Abstract
Background
Early reperfusion in the setting of an ST‐elevation myocardial infarction (STEMI) is of utmost importance. However, the effects of early versus late reperfusion in this patient group undergoing primary percutaneous coronary intervention (PCI) have so far been inconsistent in previous studies. The purpose of this study was to evaluate in a nationwide cohort the effects of delay from first medical contact to PCI (first medical contact [FMC]‐to‐PCI) and secondarily delay from symptom‐to‐PCI on clinical outcomes.
Methods and Results
Using the national Swedish Coronary Angiography and Angioplasty Register (SCAAR) registry, STEMI patients undergoing primary PCI between the years 2003 and 2008 were screened for. A total of 13 790 patients were included in the FMC‐to‐PCI analysis and 11 489 patients were included in the symptom‐to‐PCI analyses. Unadjusted as well as multivariable analyses showed an overall significant association between increasing FMC‐to‐PCI delay and 1‐year mortality. A statistically significant increase in mortality was noted at FMC‐to‐PCI delays exceeding 1 hour in an incremental fashion. FMC‐to‐PCI delays in excess of 1 hour were also significantly associated with an increase in severe left ventricular dysfunction at discharge. An overall significant association between increasing symptom‐to‐PCI delays and 1‐year mortality was noted. However, when stratified into time delay cohorts, no symptom‐to‐PCI delay except for the highest time delay showed a statistically significant association with increased mortality.
Conclusions
Delays in FMC‐to‐PCI were strongly associated with increased mortality already at delays of more than 1 hour, possibly through an increase in severe heart failure. A goal of FMC‐to‐PCI of less than 1 hour might save patient lives.
Keywords: ST‐segment elevation myocardial infarction, percutaneous coronary intervention
Introduction
Early reperfusion, preferably through a percutaneous coronary intervention (PCI), is currently the approach recommended by international guidelines for care of patients with ST‐elevation myocardial infarction (STEMI).1 Data from patients treated with primary fibrinolysis show considerable gains with early versus late reperfusion.2–5 However, effects of early reperfusion have been difficult to determine in STEMI patients undergoing primary PCI, with several published studies showing widely different treatment effects of early as compared to late reperfusion. While some studies have reported no effect on infarct size with shorter symptom‐to‐PCI timings,2,6 others have reported significant reductions in infarct size.7–10 Similarly, some studies have indicated improved survival with lower symptom‐to‐PCI time whereas others have found no such effects.9,11–14
One of the main reasons for these inconsistent findings could be related to difficulties in the measurement of symptom‐to‐PCI time. First, the timing of symptom onset is subject to recall bias, which might be substantial during a STEMI and under the effect of opiates. Second, symptom onset could be preceded by a period of instability and angina, making the exact time of the STEMI uncertain.12,15 Furthermore, early presenters could, to a higher degree, have more severe coronary disease or comorbidities compared to patients presenting late.16
Other studies have focused on other measures of time to treatment which are not dependent on patient‐reported times, such as door‐to‐balloon time which has reported better outcomes with shorter times. However, door‐to‐balloon time only focuses on the final part of the healthcare chain.13,17–19 The time from first medical contact to PCI (FMC‐to‐PCI) was recently suggested to be a more relevant metric, as it includes all factors involved in the healthcare chain for STEMI patients.12,15 A previous large study indicated reduced mortality with decreasing FMC‐to‐PCI times, but did not observe any association between mortality and decreasing symptom‐to‐PCI times.12
The primary purpose of this study was to investigate the relationship between FMC‐to‐PCI and mortality in a nationwide cohort constituting the largest study population to date using FMC‐to‐PCI as the primary time to treatment metric. The secondary purpose was to investigate the relationship between symptom‐to‐PCI and mortality.
Methods
Study Sample
All Swedish patients undergoing primary PCI for a first STEMI between January 1, 2003 and December 31, 2008 were identified from the nationwide Swedish Coronary Angiography and Angioplasty Register (SCAAR). Of 21 178 patients, a total of 14 969 had information on time from first ECG to PCI, which was used as measure of FMC‐to‐PCI time. Patients with a FMC‐to‐PCI time >6 hours were excluded (n=1179), leaving a total of 13 790 patients for the primary FMC‐to‐PCI analysis. Of these, a total of 7050 patients were diagnosed with a prehospital ECG (51%) and 10 330 patients had information on ejection fraction measured before discharge (75%). In 6495 patients there were 3 years of follow‐up regarding mortality. Of the 21 178 STEMI patients, 14 818 had information on symptom‐to‐PCI time and were included in a secondary analysis of that measure. Patients with symptom‐to‐PCI time >8 hours (n=3329) were excluded leaving 11 489 patients for symptom‐to‐PCI analyses. In 5419 patients there were 3 years of follow‐up regarding mortality.
The rationale for using upper limit cut‐offs of 6 hours for FMC‐to‐PCI and 8 hours for symptom‐to‐PCI were based on previous data regarding infarct development in men as well as clinical data from previous reperfusion trials.20–23
Nation‐wide Registries and Definitions
The primary registry used for data collection was the SCAAR registry, which includes data from all 29 centers that perform coronary angiography or PCI in Sweden. All consecutive patients undergoing a coronary angiography or PCI procedure are included. Based on the unique 10‐digit personal identification number of each Swedish citizen,24 the SCAAR register is merged with other national registries. Data on death were obtained from the national population register through February 2010. Data regarding previous medical history were obtained from the Swedish Hospital Discharge Register dating back from 1987.25 Data regarding discharge medications and ejection fraction at discharge were obtained from The Register of Information and Knowledge about Swedish Heart Intensive care Admissions (RIKS‐HIA). The policy in Sweden is that any patient presenting with chest pain should have a 12‐lead ECG taken as soon as possible upon first medical contact without delay. The time used to gauge first medical contact was thus approximated by the time the first ECG was taken. The time of PCI was determined by the start of the coronary angiography.
Endpoints
The primary endpoint studied was total 1‐year mortality. Secondary endpoints studied were 3‐year mortality as well as severe heart failure at discharge.
Statistical Analyses
Kaplan–Meier estimates of survival were computed across strata of FMC‐to‐PCI and symptom‐to‐PCI times, and compared using log‐rank tests. Adjustment for potential confounders was performed using Cox proportional hazards regression models. Statistical adjustments were made for age, sex, year of procedure, smoking status, hospital, comorbidities (previous hypertension, previous renal failure, previous chronic obstructive pulmonary disease, previous heart failure, previous myocardial infarction, previous diabetes, previous stroke, known dementia, previous bleeding, previous CABG, previous PCI), angiographic data (treated vessel, access site, procedure with stent, number of stents used, use of drug eluting stents, thrombectomy), and antithrombotic medications used (upstream treatment with aspirin, clopidogrel, heparin, low‐molecular weight heparin or GpIIb/IIIa‐inhibitors, as well as procedural use of bivalirudin, heparin, GpIIb/IIIa‐inhibitors or low‐molecular weight heparin).
The associations of FMC‐to‐PCI and symptom‐to‐PCI delays with severely reduced left ventricular ejection fraction (EF <30%) at discharge were tested using logistic regression models. Differences in FMC‐to‐PCI and symptom‐to‐PCI times according to presentation of cardiogenic shock and culprit vessel were also explored, using the Mann–Whitney U test. The proportionality assumption for hazards in the cox regression analyses were visually tested using Kaplan–Meier survival curves of the primary predictors.
All tests were 2‐sided with a P value for significance <0.05. All analyses were performed in SPSS (SPSS version 16, SPSS Inc).
Results
The median FMC‐to‐PCI delay was for the entire population 70 minutes (interquartile range [IQR] 42 to 110). Median symptom‐to‐PCI delay was 175 minutes (IQR 120 to 259). Baseline characteristics across FMC‐to‐PCI delay intervals are outlined in Table 1. The FMC‐to‐PCI groups were similar in most baseline characteristics, but a numeric increase in treatment with aspirin, clopidogrel, and GPIIb/IIIa‐inhibitors before PCI was observed in patients with longer FMC‐to‐PCI delays. Patients with longer FMC‐to‐PCI delays were also slightly older than patients with shorter FMC‐to‐PCI delay.
Table 1.
Baseline Characteristics of Patients With ST‐Segment Elevation Myocardial Infarction Treated With Primary PCI
| FMC‐to‐PCI Time | Minutes | Patients Not Included in FMC‐to‐PCI Analysis | ||||
|---|---|---|---|---|---|---|
| 0 to 30 | 31 to 60 | 61 to 90 | 91 to 120 | 121 to 360 | ||
| Number of patients | 2237 (16.2%) | 3557 (25.8%) | 3238 (23.4%) | 1934 (14.0%) | 2824 (20.5%) | 7388 |
| Age, mean (SD) | 65.5 (11.8) | 66.1 (11.9) | 66.9 (11.8) | 67.1 (11.8) | 67.2 (12.2) | 66.0 (12) |
| Male sex | 1594 (71.3%) | 2570 (72.3%) | 2317 (71.6%) | 1322 (68.4%) | 1953 (69.2%) | 5290 (71.6%) |
| Smoking status | ||||||
| Never smoked | 812 (36.3%) | 1251 (35.2%) | 1202 (37.1%) | 718 (37.1%) | 1011 (35.8%) | 2457 (33.3%) |
| Previous smoker | 487 (21.8%) | 807 (22.7%) | 797 (24.6%) | 454 (23.5%) | 762 (27.0%) | 1656 (22.4%) |
| Current smoker | 584 (26.1%) | 1093 (30.7%) | 894 (27.6%) | 561 (29.0%) | 749 (26.5%) | 1920 (26.0%) |
| Unknown | 354 (15.8%) | 406 (11.4%) | 345 (10.7%) | 201 (10.4%) | 301 (10.7%) | 1352 (18.3%) |
| Prior diseases | ||||||
| Kidney failure | 23 (1.0%) | 44 (1.2%) | 45 (1.4%) | 30 (1.6%) | 41 (1.5%) | 98 (1.3%) |
| COPD | 154 (6.9%) | 213 (6.0%) | 180 (5.6%) | 124 (6.4%) | 219 (7.8%) | 428 (5.8%) |
| Heart failure | 84 (3.8%) | 129 (3.6%) | 124 (3.8%) | 86 (4.4%) | 119 (4.2%) | 365 (4.9%) |
| Myocardial infarction | 249 (11.1%) | 354 (10.0%) | 366 (11.3%) | 237 (12.3%) | 372 (11.2%) | 1045 (14.1%) |
| Diabetes | 356 (15.9%) | 515 (14.5%) | 500 (15.4%) | 331 (17.1%) | 521 (18.4%) | 1178 (15.9%) |
| Cancer | 46 (2.1%) | 104 (2.9%) | 94 (2.9%) | 50 (2.6%) | 79 (2.8%) | 179 (2.4%) |
| Hypertension | 332 (14.8%) | 525 (14.8%) | 518 (16.0%) | 323 (16.7%) | 470 (16.6%) | 1078 (14.6%) |
| Prior CABG | 62 (2.8%) | 99 (2.8%) | 88 (2.7%) | 44 (2.3%) | 102 (3.6%) | 223 (3.0%) |
| Prior PCI | 152 (6.8%) | 250 (7.0%) | 225 (6.9%) | 137 (7.1%) | 177 (6.3%) | 542 (7.3%) |
| Antithrombotic treatment prior to PCI | ||||||
| Aspirin | 1720 (76.9%) | 2793 (78.6%) | 2713 (83.8%) | 1659 (85.8%) | 2442 (86.5%) | 5559 (75.3%) |
| Clopidogrel | 1229 (54.9%) | 2024 (56.9%) | 2135 (65.9%) | 1365 (70.6%) | 2065 (73.2%) | 3288 (44.8%) |
| Heparin | 440 (19.7%) | 834 (23.5%) | 938 (29.0%) | 499 (25.8%) | 610 (21.6%) | 672 (9.2%) |
| LMWH | 347 (15.5%) | 430 (12.1%) | 344 (10.6%) | 249 (12.9%) | 516 (18.3%) | 1292 (17.5%) |
| GpIIb/IIIa‐inhibitors | 136 (6.1%) | 263 (7.4%) | 432 (13.3%) | 280 (14.5%) | 511 (18.1%) | 659 (9.0%) |
| Angiographic data | ||||||
| Usage of stent | 2105 (94.1%) | 3329 (93.6%) | 2994 (92.5%) | 1779 (92.0%) | 2584 (91.5%) | 6726 (91.0%) |
| Usage of drug eluting stents | 350 (15.6%) | 582 (16.4%) | 604 (18.7%) | 392 (20.3%) | 567 (20.1%) | 1615 (21.9%) |
| Usage of ≥3 stents | 346 (15.4%) | 535 (15.0%) | 491 (15.2%) | 315 (16.3%) | 504 (17.8%) | 1189 (16.1%) |
| Treated vessel | ||||||
| LAD | 938 (41.9%) | 1544 (43.4%) | 1445 (44.6%) | 881 (45.6%) | 1216 (43.1%) | 3247 (44.2%) |
| Cx | 269 (12%) | 458 (12.9%) | 424 (13.1%) | 257 (13.3%) | 450 (16.0%) | 1013 (13.8%) |
| RCA | 974 (43.5%) | 1475 (41.5%) | 1286 (39.7%) | 747 (38.6%) | 1064 (37.7%) | 2836 (38.6%) |
| Other (grafts, LM) | 56 (2.5%) | 79 (2.2%) | 82 (2.5%) | 48 (2.5%) | 91 (3.2%) | 258 (3.5%) |
| Access site | ||||||
| Femoral artery | 1824 (81.5%) | 2795 (78.6%) | 2521 (77.9%) | 1473 (76.2%) | 2190 (77.5%) | 6515 (89%) |
| Right radial artery | 373 (16.7%) | 701 (19.7%) | 625 (19.3%) | 418 (21.6%) | 550 (19.5%) | 393 (5.4%) |
| Other | 40 (1.8%) | 61 (1.7%) | 92 (2.8%) | 43 (2.2%) | 75 (2.7%) | 429 (5.8%) |
| Thrombectomy used | 334 (14.9%) | 585 (16.4%) | 455 (14.1%) | 258 (13.3%) | 370 (13.1%) | 1066 (26.9%) |
CABG indicates coronary artery bypass graft; COPD, chronic obstructive pulmonary disease; Cx, circumflex artery; FMC, first medical contact; LAD, left anterior descending artery; LM, left main stem; LMWH, low‐molecular weight heparin; PCI, percutaneous coronary intervention; RCA, right coronary artery.
Patients not included in the primary analysis of this study were similar to the overall cohort regarding age, sex, smoking status, various comorbidities, and most angiographic data (including infarct territory, usage of drug eluting stents, and number of stents). However, they were to a lesser extent given antithrombotic medications prior to PCI.
FMC‐to‐PCI Delay
Unadjusted 1‐year mortality rates across intervals of FMC‐to‐PCI are shown by Kaplan–Meier curves in Figure 1. Results of adjusted and unadjusted analyses are shown in Table 2. A significant overall association between FMC‐to‐PCI delay and mortality was observed (Table 2). Using time as a continuous variable, a statistically significant association was noted between increasing FMC‐to‐PCI time and 1‐year mortality with a hazard ratio (HR) of 1.06 for every 30 minutes of time delay. When stratifying time in different time cohorts, a statistically significant association between mortality and FMC‐to‐PCI delay was observed already at 1 hour, with HR for 1‐year mortality of 1.26 (61 to 90 minutes, 95% CI: 1.03 to 1.55) compared to the <30 minutes group. Further, significantly increased mortality was noted with increasing FMC‐to‐PCI delays with adjusted HRs for 1‐year mortality of 1.41 (91 to 120 minutes, 95% CI: 1.14 to 1.76) and 1.51 (120 to 360 minutes, 95% CI: 1.23 to 1.86) compared to the <30 minutes group (Table 2).
Figure 1.
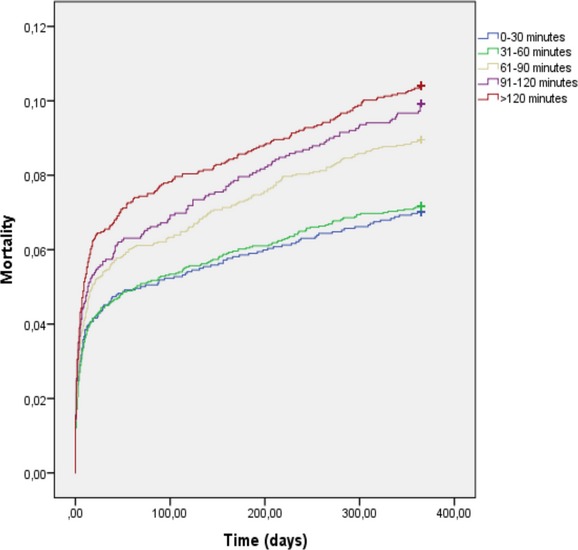
Mortality across intervals of FMC‐to‐PCI delays in the overall patient cohort (Kaplan‐Meier). FMC indicates first medical contact; PCI, percutaneous coronary intervention.
Table 2.
Treatment Delay and 1‐Year Mortality in Patients With ST‐Segment Elevation Myocardial Infarction Treated With Primary PCI
| Patient Group | Delay to PCI (Minutes) | Sample Size | Unadjusted Event Rate (%) | Unadjusted Hazard Ratio (95% CI) | Adjusted Hazard Ratio (95% CI) |
|---|---|---|---|---|---|
| FMC‐to‐PCI, entire cohort | Time as a continuous variable 0 to 360 minutes | 13 790 | 8.6 | 1.06 (1.03 to 1.09)* | 1.06 (1.04 to 1.09)* |
| 0 to 30 | 2237 | 7.0 | 1.00 | 1.00 | |
| 31 to 60 | 3557 | 7.2 | 1.02 (0.84 to 1.25) | 1.08 (0.88 to 1.33) | |
| 61 to 90 | 3238 | 9 | 1.29 (1.06 to 1.56) | 1.26 (1.03 to 1.55) | |
| 91 to 120 | 1934 | 9.9 | 1.43 (1.16 to 1.77) | 1.41 (1.14 to 1.76) | |
| 121 to 360 | 2824 | 10.4 | 1.51 (1.24 to 1.83) | 1.51 (1.23 to 1.86) | |
| FMC‐to‐PCI, patients with a pre‐hospital ECG | Time as a continuous variable 0 to 360 minutes | 7053 | 8.6 | 1.08 (1.04 to 1.13)* | 1.05 (1.01 to 1.10)* |
| 0 to 30 | 520 | 5 | 1.00 | 1.00 | |
| 31 to 60 | 2379 | 7.1 | 1.42 (0.94 to 2.15) | 1.34 (0.88 to 2.05) | |
| 61 to 90 | 2042 | 9.5 | 1.94 (1.29 to 2.92) | 1.57 (1.03 to 2.41) | |
| 91 to 120 | 1015 | 10.2 | 2.10 (1.37 to 3.23) | 1.61 (1.03 to 2.53) | |
| 121 to 360 | 1097 | 10.4 | 2.18 (1.42 to 3.33) | 1.71 (1.10 to 2.67) | |
| Symptom‐to‐PCI, entire cohort | Time as a continuous variable 0 to 480 minutes | 11 489 | 8.3 | 1.06 (1.02 to 1.10)* | 1.05 (1.01 to 1.09)* |
| 0 to 60 | 332 | 5.7 | 1.00 | 1.00 | |
| 61 to 120 | 2567 | 7.2 | 1.26 (0.79 to 2.02) | 1.50 (0.93 to 2.43) | |
| 121 to 180 | 3146 | 8.2 | 1.45 (0.91 to 2.31) | 1.47 (0.92 to 2.35) | |
| 181 to 240 | 2142 | 8.5 | 1.51 (0.94 to 2.42) | 1.45 (0.90 to 2.35) | |
| 241 to 480 | 3302 | 9.2 | 1.63 (1.03 to 2.60) | 1.68 (1.05 to 2.69) |
FMC indicates first medical contact; PCI, percutaneous coronary intervention.
Hazard ratios expressed as mortality/30 minutes of time delay.
Hazard ratios expressed as mortality/60 minutes of time delay.
In the subset of patients with a 3‐year follow‐up (n=6495), results were identical to the overall patient cohort with an increase in mortality (HR 1.06, P<0.001) for every 30 minutes of treatment delay. Additional analyses for 3‐year mortality using time as a categorical variable were not performed due to small sample sizes within individual time categories.
In patients with a pre‐hospital ECG, the results were similar compared to the entire patient cohort with a significant association between FMC‐to‐PCI delay and increased mortality (Table 2). Similar to the overall cohort, a significant association with mortality and adjusted FMC‐to‐PCI time was observed already at 1 hour with a HR of 1.57 (95% CI: 1.03 to 2.41).
FMC‐to‐PCI Delay and Ventricular Dysfunction
In 10 330 patients, information on the left ventricular ejection fraction was recorded before discharge. As shown in Figure 2, FMC‐to‐PCI delay was associated with increased risk of severe left ventricular dysfunction. Using logistic regression, all groups of FMC‐to‐PCI delay exceeding 1 hour showed a statistically significant increase in severe heart failure at discharge compared to the 0 to 30 minutes group, both prior to and after statistical adjustment (Table 3).
Figure 2.
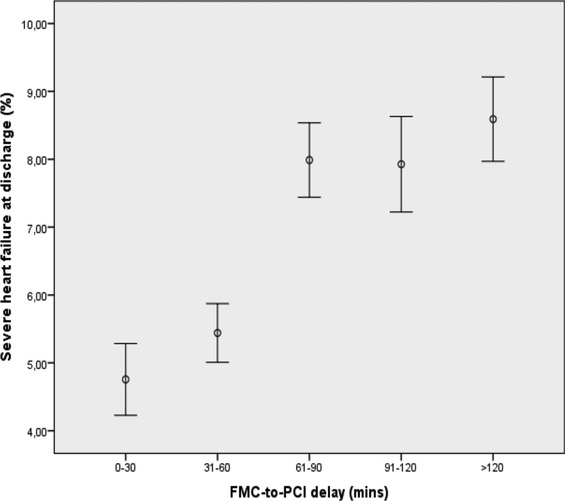
Association between FMC‐to‐PCI delay and severe heart failure at discharge (error bars denote mean with standard error of the mean). FMC indicates first medical contact; PCI, percutaneous coronary intervention.
Table 3.
Odds Ratio for Severe Heart Failure At Discharge Stratified by FMC‐to‐PCI Timings
| Patient Group (Minutes) | Unadjusted Odds Ratio for Severe Heart Failure At Discharge (95% CI) | Adjusted Odds Ratio for Severe Heart Failure at Discharge (95% CI) |
|---|---|---|
| 0 to 30 | 1.00 | 1.00 |
| 31 to 60 | 1.15 (0.87 to 1.53) | 1.11 (0.83 to 1.50) |
| 61 to 90 | 1.74 (1.33 to 2.28) | 1.54 (1.14 to 2.06) |
| 91 to 120 | 1.72 (1.28 to 2.32) | 1.54 (1.12 to 2.12) |
| 121 to 360 | 1.88 (1.43 to 2.48) | 1.70 (1.26 to 2.30) |
FMC indicates first medical contact; PCI, percutaneous coronary intervention.
Symptom‐to‐PCI Delay
Unadjusted 1‐year mortality rates in relation to intervals of symptom‐to‐PCI delay are shown in Figure 3. Using time as a continuous variable a significant overall association between symptom‐to‐PCI delay and mortality was observed both prior to and after statistical adjustment (Table 2). When stratifying time into different time cohorts, only the highest time delay (241 to 480 minutes) from symptom onset to PCI, was statistically significantly associated with increased mortality with a HR of 1.68 (95% CI: 1.05 to 2.69) compared to the <60 minutes time group (Table 2). Furthermore, with increasing symptom‐to‐PCI delays, an incremental increase in adjusted HRs was not observed, in contrast to the FMC‐to‐PCI delay analysis (Table 2). No significant association between increasing treatment delays and 3‐year mortality was observed (HR 1.007 for every hour of treatment delay, P=0.77).
Figure 3.
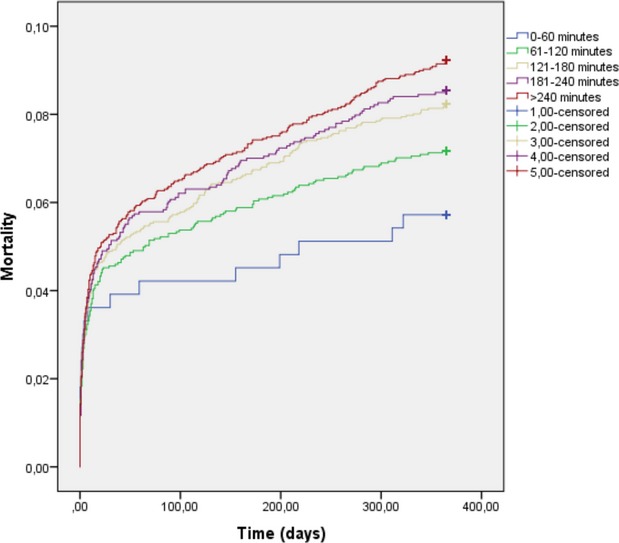
Mortality across intervals of symptom‐to‐PCI delays in the overall patient cohort (Kaplan–Meier). PCI indicates percutaneous coronary intervention.
Other Subgroups
Patients with cardiogenic shock (n=599) did not show any median increase or decrease in FMC‐to‐PCI delay (median 68 minutes, IQR 40 to 110) compared to noncardiogenic shock patients (median 70 minutes, IQR 42 to 110, P=0.43). However, patients with cardiogenic shock had significantly shorter symptom‐to‐PCI timings (median 160 minutes, IQR 102 to 240) compared to noncardiogenic shock patients (median 176 minutes, IQR 122 to 260), P<0.001. Various culprit arteries showed different FMC‐to‐PCI delays with the longest delays for the left circumflex artery (median 75 minutes IQR 45 to 118) compared to the lowest for the right coronary artery (67 minutes IQR 40 to 105, P<0.001). The left circumflex artery also showed the longest symptom‐to‐PCI delay (median 190 minutes IQR 130 to 284). However, the left anterior descending artery showed the shortest symptom‐to‐PCI delay (median 170 minutes IQR 120 to 250), P<0.001.
Discussion
This is the largest register study to date that has examined the association between time from first medical contact to PCI and mortality in STEMI patients. We observed an increase in mortality already after a delay of 1 hour from first medical contact. Furthermore, increasing FMC‐to‐PCI delay was associated with an increasing rate of severe ventricular dysfunction at discharge. Among all modifiable time factors involved in early reperfusion of ST‐elevation myocardial infarction, the time delay between FMC‐to‐PCI is the one where the entire health‐care system can be improved and streamlined.1 This involves early diagnosis with a prehospital ECG, rapid transportation to a PCI‐capable hospital, a minimum of door‐to‐balloon time, and expedient PCI. A FMC‐to‐PCI delay of more than 60 minutes resulted in a statistically significant adjusted increase in mortality ranging from HRs of 1.26 (for 61 to 90 minutes) to 1.51 (121 to 360 minutes). In patients diagnosed with a prehospital ECG the effect was even more pronounced.
The mechanism of why a shorter FMC‐to‐PCI delay is associated with better survival is unclear. For the first time we can report an association between FMC‐to‐PCI time and heart failure at discharge. Our results indicate increased rates of severe ventricular dysfunction at discharge with increasing FMC‐to‐PCI delay (Figure 2 and Table 3). Development of ventricular dysfunction and heart failure in patients with longer FMC‐to‐PCI delay thus constitutes a possible mechanism to explain the increased mortality with longer FMC‐to‐PCI times.
Symptom‐to‐PCI
The relationship between time from symptom onset to PCI and mortality is complex. Patients with more severe disease and worse prognosis could present earlier whereas patients presenting later might have less severe coronary artery disease.16 Younger patients with an overall better prognosis might be more prone to seek medical attention at an earlier notice compared to older patients. Furthermore, the exact timing of symptom onset can be difficult to recall for the patient in the acute setting, especially if the patient has experienced unstable angina prior to STEMI.12 Thus usage of symptom onset‐to‐PCI is an unstable variable with inherent limitations resulting in measurement imprecision. Time delay between first medical contact to PCI is not subject to many of these limitations.12,15
Our results indicated that increasing symptom‐to‐PCI times were associated with an adjusted increase in mortality in the entire studied time interval of 8 hours. However, when studying treatment delay stratified into different time categories, only the highest time delay group (4 to 8 hours) managed to show a statistically significant increase in mortality. There was also no clear observed incremental benefit with increasing time delay after statistical adjustment. In addition, 3‐year survival data showed no statistical significance or even trend for such, for increased mortality with increasing symptom‐to‐PCI times. However, patients with cardiogenic shock presented significantly earlier than patients without cardiogenic shock. Patients with an , left anterior descending artery ‐lesion also presented earlier, suggesting that patients with more severe disease are more likely to be early presenters, reinforcing the limitations of symptom‐to‐PCI as the metric of choice in determining benefits of early reperfusion.
Previous Studies and Current Guidelines
Previous studies have focused mainly on symptom‐to‐PCI delays. Data from 2 German studies reported no reduction in infarct size with primary PCI with decreasing symptom‐to‐PCI.2,6 However, other studies have described significant reductions in infarct size with decreasing symptom‐to‐PCI delays.7–9 Improved mortality with decreasing symptom‐to‐PCI delays has been described.11 However, other studies have shown limited to no effect on mortality with short symptom‐to‐PCI delays.13–14 Thus previous studies using symptom‐to‐PCI as a primary measure of time to treatment have been inconsistent with each other both regarding infarct size and clinical outcomes. Several other studies have focused mainly on door‐to‐balloon time and shown convincing data regarding improved clinical outcomes with decreasing door‐to‐balloon times.13,17–19 However, door‐to‐balloon time only focuses on the final part of the health‐care chain leaving out critical care elements where improvements can be done.
A previous study instead using FMC‐to‐PCI delay showed a significant and linear association with increased mortality with increasing FMC‐to‐PCI delay, whereas no statistically significant association between increasing symptom‐to‐PCI delay and mortality was observed.12 These findings are consistent with our results. However, the study did not have sufficient statistical power to determine whether a specific increase in mortality existed already after the first hour.12 Our larger sample size allowed detection of a difference in adjusted mortality already at FMC‐to‐PCI delays exceeding 1 hour, indicating that the concept of a “golden hour” of opportunity established in the fibrinolysis era, holds true also for primary PCI. Our findings thus reinforce the current European Society of Cardiology guidelines on STEMI which state that a delay of 60 minutes or less from first medical contact to PCI is desirable, and that a timing of 90 minutes should be regarded as a maximum.1 However, in the recent ACCF/AHA guidelines, a goal of 90 minutes from FMC‐to‐PCI is recommended.26 A FMC‐to‐PCI time goal of less than 60 minutes would, according to our findings, result in reduced mortality compared to a goal of 90 minutes. Our data are strictly limited to STEMI patients undergoing primary PCI and if decreasing FMC‐to‐PCI times with thrombolysis would show similar results is unknown to us.
Some studies indicate excess mortality of STEMI patients when treated in low volume centers and therefore there is currently a drive to centralization of STEMI centers to a few high‐volume geographical locations.27 However, this process should take FMC‐to‐PCI delay into account, such that the potential benefit of having only a few albeit high volume centers should not be offset by high FMC‐to‐PCI delays. Striking the right balance in availability versus higher volume will be of utmost importance and should be factored in economic and political health‐care drafts and discussions.
Limitations
Our data are observational and thus some degree of residual confounding cannot be excluded. Furthermore, for patient selection, 6209 patients did not have a recorded time of first medical contact and were excluded from the FMC‐to‐PCI analysis. A total of 6360 patients did not have a symptom onset recorded and were excluded from the symptom‐to‐PCI analysis, potentially inducing some degree of selection bias. The estimation of first medical contact was determined by the time of first ECG taken which, although ECG should be taken promptly, could underestimate the total FMC‐to‐PCI time. The time of PCI was determined by the start of the coronary angiography since data on time of first wiring or balloon inflation were not available.
Conclusions
Our study constitutes the largest study to date to examine the effects of FMC‐to‐PCI delay and mortality in patients with STEMI undergoing primary PCI. FMC‐to‐PCI delay was significantly associated with increased mortality when exceeding 1 hour. The mechanism behind the increased mortality could partially be attributed to increased rates of severe heart failure at discharge. These data suggest that the concept of a “golden hour” also applies to primary PCI for STEMI which should be taken into consideration for future guidelines and in the planning of health care organization.
Sources of Funding
This work was supported by funding from the Swedish Heart and Lung Foundation and Swedish Medical Research Council (521‐2009‐2276).
Disclosures
None.
References
- 1.Steg PG, James SK, Atar D, Badano LP, Lundqvist CB, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez‐Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, Van't Hof A, Widimsky P, Zahger D, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck‐Brentano C, Hasdai D, Hoes A, Kirchhof P, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Astin F, Astrom‐Olsson K, Budaj A, Clemmensen P, Collet JP, Fox KA, Fuat A, Gustiene O, Hamm CW, Kala P, Lancellotti P, Maggioni AP, Merkely B, Neumann FJ, Piepoli MF, Van de Werf F, Verheugt F, Wallentin L. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation: the task force on the management of ST‐segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J. 2012; 33:2569-2619 [DOI] [PubMed] [Google Scholar]
- 2.Schomig A, Ndrepepa G, Mehilli J, Schwaiger M, Schuhlen H, Nekolla S, Pache J, Martinoff S, Bollwein H, Kastrati A. Therapy‐dependent influence of time‐to‐treatment interval on myocardial salvage in patients with acute myocardial infarction treated with coronary artery stenting or thrombolysis. Circulation. 2003; 108:1084-1088 [DOI] [PubMed] [Google Scholar]
- 3.Thiele H, Kappl MJ, Linke A, Erbs S, Boudriot E, Lembcke A, Kivelitz D, Schuler G. Influence of time‐to‐treatment, TIMI‐flow grades, and ST‐segment resolution on infarct size and infarct transmurality as assessed by delayed enhancement magnetic resonance imaging. Eur Heart J. 2007; 28:1433-1439 [DOI] [PubMed] [Google Scholar]
- 4. Prehospital thrombolytic therapy in patients with suspected acute myocardial infarction. The European Myocardial Infarction Project Group. N Engl J Med. 1993; 329:383-389 [DOI] [PubMed] [Google Scholar]
- 5.Morrison LJ, Verbeek PR, McDonald AC, Sawadsky BV, Cook DJ. Mortality and prehospital thrombolysis for acute myocardial infarction: a meta‐analysis. JAMA. 2000; 283:2686-2692 [DOI] [PubMed] [Google Scholar]
- 6.Hahn JY, Song YB, Gwon HC, Choe YH, Kim JH, Sung J, Choi SH, Choi JH, Kim DK, Hong KP, Park JE, Lee SH. Relation of left ventricular infarct transmurality and infarct size after primary percutaneous coronary angioplasty to time from symptom onset to balloon inflation. Am J Cardiol. 2008; 102:1163-1169 [DOI] [PubMed] [Google Scholar]
- 7.Brodie BR, Webb J, Cox DA, Qureshi M, Kalynych A, Turco M, Schultheiss HP, Dulas D, Rutherford B, Antoniucci D, Stuckey T, Krucoff M, Gibbons R, Lansky A, Na Y, Mehran R, Stone GW. Impact of time to treatment on myocardial reperfusion and infarct size with primary percutaneous coronary intervention for acute myocardial infarction (from the EMERALD Trial). Am J Cardiol. 2007; 99:1680-1686 [DOI] [PubMed] [Google Scholar]
- 8.Francone M, Bucciarelli‐Ducci C, Carbone I, Canali E, Scardala R, Calabrese FA, Sardella G, Mancone M, Catalano C, Fedele F, Passariello R, Bogaert J, Agati L. Impact of primary coronary angioplasty delay on myocardial salvage, infarct size, and microvascular damage in patients with ST‐segment elevation myocardial infarction: insight from cardiovascular magnetic resonance. J Am Coll Cardiol. 2009; 54:2145-2153 [DOI] [PubMed] [Google Scholar]
- 9.Eitel I, Desch S, Fuernau G, Hildebrand L, Gutberlet M, Schuler G, Thiele H. Prognostic significance and determinants of myocardial salvage assessed by cardiovascular magnetic resonance in acute reperfused myocardial infarction. J Am Coll Cardiol. 2010; 55:2470-2479 [DOI] [PubMed] [Google Scholar]
- 10.Tarantini G, Cacciavillani L, Corbetti F, Ramondo A, Marra MP, Bacchiega E, Napodano M, Bilato C, Razzolini R, Iliceto S. Duration of ischemia is a major determinant of transmurality and severe microvascular obstruction after primary angioplasty: a study performed with contrast‐enhanced magnetic resonance. J Am Coll Cardiol. 2005; 46:1229-1235 [DOI] [PubMed] [Google Scholar]
- 11.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004; 109:1223-1225 [DOI] [PubMed] [Google Scholar]
- 12.Terkelsen CJ, Sorensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010; 304:763-771 [DOI] [PubMed] [Google Scholar]
- 13.Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ. Relationship of symptom‐onset‐to‐balloon time and door‐to‐balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000; 283:2941-2947 [DOI] [PubMed] [Google Scholar]
- 14.Brodie BR, Stone GW, Morice MC, Cox DA, Garcia E, Mattos LA, Boura J, O'Neill WW, Stuckey TD, Milks S, Lansky AJ, Grines CL. Importance of time to reperfusion on outcomes with primary coronary angioplasty for acute myocardial infarction (results from the stent primary angioplasty in myocardial infarction trial). Am J Cardiol. 2001; 88:1085-1090 [DOI] [PubMed] [Google Scholar]
- 15.Terkelsen CJ, Sorensen JT, Nielsen TT. Is there any time left for primary percutaneous coronary intervention according to the 2007 updated American College of Cardiology/American Heart Association ST‐segment elevation myocardial infarction guidelines and the D2B alliance? J Am Coll Cardiol. 2008; 52:1211-1215 [DOI] [PubMed] [Google Scholar]
- 16.Lowel H, Lewis M, Hormann A. [Prognostic significance of prehospital phase in acute myocardial infarct. Results of the Augsburg Myocardial Infarct Registry, 1985–1988]. Dtsch Med Wochenschr. 1991; 116:729-733 [DOI] [PubMed] [Google Scholar]
- 17.Brodie BR, Grines CL, Stone GW. Effect of door‐to‐balloon time on patient mortality. J Am Coll Cardiol. 2006; 48:2600. [DOI] [PubMed] [Google Scholar]
- 18.Blankenship JC, Scott TD, Skelding KA, Haldis TA, Tompkins‐Weber K, Sledgen MY, Donegan MA, Buckley JW, Sartorius JA, Hodgson JM, Berger PB. Door‐to‐balloon times under 90 min can be routinely achieved for patients transferred for ST‐segment elevation myocardial infarction percutaneous coronary intervention in a rural setting. J Am Coll Cardiol. 2011; 57:272-279 [DOI] [PubMed] [Google Scholar]
- 19.Muller UM, Eitel I, Eckrich K, Erbs S, Linke A, Mobius‐Winkler S, Mende M, Schuler GC, Thiele H. Impact of minimising door‐to‐balloon times in ST‐elevation myocardial infarction to less than 30 min on outcome: an analysis over an 8‐year period in a tertiary care centre. Clin Res Cardiol. 2011; 100:297-309 [DOI] [PubMed] [Google Scholar]
- 20. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. The GUSTO Investigators. N Engl J Med. 1993; 329:673-682 [DOI] [PubMed] [Google Scholar]
- 21. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic therapy trialists' (FTT) collaborative group. Lancet. 1994; 343:311-322 [PubMed] [Google Scholar]
- 22.Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996; 348:771-775 [DOI] [PubMed] [Google Scholar]
- 23.Hedstrom E, Engblom H, Frogner F, Astrom‐Olsson K, Ohlin H, Jovinge S, Arheden H. Infarct evolution in man studied in patients with first‐time coronary occlusion in comparison to different species—implications for assessment of myocardial salvage. J Cardiovasc Magn Reson. 2009; 11:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ludvigsson JF, Otterblad‐Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009; 24:659-667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Otterblad Olausson P. External review and validation of the Swedish National Inpatient Register. BMC Public Health. 2011; 11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz CB, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis‐Holland JE, Tommaso JE, Tracy CM, Woo YJ, Zhao DX. 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2013; 127:529-555 [DOI] [PubMed] [Google Scholar]
- 27.Srinivas VS, Hailpern SM, Koss E, Monrad ES, Alderman MH. Effect of physician volume on the relationship between hospital volume and mortality during primary angioplasty. J Am Coll Cardiol. 2009; 53:574-579 [DOI] [PubMed] [Google Scholar]


