Internet access and necessary hardware if needed. We used post-stratification weights to adjust for non-coverage and nonresponder bias. Demographic and geographic distributions for the population aged 18 years and older from the most recent Current Population Survey47 and the 2006 Pew Hispanic Center Survey of Latinos48 were used as benchmarks in this adjustment. Post-stratification weighting included gender, age, race/ethnicity, education, census region, urbanicity, Internet access, and dominant language.49,50 For the purpose of this study, participants from minority racial/ethnic groups and those living below the federal poverty level were oversampled. The response rate was 66.3%.
Dependent variables
We created the following dependent variables as measurements of communication inequalities:
- Assessments of knowledge: To determine respondents' levels of knowledge and misconceptions about pH1N1 transmission, we asked them, “To the best of your knowledge, how can someone get H1N1?” Possible answers included, “From being in close contact with someone who has pH1N1 (within arms-length of someone),” “From touching objects (e.g., glass) recently touched by someone with flu,” “From eating pork,” “From coming in contact with pigs,” and “None of the above.” Adapting from the knowledge scores developed by Savoia et al. in 2010,26,51 we constructed two knowledge assessment scores:
- Knowledge score: Respondents obtained a score of 0, 1, or 2: one point for checking each of the following correct options: “close contact” and “touching objects,” and one point if none of the following were checked: “eating pork,” “coming in contact with pigs,” or “none of the above.”
- Misconceptions score: Respondents obtained one point for checking each of the following: “eating pork” or “coming in contact with pigs.”
- Behavioral compliances were determined based on participants' self-report on whether or not they had changed their health behaviors and adopted precautionary measures in response to news reports of pH1N1. We assessed precautionary measures recommended by the U.S. Centers for Disease Control and Prevention (CDC) as outcome variables in the final models.
- Recommended prevention behaviors:
- Those who “reduced human contact with people outside of [their] immediate -family, such as signs of affection (hug/kiss), shaking hands, or sign of peace during worship”;
- Those who “washed [their] hands or used hand sanitizer more frequently”;
- Wrong prevention behavior: those who “avoided eating pork products.”
The aforementioned variables were dichotomously coded as “1” for items that were checked and “0” for items that were not checked.
Independent variables
We included two sets of independent variables on the basis of substantive and theoretical relevance in accordance with the SIM:7
SES, measured by education and annual household income (Table 1); and
- pH1N1-related health communication behaviors, measured by the following variables adapted from the National Cancer Institute Health Information National Trends Survey:52–54
- Information-seeking behaviors, capturing individuals' purposive rather than incidental interaction with pH1N1-related information, were measured with the question, “Have you actively searched for information about H1N1?” (“yes” = seekers, “no” = non-seekers).
- Source of pH1N1 information was reported, where participants “had received the most information about the pH1N1 outbreak.”
- We measured trust in information source by a factual statement that participants answered with “yes” or “no:” “You trust information from the source [you have received the most pH1N1 information from].”
- Communication barriers experienced during the pH1N1 pandemic were measured by (1) amount of information provided: participants were asked about “the [perceived] amount of information the media have provided on H1N1,” with possible answers including “too much information,” “not enough information,” “just the right amount of information,” and “don't know”; (2) difficulty in understanding the information delivered: participants responded to the question about “difficulty [experienced] in understanding the pH1N1 information that the media delivered” on a 10-point scale (0 = very hard to understand, 10 = very easy to understand); and (3) accessibility: “You can get the information you want from the source [you have received the most pH1N1 information from] immediately” (“yes” or “no”).
- General news exposure: Respondents were asked how many out of the past seven days they had read newspapers, watched national and local news on television, and read news on the Internet. We calculated an average exposure of news during the past seven days based on the responses.
- To determine knowledge's impact on behaviors, we calculated knowledge assessment scores as predictors in the models assessing the behaviors.
Table 1.
Socioeconomic status and demographic characteristics of a nationally regpresentative sample of 1,569 U.S. adults aged 18 years and older during 2009–2010 pH1N1a
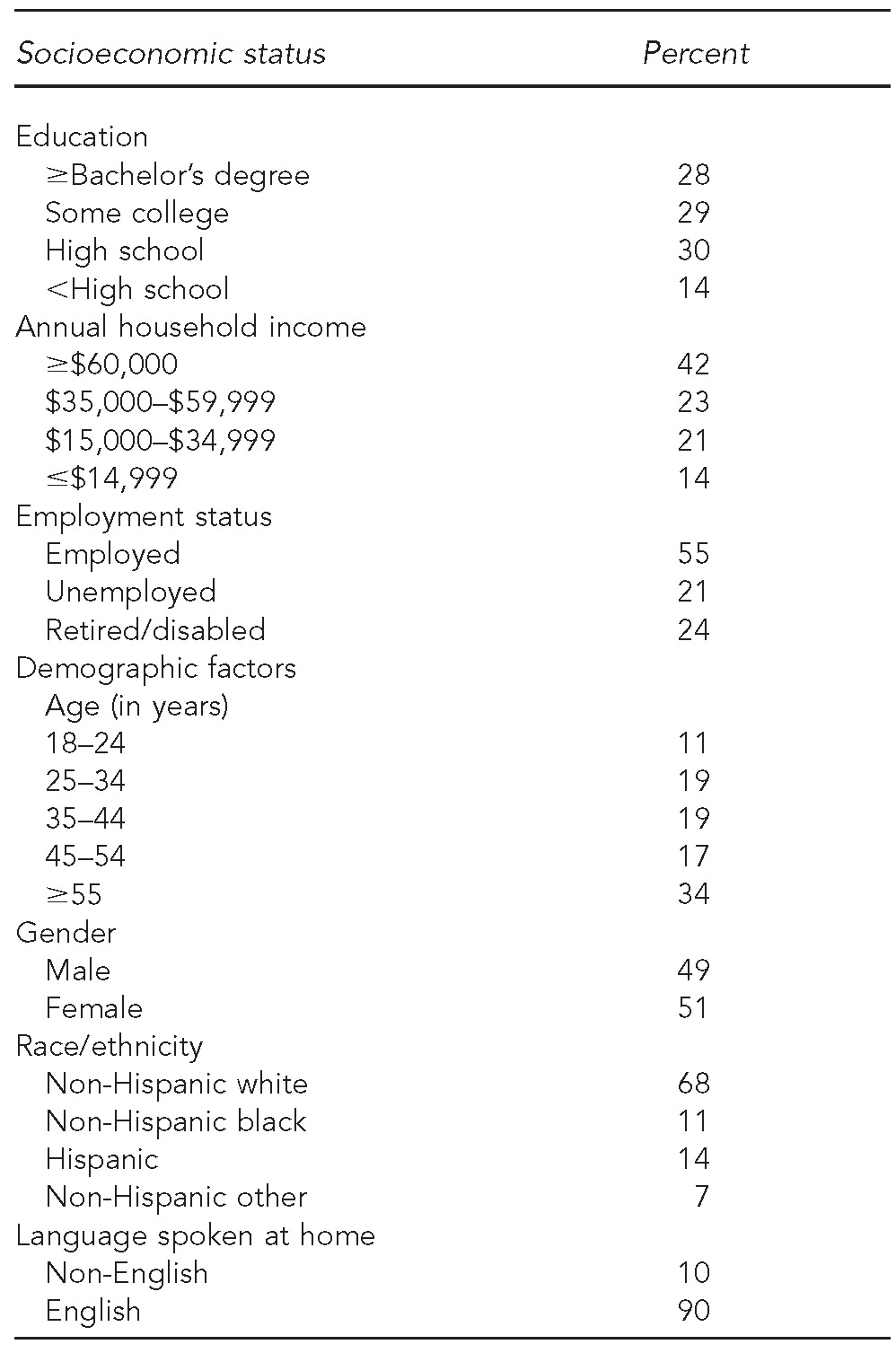
Data source: Harvard School of Public Health Preparedness and Emergency Response Learning Center LAMPS project, 2009 H1N1 and General Emergency Preparedness Communications Survey.
pH1N1 = pandemic influenza A(H1N1)
Potential confounders
According to SIM, the sociodemographic factors potentially influential in determining communication inequalities—age, sex, race/ethnicity, employment status, and language spoken at home—were controlled.
Analysis
We performed descriptive analyses, expressed as weighted frequencies and percentages, to account for the complex sampling design and to allow estimates to be nationally representative. We applied binary ordered logistic regression (knowledge models) and logistic regression (misconceptions models) to test for significant bivariate associations between each predictor and the outcome variables. Based on the results and SIM, we first conducted hierarchical multivariate logistic regression analyses and tested knowledge/misconception as major outcomes of interest and SES variables as major independent variables (tier-1). We then added mediating health communication variables such as general news exposure, information seeking, or barriers to access or use information (tier-2). Finally, knowledge was added as a third-tier variable (tier-3) to the behavioral compliances models, where adoption of recommended prevention behaviors (e.g., social distance [Models 5–7] and hand hygiene [Models 8–10]) and incorrect prevention behaviors (pork avoidance) were used as outcome variables. Using cross-tabulations, chi-square, and t-test, we examined the associations between identified significant social determinants and information sources. We conducted all analyses using Stata® version 11.0.55 We used the survey weight-related svy command or svy option when appropriate.
RESULTS
Sample demographics
Demographic data are shown in Table 1. About half (49%) of the weighted sample population was ≤44 years of age, 44% had ≤high school education, and 14% had an annual income of <$15,000. Sixty-eight percent were non-Hispanic white, 11% were non-Hispanic black, 14% were Hispanic, and 7% were of another race/ethnicity.
Sources of pH1N1 information
Most people received information through local television news (35%), national network news (23%), the Internet (11%), or a doctor, nurse, or other medical professional (11%). Sources such as cable network television news stations, non-English-speaking television stations, national newspapers, social media, and non-English newspapers were used by ≤5% of the sample population. People with ≤high school education relied more on local television news and national network news and less on local newspapers and the Internet. Surprisingly, for information exchange related to pH1N1, social media usage was very low. Of the 45% of participants who self-reported owning at least one social media account, only 4% used these sites to receive or share information about pH1N1 (data not shown).
Information seeking and barriers to access and process information
Only 15% of the population actively searched for information about pH1N1, of which two-thirds had at least some college education. Almost 60% of the participants reported trusting the source from which they received the most pH1N1 information, while about 40% of the respondents remained skeptical about the information they received. Only 23% reported that they were able to access information they wanted immediately. When asked to assess the amount of information provided by the media on pH1N1, 47% of the respondents, usually those with a higher income, thought the media had provided just the right amount of information (Table 2).
Table 2.
Logistic regression examining the association among SES, knowledge and misconception about pH1N1 virus transmission, and health communication behaviors in a nationally representative sample of adults aged 18 years and older during 2009–2010 pH1N1a
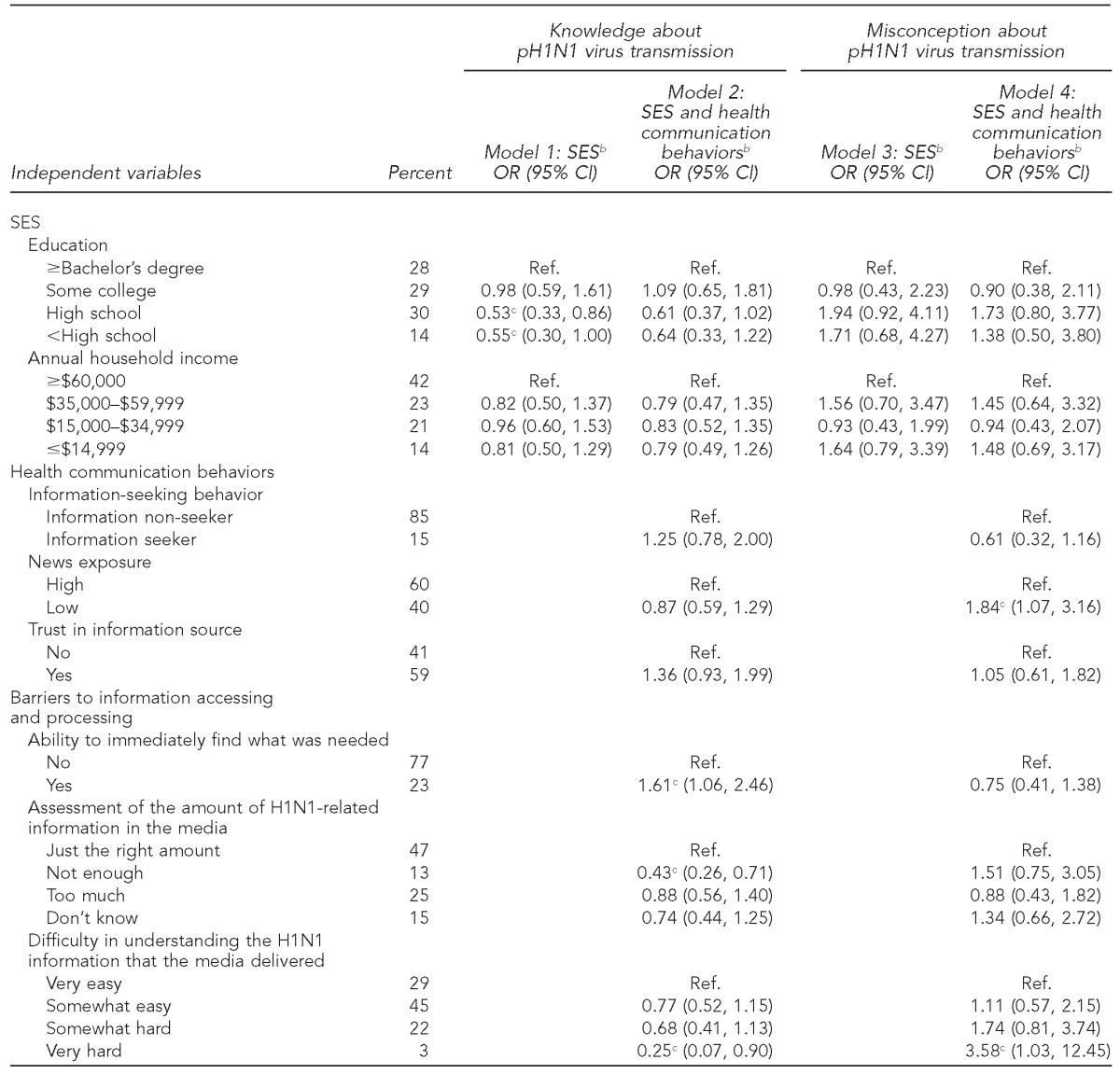
Data source: Harvard School of Public Health Preparedness and Emergency Response Learning Center LAMPS project, 2009 H1N1 and General Emergency Preparedness Communications Survey.
bAll models are adjusted for age, sex, race/ethnicity, employment status, and language spoken at home.
cStatistically significant at p<0.05
SES = socioeconomic status
pH1N1 = pandemic influenza A(H1N1)
OR = odds ratio
CI = confidence interval
Ref. = reference group
Knowledge and misconceptions
Table 2 shows the results of two-tiered multivariate logistic models for knowledge (Models 1–2) and misconceptions (Models 3–4) about pH1N1 virus transmission. The majority of the participants (88%) knew at least one of the two correct mechanisms of pH1N1 virus transmission; however, at least 12% of the participants had misconceptions about transmission and thought pH1N1 could be transmitted via pork consumption and/or contact with pigs. Models 1 and 2 showed those with <high school education had significantly less knowledge about pH1N1, but this finding became insignificant once health communication behaviors were considered. Three types of communication barriers were identified to be significantly associated with lower levels of knowledge: (1) inability to immediately find what was needed from the information source, (2) a perceived shortage of sufficient pH1N1-related information in the media, and (3) difficulty in understanding the pH1N1 information that the media delivered. Difficulty in understanding the pH1N1 information and lower general news exposure were also important predictors of misconceptions (Model 4).
Determinants of behavioral compliance
By expanding the aforementioned models, we examined an integrated model with behavior compliances as the outcome variables of interest (Tables 3–5). We found that health communication behaviors played a more significant role in the adoption of recommended behaviors than SES (Tables 3 and 4). In the social distancing models (Table 3, Model 7), participants with a knowledge score of 1 or 2 were 3.47 and 4.55 times, respectively, more likely than their counterparts to adopt recommended prevention measures, and their likelihood of adopting wrong prevention measures was greatly reduced (by 62% and 77%, respectively) (Table 5, Model 13). Those who experienced fewer communication barriers and had higher levels of knowledge were more likely to exercise hand hygiene and social distancing (Tables 3 and 4, Models 7 and 10). At the time of the survey, 5% of respondents still followed incorrect prevention measures and avoided pork products. Levels of knowledge functioned as a key and moderating determinant in increasing the adoption of recommended prevention measures and reducing the adoption of incorrect measures (Tables 3–5, Models 7, 10, and 13). The pork avoidance models (Table 5) showed that information seekers, people with higher SES, and those with high media exposure were less likely to adopt incorrect prevention behaviors than information non-seekers, those with lower SES, and those with low media exposure. Individuals who were able to find the information they wanted immediately were more likely to adopt behavior changes, correct or incorrect, than those who could not immediately find the information they wanted.
Table 3.
Logistic regression examining the association among social distancing behaviors against pH1N1 virus, SES, and health communication behaviors as well as pH1N1-related knowledge in a nationally representative sample of adults aged 18 years and older during 2009–2010 pH1N1a
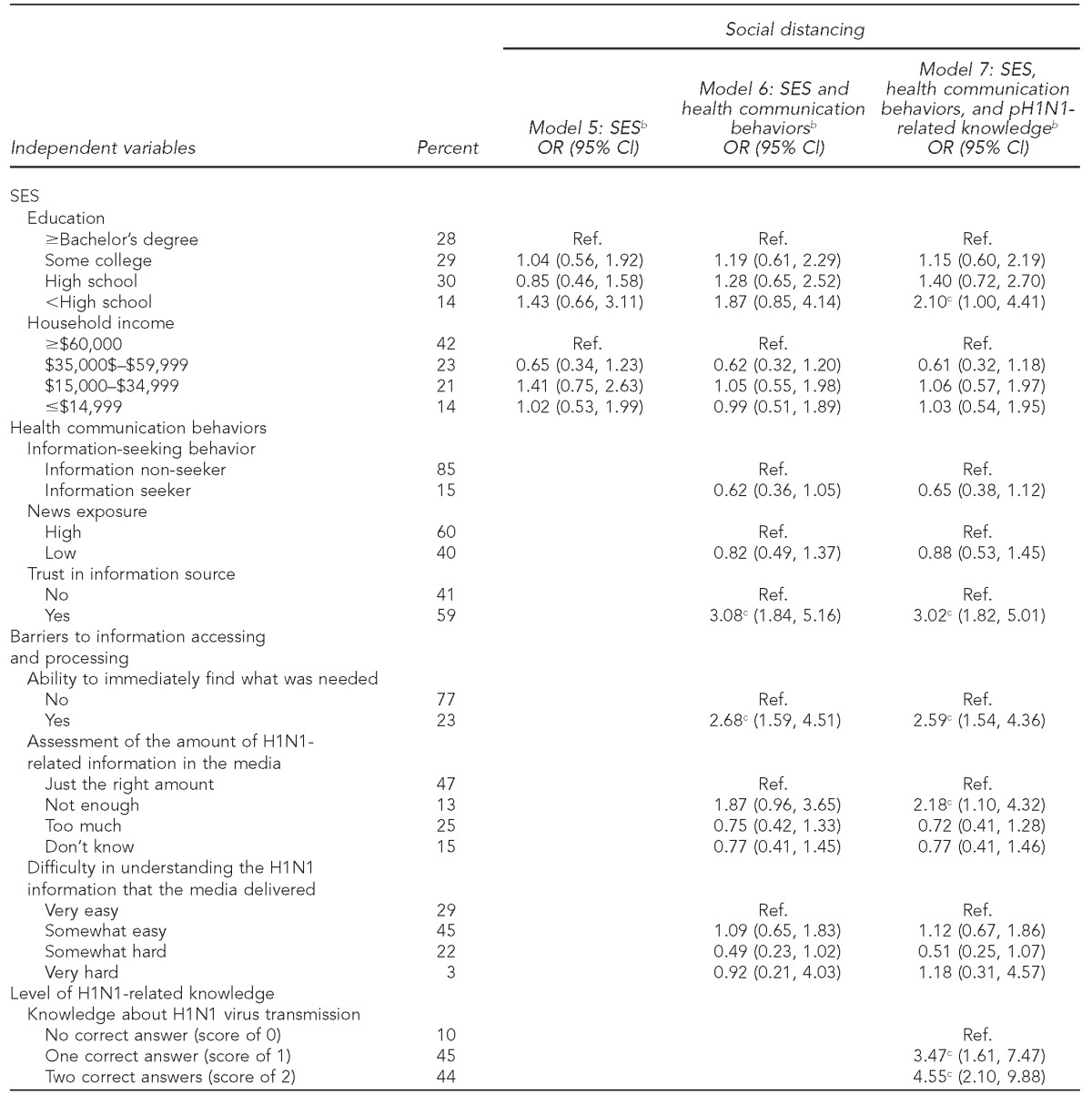
Data source: Harvard School of Public Health Preparedness and Emergency Response Learning Center LAMPS project, 2009 H1N1 and General Emergency Preparedness Communications Survey.
bAll models are adjusted for age, sex, race/ethnicity, employment status, and language spoken at home.
cStatistically significant at p<0.05
pH1N1 = pandemic influenza A(H1N1)
SES = socioeconomic status
OR = odds ratio
CI = confidence interval
Ref. = reference group
Table 4.
Logistic regression examining the association among hand hygiene practices against pH1N1 virus, SES, and health communication behaviors as well as pH1N1-related knowledge in a nationally representative sample of adults aged 18 years and older during 2009–2010 pH1N1a
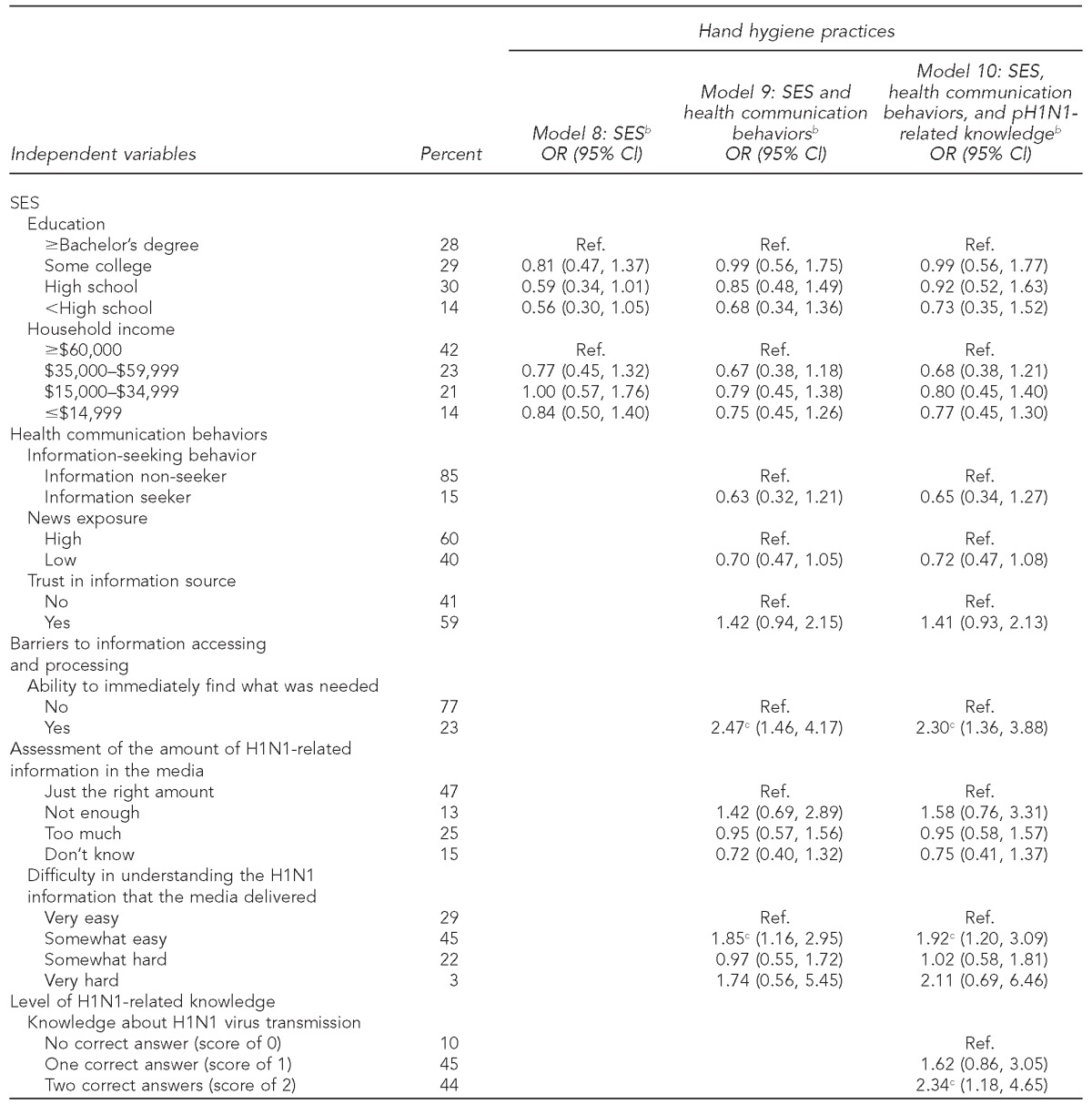
Data source: Harvard School of Public Health Preparedness and Emergency Response Learning Center LAMPS project, 2009 H1N1 and General Emergency Preparedness Communications Survey.
bAll models are adjusted for age, sex, race/ethnicity, employment status, and language spoken at home.
cStatistically significant at p<0.05
pH1N1 = pandemic influenza A(H1N1)
SES = socioeconomic status
OR = odds ratio
CI = confidence interval
Ref. = reference group
Table 5.
Logistic regression examining the association among pork avoidance behaviors against pH1N1 virus, SES, and health communication behaviors as well as pH1N1-related knowledge in a nationally representative sample of adults aged 18 years and older during 2009–2010 pH1N1a
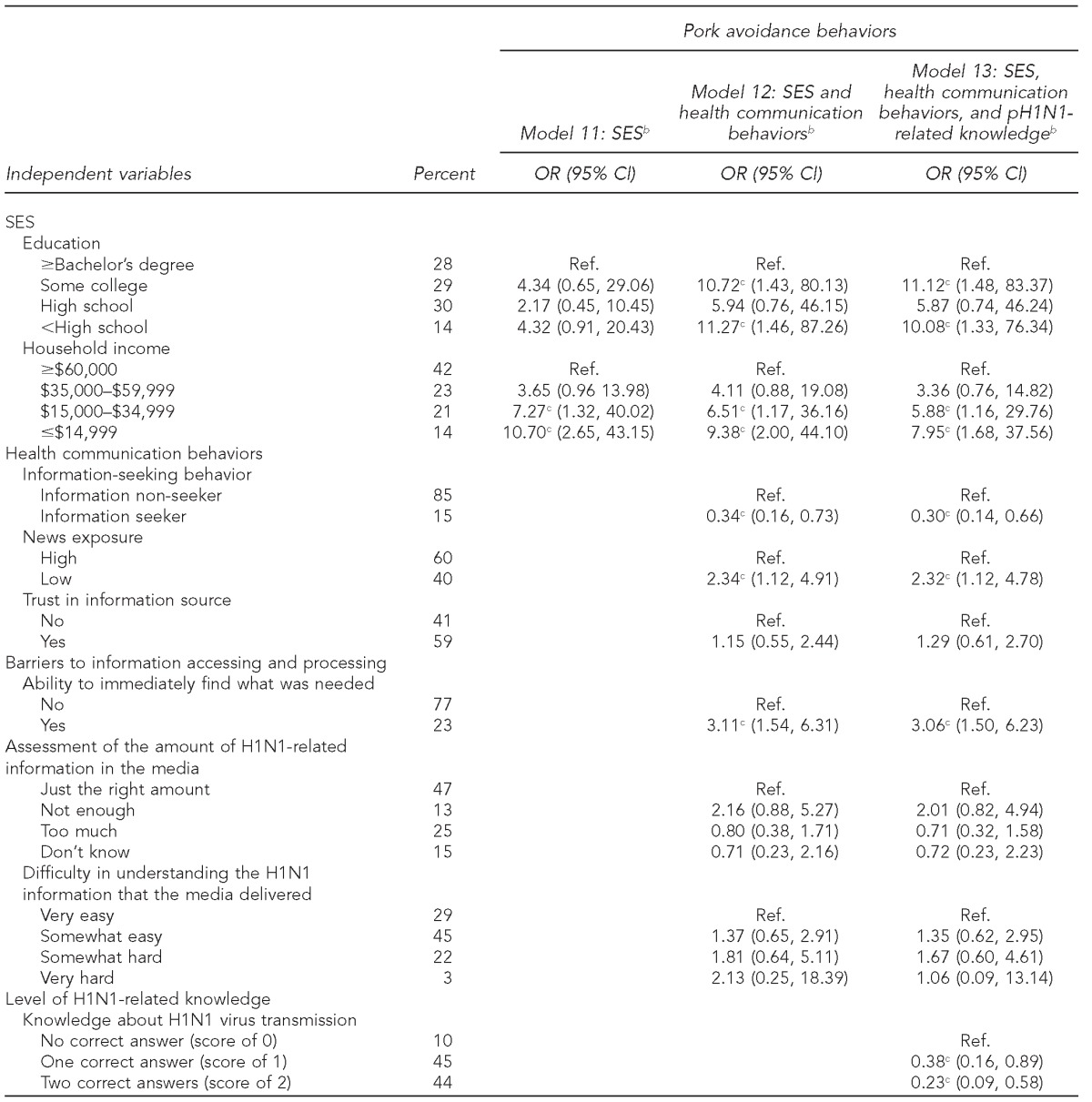
Data source: Harvard School of Public Health Preparedness and Emergency Response Learning Center LAMPS project, 2009 H1N1 and General Emergency Preparedness Communications Survey.
bAll models are adjusted for age, sex, race/ethnicity, employment status, and language spoken at home.
cStatistically significant at p<0.05
pH1N1 = pandemic influenza A(H1N1)
SES = socioeconomic status
OR = odds ratio
CI = confidence interval
Ref. = reference group
DISCUSSION
We used SIM as a guide to investigate a range of structural and communication-based factors that may impact knowledge and behaviors during a public health emergency. Misconceptions arise when public health messages are unclear or when critical information is delayed in reaching the intended recipients due to limited media exposure or information seeking. Our data showed that these communication inequalities disproportionately affected individuals with lower SES who retained incorrect information even after public officials' repeated efforts to correct misperceptions. Because those with exposure to information compared with non-exposed people were more likely to perform related behaviors, health information must be closely customized to the target audience to prevent potentially detrimental behaviors. Furthermore, respondents who reported that they received just the right amount of information about the virus responded to the threat more often than individuals who felt they received too much or too little information. Given that 25% of the sample reported hearing too much information, it could indicate possible burnout or desensitization from over-sensationalized accounts in the media. A communications campaign designed to motivate information seeking, increase news exposure, and reduce barriers to accessing and processing information can improve the public's ability to prepare for and respond to a health threat. In fact, strategies that aim to promote efficacy in prevention behaviors could help motivate people to seek out more information. These strategies should take into consideration the sociodemographic characteristics of the target audience in determining format and channel of delivery, providing important information about the threat and actionable prevention tactics via designated websites and telephone hotlines, as swiftly as possible.
Low seeking rates also mean that it is important to effectively and promptly use the media outlets people are routinely exposed to most often to provide knowledge and preventive behaviors at proper health literacy levels after a pandemic begins, particularly as this outlet seems to be the way many low SES non-seekers received the threat-related information. Such information could come from CDC or another trusted source and be disseminated through a variety of channels (e.g., media as well as community centers). Future studies are warranted to explore the additional challenges to designing prevention campaigns so that they may be intercepted and acted upon equally by all SES groups. These social inequalities manifested in people's behavioral response in a time of crisis may be particularly salient in regard to social distancing behaviors, as factors such as flexible work hours and occupation type may determine the ability to comply with this action. Therefore, public officials need to coordinate with workplaces, labor departments, and community groups so that at a structural level, people will be given more flexible hours to stay home when needed.
Limitations
Our cross-sectional study design limited us from drawing a causal relationship among social determinants, health communication behaviors, and preparedness outcomes. We were also limited by self-reported data; however, our survey items were adopted from widely tested national surveys52–54 and validated by cognitive testing. Longitudinal studies, systems science methodologies, or experiments are required to provide stronger evidence for such relationships. Also, this study was conducted a few months after the beginning of pH1N1. Because individuals may have been more affected by their social conditions early on during an emergency when information was unavailable or unclear, this time difference between the beginning of the pandemic and when the survey was conducted may have greatly decreased the effect of the social disparities detected. Therefore, a tool to rapidly develop surveys as an emergency unfolds is needed to capture timely information and assess information needs in future public health emergencies.
CONCLUSIONS
Communication inequalities could compromise public health systems' ability to effectively prevent and respond to pandemic influenza outbreaks. Low SES, communication barriers, and low levels of pH1N1-related knowledge are significantly associated with misconceptions and uptake of incorrect precautionary behaviors, which are difficult to reverse. Traditional forms of mass media and communications through pre-established social networks remain the primary information sources and channels for public health messages. Providing information about recommended prevention measures in a way that is immediately accessible and understandable to the public can increase the public's level of knowledge about the pandemic, promote the uptake of effective precautionary behaviors, and reduce ineffective prevention behaviors.
Footnotes
Institutional Review Board approval was obtained from the Harvard School of Public Health. The authors acknowledge funding support from the Centers for Disease Control and Prevention (CDC) grant #5PO1TP000307-05. The content of this publication as well as the views expressed in this article are solely those of the authors and do not necessarily represent the views of CDC.
REFERENCES
- 1.Chan M. Geneva: World Health Organization; 2009. Statement to the press: world now at the start of 2009 influenza pandemic. [Google Scholar]
- 2.World Health Organization. Influenza A(H1N1)—update 46. 2009. [cited 2012 Nov 5]. Available from: URL: http://www.who.int/csr/don/2009_06_10a/en.
- 3.Tafawa AO, Viswanath K, Kawachi I, Williams DR. Mass media exposure, social stratification, and tobacco consumption among Nigerian adults. Cancer Causes Control. 2012;23(Suppl 1):45–55. doi: 10.1007/s10552-012-9898-9. [DOI] [PubMed] [Google Scholar]
- 4.Ishikawa Y, Nishiuchi H, Hayashi H, Viswanath K. Socioeconomic status and health communication inequalities in Japan: a nationwide cross-sectional survey. PLoS One. 2012;7:e40664. doi: 10.1371/journal.pone.0040664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clayman ML, Manganello JA, Viswanath K, Hesse BW, Arora NK. Providing health messages to Hispanics/Latinos: understanding the importance of language, trust in health information sources, and media use. J Health Commun. 2010;15(Suppl 3):252–63. doi: 10.1080/10810730.2010.522697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jung M, Lin L, Viswanath K. Associations between health communication behaviors, neighborhood social capital, vaccine knowledge, and parents' H1N1 vaccination of their children. Vaccine. 2013;31:4860–6. doi: 10.1016/j.vaccine.2013.07.068. [DOI] [PubMed] [Google Scholar]
- 7.Viswanath K, Minsky S, Ramamurthi D, Kontos E. Boston: Viswanath Lab, Harvard School of Public Health, and Dana-Farber Cancer Institute; 2009. Aug, Communications under uncertainty: communication behaviors of diverse audiences during the A(H1N1) incidence of spring and summer 2009. [Google Scholar]
- 8.Viswanath K, Ramanadhan SR, Kontos EZ. Mass media and population health: a macrosocial view. In: Galea S, editor. Macrosocial determinants of population health. New York: Springer; 2007. pp. 275–94. [Google Scholar]
- 9.Andrulis DP, Siddiqui NJ, Gantner JL. Preparing racially and ethnically diverse communities for public health emergencies. Health Aff (Millwood) 2007;26:1269–79. doi: 10.1377/hlthaff.26.5.1269. [DOI] [PubMed] [Google Scholar]
- 10.Blendon RJ, Benson JM, Desroches CM, Weldon KJ. Using opinion surveys to track the public's response to a bioterrorist attack. J Health Commun. 2003;8(Suppl 1):83–92. doi: 10.1080/713851964. [DOI] [PubMed] [Google Scholar]
- 11.Taylor-Clark KA, Viswanath K, Blendon RJ. Communication inequalities during public health disasters: Katrina's wake. Health Commun. 2010;25:221–9. doi: 10.1080/10410231003698895. [DOI] [PubMed] [Google Scholar]
- 12.Viswanath K. Public communications and its role in reducing and eliminating health disparities. In: Thomson GE, Mitchell F, Williams MB, editors. Examining the health disparities research plan of the National Institutes of Health: unfinished business. Washington: Institute of Medicine; 2006. pp. 215–53. [Google Scholar]
- 13.Viswanath K, Ackerson LK. Race, ethnicity, language, social class, and health communication inequalities: a nationally-representative cross-sectional study. PLoS One. 2011;6:e14550. doi: 10.1371/journal.pone.0014550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Savoia E, Testa MA, Viswanath K. Predictors of knowledge of H1N1 infection and transmission in the U.S. population. BMC Public Health. 2012;12:328. doi: 10.1186/1471-2458-12-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cowling BJ, Ng DM, Ip DK, Liao Q, Lam WW, Wu JT, et al. Community psychological and behavioral responses through the first wave of the 2009 influenza A(H1N1) pandemic in Hong Kong. J Infect Dis. 2010;202:867–76. doi: 10.1086/655811. [DOI] [PubMed] [Google Scholar]
- 16.Gaygisiz U, Gaygisiz E, Ozkan T, Lajunen T. Individual differences in behavioral reactions to H1N1 during a later stage of the epidemic. J Infect Public Health. 2012;5:9–21. doi: 10.1016/j.jiph.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 17.Lin Y, Huang L, Nie S, Liu Z, Yu H, Yan W, et al. Knowledge, attitudes and practices (KAP) related to the pandemic (H1N1) 2009 among Chinese general population: a telephone survey. BMC Infect Dis. 2011;11:128. doi: 10.1186/1471-2334-11-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balkhy HH, Abolfotouh MA, Al-Hathlool RH, Al-Jumah MA. Awareness, attitudes, and practices related to the swine influenza pandemic among the Saudi public. BMC Infect Dis. 2010;10:42. doi: 10.1186/1471-2334-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong LP, Sam IC. Behavioral responses to the influenza A(H1N1) outbreak in Malaysia. J Behav Med. 2011;34:23–31. doi: 10.1007/s10865-010-9283-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rubin GJ, Potts HW, Michie S. The impact of communications about swine flu (influenza A H1N1) on public responses to the outbreak: results from 36 national telephone surveys in the UK. Health Technol Assess. 2010;14:183–266. doi: 10.3310/hta14340-03. [DOI] [PubMed] [Google Scholar]
- 21.Mak KK, Lai CM. Knowledge, risk perceptions, and preventive precautions among Hong Kong students during the 2009 influenza A (H1N1) pandemic. Am J Infect Control. 2012;40:273–5. doi: 10.1016/j.ajic.2011.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong LP, Sam IC. Factors influencing the uptake of 2009 H1N1 influenza vaccine in a multiethnic Asian population. Vaccine. 2010;28:4499–505. doi: 10.1016/j.vaccine.2010.04.043. [DOI] [PubMed] [Google Scholar]
- 23.Zairina AR, Nooriah MS, Yunus AM. Knowledge and practices towards influenza A (H1N1) among adults in three residential areas in Tampin Negeri Sembilan: a cross sectional survey. Med J Malaysia. 2011;66:207–13. [PubMed] [Google Scholar]
- 24.Savoia E, Lin L, Viswanath K. Communications in public health emergency preparedness: a systematic review of the literature. Biosecur Bioterror. 2013;11:170–84. doi: 10.1089/bsp.2013.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Galarce EM, Minsky S, Viswanath K. Socioeconomic status, demographics, beliefs and A(H1N1) vaccine uptake in the United States. Vaccine. 2011;29:528–94. doi: 10.1016/j.vaccine.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 26.Liao Q, Cowling B, Lam WT, Ng MW, Fielding R. Situational awareness and health protective responses to pandemic influenza A (H1N1) in Hong Kong: a cross-sectional study. PloS One. 2010;5:e13350. doi: 10.1371/journal.pone.0013350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parrott C. Japan candidates avoid pressing flesh as flu spreads. Reuters 2009 Aug 20 [cited 2013 Mar 7]. Available from: URL: http://www.reuters.com/article/2009/08/20/us-japan-election-flu-sb-idUSTRE57J1LE20090820.
- 28.Sullivan KJ. Universities collaborate on map showing the effect of H1N1 flu on campus life. Stanford Report 2009 May 13 [cited 2013 Mar 7]. Available from: URL: http://news.stanford.edu/news/2009/may13/flumap-051309.html.
- 29.1 in 3 Canadians may decline handshakes over H1N1: poll. The Hamilton Spectator 2009 Oct 19 [cited 2013 Mar 7] Available from: URL: http://www.thespec.com/news-story/2201916-1-in-3-canadians-may-decline-handshakes-over-h1n1-poll.
- 30.Skeets JE. Fearing H1N1 flu, NBA passes anti-handshake directive. Yahoo News. 2009. Oct 1, [cited 2013 Mar 7]. Available from: URL: http://sports.yahoo.com/nba/blog/ball_dont_lie/post/Fearing-H1N1-flu-NBA-passes-anti-handshake-dire?urn=nba,193384.
- 31.Christensen P. H1N1 fears put graduation tradition on hold. Association of Health Care Journalists. 2009. May 5, [cited 2013 Mar 7]. Available from: URL: http://healthjournalism.org/blog/tag/h1n1/page/6.
- 32.Winnipeg churches ban handshakes over H1N1. CBC News 2009 Sep 27 [cited 2013 Mar 7] Available from: URL: http://www.cbc.ca/news/canada/manitoba/winnipeg-churches-ban-handshakes-over-h1n1-1.794858.
- 33.Rebmann T, Elliott MB, Swick Z, Reddick D. US school morbidity and mortality, mandatory vaccination, institution closure, and interventions implemented during the 2009 influenza A H1N1 pandemic. Biosecur Bioterror. 2013;11:41–8. doi: 10.1089/bsp.2012.0050. [DOI] [PubMed] [Google Scholar]
- 34.Miller JR, Short VL, Wu HM, Waller K, Mead P, Kahn E, et al. Use of nonpharmaceutical interventions to reduce transmission of 2009 pandemic influenza A (pH1N1) in Pennsylvania public schools. J Sch Health. 2013;83:281–9. doi: 10.1111/josh.12028. [DOI] [PubMed] [Google Scholar]
- 35.Meilicke G, Riedmann K, Biederbick W, Muller U, Wierer T, Bartels C. Hygiene perception changes during the influenza A H1N1 pandemic in Germany: incorporating the results of two cross-sectional telephone surveys 2008–2009. BMC Public Health. 2013;13:959. doi: 10.1186/1471-2458-13-959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garcia-Continente X, Serral G, Lopez MJ, Perez A, Nebot M. Long-term effect of the influenza A/H1N1 pandemic: attitudes and preventive behaviours one year after the pandemic. Eur J Public Health. 2013;23:679–81. doi: 10.1093/eurpub/ckt068. [DOI] [PubMed] [Google Scholar]
- 37.Cantey PT, Chuk MG, Kohl KS, Herrmann J, Weiss P, Graffunder CM, et al. Public health emergency preparedness: lessons learned about monitoring of interventions from the National Association of County and City Health Officials survey of nonpharmaceutical interventions for pandemic H1N1. J Public Health Manag Pract. 2013;19:70–6. doi: 10.1097/PHH.0b013e31824d4666. [DOI] [PubMed] [Google Scholar]
- 38.Agolory SG, Barbot O, Averhoff F, Weiss D, Wilson E, Egger J, et al. Implementation of non-pharmaceutical interventions by New York City public schools to prevent 2009 influenza A. PLoS One. 2013;8:e50916. doi: 10.1371/journal.pone.0050916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taylor C. Obama Administration: out with the “swine,” in with the “H1N1 virus.” ABC News 2009 Apr 29 [cited 2013 Mar 7] Available from: URL: http://abcnewsgocom/blogs/politics/2009/04/obama-adminis-5.
- 40.WHO to stop using “swine flu” name to avoid confusion over risk from pigs. Chicago Tribune. 2009. Apr 30,
- 41.WHO changes flu virus strain name from swine flu. Reuters. 2009. Apr 30, [cited 2013 Mar 7]. Available from: URL: http://www.reuters.com/article/2009/04/30/us-flu-who-name-idUSTRE53T5S220090430.
- 42.Dhand NK, Hernandez-Jover M, Taylor M, Holyoake P. Public perceptions of the transmission of pandemic influenza A/H1N1 2009 from pigs and pork products in Australia. Prev Vet Med. 2011;98:165–75. doi: 10.1016/j.prevetmed.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 43.Schein R, Bruls S, Busch V, Wilson K, Hershfield L, Keelan J. A flu by any other name: why the World Health Organization should adopt the World Meteorological Association's storm naming system as a model for naming emerging infectious diseases. J Health Commun. 2012;17:532–45. doi: 10.1080/10810730.2011.626503. [DOI] [PubMed] [Google Scholar]
- 44.Vigsø O. Naming is framing: swine flu, new flu, and A(H1N1) Observatorio J. 2010;4:229–41. [Google Scholar]
- 45.Viswanath K, Breen N, Meissner H, Moser RP, Hesse B, Steele WR, et al. Cancer knowledge and disparities in the information age. J Health Commun. 2006;11(Suppl 1):1–17. doi: 10.1080/10810730600637426. [DOI] [PubMed] [Google Scholar]
- 46.Ackerson LK, Viswanath K. Communication inequalities, social determinants, and intermittent smoking in the 2003 Health Information National Trends Survey. Prev Chronic Dis. 2009;6:A40. [PMC free article] [PubMed] [Google Scholar]
- 47.Census Bureau (US) Current Population Survey 2009 [cited 2010 Jul 20] Available from: URL: http://www.census.gov/cps.
- 48.Suro R, Escobar G. Washington: Pew Research Center; 2006. 2006 National Survey of Latinos: the immigration debate. Also available from: URL: http://pewhispanic.org/reports/report.php?ReportID=68 [cited 2010 Jul 20] [Google Scholar]
- 49.Dennis JM. Menlo Park (CA): Knowledge Networks; March; 2010. KnowledgePanel®: processes & procedures contributing to sample representativeness & tests for self-selection bias. [Google Scholar]
- 50.GfK. Palo Alto (CA): Gfk; 2013. GfK-KnowledgePanel® design summary. [Google Scholar]
- 51.Savoia E, Massin-Short SB, Rodday AM, Aaron LA, Higdon MA, Stoto MA. Public health systems research in emergency preparedness: a review of the literature. Am J Prev Med. 2009;37:150–6. doi: 10.1016/j.amepre.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 52.National Cancer Institute (US) Health Information National Trends Survey 2003 (HINTS 2003) [cited 2013 Mar 13] Available from: URL: http://hints.cancer.gov/docs/HINTS_2003_Instrument-English.pdf.
- 53.Cantor D, Covell J, Davis T, Park I, Rizzo L. Bethesda (MD): National Cancer Institute (US); 2005. Health Information National Trends Survey 2005 (HINTS 2005): final report. Also available from: URL: http://hints.cancer.gov/docs/HINTS_2005_Final_Report.pdf [cited 2014 Jul 20] [Google Scholar]
- 54.Cantor D, Coa K, Crystal-Mansour S, Davis T, Dipko S, Sigman R. Bethesda (MD): National Cancer Institute (US); 2009. Health Information National Trends Survey (HINTS) 2007: final report. Also available from: URL: http://hints.cancer.gov/docs/HINTS2007FinalReport.pdf [cited 2014 Jul 20] [Google Scholar]
- 55.StataCorp. College Station (TX): StataCorp; 2009. Stata®: Version 11.0. [Google Scholar]