Abstract
Background
Time in therapeutic range (TTR) is a standard quality measure of the use of warfarin. We assessed the relative effects of rivaroxaban versus warfarin at the level of trial center TTR (cTTR) since such analysis preserves randomized comparisons.
Methods and Results
TTR was calculated using the Rosendaal method, without exclusion of international normalized ratio (INR) values performed during warfarin initiation. Measurements during warfarin interruptions >7 days were excluded. INRs were performed via standardized finger‐stick point‐of‐care devices at least every 4 weeks. The primary efficacy endpoint (stroke or non‐central nervous system embolism) was examined by quartiles of cTTR and by cTTR as a continuous function. Centers with the highest cTTRs by quartile had lower‐risk patients as reflected by lower CHADS2 scores (P<0.0001) and a lower prevalence of prior stroke or transient ischemic attack (P<0.0001). Sites with higher cTTR were predominantly from North America and Western Europe. The treatment effect of rivaroxaban versus warfarin on the primary endpoint was consistent across a wide range of cTTRs (P value for interaction=0.71). The hazard of major and non‐major clinically relevant bleeding increased with cTTR (P for interaction=0.001), however, the estimated reduction by rivaroxaban compared with warfarin in the hazard of intracranial hemorrhage was preserved across a wide range of threshold cTTR values.
Conclusions
The treatment effect of rivaroxaban compared with warfarin for the prevention of stroke and systemic embolism is consistent regardless of cTTR.
Keywords: rivaroxaban, time in therapeutic range, warfarin
Introduction
Vitamin K antagonists (VKAs) have formed the basis for the prevention of stroke and systemic embolus in patients with atrial fibrillation (AF) for several decades.1 The major impediment to VKA use is the unpredictability of the level of anticoagulation at a given dose. The international normalized ratio (INR) has been introduced as a measure of anticoagulation that enables the clinician and patient to monitor the degree of anticoagulation when VKAs are used. When the INR is <1.8 the risk of stroke and systemic embolism increases, and when the INR is >3.5 the risk of bleeding increases.2 This range includes the standard range of INR 2.0 to 3.0 widely recommended for VKA treatment for patients with AF.3–4
The estimated time in the therapeutic range (TTR) of INR 2.0 to 3.0 has become a widely applied measure of the quality of VKA anticoagulation in patients with AF, with most studies using Rosendaal's interpolation method of calculating TTR.5 Several studies have shown a direct relationship between TTR and lower rates of stroke and systemic embolism in patients with AF, while the relationship to bleeding risk has been more variable.6–7 The ROCKET AF (Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation) trial had a prospective analysis plan to estimate the relationship between TTR and the treatment effect of rivaroxaban compared with warfarin.
ROCKET AF was a blinded randomized trial that directly compared warfarin treatment with a novel factor Xa inhibitor, rivaroxaban.8 While TTR was measurable in the warfarin‐treated participants in the ROCKET AF trial, it is not an appropriate measure of anticoagulation in patients treated with factor Xa inhibitors. As a result, it becomes problematic to compare rivaroxaban‐treated patients with warfarin‐treated patients who are grouped by individual‐level TTR values. The ROCKET AF trial prespecified the alternative approach of comparing the treatment effects of rivaroxaban versus warfarin stratified by center‐level TTR, thereby preserving randomized comparisons.
Methods
Trial Design
The design and primary results of ROCKET AF have been published.8–9 In brief, ROCKET AF was a multicenter, randomized, double‐blind, double‐dummy, event‐driven trial comparing rivaroxaban 20 mg daily (or 15 mg daily in patients with creatinine clearance 30 to 49 mL/min) with dose‐adjusted warfarin (target INR 2.0 to 3.0) for prevention of all stroke (ischemic or hemorrhagic) and systemic embolism.9 A double‐blind design was chosen to minimize bias in co‐interventions and reporting of clinical events. To maintain blinding, the INRatio (HemoSense) point‐of‐care device was used to generate real INR or sham values. The sham INR results were generated using a validated algorithm that reflected the distribution of INR values in a population of patients taking warfarin with clinical characteristics similar to the study population.9 The doses of warfarin and matching placebo tablets were titrated by the investigators based on these values.9
The trial was supported by research grants from Johnson & Johnson Pharmaceutical Research & Development and Bayer HealthCare AG. The Duke Clinical Research Institute in Durham, NC coordinated the trial and performed the statistical analyses for this manuscript independent of the sponsors. All appropriate national regulatory agencies and ethics/institutional review boards at each participating center approved the study. An international, multispecialty executive committee, designed the study and takes responsibility for the accuracy and completeness of all data and subsequent analyses.
Measurement of INR
The INR was measured prior to randomization. Subjects were randomized when the INR was <3.0. Post‐randomization INR monitoring was performed using the blinded point‐of‐care device. The ROCKET AF protocol recommended that INR monitoring be performed as clinically indicated, but no less frequently than every 4 weeks.
Calculation of TTR
We present TTR using the method of Rosendaal and colleagues, without exclusion of INR values obtained during the period at the start of study‐assigned warfarin therapy or during temporary discontinuations.5 We present analyses according to center TTR (cTTR) where cTTR was calculated as the percent of all INR values at each center that fell within the therapeutic range (2.0 to 3.0).
Statistical Methods
Baseline characteristics are shown as median (25th, 75th percentiles) for continuous variables and as percent (number) for categorical variables, and were compared among cTTR quartiles using Kruskal‐Wallis tests for continuous variables and Pearson chi‐square tests for categorical variables.
The risk of outcomes for patients randomized to rivaroxaban versus warfarin was assessed using Cox proportional hazards models with treatment as a covariate and using robust sandwich variance estimators to account for correlation within centers. All analyses were done in the safety on‐treatment population. The on‐treatment period was defined as the period during which the study drug was taken plus 2 days following permanent study drug discontinuation (ie, from first study drug dose to last dose plus 2 days). Safety analyses included patients from a good clinical practice (GCP)‐violating site while efficacy analyses excluded these patients (n=93). Risk relationships within regions or within cTTR quartiles were generated using models within those subgroups. The geographic regions were the same as those described in the main trial results.8 Comparison of these risk relationships across cTTR quartiles was achieved using a model that contained treatment, cTTR quartile, and their interaction. For further examination of the association of risk relationship to cTTR, a series of models was generated at different cTTR thresholds, ie, among all centers with cTTR at or above a certain value, ranging from 0% to 80%. All models were adjusted for geographic region, except subgroup models within regions. Risk relationships are expressed as hazard ratios with 95% confidence intervals. The probability of having an event by 1 year was also derived from the Cox models.
Results
Baseline Characteristics
ROCKET AF enrolled a high‐risk population with many risk factors for stroke and systemic embolism. Among the 14 264 randomized patients, the median age was 73 years, mean CHADS2 score was 3.5, 55% had prior thromboembolism, and 62.5% had heart failure. Among the 7133 randomized to warfarin, 7025 had INR data and the mean individual TTR in warfarin patients was 55%. The distribution of cTTR across all sites is shown in Figure 1. The mean cTTR was 59% and the median was 61% (25th, 75th: 51%, 69%). The baseline characteristics of the patients according to quartiles of cTTR are shown in Table 1. Centers with higher cTTR had lower‐risk patients as evidenced by lower CHADS2 scores (P<0.0001) and a lower prevalence of prior stroke or transient ischemic attack (TIA) (P<0.0001). Centers with higher cTTR were from regions with middle‐ and high‐income countries, including Western Europe and North America.
Figure 1.
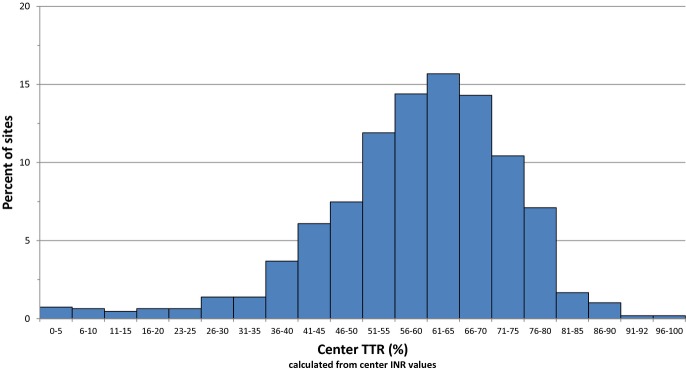
Distribution of cTTR across all sites. This histogram illustrates the distribution of the sites according to cTTR. cTTR indicates center time in therapeutic range; INR, international normalized ratio.
Table 1.
Baseline Characteristics According to Quartiles of cTTR
| Baseline Characteristics | cTTR Q1 (0.0% to 50.6%) (N=3430) | cTTR Q2 (50.7% to 58.5%) (N=3563) | cTTR Q3 (58.6% to 65.7%) (N=3496) | cTTR Q4 (65.7% to 100%) (N=3508) | P Value |
|---|---|---|---|---|---|
| Age, y | 70 (62, 76) | 72 (64, 77) | 74 (66, 78) | 75 (68, 80) | <0.0001 |
| Female | 44% (1506) | 41% (1450) | 39% (1368) | 35% (1222) | <0.0001 |
| Race | <0.0001 | ||||
| White | 73% (2490) | 85% (3011) | 83% (2904) | 92% (3231) | |
| Black | 1% (33) | 2% (56) | 2% (55) | 1% (34) | |
| Asian | 22% (767) | 11% (393) | 13% (441) | 5% (169) | |
| Other | 4% (140) | 3% (103) | 3% (96) | 2% (74) | |
| Region | <0.0001 | ||||
| Asia/Pacific Islands | 22% (766) | 11% (405) | 13% (462) | 13% (455) | |
| Eastern Europe | 57% (1947) | 50% (1797) | 35% (1210) | 12% (426) | |
| Latin America | 11% (378) | 16% (556) | 16% (573) | 10% (359) | |
| North America | 5% (182) | 12% (417) | 17% (592) | 40% (1417) | |
| Western Europe | 5% (157) | 11% (388) | 19% (659) | 24% (851) | |
| BMI, kg/m2 | 27.7 (24.7, 31.6) | 28.2 (25.1, 31.8) | 28.3 (25.1, 32.0) | 28.7 (25.6, 32.6) | <0.0001 |
| Systolic BP, mean (SD) | 132.7 (15.6) | 132.2 (15.9) | 132.1 (16.4) | 131.6 (17.1) | 0.0031 |
| AF type | 0.0001 | ||||
| Persistent | 81% (2788) | 82% (2930) | 79% (2761) | 82% (2868) | |
| Paroxysmal | 18% (604) | 17% (600) | 20% (685) | 16% (575) | |
| New onset | 1% (38) | 1% (33) | 1% (50) | 2% (65) | |
| Hypertension | 90% (3100) | 92% (3276) | 91% (3180) | 89% (3115) | <0.0001 |
| Diabetes | 37% (1262) | 39% (1385) | 42% (1454) | 42% (1460) | <0.0001 |
| Prior stroke or TIA | 58% (1995) | 53% (1891) | 51% (1798) | 47% (1657) | <0.0001 |
| CHF | 71% (2448) | 70% (2478) | 61% (2129) | 49% (1711) | <0.0001 |
| eGFR (MDRD) | 69.4 (57.1, 81.0) | 68.6 (56.7, 81.6) | 66.6 (55.9, 78.5) | 68.4 (56.3, 78.7) | <0.0001 |
| Hemoglobin, g/dL | 14.3 (13.2, 15.4) | 14.2 (13.2, 15.2) | 14.2 (13.1, 15.2) | 14.1 (13.1, 15.1) | <0.0001 |
| CAD | 20% (686) | 21% (754) | 23% (816) | 29% (1018) | <0.0001 |
| COPD | 10% (347) | 10% (345) | 10% (348) | 12% (417) | 0.010 |
| PAD | 6% (193) | 5% (169) | 6% (227) | 6% (227) | 0.0039 |
| Prior GI bleed | 2% (80) | 2% (60) | 4% (151) | 6% (195) | <0.0001 |
| Liver disease | 7% (252) | 4% (158) | 5% (187) | 4% (137) | <0.0001 |
| Alcohol consumption (past 12 months) | <0.0001 | ||||
| Abstinent | 75% (2586) | 69% (2454) | 64% (2227) | 51% (1793) | |
| Light | 22% (747) | 27% (956) | 31% (1096) | 41% (1430) | |
| Moderate | 2% (71) | 3% (122) | 4% (147) | 7% (263) | |
| Heavy | 1% (26) | 1% (31) | 1% (25) | 1% (21) | |
| CHADS2, mean (SD) | 3.5 (0.9) | 3.5 (0.9) | 3.5 (1.0) | 3.3 (1.0) | <0.0001 |
| CHADS2 score | <0.0001 | ||||
| 2 | 11% (364) | 11% (383) | 13% (446) | 18% (641) | |
| 3 | 42% (1456) | 45% (1597) | 43% (1511) | 44% (1541) | |
| 4 | 32% (1102) | 29% (1035) | 29% (1006) | 25% (872) | |
| 5 | 13% (456) | 14% (484) | 13% (444) | 11% (384) | |
| 6 | 2% (52) | 2% (64) | 3% (89) | 2% (70) | |
| VKA use at screening | 41% (1403) | 56% (1998) | 69% (2400) | 83% (2925) | <0.0001 |
| Chronic aspirin at screening | 45% (1542) | 41% (1446) | 32% (1127) | 29% (1005) | <0.0001 |
Continuous variables are shown as median (25th, 75th percentiles), except where noted. Categorical variables are shown as percent (number). P value is from Pearson chi‐square test for categorical variables, from Kruskal‐Wallis test for continuous variables. AF indicates atrial fibrillation; BMI, body mass index; BP, blood pressure; CAD, coronary artery disease; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; cTTR, center‐level time in therapeutic range; eGFR, glomerular filtration rate; GI, gastrointestinal; MDRD, Modification of Diet in Renal Disease; PAD, peripheral arterial disease; SD, standard deviation; TIA, transient ischemic attack; VKA, Vitamin K antagonist.
Geographic Variation in cTTR
The mean cTTR varied across geographic regions, as shown in Table 2. The highest mean cTTR occurred in North America (65%) and the lowest was observed in the Asia‐Pacific region and Eastern Europe (52%).
Table 2.
Mean cTTR and Treatment Effect Across Geographic Regions
| Region | Mean TTR (%) | Primary Efficacy Endpoint(Safety On‐Treatment Population) HR (95% CI) |
|---|---|---|
| North America | 65 | 0.61 (0.35, 1.06) |
| Western Europe | 64 | 0.87 (0.52, 1.46) |
| Latin America | 57 | 0.93 (0.62, 1.37) |
| Asia/Pacific Islands | 52 | 0.67 (0.44, 1.03) |
| Eastern Europe | 52 | 0.88 (0.67, 1.19) |
CI indicates confidence interval; cTTR, center‐level time in therapeutic range; HR, hazard ratio.
Outcomes and cTTR
The primary efficacy outcome (stroke or non‐central nervous system [CNS] embolism) for rivaroxaban versus warfarin is shown across the quartiles of cTTR in Table 3. Rates of stroke or non‐CNS embolism decreased with higher cTTR. The treatment effect with rivaroxaban on the primary endpoint across cTTR quartiles was consistent (P for interaction=0.71). The hazard ratio (HR) for the primary efficacy endpoint was 0.70 (95% confidence interval [CI] 0.47 to 1.04) in the lowest quartile of cTTR and 0.73 (0.50 to 1.06) in the highest quartile of cTTR. We repeated these analyses for the endpoint of ischemic stroke or non‐CNS systemic embolism and the results again showed no evidence of heterogeneity across cTTR quartiles (Table 4, interaction P=0.86).
Table 3.
Stroke and Non‐CNS Embolism by Quartiles of cTTR
| Center TTR | Rivaroxaban (N=6891) | Warfarin (N=7080) | Rivaroxaban vs Warfarin | |||
|---|---|---|---|---|---|---|
| n/J (%) | Event Rate (100 Pt‐Years) | n/J (%) | Event Rate (100 Pt‐Years) | HR (95% CI) | Interaction P Value* | |
| 0.00% to 50.6% | 45/1735 (2.6) | 1.8 | 62/1689 (3.7) | 2.5 | 0.70 (0.47, 1.04) | 0.709 |
| 50.7% to 58.5% | 53/1746 (3.0) | 1.9 | 63/1807 (3.5) | 2.2 | 0.90 (0.64, 1.26) | |
| 58.6% to 65.7% | 54/1734 (3.1) | 1.9 | 62/1758 (3.5) | 2.1 | 0.88 (0.62, 1.25) | |
| 65.7% to 100.0% | 37/1676 (2.2) | 1.3 | 55/1826 (3.0) | 1.8 | 0.73 (0.50, 1.06) | |
The population for this analysis was the safety on‐treatment population from sites with calculable cTTR. cTTR was calculated from all ITT warfarin patients at each center. All analyses are based on the time to first event. Event rates are the number of events per 100 patient‐years of follow‐up. HRs (95% CIs) are derived from a proportional hazards model with treatment as a covariate. CNS indicates central nervous system; cTTR, center‐level time in therapeutic range; J, number of subjects in each subgroup; n, number of subjects with events.
The P value for the interaction of treatment group and center‐based INR control group based on the Cox proportional hazard model including treatment group, center‐based INR control group, and their interaction.
Table 4.
Ischemic Stroke or Non‐CNS Systemic Embolism by Quartiles of cTTR
| Center TTR | Rivaroxaban (N=6891) | Warfarin (N=7080) | Rivaroxaban vs Warfarin | |||
|---|---|---|---|---|---|---|
| n/J (%) | Event Rate (100 Pt‐Year) | n/J (%) | Event Rate (100 Pt‐Year) | Hazard Ratio (95% CI) | Interaction P Value* | |
| 0.00% to 50.6% | 38/1735 (2.2) | 1.5 | 49/1689 (2.9) | 2.0 | 0.75 (0.48, 1.16) | 0.863 |
| 50.7% to 58.5% | 40/1746 (2.3) | 1.5 | 46/1807 (2.6) | 1.6 | 0.93 (0.61, 1.41) | |
| 58.6% to 65.7% | 43/1734 (2.5) | 1.5 | 46/1758 (2.6) | 1.6 | 0.95 (0.66, 1.40) | |
| 65.7% to 100.0% | 33/1676 (2.0) | 1.2 | 41/1826 (2.3) | 1.3 | 0.87 (0.58, 1.32) | |
The population for this analysis was the safety on‐treatment population from sites with calculable cTTR. cTTR was calculated from all ITT warfarin patients at each center. All analyses are based on the time to first event. Event rates are the number of events per 100 patient‐years of follow‐up. HRs (95% CIs) are derived from a proportional hazards model with treatment as a covariate. CNS indicates central nervous system; cTTR, center‐level time in therapeutic range; J, number of subjects in each subgroup; n, number of subjects with events.
The P value for the interaction of treatment group and center‐based INR control group based on the Cox proportional hazard model including treatment group, center‐based INR control group, and their interaction.
The lowest HR for the primary endpoint (rivaroxaban versus warfarin) was observed in the region with the highest cTTR (North America HR 0.61 [95% CI 0.35 to 1.06]). There was no evidence of an interaction between region and treatment (P for interaction=0.62).
As shown in Table 5, the rates of the primary safety endpoint (major and non‐major clinically relevant bleeding) increased with higher cTTR. In the lowest quartile of cTTR, rivaroxaban was associated with a lower hazard of bleeding (HR 0.80 [95% CI 0.66 to 0.98]), while in the top quartile of cTTR, rivaroxaban was associated with a higher hazard of bleeding (HR 1.25 [95% CI 1.10 to 1.41]; P for interaction=0.001).
Table 5.
Major and Non‐Major Clinically Relevant Bleeding by Quartiles of cTTR
| Center TTR | Rivaroxaban (N=6941) | Warfarin (N=7123) | Rivaroxaban vs Warfarin | |||
|---|---|---|---|---|---|---|
| n/J (%) | Event Rate (100 Pt‐Years) | n/J (%) | Event Rate (100 Pt‐Years) | HR (95% CI) | Interaction P Value* | |
| 0.00% to 50.71% | 271/1780 (15.2) | 11.30 | 315/1734 (18.2) | 14.12 | 0.80 (0.66, 0.98) | 0.001* |
| 50.89% to 58.44% | 285/1731 (16.5) | 11.72 | 313/1785 (17.5) | 12.21 | 0.96 (0.81, 1.14) | |
| 58.46% to 65.66% | 381/1741 (21.9) | 15.10 | 378/1765 (21.4) | 14.88 | 1.03 (0.87, 1.22) | |
| 65.71% to 100.0% | 484/1689 (28.7) | 20.61 | 443/1839 (24.1) | 16.72 | 1.25 (1.10, 1.41) | |
The population for this analysis was safety on‐treatment patients from sites with calculable cTTR. cTTR was calculated from all safety warfarin patients at each center. Therefore, the quartiles are slightly different from Table 3. All analyses are based on the time to first event. Event rates are number of events per 100 patient‐years of follow‐up. HRs (95% CIs) are derived from a proportional hazard model with treatment as a covariate. cTTR indicates center‐level time in therapeutic range; J, number of subjects in each subgroup; n, number of subjects with events.
The P value for the interaction of treatment group and center‐based INR control group based on the Cox proportional hazard model including treatment group, center‐based INR control group, and their interaction.
Figure 2 displays the modeled risk of stroke or non‐CNS embolism, with 95% confidence limits, according to treatment assignment (rivaroxaban or warfarin) and cTTR viewed as a continuous variable. Centers with higher cTTR values had a lower risk of stroke and non‐CNS embolism in both rivaroxaban‐ and warfarin‐treated patients. Figure 3 illustrates the treatment effect (rivaroxaban versus warfarin) at increasing thresholds of cTTR. The treatment effect was relatively consistent across the range of cTTR values. Figure 4 provides the same display for the endpoint of intracranial hemorrhage. The estimated reduction in the hazard of intracranial hemorrhage was preserved across a wide range of threshold cTTR values. There is no evidence that the benefit of rivaroxaban for prevention of intracranial bleeding is lost at any level of cTTR (Figure 4).
Figure 2.
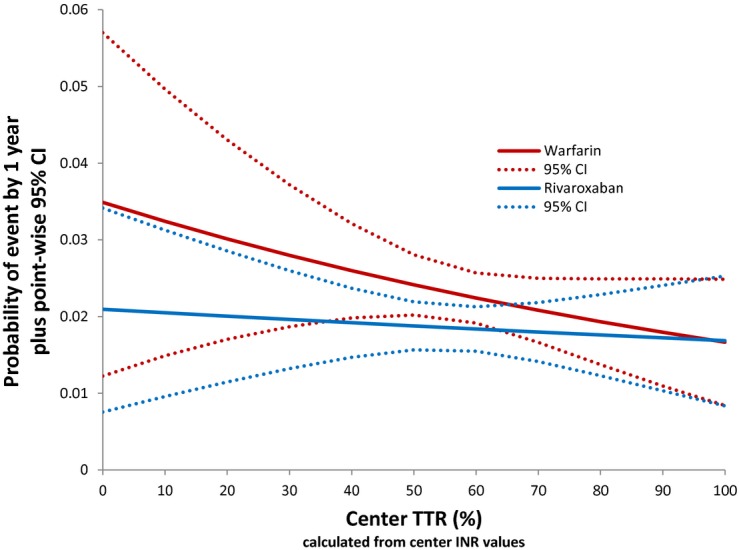
Probability of stroke or non‐CNS embolism in rivaroxaban and warfarin treated patients according to cTTR. cTTR is shown on the x‐axis. Probability of stroke or non‐CNS embolism by 1‐year of follow‐up is shown on the y‐axis. This plot shows the probability of having a stroke or non‐CNS embolism according to cTTR for rivaroxaban‐ and warfarin‐treated patients (solid lines) with corresponding 95% CIs (dashed lines). Centers with higher cTTR values had a lower risk of stroke and systemic embolus in both the rivaroxaban‐ and warfarin‐treated arms. CNS indicates central nervous system; cTTR, center time in therapeutic range; INR, international normalized ratio.
Figure 3.
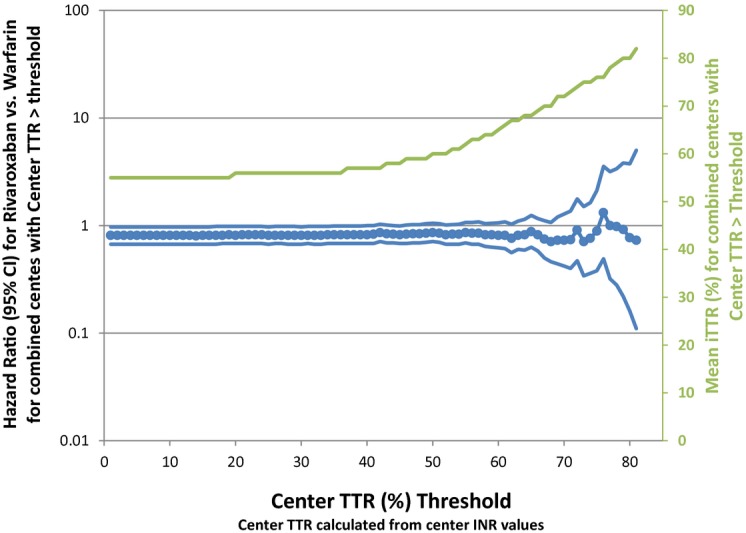
Treatment effect for the reduction of stroke or non‐CNS embolism in rivaroxaban and warfarin treated patients at a given cTTR threshold. The x‐axis shows the threshold value for cTTR and the y‐axis shows the HR for the time to stroke or non‐CNS embolism for rivaroxaban vs warfarin given a certain threshold cTTR. The y‐axis also shows the mean individual TTR in those centers that meet the threshold cTTR. There is instability in the estimate of the treatment effect at high cTTR thresholds due to smaller sample size, but no evidence that warfarin is superior to rivaroxaban in the prevention of stroke and systemic embolus at any cTTR threshold. CNS indicates central nervous system; cTTR, center time in therapeutic range; INR, international normalized ratio.
Figure 4.
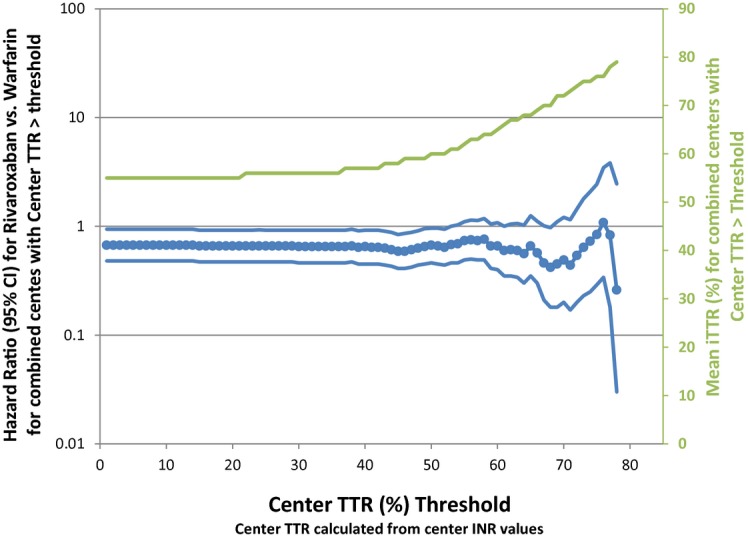
Risk of intracranial hemorrhage in rivaroxaban‐ vs warfarin‐treated patients according to cTTR at a given threshold. The x‐axis shows the threshold value for cTTR and the y‐axis shows the HR for the time to stroke or non‐CNS embolism for rivaroxaban vs warfarin given a certain threshold cTTR. The y‐axis also shows the mean individual TTR in those centers that meet the threshold cTTR. There is instability in the estimate of the treatment effect at high cTTR thresholds due to smaller sample size, but no evidence that warfarin is superior to rivaroxaban in the prevention of stroke and systemic embolus at any cTTR threshold. CNS indicates central nervous system; cTTR, center time in therapeutic range; INR, international normalized ratio.
Discussion
TTR is a widely used measure of quality of anticoagulation with warfarin. In the ROCKET AF trial the TTR correlated negatively with risk of stroke and systemic embolism, although TTR correlated positively with risk of bleeding. However, despite a wide variation of TTR levels across centers in the trial there was no evidence that the relative efficacy of rivaroxaban versus warfarin varied by cTTR.
TTR is impacted by a host of factors.7,10 Multiple comorbidities such as heart failure, liver and lung disease, and renal disease can alter INR control.11 While none of these individually have a major impact on TTR, in aggregate they have a significant impact. Perhaps more important is the adherence of the patient, which is dependent on many social, cultural, financial, and individual behavioral characteristics in addition to the direction of the prescriber.12–13 Some studies have shown that instrumental factors such as distance between the clinic and home and availability of transportation are important. We recently published the finding that the region, and more importantly, the country involved has a major impact on TTR, far outweighing all the other factors routinely measured in clinical practice or clinical trials.10 A recent analysis from the RE‐LY (Randomized Evaluation of Long‐Term Anticoagulation Therapy) trial found that much of the variation in cTTR values could be explained by whether or not an algorithmic approach to warfarin management was used.14
The relationships among TTR, outcomes, and treatment effect in the ROCKET AF trial cannot be directly assessed at the individual patient level using iTTR since it is not meaningful in patients treated with rivaroxaban. Furthermore, because TTR is a post‐randomization covariate, patients with different TTR levels are likely to have different levels of stroke and bleeding risk independent of TTR. Identifying appropriate comparator patients assigned to rivaroxaban (for whom INR values are not available) is not possible with suitable accuracy, so using it to adjust the estimate of treatment effect violates usual principles of analysis and abrogates the advantages gained by randomization.15 Because of these concerns, we and others have compared patients assigned to rivaroxaban and warfarin stratified by center‐level TTR, where the analysis still benefits from randomization.16 However, analysis at the center level allows only indirect inference about the effect of individual‐level TTR, ie, iTTR. Moreover, our analysis demonstrated that centers with higher cTTR have patients with different comorbidity profiles, including lower‐risk patients as indicated by lower CHADS2 scores and lower event rates even among the centers' patients taking rivaroxaban.
While we saw no overall relationship between cTTR and the relative effect of rivaroxaban versus warfarin, we did not have sufficient power to specifically examine centers achieving TTR levels above 70. Analyses from the large RE‐LY and ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trials also found no relationship between cTTR and the estimate of the treatment effect, including sites with cTTR >70.16–17
The increase in bleeding that we observed in centers with higher cTTR levels is consistent with higher INR levels seen in such centers. Worldwide in centers with poor TTR, the most common deviation is almost always with persistent low values rather than high values. This likely explains the preservation of the benefit for intracranial hemorrhage regardless of cTTR. Some regions of the world have more aversion to bleeding than others leading to more cautious adjustments to VKA doses.18–19
One consideration in understanding the cTTR values is the actual observed event rates in the trial on warfarin therapy. In ROCKET AF, the observed event rates for a CHADS2 score of 2 was 1.7, for CHADS2 score of ≥3 was 2.6, and for prior stroke patients was 2.9 events per 100 patient‐years versus 1.4, 2.8, and 3.2 in the ARISTOTLE trial which had a higher TTR on average. These data provide additional support for the concept that cTTR depends on a complex mix of factors, with practitioner skill being only one of them. For example, simply measuring more INRs will lead to a higher TTR, assuming that appropriate changes in doses are made. In countries with closer proximity of clinics to patients and with fewer cost constraints, INRs tend to be measured more frequently.
The question of whether there is a cTTR that is too low to allow for a valid direct comparison of a new anticoagulant with warfarin merits serious consideration. At the extreme, if cTTR was very low, one would expect the comparator treatment to be superior if it was effective. While no direct measure of TTR was available in most of the controlled trials of warfarin in AF, best estimates using meta‐analysis indicate a TTR in the range of 61%.20 The average TTR in US practice is 55% and recent data indicate that in clinical practice, TTR values are typically below 60%.2,21 Furthermore, the region with the highest TTR (North America), had the largest point estimate for treatment difference in favor of rivaroxaban, a finding that was not statistically significant, but the existing trend favors no impact of cTTR on estimates of the rivaroxaban treatment effect.
Limitations
The limitations of this analysis should be considered. These results emanate from a randomized, blinded trial at selected centers in a high‐risk population. TTR is a post‐randomization variable and therefore, the entire analysis has uncertainties and should be considered to provide a perspective akin to a sensitivity analysis. Furthermore, the analysis of cTTR in this study and in other trials has limited power.
Conclusion
TTR is an important and validated quality measure for VKA management. However, TTR does not impact the estimate of the treatment effect of rivaroxaban versus warfarin for the prevention of stroke and systemic embolism. The consistency of this finding with other major trials of novel anticoagulants versus warfarin16–17 and the observation of expected event rates on warfarin treatment in ROCKET AF provide support for this conclusion. Regardless of the choice of anticoagulation, adherence factors related to education, cultural factors, economics, and transportation need to be considered in designing systems of care for stroke prevention as well as medical comorbidities and access to expert medical care from skilled clinicians.
Sources of Funding
Supported by research grants from Johnson & Johnson Pharmaceutical Research & Development (Raritan, NJ) and Bayer HealthCare AG (Leverkusen, Germany).
Disclosures
Piccini: Research grants from GE Healthcare and Janssen; consulting fees from Forest Laboratories, Janssen, Medtronic, Pfizer/BMS, and Spectranetics. Hellkamp: None. Lokhnygina: None. Patel: Research grant from Astra Zeneca; consulting fees from Ortho McNeil. Janssen and Bayer HealthCare; advisory board for Genzyme. Harrell: None. Singer: Consulting fees from Bayer Healthcare, Boehringer Ingelheim, Bristol‐Myers Squibb, Daiichi Sankyo, Johnson & Johnson, Pfizer, CSL Behring; research grant from Johnson & Johnson. Becker: Research support from Bayer and Johnson & Johnson (modest); scientific advisory boards for Bayer. Breithardt: Honoraria from Johnson & Johnson and Bayer; advisory board fees from Boehringer Ingelheim, Bristol‐Myers Squibb, Pfizer, and Sanofi‐Aventis. Halperin: Consulting fees from Astellas Pharma, Boehringer Ingelheim, Bristol‐Myers Squibb, Daiichi Sankyo, Pfizer, and Sanofi Aventis; serves as chair of the data safety monitoring committee for the EUCLID trial, sponsored by AstraZeneca. Hankey: Consulting and advisory board fees from Bayer Pharmaceuticals, Boehringer Ingelheim, Bristol‐Myers Squibb, Pfizer; honoraria from Bayer Pharmaceuticals and theHeart.org. Berkowitz: Employee of Bayer HealthCare Pharmaceuticals. Nessel: Employee of Janssen Research & Development. Mahaffey: Consulting fees from Bayer, Boehringer Ingelheim, Bristol‐Myers Squibb, Daiichi Sankyo, Eli Lilly, GlaxoSmithKline, Johnson & Johnson, Merck, Ortho/McNeill, Pfizer, PolyMedix; grant support from AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Eli Lilly, GlaxoSmithKline, Johnson & Johnson, Merck, Portola, Regado Biotechnologies, Sanofi, The Medicines Company. Fox: Grant support and lecture fees from Eli Lilly; lecture fees from Sanofi Aventis and AstraZeneca. Califf: Consulting fees from Kowa, Nile, Orexigen, Sanofi Aventis, Novartis, and Xoma; grant support from Novartis, Merck, and Amilyn/Lilly; equity interest in Nitrox.
References
- 1.Jackson K, Gersh BJ, Stockbridge N, Fleming TR, Temple R, Califf RM, Connolly SJ, Wallentin L, Granger CB. Antithrombotic drug development for atrial fibrillation: proceedings, Washington, DC, July 25‐27, 2005. Am Heart J. 2008; 155:829-840 [DOI] [PubMed] [Google Scholar]
- 2.Wan Y, Heneghan C, Perera R, Roberts N, Hollowell J, Glasziou P, Bankhead C, Xu Y. Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes. 2008; 1:84-91 [DOI] [PubMed] [Google Scholar]
- 3.Estes NA, III, Halperin JL, Calkins H, Ezekowitz MD, Gitman P, Go AS, McNamara RL, Messer JV, Ritchie JL, Romeo SJ, Waldo AL, Wyse DG. ACC/AHA/Physician Consortium 2008 clinical performance measures for adults with nonvalvular atrial fibrillation or atrial flutter. Circulation. 2008; 117:1101-1120 [DOI] [PubMed] [Google Scholar]
- 4.Singer DE, Chang Y, Fang MC, Borowsky LH, Pomernacki NK, Udaltsova N, Go AS. Should patient characteristics influence target anticoagulation intensity for stroke prevention in nonvalvular atrial fibrillation? The ATRIA study. Circ Cardiovasc Qual Outcomes. 2009; 2:297-304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosendaal FR, Cannegieter SC, van der Meer FJ, Briet E. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost. 1993; 69:236-239 [PubMed] [Google Scholar]
- 6.Hylek EM, Go AS, Chang Y, Jensvold NG, Henault LE, Selby JV, Singer DE. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med. 2003; 349:1019-1026 [DOI] [PubMed] [Google Scholar]
- 7.Samsa GP, Matchar DB. Relationship between test frequency and outcomes of anticoagulation: a literature review and commentary with implications for the design of randomized trials of patient self‐management. J Thromb Thrombolysis. 2000; 9:283-292 [DOI] [PubMed] [Google Scholar]
- 8.Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883-891 [DOI] [PubMed] [Google Scholar]
- 9. Rivaroxaban–once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation: rationale and design of the ROCEKT AF study. Am Heart J. 2010; 159:340-347.e341 [DOI] [PubMed] [Google Scholar]
- 10.Singer DE, Hellkamp AS, Piccini JP, Mahaffey KW, Lokhnygina Y, Pan G, Halperin JL, Becker RC, Breithardt G, Hankey GJ, Hacke W, Nessel CC, Patel MR, Califf RM, Fox KA. Impact of global geographic region on time in therapeutic range on warfarin anticoagulant therapy: data from the ROCKET AF clinical trial. J Am Heart Assoc. 2013; 2:e000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rose AJ, Hylek EM, Ozonoff A, Ash AS, Reisman JI, Berlowitz DR. Patient characteristics associated with oral anticoagulation control: results of the veterans affairs study to improve anticoagulation (VARIA). J Thromb Haemost. 2010; 8:2182-2191 [DOI] [PubMed] [Google Scholar]
- 12.Hasan SS, Shamala R, Syed IA, Basariah N, Chong DW, Mei TK, Chin OH. Factors affecting warfarin‐related knowledge and INR control of patients attending physician‐ and pharmacist‐managed anticoagulation clinics. J Pharm Pract. 2011; 24:485-493 [DOI] [PubMed] [Google Scholar]
- 13. Determinants of warfarin use and international normalized ratio levels in atrial fibrillation patients in Japan: subanalysis of the J‐RHYTHM Registry. Circ J. 2011; 75:2357-2362 [DOI] [PubMed] [Google Scholar]
- 14.Van Spall HG, Wallentin L, Yusuf S, Eikelboom JW, Nieuwlaat R, Yang S, Kabali C, Reilly PA, Ezekowitz MD, Connolly SJ. Variation in warfarin dose adjustment practice is responsible for differences in the quality of anticoagulation control between centers and countries: an analysis of patients receiving warfarin in the randomized evaluation of long‐term anticoagulation therapy (RE‐LY) trial. Circulation. 2012; 126:2309-2316 [DOI] [PubMed] [Google Scholar]
- 15.Yusuf S, Wittes J, Probstfield J, Tyroler HA. Analysis and interpretation of treatment effects in subgroups of patients in randomized clinical trials. JAMA. 1991; 266:93-98 [PubMed] [Google Scholar]
- 16.Wallentin L, Yusuf S, Ezekowitz MD, Alings M, Flather M, Franzosi MG, Pais P, Dans A, Eikelboom J, Oldgren J, Pogue J, Reilly PA, Yang S, Connolly SJ. Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: an analysis of the RE‐LY trial. Lancet. 2010; 376:975-983 [DOI] [PubMed] [Google Scholar]
- 17.Wallentin L, Lopes RD, Hanna M, Thomas L, Hellkamp A, Nepal S, Hylek EM, Al‐Khatib SM, Alexander JH, Alings M, Amerena J, Ansell J, Aylward P, Bartunek J, Commerford P, De Caterina R, Erol C, Harjola VP, Held C, Horowitz JD, Huber K, Husted S, Keltai M, Lanas F, Lisheng L, McMurray JJ, Oh BH, Rosenqvist M, Ruzyllo W, Steg PG, Vinereanu D, Xavier D, Granger CB. Efficacy and safety of apixaban compared with warfarin at different levels of predicted international normalized ratio control for stroke prevention in atrial fibrillation. Circulation. 2013; 127:2166-2176 [DOI] [PubMed] [Google Scholar]
- 18.Yamaguchi T. Optimal intensity of warfarin therapy for secondary prevention of stroke in patients with nonvalvular atrial fibrillation: a multicenter, prospective, randomized trial. Japanese Nonvalvular Atrial Fibrillation‐Embolism Secondary Prevention Cooperative Study Group. Stroke. 2000; 31:817-821 [DOI] [PubMed] [Google Scholar]
- 19.Inoue H. Thromboembolism in patients with nonvalvular atrial fibrillation: comparison between Asian and Western countries. J Cardiol. 2013; 61:1-7 [DOI] [PubMed] [Google Scholar]
- 20.Reynolds MW, Fahrbach K, Hauch O, Wygant G, Estok R, Cella C, Nalysnyk L. Warfarin anticoagulation and outcomes in patients with atrial fibrillation: a systematic review and metaanalysis. Chest. 2004; 126:1938-1945 [DOI] [PubMed] [Google Scholar]
- 21.Baker WL, Cios DA, Sander SD, Coleman CI. Meta‐analysis to assess the quality of warfarin control in atrial fibrillation patients in the United States. J Manag Care Pharm. 2009; 15:244-252 [DOI] [PMC free article] [PubMed] [Google Scholar]


