Abstract
A 19-year-old woman presented with a 4-week history of headache, ataxia, vertigo, confusion, intermittent blurred vision in the right eye and intermittent hearing loss. MRI revealed white matter lesions and ‘pepper pot’ lesions of the corpus callosum. The cerebrospinal fluid had raised protein and lymphocytes. Fundal examination revealed multiple peripheral arterial occlusions in the both eyes confirmed with fundus fluorescein angiography (FFA). A diagnosis of Susac's syndrome was made. The patient was initially treated with steroids, followed by azathioprine and intravenous immunoglobulins (IVIg). Clinical improvement was noted, associated with improvement of the retinal circulation on FFA.
Background
Susac's syndrome presents a diagnostic challenge due to the unusual constellation of symptoms as a result of the classical triad of encephalopathy, branch retinal artery occlusions and hearing loss.1 MRI changes are commonly interpreted as that of multiple sclerosis (MS) or acute disseminated encephalomyelitis (ADEM).2 Ophthalmological review and investigation can help to clinch the diagnosis and pave the way for treatment. We also suggest a potential role for fundus fluorescein angiography (FFA) in monitoring the condition.
Case presentation
A 19-year-old woman presented with a 4-week history of headache, ataxia, vertigo, confusion, blurred vision in the right eye and intermittent hearing loss. There were also two episodes of urinary incontinence and slurred speech. On questioning the patient's family they noted a behavioural change for 6–8 weeks prior to the onset of the above symptoms.
Neurological examination elicited extensor plantars, a wide-based gait and an inferior visual field defect in the right eye. A provisional diagnosis of subacute encephalopathy was made, appropriate investigations undertaken and referral to ophthalmology initiated.
Ophthalmological examination revealed cotton wool spots in the retina and multiple branch retinal artery occlusions in both eyes.
Investigations
MRI showed multiple foci of high signal in periventricular locations. Areas of signal change were seen within the corpus callosum (figure 1) and lesions were also seen within the middle cerebellar peduncles.
Figure 1.
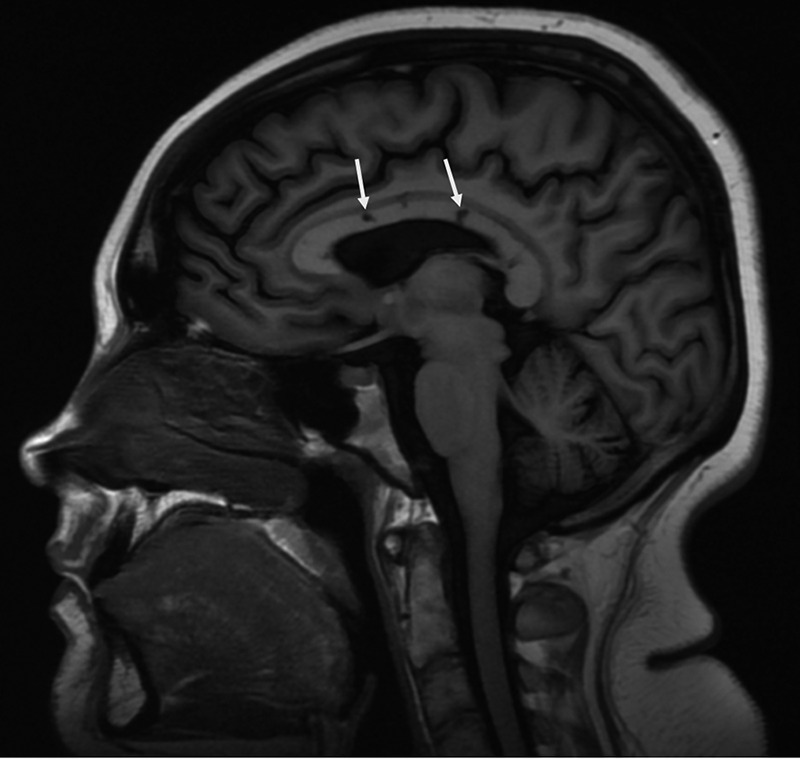
Saggital MRI of the head showing lesions of the corpus callosum (arrows).
Lumbar puncture found raised protein (1.39 g/L, range 0.15–0.45) and a raised lymphocyte count (20×106/L).
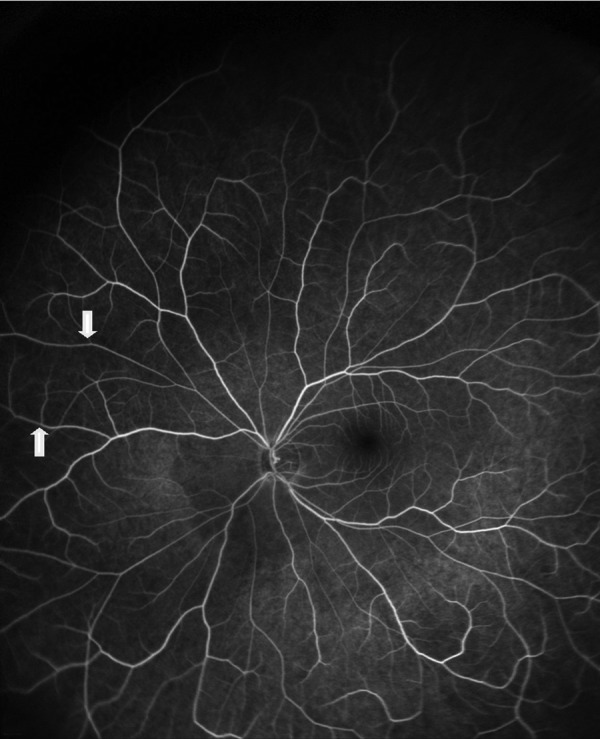
Wide field fundus fluorescein angiography showed multiple peripheral retinal arteriolar occlusions with associated leakage presumably secondary to an inflammatory process affecting the arteriolar endothelium (figure 2). A repeat FFA performed 3 months later following remission from the acute phase showed recanalisation of the occluded arteries and cessation of leakage (figure 3).
Figure 2.

Flourescein angiogram of the right eye at presentation, note the areas of hyperfluorescense denoting leakage from inflamed retinal arterioles (arrows) and the areas of arteriolar occlusion showing a fluid void due to flourscein not passing beyond the blockage (thick arrows).
Figure 3.
Repeat fluorescein angiogram 3 months after presentation. Note the lack of leakage and also reperfusion of the previously occluded retinal arterioles (thick arrows).
Differential diagnosis
The main differential diagnoses of Susac's syndrome include MS and ADEM.2 Herpes simplex encephalitis was unlikely in this case due to the prolonged history. Other conditions to consider include Beçhet's disease and systemic lupus erythematosis, of which both associated with a retinal vaso-occlusive disease.3 Systemic inflammatory conditions associated with a retinal vasculitis more commonly have a predilection to affect the retinal venous circulation.
Treatment
The patient was initially treated with pulsed intravenous methylprednisolone (1 g per day for 3 days) and then switched to oral prednisolone (40 mg per day) that was gradually tapered over a 6-month period to a maintenance dose of 10 mg per day as well as being on azathioprine. Following a presumed relapse the patient was treated with IVIg.
Outcome and follow-up
Four months following presentation the patient suffered deterioration in her clinical symptoms. She developed increasing nausea, dizziness and loss of appetite. She was admitted for 5 day of IVIg and her systemic steroid dose was temporarily increased. Lack of objective evidence, based on repeat MRI and FFA may indicate that this was a functional reporting of worsening symptoms as opposed to a true relapse of Susac's syndrome.
Since that episode she has made a gradual recovery in almost all aspects. However, neuropsychological assessment identified a number of deficits, such as recall of verbal information, problem-solving and reasoning tasks. The patient also continues to suffer with a degree of depression and anxiety.
Following the acute phase of the disease there has been no objective evidence of a relapse. Of note a repeat FFA 2 years following presentation shows no active leakage and also reperfusion of areas in the peripheral retina.
Discussion
Susac's syndrome consists of a classical triad of encephalopathy, sensorineural hearing loss and branch retinal artery occlusions. It is a presumed autoimmune inflammatory disease preferentially affecting the endothelium of arterioles in the brain, cochlea and retina.1 There are over 300 cases in the published literature.4 The triad described is not always present and the clinical course can vary with monocyclic, polycyclic and chronic progressive types being described, the monocyclic being the most common.4
Owing to its rarity there is no consensus on effective treatment with empirical treatment based on the presumptive autoimmune inflammatory endotheliopathy aetiology.4
The wide field FFA can be very useful to help clinch the diagnosis in such cases. Figure 2 shows marked changes in the peripheral retinal vasculature that may be missed with conventional FFA. We also propose a potential role of repeat FFA in monitoring disease activity based on the degree of leakage (hyperfluorescence attributed to inflammation) from the retinal arterioles demonstrated in this patient from repeat FFA performed early and then late in the clinical course.
Radiological changes can often be mistaken for those of MS although there are some distinguishing features. In both conditions areas of signal change are seen within the corpus callosum. In Susac syndrome the corpus callosum lesions usually involve the central fibres whereas in MS and ADEM involvement is of the undersurface at the septal interface.
Learning points.
Any unexplained encephalopathy warrants referral to an ophthalmologist for a dilated fundus examination.
Fundus fluorescein angiography (FFA) is of great value, demonstrating the branch retinal artery occlusions and hyperfluorescence of the leaking arterioles. Repeat FFA can show reduced hyperfluorescence which may correlate with disease activity.
Lesions of the corpus callosum on MRI are not pathognomonic of multiple sclerosis. If they are involving the central fibres with relative peripheral sparing a diagnosis of Susac's syndrome should be considered.
Footnotes
Contributors: IJK was involved in writing of the manuscript and obtained patient consent. HA was responsible for patient's care from presentation to present day, carried out the diagnosis and critically reviewed and edited manuscript. SP was responsible for ophthalmological input, organisation, interpretation of angiograms, critically appraised and edited the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Susac JO, Egan RA, Rennenbohm RM, et al. Susac's syndrome: 1975–2005 microangiopathy/autoimmune endotheliopathy. J Neurol Sci 2007;257:270–2 [DOI] [PubMed] [Google Scholar]
- 2.Susac JO Susac's syndrome. AJNR Am J Neuroradiol 2004;25:351–2 [PMC free article] [PubMed] [Google Scholar]
- 3.Mohsenin A, Huang JJ. Ocular manifestations of systemic inflammatory diseases. Conn Med 2012;76:533–44 [PubMed] [Google Scholar]
- 4.Dörr J, Krautwald S, Wildemann B, et al. Characteristics of Susac syndrome: a review of all reported cases. Nat Rev Neurol 2013;9:307–16 [DOI] [PubMed] [Google Scholar]


