Abstract
Objective
Collaboration between existing components of the public health system is important for protecting public health and promoting community resilience. We describe the factors that promote collaborative emergency preparedness and response activities between local health departments (LHDs) and school systems.
Methods
We gathered data from a multistage, stratified random sample of 750 LHDs nationwide. Utilizing a mailed invitation, we recruited respondents to participate in an online questionnaire. We calculated descriptive and inferential statistics.
Results
The majority of LHDs collaborated with school systems for emergency preparedness and response activities and most indicated they were likely to collaborate in the future. Characteristics of the jurisdiction, general experience and perceptions of collaboration, and characteristics of the preparedness collaboration itself predicted future collaboration.
Conclusion
Our results help us understand the nature of collaborations between LHDs and school systems on emergency preparedness and response activities, which can be used to identify priority areas for developing successful and sustainable joint efforts in the future. By focusing on the perceived value of collaboration and building on existing non-preparedness partnering, communities can increase the likelihood of ongoing successful LHD-school system emergency preparedness collaborations.
To protect and promote public health, a system of intertwined agencies and organizations is essential. While the core responsibility for protecting the public's health lies with governmental public health agencies, interagency coordination with community and collaborative partners is necessary for an efficient and effective response to public health emergencies and disasters. These agencies include those traditionally thought of as part of the public health system, such as local health departments (LHDs), as well as many that may not be initially considered as part of the public health system, such as kindergarten through 12th grade (K–12) school systems.
Collaboration between agencies is defined in the literature as “a process in which organizations exchange information, alter activities, share resources, and enhance each other's capacity for mutual benefit and a common purpose by sharing risks, responsibilities, and rewards.”1,2 Collaborative efforts are important for partner agencies for many reasons. Joint efforts can provide outcomes for partner agencies that may not have been accomplishable individually, as services and programs can be coordinated and resources can be pooled. These outcomes can include enhancing advocacy and resource development, creating more recognition and visibility, providing a more systematic/comprehensive approach, and granting additional opportunities for new projects. Collaborations may also prevent duplication of effort by various agencies. Effective collaborations promote team building, a sense of ownership, and an environment that provides the maximum resources for success.3 In a review of empirical studies on public health partnerships, Mays and Scutchfield found that most studies provided evidence that partnerships between multiple agencies promoted better health outcomes at the population level or, at a minimum, promoted policies and practices that over time would potentially improve population health.4
Successful partnerships build upon the strengths that each partner brings and rely on the cooperation of each contributing party to work toward attaining the goals of the collaboration. Joint efforts are enhanced when involved partners educate each other on each organization's roles and responsibilities, with mutual awareness of resources and expertise improving the collaboration's overall functionality.5–8 Within ongoing collaborative efforts, partner agencies must trust each other, as trusted partners are reliable, follow through, share common missions and goals, and are willing to be open and honest with each other.9 Establishing levels of trust and open communication is important as a component of effective collaborations, which include regular, ongoing, and open communications; cooperation; and coordination.1,3,8,10,11
School systems are important for LHDs to consider when building community partnerships for collaborative efforts. School systems serve a substantial portion of the U.S. population: As reported by the National Center for Education Statistics in 2010, on any given day, 55.4 million students and 3.6 million staff members/faculty can be found at both public and private K–12 schools.12 Physiological characteristics of children, including their smaller stature, may place them at higher risk of harm in an emergency situation. Children may also be less able to psychologically manage the aftereffects of a disaster or other emergency situation.13,14 Although school systems have an obligation to ensure the safety of their students and staff, they may be unable to provide all the necessary services on their own, particularly during an emergency.15 Meeting the health needs of children during an emergency may be especially problematic as fewer schools have onsite health or nursing staff. Public health agencies are tasked with protecting the health of their jurisdictions, including during emergency situations, and working with schools can help achieve this mission.16 Collaborative efforts between school systems and LHDs can improve the ability of schools to provide adequate services to this at-risk population.
Existing collaborative efforts between LHDs and other community partners can serve as an entry point for emergency preparedness efforts. Many school systems have health-related programs already in place, including obesity prevention, tobacco education and cessation, and in some cases education about sexually transmitted diseases/infections. Building upon existing relationships and programs can be beneficial in developing joint preparedness strategies for LHDs and school systems. Preparedness activity collaborations can include cowriting plans, implementing disaster drills and exercises, and preparing schools to be a shelter or point of dispensing during emergencies.
To develop effective, sustainable collaborations between LHDs and school systems, it is important to assess factors that may contribute to the success of such efforts. We discuss findings from this research project on enhancing the resiliency of public health systems through partnerships. We aim to (1) discuss the current nature of strategic and operational collaboration between LHDs and school systems and (2) assess factors that promote sustainable collaborations that focus on emergency preparedness and response.
METHODS
Study sample
Our study used a stratified national sample of LHDs that were members of the National Association of County and City Health Officials (NACCHO) in 2010.17 We stratified LHDs based on size of jurisdiction served into small (<25,000 people), medium (25,000–249,999 people), and large (≥250,000 people) agencies, and then used a probability-proportional-to-size sampling design to select 750 LHDs for the study.
Questionnaire design and distribution
We developed an online questionnaire, based on a review of both the preparedness literature and the interagency collaboration literature, to measure the current nature of strategic and operational collaboration between LHDs and schools systems for general health issues as well as emergency preparedness and response activities. We adopted or adapted questionnaire items from existing instruments when possible to increase validity of the instrument. Members of the research team with expertise in school health and emergency public health reviewed new items. The resultant questionnaire was pretested with a panel of experts in school health and emergency public health known to the research team and then the instrument was revised based on their input.
In spring 2011, we sent invitation letters to the directors of each LHD, asking the individual responsible for emergency preparedness and response to complete the corresponding online survey. LHDs that had not completed the online survey two weeks after the initial invitation mailing received a reminder postcard. Two weeks after the reminder postcard was sent, we mailed a follow-up letter to LHDs that had not submitted a complete survey. We collected participant responses electronically using Snap® Survey Software version 10.018 in spring and early summer 2011. In all, we received 159 responses from LHDs for a response rate of 21.2%. Small LHDs had a lower response rate than those in medium and large strata (13.3% compared with 23.8% and 24.0%, respectively), causing them to be slightly underrepresented when comparing the final sample of 159 responses with the 750 LHDs initially invited.
Measures
We primarily designed the analyses to identify predictors of an LHD's intent to continue existing collaborative efforts with schools, or to start collaborative efforts if not currently collaborating. We measured future intent to collaborate with schools on a Likert scale from 1 (extremely unlikely) to 5 (extremely likely). We hypothesized that characteristics of the LHD, past collaborative efforts (i.e., the success of and satisfaction with such efforts), and the perceived value of collaboration would be predictive of intended continuation or initiation of collaboration with school districts for preparedness purposes.
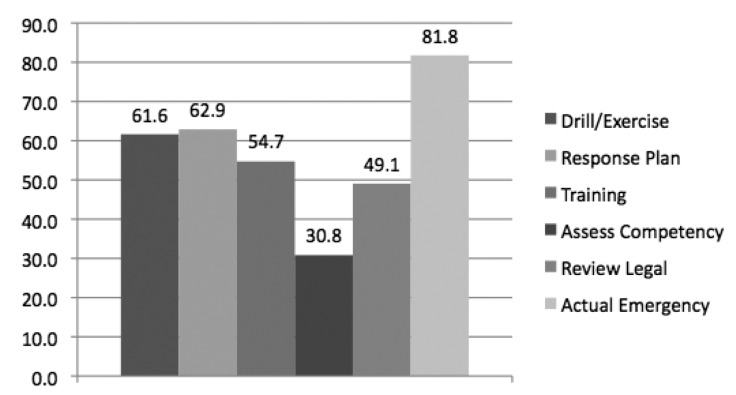
LHD characteristics that we examined included (1) urban vs. rural location, (2) self-reported size of the population served, and (3) number of employees working full time on emergency preparedness and response efforts within their LHD. Aspects of past collaborative efforts that we measured included (1) number of non-preparedness efforts engaged in with the school district, (2) feelings that their existing preparedness efforts were successful, and (3) satisfaction with the existing preparedness efforts. The perceived value of collaboration variable consisted of a scale of 18 positively and negatively worded items on the benefits and drawbacks of collaboration (Figure 1). We reverse-coded the negatively worded items, and the 18 items were scaled using the means (Chronbach's α=0.851).
Figure 1.
Items included in the Perceived Value of Collaboration Scale from a 2011 questionnaire assessing the current nature of LHD-school system interagency collaboration in the U.S.a
aBenefits and drawbacks were scored on a Likert scale from 1 (strongly disagree) to 5 (strongly agree). Scores on perceived drawbacks were reverse-coded within the calculation of perceived value.
bChronbach's a=0.851
LHD = local health department
Analytic strategy
We performed our analysis using SPSS® version 22.0.19 We weighted observations inversely to their probability of selection to adjust for the sample design and calculated descriptive statistics prior to testing for associations. Correlations between the variables were calculated to identify the predictors of intended continued (or new) collaboration with schools for public health preparedness purposes. We conducted multiple linear regression analyses to predict the likelihood of future collaboration efforts with schools. Independent variables were entered as blocks representing characteristics of the health department, value and history of collaboration, and success of and satisfaction with collaboration. A final model was fit with only variables that were statistically significant predictors, including number of full-time preparedness employees, whether or not the LHD classified itself as urban/suburban vs. frontier/rural, number of non-preparedness collaborative activities, number of preparedness activities, perceived value of collaborations, and perceived success of collaborations with schools. We did not find self-reported size of the population served and satisfaction with collaborations to be statistically significant predictors of the likelihood of future collaborations (p=0.718 and p=0.180, respectively); therefore, we did not include them in the final model.
RESULTS
The majority of respondents (73.6%, n=117) were from county health departments, followed by city (14.5%, n=23) and regional (11.3%, n=18) jurisdiction types (data not shown). About half (51.6%, n=82) of the LHDs in the sample were in rural locations, with many serving <50,000 people (47.2%, n=75). LHDs in suburban areas represented 23.3% (n=37) of the sample, and 16.4% (n=26) were from departments primarily providing services to urban areas, with some serving >1 million people (2.5%, n=4). LHDs had a mean of six full-time staff members working on emergency public health preparedness and response, but personnel levels varied from no full-time staff to 220 personnel (Table 1).
Table 1.
Characteristics of LHDs responding to a 2011 questionnaire assessing the current nature of LHD-school system interagency collaboration in the U.S.
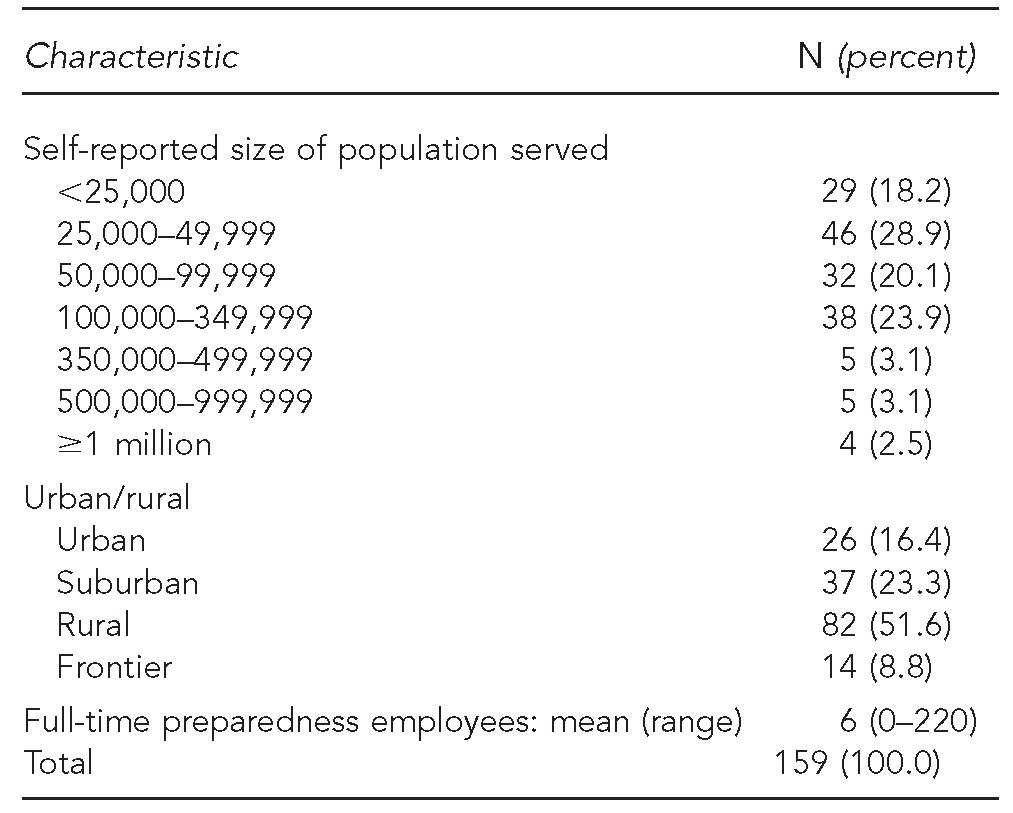
LHD = local health department
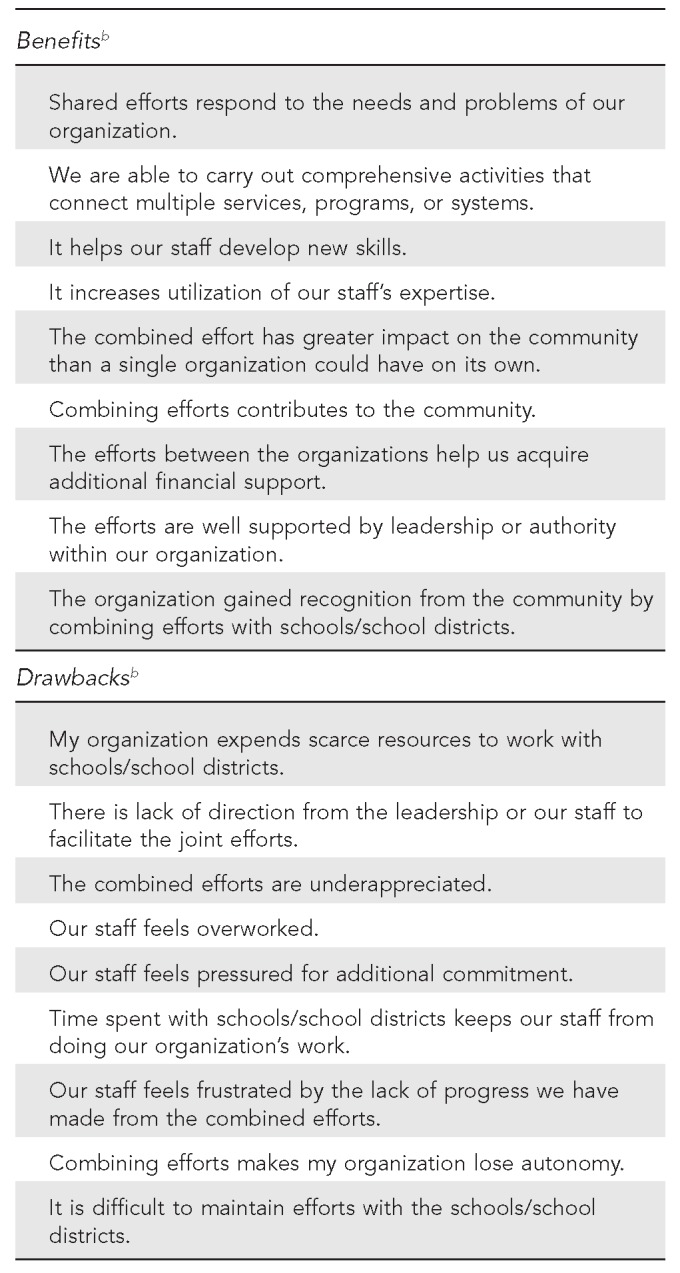
The majority of health departments (85%, n=135) reported participating in joint preparedness efforts with their local school systems. However, only 6.1% (n=10) said they did not engage in any preparedness activities with their school partners in the past year. Joint preparedness activities reported by LHDs included planning, exercises, training staff, assessing staff competency, reviewing legal authorities, and participating in an actual emergency (data not shown). Figure 2 shows the distribution of preparedness activities that LHDs engaged in with their school partners. The number of collaborative preparedness activities ranged from 0 to 6 (mean = 3.5).
Figure 2.
Percentage of LHDs engaging with schools on preparedness activities based on responses to a 2011 questionnaire assessing the current nature of LHD-school system interagency collaboration in the U.S.
LHD = local health department
Most respondents reported intending to collaborate with their school partners in the future. On the Likert scale of 1–5 (where 5 = extremely likely), 62.3% (n=99) rated their likelihood to collaborate as a 5 (mean = 4.4). Inversely, only 3.8% (n=6) reported that they were completely or somewhat unlikely to collaborate with their school partners in the future (data not shown).
Figure 1 depicts variables on the benefits and drawbacks of collaborations included in the composite variable of perceived value of collaboration. Table 2 depicts variables predictive of future collaboration, including characteristics of the jurisdiction, history and perceived value of collaboration, and perceptions of current collaborative efforts. Predictive jurisdictional characteristics on increased likelihood of collaboration included being in an urban area and having fewer full-time preparedness employees. Having a positive view regarding the value of collaboration, engaging in more non-preparedness collaborative efforts, and perceiving the current preparedness collaborative efforts as successful were also predictive of future collaboration. Interestingly, the number of preparedness activities engaged in with schools was inversely related to the likelihood of continued collaboration, with more activities predictive of less likelihood of future engagement.
Table 2.
Regression analysis of the likelihooda of future collaboration with statistically significant predictors, based on responses to a 2011 questionnaire assessing the current nature of LHD-school system interagency collaboration in the U.S.b
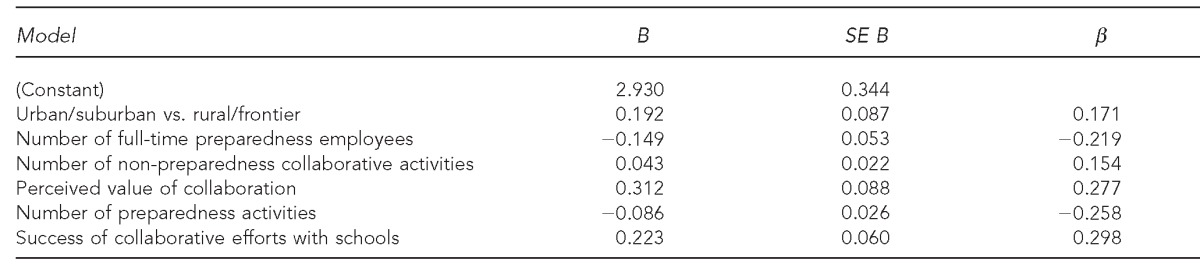
The likelihood of future collaborations was measured on a Likert scale from 1 (extremely unlikely) to 5 (extremely likely).
R2 = 0.322 (p<0.001)
LHD = local health department
SE = standard error
DISCUSSION
The results of this study are encouraging for public health preparedness efforts. Clearly, a majority of LHDs are engaging with their school partners for emergency preparedness and response purposes. However, the majority of interactions with the schools might not necessarily be intentional. Most collaborative activity occurred during an actual emergency. As this study was conducted shortly after the H1N1 pandemic of 2009, it is highly likely that the response to the pandemic was a motivating factor for collaboration. However, most LHDs intended to continue (or start) collaborative efforts in the future. It may be that working with schools during the H1N1 pandemic was seen as positive and, thus, motivated LHDs to continue the collaboration.
The results of the regression model provide a mechanism for increasing and improving collaboration between LHDs and schools. Health departments located in urban/suburban areas and those with fewer full-time preparedness employees were more likely to indicate they would collaborate with schools in the future. While at first thought this finding may be counterintuitive, past research has shown that collaboration in rural areas is different than that in urban/suburban areas.4 In rural communities, the collaboration may be less interdepartmental and more a function of personal relationships in a close-knit community, which may result in less intentional collaborative efforts. The inverse relationship between number of employees and likelihood of future collaboration may be due to less perceived urgency to work with partners among those employed at larger health departments. This lack of urgency could result from the view that there is sufficient staff in the health department to do the preparedness work.
Engagement in more non-preparedness -collaborative efforts was also significant in predicting ongoing collaboration with school systems. As health departments engage in varied efforts with school systems, the support for continued efforts may grow, as well as the potential efficiency of the establishment and implementation of efforts. Areas that do not yet have existing collaborations may benefit from using established collaborations from other jurisdictions as models for developing efforts among their own LHD and school system.
The LHD's perceived value of collaboration, in general, was also important. As this variable comprised several factors including leadership, support, availability of time, and appreciation, attempts to improve upon these factors could have an impact on increasing the perceived value of collaboration. Improving the perceived value of collaboration within the agency may lead to more incentive for continuing or beginning collaborations. Public health leaders may have an effect on the increasing likelihood of future collaborations by providing staff with better recognition, appreciation, and financial support for collaborations. They may also help increase perceived value by providing time and incentives for staff to work with their peers in schools, as well as by promoting the benefits of collaboration.
The final set of predictors includes the nature of the current collaboration for preparedness. Both the perceived success of the preparedness collaboration with schools and the number of preparedness activities engaged in with the schools were predictive of intended future collaboration. As expected, the more successful participants perceived their collaborative efforts with the schools to be, the more likely they would continue those efforts. However, more shared preparedness activities led to less likelihood of future collaboration. One explanation of this finding may be that those departments with a higher number of efforts may be spreading staff and resources too thinly over varied projects, reducing the efficiency, success, or satisfaction of these efforts. Another related explanation may be that those departments with less preparedness activities form more tightly knit groups, which might increase positive attitudes toward future collaborations. It is also possible that those engaging in fewer activities do so in part because of scarcity of resources, so those LHDs might be more inclined to engage in future collaborations out of necessity.
Limitations
While the sampling procedure employed attempted to include a representative sample of LHDs from the initial NACCHO list, the smaller health departments had a lower response rate than larger LHDs and may have been underrepresented. Combined with the overall moderate response rate of 21.2%, this underrepresentation of smaller health departments may limit the ability to generalize results from this study to the national population of LHDs. Additionally, as this study was conducted shortly after the H1N1 pandemic, necessary collaborations during that period may have distorted observed results from those expected outside of such a large-scale event. While this distortion may have affected perceptions of success and value and the likelihood of future collaborations, any successes or failures during this type of real event can be used as the basis for establishing and improving future collaborations. Further research comparing findings both including and excluding an event of this scale during different time periods would produce useful comparisons with current study results.
CONCLUSIONS
Our research suggests that public health agencies view collaboration with schools as important and positive and that those positive perceptions are important for future collaborations to occur. These findings may indicate that an important focus of improving collaboration success might lie within emphasizing leadership support, encouragement, and incentives for staff members who are creating or implementing joint efforts. Using current effective efforts as models to develop new collaborations may lead to greater and more successful collaborations between these organizations.
Footnotes
This research was made possible by funding from the Centers for Disease Control and Prevention (CDC) Preparedness and Emergency Response Research Center funding award #1P01TP000303. The views expressed in this article are those of the authors and do not necessarily represent the views of CDC. The project was reviewed and approved by the University of California, Los Angeles South Campus General Institutional Review Board.
REFERENCE
- 1.Friedman SR, Reynolds J, Quan MA, Call S, Crusto CA, Kaufman JS. Measuring changes in interagency collaboration: an examination of the Bridgeport Safe Start Initiative. Eval Program Plann. 2007;30:294–306. doi: 10.1016/j.evalprogplan.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 2.Himmelman AT. Minneapolis: Himmelman Consulting; 2004. Collaboration for a change: definitions, decision-making models, roles, and collaboration process guide. [Google Scholar]
- 3.Rinehart TA, Laszlo AT, Briscoe GO. Washington: Department of Justice (US); 2001. Collaboration toolkit: how to build, fix, and sustain productive partnerships. [Google Scholar]
- 4.Mays GP, Scutchfield FD. Improving public health system performance through multiorganizational partnerships. Prev Chronic Dis. 2010;7:A116. [PMC free article] [PubMed] [Google Scholar]
- 5.Weist MD, Lowie JA, Flaherty LT, Pruitt D. Collaboration among the education, mental health, and public health systems to promote youth mental health. Psychiatr Serv. 2001;52:1348–51. doi: 10.1176/appi.ps.52.10.1348. [DOI] [PubMed] [Google Scholar]
- 6.Weist MD, Prosecher E, Prodente C, Ambrose MG, Waxman RP. Mental health, health, and education staff working together in schools. Child Adolesc Psychiatr Clin N Am. 2001;10:33–43. [PubMed] [Google Scholar]
- 7.Pruitt DB. Leeches and hematomas: a discussion. J Am Acad Child Adolesc Psychiatry. 1998;37:2–8. doi: 10.1097/00004583-199801000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Leonard LG. Primary health care and partnerships: collaboration of a community agency, health department, and university nursing program. J Nurs Educ. 1998;37:144–8. doi: 10.3928/0148-4834-19980301-12. [DOI] [PubMed] [Google Scholar]
- 9.Varda DM, Chandra A, Stern SA, Lurie N. Core dimensions of connectivity in public health collaboratives. J Public Health Manag Pract. 2008;14:E1–7. doi: 10.1097/01.PHH.0000333889.60517.46. [DOI] [PubMed] [Google Scholar]
- 10.Bashir Z, Lafronza V, Fraser MR, Brown CK, Cope JR. Local and state collaboration for effective preparedness planning. J Public Health Manag Pract. 2003;9:344–51. doi: 10.1097/00124784-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Titanich K, McDonough J, Woodhead-Lyons S, Snell S. Black Lakes community health pilot project—Alberta, Canada. In: Anderson ET, McFarlane J, editors. Community as partner: theory and practice in nursing. 2nd ed. Philadelphia: J.B. Lippincott; 1996. pp. 3–19. [Google Scholar]
- 12.Department of Education (US), National Center for Education Statistics. Table 1. Projected number of participants in educational institutions, by level and control of institution: fall 2010 [cited 2012 May 10] Available from: URL: http://nces.ed.gov/programs/digest/d10/tables/dt10_001.asp?referrer=report.
- 13.Allen GM, Parrillo SJ, Will J, Mohr JA. Principles of disaster planning for the pediatric population. Prehosp Disaster Med. 2007;22:537–40. doi: 10.1017/s1049023x00005392. [DOI] [PubMed] [Google Scholar]
- 14.Emergency Management Watch. Emergency preparation for special populations, part 1: pediatrics: vulnerable patients need extra care. Environ Care News. 2005;8:8–10. [Google Scholar]
- 15.Federal Emergency Management Agency (US), Emergency Management Institute. Multi-hazard emergency planning for schools [cited 2012 Nov 13] Available from: URL: www.tn.gov/education/health_safety/docs/MultiHazardforSchools.pdf.
- 16. Pub. L. No. 109-417, 120 Stat. 2831 (Dec 19, 2006)
- 17.National Association of County and City Health Officials. 2010 national profile of local health departments. Washington: NACCHO; 2011. [Google Scholar]
- 18.Snap Surveys Limited. Portsmouth (NH): Snap Surveys Limited; 2010. Snap® Survey: Version 10.0. [Google Scholar]
- 19.IBM Corp. Armonk (NY): IBM Corp.; 2013. SPSS® for Windows: Version 22.0. [Google Scholar]