Abstract
Background
Organized stroke care is associated with improved outcomes. Data are limited on differences in changes in the quality of acute stroke care at The Joint Commission–certified Primary Stroke Centers (PSCs) versus non‐PSCs over time.
Methods and Results
We compared compliance with the Joint Commission's 10 acute stroke care performance measures and defect‐free care in PSCs and non‐PSCs participating in the Registry of the North Carolina Stroke Care Collaborative from January 2005 through February 2010. We included 29 654 cases presenting at 47 hospitals—10 PSCs, 8 preparing for certification, and 29 non‐PSCs—representing 43% of North Carolina's non–Veterans Affairs, acute care hospitals. Using a non‐PSC referent, odds ratios and 95% CIs were calculated using logistic regression and generalized estimating equations accounting for clustering of cases within hospitals. Time trends were presented graphically using simple linear regression. Performance measure compliance increased for all measures for all 3 groups in 2005–2010, with the exception of discharge on antithrombotics, which remained consistently high. PSCs and hospitals preparing for certification had better compliance with all but 2 performance measures compared with non‐PSCs (each P<0.01). Defect‐free care was delivered most consistently at hospitals preparing for certification (52.8%), followed by PSCs (45.0%) and non‐PSCs (21.9%). Between 2005 and 2010, PSCs and hospitals preparing for certification had a higher average annual percent increase in the provision of defect‐free care (P=0.01 and 0.04, respectively) compared with non‐PSCs.
Conclusions
PSC certification is associated with an overall improvement in the quality of stroke care in North Carolina; however, room for improvement remains.
Keywords: epidemiology, registry, stroke
Introduction
Stroke is a leading cause of death and disability in the United States.1 Although effective therapies and evidence‐based processes that can improve stroke diagnosis and treatment have been identified,2 gaps remain in their use.3 To address these gaps, the American Heart Association/American Stroke Association recommends establishing coordinated care systems that integrate best practices in prevention, diagnosis, treatment, and access.4 In 2004, The Joint Commission (JC) launched the Primary Stroke Center (PSC) hospital certification program that includes assessments of compliance with consensus‐based national standards, adherence to clinical practice guidelines, and collection of standardized performance measure (PM) data. Although there is considerable support for the PSC concept—as of January 1, 2011, there were >800 PSCs in 49 states5—limited data exist comparing the quality of acute stroke care at PSCs versus non‐PSCs over time.5–6
The state‐based registry of the North Carolina Stroke Care Collaborative (NCSCC) collects data on PMs identical to those required of PSC hospitals in a variety of hospitals, including those that are neither capable of nor interested in becoming a PSC. We compared compliance with the JC's 10 PMs based on data collected between January 2005 and February 2010 in PSC and non‐PSC hospitals, as well as in those preparing for certification.
Methods
The NCSCC is part of the Centers for Disease Control and Prevention–funded Paul Coverdell National Acute Stroke Registry program. The prospective registry includes patients 18 years of age or older who present to North Carolina (NC) hospital emergency departments (EDs) with signs or symptoms of stroke or transient ischemic attack. Hospitals eligible for participation include all non–Veterans Affairs, NC acute care hospitals with a dedicated ED, including critical‐access hospitals. All 110 eligible hospitals were invited to participate. A detailed description of hospital characteristics has been published.7
As previously described,7–9 trained hospital staff collect data on demographics, initial presentation, quality‐of‐care indicators, in‐hospital outcomes, and discharge disposition using a standardized, Internet‐based data collection tool. Whenever possible, data are collected concurrent with care. A random sample of cases was reabstracted to assess data quality (agreement 95.7%, κ statistic .94). Patients directly admitted to the hospital with a stroke are included; those with a stroke during hospitalization are excluded.
Hospitals were grouped into 3 categories: hospitals certified before registry enrollment (PSC), hospitals certified after enrollment (preparing for certification), or hospitals that remained uncertified by January 2011 (non‐PSC).
Quality measures include the 10 items in the JC Stroke Measure Set, used as part of the PSC certification process. We also measured 2 additional, related measures of quality of care: (1) received tissue plasminogen activator (tPA) within 3 hours of symptom onset and (2) received statin therapy as indicated. We also measured “defect‐free care,” a summary variable reflecting whether a patient received all of the PMs for which he or she was eligible.
Statistical Analysis
The χ2 tests were used to compare baseline categorical variables, and ANOVA was used for age in years. Proportions were calculated to describe percent compliance with JC PMs and defect‐free care. The overall, unadjusted association between PSC group and each PM and defect‐free care was evaluated using Pearson χ2 statistics and 2×3 contingency tables. Odds ratios (ORs) and 95% CIs for unadjusted models were calculated using logistic regression, with non‐PSCs as the referent. Separate models were constructed for each of the PMs and defect‐free care. Models adjusted for patient‐level variables included age in years, sex, race (black, white, and/or other), and stroke type (hemorrhagic, ischemic, transient ischemic attack, or stroke not otherwise specified) and used logistic regression. To investigate the effect of PSC status while controlling for both patient‐level factors and the hospital size (<100, 100 to 349, or ≥350 beds), as well as accounting for clustering of patients within hospitals, a generalized estimating equations (GEE) approach was used. Change in the percentage of cases in compliance with each PM was averaged for each year between 2005 and 2010, and absolute annual percent change was calculated and compared using 2‐sided F tests, with non‐PSC hospitals as the reference group. Trend lines in the plots of compliance with PMs over time were created using simple linear regression and 3‐month time intervals.
All comparisons used an a priori .05 rejection level for the null hypothesis. All statistical analyses were conducted using SAS Version 9.1.10
This study was approved by the University of North Carolina at Chapel Hill Institutional Review Board and individual hospitals' institutional review boards as required.
Results
Between January 1, 2005, and February 15, 2010, we enrolled 38 983 patients from 53 hospitals in NCSCC for whom we had complete data (Figure 1). Cases at the 6 hospitals that collected <6 months of data were excluded (n=291) as were cases discharged as “no stroke” (n=2389). Cases entered during the first 2 months of data collection were excluded (n=1346) to minimize the “learning curve” effect, leaving 47 hospitals and 29 654 cases for analysis. During the study period, there were 10 PSCs (n=14 885), 8 hospitals preparing for certification (n=6974), and 29 non‐PSCs (n=7795) in the NCSCC. One third (n=17) of hospitals included in analyses were located in nonmetropolitan counties, whereas nearly half (n=23) were located in metropolitan areas with a population of ≥250 000. Two hospitals were located in completely rural areas (<2500 urban population). The median number of beds for hospitals in the study population was 162 (interquartile range 113 to 457) in 2012.
Figure 1.
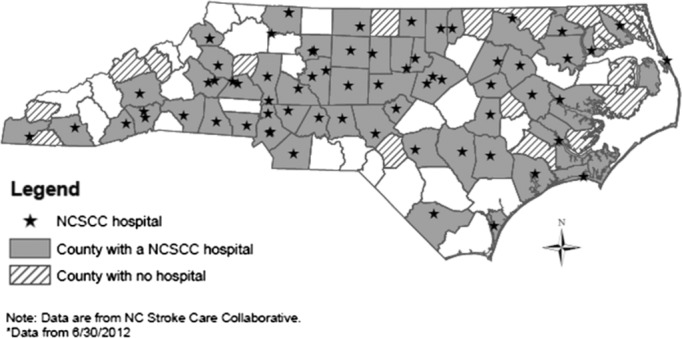
North Carolina counties with a North Carolina Stroke Care Collaborative (NCSCC) hospital, 2005–2012.*
Compared with non‐PSCs, PSCs and hospitals preparing for certification tended to be larger (P<0.01), teaching hospitals (P<0.01), and urban hospitals (P=0.03) (Table 1). They were also more likely to have an intravenous (IV) tPA protocol (P=0.04), an ED stroke protocol (P=0.02), a stroke unit (P<0.01), and a neurosurgeon on staff (P<0.01). Cases at PSCs tended to be younger (P<0.01), male (P<0.01), and nonwhite (P<0.01) (Table 2).
Table 1.
Characteristics of Hospitals Participating in the North Carolina Stroke Care Collaborative, 2005–2010, by PSC Certification Status
| PSC | Preparing for Certification | Non‐PSC | χ2 P Value | |
|---|---|---|---|---|
| N | 10 | 8 | 29 | |
| Community type, % | ||||
| Rural | 0 | 0 | 3.5 | 0.73 |
| Small town | 0 | 0 | 20.7 | 0.12 |
| Micropolitan | 10.0 | 50.0 | 37.9 | 0.16 |
| Urban/metropolitan | 90.0 | 50.0 | 37.9 | 0.03 |
| Bed size, % | ||||
| <100 | 0 | 25.0 | 31.0 | 0.13 |
| 100 to 249 | 20.0 | 25.0 | 58.6 | 0.05 |
| 250 to 499 | 0 | 37.5 | 10.3 | 0.05 |
| 500+ | 80.0 | 12.5 | 0 | <0.01 |
| Teaching hospital, % | 90.0 | 37.5 | 13.8 | 0.01 |
| Community access hospital, % | 0 | 0 | 24.1 | 0.08 |
| Process measures, % | ||||
| Acute stroke team | 80.0 | 50.0 | 24.1 | 0.07 |
| tPA protocol | 100 | 87.5 | 51.7 | 0.04 |
| Emergency department protocol | 100 | 50.0 | 44.8 | 0.02 |
| Protocols revised weekly | 90.0 | 37.5 | 34.5 | 0.02 |
| Stroke unit | 80.0 | 62.5 | 20.7 | <0.01 |
| Stroke unit general ward | 80.0 | 62.5 | 13.8 | <0.01 |
| Neurosurgery on staff | 90.0 | 62.5 | 24.1 | <0.01 |
| Neurosurgery 24/7 in 2 hours | 90.0 | 37.5 | 13.8 | <0.01 |
| Written plan for EMS transport | 80.0 | 50.0 | 41.4 | 0.16 |
| EMS notification activate protocol | 90.0 | 62.5 | 20.7 | <0.01 |
PSC indicates Primary Stroke Center; tPA, tissue plasminogen activator; EMS, emergency medical services.
Table 2.
Characteristics of Cases Enrolled in the North Carolina Stroke Care Collaborative, 2005–2010, by PSC Certification Status
| PSC | Preparing for Certification | Non‐PSC | P Value | |
|---|---|---|---|---|
| N | 14 885 | 6974 | 7795 | |
| Age, mean (SD) | 66.8 (15.0) | 69.4 (14.4) | 70.7 (14.0) | <0.01 |
| Male, n (%) | 7267 (48.8) | 3339 (47.9) | 3536 (45.4) | <0.01 |
| Nonwhite, n (%) | 5223 (35.1) | 1301 (18.7) | 2025 (26.0) | <0.01 |
| Hispanic, n (%) | 193 (1.4) | 74 (1.1) | 84 (1.1) | 0.13 |
| Health insurance, n (%) | ||||
| Medicare | 8343 (56.1) | 4757 (68.2) | 5423 (69.6) | <0.01 |
| Other | 9677 (65.0) | 4110 (58.9) | 5235 (67.2) | <0.01 |
| None | 1729 (11.6) | 491 (7.0) | 639 (8.2) | <0.01 |
| Stroke type, n (%)* | ||||
| Ischemic | 7049 (47.4) | 2952 (42.3) | 1933 (24.8) | <0.01 |
| Hemorrhagic | 2942 (19.8) | 817 (11.7) | 628 (8.1) | <0.01 |
| Transient ischemic attack | 3391 (22.8) | 1477 (21.2) | 2163 (27.8) | <0.01 |
| Not otherwise specified | 1936 (13.0) | 1945 (27.9) | 3433 (44.0) | <0.01 |
PSC indicates primary stroke center.
Categories not mutually exclusive.
PSCs and hospitals preparing for certification had higher compliance with all but 2 PMs (smoking cessation counseling and treatment of cases with atrial fibrillation with anticoagulant therapy) compared with non‐PSCs (P<0.01) (Table 3). PSCs were the most likely to provide deep vein thrombosis prophylaxis, antithrombotic agents, and IV tPA. Hospitals preparing for certification were the most likely to measure lipids during hospitalization, screen for dysphagia, provide stroke education, and provide smoking cessation counseling. Defect‐free care was most common at hospitals preparing for PSC certification (52.8%), followed by PSCs (45.0%) and non‐PSCs (21.9%).
Table 3.
Percentage of Cases in Compliance with Joint Commission Performance Measures, North Carolina Stroke Care Collaborative, 2005–2010, by PSC Certification Status
| Performance Measures | PSC (n=15 405) | Preparing for Certification (n=7281) | Non‐PSC (n=8314) | χ2 P Value |
|---|---|---|---|---|
| 1. Received deep vein thrombosis prophylaxis | 93.4 | 90.1 | 77.34 | <0.01 |
| 2. Discharged on antithrombotic | 98.7 | 97.8 | 95.1 | <0.01 |
| 3. Patients with atrial fibrillation received anticoagulant | 88.8 | 87.9 | 85.7 | 0.14 |
| 4 a. IV tPA received (among eligible ischemic strokes) | 30.0 | 20.7 | 13.2 | <0.01 |
| b. IV tPA considered | 70.7 | 70.3 | 31.1 | <0.01 |
| c. IV tPA received (among all ischemic strokes) | 6.6 | 3.5 | 2.7 | <0.01 |
| 5. Received antithrombotics within 48 hours | 94.5 | 94.5 | 89.9 | <0.01 |
| 6 a. Lipid profile measured during hospitalization | 72.7 | 73.9 | 64.1 | <0.01 |
| b. If lipid profile measured, discharged on statin | 97.0 | 96.3 | 94.9 | <0.01 |
| 7. Screened for dysphasia | 67.7 | 71.6 | 42.8 | <0.01 |
| 8. Given stroke education | 69.2 | 76.0 | 47.6 | <0.01 |
| 9. Given smoking cessation counseling | 87.6 | 94.0 | 91.2 | <0.01 |
| 10. Considered for a rehabilitation plan | 93.4 | 94.0 | 90.9 | <0.01 |
| Defect‐free care | 45.0 | 52.0 | 21.9 | <0.01 |
Denominators vary based on exclusion/inclusion criteria. PSC indicates primary stroke center; IV tPA, intravenous tissue plasminogen activator.
As shown in Table 4, PSC hospitals and those preparing for certification had higher odds of complying with all measured stroke performance indicators (including defect‐free care) with the exception of providing anticoagulants to patients with atrial fibrillation (no statistical difference) and providing smoking cessation counseling (PSCs had lower compliance than non‐PSCs). Adjustment for age, sex, race, and stroke type altered ORs only modestly. Further adjustment for hospital bed size and accounting for clustering of patients within hospitals modestly attenuated some, but not all, ORs but did widen CIs. With regard to hospitals preparing for certification, CIs were widened to the point of nonsignificance for discharge on antithrombotic, receipt of IV tPA, measurement of lipids, and consideration for a rehabilitation plan.
Table 4.
Odds Ratio and 95% CIs of Compliance with Joint Commission Performance Measures Among Cases Enrolled in the North Carolina Stroke Care Collaborative, 2005–2010, by PSC Certification Status (Referent=non‐PSC)
| Performance Measures | Model 1* | Model 2* | Model 3* | |||
|---|---|---|---|---|---|---|
| PSC | Preparing for Certification | PSC | Preparing for Certification | PSC | Preparing for Certification | |
| 1. Received deep vein thrombosis prophylaxis | 4.2 (3.7 to 4.7) | 2.7 (2.3 to 3.1) | 3.9 (3.4 to 4.4) | 2.7 (2.4 to 3.2) | 3.9 (2.6 to 5.9) | 2.7 (1.3 to 5.6) |
| 2. Discharged on antithrombotic | 4.0 (3.3 to 4.8) | 2.3 (1.8 to 2.8) | 4.1 (3.4 to 5.0) | 2.2 (1.8 to 2.7) | 2.5 (1.7 to 3.7) | 1.6 (1.0 to 2.5) |
| 3. Patients with atrial fibrillation received anticoagulant | 1.3 (1.0 to 1.8) | 1.2 (0.9 to 1.7) | 1.3 (1.0 to 1.7) | 1.2 (0.8 to 1.6) | 1.2 (0.7 to 2.0) | 1.2 (0.6 to 2.4) |
| 4 a. IV tPA received (among eligible ischemic strokes) | 2.8 (2.3 to 3.5) | 1.7 (1.3 to 2.2) | 2.8 (2.2 to 3.4) | 1.7 (1.3 to 2.2) | 2.4 (1.4 to 4.1) | 1.5 (0.8 to 3.1) |
| b. IV tPA considered | 5.4 (4.0 to 7.0) | 5.2 (3.6 to 7.7) | 5.4 (4.1 to 7.2) | 5.3 (3.6 to 7.8) | 4.8 (1.8 to 12.5) | 2.9 (0.9 to 8.8) |
| c. IV tPA received (among all ischemic strokes) | 2.6 (2.1 to 3.1) | 1.3 (1.0 to 1.6) | 2.6 (2.2 to 3.1) | 1.3 (1.0 to 1.6) | 2.2 (1.2 to 3.7) | 1.2 (0.5 to 2.5) |
| 5. Received antithrombotics within 48 hours | 1.9 (1.7 to 2.2) | 1.9 (1.7 to 2.3) | 1.9 (1.7 to 2.2) | 2.0 (1.7 to 2.3) | 2.5 (1.5 to 4.1) | 3.1 (1.9 to 5.1) |
| 6 a. Lipid profile measured during hospitalization | 1.5 (1.4 to 1.6) | 1.6 (1.5 to 1.7) | 1.4 (1.3 to 1.5) | 1.5 (1.4 to 1.7) | 1.1 (0.8 to 1.4) | 1.2 (0.9 to 1.6) |
| b. If lipid profile measured, discharged on statin | 1.7 (1.3 to 2.4) | 1.4 (1.0 to 2.0) | 1.6 (1.2 to 2.2) | 1.4 (1.0 to 1.9) | 1.0 (0.6 to 1.7) | 0.9 (0.4 to 2.3) |
| 7. Screened for dysphasia | 2.8 (2.6 to 3.0) | 3.4 (3.1 to 3.6) | 2.8 (2.7 to 3.0) | 3.3 (3.1 to 3.6) | 3.2 (2.1 to 5.0) | 3.5 (2.5 to 4.9) |
| 8. Given stroke education | 2.5 (2.3 to 2.6) | 3.5 (3.2 to 3.8) | 2.5 (2.3 to 2.6) | 3.3 (3.1 to 3.6) | 4.0 (2.2 to 7.0) | 3.9 (2.3 to 6.9) |
| 9. Given smoking cessation counseling | 0.7 (0.6 to 0.9) | 1.5 (1.1 to 2.0) | 0.7 (0.6 to 0.9) | 1.5 (1.1 to 1.9) | 1.2 (0.5 to 2.9) | 1.1 (0.5 to 2.6) |
| 10. Considered for a rehabilitation plan | 1.4 (1.3 to 1.6) | 1.6 (1.4 to 1.8) | 1.7 (1.5 to 1.9) | 1.8 (1.6 to 2.2) | 1.5 (0.9 to 2.4) | 1.6 (1.0 to 2.5) |
| Defect‐free care | 2.9 (2.8 to 3.1) | 3.9 (3.6 to 4.1) | 2.9 (2.7 to 3.1) | 3.5 (3.3 to 3.8) | 3.2 (2.1 to 4.7) | 3.7 (2.5 to 5.5) |
PSC indicates primary stroke center; IV tPA, intravenous tissue plasminogen activator.
Unadjusted.
Adjusted for age, sex, race, and stroke type.
Adjusted for age, sex, race, stroke type, and hospital bed size and accounting for clustering of patients within hospitals.
There were substantial improvements in the quality of acute stroke care from 2005 to 2010 (Table 5). Overall, PM compliance increased for all measures and for all 3 hospital groups (Figure 2), with the exception of discharge on antithrombotic medication, which remained high throughout the study period in all 3 groups. PSCs and hospitals in the process of certification had consistently higher PM compliance. Compared with non‐PSCs, PSCs had a higher average annual percent increase in smoking cessation counseling (P<0.01), and those preparing for certification had the greatest increases in the percent of patients for whom IV tPA was considered (P<0.01) and in the percentage of eligible cases who received IV tPA (P=0.04), those who had a lipid profile measured during hospitalization (P<0.01), and those who were discharged on a statin (P=0.04). PSCs and those preparing for certification had a higher average annual percent increase in the provision of defect‐free care (P=0.01 and 0.04, respectively) than non‐PSCs. Compared with hospitals preparing for certification, non‐PSCs had a higher average annual percent increase in the provision of DVT prophylaxis (P=0.04), and compared with PSCs, non‐PSCs had a higher average annual percent increase in cases administered IV tPA (P=0.01) and in cases discharged on a statin (P=0.01).
Table 5.
Average Annual Absolute Percentage Change in Compliance with Joint Commission Performance Measures among Cases Enrolled in the North Carolina Stroke Care Collaborative, 2005–2010, by PSC* Status (Referent=non‐PSC)
| Performance Measures | PSC | Preparing for Certification | Non‐PSC (Ref) |
|---|---|---|---|
| 1. Received deep vein thrombosis prophylaxis | 2.3 | 1.1* | 5.1 |
| 2. Discharged on antithrombotic | −0.1 | 0.2 | 0.1 |
| 3. Patients with atrial fibrillation received anticoagulant | 3.4 | 9.9 | 7.7 |
| 4 a. IV tPA received (among eligible ischemic strokes) | 1.6 | 3.0 | 1.1 |
| b. IV tPA considered | 9.9 | 18.4* | 5.3 |
| c. IV tPA received (among all ischemic strokes) | <−0.1* | 0.9* | 0.1 |
| 5. Received antithrombotics within 48 hours | 2.3 | 4.5 | 4.3 |
| 6 a. Lipid profile measured during hospitalization | 7.9 | 10.3* | 6.3 |
| b. If lipid profile measured, discharged on statin | 1.1* | 3.1* | 2.2 |
| 7. Screened for dysphasia | 3.9 | 6.6 | 3.7 |
| 8. Given stroke education | 6.7 | 6.3 | 6.9 |
| 9. Given smoking cessation counseling | 8.2* | 3.2 | 2.1 |
| 10. Considered for a rehabilitation plan | 1.9 | 2.5 | 2.0 |
| Defect‐free care | 7.7* | 8.1* | 3.7 |
Denominators vary based on exclusion/inclusion criteria. PSC indicates primary stroke center; IV tPA, intravenous tissue plasminogen activator.
Compliance measured in 3‐month intervals, with the first 2 months of data excluded.
F‐test P<0.05.
F‐test P<0.01.
Figure 2.
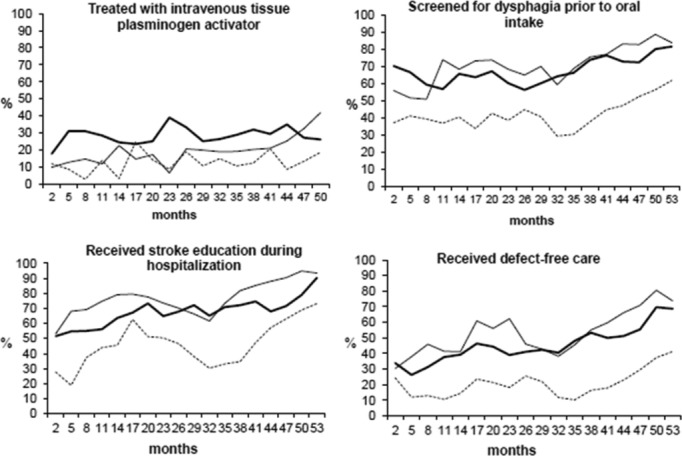
Percentage of cases enrolled in the North Carolina Stroke Care Collaborative meeting Joint Commission performance measures, 2005–2010, by Primary Stroke Center certification status over time (months).
Discussion
We found that the quality of stroke‐related care improved in hospitals participating in the NCSCC registry 2005 through 2010, but PSCs and hospitals preparing for certification had higher compliance with most PMs. Moreover, PSCs and hospitals preparing for certification had greater improvements over time on a number of measures.
In unadjusted analyses, hospitals preparing for certification had higher compliance than established PSCs for lipids measured during hospitalization, dysphagia screening, stroke education, smoking cessation counseling, consideration for a rehabilitation plan, and overall defect‐free care. These differences initially suggested support for the theory that when preparing for certification, hospital personnel must devote a great deal of time effort and commitment to improving stroke care; however, thereafter, there may be a tendency toward “complacency with past improvements”11 and a diminishment in the urgency for continued quality improvement or a ceiling effect with further improvements having relatively less impact. However, after adjustment for patient‐level factors and hospital bed size and after accounting for the clustering of patients within hospitals, these differences were removed, suggesting PSCs continue to improve quality of stroke care, even after certification.
Our finding that non‐PSCs had a higher average annual percent increase in cases administered IV tPA and in cases discharged on a statin is likely due to the fact that baseline IV tPA rates were much lower at baseline at non‐PSCs (Table 3), allowing for greater improvements in response to secular trends. Rate of discharge on a statin was high for all 3 groups (Table 3) but lowest for non‐PSCs, again allowing for greater improvement over time. PSC certification aims to improve the process of stroke care delivery at many levels. Certification requires hospitals to have stroke teams and stroke units and to use standardized stroke care pathways to guide evaluation and treatment of stroke.12 The quality of stroke care has improved in recent years, both nationally13 and in NC.14 These trends are reflected in our data, as even non‐PSCs, which include primarily small, rural, nonteaching hospitals, showed improvements. A 2010 statewide survey of hospital‐based stroke services in NC reported that the introduction of the JC's PSC certification process occurred concurrent with significant improvements in a number of important organizational features in NC hospitals, including the use of stroke care maps, IV tPA protocols, stroke teams, prewritten stroke orders, and diagnostic tests that were not seen in the period preceding the PSC certification program.14 Organizational and procedural changes such as these are likely important drivers of improved compliance with stroke treatment recommendations.15
Differences in acute stroke care quality at PSCs compared with non‐PSCs have been reported. For example, one study found that patients admitted to PSCs were more likely to receive IV tPA.6 Another reported that in New York State, patients cared for at PSCs had shorter median door‐to‐physician times, a higher probability of appropriate IV tPA administration, and a higher probability of stroke unit admission.16 Shorter time to computed tomography scan at PSCs compared with non‐PSCs has been reported in a previous NCSCC study.9 PSC‐like programs in other countries have reported similar improvements in acute stroke care. In Japan, investigators reported an increase from 1.2% to 2.8% in IV tPA administration among eligible patients and a significant decrease in response time following PSC establishment.17
Studies of the effect of PSC certification on mortality and discharge destination suggest a survival benefit. Stroke mortality rates at PSCs were lower than non‐PSCs in New York State (ie, 30‐day mortality, 10.1% versus 12.5%; P<0.001).6 Studies based on US national data also found lower risk‐adjusted mortality rates for PSC patients with both ischemic and hemorrhagic stroke.18–19 Similarly, a Finnish study reported lower 1‐year stroke case fatality at certified stroke centers.20 In contrast, an AHA Get With The Guidelines Stroke study reported that while the hospitals' geographical region and academic status were independently associated with risk‐adjusted mortality and morbidity, PSC designation was not.21 All of the hospitals, however, were participating in a performance improvement program including all PSC PMs, which may have reduced the potential effect of PSC designation. A study evaluating the impact of the Get With The Guidelines Stroke program reported that, independent of secular trends, time of participation in the program was associated with increased adherence to all stroke PMs.22 Still, the greatest improvements were noted among hospitals that received PSC certification. The similarity in percent change in compliance with PMs among PSCs and those preparing for certification suggests a continuum of quality improvement and a benefit in the process of attaining certification.
Certain hospital characteristics such as bed size23 and academic status14 have been associated with stroke care quality, and hospitals with greater resources may have provided high‐quality care before the certification process began.14 Although many key acute stroke care processes (eg, stroke teams, stroke units, neurosurgery on staff, and treatment protocols) may have been developed or improved during certification, precertification differences in hospital characteristics—including more physicians, specialists, equipment, and other resources—may have facilitated their implementation.24 Though PSCs tend to have different characteristics than non‐PSCs, PSCs do not have uniform access, resources, capacity, and quality. Further, although certain characteristics (eg, larger size, teaching status, and urban setting) are associated with higher‐quality care, high‐quality care can still be provided in a dedicated center that provides a coordinated system of care.23,25–26 Strategies such as telemedicine to access stroke teams, ambulance rerouting, and transfer agreements make process measures attainable even by small rural hospitals.27 Multilevel modeling to include the effect of hospital bed size was conducted to address this concern.
Stroke patients treated at PSCs were generally younger, male, and nonwhite and more likely to have hemorrhagic strokes. PSCs treated a more severe patient population, as suggested by the higher proportion of hemorrhagic stroke cases.28 Stroke type may further affect care quality. Hemorrhagic stroke cases are less likely to receive smoking cessation education and stroke education than were patients with ischemic stroke or transient ischemic attack but are more likely to receive care compliant with other PMs.29 Although few age differences have been reported,30 women were less likely to receive IV tPA treatment and lipid testing,31 and black patients were more likely to have longer ED waiting times32 and receive fewer evidence‐based care processes than were white or Hispanic patients.33
Participation in the NCSCC is voluntary, and participating hospitals are more likely to have an interest in stroke quality improvement. NCSCC hospitals, however, are similar to those in other large stroke registries.13,34–37 Our study included hospitals from all regions of NC and included a mix of academic and nonacademic, rural and urban, and small and large hospitals. Because the NCSCC requires no fee for participation—in fact, it assists hospitals with the costs associated with participation—barriers to participation are low, and the NCSCC is more likely to include a diverse population of hospitals. Approximately 62% of the nearly 27 000 stroke hospitalizations in NC each year are at hospitals participating in the NCSCC.
Hospitals were encouraged to include all acute stroke admissions; however, bias may occur if hospitals do not follow instructions consistently.38 Periodic quality control studies found that 83.7% of all acute strokes discharged from participating hospitals were enrolled. This high case ascertainment rate may be attributed to the use of both prospective and retrospective case capture methods and no requirements to obtain written consent. Because the NCSCC is a quality improvement registry and patient consent is not required, the lack of consent precludes obtaining postdischarge outcomes data.
Conclusions
PSC certification is associated with an overall improvement in the quality of stroke care in NC. Still, considerable room for improvement remains, even among certified hospitals. Additional organizational and policy changes and provider and community education are needed for continued progress.14 Improved public knowledge about stroke symptoms and the proper response is particularly critical if patients are to be eligible for the most effective acute stroke care options.
Nearly one‐fifth of NC's population resides in a county without a PSC or a facility with telemedicine or a standing transfer plan,14 underscoring the importance of identifying facilities appropriate for PSC certification or, where unable, using alternative quality improvement strategies.39 Assessment of compliance with PMs allows for the monitoring of changes and improvements in systems, operations, and organization within hospitals. Continuous monitoring of care measures in both PSCs and non‐PSCs—particularly in a real‐time, prospective manner as done in the NCSCC—is critical if quality improvement is to continue. Linking compliance levels with outcomes will also be an important measure of the true value of these system‐level changes and must be addressed in future studies.
Sources of Funding
This study was supported by the Centers for Disease Control and Prevention as a Paul Coverdell National Acute Stroke Registry through a subcontract with the North Carolina Division of Public Health (contract 01602‐10).
Disclosures
None.
Acknowledgments
We thank participating hospitals and staff.
References
- 1.Sidney S, Rosamond WD, Howard VJ, Luepker RV. The “heart disease and stroke statistics—2013 update” and the need for a national cardiovascular surveillance system. Circulation. 2013; 127:21-23 [DOI] [PubMed] [Google Scholar]
- 2.Freeman WD, Dawson SB, Flemming KD. The ABC's of stroke complications. Semin Neurol. 2010; 30:501-510 [DOI] [PubMed] [Google Scholar]
- 3.Williams SC, Schmaltz SP, Morton DJ, Koss RG, Loeb JM. Quality of care in U.S. hospitals as reflected by standardized measures, 2002–2004. N Engl J Med. 2005; 353:255-264 [DOI] [PubMed] [Google Scholar]
- 4.Schwamm LH, Pancioli A, Acker JE, III, Goldstein LB, Zorowitz RD, Shephard TJ, Moyer P, Gorman M, Johnston SC, Duncan PW, Gorelick P, Frank J, Stranne SK, Smith R, Federspiel W, Horton KB, Magnis E, Adams RJAmerican Stroke Association's Task Force on the Development of Stroke Systems. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association's Task Force on the Development of Stroke Systems. Circulation. 2005; 111:1078-1091 [DOI] [PubMed] [Google Scholar]
- 5.Kidwell CS, Shephard T, Tonn S, Lawyer B, Murdock M, Koroshetz W, Alberts M, Hademenos GJ, Saver JL. Establishment of primary stroke centers: a survey of physician attitudes and hospital resources. Neurology. 2003; 60:1452-1456 [DOI] [PubMed] [Google Scholar]
- 6.Xian Y, Holloway RG, Chan PS, Noyes K, Shah MN, Ting HH, Chappel AR, Peterson ED, Friedman B. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011; 305:373-380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosamond W, Johnson A, Bennett P, O'Brien E, Mettam L, Jones S, Coleman S. Monitoring and improving acute stroke care: the North Carolina Stroke Care Collaborative. N C Med J. 2012; 73:494-498 [PubMed] [Google Scholar]
- 8.George MG, Tong X, McGruder H, Yoon P, Rosamond W, Winquist A, Hinchey J, Wall HK, Pandey DKCenters for Disease Control and Prevention (CDC). Paul Coverdell National Acute Stroke Registry Surveillance—four states, 2005–2007. Morb Mortal Wkly Rep Surveill Summ. 2009; 58:1-23 [PubMed] [Google Scholar]
- 9.Rose KM, Rosamond WD, Huston SL, Murphy CV, Tegeler CH. Predictors of time from hospital arrival to initial brain‐imaging among suspected stroke patients: the North Carolina Collaborative Stroke Registry. Stroke. 2008; 39:3262. [DOI] [PubMed] [Google Scholar]
- 10.SAS Institute Inc. SAS OnlineDoc 9.1.3. 2002Cary, NC: SAS Institute Inc. [Google Scholar]
- 11.Silow‐Carroll S, Alteras T, Meyer JA. 2007. Hospital quality improvement: strategies and lessons from U.S. hospitals. USA: Commonwealth Fund; Report No.: Commonwealth Fund pub. no. 1009.
- 12.Stradling D, Yu W, Langdorf ML, Tsai F, Kostanian V, Hasso AN, Welbourne SJ, Schooley Y, Fisher MJ, Cramer SC. Stroke care delivery before vs. after JCAHO stroke center certification. Neurology. 2007; 68:469-470 [DOI] [PubMed] [Google Scholar]
- 13.Fonarow GC, Gregory T, Driskill M, Stewart MD, Beam C, Butler J, Jacobs AK, Meltzer NM, Peterson ED, Schwamm LH, Spertus JA, Yancy CW, Tomaselli GF, Sacco RL. Hospital certification for optimizing cardiovascular disease and stroke quality of care and outcomes. Circulation. 2010; 122:2459-2469 [DOI] [PubMed] [Google Scholar]
- 14.Goldstein LB. Statewide hospital‐based stroke services in North Carolina: changes over 10 years. Stroke. 2010; 41:778-783 [DOI] [PubMed] [Google Scholar]
- 15.Lichtman JH, Watanabe E, Allen NB, Jones SB, Dostal J, Goldstein LB. Hospital arrival time and intravenous t‐PA use in US Academic Medical Centers, 2001–2004. Stroke. 2009; 40:3845-3850 [DOI] [PubMed] [Google Scholar]
- 16.Gropen TI, Gagliano PJ, Blake CA, Sacco RL, Kwiatkowski T, Richmond NJ, Leifer D, Libman R, Azhar S, Daley MBNYSDOH Stroke Center Designation Project Workgroup. Quality improvement in acute stroke: the New York State Stroke Center Designation Project. Neurology. 2006; 67:88-93 [DOI] [PubMed] [Google Scholar]
- 17.Sung SF, Ong CT, Wu CS, Hsu YC, Su YH. Increased use of thrombolytic therapy and shortening of in‐hospital delays following acute ischemic stroke: experience on the establishment of a primary stroke center at a community hospital. Acta Neurol Taiwan. 2010; 19:246-252 [PubMed] [Google Scholar]
- 18.Lichtman JH, Jones SB, Wang Y, Watanabe E, Leifheit‐Limson EC, Goldstein LB. Outcomes after ischemic stroke for hospitals with and without Joint Commission—certified primary stroke centers. Neurology. 2011; 76:1976-1982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lichtman JH, Jones SB, Leifheit‐Limson EC, Wang Y, Goldstein LB. 30‐Day mortality and readmission after hemorrhagic stroke among Medicare beneficiaries in Joint Commission primary stroke center‐certified and noncertified hospitals. Stroke. 2011; 42:3387-3391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meretoja A, Roine RO, Kaste M, Linna M, Roine S, Juntunen M, Erilä T, Hillbom M, Marttila R, Rissanen A, Sivenius J, Häkkinen U. Effectiveness of primary and comprehensive stroke centers: PERFECT stroke: a nationwide observational study from Finland. Stroke. 2010; 41:1102-1107 [DOI] [PubMed] [Google Scholar]
- 21.Fonarow GC, Smith EE, Reeves MJ, Pan W, Olson D, Hernandez AF, Peterson ED, Schwamm LHGet With The Guidelines Steering Committee and Hospitals. Hospital‐level variation in mortality and rehospitalization for Medicare beneficiaries with acute ischemic stroke. Stroke. 2011; 42:159-166 [DOI] [PubMed] [Google Scholar]
- 22.Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, Ellrodt G, Cannon CP, Liang L, Peterson E, Labresh KA. Get with the Guidelines‐Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009; 119:107-115 [DOI] [PubMed] [Google Scholar]
- 23.Reeves MJ, Gargano J, Maier KS, Broderick JP, Frankel M, LaBresh KA, Moomaw CJ, Schwamm L. Patient‐level and hospital‐level determinants of the quality of acute stroke care: a multilevel modeling approach. Stroke. 2010; 41:2924-2931 [DOI] [PubMed] [Google Scholar]
- 24.Keeler EB, Rubenstein LV, Kahn KL, Draper D, Harrison ER, McGinty MJ, Rogers WH, Brook RH. Hospital characteristics and quality of care. JAMA. 1992; 268:1709-1714 [PubMed] [Google Scholar]
- 25.O'Toole LJ, Jr, Slade CP, Brewer GA, Gase LN. Barriers and facilitators to implementing primary stroke center policy in the United States: results from 4 case study states. Am J Public Health. 2011; 101:561-566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Derdeyn CP, Panagos PD. Stroke center certification: where are we in 2010? J Neurointerv Surg. 2010; 2:41-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith EE, Dreyer P, Prvu‐Bettger J, Abdullah AR, Palmeri G, Goyette L, McElligott C, Schwamm LH. Stroke center designation can be achieved by small hospitals: the Massachusetts experience. Crit Pathw Cardiol. 2008; 7:173-177 [DOI] [PubMed] [Google Scholar]
- 28.Goldstein LB, Edwards MG, Wood DP. Delay between stroke onset and emergency department evaluation. Neuroepidemiology. 2001; 20:196-200 [DOI] [PubMed] [Google Scholar]
- 29.Fonarow GC, Reeves MJ, Smith EE, Saver JL, Zhao X, Olson DW, Hernandez AF, Peterson ED, Schwamm LHGWTG‐Stroke Steering Committee Investigators. Characteristics, performance measures, and in‐hospital outcomes of the first one million stroke and transient ischemic attack admissions in get with the guidelines‐stroke. Circ Cardiovasc Qual Outcomes. 2010; 3:291-302 [DOI] [PubMed] [Google Scholar]
- 30.Saposnik G, Black SE, Hakim A, Fang J, Tu JV, Kapral MK. Age disparities in stroke quality of care and delivery of health services. Stroke. 2009; 40:3328-3335 [DOI] [PubMed] [Google Scholar]
- 31.Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, Khatiwoda A, Lisabeth L. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008; 7:915-926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karve SJ, Balkrishnan R, Mohammad YM, Levine DA. Racial/ethnic disparities in emergency department waiting time for stroke patients in the United States. J Stroke Cerebrovasc Dis. 2011; 20:30-40 [DOI] [PubMed] [Google Scholar]
- 33.Schwamm LH, Reeves MJ, Pan W, Smith EE, Frankel MR, Olson D, Zhao X, Peterson E, Fonarow GC. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010; 121:1492-1501 [DOI] [PubMed] [Google Scholar]
- 34.Palnum KD, Petersen P, Sorensen HT, Ingeman A, Mainz J, Bartels P, Johnsen SP. Older patients with acute stroke in Denmark: quality of care and short‐term mortality: a nationwide follow‐up study. Age Ageing. 2008; 37:90-95 [DOI] [PubMed] [Google Scholar]
- 35.Di Carlo A, Lamassa M, Baldereschi M, Pracucci G, Basile AM, Wolfe CD, Giroud M, Rudd A, Ghetti A, Inzitari DEuropean BIOMED Study of Stroke Care Group. Sex differences in the clinical presentation, resource use, and 3‐month outcome of acute stroke in Europe: data from a multicenter multinational hospital‐based registry. Stroke. 2003; 34:1114-1119 [DOI] [PubMed] [Google Scholar]
- 36.Heuschmann PU, Kolominsky‐Rabas PL, Misselwitz B, Hermanek P, Leffmann C, Janzen RW, Rother J, Buecker‐Nott HJ, Berger KGerman Stroke Registers Study Group. Predictors of in‐hospital mortality and attributable risks of death after ischemic stroke. Arch Intern Med. 2004; 164:1761-1768 [DOI] [PubMed] [Google Scholar]
- 37.Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project—1981–86. 2. Incidence, case fatality rates and overall outcome at one year of cerebral infarction, primary intracerebral and subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 1990; 53:16-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwamm LH, Holloway RG, Amarenco P, Audebert HJ, Bakas T, Chumbler NR, Handschu R, Jauch EC, Knight WA, IV, Levine SR, Mayberg M, Meyer BC, Meyers PM, Skalabrin E, Wechsler LRAmerican Heart Association Stroke Council; Interdisciplinary Council on Peripheral Vascular Disease. A review of the evidence for the use of telemedicine within stroke systems of care. Stroke. 2009; 40:2616-2634 [DOI] [PubMed] [Google Scholar]
- 39.Gladstone DJ, Rodan LH, Sahlas DJ, Lee L, Murray BJ, Ween JE, Perry JR, Chenkin J, Morrison LJ, Beck S, Black SE. A citywide prehospital protocol increases access to stroke thrombolysis in Toronto. Stroke. 2009; 40:3841-3844 [DOI] [PubMed] [Google Scholar]


