Abstract
Background
Control of blood pressure (BP) remains a major challenge in primary care. Innovative interventions to improve BP control are therefore needed. By updating and combining data from 2 previous systematic reviews, we assess the effect of pharmacist interventions on BP and identify potential determinants of heterogeneity.
Methods and Results
Randomized controlled trials (RCTs) assessing the effect of pharmacist interventions on BP among outpatients with or without diabetes were identified from MEDLINE, EMBASE, CINAHL, and CENTRAL databases. Weighted mean differences in BP were estimated using random effect models. Prediction intervals (PI) were computed to better express uncertainties in the effect estimates. Thirty‐nine RCTs were included with 14 224 patients. Pharmacist interventions mainly included patient education, feedback to physician, and medication management. Compared with usual care, pharmacist interventions showed greater reduction in systolic BP (−7.6 mm Hg, 95% CI: −9.0 to −6.3; I2=67%) and diastolic BP (−3.9 mm Hg, 95% CI: −5.1 to −2.8; I2=83%). The 95% PI ranged from −13.9 to −1.4 mm Hg for systolic BP and from −9.9 to +2.0 mm Hg for diastolic BP. The effect tended to be larger if the intervention was led by the pharmacist and was done at least monthly.
Conclusions
Pharmacist interventions – alone or in collaboration with other healthcare professionals – improved BP management. Nevertheless, pharmacist interventions had differential effects on BP, from very large to modest or no effect; and determinants of heterogeneity could not be identified. Determining the most efficient, cost‐effective, and least time‐consuming intervention should be addressed with further research.
Keywords: hypertension, pharmacist, prediction interval, systematic review, team‐based care
Introduction
Elevated blood pressure (BP) is a major cause of death worldwide.1 Although reduction of BP is a cornerstone of the prevention of cardiovascular diseases (CVD),2 numerous hypertensive patients do not achieve adequate BP control. In the United States in 2009‐2010, it was estimated that 53% of all hypertensive people and 40% of treated hypertensive people had uncontrolled BP.3 Lower rates of BP control have been reported in European countries.4
Innovative interventions to improve BP control are therefore needed in primary care, where management of hypertension takes place. One such approach is a greater use of community‐based models of care with the involvement of non‐physician healthcare professionals, specifically, pharmacists and nurses.5–6 The US Community Preventive Services Task Force has recently recommended team‐based care, including pharmacists, to improve BP control.7 Pharmacists are highly accessible healthcare professionals and a valuable asset in the management of hypertension.8–9 Recently, we conducted a systematic review and meta‐analysis of 30 RCTs underlining that pharmacist interventions – conducted alone or in collaboration with physicians or nurses – substantially reduced systolic and diastolic BP and helped control other major CVD risk factors (total and LDL cholesterol, smoking) among outpatients with CVD risk factors.9 In a second systematic review and meta‐analysis of 15 RCTs, we showed that pharmacist interventions were associated with a better control of systolic and diastolic BP and other major CVD risk factors (total and LDL cholesterol, body mass index) among outpatients with diabetes.10
However, in both systematic reviews, a major issue was that various pharmacist interventions were evaluated in different clinical settings with a substantial heterogeneity in the effect estimates on BP. Therefore, some interventions are possibly more efficient than others to reduce BP. The identification of the more efficient pharmacist interventions on BP is of major importance to guide policy and to decide which intervention should be recommended. However, it requires the comparison of data on a large number of studies. Therefore, we combined and updated BP data from these 2 previous systematic reviews to assess the effect of pharmacist interventions on BP among outpatients and to identify determinants of heterogeneity.
Methods
Data were updated and combined from 2 previous systematic reviews of RCTs in which we assessed the effect of pharmacist interventions on CVD risk factors among outpatients.9–10 Both reviews were conducted following the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) recommendations11 and using methods outlined in the Cochrane Handbook for Systematic Reviews of Interventions,12 including the preparation of a protocol and analysis plan.
Research Methods
Details of the research methods are given in the original publications.9–10 Briefly, both reviews used the same selection criteria (study design, interventions, and outcomes), search strategy, study selection, data extraction, and assessment of risk of bias across the included studies. The first review included patients with any modifiable CVD risk factors but excluded studies, which targeted patients with diabetes.9 The second review included only studies including patients with diabetes.10 For both reviews, we included RCTs evaluating the effect of pharmacist intervention delivered by a pharmacist alone or in collaboration with other healthcare professionals, among adult outpatients with any modifiable CVD risk factors (hypertension, dyslipidemia, diabetes, smoking, or obesity) compared with the usual care group.
Pharmacist interventions were classified using the a priori‐defined categories of pharmacist‐directed care (pharmacist initiated and managed interventions) or as pharmacist collaborative care (pharmacist collaborated in interventions conducted with other health care professionals).13
Search strategy and study selection
The description of the search strategy and the flow diagram of assessed and included studies in each review are given in detail in the 2 original publications.9–10 Briefly, we searched, in collaboration with a research librarian (A.L.C.), the following electronic databases: MEDLINE via PubMed, EMBASE, CINAHL, and CENTRAL for published articles using predefined search terms. The first review, which excluded studies on patients with diabetes, retrieved articles up to November 2010, while the second review of patients with diabetes retrieved articles up to March 2012. For the current review, an update of the original literature searches of both reviews was conducted in September 2013. For the current review, we considered only studies where systolic or diastolic BP was the outcome and presented as weighted mean differences in BP.
Data extraction and assessment of risk of bias
A data extraction form was created and pilot tested with some eligible studies and then finalized.
In both reviews, data extraction was independently preformed by 2 authors (V.S. and A.C.). Discrepancies were resolved through discussion. Extracted data included: (1) study author, year of publication, and country where the study was conducted; (2) study characteristics (including study setting and design, duration of follow‐up, and sample size); (3) participants characteristics (including sex, age, CVD risk factors, and medications); (4) characteristics of interventions (including description and frequency of the pharmacist intervention); (5) characteristics of usual care group; and (6) types of outcome measure. Details of pharmacist interventions were documented using the a priori‐defined categories of pharmacist‐directed care or pharmacist collaborative care.13
The risk of bias for all included studies was independently assessed by 2 authors (V.S. and A.C.) using the Cochrane Risk of Bias Tool, a validated tool for quality in RCTs,12 which addresses random sequence generation, allocation concealment, blinding of outcome assessors, completeness of outcome data, selective outcome reporting, and other potential bias (e.g., important baseline imbalance in patient characteristics). Each of these 6 domains in the tool was rated as (1) low risk of bias; (2) unclear risk of bias; and (3) high risk of bias. A study was of high quality if it had a low risk of bias on ≥4 of the 6 domains in the tool.
Statistical Analysis
Data were analyzed using Stata 12.0 software (StataCorp LP). Outcomes of interest were systolic BP and diastolic BP. Heterogeneity in the effect of interventions was expected across studies and random effect models were used to estimate intervention effects and 95% confidence intervals (CI).14 Effects were calculated as weighted mean differences in BP between intervention and usual care group.
Between studies heterogeneity was quantified using the I2 statistic. To better express uncertainties in the effect estimates, 95% prediction intervals (PI) were computed because they are advocated in case of substantial heterogeneity. While the CI quantifies the accuracy of the mean effect, the PI quantifies the dispersion (or distribution) of effect estimates15–16 and will include the true effect from a unique study 95% of the time.16 The PI is wider than the CI unless there is no heterogeneity.
Reasons for heterogeneity in effect estimates should be sought in meta‐analyses.14 To explore the possible sources of heterogeneity, we conducted subgroup analyses according to selected study characteristics: (1) country where the study was conducted; (2) setting (outpatient clinic versus community pharmacy); (3) including patients with diabetes or not; (4) type of pharmacist care (pharmacist‐led care versus collaborative care); (5) type of interventions, (6) including a nurse or not in the intervention; and (7) frequency of intervention. Statistical significance of between subgroup differences was evaluated by meta‐regression.17
Publication bias was evaluated with funnel plots to check symmetrical distribution and convergence toward the pooled effect, along with Egger tests. Further, sensitivity analyses were performed (1) excluding relatively small studies (with fewer than 80 participants per randomization group) and (2) restricting analyses to studies of high quality.
Results
Study Selection
Initially, 30 RCTs with 19 studies having BP outcome were included in the first systematic review.9 Of the 5522 additional citations identified in the updated searches of this first review, 33 potentially relevant full‐text studies were assessed and screened; 10 additional RCTs met the inclusion criteria, with 6 studies having BP as outcome. Initially, 15 RCTs with 12 studies having BP as outcome were included in the second systematic review.10 Of the 2742 additional citations identified in the updated searches of the second review, 10 potentially relevant full‐text studies were assessed and screened; 2 additional RCTs met the inclusion criteria with 2 studies having BP as outcome. Overall, with the update, data from 39 RCTs with BP as outcome are included in the current review.
Study and Patient Characteristics
Thirty‐nine RCTs representing a total of 14 224 patients were included for the current review. Trials were published between 1973 and 2013 in peer‐reviewed journals. Details of included studies are given in Table S1. Most trials were conducted in the USA or Canada (N=25); 4 trials18–21 were conducted in European countries and 10 trials22–31 in Asia, South America, and Australia.
The within‐study mean age of participants ranged from 48 to 77 years (mean, 62 years). Overall, 53% of participants were women. The mean duration of follow‐up was 8.3 months (median, 6 months; range, 3 to 13 months). For most trials19–20,19–28,19–52 (N=31), participants were followed‐up in outpatient clinics or by general practitioners; 6 trials8,18–19,18–55 were conducted in community pharmacy and 2 trials21,29 in both outpatient clinics and community pharmacies.
The interventions were led by the pharmacist in 23 studies and conducted in collaboration with other healthcare professionals, such as physician, nurse, dietitian, or physical therapist, in 16 studies (Table S1). In the 16 pharmacist collaborative care studies, the team composition was pharmacist/physician (N=10); pharmacist/nurse/physician (N=3); pharmacist/nurse/physician/dietitian or nutritionist therapist (N=2), or pharmacist/nurse (N=1). Overall, a nurse was involved in the intervention in 6 studies.
The interventions consisted of (1) patient education and counseling about lifestyle, medication and medication adherence (N=35 studies); (2) feedback to healthcare professional (including drug‐related problems identification; recommendation to physician for medication change; team meeting, development of treatment plan) (N=35); (3) medication management (including drug monitoring with adjustment or change in medication) (N=34); (4) measurement of BP, hypertension staging and risk of stratification, and reviewing of home BP measurements (N=13); (5) reminder system (including telephone contact, web services, home visits, or drug adherence aid) (N=12); and (6) healthcare professional education (including training program) (N=2).
The frequency of intervention was monthly or more frequently in 17 studies and less frequently than once a month in 11 studies. In the 11 remaining studies, the frequency of intervention was irregular (e.g., at every patient encounter) or not clearly specified.
Overall, study quality was moderate (Figure S1), with considerable variation in quality. Sixteen studies were considered of relatively high quality. In all studies, the participants were not blinded to the intervention.
Main Results
The outcome included systolic BP in 39 studies, involving 14 224 patients, and diastolic BP in 36 studies, involving 13 826 patients. On average, pharmacist interventions were associated with a large reduction in systolic and diastolic BP of −7.6 mm Hg (95% CI: −9.0 to −6.3 mm Hg) and −3.9 mm Hg (95% CI: −5.1 to −2.8 mm Hg), respectively (Figures 1A and 1B). There was a substantial heterogeneity for systolic (I2=67%) and diastolic BP (I2=83%). The 95% PI ranged from −13.9 to −1.4 mm Hg for systolic BP and from −9.9 to +2.0 mm Hg for diastolic BP.
Figure 1.
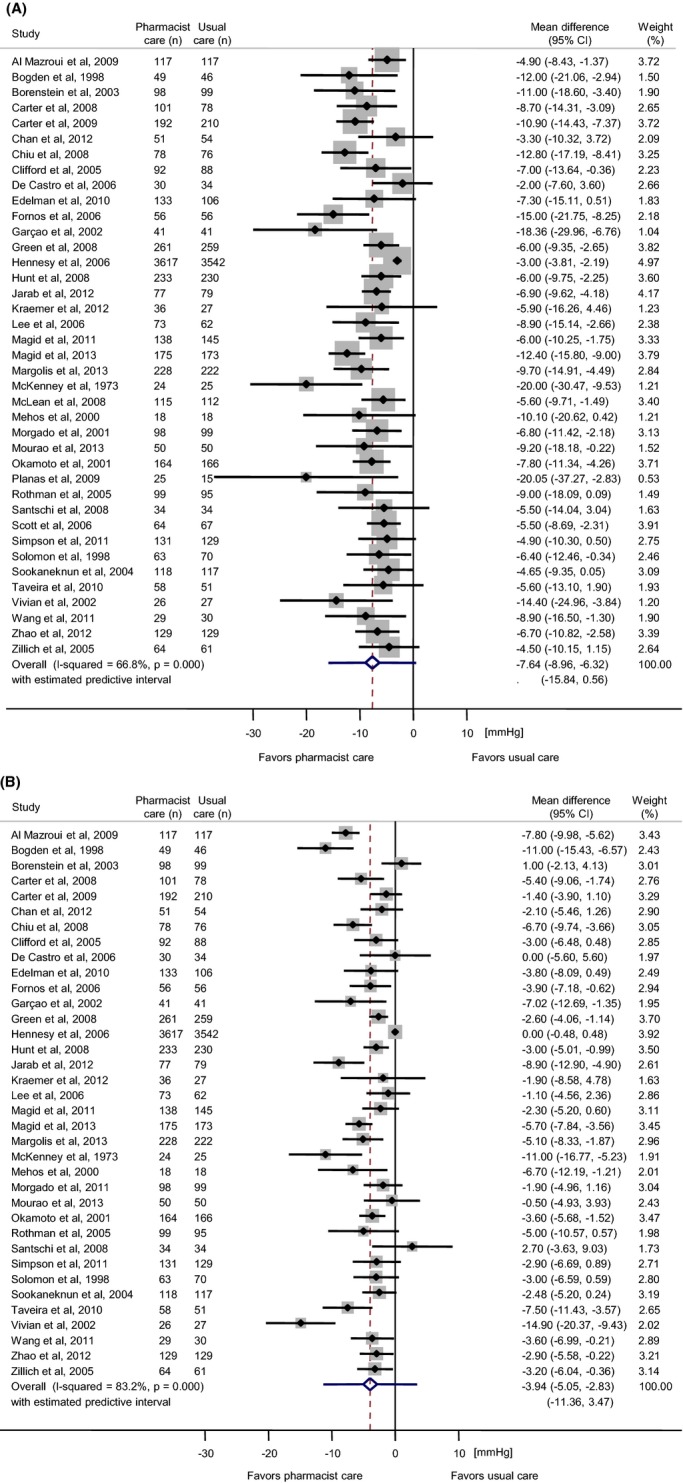
Forest plot of the mean difference in (A) systolic and (B) diastolic blood pressure with pharmacist care compared with usual care group. n=number of participants.
Subgroup Analyses
Results of subgroup analyses according to selected study characteristics are summarized in Table. No difference was observed in BP reductions according to the country where the study was conducted, to the type of interventions (data not shown), to the involvement or not of a nurse in the intervention, or to the inclusion or not of patients with diabetes. The effect was slightly better if the intervention was conducted in community pharmacies. A more substantial difference in effect on BP was observed according to the type of pharmacist care, pharmacist‐led care being associated with a larger effect on systolic and diastolic BP compared with collaborative care (Table, Figures 2A and 2B; systolic BP: −8.5 mm Hg [95% CI, −10.0 to −7.0 mm Hg] versus −6.3 mm Hg [95% CI, −8.0 to −4.5], P=0.046; diastolic BP: −4.6 mm Hg [95% CI, −5.7 to −3.4 mm Hg] versus −2.8 mm Hg [95% CI, −4.4 to −1.2 mm Hg], P=0.10). Furthermore, the effect on BP tended to be more important if the intervention was conducted monthly or more frequently compared with less frequently than once a month (Table, Figures 3A and 3B; systolic BP: −9.1 mm Hg [95% CI, −11.4 to −6.7 mm Hg] versus −6.7 mm Hg [95% CI, −9.1 to −4.4 mm Hg], P=0.14; diastolic BP: −4.5 mm Hg [95% CI, −6.1 to −2.9] versus −1.9 mm Hg [95% CI, −3.5 to −0.3 mm Hg], P=0.08). Nevertheless, the differences between these subgroups reached statistical significance (P<0.05) only for the difference in systolic BP according to the type of pharmacist care. Furthermore, the between‐study heterogeneity within subgroups remained substantial in most analyses.
Table 1.
Subgroup Analyses for the Difference in Systolic and Diastolic Blood Pressure With Pharmacist Care Compared With Usual Care Group According to Study Characteristics
| Study Characteristics | Systolic Blood Pressure Mean Difference (mm Hg) | Between Subgroup Differences | Diastolic Blood Pressure Mean Difference (mm Hg) | Between Subgroup Difference | ||
|---|---|---|---|---|---|---|
| N | (95% CI) | P Value | N | (95% CI) | P Value | |
| Country | ||||||
| US/Canada | 25 | −7.8 (−9.6 to −6.1) | Ref | 22 | −4.1 (−5.5 to −2.7) | Ref |
| Other countries | 14 | −7.3 (−9.2 to −5.4) | 0.83 | 14 | −3.7 (−5.3 to −2.2) | 0.76 |
| Setting | ||||||
| Outpatient clinics/GP | 31 | −7.5 (−8.9 to −6.1) | Ref | 29 | −4.0 (−5.2 to −2.7) | Ref |
| Community pharmacy | 6 | −10.5 (−15.7 to −5.3) | 0.29 | 5 | −5.0 (−7.6 to −2.3) | 0.51 |
| Other | 2 | −4.9 (−9.0 to −0.7) | 0.39 | 2 | −0.7 (−2.5 to 2.7) | 0.22 |
| Targeted patients | ||||||
| Without diabetes | 25 | −8.2 (−10.0 to −6.3) | Ref | 25 | −3.7 (−5.0 to −2.5) | Ref |
| With diabetes | 14 | −6.4 (−7.8 to −5.1) | 0.37 | 11 | −4.5 (−6.3 to −2.8) | 0.51 |
| Pharmacist care | ||||||
| Collaborative care | 16 | −6.3 (−8.0 to −4.5) | Ref | 14 | −2.8 (−4.4 to −1.2) | Ref |
| Pharmacist‐led care | 23 | −8.5 (−10.0 to −7.0) | 0.046 | 22 | −4.6 (−5.7 to −3.4) | 0.10 |
| Nurse interventions | ||||||
| Without nurse | 33 | −7.8 (−9.3 to −6.3) | Ref | 32 | −4.0 (−5.1 to −2.8) | Ref |
| With nurse | 6 | −6.5 (−8.5 to −4.4) | 0.65 | 4 | −3.8 (−7.7 to 0.1) | 0.92 |
| Frequency of intervention | ||||||
| Once a month or more frequently | 17 | −9.1 (−11.4 to −6.7) | Ref | 16 | −4.5 (−6.1 to −2.9) | Ref |
| Less than once a month | 11 | −6.7 (−9.1 to −4.4) | 0.14 | 9 | −1.9 (−3.5 to −0.3) | 0.08 |
| Irregular or not clearly specified | 11 | −7.1 (−8.6 to −5.6) | 0.22 | 11 | −4.6 (−6.1 to −3.0) | 0.93 |
N indicates number of studies.
Figure 2.
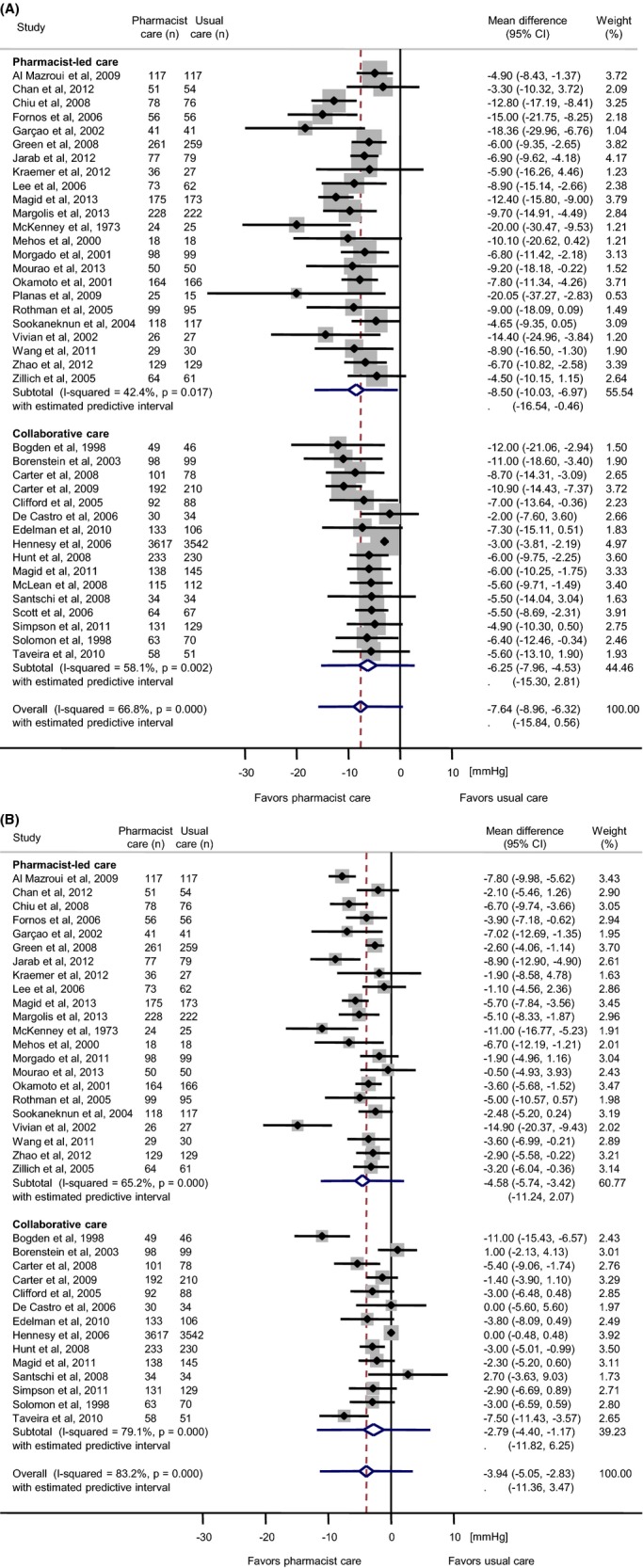
Forest plot of the mean difference in (A) systolic and (B) diastolic blood pressure with pharmacist care compared with usual care group according to type of care (pharmacist‐led care vs collaborative care). n=number of participants.
Figure 3.
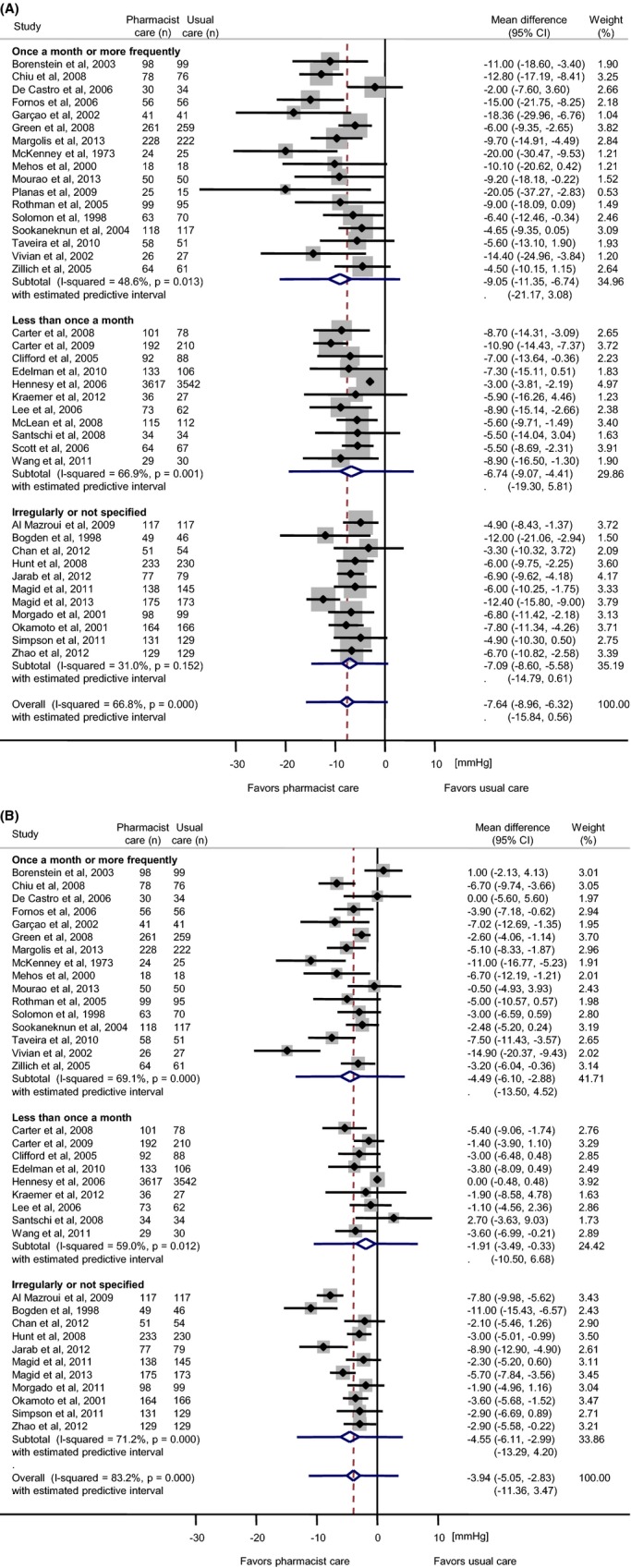
Forest plot of the mean difference in (A) systolic and (B) diastolic blood pressure with pharmacist care compared with usual care group according to frequency of intervention (once a month or more frequently, less than once a month, irregularly/not specified). n=number of participants.
Publication Bias and Sensitivity Analysis
Asymmetries in the funnel plots were observed for both systolic and diastolic BP. The Egger test results were statistically significant (P<0.001 for systolic BP; P<0.001 for diastolic BP). To account for this potential publications bias and to evaluate the impact of relatively small studies, we conducted a first sensitivity analysis restricted to the 19 studies with >80 patients per arm. For these studies, the weighted mean difference between pharmacist intervention and usual care was −7.0 mm Hg (95% CI, −8.7 to −5.4 mm Hg; I2=72%) for systolic BP and −3.1 mm Hg (95% CI, −4.4 to −1.8 mm Hg; I2=84%) for diastolic BP. These differences were of the same magnitude compared with the differences observed when all studies were included.
The second sensitivity analysis was restricted to the 16 studies of relatively high quality. For these studies, the weighted mean difference between pharmacist intervention and usual care was −7.3 mm Hg (95% CI, −8.6 to −6.0 mm Hg; I2=8%) for systolic BP and −3.6 mm Hg (95% CI, −4.6 to −2.6 mm Hg; I2=41%) for diastolic BP. These differences were of the same magnitude compared with the differences observed when all studies were included.
Discussion
By updating and combining data from our previous systematic reviews, we analyzed data from 39 RCTs including 14 224 outpatients. Findings from the current review are similar to those of the 2 previous systematic reviews: positive evidence was found supporting pharmacist interventions for improving systolic and diastolic BP control among outpatients. The observed effect was indeed substantial compared with powerful antihypertensive drugs like loop diuretics that decrease systolic blood pressure, on average, by 8 mm Hg.56 The interventions – conducted by the pharmacist alone or in collaboration with physician, nurse or dietitian, or physical therapist – were most often educational interventions to patients about medication, lifestyle and physical activity, feedback to physician (such as recommendation regarding medications changes or problems to medication adherence), and medication management (such as drug monitoring with adjustment or change in medication). A substantial heterogeneity in the effect estimate was observed for both systolic and diastolic BP. Although our subgroup analyses could not explain this heterogeneity, interventions led by the pharmacist tended to be more effective. Furthermore, interventions conducted at least monthly might be more effective, albeit the difference did not reach statistical significance. Finally, wide prediction intervals were observed, suggesting differential effects of pharmacist interventions on BP in individual studies, from a very large effect to modest or no effect.
Findings from the current systematic review and meta‐analysis are consistent with previous reviews showing that pharmacist‐led care or involved in a team‐based care with physician or nurse improves patient health outcomes6,57 including BP control.5,9–10 In most RCTs included in this updated and combined review, complex pharmacist interventions with multiple components (i.e., co‐interventions) were evaluated, making it difficult to identify precisely which component of the intervention was more potent to control BP. Despite the large number of included studies, our analyses did not clearly identify which (aspect of the) intervention is the most efficient. We have shown in a previous review that the number of interventions was not associated with a better BP control.9 In this current combined review, we observed a slightly larger effect on BP with pharmacist‐led care compared with pharmacist interventions implemented in collaboration with other health professionals. Nevertheless, the difference was modest.
Our findings that the effect on BP was slightly greater if the intervention was led by the pharmacist differ to some extend from a recent umbrella review of systematic reviews evaluating the effectiveness of community pharmacist intervention.58 Mossialos et al58 reported mixed or inconclusive evidence in support of expanding the role of community pharmacist in healthcare delivery. One reason for the difference may be that the review by Mossialos et al58 was focused specifically on community pharmacists. Our review evaluated not only studies with community pharmacist interventions but also clinical pharmacist interventions working, for example in outpatient clinic or medical groups. Nevertheless, we agree with Mossialos et al58 that expanding the role of community pharmacist needs significant changes in healthcare systems, further training of pharmacists and involves policy development.
Furthermore, based on a thorough review, the team‐based hypertension care has been recently recommended by the US Preventive Services Task Forces as an effective strategy to improve BP, with nonphysician healthcare professionals – involving pharmacist, nurses, dietitian – working in collaboration with physician and sharing responsibilities of hypertension care.7 Comparative effectiveness studies are therefore needed to determine the most efficient interventions and long‐term effect.
Potentially important components of effective pharmacist interventions such as adequate pharmacist training (e.g., measurement of BP or management of hypertension) and remuneration for services (e.g., reviews of medications, resolution of drug related‐problems, patient counseling to improve adherence) should be considered to better understand the heterogeneity of the results of pharmacist interventions reported here. Another possible factor that might explain the reported difference in the reviewed papers is the various types of healthcare delivery system. Indeed, pharmacist involvement is typical and well accepted in the care, for example in the United States or in Canada, compared with European countries, and that could influence the effect size of pharmacist interventions. Obstacles to the implementation of intervention should be also considered. It would be especially relevant for policy recommendations to have such information. However, and this is one limitation of the current review, information about these factors was not available or only partly reported in the studies identified.
To better express uncertainties in the effect estimates of pharmacist intervention, we reported prediction intervals.15–16 When there is substantial heterogeneity, the interpretation of the mean effect and the related confidence interval may be problematic, especially when the statistical heterogeneity is due to true clinical heterogeneity.15 Prediction interval reveals the distribution of effect estimates for individual studies, and our results suggest that there could be large differences in effect estimates, with some intervention having modest or no effect on BP. Prediction interval gives the range of effects that would be expected from a new study with similar characteristics to the current studies. Reporting prediction intervals can be enlightening especially when complex healthcare interventions, with expected true clinical heterogeneity in their effects, are evaluated.
Some limitations should be considered in interpreting the results of this study. Asymmetries in funnel plots were clearly observed for systolic and diastolic BP, and this may reflect a publication bias.59 Indeed, such a bias is possible because we did not search systematically for unpublished studies and because small studies showing no or weak effect of pharmacist intervention may not have been published. Nevertheless, our sensitivity analyses did not suggest any major impact of small studies on the effect estimates. Furthermore, the asymmetry may also be due to other factors, such as the heterogeneity of the effect of interventions.59 The difference reached statistical significance only for the difference in the effect on systolic BP between collaborative care and pharmacist‐led care. However, statistical tests with meta‐regression in meta‐analyses are known to have low power to show statistically significant differences between subgroups. The absence of statistically significant differences does not exclude the possibility of a true and clinically relevant difference in effect size. Therefore, we considered with precaution that the effect size could differ according to the frequency of interventions and the type of care despite the absence of statistically significant differences in most comparisons.
Another limitation is that the quality of studies was moderate on average. A reassuring observation is the consistency of the effect on BP when the analysis was restricted to high‐quality studies: no difference was observed compared to the effect estimates when all studies were included. The relatively short duration of follow‐up (median of 6 months) is also a limitation. It is indeed possible that the effect of pharmacist interventions could be reduced over a longer duration of follow‐up, as reported in a recent RCT evaluating the effect of home BP telemonitoring and pharmacist management on BP control.43 Finally, a cost‐effectiveness analysis of these interventions is lacking. This would help determine which intervention should be preferably implemented.
In addition to contributing to the current state of literature supporting the beneficial effects of pharmacists interventions in BP control, our findings underline that the impact of long‐term (e.g., >1 year) pharmacist interventions on BP control is lacking. Moreover, most of the included studies evaluating the impact of pharmacist care on BP among outpatients were conducted in the United States and Canada, reflecting an enhanced and more successfully implemented role of pharmacist in these healthcare systems.
Conclusions
Our meta‐analysis shows evidence that pharmacist interventions improve BP control in outpatients compared with usual care. Given the large heterogeneity between studies, it is difficult to predict which effect size would be expected when implementing such interventions in practice. Comparative effectiveness studies, with a long duration of follow‐up, are still needed to determine the most efficient, implementable, cost‐effective, and least time‐consuming intervention for improving BP control in various healthcare systems.
Sources of Funding
This project was supported in part by the Canadian Institutes of Health Research (CIHR) from the Applied Public Health research Chair in Chronic Diseases Prevention to G. Paradis, and by research and development funding from the Department of Community Medicine and Health, CHUV, Lausanne, Switzerland. The funders have no role in study design, data collection and analysis, decision to publish, or preparation to the manuscript.
Disclosures
None.
References
- 1.Lawes CM, Vander Hoorn S, Rodgers AInternational Society of Hypertension. Global burden of blood pressure‐related disease, 2001. Lancet. 2008; 371:1513-1518 [DOI] [PubMed] [Google Scholar]
- 2.U.S. Preventive Services Task Force. Screening for high blood pressure: U.S. Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2007; 147:783-786 [DOI] [PubMed] [Google Scholar]
- 3.Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health and Nutrition Examination Survey, 2001 to 2010. Circulation. 2012; 126:2105-2114 [DOI] [PubMed] [Google Scholar]
- 4.Wolf‐Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, Poulter N, Primatesta P, Stegmayr B, Thamm M. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004; 43:10-17 [DOI] [PubMed] [Google Scholar]
- 5.Carter BL, Bosworth HB, Green BB. The hypertension team: the role of the pharmacist, nurse, and teamwork in hypertension therapy. J Clin Hypertens. 2012; 14:51-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chisholm‐Burns MA, Kim Lee J, Spivey CA, Slack M, Herrier RN, Hall‐Lipsy E, Graff Zivin J, Abraham I, Palmer J, Martin JR, Kramer SS, Wunz T. US pharmacists' effect as team members on patient care: systematic review and meta‐analyses. Med Care. 2010; 48:923-933 [DOI] [PubMed] [Google Scholar]
- 7.Community Preventive Services Task Force. The community guide to community preventive services Available at: http://www.thecommunityguide.org/cvd/supportingmaterials/IS-team-based-care.html. Accessed January, 2014. [DOI] [PubMed]
- 8.McLean DL, McAlister FA, Johnson JA, King KM, Makowsky MJ, Jones CA, Tsuyuki RT. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists‐hypertension (SCRIP‐HTN). Arch Intern Med. 2008; 168:2355-2361 [DOI] [PubMed] [Google Scholar]
- 9.Santschi V, Chiolero A, Burnand B, Colosimo AL, Paradis G. Impact of pharmacist care in the management of cardiovascular disease risk factors: a systematic review and meta‐analysis of randomized trials. Arch Intern Med. 2011; 171:1441-1453 [DOI] [PubMed] [Google Scholar]
- 10.Santschi V, Chiolero A, Paradis G, Colosimo AL, Burnand B. Pharmacist interventions to improve cardiovascular disease risk factors in diabetes: a systematic review and meta‐analysis of randomized controlled trials. Diabetes Care. 2012; 35:2706-2717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. 2008Chichester, West Sussex, UK; Hoboken NJ: Wiley‐Blackwell [Google Scholar]
- 13.Koshman SL, Charrois TL, Simpson SH, McAlister FA, Tsuyuki RT. Pharmacist care of patients with heart failure: a systematic review of randomized trials. Arch Intern Med. 2008; 168:687-694 [DOI] [PubMed] [Google Scholar]
- 14.Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta‐analyses. BMJ. 2011; 342:d549. [DOI] [PubMed] [Google Scholar]
- 15.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Prediction intervals. Introduction to Meta‐Analysis. 2009Chichester, UK: John Wiley & Sons, Ltd; 127-133 [Google Scholar]
- 16.Chiolero A, Santschi V, Burnand B, Platt RW, Paradis G. Meta‐analyses: with confidence or prediction intervals? Eur J Epidemiol. 2012; 27:823-825 [DOI] [PubMed] [Google Scholar]
- 17.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Notes on subgroup analyses and meta‐regression. Introduction to Meta‐Analysis. 2009Chichester, UK: John Wiley & Sons, Ltd; 205-212 [Google Scholar]
- 18.Fornos JA, Andres NF, Andres JC, Guerra MM, Egea B. A pharmacotherapy follow‐up program in patients with type‐2 diabetes in community pharmacies in Spain. Pharm World Sci. 2006; 28:65-72 [DOI] [PubMed] [Google Scholar]
- 19.Garcao JA, Cabrita J. Evaluation of a pharmaceutical care program for hypertensive patients in rural Portugal. J Am Pharm Assoc (Wash). 2002; 42:858-864 [DOI] [PubMed] [Google Scholar]
- 20.Morgado M, Rolo S, Castelo‐Branco M. Pharmacist intervention program to enhance hypertension control: a randomised controlled trial. Int J Clin Pharm. 2011; 33:132-140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Santschi V, Rodondi N, Bugnon O, Burnier M. Impact of electronic monitoring of drug adherence on blood pressure control in primary care: a cluster 12‐month randomised controlled study. Eur J Intern Med. 2008; 19:427-434 [DOI] [PubMed] [Google Scholar]
- 22.Al Mazroui NR, Kamal MM, Ghabash NM, Yacout TA, Kole PL, McElnay JC. Influence of pharmaceutical care on health outcomes in patients with type 2 diabetes mellitus. Br J Clin Pharmacol. 2009; 67:547-557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan CW, Siu SC, Wong CK, Lee VW. A pharmacist care program: positive impact on cardiac risk in patients with type 2 diabetes. J Cardiovasc Pharmacol Ther. 2012; 17:57-64 [DOI] [PubMed] [Google Scholar]
- 24.Chiu CC, Wu SS, Lee PY, Huang YC, Tan TY, Chang KC. Control of modifiable risk factors in ischemic stroke outpatients by pharmacist intervention: an equal allocation stratified randomized study. J Clin Pharm Ther. 2008; 33:529-535 [DOI] [PubMed] [Google Scholar]
- 25.Clifford RM, Davis WA, Batty KT, Davis TM. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care. 2005; 28:771-776 [DOI] [PubMed] [Google Scholar]
- 26.de Castro MS, Fuchs FD, Santos MC, Maximiliano P, Gus M, Moreira LB, Ferreira MB. Pharmaceutical care program for patients with uncontrolled hypertension. Report of a double‐blind clinical trial with ambulatory blood pressure monitoring. Am J Hypertens. 2006; 19:528-533 [DOI] [PubMed] [Google Scholar]
- 27.Jarab AS, Alqudah SG, Mukattash TL, Shattat G, Al‐Qirim T. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm. 2012; 18:516-526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mourao AO, Ferreira WR, Martins MA, Reis AM, Carrillo MR, Guimaraes AG, Ev LS. Pharmaceutical care program for type 2 diabetes patients in Brazil: a randomised controlled trial. Int J Clin Pharm. 2013; 35:79-86 [DOI] [PubMed] [Google Scholar]
- 29.Sookaneknun P, Richards RM, Sanguansermsri J, Teerasut C. Pharmacist involvement in primary care improves hypertensive patient clinical outcomes. Ann Pharmacother. 2004; 38:2023-2028 [DOI] [PubMed] [Google Scholar]
- 30.Wang J, Wu J, Yang J, Zhuang Y, Chen J, Qian W, Tian J, Chen X, She D, Peng F. Effects of pharmaceutical care interventions on blood pressure and medication adherence of patients with primary hypertension in China. Clin Res Regul Aff. 2011; 28:1-6 [Google Scholar]
- 31.Zhao PX, Wang C, Qin L, Yuan M, Xiao Q, Guo YH, Wen AD. Effect of clinical pharmacist's pharmaceutical care intervention to control hypertensive outpatients in China. Afr J Pharm Pharmacol. 2012; 6:48-56 [Google Scholar]
- 32.Bogden PE, Abbott RD, Williamson P, Onopa JK, Koontz LM. Comparing standard care with a physician and pharmacist team approach for uncontrolled hypertension. J Gen Intern Med. 1998; 13:740-745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borenstein JE, Graber G, Saltiel E, Wallace J, Ryu S, Archi J, Deutsch S, Weingarten SR. Physician‐pharmacist comanagement of hypertension: a randomized, comparative trial. Pharmacotherapy. 2003; 23:209-216 [DOI] [PubMed] [Google Scholar]
- 34.Carter BL, Ardery G, Dawson JD, James PA, Bergus GR, Doucette WR, Chrischilles EA, Franciscus CL, Xu Y. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med. 2009; 169:1996-2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carter BL, Bergus GR, Dawson JD, Farris KB, Doucette WR, Chrischilles EA, Hartz AJ. A cluster randomized trial to evaluate physician/pharmacist collaboration to improve blood pressure control. J Clin Hypertens. 2008; 10:260-271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Edelman D, Fredrickson SK, Melnyk SD, Coffman CJ, Jeffreys AS, Datta S, Jackson GL, Harris AC, Hamilton NS, Stewart H, Stein J, Weinberger M. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med. 2010; 152:689-696 [DOI] [PubMed] [Google Scholar]
- 37.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, Carrell D, Tyll L, Larson EB, Thompson RS. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008; 299:2857-2867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hennessy S, Leonard CE, Yang W, Kimmel SE, Townsend RR, Wasserstein AG, Ten Have TR, Bilker WB. Effectiveness of a two‐part educational intervention to improve hypertension control: a cluster‐randomized trial. Pharmacotherapy. 2006; 26:1342-1347 [DOI] [PubMed] [Google Scholar]
- 39.Hunt JS, Siemienczuk J, Pape G, Rozenfeld Y, MacKay J, LeBlanc BH, Touchette D. A randomized controlled trial of team‐based care: impact of physician‐pharmacist collaboration on uncontrolled hypertension. J Gen Intern Med. 2008; 23:1966-1972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low‐density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006; 296:2563-2571 [DOI] [PubMed] [Google Scholar]
- 41.Magid DJ, Ho PM, Olson KL, Brand DW, Welch LK, Snow KE, Lambert‐Kerzner AC, Plomondon ME, Havranek EP. A multimodal blood pressure control intervention in 3 healthcare systems. Am J Manag Care. 2011; 17:e96-e103 [PubMed] [Google Scholar]
- 42.Magid DJ, Olson KL, Billups SJ, Wagner NM, Lyons EE, Kroner BA. A pharmacist‐led, American Heart Association Heart360 Web‐enabled home blood pressure monitoring program. Cir Cardiovasc Qual Outcomes. 2013; 6:157-163 [DOI] [PubMed] [Google Scholar]
- 43.Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, O'Connor PJ, Pritchard RA, Sekenski JL, Sperl‐Hillen JM, Trower NK. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013; 310:46-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mehos BM, Saseen JJ, MacLaughlin EJ. Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension. Pharmacotherapy. 2000; 20:1384-1389 [DOI] [PubMed] [Google Scholar]
- 45.Okamoto MP, Nakahiro RK. Pharmacoeconomic evaluation of a pharmacist‐managed hypertension clinic. Pharmacotherapy. 2001; 21:1337-1344 [DOI] [PubMed] [Google Scholar]
- 46.Planas LG, Crosby KM, Mitchell KD, Farmer KC. Evaluation of a hypertension medication therapy management program in patients with diabetes. J Am Pharm Assoc. 2009; 49:164-170 [DOI] [PubMed] [Google Scholar]
- 47.Rothman RL, Malone R, Bryant B, Shintani AK, Crigler B, Dewalt DA, Dittus RS, Weinberger M, Pignone MP. A randomized trial of a primary care‐based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am J Med. 2005; 118:276-284 [DOI] [PubMed] [Google Scholar]
- 48.Scott DM, Boyd ST, Stephan M, Augustine SC, Reardon TP. Outcomes of pharmacist‐managed diabetes care services in a community health center. Am J Health Syst Pharm. 2006; 63:2116-2122 [DOI] [PubMed] [Google Scholar]
- 49.Simpson SH, Majumdar SR, Tsuyuki RT, Lewanczuk RZ, Spooner R, Johnson JA. Effect of adding pharmacists to primary care teams on blood pressure control in patients with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2011; 34:20-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Solomon DK, Portner TS, Bass GE, Gourley DR, Gourley GA, Holt JM, Wicke WR, Braden RL, Eberle TN, Self TH, Lawrence BL. Clinical and economic outcomes in the hypertension and COPD arms of a multicenter outcomes study. J Am Pharm Assoc (Wash). 1998; 38:574-585 [DOI] [PubMed] [Google Scholar]
- 51.Taveira TH, Wu WC, Martin OJ, Schleinitz MD, Friedmann P, Sharma SC. Pharmacist‐led cardiac risk reduction model. Prev Cardiol. 2006; 9:202-208 [DOI] [PubMed] [Google Scholar]
- 52.Vivian EM. Improving blood pressure control in a pharmacist‐managed hypertension clinic. Pharmacotherapy. 2002; 22:1533-1540 [DOI] [PubMed] [Google Scholar]
- 53.Kraemer DF, Kradjan WA, Bianco TM, Low JA. A randomized study to assess the impact of pharmacist counseling of employer‐based health plan beneficiaries with diabetes: the EMPOWER study. J Pharm Pract. 2012; 25:169-179 [DOI] [PubMed] [Google Scholar]
- 54.McKenney JM, Slining JM, Henderson HR, Devins D, Barr M. The effect of clinical pharmacy services on patients with essential hypertension. Circulation. 1973; 48:1104-1111 [DOI] [PubMed] [Google Scholar]
- 55.Zillich AJ, Sutherland JM, Kumbera PA, Carter BL. Hypertension outcomes through blood pressure monitoring and evaluation by pharmacists (HOME study). J Gen Intern Med. 2005; 20:1091-1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Musini VM, Rezapour P, Wright JM, Bassett K, Jauca CD. Blood pressure lowering efficacy of loop diuretics for primary hypertension. Cochrane Database Syst Rev. 2012:CD003825. [DOI] [PubMed] [Google Scholar]
- 57.Blalock SJ, Roberts AW, Lauffenburger JC, Thompson T, O'Connor SK. The effect of community pharmacy‐based interventions on patient health outcomes: a systematic review. Med Care Res Rev. 2013; 70:235-266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mossialos E, Naci H, Courtin E. Expanding the role of community pharmacists: policymaking in the absence of policy‐relevant evidence? Health Policy. 2013; 111:135-148 [DOI] [PubMed] [Google Scholar]
- 59.Lau J, Ioannidis JP, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. BMJ. 2006; 333:597-600 [DOI] [PMC free article] [PubMed] [Google Scholar]


