Abstract
Successful treatment with heart rate lowering medication has been used to treat adults with chronic myocardial dysfunction of various aetiologies for a number of years. There has been recent evidence for the successful use of β-receptor blocking medication in highly selected group of infants with diastolic myocardial dysfunction. This case series demonstrates that while the use of β-receptor blockers in infants early following initial treatment of congenital left heart obstructive lesions appears promising and safe adjunct to more conventional management, the medium-term and long-term care of these patients remains as challenging as before.
Background
Following successful treatment of adults with myocardial dysfunction of various aetiologies for a number of years with β-blockers,1–3 there is recent evidence of its successful use in paediatric patients with postoperative myocardial dysfunction. The use of intravenous esmolol successfully improved postoperative recovery in selected infants with significant postoperative diastolic myocardial dysfunction.4
Our case reports demonstrate that such patients can present with significant residual congenital lesions of the left heart despite initial favourable response to surgical and medical treatment and successful hospital discharge.
Case presentation
Case A
A neonate with antenatal diagnosis of coarctation of the aorta was found to have a small mitral valve (Z score −3.5) and the left ventricle (long axis Z score −6.5) postnatally. He was operated on day 3 of life with resection of his coarctation and extended end to end anastomosis. Postoperative recovery was prolonged despite successful relief of his coarctation, good ventricular systolic function, no evidence of pulmonary hypertension or significant left-sided obstruction. He was successfully weaned off his ventilatory support once he was on intravenous esmolol (250 μg/kg/min) to achieve satisfactory heart rate reduction and improve left ventricular diastolic function. He was extubated on the 34th postoperative day and was converted to oral propanolol treatment while on continuous positive airway pressure (CPAP) support. He was subsequently discharged on the 77th postoperative day.
On review at 4 months of age, he had developed severe mitral valve stenosis (mean gradient 12 mm Hg), severe subvalvar muscular aortic stenosis (peak systolic gradient 109 mm Hg) and left ventricular hypertrophy. He had good biventricular systolic function, and peak systolic gradient across the coarctation repair site 23 mm Hg. He underwent cardiac catheterisation with balloon angioplasty of recoarctation followed by surgical resection of subaortic obstruction and repair of mitral valve. He required venoarterial (V-A) extracorporeal membrane oxygenation (ECMO) support following an early postoperative cardiac arrest. He was successfully weaned off ECMO after 9 days.
Owing to and worsening mitral stenosis he underwent mitral valve replacement with an 18 mm St Jude's mechanical valve. To wean him off the ventilator he was started on β-blockers initially with intravenous esmolol and later oral propanolol. His clinical progress plateaued and a diagnostic cardiac catheterisation showed significant mitral paravalvular leak without significant left-sided obstruction. He deteriorated while awaiting mitral valve repair and suffered two cardiac arrests. He underwent emergency mitral valve replacement with a 17 mm St Jude's valve in supravalvar position with subsequent elective ECMO support.
Case B
A neonate born with critical aortic stenosis diagnosed on postnatal echocardiogram showing small dysplastic aortic valve (Z score −3.2), apex forming left ventricle with poor systolic function, was treated by emergency transcatheter balloon valvuloplasty at the age of 2 days. Ross procedure followed at the age of 2.5 months. Postoperative recovery was complicated by poor left ventricular diastolic function (figure 1) and artificial ventilation dependency. Diagnostic cardiac catheterisation demonstrated elevated left ventricular end-diastolic pressure of 24 mm Hg, no aortic stenosis or coarctation. On the 24th postoperative day he was started on intravenous esmolol (200 μg/kg/min) to reduce his heart rate satisfactorily and to improve left ventricular diastolic function (figure 2). He was successfully extubated 4 days later.
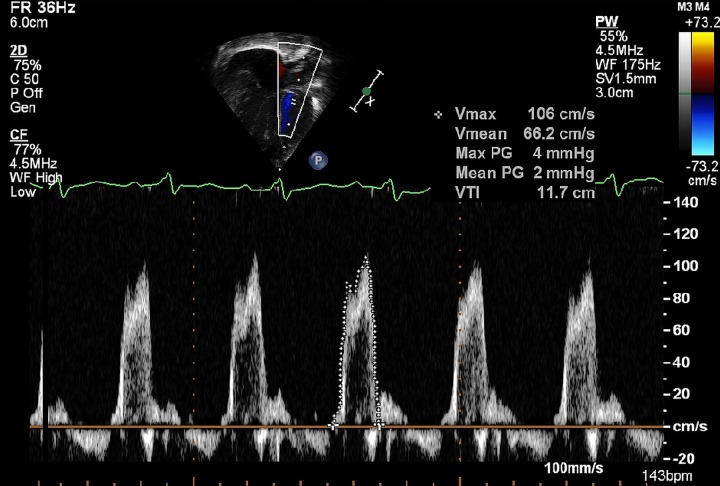
Figure 1.
Pulse wave Doppler across the mitral valve showing E and A wave reversal suggesting diastolic dysfunction.
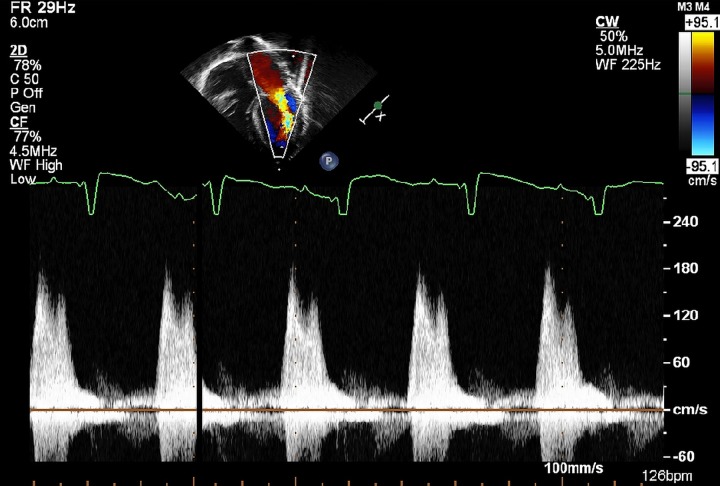
Figure 2.
Pulse wave Doppler across the mitral valve showing normal E and A wave pattern. This is consistent with normal diastolic function.
Case C
A neonate born at 33 weeks of gestation with Kabuki syndrome had a surgical valvuloplasty for thickened and stenotic bicuspid aortic valve (Z score −2.5)—peak systolic gradient on echocardiogram of 72 mm Hg, (mean gradient 40 mm Hg) at the corrected age of term plus 2 weeks. Postoperative course was complicated by dependency on non-invasive ventilatory support. Echocardiogram on postoperative day 5 showed good left ventricular systolic function with diastolic dysfunction and a peak systolic gradient across the aortic valve of 30 mm Hg (mean gradient 15 mm Hg). The left ventricular diastolic function was improved by use of intravenous esmolol with subsequent conversion to oral propanolol. The patient was successfully weaned off CPAP and discharged from hospital 17 days postoperatively.
Review at corrected age of 13 weeks showed the peak systolic gradient across aortic valve to be 80 mm Hg. Transcatheter balloon valvuloplasty lead to reduction of an echocardiographic peak systolic gradient to 71 mm Hg partly due to dynamic muscular subvalvar obstruction.
Outcome and follow-up
The three patients had the following outcomes. The patient in case A was weaned from ECMO and died 14 days after his last surgery. The patient in case B remains well and continues to be followed in outpatient clinic while on treatment with propranolol. The patient in case C was successfully weaned off the β-receptor blocking medication without adverse changes to his left ventricular diastolic dysfunction. She remains well while followed-up in the outpatient clinic.
Discussion
Neonates and infants with borderline size of the left ventricular structures represent a challenging group of patients with uncertain outcome when biventricular treatment pathway is chosen.5 The initial use of Esmolol, a selective β-1-receptor blocking agent and subsequently the use of propanolol, non-selective β-receptor blocker have been advocated in these patients in their postoperative course complicated by diastolic left ventricular dysfunction, tachycardia, and dependency on ventilatory support.4 Although in all our patients the short-term benefits of such treatment were obvious from their echocardiographic findings of improved left ventricular diastolic function matched by successful weaning from ventilatory support, the medium and long term outcome of these patients remains uncertain. This outcome is likely to be dictated by the postnatal growth of left heart structures and the presence of residual and/or development of new obstructive lesions.
All our patients required subsequent hospital readmission and cardiac catheter interventional and/or surgical treatment. Close follow-up of infants following initial successful introduction of β-receptor blocking medication is therefore mandatory.
While the use of β-receptor blocking medication in selected infants early following initial treatment of congenital left heart obstructive lesions appears promising and safe adjunct to more conventional management, the medium and long-term care of these patients remains as challenging as previously.
Learning points.
Short-term benefits of β-blockade treatment was clear as demonstrated in echocardiographic findings of improved left ventricular diastolic function matched by successful weaning from ventilatory support.
β-Blockers in selected infants following initial treatment of congenital left heart obstructive lesions appears promising and safe adjunct.
The medium and long-term care of these patients remains as challenging as previously.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Cucherat M Quantitative relationship between resting heart rate reduction and magnitude of clinical benefit in post-myocardial infarction: a meta-regression of randomised clinical trials. Eur Heart J 2007;28:3012–19 [DOI] [PubMed] [Google Scholar]
- 2.Hjalmarson A, Kneider M, Waagstein F. The role of beta-blockers in left ventricular dysfunction and heart failure. Drugs 1997;54:501–10 [DOI] [PubMed] [Google Scholar]
- 3.Kjekshus JK Importance of heart rate in determining beta blocker efficacy in acute and long term acute myocardial infarction intervention trials. Am J Cardiol 1986;57:43F–9F [DOI] [PubMed] [Google Scholar]
- 4.Furck AK, Desai A, Macrae DM, et al. Novel post operative use of beta-blocking medication for infants with left ventricular outflow obstruction and diastolic myocardial dysfunction. Pediatr Cardiol 2012;33:1450–2 [DOI] [PubMed] [Google Scholar]
- 5.Tuo G, Khambadkone S, Tann O, et al. Obstructive left heart disease in neonates with a “Borderline” left ventricle: diagnostic challenges to choosing the best outcome. Pediatr Cardiol 2013;34:1567–76 [DOI] [PubMed] [Google Scholar]