Abstract
Objective
The Rapid Emergency Alert Communication in Health (REACH) Trial was a randomized control trial to systematically compare and evaluate the effectiveness of traditional and mobile communication modalities for public health agencies to disseminate time-sensitive information to health-care providers (HCPs). We conducted a sub-study to identify the communication channels by which HCPs preferred receiving public health alerts and advisories.
Methods
Enrolled HCPs were blindly randomized into four message delivery groups to receive time-sensitive public health messages by e-mail, fax, or short message service (SMS) or to a no-message control group. Follow-up interviews were conducted 5–10 days after the message. In the final interview, additional questions were asked regarding HCP preferences for receiving public health alerts and advisories. We examined the relationship between key covariates and preferred method of receiving public health alert and advisory messages.
Results
Gender, age, provider type, and study site showed statistically significant associations with delivery method preference. Older providers were more likely than younger providers to prefer e-mail or fax, while younger providers were more likely than older providers to prefer receiving messages via SMS.
Conclusions
There is currently no evidence-based research to guide or improve communication between public health agencies and HCPs. Understanding the preferences of providers for receiving alerts and advisories may improve the effectiveness of vital public health communications systems and, in turn, may enhance disease surveillance, aid in early detection, and improve case finding and situational awareness for public health emergencies.
Public health agencies and health-care providers (HCPs) are essential partners,1 and the importance of the relationship and interdependence of communication and information exchanges between these two entities has become increasingly evident. Public health's ability to conduct early event detection and maintain situational awareness depends on HCPs who are often the first point of contact for those with unexplained or unusual illnesses. Identification of epidemiologic patterns, as illustrated by recent public health alarms regarding West Nile virus,2 severe acute respiratory syndrome (SARS),3 influenza,4 foodborne illnesses,5 and illnesses associated with the intentional release of anthrax6 have been aided by communications between HCPs and public health. In addition, HCPs are activated to respond during natural disasters7 and are considered the trusted and preferred communicators of health information to the public during emergencies.8,9 HCPs rely on public health agencies to provide population health guidelines and updates and facilitate surveillance so they will recognize and control communicable diseases, prevent excess deaths, and mitigate suffering. And communication between public health and HCPs plays a critical role in planning, event detection, response, and communication with the public during and after a public health emergency.
Yet, the most common enduring source of failure in disaster response is communication breakdown on all levels.10,11 Public health emergency and crisis events since 9/11 have generated numerous studies of communication failures and reports of lessons learned from these experiences. In its assessment of the 2002–2003 international SARS outbreak, the World Medical Association cited a significant gap between national and international public health authorities and clinical medicine attributable, in part, to a lack of effective, real-time, two-way communication channels to frontline physicians during this crisis.12 And a wealth of literature has documented the lack of communication and coordination within U.S. federal, state, and local public health agencies, and between public health and key partners such as health-care organizations and HCPs, during the 2001 anthrax attacks,13,14 Hurricanes Katrina and Rita,7,15 and the 2009 novel influenza A (H1N1) pandemic,16,17 among other events.18,19
Today's public health agencies have access to an ever-expanding range of communication strategies and solutions for getting time-sensitive information to the right person at the right time. They range from traditional methods (e.g., faxing, paging, and e-mail) to more novel approaches (e.g., posting to websites, social media sites, instant messaging, and micro-blogging) to mobile modalities such as cell phone short message service (SMS). With so many options available, public health agencies need to know not only how to maximize the likelihood that an emergency preparedness and response message is received, deemed credible, and, when appropriate, acted upon, but also if the message is sent through a modality that meets the recipient's delivery needs and/or preferences.
Outside of emergency preparedness and response, public health is using social marketing—the use of marketing, audience segmentation, and consumer research to design and implement programs—to promote behavior change and inform health communication programs, such as those that aim to increase fruit and vegetable consumption, promote breastfeeding, and decrease the use of tobacco, among other preventive health behaviors.20 A key to successful social marketing is understanding consumers' preferences to distribute communications to groups on a targeted level or tailoring messages to individuals based on message and channel preferences.21,22 In particular, tailored communication can be customized at the individual level, not only to communication delivery preferences, but also to how those preferences may change over time. Reviews of tailored communications of health behavior interventions have concluded that recipients perceive tailored messages as more relevant, likely to be read, memorable, and effective at impacting health behavior change.23,24
It would follow, then, that tailoring public health communications with HCPs could be similarly beneficial. However, few studies to date have investigated message and channel preferences HCPs may have for receiving communications from public health agencies. Staes et al. (2011) surveyed frontline clinicians during the first wave of the 2009 H1N1 pandemic regarding their preferences about e-mail communications during a public health emergency. The study reported that HCPs preferred a single source of authoritative, locally relevant information distributed by their health-care institution and recommended that public health agencies collaborate with these institutions to distribute public health messages by e-mail to their affiliated clinicians.25 Related research by Ockers (2011) examined public health messages to HCPs in four states regarding emergency H1N1 vaccination distributions and their further dissemination to clinic staff. The study reported that e-mail and blast fax were the preferred communication channels for public health messaging to HCPs, while face-to-face interactions were the most frequently chosen method to further disseminate this information to clinic staff.26
Numerous and diverse communication systems can inundate HCPs with multiple, redundant, and conflicting messages disseminated through national, state, local, and professional communication channels and engender alert overload.27,28 Given HCPs' essential roles in a public health emergency, it is critical to know how HCPs prefer to receive time-sensitive information to ensure it is received, deemed credible, and, when appropriate, acted upon. We report findings regarding HCP preferences for receiving messages with varied levels of urgency (i.e., public health alerts and advisories) from a sub-study of the Rapid Emergency Alert Communication in Health (REACH) Trial at the University of Washington Northwest Preparedness and Emergency Response Research Center.
METHODS
Overall study design
The REACH Trial was conducted from 2008 to 2012 in partnership with three public health agencies in the U.S. Pacific Northwest to systematically compare and evaluate the effectiveness of traditional and mobile communication modalities for public health agencies to disseminate time-sensitive information to HCPs. Providers who might contribute to emergency preparedness and response activities (primary care physicians, nurse practitioners, physician assistants, pharmacists, and veterinarians) were invited to participate in each study site.
Enrolled HCPs were blindly randomized into one of four message exposure groups—e-mail, fax, SMS, and control (no message)—regardless of ability to receive communications through the allocated method. For example, if an HCP did not provide a fax number on enrollment, s/he could still be randomized into the fax group.
During one year, quarterly messages based on real public health events were sent to HCPs through their allocated delivery method. Follow-up telephone interviews were conducted 5–10 days after the delivery date. Details regarding site selection, sampling, inclusion/exclusion criteria, recruitment and enrollment, randomization and blinding, messaging intervention, interview development, and intervention assessment for the overall study have been reported elsewhere.27,29 In the final interview at each site, questions were asked to identify HCP channel preferences for receiving public health alerts and advisories.
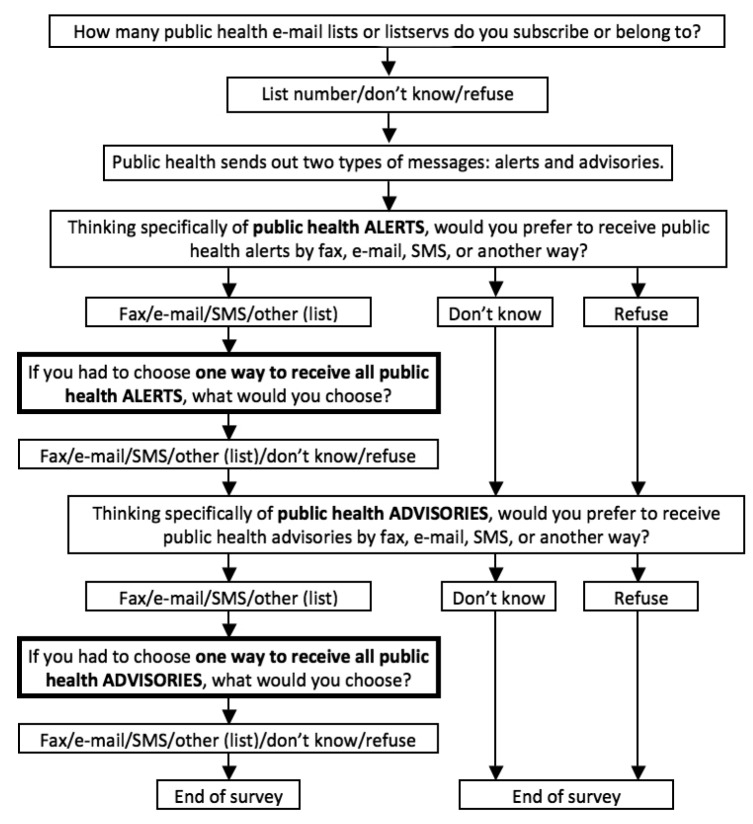
We focused solely on the preferences component of the final intervention assessment follow-up interview. Figure 1 illustrates the interview questions used for the HCP preference analysis. Sub-study interviews were conducted from February 1–11, 2011, for Site 1 HCPs; September 6–23, 2011, for Site 2 HCPs; and May 2–11, 2012, for Site 3 HCPs.
Figure 1.
Follow-up interview question flow in a sub-studya of health-care provider communication channel preferences for public health alerts and advisories in three locations in the U.S. Pacific Northwest, 2011–2012b
aThe Rapid Emergency Alert Communication in Health (REACH) Trial was conducted from 2008 to 2012 in partnership with three public health agencies in the U.S. Pacific Northwest to systematically compare and evaluate the effectiveness of traditional and mobile communication modalities for public health agencies to disseminate time-sensitive information to health-care providers. The sub-study was conducted in the final quarter at each site to elicit health-care provider preferences for receiving alerts and advisories from public health agencies by e-mail, fax, or SMS.
bThe three Pacific Northwest locations and timing of the study were Western Washington, February 2011; Montana, September 2012; and Eastern Washington, March 2012.
SMS = short message service
Data analysis
All HCPs who were contacted in the follow-up surveys were included in the analysis. We analyzed the relationship between exposure group and alert channel preference to specifically test if HCPs expressed a preference for receiving public health alerts and advisories according to the exposure group to which they were assigned. We used a chi-square test to determine differences between alert and advisory preferences, and log-linear models to examine whether the relationship between randomization group and preference was the same for alerts and advisories. We conducted a permutation test using 10,000 permutations to evaluate whether or not HCPs expressed a preference for receiving alert or advisory messages by the same communication channel to which they had been randomized. This test compared the observed proportion of HCPs whose reported delivery preference was equal to the method by which they received study messages with the proportion that would be expected if the exposure group did not influence delivery method preference. We conducted analyses of the relationship between key covariates (gender, age, and provider type) and preferred method of receiving public health alerts and advisories using Fisher's exact test or chi-square tests.
Some HCPs routinely receive public health messages through an e-mail listserv, which may bias their preference toward e-mail regardless of study exposure group. To account for this additional exposure on preferences and investigate whether HCPs on a listserv might have a higher preference for e-mail compared with HCPs who did not report any listserv membership, we performed separate permutation tests to evaluate if self-reported public health e-mail list or listserv membership might impact preference. Participants in the control group were excluded from this analysis. In addition, because it is possible that an HCP in the e-mail exposure group could read study messages on a cell phone, we conducted a separate analysis, using Fisher's exact test, of the relationship between ever reading a study message using a cell phone and channel preference on those providers who received study e-mail messages. All analyses were un-blinded intent-to-treat analyses conducted using R version 2.13.0.30
RESULTS
A total of 846 HCPs enrolled in the study. Table 1 details participation in the preferences interview at each site. Only those HCPs who participated in the preferences interview (n=690; 81.5% of the total HCP enrolled population) were included in the analysis.
Table 1.
Completion and cooperation rates of HCPs in a sub-studya of communication channel preferences conducted in three locationsb in the U.S. Pacific Northwest, 2011–2012
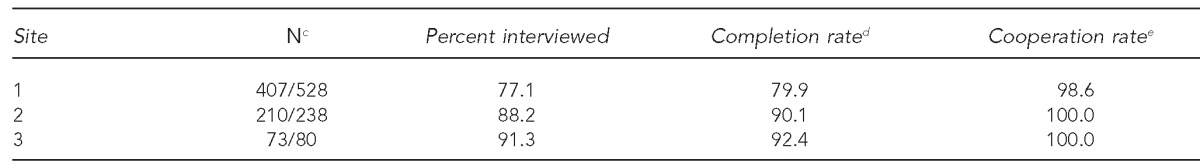
The Rapid Emergency Alert Communication in Health (REACH) Trial was conducted from 2008 to 2012 in partnership with three public health agencies in the U.S. Pacific Northwest to systematically compare and evaluate the effectiveness of traditional and mobile communication modalities for public health agencies to disseminate time-sensitive information to HCPs. The sub-study was conducted in the final quarter at each site to elicit HCP preferences for receiving alerts and advisories from public health agencies by e-mail, fax, or short message service.
The three Pacific Northwest locations and timing of the study were Western Washington, February 2011; Montana, September 2012; and Eastern Washington, March 2012.
cOnly those HCPs who participated in the preferences interview (n=690, 81.5% of total sample) were included in the analysis.
dCompleted interviews/providers enrolled
eCompleted and partially completed interviews/(completed + partially completed interviews) + refusals
HCP = health-care provider
Alert channel preferences
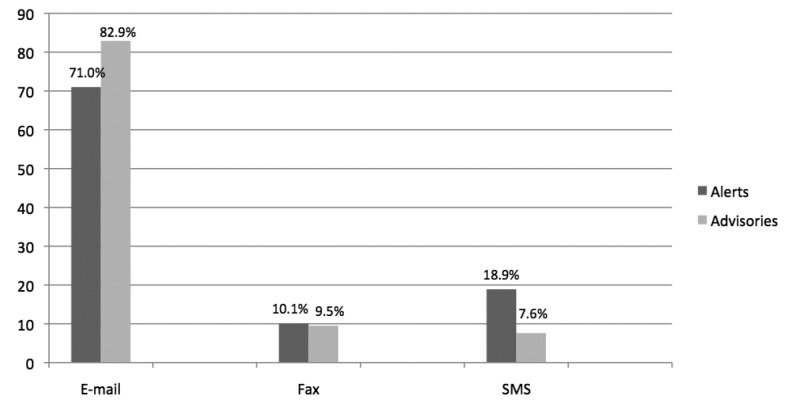
Overall, e-mail (71.0%) was the preferred mode of message delivery of public health alerts for most HCPs, followed by SMS (18.9%), then fax (10.1%) (Figure 2). Table 2A shows the preference for receiving public health alerts by exposure group. Alert channel preference was related to exposure group among those not in the control group (chi-square test, p<0.001) and held when examined separately for listserv membership (p<0.001) and no listserv membership (p<0.001). We used a permutation test to compare the observed proportion of HCPs whose reported alert channel preference was equal to their exposure group with the proportion that would be expected if exposure group did not influence alert channel preference. Because listserv membership might have an influence on this relationship, we performed separate permutation tests by listserv membership status. HCPs in the control group were excluded from this analysis. Results indicated that HCPs were statistically more likely to express a preference for public health alerts to be delivered by the exposure group to which they were assigned, as seen in Table 3, regardless of listserv membership status.
Figure 2.
Message channel preference for public health alerts and advisories in a sub-studya of health-care provider communication channel preferences for public health alerts and advisories conducted in three locationsb in the U.S. Pacific Northwest, 2011–2012
aThe Rapid Emergency Alert Communication in Health (REACH) Trial was conducted from 2008 to 2012 in partnership with three public health agencies in the U.S. Pacific Northwest to systematically compare and evaluate the effectiveness of traditional and mobile communication modalities for public health agencies to disseminate time-sensitive information to health-care providers (HCPs). The sub-study was conducted in the final quarter at each site to elicit HCP preferences for receiving alerts and advisories from public health agencies by e-mail, fax, or SMS.
bThe three Pacific Northwest locations and timing of the study were Western Washington, February 2011; Montana, September 2012; and Eastern Washington, March 2012.
SMS = short message service
Table 2.
HCP preference for receiving public health alerts (A) and public health advisories (B), by exposure group (e-mail, fax, SMS, or control group), in a sub-studya of HCP communication channel preferences for public health alerts and advisories in the U.S. Pacific Northwest, 2011–2012b
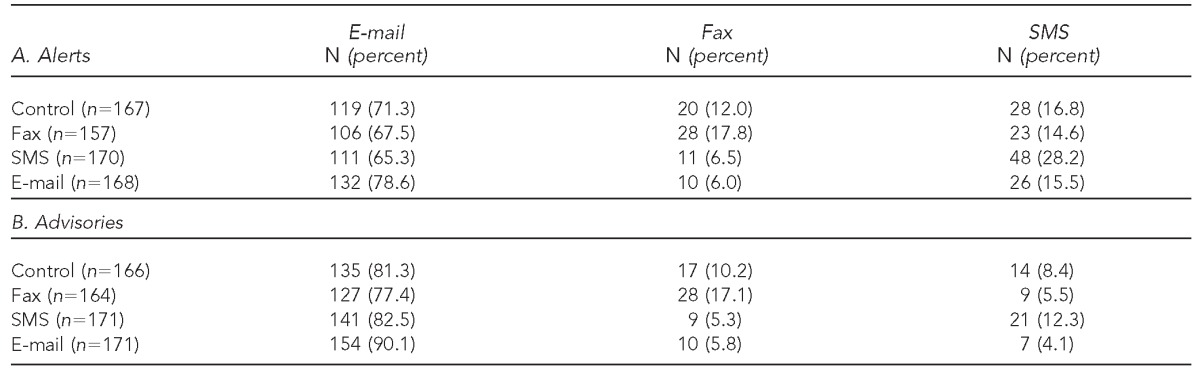
The Rapid Emergency Alert Communication in Health (REACH) Trial was conducted from 2008 to 2012 in partnership with three public health agencies in the U.S. Pacific Northwest to systematically compare and evaluate the effectiveness of traditional and mobile communication modalities for public health agencies to disseminate time-sensitive information to HCPs. The sub-study was conducted in the final quarter at each site to elicit HCP preferences for receiving alerts and advisories from public health agencies by e-mail, fax, or SMS.
The three Pacific Northwest locations and timing of the study were Western Washington, February 2011; Montana, September 2012; and Eastern Washington, March 2012.
HCP = health-care provider
SMS = short message service
Table 3.
Permutation tests examining HCP preference for receiving public health alerts (A) and public health advisories (B), as influenced by study exposure (e-mail, fax, SMS, or control group) or by membership on a listserv, in a sub-studya of HCP communication channel preferences for public health alerts and advisories in the U.S. Pacific Northwest, 2011–2012b
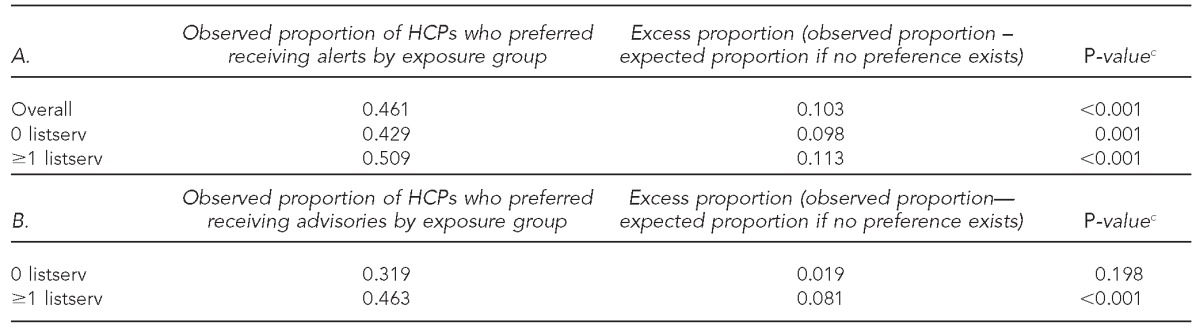
The Rapid Emergency Alert Communication in Health (REACH) Trial was conducted from 2008 to 2012 in partnership with three public health agencies in the U.S. Pacific Northwest to systematically compare and evaluate the effectiveness of traditional and mobile communication modalities for public health agencies to disseminate time-sensitive information to HCPs. The sub-study was conducted in the final quarter at each site to elicit HCP preferences for receiving alerts and advisories from public health agencies by e-mail, fax, or SMS.
The three Pacific Northwest locations and timing of the study were Western Washington, February 2011; Montana, September 2012; and Eastern Washington, March 2012.
cBased on 10,000 permutations
HCP = health-care provider
SMS = short message service
We also examined the relationship among key covariates (gender, age, provider type, listserv membership, and study site) and alert channel preference (Table 4). Gender, age, provider type, and site all showed statistically significant relationships with alert -channel preference. In particular, older HCPs were more likely than younger HCPs to prefer e-mail or fax, while younger HCPs were more likely than older HCPs to prefer receiving alerts by SMS.
Table 4.
Relationship between HCP preference for receiving public health alerts by e-mail, fax, or SMS and HCP communication channel preferences for public health alerts and advisories in a sub-studya of HCP communication channel preferences for public health alerts and advisories in the U.S. Pacific Northwest, 2011–2012b
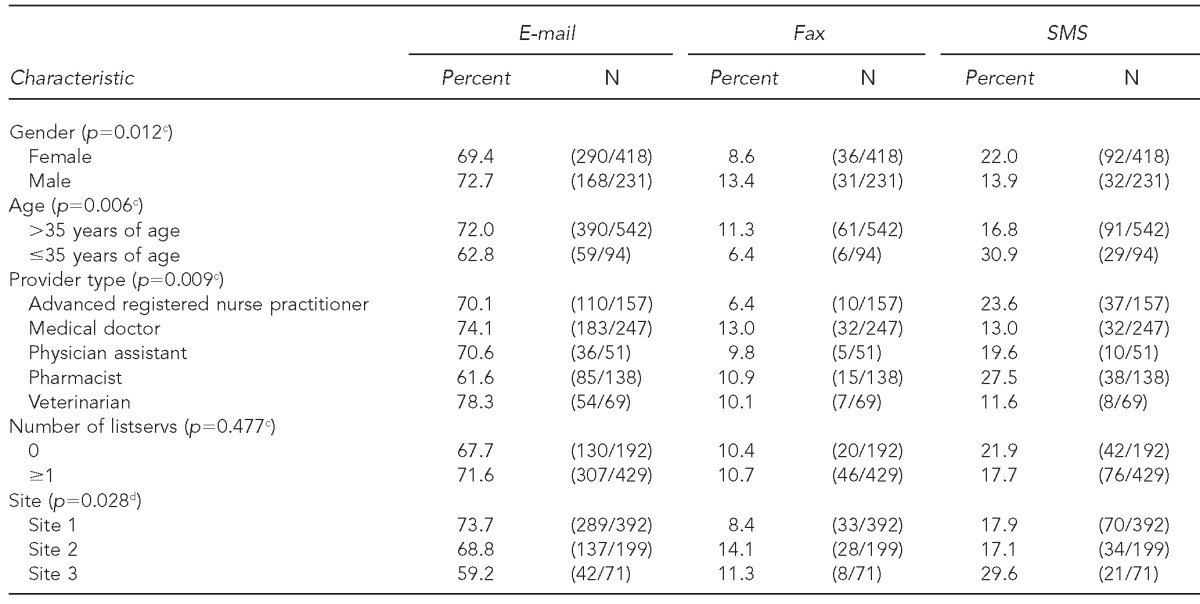
The Rapid Emergency Alert Communication in Health (REACH) Trial was conducted from 2008 to 2012 in partnership with three public health agencies in the U.S. Pacific Northwest to systematically compare and evaluate the effectiveness of traditional and mobile communication modalities for public health agencies to disseminate time-sensitive information to HCPs. The sub-study was conducted in the final quarter at each site to elicit HCP preferences for receiving alerts and advisories from public health agencies by e-mail, fax, or SMS.
The three Pacific Northwest locations and timing of the study were Western Washington, February 2011; Montana, September 2012; and Eastern Washington, March 2012.
cFisher's exact test
dChi-square test
HCP = health-care provider
SMS = short message service
Among the HCPs who recalled receiving a study message by e-mail, the device used to read e-mail was related to channel preference, with 27.3% of those HCPs who read at least one study e-mail message on their phone preferring SMS for alerts vs. 9.9% of those who did not read any study e-mail messages on their phone (p<0.001) (data not shown).
Advisory channel preferences
Overall, e-mail (82.9%) was the preferred mode of message delivery of public health advisories for most HCPs, followed by fax (9.5%), then SMS (7.6%) (Figure 2). Table 2B shows public health advisory channel preferences by exposure group. We conducted an examination of a shift between channel preferences independent of exposure group. As seen in Figure 3, advisory channel preference was similar to alert channel preference, but with a shift toward a preference for receiving advisories by e-mail (p<0.001). Fewer HCPs expressed a preference for receiving advisories by SMS (7.6%) than for receiving alerts by SMS (18.9%), while more HCPs expressed a preference for receiving advisories by e-mail (82.9%) than for receiving alerts by e-mail (71.0%). Little difference was seen between willingness to receive alerts by fax (10.1%) and willingness to receive advisories by fax (9.5%). No evidence was observed that exposure group was related to the magnitude of the shift toward e-mail (p=0.461) (Table 3A). An analysis of the effect of exposure group assignment on advisory channel preference showed similar results to that for alert channel preference among HCPs who belonged to at least one listserv, but no relationship was observed for HCPs who did not belong to a listserv (data not shown).
Figure 3.
Relationship between HCP preference for only one communication channel to receive all public health alerts and receiving all public health advisories by fax, e-mail, or SMSa in a sub-studyb of HCP communication channel preferences for public health alerts and advisories conducted in three locationsc in the U.S. Pacific Northwest, 2011–2012
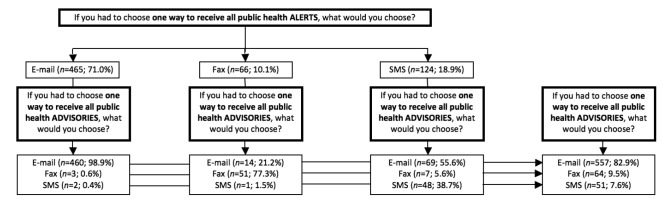
aFigure does not include HCPs who did not answer both the alert and advisory questions (n=665) with either e-mail, fax, or SMS (i.e., excludes HCPs who answered with a different communication channel or answered “refuse” or “don't know” to either question).
bThe Rapid Emergency Alert Communication in Health (REACH) Trial was conducted from 2008 to 2012 in partnership with three public health agencies in the U.S. Pacific Northwest to systematically compare and evaluate the effectiveness of traditional and mobile communication modalities for public health agencies to disseminate time-sensitive information to HCPs. The sub-study was conducted in the final quarter at each site to elicit HCP preferences for receiving alerts and advisories from public health agencies by e-mail, fax, or SMS.
cThe three Pacific Northwest locations and timing of the study were Western Washington, February 2011; Montana, September 2012; and Eastern Washington, March 2012.
HCP = health-care provider
SMS = short message service
Among those HCPs who recalled receiving a study message by e-mail, the device used to read e-mail was not strongly related to an advisory channel preference for SMS, with 4.5% of those HCPs who read at least one study e-mail message on their phone preferring SMS for advisories vs. 4.2% of those who did not read any study e-mail messages on their phone (p=0.094) (data not shown).
DISCUSSION
Recent assessments of national progress in emergency planning, preparedness, and response efforts in the U.S. have noted that the use of new and mobile -technologies needs to be explored for their effectiveness in disaster response.31 To our knowledge, this study is the first to systematically assess preferences for various communication channels for receiving public health alerts and advisories among HCPs who might contribute to emergency preparedness and response activities and who could be potential first points of public contact for information or care during an emergency. While we found that e-mail appears to be the preferred communication channel for receiving both public health alerts and advisories among HCPs, we also noted that prior exposure to communication channel through the parent study (i.e., exposure group) was associated with an increased preference for that channel. This finding suggests that familiarity with the communication channel and preference may be associated—a phenomenon called exposure effect that is well known in marketing, advertising, audience preference, social psychology, and communications research and informs a number of health communication interventions and strategies.32–34
Exposure effect is understood to play a role in preferences. This finding is consistent with our findings indicating that HCPs who were exposed to a communication channel in our study appeared to be more likely to prefer that channel than those who were not exposed. However, our finding that 27.3% of the providers who read at least one e-mail on their cell phone preferred SMS for alerts indicates that increased exposure to and comfort with mobile technology might logically result in a preference for SMS. Exposure effect may also be at play in our finding that younger HCPs vs. older HCPs preferred SMS. The highest levels of cell phone penetration, smart phone ownership, and rates of text messaging are in younger age groups in the U.S.35,36 And, specific to HCPs, ownership and use of mobile technology and smart phones is increasing, particularly among residents and fellows compared with more experienced, older attending physicians.37
We also observed a shift in HCP preference to receive messages by SMS via e-mail when the messages were alerts rather than advisories, suggesting that for more urgent public health issues, HCPs may perceive SMS to be a timelier means of reaching them.
What is unknown, however, is whether or not public health should tailor its messaging to the preferences of HCPs. Our study is a small and limited first step toward a larger investigation of public health message recipient preferences to inform changes in public health policy. Larger randomized trials are needed that compare a variety of incrementally modified intervention conditions—variations in message preference channels, formatting of messages, and time frames of delivery—to investigate their influence on outcomes. Noar et al. (2009) have suggested that studies in this area need to integrate persuasive communications and communication theories, message tailoring, and health behavior theories to inform the design of intervention messages, ensure their relevance and meaningfulness, and, ultimately, improve the efficacy of messaging.33 Health communications research supports tailoring communications by demographic and cultural variables to enhance the efficacy of distributed information. Further research is needed for public health to understand what aspects of message content, timing, and delivery should be incorporated into messaging strategies. It is possible that public health messaging that matches content and communication channel to the preferences and changing preferences of its key audiences may not only make public health alerts and advisories more relevant and meaningful to HCPs, but may also improve the practice of communication between public health agencies and HCPs before, during, and after a public health emergency.
Limitations
This study was subject to several limitations. For one, although this study included 690 providers, we did not have a large enough sample to determine if there were differences among provider type groups (e.g., between advanced registered nurse practitioners and physicians), and our within-group comparison was limited to older vs. younger physicians, as we were not powered to analyze the influence of other covariates (e.g., rural vs. urban provider practice location) on preference. Second, the interview items regarding preferences were only asked during the last provider interview and after interview questions related to the study intervention. It is possible that questions asked prior to the preferences section, which focused on recall of study message and content, may have impacted how HCPs answered questions about message channel preference. Perhaps most importantly, we were not able to test if an HCP's stated preference for receiving alerts or advisories through a specific communication channel might impact the effectiveness of a public health message, improve message recall, or change future behavior in the event of a public health emergency or disaster.
CONCLUSION
This study is the first to systematically identify and compare the preferences for different communication strategies for delivering messages of varying importance and time sensitivity to HCPs. But technological ability alone will not ensure that public health is able to fulfill recipients' communication needs and satisfy stated or known preferences. Systematic objective research is needed so that public health can maximize its effectiveness in delivering time-sensitive information to the right person at the right time—particularly in emergency preparedness, response, and recovery situations.
Footnotes
The study protocol received approval (Minimal Risk Category 7) from the University of Washington Institutional Review Board. The Rapid Emergency Alert Communication in Health Trial is not registered with clinicaltrials.gov, as the protocols were determined to be outside the scope for randomized control trial registration.
The authors thank collaborators at Public Health – Seattle & King County, the Montana Department of Health & Human Services, and the Spokane Regional Health District, as well as the research core at the University of Washington Northwest Preparedness and Emergency Response Research Center.
This work was made possible by the Centers for Disease Control and Prevention (CDC) Office of Public Health Preparedness and Response Extramural Research Program Preparedness and Emergency Response Research Centers award (grant #5P01TP000297) to the University of Washington. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of CDC.
REFERENCES
- 1.Gerberding JL, Hughes JM, Koplan JP. Bioterrorism preparedness and response: clinicians and public health agencies as essential partners. JAMA. 2002;287:898–900. doi: 10.1001/jama.287.7.898. [DOI] [PubMed] [Google Scholar]
- 2.Asnis DS, Conetta R, Waldman G, Teixeira AA. The West Nile virus encephalitis outbreak in the United States (1999–2000): from Flushing, New York, to beyond its borders. Ann N Y Acad Sci. 2001;951:161–71. doi: 10.1111/j.1749-6632.2001.tb02694.x. [DOI] [PubMed] [Google Scholar]
- 3.Severe acute respiratory syndrome (SARS) and coronavirus testing—United States, 2003 [published erratum appears in MMWR Morb Mortal Wkly Rep 2003;52(15):345] MMWR Morb Mortal Wkly Rep. 2003;52(14):297–302. [PubMed] [Google Scholar]
- 4.Outbreak of swine-origin influenza A (H1N1) virus infection—Mexico, March–April 2009. MMWR Morb Mortal Wkly Rep. 2009;58:467–70. [PubMed] [Google Scholar]
- 5.Surveillance for foodborne disease outbreaks—United States, 2006. MMWR Morb Mortal Wkly Rep. 2009;58(22):609–15. [PubMed] [Google Scholar]
- 6.Jernigan JA, Stephens DS, Ashford DA, Omenaca C, Topiel MS, Galbraith M, et al. Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Emerg Infect Dis. 2001;7:933–44. doi: 10.3201/eid0706.010604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pierce JR, Jr, Pittard AE, West TA, Richardson JM. Medical response to Hurricanes Katrina and Rita: local public health preparedness in action. J Public Health Manag Pract. 2007;13:441–6. doi: 10.1097/01.PHH.0000285194.31555.3c. [DOI] [PubMed] [Google Scholar]
- 8.Kahan E, Fogelman Y, Kitai E, Vinker S. Patient and family physician preferences for care and communication in the eventuality of anthrax terrorism. Fam Pract. 2003;20:441–2. doi: 10.1093/fampra/cmg419. [DOI] [PubMed] [Google Scholar]
- 9.Markenson D, Reynolds S. The pediatrician and disaster preparedness. Pediatrics. 2006;117:e340–62. doi: 10.1542/peds.2005-2752. [DOI] [PubMed] [Google Scholar]
- 10.Inglesby TV, Grossman R, O'Toole T. A plague on your city: observations from TOPOFF. Clin Infect Dis. 2001;32:436–45. doi: 10.1086/318513. [DOI] [PubMed] [Google Scholar]
- 11.Reddy MC, Paul SA, Abraham J, McNeese M, DeFlitch C, Yen J. Challenges to effective crisis management: using information and communication technologies to coordinate emergency medical services and emergency department teams. Int J Med Inform. 2009;78:259–69. doi: 10.1016/j.ijmedinf.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 12.World Medical Association. Ferney-Voltaire (France): World Medical Association; 2004. WMA statement on health emergencies communication and coordination. Also available from: URL: www.wma.net/en/30publications/10policies/h32 [cited 2014 Mar 27] [Google Scholar]
- 13.Quinn SC, Thomas T, McAllister C. Postal workers' perspectives on communication during the anthrax attack. Biosecur Bioterror. 2005;3:207–15. doi: 10.1089/bsp.2005.3.207. [DOI] [PubMed] [Google Scholar]
- 14.Chess C, Clarke L. Facilitation of risk communication during the anthrax attacks of 2001: the organizational backstory. Am J Public Health. 2007;97:1578–83. doi: 10.2105/AJPH.2006.099267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ringel JS, Chandra A, Leuschner KJ, Lim YW, Lurie N, Ricci KA, et al. Santa Monica (CA): RAND Health; 2007. Lessons learned from the state and local public health response to Hurricane Katrina. Working paper #WR-473-DHHS. [Google Scholar]
- 16.Stoto MA, Nelson C, Higdon MA, Kraemer J, Hites L, Singleton CM. Lessons about the state and local public health system response to the 2009 H1N1 pandemic: a workshop summary. J Public Health Manag Pract. 2013;19:428–35. doi: 10.1097/PHH.0b013e3182751d3e. [DOI] [PubMed] [Google Scholar]
- 17.Janssen AP, Tardif RR, Landry SR, Warner JE. “Why tell me now?” The public and healthcare providers weigh in on pandemic influenza messages. J Public Health Manag Pract. 2006;12:388–94. doi: 10.1097/00124784-200607000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Crupi RS, Asnis DS, Lee CC, Santucci T, Marino MJ, Flanz BJ. Meeting the challenge of bioterrorism: lessons learned from West Nile virus and anthrax. Am J Emerg Med. 2003;21:77–9. doi: 10.1053/ajem.2003.50015. [DOI] [PubMed] [Google Scholar]
- 19.Dausey DJ, Buehler JW, Lurie N. Designing and conducting tabletop exercises to assess public health preparedness for manmade and naturally occurring biological threats. BMC Public Health. 2007;7:92. doi: 10.1186/1471-2458-7-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grier S, Bryant CA. Social marketing in public health. Annu Rev Public Health. 2005;26:319–39. doi: 10.1146/annurev.publhealth.26.021304.144610. [DOI] [PubMed] [Google Scholar]
- 21.Storey JD, Saffitz GB, Rimon JG. Social marketing. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. San Francisco: Jossey-Bass; 2008. pp. 435–64. [Google Scholar]
- 22.Hornik RC, Ramirez AS. Racial/ethnic disparities and segmentation in communication campaigns. Am Behav Sci. 2006;49:868–84. [Google Scholar]
- 23.Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51:214–21. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133:673–93. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 25.Staes CJ, Wuthrich A, Gesteland P, Allison MA, Leecaster M, Shakib JH, et al. Public health communication with frontline clinicians during the first wave of the 2009 influenza pandemic. J Public Health Manag Pract. 2011;17:36–44. doi: 10.1097/PHH.0b013e3181ee9b29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ockers SB. Atlanta: Emory University, Rollins School of Public Health; 2011. Communication preferences of health care providers during an emergency: data from four state surveys conducted before and after the H1N1 influenza mass vaccination campaigns. Master's thesis. Also available from: URL: pid.emory.edu/ark:/25593/bmfpp [cited 2014 Mar 27] [Google Scholar]
- 27.Baseman JG, Revere D, Painter I, Toyoji M, Thiede H, Duchin J. Public health communications and alert fatigue. BMC Health Serv Res. 2013;13:295. doi: 10.1186/1472-6963-13-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Revere D, Nelson K, Thiede H, Stergachis A, Duchin J, Baseman J. Public health emergency preparedness and response communications with health care providers: a literature review. BMC Public Health. 2011;11:337. doi: 10.1186/1471-2458-11-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Revere D, Painter I, Baseman J. Traditional and mobile public health alert communications with health care providers. Online J Public Health Inform. 2013;5:e124. [Google Scholar]
- 30.R Development Core Team. R: Version 2.13.0. Vienna (Austria): R Foundation for Statistical Computing; 2009. [Google Scholar]
- 31.Inglesby TV. Progress in disaster planning and preparedness since 2001. JAMA. 2011;306:1372–3. doi: 10.1001/jama.2011.1359. [DOI] [PubMed] [Google Scholar]
- 32.MacDonald EK, Sharp BM. Brand awareness effects on consumer decision making for a common, repeat purchase product: a replication. J Bus Res. 2000;48:5–15. [Google Scholar]
- 33.Noar SM, Harrington NG, Aldrich RS. The role of message tailoring in the development of persuasive health communication messages. In: Beck CS, editor. Communication yearbook. New York: Routledge; 2009. pp. 73–134. [Google Scholar]
- 34.Snyder LB, Hamilton MA, Mitchell EW, Kiwanuka-Tondo J, Fleming-Milici F, Proctor D. A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States. J Health Commun. 2004;9(Suppl 1):71–96. doi: 10.1080/10810730490271548. [DOI] [PubMed] [Google Scholar]
- 35.Smith A. Washington: Pew Research Center, Internet & American Life Project; 2013. Smartphone ownership 2013. Also available from: URL: http://www.pewinternet.org/Reports/2013/Smartphone-Ownership-2013.aspx [cited 2014 Mar 27] [Google Scholar]
- 36.Duggan M, Rainie L. Washington: Pew Research Center, Internet & American Life Project; 2013. Cell phone activities 2013. Also available from: URL: http://www.pewinternet.org/2013/09/19/cell-phone-activities-2013 [cited 2014 Mar 27] [Google Scholar]
- 37.Franko OI, Tirrell TF. Smartphone app use among medical providers in ACGME training programs. J Med Syst. 2012;36:3135–9. doi: 10.1007/s10916-011-9798-7. [DOI] [PubMed] [Google Scholar]