Abstract
Background
The strategy to place public‐access automated external defibrillators (AEDs) has not yet been established in real settings.
Methods and Results
This, prospective, population‐based observational study in Osaka, Japan, included consecutive out‐of‐hospital cardiac arrest (OHCA) patients with resuscitation attempts during 7 years, from January 2005 through December 2011. The trends in the proportion of public‐access AED use and 1‐month survival with neurologically favorable outcome were evaluated by location. Factors associated with neurologically favorable outcome (defined as cerebral performance category 1 or 2) after ventricular fibrillation were also assessed using multiple logistic regression analysis. A total of 9453 bystander‐witnessed OHCAs of cardiac origin were documented and 894 (9.5%) of them occurred at public places. The proportion of public‐access AED use significantly increased from 0.0% (0/20) in 2005 to 41.2% (7/17) in 2011 at railway stations and from 0.0% (0/7) to 56.5% (13/23) at sports facilities. Mean time from collapse to shock was 5.0 minutes among those who received shocks with public‐access AEDs. The proportion of neurologically favorable outcome was 28.0% (33/118) at railway stations, 51.6% (48/93) at sports facilities, 23.3% (20/86) in public buildings, and 41.9% (13/31) in schools. In multivariate analysis, early defibrillation, irrespective of bystander or emergency medical service (EMS) personnel, was significantly associated with neurologically favorable outcome (adjusted odds ratio for 1‐minute increment, 0.89; 95% confidence interval, 0.87 to 0.92).
Conclusions
This large, population‐based OHCA registry demonstrated that earlier shock, irrespective the shock provider (bystander or EMS personnel), contributed to improving outcome, and a public‐access defibrillation program was successfully implemented so that shocks with public‐access AEDs were delivered to over 40% of bystander‐witnessed OHCAs and time to shock was shortened in some kinds of public places.
Keywords: automated external defibrillator; cardiac arrest; cardiopulmonary resuscitation; death, sudden; epidemiology
Introduction
Sudden cardiac arrest is one of the major public health problems in the industrialized world.1 More than 60 000 events occur annually in out‐of‐hospital settings in Japan, but survival is still low.2 Earlier defibrillation by laypersons plays a key role to improve survival after out‐of‐hospital cardiac arrest (OHCA).1,3–5 In Japan, public use of automated external defibrillators (AEDs) was legally permitted in July 2004, and the number of public‐access AEDs (≈297 000 in 2011) has been widely disseminated.6
OHCAs occurring in public places are more likely to be witnessed by laypersons, and survival was greater than in nonpublic places.7–10 Some studies showed that dissemination of public‐access AEDs in public places produced an increased survival after OHCA.11–12 However, the rate of public‐access AED use differs by location.12–13 Previous studies have proposed some ideas as to where to place public‐access AEDs,10,14–16 but the strategy has not yet been established in an actual community setting.
Currently, Japan is one of the most developed countries in the world where the public‐access defibrillation (PAD) program is widespread. The Utstein Osaka Project is a large, prospective, population‐based OHCA registry in Osaka, Japan, covering approximately 8.8 million residents.17 During the 7 years from 2005 through 2011, there were ≈9500 bystander‐witnessed and resuscitation‐attempted OHCAs of presumed cardiac origin. Using this database, we aimed to assess the current situation of PAD and outcomes after OHCA by location.
Methods
Study Design, Setting, and Population
The Utstein Osaka Project enrolled all patients who suffered an OHCA of cardiac origin, were witnessed by bystanders, treated by emergency medical service (EMS) personnel, and then transported to medical institutions in Osaka Prefecture, Japan, based on the standardized Utstein style.18 The period of this study was from January 1, 2005 through December 31, 2011. This study was approved by the ethics committees of the Kyoto University Graduate School of Medicine. The requirement of giving individual informed consent for the reviews of patients' outcomes was waived by the Personal Information Protection Law and the national research ethics guidelines of Japan.
Cardiac arrest was defined as the cessation of cardiac mechanical activity, as confirmed by the absence of signs of circulation.18 The arrest was presumed to be of cardiac origin unless it was caused by cerebrovascular disease, respiratory disease, malignant tumors, external factors, including trauma, hanging, drowning, drug overdose, and asphyxia, or any other noncardiac factor. The cardiac or noncardiac origin was clinically determined by the physician in charge, in collaboration with the EMS personnel.
EMS Systems in Osaka
Osaka Prefecture, which is the largest urban community in western Japan, has an area of 1892 km2 and a population of ≈8.8 million. The EMS system is operated by 34 fire stations with a corresponding number of emergency dispatch centers, single tiered in 32 stations and 2 tiered (paramedics followed by physicians) in 2 stations. The emergency services are available 24 hours every day. The free emergency telephone number 119 is used to call for an ambulance from anywhere in Japan. When called, an ambulance is dispatched from the nearest fire station. Usually, each ambulance has a crew of 3 emergency providers including at least 1 emergency life‐saving technician (ELST), the highly trained prehospital emergency care providers. They were allowed to insert an intravenous line and an adjunct airway and to use a semiautomated defibrillator for OHCA patients. Specially trained ELSTs were permitted to insert tracheal tubes in July 2004 and to administer intravenous epinephrine in April 2006. All EMS providers perform cardiopulmonary resuscitation (CPR) according to the Japanese CPR guidelines.5,19
Do‐not‐resuscitate orders or living wills are not generally accepted in Japan. EMS providers are not permitted to terminate resuscitation in the field. Therefore, all patients suffering OHCA who were treated by EMS personnel were transported to a hospital and registered in this cohort, excluding cases of decapitation, incineration, decomposition, rigor mortis, or dependent cyanosis.
Dissemination of Public‐Access AEDs and CPR Training in Osaka
PAD programs started in July 2004 in Japan. The cumulative number of public‐access AEDs increased from 713 in 2005 to 17 688 in 2011 in Osaka.6 Although no complete AED location data have been available in this region, the voluntary AED registry in Osaka (Osaka AED Map)20 showed that 31% of public‐access AEDs were deployed in schools, 13% in workplaces, and 5% in public transportation facilities, such as railway stations. In Osaka, CPR training programs, including chest compressions, rescue breathing, and AED operation, have been offered to ≈140 000 citizens annually by local fire departments, the Japan Red Cross, Inc., and the Osaka Life Support Association during the study period.2
Data Collection and Quality Control
Data were collected prospectively using a data form based on the Utstein‐style guidelines for reporting OHCAs,18 including sex, age, first documented cardiac rhythm, witness status, location of arrest, activity of daily living (ADL) before arrests, time course of resuscitation, bystander‐initiated CPR, public‐access AED use, intubation, and epinephrine administration, as well as prehospital return of spontaneous circulation (ROSC), total ROSC, 1‐month survival, and neurological status 1 month after the event. A series of EMS times of call receipt, vehicle arrival at the scene, contact with patients, initiation of CPR, defibrillation by EMS, and hospital arrival were recorded automatically at the dispatch center. First documented rhythm was recorded and diagnosed by the EMS personnel with semiautomated defibrillators on the scene and confirmed by the physician who was responsible for the online medical direction. When shocks were delivered using a public‐access AED, the victims' first documented rhythm was regarded as ventricular fibrillation (VF). Both bystander‐initiated chest compression‐only and conventional CPR with rescue breathing were considered as bystander CPR. The time of collapse and initiation of bystander CPR and public‐access AED use was obtained by EMS interview with the bystander or public‐access AED records before leaving the scene. EMS personnel manually synchronized the defibrillation time data obtained from public‐access AEDs in time with other reported events during resuscitation as accurately as possible after going back to fire departments. The time of defibrillation by EMS personnel was recorded in the semiautomated defibrillator. The time interval from collapse to first shock was defined as the shorter time from collapse to shock by bystanders and that by EMS personnel.
The data form was filled out by the EMS personnel in cooperation with the physicians in charge of the patient, transferred to the Information Center for Emergency Medical Services of Osaka, and then checked by the investigators. If the data sheet was incomplete, the relevant EMS personnel were contacted and questioned, and the data sheet was completed.
All survivors were followed up for up to 1 month after the event by the EMS personnel in charge. Neurological outcome was determined by the physician responsible for the care of the patient, using the Cerebral Performance Category (CPC) scale: category 1, good cerebral performance; category 2, moderate cerebral disability; category 3, severe cerebral disability; category 4, coma or vegetative state; and category 5, death.18 The primary outcome measure was 1‐month survival with neurologically favorable outcome. Neurologically favorable outcome was defined as CPC 1 or 2.18 Secondary outcome measures included prehospital ROSC, total ROSC, admission to hospital, and 1‐month survival.
Statistical Analysis
Patient and EMS characteristics of bystander‐witnessed OHCAs of cardiac origin and their outcomes were compared between the groups using ANOVA for numerical variables and chi‐square test or Fisher's exact test for categorical variables by location of arrests. First, OHCA locations were divided into the following 6 groups; home; streets; workplaces; public places; healthcare facilities; and others. Others included areas such as car inferiors, parking areas, prisons, and rice fields. Next, public places were further divided into public buildings, railway stations, airports, sports facilities, schools, and other public spaces. Other public spaces included areas such as Japanese pinball parlors, shopping malls, and public bathhouses. The trends in the proportion of public‐access AED use in public places were analyzed with the use of univariate regression models. Multivariate logistic regression analysis was applied to assess the factors associated with better neurological outcome among out‐of‐hospital VF patients, and adjusted odds ratios (AORs) and their 95% confidence intervals (CIs) were calculated. As potential confounders, factors that were biologically essential and considered to be associated with clinical outcomes were taken in the multivariable analyses. These variables included age (children aged 0 to 17 years, adults aged 18 to 64 years, and elderly aged ≥65 years), sex (male, female), ADL before arrests (none, good defined as having ability to perform common ADLs without assistance by other persons), type of bystander‐initiated CPR (none, chest compression‐only CPR, or conventional CPR with rescue breathing), public‐access AED use (no, yes), location of arrests (the 11 categories described above), the time interval from collapse to first shock, and year of arrest. Multivariate logistic regression analysis using the time interval from call instead of collapse time, which was estimated by bystanders, was also conducted as a sensitive analysis, because it was reported that clinical time estimates by patients and bystanders was unreliable.21 All of the tests were 2 tailed, and P values of <0.05 was considered statistically significant. All statistical analyses were performed using the SPSS statistical package (ver16.0J; SPSS, Inc., Chicago, IL).
The authors had full access to the data and take responsibility for its integrity. All authors have read and agree to the manuscript as written.
Results
Figure 1 shows an overview of the study patients based on the Utstein template. A total of 48 760 arrests were documented during these 7 years. Resuscitation was attempted in 44 787, and 28 706 were presumed of cardiac origin. Excluding 17 042 victims who were not witnessed and 2211 witnessed by EMS (arrests after EMS arrival), 9453 witnessed by bystanders were eligible for our analyses. Among these arrests, 6190 occurred at home (65.5%), 1108 in healthcare facilities (11.7%), 894 in public places (9.5%), 652 on streets (6.9%), 306 at workplaces (3.2%), and 303 others (3.2%). Among public places, 118 (1.2%) occurred at railway stations, 93 (1.0%) at sports facilities, 86 (0.9%) in public buildings, 31 (0.3%) at schools, 4 (0.04%) at airports, and 562 (5.9%) in other public spaces.
Figure 1.
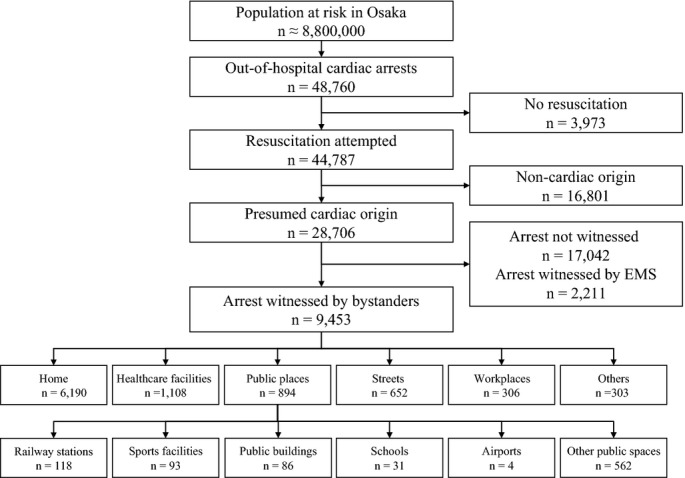
Overview of emergency medical service (EMS)‐treated cardiac arrests with an abridged Utstein template from January 1, 2005 to December 31, 2011. EMS indicates emergency medical service.
Patient and EMS characteristics of bystander‐witnessed OHCAs of cardiac origin according to the OHCA location are shown in Table 1 and their outcomes in Table 2. The proportion of public‐access AED use by laypersons was 0.02% (1/6190) at home, 1.8% (20/1108) in healthcare facilities, 12.8% (114/894) in public places, 2.1% (14/652) on streets, 5.2% (16/306) at workplaces, and 3.0% (9/303) others. Among those who received shocks with public‐access AEDs, mean time interval from collapse to shock was 5.0 minutes. The proportion of 1‐month survival with neurologically favorable outcome was 5.4% (332/6190) at home, 2.6% (29/1108) in healthcare facilities, 20.8% (179/863) in public places, 15.3% (100/652) on streets, 22.2% (68/306) at workplaces, and 8.6% (26/303) at others.
Table 1.
Patient and EMS Characteristics of Bystander‐Witnessed Out‐of‐Hospital Cardiac Arrest of Cardiac Origin According to the Location
| Home (n=6190) | Healthcare Facilities (n=1108) | Public Places (n=894) | Streets (n=652) | Workplaces (n=306) | Others (n=303) | P Value* | |
|---|---|---|---|---|---|---|---|
| Age, y, mean (SD) | 73.0 (15.2) | 85.3 (9.3) | 63.3 (15.8) | 66.7 (13.3) | 56.1 (11.2) | 65.7 (16.0) | <0.001 |
| Age group, n (%) | <0.001 | ||||||
| Children aged 0 to 17 years | 32 (0.5) | 1 (0.1) | 20 (2.2) | 4 (0.6) | 1 (0.3) | 1 (0.3) | |
| Adults aged 18 to 64 years | 1422 (23.0) | 27 (2.4) | 398 (44.5) | 256 (39.3) | 238 (77.8) | 132 (43.6) | |
| Elderly aged ≥65 years | 4736 (76.5) | 1080 (97.5) | 476 (53.2) | 392 (60.1) | 67 (21.9) | 170 (56.1) | |
| Male, n (%) | 3866 (62.5) | 362 (32.7) | 712 (79.6) | 497 (76.2) | 285 (93.1) | 238 (78.5) | <0.001 |
| Good activities of daily living, n (%) | 4312 (69.7) | 292 (26.4) | 766 (85.7) | 514 (78.8) | 298 (97.4) | 241 (79.5) | <0.001 |
| First documented rhythm, % | <0.001 | ||||||
| VF | 1135 (18.3) | 90 (8.1) | 449 (50.2) | 271 (41.6) | 180 (58.8) | 106 (35.0) | |
| PEA | 2134 (34.5) | 393 (35.5) | 224 (25.1) | 211 (32.4) | 81 (26.5) | 80 (26.4) | |
| Asystole | 2838 (45.8) | 596 (53.8) | 205 (22.9) | 160 (24.5) | 43 (14.1) | 111 (36.6) | |
| Others | 83 (1.3) | 29 (2.6) | 16 (1.8) | 10 (1.5) | 2 (0.7) | 6 (2.0) | |
| Public‐access AED use, n (%) | 1 (0.02) | 20 (1.8) | 114 (12.8) | 14 (2.1) | 16 (5.2) | 9 (3.0) | <0.001 |
| Type of bystander CPR, n (%) | <0.001 | ||||||
| No CPR | 4063 (65.6) | 258 (23.3) | 468 (52.3) | 457 (70.1) | 152 (49.7) | 176 (58.1) | |
| Chest compression‐only CPR | 1362 (22.0) | 418 (37.7) | 238 (26.6) | 127 (19.5) | 101 (33.0) | 84 (27.7) | |
| Conventional CPR with rescue breathing | 765 (12.4) | 432 (39.0) | 188 (21.0) | 68 (10.4) | 53 (17.3) | 43 (14.2) | |
| Intubation, n (%) | 1617 (26.1) | 270 (24.4) | 202 (22.6) | 145 (22.2) | 61 (19.9) | 69 (22.8) | 0.011 |
| Epinephrine, n (%) | 997 (16.1) | 166 (15.0) | 151 (16.9) | 125 (19.2) | 67 (21.9) | 52 (17.2) | 0.027 |
| Collapse to call, min, mean (SD) | 4.8 (6.8) | 4.8 (6.0) | 3.2 (4.2) | 2.8 (5.1) | 2.9 (4.0) | 3.4 (5.2) | <0.001 |
| Collapse to shocks by public‐access AEDs, min, mean (SD)* | 9.0 (NA) | 4.9 (4.9) | 5.0 (3.1) | 4.8 (2.3) | 5.9 (2.7) | 6.1 (3.4) | 0.309 |
| Call to contact with patients by EMS (EMS activation time), min, mean (SD) | 7.8 (2.6) | 7.8 (2.6) | 7.2 (2.8) | 6.6 (2.5) | 7.7 (3.0) | 7.9 (4.3) | <0.001 |
| Collapse to first shocks by bystanders or EMS, min, mean (SD)* | 11.0 (4.6) | 9.4 (6.8) | 9.0 (4.6) | 9.0 (4.3) | 9.8 (4.5) | 10.3 (4.4) | <0.001 |
| Collapse to CPR by EMS, min, mean (SD) | 11.0 (7.1) | 10.3 (6.6) | 9.5 (5.3) | 8.3 (5.0) | 9.4 (5.2) | 10.0 (5.8) | <0.001 |
| Collapse to hospital arrival, min, mean (SD) | 31.6 (9.8) | 29.4 (10.0) | 28.9 (8.8) | 25.2 (8.1) | 30.0 (8.7) | 29.4 (9.9) | <0.001 |
AED indicates automated external defibrillator; CPR, cardiopulmonary resuscitation; EMS, emergency medical services; NA, not analysis; PEA, pulseless electrical activity; SD, standard deviation; VF, ventricular fibrillation.
P values are calculated to test the homogeneity among the 6 location groups.
Calculated for cases with time data on public‐access AEDs.
Calculated for cases with VF as first documented rhythm.
Table 2.
Outcomes After Bystander‐Witnessed Out‐of‐Hospital Cardiac Arrest of Cardiac Origin According to the Location
| Homes (n=6190) | Healthcare Facilities (n=1108) | Public Places (n=863) | Streets (n=652) | Workplaces (n=306) | Others (n=303) | P Value* | |
|---|---|---|---|---|---|---|---|
| Prehospital ROSC, n (%) | 797 (12.9) | 102 (9.2) | 233 (27.0) | 143 (21.9) | 86 (28.1) | 41 (13.5) | <0.001 |
| Total ROSC, n (%) | 2549 (41.2) | 398 (35.9) | 477 (55.3) | 351 (53.8) | 162 (52.9) | 122 (40.3) | <0.001 |
| Hospital admission, n (%) | 2113 (34.1) | 321 (29.0) | 429 (49.7) | 314 (48.2) | 158 (51.6) | 108 (35.6) | <0.001 |
| 1‐month survival, n (%) | 620 (10.0) | 57 (5.1) | 267 (31.0) | 173 (26.5) | 98 (32.0) | 49 (16.2) | <0.001 |
| Neurologically favorable outcome, n (%) | 332 (5.4) | 29 (2.6) | 179 (20.8) | 100 (15.3) | 68 (22.2) | 26 (8.6) | <0.001 |
ROSC indicates return of spontaneous circulation.
P values are calculated to test the homogeneity among the 6 location groups.
Patient and EMS characteristics of OHCA in public places are shown in Table 3 and their outcomes in Table 4. The proportion of public‐access AED use was 27.1% (32/118) at railway stations, 45.2% (42/93) at sports facilities, 11.6% (10/86) in public buildings, 25.8% (8/31) at schools, 50.0% (2/4) at airports, and 3.6% (20/562) in other public spaces. The proportion of neurologically favorable outcome was 28.0% (33/118) at railway stations, 51.6% (48/93) at sports facilities, 23.3% (20/86) in public buildings, 41.9% (13/31) at schools, 50.0% (2/4) at airports, and 13.6% (76/562) in other public spaces.
Table 3.
Patient and EMS Characteristics of Bystander‐Witnessed Out‐of‐Hospital Cardiac Arrest of Cardiac Origin at Public Places According to the Location
| Railway Stations (n=118) | Sports Facilities (n=93) | Public Buildings (n=86) | Schools (n=31) | Airports (n=4) | Other Public Spaces (n=562) | P Value* | |
|---|---|---|---|---|---|---|---|
| Age, y, mean (SD) | 62.7 (14.0) | 61.1 (15.8) | 63.0 (17.9) | 41.4 (25.4) | 56.8 (16.3) | 65.1 (14.1) | <0.001 |
| Age group, n (%) | |||||||
| Children aged 0 to 17 years | 1 (0.8) | 2 (2.2) | 4 (4.7) | 8 (25.8) | 0 (0.0) | 5 (0.9) | <0.001 |
| Adults aged 18 to 64 years | 60 (50.8) | 41 (44.1) | 32 (37.2) | 16 (51.6) | 2 (50.0) | 247 (44.0) | |
| Elderly aged ≥65 years | 57 (48.3) | 50 (53.8) | 50 (58.1) | 7 (22.6) | 2 (50.0) | 310 (55.2) | |
| Male, n (%) | 93 (78.8) | 77 (82.8) | 67 (77.9) | 24 (77.4) | 4 (100.0) | 447 (79.5) | 0.880 |
| Good activities of daily living, n (%) | 101 (85.6) | 92 (98.9) | 72 (83.7) | 30 (96.8) | 4 (100.0) | 467 (83.1) | 0.002 |
| First documented rhythm, % | 0.001 | ||||||
| VF | 79 (66.9) | 65 (69.9) | 41 (47.7) | 26 (83.9) | 3 (75.0) | 235 (41.8) | |
| PEA | 18 (15.3) | 15 (16.1) | 18 (20.9) | 3 (9.7) | 1 (25.0) | 169 (30.1) | |
| Asystole | 18 (15.3) | 11 (11.8) | 24 (27.9) | 1 (3.2) | 0 (0.0) | 151 (26.9) | |
| Others | 3 (2.5) | 2 (2.2) | 3 (3.5) | 1 (3.2) | 0 (0.0) | 7 (1.2) | |
| Public‐access AED use, n (%) | 32 (27.1) | 42 (45.2) | 10 (11.6) | 8 (25.8) | 2 (50.0) | 20 (3.6) | <0.001 |
| Type of bystander CPR, n (%) | <0.001 | ||||||
| No CPR | 44 (37.3) | 30 (32.3) | 41 (47.7) | 7 (22.6) | 0 (0) | 346 (61.6) | |
| Chest compression‐only CPR | 49 (41.5) | 25 (26.9) | 22 (25.6) | 7 (22.6) | 2 (50.0) | 133 (23.7) | |
| Conventional CPR with rescue breathing | 25 (21.2) | 38 (40.9) | 23 (26.7) | 17 (54.8) | 2 (50.0) | 83 (14.8) | |
| Intubation, n (%) | 26 (22.0) | 15 (16.1) | 21 (24.4) | 9 (29.0) | 1 (25.0) | 130 (23.1) | 0.058 |
| Epinephrine, n (%) | 18 (15.3) | 15 (16.1) | 17 (19.8) | 0 (0.0) | 0 (0.0) | 101 (18.0) | 0.020 |
| Collapse to call, min, mean (SD) | 2.8 (2.6) | 2.8 (2.6) | 3.3 (4.6) | 3.7 (3.7) | 3.5 (1.7) | 3.3 (4.6) | 0.811 |
| Collapse to shocks by public‐access AEDs, min, mean (SD)* | 5.7 (3.4) | 4.4 (2.5) | 4.3 (3.4) | 4.1 (2.0) | 6.0 (NA) | 6.0 (3.8) | 0.327 |
| Call to contact with patients by EMS (EMS activation time), min, mean (SD) | 7.5 (2.3) | 8.2 (3.7) | 6.6 (2.8) | 7.4 (3.0) | 7.0 (5.0) | 7.1 (2.7) | 0.004 |
| Collapse to first shocks by bystanders or EMS, min, mean (SD)* | 9.1 (4.7) | 5.9 (3.8) | 8.6 (4.4) | 9.1 (5.5) | 6.5 (0.7) | 9.9 (4.4) | <0.001 |
| Collapse to CPR by EMS, min, mean (SD) | 9.7 (4.0) | 9.7 (6.7) | 9.2 (5.4) | 10.1 (4.2) | 11.7 (7.4) | 9.4 (5.4) | 0.914 |
| Collapse to hospital arrival, min, mean (SD) | 29.4 (8.5) | 30.0 (9.6) | 29.4 (9.4) | 27.8 (7.7) | 27.5 (10.3) | 28.6 (8.6) | 0.693 |
AED indicates automated external defibrillator; CPR, cardiopulmonary resuscitation; EMS, emergency medical services; NA, not analysis; PEA, pulseless electrical activity; SD, standard deviation; VF, ventricular fibrillation.
P values are calculated to test the homogeneity among the 6 location groups.
Calculated for cases with time data on public‐access AEDs.
Calculated for cases with VF as first documented rhythm.
Table 4.
Outcomes After Bystander‐Witnessed Out‐of‐Hospital Cardiac Arrest of Cardiac Origin at Public Places According to the Location
| Railway Stations (n=118) | Sports Facilities (n=93) | Public Buildings (n=86) | Schools (n=31) | Airports (n=4) | Other Public Spaces (n=562) | P Value* | |
|---|---|---|---|---|---|---|---|
| Prehospital ROSC, n (%) | 35 (29.7) | 46 (49.5) | 20 (23.3) | 11 (35.5) | 1 (25.0) | 131 (23.3) | <0.001 |
| Total ROSC, n (%) | 69 (58.5) | 64 (68.8) | 44 (51.2) | 19 (61.3) | 4 (100.0) | 296 (52.7) | 0.018 |
| Hospital admission, n (%) | 63 (53.4) | 65 (69.9) | 40 (46.5) | 19 (61.3) | 4 (100.0) | 257 (45.7) | <0.001 |
| 1‐month survival, n (%) | 42 (35.6) | 50 (53.8) | 27 (31.4) | 15 (48.4) | 2 (50.0) | 146 (26.1) | <0.001 |
| Neurologically favorable outcome, n (%) | 33 (28.0) | 48 (51.6) | 20 (23.3) | 13 (41.9) | 2 (50.0) | 76 (13.6) | <0.001 |
ROSC indicates return of spontaneous circulation.
P values are calculated to test the homogeneity among the 6 location groups.
Figure 2 shows the temporal trends in the proportion of public‐access AED use among bystander‐witnessed OHCAs of cardiac origin at public places. The proportion significantly increased from 0.0% (0/7) in 2005 to 56.5% (13/23) in 2011 at sports facilities (P=0.006), from 0.0% (0/20) to 41.2% (7/17) at railway stations (P=0.001), and from 0.0% (0/7) to 33.3% (1/3) at schools (P=0.046).
Figure 2.
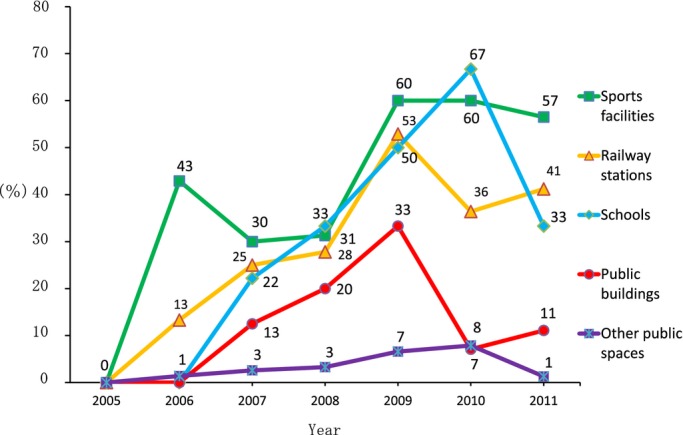
Trends in the proportion of public‐access AED use by laypersons among bystander‐witnessed OHCAs of cardiac origin in public places according to the location. AED indicates automated external defibrillation; OHCAs, out‐of‐hospital cardiac arrests.
Table 5 shows factors contributing to 1‐month survival with neurologically favorable outcome after bystander‐witnessed VF arrests. Earlier first shock (AOR for 1‐minute increment, 0.89; 95% CI, 0.87 to 0.92) and both chest compression‐only CPR (AOR, 1.54; 95% CI, 1.21 to 1.96) and conventional CPR with rescue breathing (AOR, 1.66; 95% CI, 1.25 to 2.19) contributed to improving outcome. However, the shock provider (bystander or EMS personnel) did not (AOR, 1.27; 95% CI, 0.82 to 1.97). As for locations, sports facilities (AOR, 3.62; 95% CI, 1.92 to 6.85) were only associated with neurologically favorable outcome. Multivariate logistic regression analysis using the time interval from call instead of collapse time showed almost the same results as those based on the time intervals from collapse (data not shown).
Table 5.
Factors Associated With Neurologically Favorable Outcome After Bystander‐Witnessed VF Arrest
| Crude OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|
| Age group | ||
| Children aged 0 to 17 years | 3.43 (1.44 to 8.18) | 2.23 (0.83 to 6.02) |
| Adults aged 18 to 64 years | 1.81 (1.50 to 2.20) | 1.64 (1.32 to 2.04) |
| Elderly aged ≥65 years | Reference | Reference |
| Male | 1.12 (0.88 to 1.41) | 0.85 (0.66 to 1.11) |
| Good activities of daily living | 2.11 (1.53 to 2.92) | 1.74 (1.21 to 2.56) |
| Type of bystander CPR | ||
| No CPR | Reference | Reference |
| Chest compression‐only CPR | 1.59 (1.33 to 1.89) | 1.54 (1.21 to 1.96) |
| Conventional CPR with rescue breathing | 1.88 (1.55 to 2.28) | 1.66 (1.25 to 2.19) |
| Public‐access defibrillation by laypersons | 4.10 (2.99 to 5.63) | 1.27 (0.82 to 1.97) |
| Location of arrest | ||
| Home | Reference | Reference |
| Healthcare facilities | 0.92 (0.54 to 1.58) | 0.90 (0.48 to 1.68) |
| Streets | 1.52 (1.13 to 2.05) | 1.34 (0.97 to 1.84) |
| Workplaces | 1.89 (1.35 to 2.66) | 1.28 (0.89 to 1.85) |
| Railway stations | 2.65 (1.66 to 4.23) | 1.69 (0.98 to 2.90) |
| Sports facilities | 9.64 (5.50 to 16.89) | 3.62 (1.92 to 6.85) |
| Public buildings | 2.36 (1.24 to 4.49) | 1.56 (0.77 to 3.13) |
| Schools | 3.16 (1.44 to 6.93) | 1.61 (0.68 to 3.83) |
| Airports | 7.38 (0.67 to 81.73) | NA* |
| Other public spaces | 1.55 (1.13 to 2.13) | 1.29 (0.92 to 1.81) |
| Others | 0.87 (0.52 to 1.44) | 0.69 (0.40 to 1.18) |
| Collapse to first shocks (for 1‐minute increment) | 0.87 (0.86 to 0.90) | 0.89 (0.87 to 0.92) |
| Year (for 1‐year increment) | 1.11 (1.05 to 1.16) | 1.10 (1.04 to 1.16) |
CI indicates confidence interval; CPR, cardiopulmonary resuscitation; NA, not analysis; OR, odds ratio; VF, ventricular fibrillation.
Uncalculable because of the small number.
Discussion
From this large, population‐based registry of OHCA in Osaka, where the public‐access AEDs were well disseminated, we clearly demonstrated that the proportion of public‐access AED use by laypersons has increased rapidly and worked effectively in public places, and that the characteristics and outcomes of OHCA with PAD were quite different, depending on the location. Rapid and massive distribution of public‐access AEDs and continuous registration of OHCA cases in this region made it possible to assess the impact of implementation of the PAD program in a community. This study shows the actual situations of public‐access AED use in the PAD era and provides important clues for implementing an appropriate placement of public‐access AEDs.
Railway stations were the most common places where shocks by public‐access AEDs were delivered. The proportion has increased rapidly and has just reached ≈50%, similar to those in the preceding studies from Japan.8,13 By contrast, shocks by public‐access AEDs have been more common at sports facilities, airports, and amusement facilities in western countries.12 Because the annual total number of railway passengers in Japan was ≈22.6 billion in 2011,22 further promotion of PAD programs for railway station users would therefore be important. These findings indicate the need of a region‐specific strategy in public‐access AED deployment.
The proportion of both public‐access AED use and neurologically favorable outcome after OHCA were the highest at sports facilities. Many OHCAs have occurred at sports facilities,23 and the national CPR guidelines recommend the placement of public‐access AEDs at sports facilities and athletic gyms.3–4,24 Previous studies have shown that OHCA people who were healthy and fit might be more likely to frequent a sports facility and have a better outcome after a cardiac arrest.25–26 Because sports facilities are more equipped with public‐access AEDs and their staff had more CPR skills, a collapsed person would be more likely to be discovered quickly and treated properly after an OHCA. Even though the proportion of public‐access AED use and bystander CPR were relatively greater at sports facilities than other locations, continuous CPR training, including an AED operation for their instructors, staffs, and participants, should be emphasized.
There were only a few bystander‐witnessed OHCAs of cardiac origin at airports. Although Osaka has 2 public airports, the annual total number of passengers using them was ≈79 million,27 far lower than that at railway stations, and these differences might influence the OHCA occurrence. Still, the OHCA occurrence at airports was not rare, and the effectiveness of public‐access AED deployment was already demonstrated.28
This study underscored that >80% of OHCA patients at schools had VF as the first documented rhythm, 67% received shocks by public‐access AEDs in 2010, and 42% had neurologically favorable outcome after an OHCA. The preceding studies showed that OHCA occurrence at schools was more frequent than expected,29 and school PAD programs contributed to improving outcome after an OHCA among both students and teachers.26 Commotio cordis is the second leading cause of sudden cardiac death among young athletes attending elementary and junior high school.30 Hence, the dissemination of public‐access AEDs at schools is essential. Although at least one public‐access AED has been deployed at almost all schools in Japan,31 further deployment of public‐access AEDs and CPR training for both teachers and students is warranted to shorten the time to shock and improve outcomes after OHCA at schools.32 In addition, it was well known that characteristics and outcomes from OHCA were different between children and adults.33–34 To prevent OHCA and improve the outcome after OHCA at schools, further studies would be needed to investigate incidences, characteristics, including detailed data on activities preceding OHCA and past medical histories, and outcomes from OHCAs among children and adults at schools.
Although the PAD program in public places was well disseminated, home use of AEDs was quite rare in this region. This might be caused by poor dissemination of AEDs at home.20 The Home AED Trial failed to show the effectiveness of AED deployment at home,35 whereas a report demonstrated that the dissemination of public‐access AEDs in multidwelling houses, such as apartments and condominiums, might be effective.10 In Japan, the number of multidwelling houses is increasing; 70% of inhabitants in Tokyo and 50% in Osaka live in such types of housing.36 In these areas, the public‐access AED deployment at apartment‐type houses should also be considered.
In our multivariate analysis, earlier defibrillation, irrespective of the shock provider, was associated with neurologically favorable outcome, a finding that was consistent with that of a previous study.11 In addition, both chest compression‐only CPR and conventional CPR with rescue breathing were also effective for improving neurologically favorable outcome. The present study demonstrated the effectiveness of bystander CRP and early defibrillation, reinforcing the importance of PAD program dissemination to improve the outcome after OHCA.1,3–5
In Osaka, the survival from OHCA increased during the study period, but it was still low. In addition, the proportions of bystander CPR and public‐access AED use in this area were only 40% and 2% among bystander‐witnessed OHCA. To further improve survival from OHCA, wider dissemination of CPR training, including at least chest compressions and public‐access AED use for the general public, should be particularly encouraged, as the new national CPR guidelines emphasized.1,3–5 The Japan Circulation Society also started to recommend chest compression‐only CPR training for lay rescuers to increase CPR and AED use since 2010.37
Limitations
Among the limitations of this study is having included only OHCA patients to whom shocks were delivered by public‐access AEDs. Data on patients for whom AED was attempted, but no shocks were delivered, were lacking. In future studies, we will investigate OHCA occurrence, AED geographic distribution, and all AED uses involving persons actually shocked or not. Second, we did not obtain information on the distribution of public‐access AEDs in the study area. Without such data, we can neither evaluate the rate of AED use nor the cost‐effectiveness of the widely disseminated public‐access AEDs. Third, our data do not address potential variability in postarrest care (hemodynamic support, induced hypothermia, and coronary interventional therapies).38 Fourth, there might be unmeasured confounding factors that might have influenced the association between locations and outcomes. Fifth, the time of collapse estimated from EMS interview with the bystander would be sometimes unreliable.21 Finally, as with all epidemiologic studies, the integrity and validity of the data, as well as ascertainment bias, are potential limitations of our study. The use of uniform data collection based on the Utstein‐style guidelines for reporting cardiac arrest, the large sample size, and the population‐based design should minimize these potential sources of bias.
Conclusions
This large, population‐based OHCA registry demonstrated that earlier shock, irrespective the shock provider (bystander or EMS personnel), contributed to improving outcome, and a public‐access defibrillation program was successfully implemented so that shocks with public‐access AEDs were delivered to over 40% of bystander‐witnessed OHCAs and time to shock was shortened in some kinds of public places.
Sources of Funding
This study was supported by a scientific research grant from the Ministry of Education, Culture, Sports, Science and Technology (25870391 and 25460750).
Disclosures
None.
Acknowledgments
The authors are deeply indebted to all of the EMS personnel and concerned physicians in Osaka Prefecture as well as the Osaka Medical Association for their indispensable cooperation and support. The authors also thank all members of the Utstein Osaka Project for their contribution in organization, coordination, and oversight as the steering committee.
References
- 1. 2010 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010; 122:S250-S605 [DOI] [PubMed] [Google Scholar]
- 2.Ambulance Service Planning Office of Fire and Disaster Management Agency of Japan. Effect of first aid for cardiopulmonary arrest Availbale at: http://www.fdma.go.jp/neuter/topics/kyukyukyujo_genkyo/h24/01_kyukyu.pdf. Accessed May 07, 2013 (in Japanese).
- 3. 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010; 122:S639-S946 [DOI] [PubMed] [Google Scholar]
- 4. European resuscitation council guidelines for resuscitation 2010. Resuscitation. 2010; 81:1219-1451 [DOI] [PubMed] [Google Scholar]
- 5.2010 Japanese Guidelines for Emergency Care and Cardiopulmonary Resuscitation. 20111st edTokyo: Health Shuppansha [Google Scholar]
- 6.Report on a study on social system development to improve survival from emergency cardiovascular disease using automated external defibrillator (Marukawa's report) Available at: http://aed-hyogo.sakura.ne.jp/wpm/archivepdf/23/2_11a.pdf. Accessed May 07, 2013 (in Japanese).
- 7.Iwami T, Hiraide A, Nakanishi N, Hayashi Y, Nishiuchi T, Uejima T, Morita H, Shigemoto T, Ikeuchi H, Matsusaka M, Shinya H, Yukioka H, Sugimoto H. Outcome and characteristics of out‐of‐hospital cardiac arrest according to location of arrest: a report from a large‐scale, population‐based study in Osaka, Japan. Resuscitation. 2006; 69:221-228 [DOI] [PubMed] [Google Scholar]
- 8.Muraoka H, Ohishi Y, Hazui H, Negoro N, Murai M, Kawakami M, Nishihara I, Fukumoto H, Morita H, Hanafusa T. Location of out‐of‐hospital cardiac arrests in Takatsuki City: where should automated external defibrillator be placed. Circ J. 2006; 70:827-831 [DOI] [PubMed] [Google Scholar]
- 9.Weisfeldt ML, Everson‐Stewart S, Sitlani C, Rea T, Aufderheide TP, Atkins DL, Bigham B, Brooks SC, Foerster C, Gray R, Ornato JP, Powell J, Kudenchuk PJ, Morrison LJResuscitation Outcomes Consortium Investigators. Ventricular tachyarrhythmia after cardiac arrest in pubic versus at home. N Engl J Med. 2011; 364:313-321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Folke F, Gislason GH, Lippert FK, Nielsen SL, Weeke P, Hansen ML, Fosbøl EL, Andersen SS, Rasmussen S, Schramm TK, Køber L, Torp‐Pedersen C. Differences between out‐of‐hospital cardiac arrest in residential and public locations and implications for public‐access defibrillation. Circulation. 2010; 122:623-630 [DOI] [PubMed] [Google Scholar]
- 11.Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Hiraide AImplementation Working Group for the All‐Japan Utstein Registry of the Fire and Disaster Management Agency. Nationwide public‐access defibrillation in Japan. N Engl J Med. 2010; 362:994-1004 [DOI] [PubMed] [Google Scholar]
- 12.Weisfeldt ML, Sitlani CM, Ornato JP, Rea T, Aufderheide TP, Davis D, Dreyer J, Hess EP, Jui J, Maloney J, Sopko G, Powell J, Nichol G, Morrison LJROC Investigators. Survival after application of automatic external defibrillators before arrival of the emergency medical system: evaluation in the resuscitation outcomes consortium population of 21 million. J Am Coll Cardiol. 2010; 55:1713-1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sasaki M, Iwami T, Kitamura T, Nomoto S, Nishiyama C, Sakai T, Tanigawa K, Kajino K, Irisawa T, Nishiuchi T, Hayashida S, Hiraide A, Kawamura T. Incidence and outcome of out‐of‐hospital cardiac arrest with public‐access defibrillation. Circ J. 2011; 75:2821-2826 [DOI] [PubMed] [Google Scholar]
- 14.Brooks SC, Hsu JH, Tang SK, Jeyakumar R, Chan TC. Determining risk for out‐of‐hospital cardiac arrest by location type in a Canadian urban setting to guide future public access defibrillator placement. Ann Emerg Med. 2013; 61:530-538 [DOI] [PubMed] [Google Scholar]
- 15.Chan TC, Li H, Lebovic G, Tang SK, Chan JY, Cheng HC, Morrison LJ, Brooks SC. Identifying locations for public access defibrillators using mathematical optimization. Circulation. 2013; 127:1801-1809 [DOI] [PubMed] [Google Scholar]
- 16.Folke F, Lippert FK, Nielsen SL, Gislason GH, Hansen ML, Schramm TK, Sørensen R, Fosbøl EL, Andersen SS, Rasmussen S, Køber L, Torp‐Pedersen C. Location of cardiac arrest in a city center: strategic placement of automated external defibrillators in public locations. Circulation. 2009; 120:510-517 [DOI] [PubMed] [Google Scholar]
- 17.Iwami T, Nichol G, Hiraide A, Hayashi Y, Nishiuchi T, Kajino K, Morita H, Yukioka H, Ikeuchi H, Sugimoto H, Nonogi H, Kawamura T. Continuous improvements in “chain of survival” increased survival after out‐of‐hospital cardiac arrests: a large‐scale population‐based study. Circulation. 2009; 119:723-734 [DOI] [PubMed] [Google Scholar]
- 18.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D'Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004; 110:3385-3397 [DOI] [PubMed] [Google Scholar]
- 19.2005 Japanese Guidelines for Emergency Care and Cardiopulmonary Resuscitation. 20073rd edTokyo: Health Shuppansha [Google Scholar]
- 20.Osaka Life Support Association. Osaka AED map Available at: http://osakaaed.jp. Accessed May 07, 2013 (in Japanese).
- 21.Isaacs E, Callaham ML. Ability of laypersons to estimate short time intervals in cardiac arrest. Ann Emerg Med. 2000; 35:147-154 [DOI] [PubMed] [Google Scholar]
- 22.Ministry of Land, Infrastructure, Transport and Tourism. Annual report on railway transportation Available at: http://www.mlit.go.jp/k-toukei/10/annual/index.pdf. Accessed May 07, 2013 (in Japanese).
- 23.Becker L, Eisenerg M, Fahrenbruch C, Cobb L. Public locations of cardiac arrest. Implications for public access defibrillation. Circulation. 1998; 97:2106-2109 [DOI] [PubMed] [Google Scholar]
- 24.American College of Sports Medicine; American Heart Association. American College of Sports Medicine and American Heart Association joint position statement: automated external defibrillators in health/fitness facilities. Med Sci Sports Exerc. 2002; 34:561-564 [DOI] [PubMed] [Google Scholar]
- 25.Nishiyama C, Iwami T, Nichol G, Kitamura T, Hiraide A, Nishiuchi T, Hayashi Y, Nonogi H, Kawamura T. Association of out‐of‐hospital cardiac arrest with prior activity and ambient temperature. Resuscitation. 2011; 82:1008-1012 [DOI] [PubMed] [Google Scholar]
- 26.Drezner JA, Rao AL, Heistand J, Bloomingdale MK, Harmon KG. Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation. 2009; 120:518-525 [DOI] [PubMed] [Google Scholar]
- 27.Ministry of Land, Infrastructure, Transport and Tourism. Annual statistical report on air transportation Available at: http://www.mlit.go.jp/k-toukei/search/pdf/11/11201100cc0000.pdf. Accessed May 07, 2013 (in Japanese)
- 28.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002; 347:1242-1247 [DOI] [PubMed] [Google Scholar]
- 29.Lotfi K, White L, Rea T, Cobb L, Copass M, Yin L, Becker L, Eisenberg M. Cardiac arrest in schools. Circulation. 2007; 116:1374-1379 [DOI] [PubMed] [Google Scholar]
- 30.Maron BJ, Estes NA, III, Link MS. Task Force 11: commotion cordis. J Am Coll Cardiol. 2005; 45:1371-1373 [DOI] [PubMed] [Google Scholar]
- 31.Ministry of Education, Culture, Sports, Science and Technology. A survey on AED deployment in schools Available at: http://www.mext.go.jp/component/a_menu/education/detail/__icsFiles/afieldfile/2012/04/04/1289307_04.pdf. Accessed May 07, 2013 (in Japanese).
- 32.Cave DM, Aufderheide TP, Beeson J, Ellison A, Gregory A, Hazinski MF, Hiratzka LF, Lurie KG, Morrison LJ, Mosesso VN, Jr, Nadkarni V, Potts J, Samson RA, Sayre MR, Schexnayder SMAmerican Heart Association Emergency Cardiovascular Care Committee; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Cardiovascular Diseases in the Young; Council on Cardiovascular Nursing; Council on Clinical Cardiology, and Advocacy Coordinating Committee. Importance and implementation of training in cardiopulmonary resuscitation and automated external defibrillation in schools: a science advisory from the American Heart Association. Circulation. 2011; 123:691-706 [DOI] [PubMed] [Google Scholar]
- 33.Nitta M, Iwami T, Kitamura T, Nadkarni VM, Berg RA, Shimizu N, Ohta K, Nishiuchi T, Hayashi Y, Hiraide A, Tamai H, Kobayashi M, Morita HUtstein Osaka Project. Age‐specific differences in outcomes after out‐of‐hospital cardiac arrests. Pediatrics. 2011; 128:e812-e820 [DOI] [PubMed] [Google Scholar]
- 34.Atkins DL, Everson‐Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, Berg RAResuscitation Outcomes Consortium Investigators. Epidemiology and outcomes from out‐of‐hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry‐Cardiac Arrest. Circulation. 2009; 119:1484-1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bardy GH, Lee KL, Mark DB, Poole JE, Toff WD, Tonkin AM, Smith W, Dorian P, Packer DL, White RD, Longstreth WT, Jr, Anderson J, Johnson G, Bischoff E, Yallop JJ, McNulty S, Ray LD, Clapp‐Channing NE, Rosenberg Y, Schron EBHAT Investigators. Home use of automated external defibrillators for sudden cardiac arrest. N Engl J Med. 2008; 358:1793-1804 [DOI] [PubMed] [Google Scholar]
- 36.Statistics Bureau, Ministry of Internal Affairs and Communications. 2008 Statistical survey on home and land Available at: http://www.stat.go.jp/data/jyutaku/2008/pdf/kgiy00.pdf Accessed May 07, 2013 (in Japanese).
- 37.The Japan Circulation Society. Call and push Available at: http://www.j-circ.or.jp/cpr/. Accessed September 25, 2013 (in Japanese).
- 38.Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT, Jr, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez‐Nunez A, Sellke FW, Spaulding C, Sunde K, Vanden Hoek T. Post‐cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A scientific statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Circulation. 2008; 118:2452-2458 [DOI] [PubMed] [Google Scholar]


